Summary
Background
Choroideremia is an X-linked recessive disease that leads to blindness due to mutations in the CHM gene, which encodes the Rab escort protein 1 (REP1). We assessed the effects of retinal gene therapy with an adeno-associated viral (AAV) vector encoding REP1 (AAV.REP1) in patients with this disease.
Methods
In a multicentre clinical trial, six male patients (aged 35–63 years) with choroideremia were administered AAV.REP1 (0·6–1·0×1010 genome particles, subfoveal injection). Visual function tests included best corrected visual acuity, microperimetry, and retinal sensitivity tests for comparison of baseline values with 6 months after surgery. This study is registered with ClinicalTrials.gov, number NCT01461213.
Findings
Despite undergoing retinal detachment, which normally reduces vision, two patients with advanced choroideremia who had low baseline best corrected visual acuity gained 21 letters and 11 letters (more than two and four lines of vision). Four other patients with near normal best corrected visual acuity at baseline recovered to within one to three letters. Mean gain in visual acuity overall was 3·8 letters (SE 4·1). Maximal sensitivity measured with dark-adapted microperimetry increased in the treated eyes from 23·0 dB (SE 1·1) at baseline to 25·3 dB (1·3) after treatment (increase 2·3 dB [95% CI 0·8–3·8]). In all patients, over the 6 months, the increase in retinal sensitivity in the treated eyes (mean 1·7 [SE 1·0]) was correlated with the vector dose administered per mm2 of surviving retina (r=0·82, p=0·04). By contrast, small non-significant reductions (p>0·05) were noted in the control eyes in both maximal sensitivity (–0·8 dB [1·5]) and mean sensitivity (–1·6 dB [0·9]). One patient in whom the vector was not administered to the fovea re-established variable eccentric fixation that included the ectopic island of surviving retinal pigment epithelium that had been exposed to vector.
Interpretation
The initial results of this retinal gene therapy trial are consistent with improved rod and cone function that overcome any negative effects of retinal detachment. These findings lend support to further assessment of gene therapy in the treatment of choroideremia and other diseases, such as age-related macular degeneration, for which intervention should ideally be applied before the onset of retinal thinning.
Funding
UK Department of Health and Wellcome Trust.
Introduction
Choroideremia (OMIM 303100) is currently an incurable X-linked recessive degenerative disease of the retina and choroid that might first have been described by Mauthner in 1872.1 It has a prevalence of about 1:50 000, with northern Finland having the highest reported prevalence.2 Loss of night vision begins in the first decade of life and progresses with a gradual loss of peripheral vision and legal blindness by the fifth decade. Choroideremia is caused by mutations in the CHM gene, which was one of the first genes identified by use of positional cloning.3,4 Subsequently, prenylation deficiency due to absence of Rab escort protein-1 (REP1) encoded by CHM was identified as the cause of retinal degeneration in choroideremia.5 Nearly all reported cases of choroideremia so far have been attributed to functionally null mutations that, combined with the slow rate of degeneration and small size of the CHM protein coding sequence (1·9 kb), make gene therapy with adeno-associated viral (AAV) vectors an appealing treatment strategy.
In patients with choroideremia, generally good visual acuity is maintained until the degeneration encroaches on the fovea; however, underlying changes in the retina can be identified in childhood and are associated with clinically significant reductions in parafoveal retinal sensitivity as measured with psychophysical testing.6 Therefore, before the onset of loss in visual acuity, retinal sensitivity might be a useful indicator of the functional effects of gene therapy in patients with choroideremia. Furthermore, in a phase 1 clinical trial to assess the effects of an intravitreal ciliary neurotrophic factor implant, one of the ten patients enrolled had choroideremia and this patient was noted to have an improvement of 13 letters (over two lines) in visual acuity 24 weeks after the implantation.7 Hence, the few data available so far suggest that loss of visual acuity might have a reversible component in the later stages of the disease. Although improvements in visual function provide a useful early marker of successful gene transfer, ultimately any genetic treatment should be aimed at halting or at least significantly slowing the rate of degeneration.
Choroideremia derives its name from the almost complete loss of the retina, choroid, and retinal pigment epithelium that leads to exposure of the underlying white sclera, which is a unique feature compared with other retinal degenerations. Centripetal to the advancing degeneration, the retinal layers remain fairly intact and normal central retinal thickness might be maintained until the fifth decade.6 These anatomical features are relevant to gene therapy approaches because the volume of tissue to be targeted is continually shrinking and the multiplicity of infection of viral particles per cell will vary at different stages of the disease. The area of surviving tissue can, however, be measured with autofluorescence imaging, which detects fluorescent visual cycle products in the retinal pigment epithelium.8 Furthermore, the functional central retina is generally much thicker in choroideremia than in Leber congenital amaurosis and hence might be more resilient to damage from foveal detachment that is induced by subretinal injection.9 We therefore assessed AAV gene therapy in patients with different stages of choroideremia.
Methods
Patients and study design
Six male patients with a clinical phenotype of choroideremia and predicted null mutations in the CHM gene were enrolled into this multicentre trial after they provided written informed consent. The ages of patients 1–6 were 63 years, 47 years, 35 years, 55 years, 41 years, and 56 years, respectively. The patients represented different stages of the disease against which to assess the efficacy of the intervention—a normal foveal structure, partial foveal collapse, and complete foveal loss (figure 1). The Gene Therapy Advisory Committee (UK Department of Health) provided ethics approval.
