Abstract
Background
The association between early outpatient follow-up and 30-day readmission has not been evaluated in any surgical population. Our study characterizes the relationship between outpatient follow-up and early readmissions among surgical patients.
Methods
We queried the medical record at a large, tertiary care institution (July 2008-December 2012) to determine rates of 30-day outpatient follow-up and readmission for general or vascular surgical procedures.
Results
The majority of discharges for general (84% of 7552) and vascular (75% of 2362) surgery had a follow-up visit before readmission or within 30 days of discharge. General surgery patients who were not readmitted had high rates of follow-up (88%) and received follow-up at approximately 2-weeks post-discharge (median time 11 days after discharge). In contrast, readmitted general surgery patients received first follow-up at one week (a median time of 8 days); 49% had follow-up. Vascular surgery patients showed a similar trend. Over half of patients readmitted after follow-up were readmitted within 24 hours of their most recent outpatient visit.
Conclusions
Current routine follow-up does not occur early enough to detect adverse events and prevent readmission. Early outpatient care may prevent readmission in some patients, but often serves as a conduit for readmission among patients already experiencing complications.
Keywords: Readmission, Rehospitalization. General Surgery, Vascular Surgery, Outpatient Care
BACKGROUND
Outpatient follow-up (FU) is a routine part of the post-operative process intended to evaluate and monitor patient’s recovery from surgery. Ideally, the follow-up visit should allow detection of any anomalies in the patient’s recovery. If follow-up visits are timed appropriately, they may allow early treatment of complications and preclude costly and morbid hospital readmissions. The objective of this study is to determine whether current outpatient follow-up patterns are adequate to allow the timely diagnosis and treatment of post discharge complications after general or vascular surgical procedures, thus preventing the need for hospital readmission.
Unplanned readmission within 30 days of a surgical discharge has been established as a quality of care indicator.1 Medicare is increasingly instituting financial penalties for higher-than-expected readmissions rates as part of the Readmissions Reduction Program created by the Affordable Care Act of 2010.2 Consequently, both hospital administrators and healthcare providers have prioritized reducing 30-day hospital readmission rates. Several interventions have been designed to reduce readmissions, including improved discharge planning, patient education, and medication reconciliation, among others.3 These interventions are broadly classified into pre-discharge, post-discharge, and bridging/coordinating interventions.3
Timely outpatient follow-up has been evaluated and is inconsistently associated with readmission. This has been studied for the most part in patients with medical illnesses. Several investigators have demonstrated a decreased risk of readmission for patients with timely follow-up with their primary care physician.4,5 For example, early outpatient follow-up led to decreased readmission rates for patients with congestive heart failure and atrial fibrillation.6,7 In contrast, in patients treated for myocardial infarction, aggressive follow-up did not significantly lower rates of readmission.8
The importance of early outpatient follow-up in preventing readmission has not been evaluated in a surgical population. One possible reason for this is that outpatient follow-up after surgery is not captured by traditional claims databases, such as Medicare. This is because global billing for most open surgical procedures, which is 90 days, is inclusive of the payment for outpatient visits during that interval. Thus there are no registered or paid claims for these visits. To overcome this limitation, we utilized data from the electronic medical record from a large, tertiary care institution and evaluated follow-up visits and compared these to readmission rates for patients undergoing general or vascular surgical procedures. Our study provides a description of the relationship between outpatient follow-up and 30-day readmissions among surgical patients.
METHODS
We used data derived from a review of the electronic medical record at a single tertiary care institution from July 2008 through December 2012 for all general (GS) and vascular surgical (VS) procedures performed as part of an inpatient hospitalization as previously described.9 The hospital business planning and analysis office created the data set by querying the institutional medical record. This study was approved by the University of Wisconsin, Madison Health Sciences Institutional Review Board.
