Abstract
Background:
Calcific uremic arteriolopathy (CUA), a debilitating condition with high morbidity and mortality, is most commonly seen in patients with kidney disease. The pathophysiology of CUA is multifactorial, leading to a disruption in the balance between factors that promote and those that inhibit calcification, although the exact pathophysiological mechanisms of CUA remain to be elucidated.
Methods:
This review provides an overview of the pathophysiology, clinical presentation and diagnosis, and treatment of CUA.
Results:
Diagnosis of CUA requires a high degree of suspicion; skin biopsy with histological examination remains the gold standard to confirm the diagnosis. Treatment of CUA requires a multidisciplinary approach.
Conclusion:
With a high degree of clinical suspicion and early diagnosis, an aggressive multifactorial treatment approach involving optimal wound management, minimization/avoidance of risk factors and precipitating causes, and correction of calcium-phosphorus abnormalities can significantly improve patient outcomes.
Keywords: Calciphylaxis, hyperparathyroidism, sodium thiosulfate, vascular calcification, wound healing
INTRODUCTION
Calcific uremic arteriolopathy (CUA), often referred to as calciphylaxis, is a condition with high morbidity and mortality seen in patients with kidney disease, especially in those with end stage renal disease (ESRD). When this condition is seen in patients without kidney disease, most notably those with primary hyperparathyroidism, malignancy, alcoholic liver disease, or connective tissue disease, it is known as nonuremic CUA.1 This review focuses on the pathophysiology and management of CUA in the ESRD population.
Although previous small studies have reported a CUA prevalence of 4% in patients on hemodialysis, and 1.3-4.5 per 100 patient years in patients with ESRD, the exact prevalence remains unknown.2,3 The number of reported CUA cases has increased in recent years, probably because of the increased recognition of this condition.
In 1962, Hans Selye coined the term calciphylaxis to describe skin necrosis in animals triggered by exposure to certain substances during experiments, such as parathyroid hormone and vitamin D, and associated with cutaneous calcification.4 However, these lesions are different from the CUA lesions now described in humans. Histopathological examination of human CUA lesions shows small-vessel medial calcification and intimal hypertrophy in association with panniculitis and small-vessel thrombosis that were not described in Selye's animals. Coates et al suggested that the term calcific uremic arteriolopathy would be more apt to describe these lesions;5 however, the term calciphylaxis is still frequently used to refer to this condition in humans.
PATHOPHYSIOLOGY
CUA is thought to develop secondary to a disruption of balance between factors that favor calcification and those that normally prevent pathologic calcification.6 Previously, an increase in the calcium-phosphorus product was thought to cause calcification leading to CUA, but recent research suggests that this calcification involves active cellular processes, not just passive mineralization, because of an increase in calcium-phosphorus concentrations.7
Extensive vascular medial calcification is a hallmark of the vasculopathy seen with chronic kidney disease and is associated with increased cardiovascular mortality. CUA involves vascular medial calcification of small arterioles with different clinical manifestations depending on the organ involved, but most commonly skin necrosis.