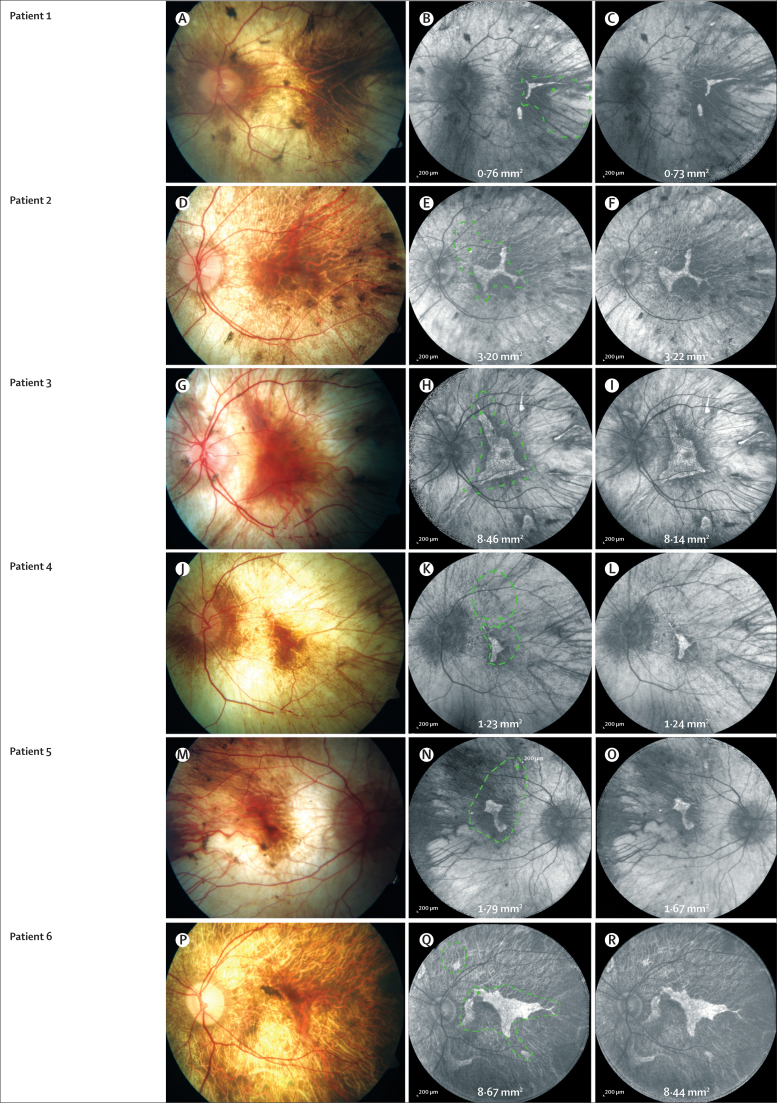
Figure 1.
Retinal detachment in patients' eyes exposed to vector
Images show the retina in patients 1–6 (A, D, G, J, M, and P, respectively) and the corresponding baseline autofluorescent retina (B, E, H, K, N, and Q, respectively). The area of autofluorescent retinal pigment epithelium exposed to vector is annotated on each panel in mm2. The limits of the retinal detachment are indicated by the green dotted line and the injection site is indicated with a green dot. The corresponding autofluorescence images and measurements in the retinal pigment epithelium at 6 months are shown in panels C, F, I, L, O, and R. The area of the retinal pigment epithelium did not change substantially 6 months after surgery, although focal loss of autofluorescence superior to the injection site was noted in patient 3 (I). In patients 4 and 6, more than one injection was required to detach the fovea (additional green lines).
Vector production
The AAV2 expression cassette comprised a chicken β actin promoter, established for long-term transduction of the retinal pigment epithelium in previous clinical trials of human retinal gene therapy,9,10 and a Woodchuck hepatitis virus post-translational regulatory element (WPRE) downstream of the CHM cDNA (encoding REP1). WPRE is known to enhance AAV-mediated transgene expression,11 and was approved by the US Food and Drug Administration for a clinical trial of AAV2 for Parkinson's disease.12 This human REP1 sequence was previously shown in vitro to restore prenylation activity when delivered by an adenoviral vector to cells isolated from patients with choroideremia.13 The subsequent preclinical data for the effects of this vector (AAV2.REP1) in restoring prenylation activity to human choroideremia fibroblasts and the electroretinogram in mouse choroideremia are described elsewhere.14 PF68 surfactant was added to prevent non-specific binding of AAV particles to plastics inside the injection system.15
Surgery
Because of the unpredictability of detachment of the retina in choroideremia, patients were injected with AAV2.REP1 as a two-step procedure. Surgery was first undertaken to detach the retina through a 41G Teflon cannula (DORC International BV, Zuidland, Netherlands) using balanced salt solution (Alcon Laboratories, Fort Worth, TX, USA). Once the retinal target area had been detached from the underlying retinal pigment epithelium, a fixed volume (0·1 mL) containing 1×1010 genome particles of AAV2.REP1 was injected through a fresh syringe into the subretinal space that had been created in the first five patients. In patient 6, a reduced dose of up to 6×109 genome particles was injected. The vector was injected slowly through the same retinotomy, causing the detachment to extend further. Surgery was uncomplicated in the first five patients, but in patient 6 difficulty in detachment of the retina from the peripheral macula necessitated the induction of detachment from a point close to the fovea (figure 1Q), which caused visible stretching of the papillomacular bundle. Because of concerns about stretch-related damage of this vital structure in a patient with 6/7·5 vision, a smaller volume of vector (maximum 0·06 mL) was injected in the second step. In all patients, the surplus vector remaining in the syringe was expelled through the cannula into a polypropylene vial and then frozen. This surplus vector was later tested for potency with western blot after transduction of the human-derived HT1080 cell line (appendix). Patients were treated with a 10-day oral course of prednisolone, starting 2 days before surgery at 1 mg/kg (70–100 mg) for 7 days and then reduced to 40 mg for 1 day, 20 mg for 1 day, and 10 mg for 1 day. Blood samples were taken for immunological tests before, and 1 week and 5–6 weeks after surgery.