Study cohort inclusion required an inpatient surgical procedure performed by a surgeon on the general or vascular surgery service. Patients excluded from this analysis were pediatric patients (age less than 18 years old at time of procedure), those who died during the initial hospitalization, patients discharged against medical advice, and patients with a scheduled readmission within 30 days of initial discharge. Qualifying admissions more than 30 days after discharge were treated as separate primary admission; only one admission/readmission pair per patient was allowed within a given 30 day period. Outpatient encounters within the single-hospital system were linked to inpatient hospitalizations using the patient identification number. For readmitted patients, outpatient visits were excluded from the analysis if they occurred after readmission. For patients without a subsequent readmission, outpatient visits occurring within 30 days of initial discharge were included. We excluded outpatient visits if they were for a specific test, study, or service involving a limited aspect of care (e.g. laboratory tests, radiology studies, rehabilitation services). These visits were excluded to ensure that the outpatient follow-up was a meaningful visit with a surgeon, primary care provider, or another medical specialist.
Sociodemographic characteristics obtained from the medical record included age (years), race (white or non-white), gender, proximity to primary hospital (in-county versus remote residence), and insurance type (fee for service, HMO, Medicare, Medicaid, and other/self-pay). Additional statistical descriptions of the initial hospitalization included the length of stay (days), severity of illness (3M All Patient Refined Diagnosis Related Groups classification),10 discharge destination (home, home with home health care, SNF, rehabilitation, and other facility), and whether the hospitalization included time spent in an intensive care unit (ICU).
Our level of analysis is the hospitalization rather than the patient. Descriptive analyses, including frequencies, medians, and percentages, were performed using STATA 12 software (StataCorp LP, College Station, TX) and R statistical software.11 Descriptive characteristics are summarized with percentages or median with associated interquartile range where appropriate. Graphics depicting follow-up and readmission timelines were generated using the ggplot2 package in R.12
RESULTS
Sociodemographic and Clinical Characteristics Associated with Follow-up
There were 7552 discharges (6620 unique patients) from the general surgery service during the study period, and vascular surgery had 2362 discharges (2000 unique patients). The majority of patients undergoing general or vascular surgical procedures had at least one outpatient follow-up visit (84% and 75% respectively) within 30 days of discharge or prior to readmission. Sociodemographic and clinical characteristics were significantly associated with whether the patient received follow-up care in each surgical group (Table 1). The patients most likely to receive any outpatient care within 30 days following discharge were disproportionately white, were locally residing, had lower disease severity, and experienced shorter lengths of stay. They were more likely to have private insurance, no ICU stay, and a routine procedure. Women were more likely to have follow-up in general surgery, but this difference was not as pronounced for vascular surgery.
Table 1.
Univariate Analysis of Follow-up and Sociodemographic/Clinical Characteristics
| % with Follow-up for General Surgery | % with Follow-up for Vascular Surgery | |||
|---|---|---|---|---|
| Male | 82.3% | * | 74.5% | |
| Female | 85.7% | 76.5% | ||
| White | 84.4% | * | 75.9% | * |
| Black | 78.5% | 78.8% | ||
| Other | 83.8% | 53.7% | ||
| In-county Residence | 87.5% | * | 90.9% | * |
| Remote Residence | 81.3% | 69.1% | ||
| Low severity illness | 86.9% | * | 86.1% | * |
| Moderate severity illness | 88.4% | 80.1% | ||
| High severity illness | 82.5% | 72.9% | ||
| Very high severity illness | 61.2% | 55.7% | ||
| Routine | 90.4% | * | 77.6% | * |
| Emergent/Urgent | 75.2% | 71.2% | ||
| ICU Stay | 43.3% | * | 65.6% | * |
| No ICU Stay | 84.8% | 75.6% | ||
| Fee for Service | 85.2% | * | 80.0% | * |