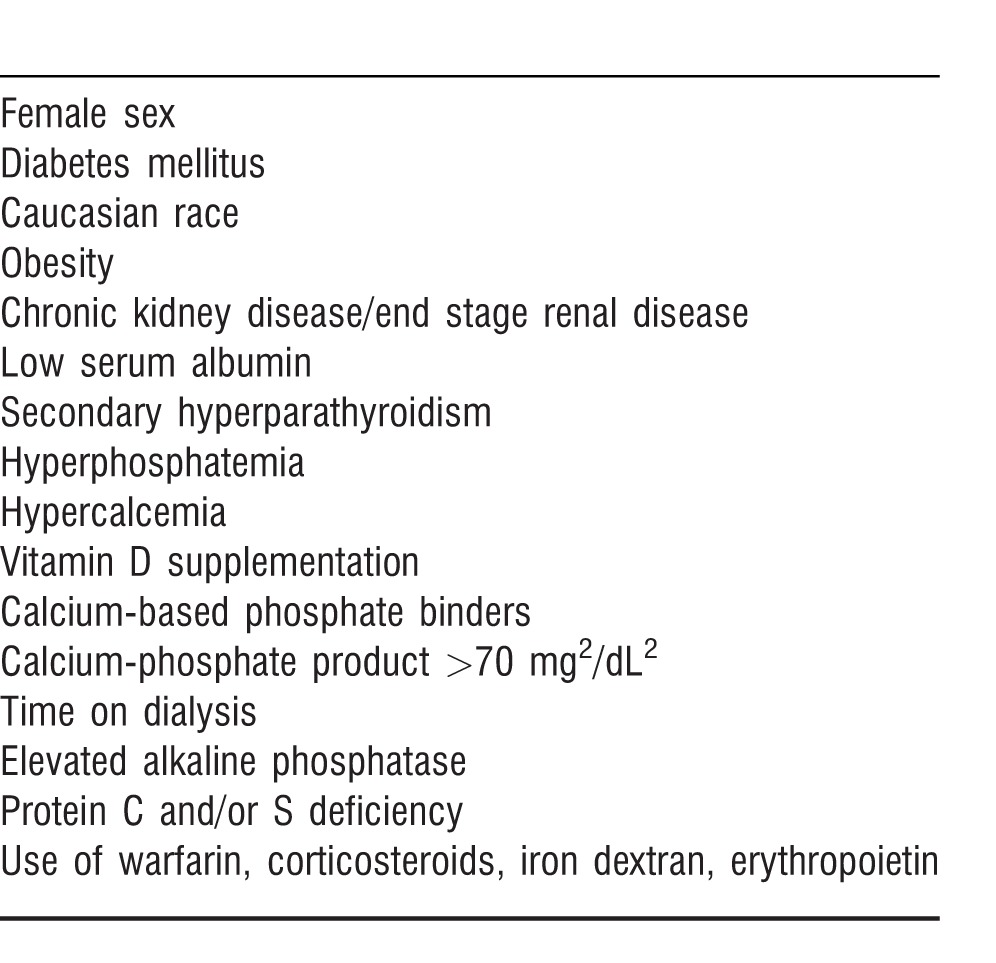
Multiple risk factors have been associated with the development of CUA (Table).2,8-12 Of these, female sex, diabetes, and obesity have been shown to be independent risk factors.9,12 One study showed peritoneal dialysis as a risk factor for CUA, but the exact mechanism is unclear,1 and this association has not been validated in further studies.13
Table.
Risk Factors for Calcific Uremic Arteriolopathy
In vitro studies of human smooth muscle cells have shown an increase in the expression of osteogenic markers that predispose patients to calcification on recurrent exposure to high phosphorus levels and other uremic toxins.14,15
Vascular smooth muscle cells in CUA lesions have increased osteopontin expression that is thought to promote vessel lumen occlusion prior to thrombosis by causing cell sloughing into the lumen.8 In addition, bone morphogenetic protein-4 (BMP-4), which is normally involved in bone repair and development, has appeared in CUA lesions and is thought to promote calcification.16 The action of BMP-4 is thought to be dependent on the production of reactive oxygen species (ROS) that can activate nuclear factor kappa B (NFκB).17 In addition, ESRD is a chronic inflammatory state associated with increased generation of NFκB and receptor activator of NFκB ligand (RANKL), suggesting the role of NFκB-osteoprotegerin/receptor activator of NFκB/RANKL axis in bone homeostasis and vascular calcification.18
Patients on hemodialysis also have low levels of fetuin-A/α 2-Heremans-Schmid glycoprotein (AHSG), a circulating inhibitor of calcification found in human and animal models.19 The production of AHSG is also downregulated in systemic inflammation because it is a negative phase reactant.7
Matrix Gla protein (MGP) is another calcification inhibitor expressed by in vitro calcification models; MGP knockout mice show extensive vascular calcification but not CUA. The role of MGP in the development of CUA is unclear,7 but based on the association between CUA and warfarin (a vitamin K antagonist that inhibits γ-carboxylation of MGP), MGP may play a role in the pathogenesis of CUA.20 A case-control study from Japan indicated warfarin therapy and low albumin level as strong and significant risk factors for the development of CUA in patients on hemodialysis.21
A decrease in the levels of circulating inhibitors of calcification in ESRD under the influence of uremic mileu, hyperphosphatemia in particular, is thought to trigger the differentiation of vascular smooth muscle cells into osteoblasts, resulting in vascular calcification. However, vascular calcification alone does not lead to CUA lesions, is thought to precede the development of typical CUA, and can occur either concurrently or be separated by months or years.22-24 Wilmer and Magro hypothesized that the vascular lesion develops in the first stage of CUA, which is a period of sensitization induced by parathyroid hormone, vitamin D, or high calcium/phosphorus (similar to Selye's calciphylaxis).24 The second stage is a period of challenge such as trauma, surgery, or any other event associated with an increase in inflammatory cytokines. The second stage is marked by end-organ ischemia developments because of expansion of calcific vascular lesions associated with obliterative endovascular fibrosis/vascular thrombosis.