Clinical assessments
All patients had best corrected visual acuity and contrast sensitivity measured in each eye separately after a standardised refraction. Measurement of best corrected visual acuity was done in accordance with the established protocols of the Early Treatment for Diabetic Retinopathy Study16 with a masked tester. Microperimetry was done with a Maia system (CenterVue, Padova, Italy) in accordance with the manufacturer's protocol with 20 min of dark adaptation (1·5 cd/m2) before testing with a background luminance set at 4 apostilb (equivalent to 1·3 cd/m2). At least three full microperimetry tests were done by one of two operators before they obtained baseline data so as to reduce any learning effects and to identify accurately the regions of seeing retina around which the customised maps were plotted. Before the start of the study, CenterVue adapted the autoexposure of the inbuilt camera to avoid overexposure in patients with choroideremia.
This study is registered with ClinicalTrials.gov, number NCT01461213.
Role of the funding source
The Health Innovation Challenge Fund requested securing of background intellectual property relating to the vector before it provided funding for the trial. Milestones for funding tranches were imposed with regard to obtaining regulatory approvals and recruitment of patients. The funding source had no role in data gathering or interpretation, or in writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
The study started on Oct 20, 2012, and is ongoing. The residual retina overlying the area of autofluorescence was detached in all six patients and the limits of detachment (vector exposure) are shown in figure 1. The size range of the target area in the surviving retina that was exposed to vector was greater than 1 log unit, from 0·76 mm2 to 8·67 mm2 (figure 1; table).
Table.
Changes in visual function from baseline to 6 months after gene therapy
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Mean (SE) | |
|---|---|---|---|---|---|---|---|
| Change in treated eye visual acuity (ETDRS) | +21 | −1 | −3 | +11 | −2 | −3 | +3·8 (4·1) |
| Change in control eye visual acuity (ETDRS) | +11 | −3 | +4 | −1 | 0 | −2 | +1·5 (2·1) |
| Change in maximal sensitivity (dB) | +5 | +2 | +4 | 0 | +2 | +1 | +2·3 (0·8) |
| Change in mean sensitivity (dB) | +4·4 | +0·6 | +2·0 | +4·5 | +1·1 | −2·3 | +1·7 (1·0) |
| Change in control eye mean sensitivity (dB) | −2·3 | −3·1 | +2·2 | −4·1 | −1·1 | −1·2 | −1·6 (0·9) |
| Area of retina treated with vector (mm2) | 0·76 | 3·20 | 8·46 | 1·23 | 1·79 | 8·67 | 4·02 (1·48) |
| Dose of vector (genome particles × 109 per mm2 retina) | 13·2 | 3·1 | 1·2 | 8·1 | 5·6 | 0·7 | 5·3 (1·9) |
ETDRS=Early Treatment for Diabetic Retinopathy Study (a standard vision test).
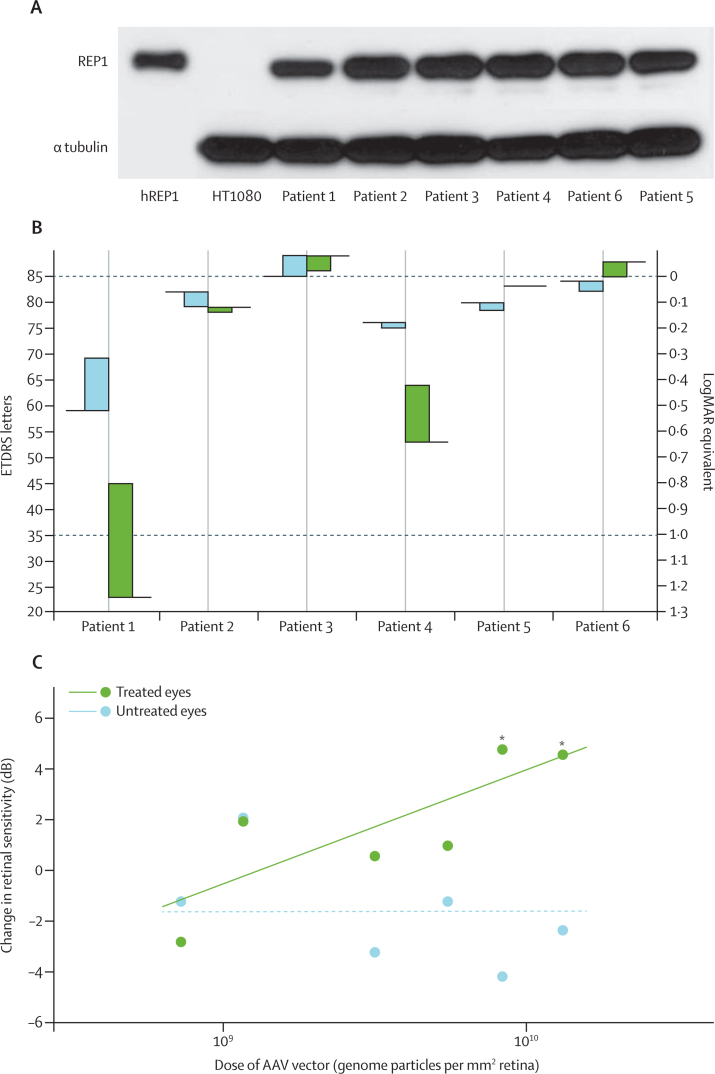
The six patients had a mean gain in visual acuity in their treated eyes of 3·8 letters (SE 4·1), but this value masked two distinct emerging patterns in the group (table). Patients 1 and 4, in whom visual acuity was reduced at baseline, gained 21 letters and 11 letters, respectively, whereas the other four patients with baseline visual acuity better than 6/9 had a marginal loss of one to three letters by 6 months (table). Both patients 1 and 4 reported subjective improvements in vision in their treated eyes (appendix p 13) that were consistent with the gains in their visual acuity. Since the measured gains in visual acuity in these two patients were substantial (table), additional verification was obtained with the patients' permission from their regular optometrists. These additional independent records, with data from at least the past 4 years, were used to confirm the baseline measurements and subsequent gains in visual acuity after gene therapy in patients 1 and 4 (appendix p 13).