| Health Maintenance Org. | 88.9% | 91.7% | ||
| Medicaid | 79.6% | 76.3% | ||
| Medicare | 82.3% | 72.9% | ||
| Other/Self Pay | 75.6% | 58.3% | ||
| Discharged Home | 87.3% | * | 79.2% | * |
| Discharged Home Health | 86.8% | 77.8% | ||
| Discharged to skilled nursing facility | 69.4% | 74.4% | ||
| Discharged to Rehab | 51.1% | 51.9% | ||
| Discharged to Other | 34.9% | 37.4% | ||
| Facility | ||||
| Length of Stay (days) | 4(5) v. 6(12) No FU | * | 4(5) vs. 7(8) No FU | * |
| Age | 53.5(24) v. 52(31) No FU | * | 65(19) v. 69(17) No FU | * |
| N | 7552 | 2362 |
p<.01; joint significance for characteristics with multiple categories; FU=follow up; median(interquartile range) reported for continuous variables
Overall Rates of Follow-Up and Readmission
For both surgical groups, patients who had follow-up were less likely to be readmitted (Table 2). However this finding does not necessarily imply a positive relationship between follow-up and prevention of readmission. The majority of readmissions occurred within the first two weeks following discharge (Table 3) and patients who experienced very early readmission (within the first or second week following discharge) did not have the opportunity to attend a routine follow-up. A significant proportion of general surgery (28%) patients were readmitted within 24 hours of their first follow up visit; 8% of vascular surgery patients were readmitted within 24 hours of their first visit (Table 4). More than half of general and vascular surgery patients readmitted after follow-up were readmitted within 24 hours of their most recent (not necessarily their first) outpatient visit. These findings could be related to the discovery of a serious complication at the time of a routine follow-up visit leading to readmission. Alternatively, an urgent or non-routine follow-up visit might have been arranged secondary to the development of a complication.
Table 2.
Follow-up and Readmission Status
| General Surgery | Vascular Surgery | |
|---|---|---|
| Overall rate of Follow-up | 84.1% | 75.3% |
| Overall rate of Readmission | 10.3% | 9.8% |
| Readmission Rate without Follow-up | 33.0% | 16.6% |
| Readmission Rate with Follow-up | 6.0% | 7.6% |
| N | 7552 | 2362 |
Table 3.
Time between Discharge and Readmission among Readmitted Patients
| General Surgery | Vascular Surgery | |
|---|---|---|
| Readmitted 0–7 days following discharge | 45.6% | 28.9% |
| Readmitted 8–14 days following discharge | 25.5% | 31.0% |
| Readmitted 15–21 days following discharge | 15.0% | 23.7% |
| Readmitted 21–30 days following discharge | 13.9% | 16.4% |
| Readmitted Patients | n=779 | n=232 |
Table 4.
The Relationship between Follow-Up and Timing of Readmission
| General Surgery | Vascular Surgery | |
|---|---|---|
| Time between first follow-up and readmission | ||
| Readmitted within 24 hours of first follow-up | 27.9% | 8.1% |
| Readmitted within 2–7 days of first follow-up | 18.5% | 12.6% |
| Readmitted within 8–14 days of first follow-up | 8.6% | 6.7% |
| Readmitted more than 2 weeks after first follow-up | 2.3% | 3.7% |
| Time between most recent follow-up and readmission | ||
| Readmitted within 24 hours of most recent follow-up | 52.3% | 51.1% |
| Readmitted within 2–7 days of most recent follow-up | 30.2% | 32.6% |
| Readmitted within 8–14 days of most recent follow-up | 14.3% | 11.9% |
| Readmitted more than 2 weeks after most recent follow-up | 3.1% | 4.4% |
| Patients readmitted after follow-up | n=384 | n=135 |
Timing of First Follow-Up Relative to Discharge by Readmission Status
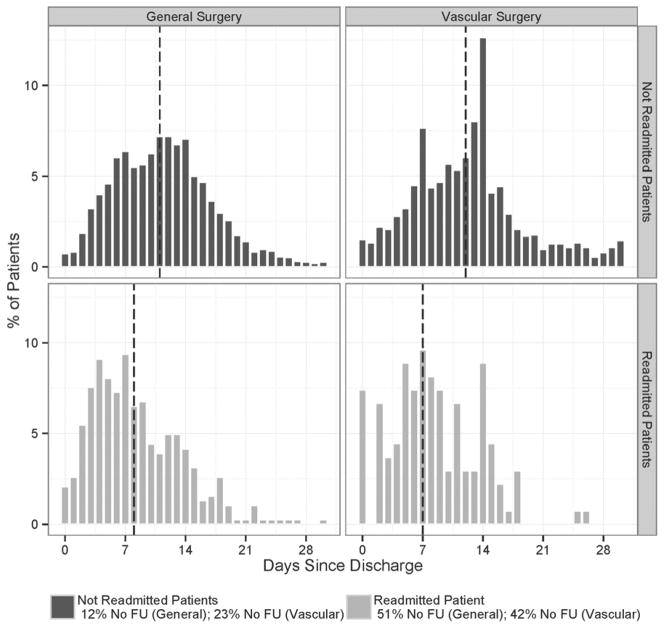
The timing of first follow-up for readmitted and not readmitted patients is depicted for general and vascular surgery patients in Figure 1.1. The graphs show the number of days to first follow-up for readmitted patients and not readmitted patients. First outpatient contact occurred earlier for patients who were readmitted than for patients that were not. General surgery patients who were not readmitted received follow-up at a median time of 11 days after discharge with a smaller spike in outpatient visits at one week; their rates of no follow-up were low at 12%. In contrast, general surgery patients that were readmitted received first follow-up at a median time of 8 days with 51% having no follow-up.