CLINICAL PRESENTATION AND DIAGNOSIS
Clinical diagnosis of CUA requires a high degree of suspicion. Other conditions need to be considered and excluded during the diagnosis of CUA, including warfarin-induced skin necrosis, vasculitis, cholesterol embolism syndrome, and nephrogenic systemic fibrosis. CUA lesions initially present as excruciatingly painful subcutaneous nodules with violaceous mottling, similar to livedo reticularis. These lesions can form ulcers and eschars as a result of ischemic necrosis. CUA lesions typically affect areas of the body with higher fat concentrations, such as breasts, abdomen, thighs, hips, and shoulders. Secondary infection is common and can lead to sepsis, which is the main cause of mortality in this patient population. Although the diagnosis of CUA can be made clinically, histopathological examination of a skin biopsy specimen remains the gold standard. The pathognomonic histopathological findings of CUA have been described as medial calcification of small arteries and arterioles up to 600 μm with intimal hyperplasia, inflammation, endovascular fibrosis, thrombosis, and tissue necrosis. Panniculitis can also be present.10,23-25
The biopsy method, however, raises concern for initiating a new ulcer that may not heal. Bone scintigraphy, a noninvasive procedure, has been described as useful in the diagnosis of CUA because of its ability to detect soft tissue microcalcifications.26-28 Bone scintigraphy has a sensitivity of 97% in detecting abnormal calcifications and is also thought to reveal the true extent of disease better than clinical examination alone. Bone scintigraphy has also been described as a useful tool for monitoring progress/improvement with treatment.9
TREATMENT
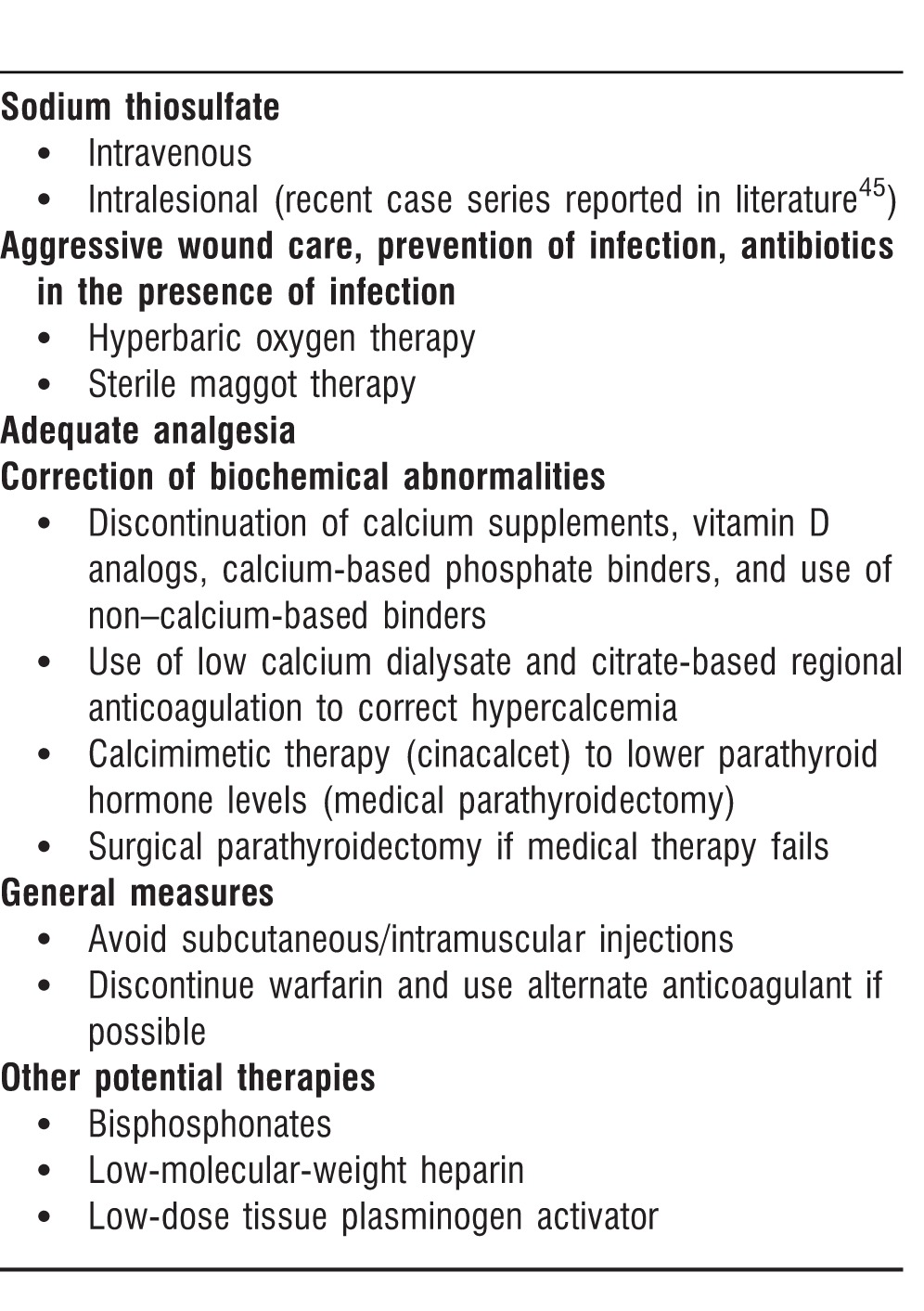
Treatment of CUA requires a multidisciplinary approach involving optimal wound management, antibiotic use in the presence of infection, correction of biochemical abnormalities, avoidance of cutaneous/subcutaneous trauma, and use of sodium thiosulfate (Treatment Options sidebar).