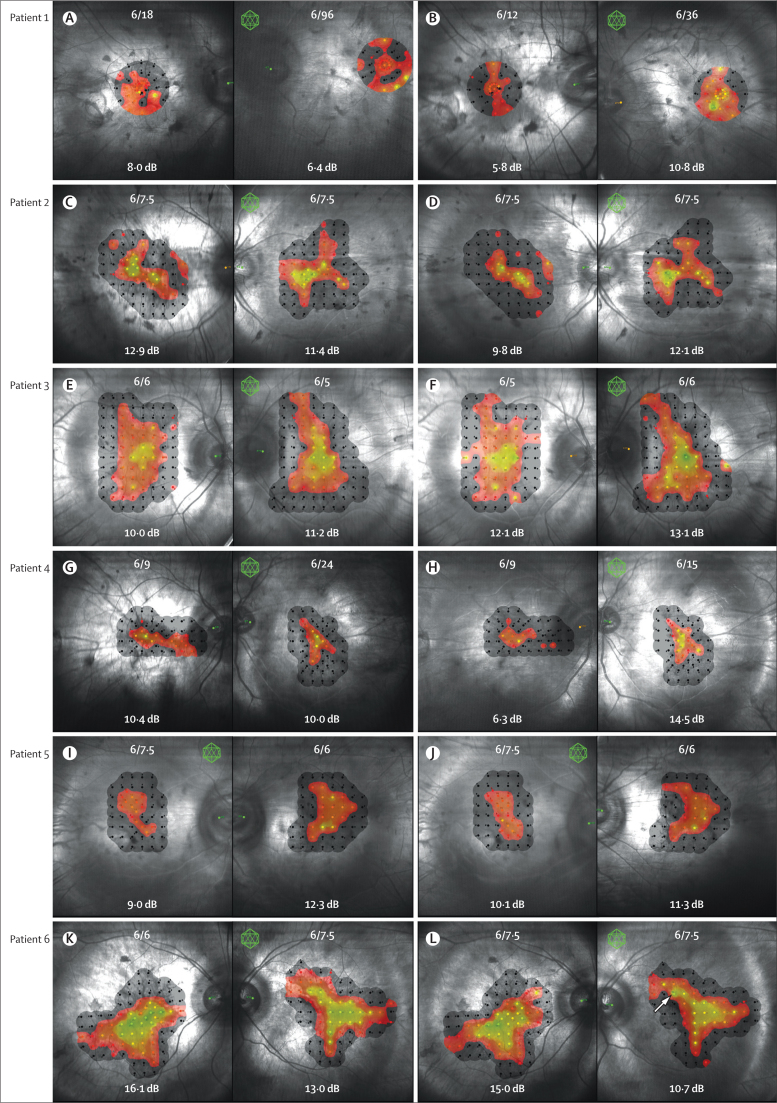
The point of maximal sensitivity represents the minimal detectable light stimulus and is therefore more relevant than visual acuity to rod photoreceptor function in patients who have been adapted to mesopic light levels. It increased by a mean of 2·3 dB (95% CI 0·8–3·8) in the treated eyes from 23·0 dB (SE 1·1) at baseline to 25·3 dB (1·3) 6 months after surgery, reaching 28 dB (which is within the normal population range) in two of the treated eyes. Mean retinal sensitivity increased by 2·5 dB (1·1) in the five eyes administered the full dose of vector, but fell by 2·3 dB in the eye administered the reduced dose, which also had the largest target area (figure 2; table). A similar non-significant increase was seen for the changes in visual field sizes in these eyes (appendix p 12).
Figure 2.
Microperimetry at baseline and 6-month follow-up in both eyes of patients with choroideremia given gene therapy
Snellen equivalents and microperimetry measurements are shown for both eyes. The left column shows measurements at baseline in patients 1–6 (A, C, E, G, I, and K, respectively) and the right column shows the results 6 months after surgery (B, D, F, H, J, and L, respectively). The eyes injected with vector are indicated by a green icosahedron. The stimulus points from the baseline measurements are stored in the software and mapped onto identical regions of retina during follow-up testing. Black dots indicate points not seen at 0 dB. The movement of the left fundus image in patient 1 (A, B) represents a real shift in fixation (figure 3). The white arrow in panel L is adjacent to the site of the subretinal injection. Although there was thinning in this area, it become the most sensitive point in this retina at 26 dB (fovea 21 dB).
As a subjective visual assessment, microperimetry is subject to concentration and learning effects and possibly seasonal effects when tests are done 6 months apart.17 Hence, microperimetry measurements for the treated eyes were compared with those for the untreated eyes, which also provided a control for the natural course of the degeneration (table; appendix p 12). At 6-month follow-up, mean reduction in retinal sensitivity was noted in the unoperated control eyes with respect to the dimmest stimulus seen (–0·8 dB [SE 1·5]), mean retinal sensitivity (–1·6 dB [0·9]), and total number of test points seen (–1·3 [1·4]). Conversely, 6 months after gene therapy, a mean increase was noted in retinal sensitivity in the treated eyes with respect to the dimmest stimulus seen (2·3 dB [0·8]), mean retinal sensitivity (1·7 dB [1·0]), and total number of test points seen (1·5 [2·3]). Although these measurements were not independently significant (p>0·05), the overall trend is in keeping with a slow degeneration in the control eyes, against a treatment effect from gene therapy in the eyes undergoing retinal detachment by 6 months (table; appendix pp 11–12).