Figure 1.
Figure 1.1. Day of First Follow-up by Readmission Status
Post-discharge day of first follow-up visit by readmission status for general and vascular surgery patients
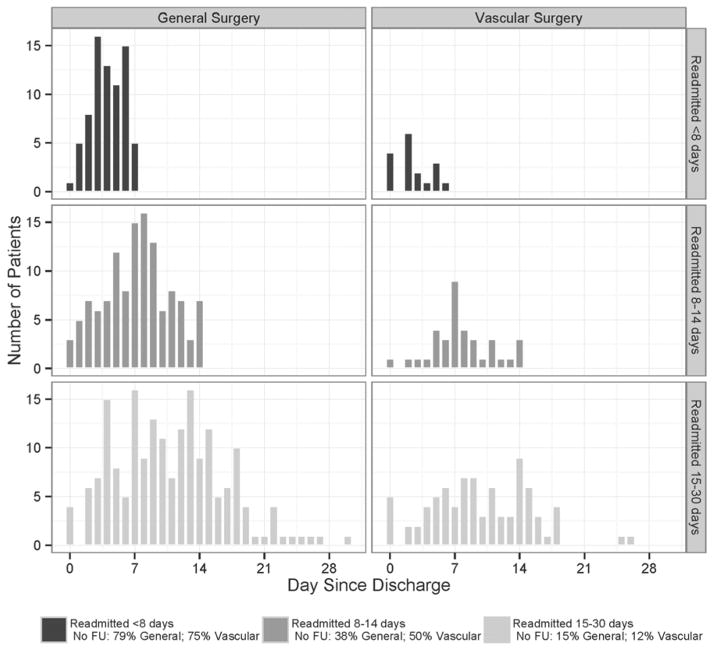
Figure 1.2. Day of First Follow-up for Readmitted Patients by Time From Discharge to Readmission
Post-discharge day of first follow-up visit stratified by days to readmission for general and vascular surgery patients
Figure 1.2 shows time of first follow-up for readmitted patients stratified by week of readmission. For general surgery patients readmitted within the first week following discharge, 79% received no outpatient care; for the remaining 21% the median time to follow-up was 4 days following discharge. Similarly, among patients readmitted within the second week following discharge, 38% received no outpatient care, with the remainder receiving outpatient care at a median 7 days after discharge. General surgery patients who were readmitted in the third and fourth week following discharge were similar to non-readmitted patients in that time to first follow-up was a median of 11 days and the rate of no follow-up was 15%.
There was a similar trend for vascular surgery patients, although rates of no follow-up were higher (Fig. 1.1). First outpatient contact occurred earlier for patients who were readmitted than for patients that were not. Vascular surgery patients who were not readmitted received follow-up at a median time of 12 days after discharge with a smaller spike in outpatient visits at one week; their rates of no follow-up were 23%. In contrast, vascular surgery patients who were readmitted received first follow-up at a median time of 8 days with 42% having no follow-up.