General Measures
Subcutaneous or intramuscular injections should be avoided to prevent trauma and ulcer formation. The risk factors associated with the development of CUA should be minimized where possible, including discontinuing warfarin if alternate anticoagulants are possible because warfarin has been implicated in the development of CUA by blocking vitamin K-dependent carboxylation of MGP.
Anecdotal data suggest intensifying the hemodialysis regimen (4 hours daily for 7 days followed by 5-6 times a week) as part of a multiinterventional approach in the treatment of CUA;29 this treatment may help correct hyperphosphatemia.
Wound Care
Optimal wound care with special attention to prevention of superinfection and sepsis is vital in the management of CUA. Wound management aims to remove the necrotic tissue, aid in wound healing, prevent infection, and help with pain control. Gentle debridement to remove the necrotic tissue may be needed to allow proper wound healing, although debridement is not indicated for wounds covered with eschars. Sterile maggot therapy has also been used successfully in the debridement of necrotic CUA ulcers and is an option for wound management in CUA.30,31
CUA lesions are extremely painful, often requiring use of narcotic analgesia for general pain control. Morphine is thought to cause accumulation of toxic morphine glucuronide by-products that may cause hypotension and further decrease tissue perfusion; therefore, fentanyl may be preferred for pain control.7
Hyperbaric oxygen (HBO) has been described to promote wound healing in CUA lesions.32 HBO therapy is thought to promote angiogenesis, arteriolar vasoconstriction, and bactericidal activity of neutrophils by forming ROS and to stimulate fibroblast function by improving oxygenation of the wound.32,33
Although not a routine practice, according to one report, limb revascularization as a treatment for CUA lesions involving the extremities led to poor outcomes; lesions did not improve and continued to progress in many patients.34
Correction of Biochemical Abnormalities
Once the diagnosis of CUA is made, measures should be taken to lower calcium, phosphorus, and parathyroid hormone levels. Calcium-based phosphorus binders should be replaced with non–calcium-based binders; calcium supplements and vitamin D analogs should be discontinued to prevent or treat hypercalcemia.
In our experience, we have used low-calcium dialysate and extended dialysis therapies with citrate-based regional anticoagulation and systemic calcium infusion to maintain serum calcium levels in the normal to low-normal levels for patients with hypercalcemia.
Secondary hyperparathyroidism can be treated medically with a calcimimetic such as cinacalcet, but parathyroidectomy may be required in cases that do not respond to medical treatment. A prospective randomized trial studying the effect of parathyroidectomy on survival from CUA showed that surgical correction afforded superior benefit compared to medical therapy; however, this study was completed prior to the availability of newer non–calcium-based phosphate binders and calcimimetic agents such as cinacalcet.35
Sodium Thiosulfate
Sodium thiosulfate (STS) is known as an antidote for cyanide poisoning, but it has also been used to prevent cisplatin and carboplatin toxicity. It is now becoming known as a treatment for CUA.