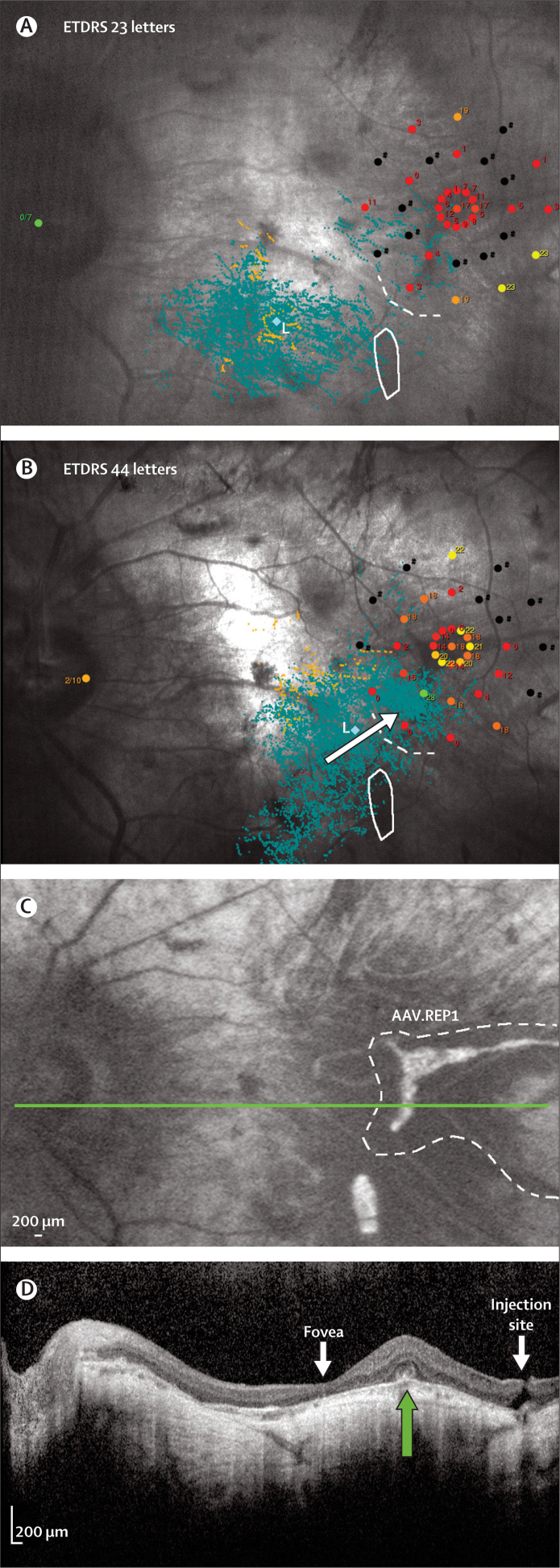
Further analysis of the visual function in patient 1 at 6 months showed that his fixation points had moved towards the region exposed to the vector (figure 3). Before surgery he had lost foveal fixation and his preferred retinal locus was variable, but mainly in the region just below where the fovea previously existed (figure 3A). By 6 months after gene therapy, his preferred retinal locus, although still variable, had shifted towards, and at times incorporated, the residual area of autofluorescence exposed to vector (figure 3B; appendix p 21). Importantly, this shift in fixation bypassed a closer island of autofluorescence that had not been exposed to the vector (figure 3C, D). The five other patients maintained foveal fixation throughout, and this fixation correlated with the point of maximal sensitivity measured with microperimetry in patients 2–5 (figure 2). In patient 6, however, the point of maximal sensitivity moved superonasally away from the fovea to the region adjacent to where the vector had been injected (figure 2L, location indicated by arrow).
Figure 3.
Detailed analysis of retinal function and structure in patients with choroideremia
(A) Pre-surgery and (B) 6 months post-surgery analysis of patient 1 showing a shift in the cloud of variable fixation (blue dots; B, white arrow) into the area of retina exposed to vector (dotted white line), but away from the area of surviving autofluorescent retinal pigment epithelium (white solid line) that was not exposed to vector. The increase in retinal sensitivity also correlated anatomically with the region of surviving retina exposed to AAV.REP1 (C, dotted line) and residual outer retina identified with optical coherence tomography scanning (D, green arrow). The thin fovea and injection site can be seen on either side of the residual retina (green arrow). Green dot (L) is the mean centre of all fixation points. ETDRS=Early Treatment for Diabetic Retinopathy Study (a standard vision test). AAV=adeno-associated virus. REP1=Rab escort protein 1.
In choroideremia, the area of residual autofluorescence in the retinal pigment epithelium is broadly representative of the amount of remaining tissue that needs to be targeted by gene therapy.8 This area varied over 1 log unit in our patients and the amount of vector administered differed between patients 1–5 and patient 6. Furthermore, the vector had been stored for different periods and diluted 1:10 before administration in the operating theatre. Hence, to assess any treatment effect, the potency of the vector administered to each patient was compared. The dose was then calculated relative to the area of target tissue into which the vector would be absorbed from the subretinal space. A western blot of the proteins from HT1080 cells transduced with the unused surplus vector remaining from administration from each patient showed broadly similar levels of protein expression (figure 4A). The increase in mean retinal sensitivity was correlated with the dose administered per unit area (log genome particles per mm2 retina) to the treated eyes (r=0·82, p=0·04; figure 4C). No correlation was noted in the untreated eyes, which showed the opposite trend (r=–0·59, p=0·21; figure 4C), in keeping with the slow progression of the disease in the later stages.