For vascular surgery patients readmitted within the first week following discharge, 75% received no outpatient care; for the remaining 25% the median time to follow-up was 4 days following discharge (Fig. 1.2). Similarly, among patients readmitted within the second week following discharge, 50% received no outpatient care, with the remainder receiving outpatient care at a median 7 days after discharge. Vascular surgery patients who were readmitted in the third and fourth week following discharge were similar to non-readmitted patients in that time to first follow-up was a median of 11 days and the rate of no follow-up was 12%.
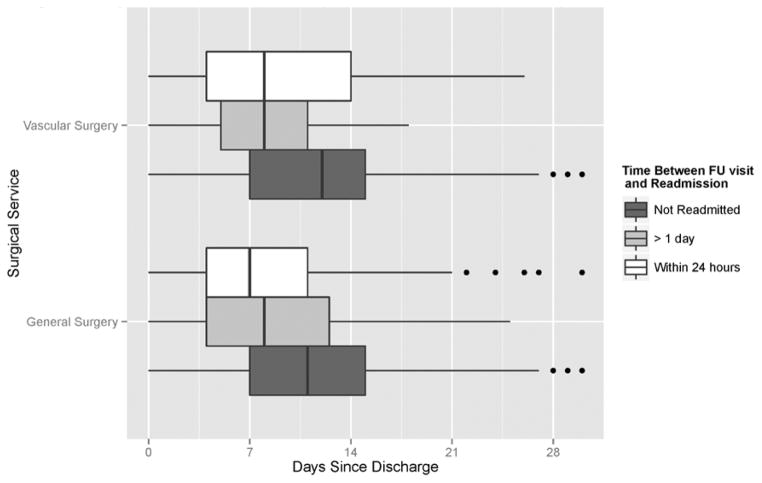
Timing of Readmission Relative to Follow-Up
The time between first follow-up and readmission is essential to understanding whether existing follow-up patterns preclude readmission or simply act as a conduit for readmission. The boxplots in Figure 2 depict which day following discharge the first outpatient visit occurred for the following patient groups: (1) not readmitted, (2) readmitted within 24 hours of follow-up, (3) readmitted more than 1 day after follow-up. Patients who were readmitted within 24 hours of their first outpatient visit had that visit at a median time of one week (7–8 days) after discharge (GS IQR: 7; VS IQR: 10). In contrast, the median time to first follow-up for these “rapidly readmitted” patients approximately corresponds to the 25th percentile of time to first follow-up among patients who were not readmitted (GS median NR=11 days; VS median NR=12 days). In sum, for readmitted patients, first follow-up was sooner following discharge than was first follow-up for patients who were not readmitted.
Figure 2.
Day of First Follow-up Visit by Time Between First Follow-up and Readmission
Post-discharge day of first follow-up visit stratified by time between follow-up and readmission for general and vascular surgery patients
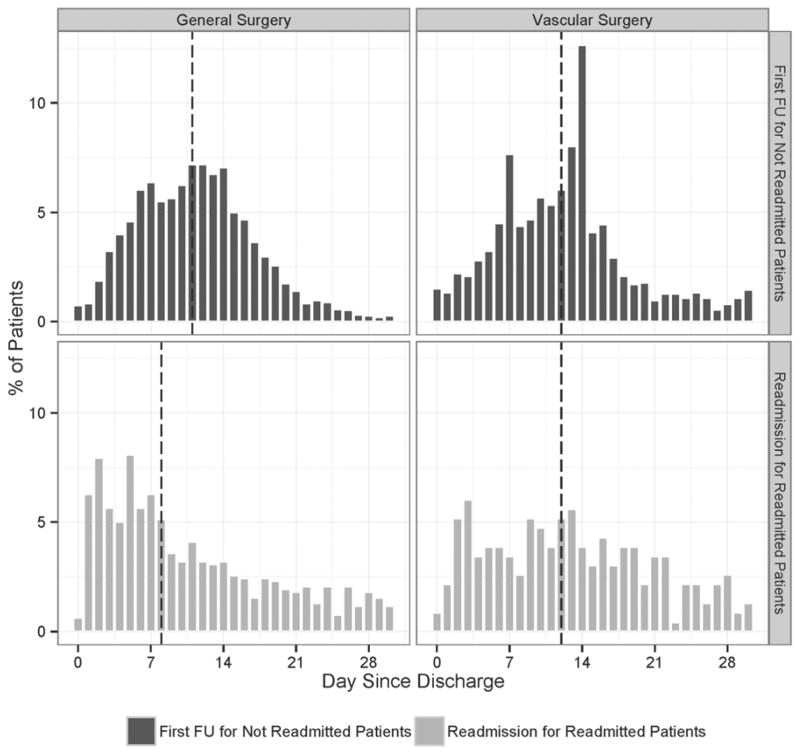
Timing of First Follow-Up Relative to Discharge vs. Timing of Readmission Relative to Discharge
A similar trend can be seen in histograms showing (1) time from discharge to first follow-up among patients who were not readmitted and (2) time from discharge to readmission among all patients who were readmitted (Figure 3). Among general surgery patients, a median 8 days between discharge and readmission was much earlier than the median 11 days between discharge and first follow-up for patients who were not readmitted (medians shown with dashed lines). The median time between discharge and follow-up for vascular patients who were not readmitted was the same as the median time from discharge to readmission for readmitted vascular surgery patients. Overall, readmissions occurred at the same time or earlier than the average follow-up visit for patients with “usual care” (i.e., no readmission).