A study by Nigwekar et al evaluated the response of 172 patients with CUA to intravenous (IV) STS treatment and found that the majority of the patients showed improvement with this therapy.36 STS is thought to treat CUA through its antioxidant activity and the chelation of calcium to form calcium thiosulfate complexes.22,37 STS has been shown to prevent vascular calcification in a uremic rat model by forming highly soluble complexes with calcium, thus preventing calcium phosphate precipitation.38 The antioxidant activity of STS may result from the 2 unpaired electrons it has, which it donates to scavenge the unpaired electrons associated with ROS.23 STS has been reported to provide rapid pain relief within a few weeks for patients with CUA, perhaps the result of its antioxidant properties leading to recoupling of the endothelial nitric oxide synthase and, consequently, to a decrease in subdermal ischemia and associated pain.22,23
STS is usually given at a dose of 25 gm IV (at the end of dialysis for patients on hemodialysis) 3 times a week. It is usually well tolerated; the most common side effects are nausea, vomiting, diarrhea, and abdominal cramping. Long-term STS use has been associated with decreased bone strength, and, as a result, bone density should be monitored for patients with long-term use.38 STS use has also been associated with increased anion gap metabolic acidosis that can be managed by adjusting bicarbonate concentration in the dialysate.39,40 Successful intraperitoneal use of STS has also been reported for the treatment of CUA,41 but another case reported chemical peritonitis with its use.42
Although the antioxidant effects of STS are seen early in the treatment, the chelating effects that potentially decrease the subcutaneous and vascular calcification with subsequent healing of the CUA lesions may take longer.22,23,38,43,44 In our experience, we have used STS until the wounds are completely healed, about 3 months on average; other anecdotal experiences recommend continuing STS treatment for about 2 months after the CUA lesions are healed.22,23
A report of 4 patients successfully treated with intralesional STS published in 2013 suggests that this highly targeted therapy has some promise, but this use must be studied further.45 The use of oral STS following IV STS treatment in 4 patients stabilized or improved CUA lesions, suggesting oral STS as maintenance therapy given the high cost of IV STS.46
Other Potential Therapeutic Options
Given the histological findings of arterial thrombi in CUA, anticoagulants such as low-molecular-weight heparin and thrombolytic therapy have been tried as treatment. One study reported complete healing of CUA lesions with the use of Fraxiparine.47 In another case report, low-dose tissue plasminogen activator was shown to help with wound healing in CUA.48
Bisphosphonates, which reportedly increase osteoprotegerin production and inhibit NFκB/RANKL activity that can decrease osseous mineral loss and extraosseous mineralization, have been used to treat CUA with some success.43,44,49,50 Bisphosphonates can also decrease proinflammatory cytokines such as tumor necrosis factor α, interleukin (IL)-1, and IL-6.51
The use of corticosteroids in the treatment of CUA remains controversial. In one report, the use of prednisone in patients with nonulcerated lesions resulted in stabilization or improvement of the lesions;9 however, prednisone is considered a risk factor for CUA and may predispose the patient to systemic infection.10
TREATMENT OPTIONS FOR CALCIFIC UREMIC ARTERIOLOPATHY
CALCIPHYLAXIS REGISTRY
The Kansas University Medical Center has established a global registry of calciphylaxis cases, and practitioners managing patients with CUA can provide medical information at the following website: www2.kumc.edu/calciphylaxisregistry/. This registry may provide valuable information on the progression and treatment of this debilitating condition.
CONCLUSION