Figure 4.
Vector doses administered to and vision changes in patients with choroideremia
(A) Western blot showing REP1 expression from aliquots of 1:10 residual diluted vectors that were removed from syringes after administration to patients and applied to a human cell line (HT1080) in culture. Also shown are the positive (hREP1) and negative controls (lysate from non-transduced cells) and the loading control (α tubulin). (B) Changes in best corrected visual acuity in ETDRS letters in each of the six patients. Horizontal lines represent baseline levels and the columns represent changes at 6 months in the treated (green) and fellow eyes (blue). (C) Shows the changes in retinal sensitivity measured with microperimetry before and 6 months after surgery in the treated and control eyes. The improvement in the treated eyes was correlated with the dose of vector genome particles per mm2 in the surviving retina. hREP1=human Rab escort protein 1 (tagged protein positive control). REP1=Rab escort protein 1. ETDRS=Early Treatment for Diabetic Retinopathy Study (a standard vision test). AAV=adeno-associated virus. *Patients 1 and 4 with the greatest improvement in retinal sensitivity also had notable improvements in visual acuity.
Since retinal thinning after subfoveal gene delivery has been a concern in other gene therapy trials,9 the thickness of the outer retina was measured in each patient before and 6 months after surgery. Because the fovea could not be identified clearly in patients 1 and 4, the thickest region of the retina was chosen. The mean thickness of the retina in the six patients was similar before and 6 months after surgery at 175 μm (SE 27) and 169 μm (26), respectively. Notable outer retinal thinning was seen only in patient 6 in a non-seeing area just nasal to the fovea (appendix p 16), which corresponded to the region that stretched during subretinal injection. There was no clinically significant loss of visual acuity in this patient. In the six patients, the mean area of surviving retina, as measured with autofluorescence, was similar at baseline and 6 months after surgery (4·0 mm2 [1·8] and 3·9 mm2 [1·7], respectively; figure 1).
Discussion
After subretinal administration of the AAV.REP1, the two patients with the most advanced choroideremia had substantial gains in visual acuity (panel). The other four patients with near-normal visual acuity at baseline received subretinal vector without any significant detrimental effects. In the cohort, we noted an improvement in maximal retinal sensitivity in the eyes treated with AAV.REP1, despite detachment of the macula, which is usually associated with a reduction in retinal sensitivity. The five patients who received the full dose of AAV vector had improvements in mean retinal sensitivity in their detached retinas 6 months after surgery.
Panel. Research in context.
Systematic review
We searched PubMed for all publications, including clinical trial reports and reviews, with the terms “retina”, “gene therapy”, “choroideremia” (or “choroideraemia”), and “retinitis pigmentosa”, and found reports of gene therapy used to target the retinal pigment epithelium in patients with Leber congenital amaurosis due to deficiencies in the RPE65 gene.
Interpretation
To our knowledge, this study is the first assessment of retinal gene therapy administered to patients who have normal visual acuity. It is also the first report of targeting a gene expressed in the photoreceptors. The results show the potential for gene therapy, not just in the treatment of choroideremia, but also for other chronic retinal degenerations that require early intervention before the onset of visual loss. These retinal degenerative diseases include retinitis pigmentosa and age-related macular degeneration.
A notable difference compared with other retinal degenerations is that all target tissue layers (photoreceptors, retinal pigment epithelium, and choroid) are continually shrinking in choroideremia. Since subretinal fluid is taken up largely through the retinal pigment epithelium and into the choroid rather than across bare sclera, it is likely that the multiplicity of infection per cell in the retinal pigment epithelium will increase for a fixed titre of vector as the target area shrinks in size. Hence, comparison of the dose per mm2 of target tissue might be advantageous, and was correlated with the treatment effect. An alternative explanation for the apparent dose effect, however, might be that the smaller areas have more advanced disease in which the capacity for functional improvement might be greater.
Previous reports of retinal gene therapy have shown long-term beneficial effects on visual function in patients with Leber congenital amaurosis,8,18 including treatment of their second eyes.19 Although assessment with microperimetry is subjective, the results were consistent in the patients in our study in whom the most significant improvements were also accompanied by measurable gains in best corrected visual acuity, which was an independent test. In our cohort, only one patient had complete loss of foveal fixation before surgery. Although still variable, by 6 months his fixation had shifted to include the small residual island of retina ectopic to the fovea that had been exposed to vector. This finding is noteworthy because the fixation shift bypassed a closer island of residual retina that was not exposed to vector, and it is difficult to explain how a patient might change his fixation in this way if the sensitivity of the island exposed to vector had not improved by a clinically significant amount. This fixation shift is similar to that reported in a patient with RPE65 mutations treated with vector that was ectopic to the fovea.20 This patient also had a slight improvement in visual acuity in his control eye, equivalent to about one line in the Snellen test. Although this outcome most likely represents inter-test variability, improvements in control eyes with low vision have been noted after gene therapy in some patients with Leber congenital amaurosis, possibly due to reduced nystagmus.19 By contrast, the microperimetry measurements deteriorated in the control eye of this patient, but the test was done under mesopic conditions and therefore included measurement of rod function, whereas visual acuity measurements were done in bright scotopic conditions. Hence, microperimetry and visual acuity tests to some extent provide complementary information about rod and cone function.