Figure 3.
Day of First Follow-up vs. Day of Readmission
Post-discharge day of first follow-up for not readmitted patients as compared to post discharge day of readmission for readmitted patients
Number of Follow-Up Visits
Whereas patients who were readmitted within 2 weeks of discharge were less likely to have any follow-up (Table 5: median number of visits GS=1;VS=2; mode=0), patients who were not readmitted usually had a single visit (median GS=2; VS=2; mode=1). Patients readmitted between 15 and 30 days of discharge appear to be more like not readmitted patients in terms of outpatient care utilization, although proportionally more of them had multiple outpatient visits prior to readmission (not shown). The first follow-up visit was also the last (i.e., only) for 57% of readmitted general surgery patients and 31% of readmitted vascular surgery patients. Overall, it is uncommon for patients discharged after general or vascular surgery to have burgeoning complications monitored on an early and ongoing basis in the outpatient setting prior to readmission.
Table 5.
Number of Follow-Up Visits in the First 30 Days Following Discharge
| General Surgery | Vascular Surgery | |
|---|---|---|
| Not Readmitted | 2(1);1 | 1(1);1 |
| Readmitted | 2(2);0 | 2(2);0 |
Median(interquartile range);mode reported for number of visits
Providers of Follow-Up Visits
The majority of patients who received outpatient care had their first visit with a surgical service (Figure 4). Of those, the vast majority received care from the operating service (i.e., general surgery or peripheral vascular/vascular surgery). All patients groups had low rates of outpatient care by a primary care physician in the immediate post-operative interval. Patients who were ultimately readmitted most often had follow-up with a medical specialist, likely to manage a comorbid condition or incompletely resolved post-operative complication; these sicker patients were predisposed to readmission.
Figure 4.
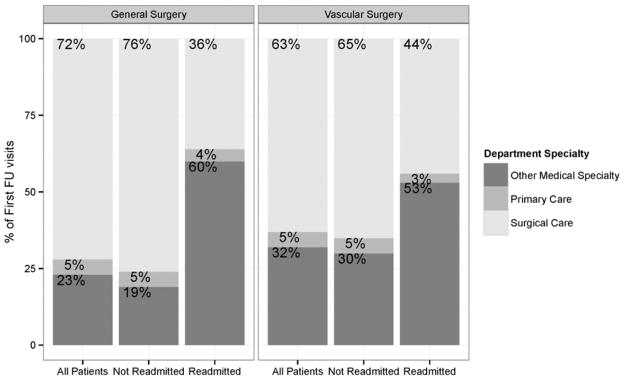
Provider Specialty for First Follow-up Visit
Provider specialties for first follow-up visits of general and vascular surgery patients
DISCUSSION
Transitioning patients from the inpatient setting to home or a post-acute care facility following surgery has received little attention from researchers and practitioners, leading to fragmented care from the perspective of the patient. The data summarized here represent a preliminary step in evaluating when first outpatient follow-up might be timed to preclude costly and preventable readmissions following discharge after general or vascular surgery procedures.