CUA is a debilitating and potentially fatal disorder, primarily affecting patients with kidney disease. However, with a high degree of clinical suspicion and early diagnosis, an aggressive multifactorial treatment approach involving optimal wound management, minimization/avoidance of risk factors and precipitating causes, and correction of calcium-phosphorus abnormalities can significantly improve patient outcomes, especially with the recent promise of STS use.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Nigwekar SU, Wolf M, Sterns RH, Hix JK. Calciphylaxis from nonuremic causes: a systematic review. Clin J Am Soc Nephrol. Jul. 2008;3(4):1139–1143. doi: 10.2215/CJN.00530108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Angelis M, Wong LL, Myers SA, Wong LM. Calciphylaxis in patients on hemodialysis: a prevalence study. Surgery. 1997 Dec;122(6):1083–1089. doi: 10.1016/s0039-6060(97)90212-9. discussion 1089-1090. [DOI] [PubMed] [Google Scholar]
- 3.Fine A, Fontaine B. Calciphylaxis: the beginning of the end? Perit Dial Int. 2008 May-Jun;28(3):268–270. [PubMed] [Google Scholar]
- 4.Selye H. Calciphylaxis. Chicago, IL: University of Chicago Press;; 1962. [Google Scholar]
- 5.Coates T, Kirkland GS, Dymock RB, et al. Cutaneous necrosis from calcific uremic arteriolopathy. Am J Kidney Dis. 1998 Sep;32(3):384–391. doi: 10.1053/ajkd.1998.v32.pm9740153. [DOI] [PubMed] [Google Scholar]
- 6.Schlieper G, Westenfeld R, Brandenburg V, Ketteler M. Inhibitors of calcification in blood and urine. Semin Dial. 2007 Mar-Apr;20(2):113–121. doi: 10.1111/j.1525-139X.2007.00257.x. [DOI] [PubMed] [Google Scholar]
- 7.Rogers NM, Teubner DJ, Coates PT. Calcific uremic arteriolopathy: advances in pathogenesis and treatment. Semin Dial. 2007 Mar-Apr;20(2):150–157. doi: 10.1111/j.1525-139X.2007.00263.x. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed S, O'Neill KD, Hood AF, Evan AP, Moe SM. Calciphylaxis is associated with hyperphosphatemia and increased osteopontin expression by vascular smooth muscle cells. Am J Kidney Dis. 2001 Jun;37(6):1267–1276. doi: 10.1053/ajkd.2001.24533. [DOI] [PubMed] [Google Scholar]
- 9.Fine A, Zacharias J. Calciphylaxis is usually non-ulcerating: risk factors, outcome and therapy. Kidney Int. 2002 Jun;61(6):2210–2217. doi: 10.1046/j.1523-1755.2002.00375.x. [DOI] [PubMed] [Google Scholar]
- 10.Weenig RH, Sewell LD, Davis MD, McCarthy JT, Pittelkow MR. Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007 Apr;56(4):569–579. doi: 10.1016/j.jaad.2006.08.065. Epub 2006 Dec 1. [DOI] [PubMed] [Google Scholar]
- 11.Bleyer AJ, Choi M, Igwemezie B, de la Torre E, White WL. A case control study of proximal calciphylaxis. Am J Kidney Dis. 1998 Sep;32(3):376–383. doi: 10.1053/ajkd.1998.v32.pm9740152. [DOI] [PubMed] [Google Scholar]
- 12.Mazhar AR, Johnson RJ, Gillen D, et al. Risk factors and mortality associated with calciphylaxis in end-stage renal disease. Kidney Int. 2001 Jul;60(1):324–332. doi: 10.1046/j.1523-1755.2001.00803.x. [DOI] [PubMed] [Google Scholar]
- 13.New N, Mohandas J, John GT, et al. Calcific uremic arteriolopathy in peritoneal dialysis populations. Int J Nephrol. 2011;2011:982854. doi: 10.4061/2011/982854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giachelli CM, Jono S, Shioi A, Nishizawa Y, Mori K, Morii H. Vascular calcification and inorganic phosphate. Am J Kidney Dis. 2001 Oct;38((4 Suppl 1)):S34–S37. doi: 10.1053/ajkd.2001.27394. [DOI] [PubMed] [Google Scholar]
- 15.Nishizawa Y, Jono S, Ishimura E, Shioi A. Hyperphosphatemia and vascular calcification in end-stage renal disease. J Ren Nutr. 2005 Jan;15(1):178–182. doi: 10.1053/j.jrn.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 16.Griethe W, Schmitt R, Jurgensen JS, Bachmann S, Eckardt KU, Schindler R. Bone morphogenic protein-4 expression in vascular lesions of calciphylaxis. J Nephrol. 2003 Sep-Oct;16(5):728–732. [PubMed] [Google Scholar]
- 17.Feng JQ, Xing L, Zhang JH, et al. NF-kappaB specifically activates BMP-2 gene expression in growth plate chondrocytes in vivo and in a chondrocyte cell line in vitro. J Biol Chem. 2003 Aug 1;278(31):29130–29135. doi: 10.1074/jbc.M212296200. Epub 2003 May 20. [DOI] [PubMed] [Google Scholar]