The results of a recent report have suggested that retinal degeneration continues in some patients with RPE65 mutations despite successful gene transfer.18 It is important to note, however, that the neurosensory retina and retinal pigment epithelium had advanced disease and degeneration at the time of intervention in patients and might have been beyond the point of recovery. By contrast, the goal in treatment of choroideremia would be to intervene while the retinal architecture remains fairly well preserved. Furthermore, phase 1 data from the RPE65 gene therapy trials should not be overinterpreted—the continued degeneration might simply reflect a requirement for a higher vector dose than that administered. In our study, there were no obvious detrimental effects from detachment and treatment of the fovea. Although there will undoubtedly be some damage to photoreceptors as a result of retinal detachment, it was not clinically significant in our patients and anatomical evidence of thinning was only seen in one of six cases. Foveal thinning including macular hole formation has, however, been noted after subfoveal gene therapy in several patients in the RPE65 gene therapy trials.9 This outcome might be explained partly by the fairly thick foveal tissue in patients with choroideremia compared with the thin surrounding degenerate retina and might (according to Hooke's law) undergo proportionately less horizontal stretch during the subretinal injection. The lack of thinning of the central retina in the early years of choroideremia might also provide the opportunity for gene therapy to slow or possibly even stop the ensuing degeneration, as predicted in the early stages of Leber congenital amaurosis.18
Since CHM is expressed ubiquitously, a key question in gene therapy for patients with choroideremia is to decide which retinal layer to target with the vector. Regeneration of choroidal vessels has been reported in patients with this disease,21 suggesting that the choroidal vasculature has no intrinsic dependence on REP1. Hence, the choroidal atrophy could all be secondary to loss of the overlying retinal pigment epithelium, as occurs in dominantly inherited mutations in RPE65, which result in a phenotype similar to choroideremia.22 Although photoreceptors will degenerate secondary to the loss of retinal pigment epithelium, we have previously noted in the mouse model of choroideremia that rod photoreceptors might also degenerate independently.23 Hence, AAV2 was chosen for this gene therapy trial because it is known to be safe for use in the human retina and has good tropism for primate retinal pigment epithelium and to some extent rod photoreceptors.24 The chicken β actin promoter also has long-term proven efficacy in the previous RPE65 gene therapy trials,25 including readministration to the second eye.19 Choroideremia results almost exclusively from functionally null mutations,4,26 which has the additional advantage that transgenic mRNA will in most cases not be in competition with mutant mRNA27 and might make gene therapy dosing more predictable than in other genetic diseases. To our knowledge, our report is the first in which the effects of retinal gene therapy in patients with good visual acuity of 6/6 or better and before the onset of clinically significant retinal thinning are described. These findings support the development and use of gene therapy to prevent loss of sight in other retinal diseases, such as age-related macular degeneration.
Acknowledgments
Acknowledgments
This study was funded by the UK Department of Health and Wellcome Trust with additional support from the NIHR Oxford and Moorfields Biomedical Research Centres.
Contributors
REM, MG, CLC, ARB, TT, MCS, ARW, MJD, GCMB, KRC, FPMC, SMD, and AJL contributed to data collection and analysis. REM, ARB, MG, SMD, GCMB, CLC, ARW, and AJL contributed to study design. REM and MCS obtained funding. LS and KRC provided regulatory advice. REM did the surgery. REM, MG, ARB, TT, CLC, GCMB, AJL, FPMC, SMD, ARW, MJD, and MCS contributed to writing the report.
Conflicts of interest
REM, MJD, and MCS are named co-inventors on UK patent application 1103062.4, filed on Feb 22, 2011, and owned by the University of Oxford. MJD is a Director of Gene Technology Solutions, Auckland, New Zealand. The other authors declare that they have no conflicts of interest.
Supplementary Material
Robert E MacLaren discusses how gene therapy improves eyesight in people born with choroideremia.
References
- 1.Mauthner L. Ein Fall von Choroideremie. Ber Naturwissensch-med Ver Inssbruck. 1872;2:191–197. [Google Scholar]
- 2.Sankila EM, Tolvanen R, van den Hurk JA, Cremers FP, de la Chapelle A. Aberrant splicing of the CHM gene is a significant cause of choroideremia. Nat Genet. 1992;1:109–113. doi: 10.1038/ng0592-109. [DOI] [PubMed] [Google Scholar]
- 3.Cremers FP, van de Pol DJ, van Kerkhoff LP, Wieringa B, Ropers HH. Cloning of a gene that is rearranged in patients with choroideraemia. Nature. 1990;347:674–677. doi: 10.1038/347674a0. [DOI] [PubMed] [Google Scholar]
- 4.van Bokhoven H, van den Hurk JAJM, Bogerd LPM. Cloning and characterization of the human choroideremia gene. Hum Mol Genet. 1994;3:1041–1046. doi: 10.1093/hmg/3.7.1041. [DOI] [PubMed] [Google Scholar]
- 5.Seabra MC, Brown MS, Goldstein JL. Retinal degeneration in choroideremia: deficiency of rab geranylgeranyl transferase. Science. 1993;259:377–381. doi: 10.1126/science.8380507. [DOI] [PubMed] [Google Scholar]