Our results show that current patterns of outpatient follow-up in the immediate postoperative period are not conducive to detecting adverse events and burgeoning complications. The most compelling finding of this study was that the majority of 30-day readmissions occurred within 2 weeks of discharge, before patients could return for their traditional 2-week follow-up appointment. Since the primary goal of follow-up is to monitor for complications, this finding calls into question the value of the “routine follow-up,” particularly as a tool to prevent readmission. There were also a number of patients readmitted between weeks 2 and 4 that had non-routine follow-up before the traditional 2-week appointment, likely for a complication that developed soon after discharge. Additionally there were patients first evaluated at their routine follow-up that already had complications too advanced to prevent readmission. Thus, the forgoing suggests that the routine 2-week follow-up visit allowed early identification and treatment of a complication or the prevention of a readmission in at best, a small subset of patients. In other words, the routine 2 week follow-up visit appears useful only as a mechanism to connect surgeons with the patients who experience a routine and uneventful postoperative course.
Does this mean that the routine 2-week follow-up should be abandoned? Perhaps not. Most patients wish to see their surgeon following discharge for reassurance that all is well, even if their postoperative course is uneventful. However, our findings do suggest that the timing of follow-up should be predicated upon the patient’s likelihood of developing complications. Moreover, if a patient has already developed a complication before discharge, early follow-up and monitoring of this complication is advisable. Although both of these recommendations seem intuitive, it appears that this practice is infrequently followed. The opportunity may exist to decrease readmission by designing programs that personalize the timing of the follow-up visit based on individual patient needs.
Patients not readmitted were most often evaluated postoperatively by the surgical team, whereas readmitted patients were more often evaluated by a non-surgeon. One interpretation of these findings is that, in the absence of close postoperative monitoring by the surgical service, patients with complications are reaching out to medical physicians for care. It is also possible that routine follow-up was scheduled for some patients who had significant comorbidities, with their medical specialist rather than a surgeon; and these sicker patients are more likely to be readmitted. The latter explanation seems less probable than the former; it is unusual for a surgical service to overtly secede follow-up to medical specialists. These findings suggest that failure of a surgical service to closely monitor patients predisposed to complications, leads to these patients finding an alternative and perhaps more familiar source of care.
Existing studies have demonstrated an inconsistent relationship between early outpatient follow-up and readmissions. The literature examining the association between follow-up and readmission is heterogeneous, involving multiple disease processes, different definitions of timely follow up, and different research methods.4–8,13 These differences may account for the variability in findings. Different disease processes likely require follow-up at different intervals to prevent adverse events. Definitions of follow-up were also variable. The studies reviewed define timely follow-up as either the first 7 6,8 or the first 14 7,13 days following discharge, but provide little justification for this interval. Primary and specialty care visits were both studied, although most studies involved specialty care.4,7,8,13 Consistent with our results, these studies show that early follow-up can both expedite readmission and preclude readmission, and the net effect of follow-up depends on the disease process and population of interest.
Limitations
The results of this study should be interpreted in the context of some important limitations. Most notably, we used single institution data. Because we were unable to measure follow-up or readmission of our patients at clinics or hospitals outside of our system, our data are biased. This is particularly true for the vascular surgery service, which serves as a regional center that routinely discharges patients to remote/rural care settings for follow-up; some percentage of these patients likely had follow up in their local care setting or at their local hospital. Consequently, our conclusions are limited regarding those patients we classified as “not readmitted,” or having no follow-up. In addition, inference methods for these data, in which follow-up has the potential to preclude readmission and vice versa, are challenging. These events may be defined as “semi-competing risks,” but the limited scope of our study renders this type of analysis inappropriate. With this limitation, the goal of our study was to describe trends and patterns at a single institution and inform preliminary research in this area. Finally, because of medical record functionality, we were unable to determine when the follow-up visit was scheduled (i.e., at the time of hospital discharge or urgently just before the appointment); therefore, we could not determine whether a given follow-up visit was routine or urgent.