- 18.Kiechl S, Werner P, Knoflach M, Furtner M, Willeit J, Schett G. The osteoprotegerin/RANK/RANKL system: a bone key to vascular disease. Expert Rev Cardiovasc Ther. 2006 Nov;4(6):801–811. doi: 10.1586/14779072.4.6.801. [DOI] [PubMed] [Google Scholar]
- 19.Schafer C, Heiss A, Schwarz A, et al. The serum protein alpha 2-Heremans-Schmid glycoprotein/fetuin-A is a systemically acting inhibitor of ectopic calcification. J Clin Invest. 2003 Aug;112(3):357–366. doi: 10.1172/JCI17202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wallin R, Cain D, Hutson SM, Sane DC, Loeser R. Modulation of the binding of matrix Gla protein (MGP) to bone morphogenetic protein-2 (BMP-2) Thromb Haemost. 2000 Dec;84(6):1039–1044. [PubMed] [Google Scholar]
- 21.Hayashi M, Takamatsu I, Kanno Y, Yoshida T, Abe T, Sato Y. Japanese Calciphylaxis Study Group. A case-control study of calciphylaxis in Japanese end-stage renal disease patients. Nephrol Dial Transplant. 2012 Apr;27(4):1580–1584. doi: 10.1093/ndt/gfr658. Epub 2011 Nov 25. [DOI] [PubMed] [Google Scholar]
- 22.Hayden MR, Goldsmith D, Sowers JR, Khanna R. Calciphylaxis: calcific uremic arteriolopathy and the emerging role of sodium thiosulfate. Int Urol Nephrol. 2008;40(2):443–451. doi: 10.1007/s11255-008-9373-4. [DOI] [PubMed] [Google Scholar]
- 23.Hayden MR, Tyagi SC, Kolb L, Sowers JR, Khanna R. Vascular ossification-calcification in metabolic syndrome, type 2 diabetes mellitus, chronic kidney disease, and calciphylaxis-calcific uremic arteriolopathy: the emerging role of sodium thiosulfate. Cardiovasc Diabetol. 2005 Mar 18;4(1):4. doi: 10.1186/1475-2840-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilmer WA, Magro CM. Calciphylaxis: emerging concepts in prevention, diagnosis, and treatment. Semin Dial. 2002 May-Jun;15(3):172–186. doi: 10.1046/j.1525-139x.2002.00052.x. [DOI] [PubMed] [Google Scholar]
- 25.Don BR, Chin AI. A strategy for the treatment of calcific uremic arteriolopathy (calciphylaxis) employing a combination of therapies. Clin Nephrol. 2003 Jun;59(6):463–470. doi: 10.5414/cnp59463. [DOI] [PubMed] [Google Scholar]
- 26.Han MM, Pang J, Shinkai K, Franc B, Hawkins R, Aparici CM. Calciphylaxis and bone scintigraphy: case report with histological confirmation and review of the literature. Ann Nucl Med. 2007 Jun;21(4):235–258. doi: 10.1007/s12149-007-0013-3. Epub 2007 Jun 25. [DOI] [PubMed] [Google Scholar]
- 27.Norris B, Vaysman V, Line BR. Bone scintigraphy of calciphylaxis: a syndrome of vascular calcification and skin necrosis. Clin Nucl Med. 2005 Nov;30(11):725–727. doi: 10.1097/01.rlu.0000182215.97219.72. [DOI] [PubMed] [Google Scholar]
- 28.Cosmin A, Soudry G. A case of severe calciphylaxis seen on three-phase bone scan. Clin Nucl Med. 2005 Nov;30(11):765–766. doi: 10.1097/01.rlu.0000182282.66664.64. [DOI] [PubMed] [Google Scholar]
- 29.Baldwin C, Farah M, Leung M, et al. Multi-intervention management of calciphylaxis: a report of 7 cases. Am J Kidney Dis. 2011 Dec;58(6):988–991. doi: 10.1053/j.ajkd.2011.06.022. Epub 2011 Aug 26. [DOI] [PubMed] [Google Scholar]
- 30.Picazo M, Bover J, de la Fuente J, Sans R, Cuxart M, Matas M. Sterile maggots as adjuvant procedure for local treatment in a patient with proximal calciphylaxis [in Spanish] Nefrologia. 2005;25(5):559–562. [PubMed] [Google Scholar]
- 31.Tittelbach J, Graefe T, Wollina U. Painful ulcers in calciphylaxis - combined treatment with maggot therapy and oral pentoxyfillin. J Dermatolog Treat. 2001 Dec;12(4):211–214. doi: 10.1080/09546630152696035. [DOI] [PubMed] [Google Scholar]
- 32.Rogers NM, Chang S, Teubner D, Coates P. Hyperbaric oxygen as effective adjuvant therapy in the treatmentof distal calcific uraemic arteriolopathy. Nephrol Dial Transplant Plus. 2008;1(4):244–249. doi: 10.1093/ndtplus/sfn036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gordillo GM, Sen CK. Revisiting the essential role of oxygen in wound healing. Am J Surg. 2003 Sep;186(3):259–263. doi: 10.1016/s0002-9610(03)00211-3. [DOI] [PubMed] [Google Scholar]
- 34.Friedman SG. Leg revascularization in patients with calciphylaxis. Am Surg. 2002 Jul;68(7):591–592. [PubMed] [Google Scholar]