- 6.Jacobson SG, Cideciyan AV, Sumaroka A. Remodeling of the human retina in choroideremia: rab escort protein 1 (REP-1) mutations. Invest Ophthalmol Vis Sci. 2006;47:4113–4120. doi: 10.1167/iovs.06-0424. [DOI] [PubMed] [Google Scholar]
- 7.Sieving PA, Caruso RC, Tao W. Ciliary neurotrophic factor (CNTF) for human retinal degeneration: phase I trial of CNTF delivered by encapsulated cell intraocular implants. Proc Natl Acad Sci USA. 2006;103:3896–3901. doi: 10.1073/pnas.0600236103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Syed R, Sundquist SM, Ratnam K. High-resolution images of retinal structure in patients with choroideremia. Invest Ophthalmol Vis Sci. 2013;54:950–961. doi: 10.1167/iovs.12-10707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobson SG, Cideciyan AV, Ratnakaram R. Gene therapy for Leber congenital amaurosis caused by RPE65 mutations: safety and efficacy in 15 children and adults followed up to 3 years. Arch Ophthalmol. 2012;130:9–24. doi: 10.1001/archophthalmol.2011.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maguire AM, Simonelli F, Pierce EA. Safety and efficacy of gene transfer for Leber's congenital amaurosis. N Engl J Med. 2008;358:2240–2248. doi: 10.1056/NEJMoa0802315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loeb JE, Cordier WS, Harris ME, Weitzman MD, Hope TJ. Enhanced expression of transgenes from adeno-associated virus vectors with the woodchuck hepatitis virus posttranscriptional regulatory element: implications for gene therapy. Hum Gene Ther. 1999;10:2295–2305. doi: 10.1089/10430349950016942. [DOI] [PubMed] [Google Scholar]
- 12.LeWitt PA, Rezai AR, Leehey MA. AAV2-GAD gene therapy for advanced Parkinson's disease: a double-blind, sham-surgery controlled, randomised trial. Lancet Neurol. 2011;10:309–319. doi: 10.1016/S1474-4422(11)70039-4. [DOI] [PubMed] [Google Scholar]
- 13.Anand V, Barral DC, Zeng Y. Gene therapy for choroideremia: in vitro rescue mediated by recombinant adenovirus. Vision Res. 2003;43:919–926. doi: 10.1016/s0042-6989(02)00389-9. [DOI] [PubMed] [Google Scholar]
- 14.Tolmachova T, Tolmachov OE, Barnard AR. Functional expression of Rab escort protein 1 following AAV2-mediated gene delivery in the retina of choroideremia mice and human cells ex vivo. J Mol Med (Berl) 2013;91:825–837. doi: 10.1007/s00109-013-1006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bennicelli J, Wright JF, Komaromy A. Reversal of blindness in animal models of Leber congenital amaurosis using optimized AAV2-mediated gene transfer. Mol Ther. 2008;16:458–465. doi: 10.1038/sj.mt.6300389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klein R, Klein BE, Moss SE, DeMets D. Inter-observer variation in refraction and visual acuity measurement using a standardized protocol. Ophthalmology. 1983;90:1357–1359. doi: 10.1016/s0161-6420(83)34382-7. [DOI] [PubMed] [Google Scholar]
- 17.Chen FK, Patel PJ, Xing W. Test-retest variability of microperimetry using the Nidek MP1 in patients with macular disease. Invest Ophthalmol Vis Sci. 2009;50:3464–3472. doi: 10.1167/iovs.08-2926. [DOI] [PubMed] [Google Scholar]
- 18.Cideciyan AV, Jacobson SG, Beltran WA. Human retinal gene therapy for Leber congenital amaurosis shows advancing retinal degeneration despite enduring visual improvement. Proc Natl Acad Sci USA. 2013;110:E517–E525. doi: 10.1073/pnas.1218933110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bennett J, Ashtari M, Wellman J. AAV2 gene therapy readministration in three adults with congenital blindness. Sci Transl Med. 2012;4:120ra15. doi: 10.1126/scitranslmed.3002865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cideciyan AV, Hauswirth WW, Aleman TS. Vision 1 year after gene therapy for Leber's congenital amaurosis. N Engl J Med. 2009;361:725–727. doi: 10.1056/NEJMc0903652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Endo K, Yuzawa M, Ohba N. Choroideremia associated with subretinal neovascular membrane. Acta Ophthalmol Scand. 2000;78:483–486. doi: 10.1034/j.1600-0420.2000.078004483.x. [DOI] [PubMed] [Google Scholar]
- 22.Bowne SJ, Humphries MM, Sullivan LS. A dominant mutation in RPE65 identified by whole-exome sequencing causes retinitis pigmentosa with choroidal involvement. Eur J Hum Genet. 2011;19:1074–1081. doi: 10.1038/ejhg.2011.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tolmachova T, Wavre-Shapton ST, Barnard AR, MacLaren RE, Futter CE, Seabra MC. Retinal pigment epithelium defects accelerate photoreceptor degeneration in cell type-specific knockout mouse models of choroideremia. Invest Ophthalmol Vis Sci. 2010;51:4913–4920. doi: 10.1167/iovs.09-4892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vandenberghe LH, Bell P, Maguire AM. Dosage thresholds for AAV2 and AAV8 photoreceptor gene therapy in monkey. Sci Transl Med. 2011;3:88ra54. doi: 10.1126/scitranslmed.3002103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maguire AM, High KA, Auricchio A. Age-dependent effects of RPE65 gene therapy for Leber's congenital amaurosis: a phase 1 dose-escalation trial. Lancet. 2009;374:1597–1605. doi: 10.1016/S0140-6736(09)61836-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van den Hurk JA, Schwartz M, van Bokhoven H. Molecular basis of choroideremia (CHM): mutations involving the Rab escort protein-1 (REP-1) gene. Hum Mutat. 1997;9:110–117. doi: 10.1002/(SICI)1098-1004(1997)9:2<110::AID-HUMU2>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 27.MacLaren RE. An analysis of retinal gene therapy clinical trials. Curr Opin Mol Ther. 2009;11:540–546. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Robert E MacLaren discusses how gene therapy improves eyesight in people born with choroideremia.