Conclusion
Overall, our findings represent a preliminary proof of concept study for redesigning transitional care after surgery. As quality improvement efforts and financial incentives increasingly incorporate the immediate post-discharge interval, research on surgical care must address the question of how to best meet patients’ needs as they recover in the outpatient or post-acute care setting. Specifically, when and how often do surgical patients need follow-up? What clinical characteristics determine whether a patient is likely to experience an adverse event in the first week or two following discharge? How can providers better identify patients who are unable to care for themselves at home and ensure that these patients receive home health care? The answers to these questions and others will become central to improving care coordination and designing appropriate outpatient care archetypes for surgical patients. In order to treat early complications and stem readmissions, more study will be necessary. Ultimately a randomized, controlled trial including individually tailored follow-up vs. usual care would be an appropriate first step in redesigning transitional care for surgical patients.
Acknowledgments
Sources of Funding and Conflicts of Interest:
The project described was supported in part by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Richard S. Saunders and Jason T. Wiseman are supported by an NIH training grant (T32 HL110853). Jon Matsumura receives research grant assistance from W. L. Gore & Associates, Inc., Cook Medical, Endologix, Inc., Covidien, Abbott Vascular, and the National Institute of Health. K. Craig Kent, MD receives financial compensation from Medtronic Vascular, Inc. for clinical trial consulting.
Footnotes
The other authors declare no relevant conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med. 2013;369:1134–1142. doi: 10.1056/NEJMsa1303118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Medicare and Medicaid Services [Internet] Readmissions Reduction Program. [updated 2013 August 02; cited 2014 January 22]. Available from: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
- 3.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 4.Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392–397. doi: 10.1002/jhm.666. [DOI] [PubMed] [Google Scholar]
- 5.Lin CY, Barnato AE, Degenholtz HB. Physician follow-up visits after acute care hospitalization for elderly Medicare beneficiaries discharged to noninstitutional settings. J Am Geriatr Soc. 2011;59:1947–1954. doi: 10.1111/j.1532-5415.2011.03572.x. [DOI] [PubMed] [Google Scholar]
- 6.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 7.Hubbard M, Frost S, Siu K, Quon N, Esposito D. Association between outpatient visits following hospital discharge and readmissions among Medicare beneficiaries with atrial fibrillation and other chronic conditions. Am J Med Qual. 2013 Jul 29; doi: 10.1177/1062860613493827. 1062860613493827. [DOI] [PubMed] [Google Scholar]
- 8.Hess CN, Shah BR, Peng SA, Thomas L, Roe MT, Peterson ED. Association of early physician follow-up and 30-day readmission after non-ST-segment-elevation myocardial infarction among older patients. Circulation. 2013;128:1206–1213. doi: 10.1161/CIRCULATIONAHA.113.004569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Engelbert TL, Fernandes-Taylor S, Gupta PK, Kent KC, Matsumura J. Clinical characteristics associated with readmission among patients undergoing vascular surgery. J Vasc Surg. 2013 doi: 10.1016/j.jvs.2013.10.103. In press. Epub 2013 December 22. [DOI] [PubMed] [Google Scholar]
- 10.3M HIS Hughessumm.pdf [Internet] APR™-DRG Classification Software –Overview. [cited 2014 January 22]. Available from: http://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/mortality/Hughessumm.pdf.
- 11.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2014. URL http://www.R-project.org. [Google Scholar]
- 12.Wickham H. ggplot2: elegant graphics for data analysis. 1. New York: Springer; 2009. [Google Scholar]
- 13.Kashiwagi DT, Burton MC, Kirkland LL, Cha S, Varkey P. Do timely outpatient follow-up visits decrease hospital readmission rates? Am J Med Qual. 2012;27:11–15. doi: 10.1177/1062860611409197. [DOI] [PubMed] [Google Scholar]