- 35.Girotto JA, Harmon JW, Ratner LE, Nicol TL, Wong L, Chen H. Parathyroidectomy promotes wound healing and prolongs survival in patients with calciphylaxis from secondary hyperparathyroidism. Surgery. 2001 Oct;130(4):645–650. doi: 10.1067/msy.2001.117101. discussion 650-651. [DOI] [PubMed] [Google Scholar]
- 36.Nigwekar SU, Brunelli SM, Meade D, Wang W, Hymes J, Lacson E., Jr Sodium thiosulfate therapy for calcific uremic arteriolopathy. Clin J Am Soc Nephrol. 2013 Mar 21;8(7):1162–1170. doi: 10.2215/CJN.09880912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raymond CB, Wazny LD. Sodium thiosulfate, bisphosphonates, and cinacalcet for treatment of calciphylaxis. Am J Health Syst Pharm. 2008 Aug 1;65(15):1419–1429. doi: 10.2146/ajhp070546. Erratum in: Am J Health Syst Pharm. 2010 Jan 1;67(1):8. [DOI] [PubMed] [Google Scholar]
- 38.Pasch A, Schaffner T, Huynh-Do U, Frey BM, Frey FJ, Farese S. Sodium thiosulfate prevents vascular calcifications in uremic rats. Kidney Int. 2008 Dec;74(11):1444–1453. doi: 10.1038/ki.2008.455. Epub 2008 Sep 24. [DOI] [PubMed] [Google Scholar]
- 39.Cicone JS, Petronis JB, Embert CD, Spector DA. Successful treatment of calciphylaxis with intravenous sodium thiosulfate. Am J Kidney Dis. 2004 Jun;43(6):1104–1108. doi: 10.1053/j.ajkd.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 40.Brucculeri M, Cheigh J, Bauer G, Serur D. Long-term intravenous sodium thiosulfate in the treatment of a patient with calciphylaxis. Semin Dial. 2005 Sep-Oct;18(5):431–434. doi: 10.1111/j.1525-139X.2005.00082.x. [DOI] [PubMed] [Google Scholar]
- 41.Mataic D, Bastani B. Intraperitoneal sodium thiosulfate for the treatment of calciphylaxis. Ren Fail. 2006;28(4):361–363. doi: 10.1080/08860220600583781. [DOI] [PubMed] [Google Scholar]
- 42.Gupta DR, Sangha H, Khanna R. Chemical peritonitis after intraperitoneal sodium thiosulfate. Perit Dial Int. 2012 Mar-Apr;32(2):220–222. doi: 10.3747/pdi.2011.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shiraishi N, Kitamura K, Miyoshi T, et al. Successful treatment of a patient with severe calcific uremic arteriolopathy (calciphylaxis) by etidronate disodium. Am J Kidney Dis. 2006 Jul;48(1):151–154. doi: 10.1053/j.ajkd.2006.04.062. [DOI] [PubMed] [Google Scholar]
- 44.Rogers NM, Coates PT. Calcific uraemic arteriolopathy: an update. Curr Opin Nephrol Hypertens. 2008 Nov;17(6):629–634. doi: 10.1097/MNH.0b013e32830f4566. [DOI] [PubMed] [Google Scholar]
- 45.Strazzula L, Nigwekar SU, Steele D, et al. Intralesional sodium thiosulfate for the treatment of calciphylaxis. JAMA Dermatol. 2013 Aug;149(8):946–949. doi: 10.1001/jamadermatol.2013.4565. [DOI] [PubMed] [Google Scholar]
- 46.AlBugami MM, Wilson JA, Clarke JR, Soroka SD. Oral sodium thiosulfate as maintenance therapy for calcific uremic arteriolopathy: a case series. Am J Nephrol. 2013;37(2):104–109. doi: 10.1159/000346410. Epub 2013 Jan 25. [DOI] [PubMed] [Google Scholar]
- 47.Perez-Mijares R, Guzman-Zamudio JL, Payan-Lopez J, Rodriguez-Fernandez A, Gomez-Fernandez P, Almaraz-Jimenez M. Calciphylaxis in a haemodialysis patient: functional protein S deficiency? Nephrol Dial Transplant. 1996 Sep;11(9):1856–1859. [PubMed] [Google Scholar]
- 48.Sewell LD, Weenig RH, David MD, McEvoy MT, Pittelkow MR. Low-dose tissue plasminogen activator for calciphylaxis. Arch Dermatol. 2004 Sep;140(9):1045–1048. doi: 10.1001/archderm.140.9.1045. [DOI] [PubMed] [Google Scholar]
- 49.Monney P, Nguyen QV, Perroud H, Descombes E. Rapid improvement of calciphylaxis after intravenous pamidronate therapy in a patient with chronic renal failure. Nephrol Dial Transplant. 2004 Aug;19(8):2130–2132. doi: 10.1093/ndt/gfh305. [DOI] [PubMed] [Google Scholar]
- 50.Viereck V, Emons G, Lauck V, et al. Bisphosphonates pamidronate and zoledronic acid stimulate osteoprotegerin production by primary human osteoblasts. Biochem Biophys Res Commun. 2002 Mar 1;291(3):680–686. doi: 10.1006/bbrc.2002.6510. [DOI] [PubMed] [Google Scholar]
- 51.Pennanen N, Lapinjoki S, Urtti A, Mönkkönen J. Effect of liposomal and free bisphosphonates on the IL-1 beta, IL-6 and TNF alpha secretion from RAW 264 cells in vitro. Pharm Res. 1995 Jun;12(6):916–922. doi: 10.1023/a:1016281608773. [DOI] [PubMed] [Google Scholar]


