Abstract
Treatment of type 1 diabetes is a challenging issue in South East Asia. Unlike in the developed countries, patients have to procure insulin, glucometer strips and other treatment facilities from their own pockets. Coupled with poor resources are the difficulties with diagnosis, insulin initiation, insulin storage, marital and emotional challenges. Being a disease affecting only a minority of people, it is largely ignored by the governments and policy makers. Comprehensive diagnostic, treatment and team based educational facilities are available only in the speciality diabetes centers in the private sector whereas majority of the subjects with type 1 diabetes are from a poor socio-economic background. Unlike in the Western world, being known as a diabetes patient is a social sigma and poses huge emotional burden living with the disease and getting married. Even with best of the resources, long-term treatment of type 1 diabetes still remains a huge challenge across the globe. In this review, authors from India, Pakistan, Nepal, Sri Lanka, Myanmar and Bangladesh detail the country-specific challenges and discuss the possible solutions.
Keywords: Challenges, South East Asia, type 1 diabetes
INTRODUCTION
Type 1 diabetes (T1DM) is a chronic autoimmune metabolic disorder characterized by widespread damage of beta cells, ensuing insulin deficiency and corresponding hyperglycemia. Certain environmental factors trigger the autoimmune pathways in genetically predisposed children and adolescents.[1] As compared to type 2 diabetes (T2DM), T1DM is relatively less common but is associated with greater morbidity and mortality.
IDF Atlas 2013 reported nearly 78,000 T1DM patients in South-East Asia (SEA) with an addition of 12,500 new cases each year.[2] The chronicity and absolute insulin deficiency makes T1DM a challenging disease to manage. Coupled to therapeutic issues, other factors like insulin acceptance, availability, storage and compliance also contribute to the complexity of the management. These factors operate more strongly in SEA countries due to their typical cultural and socio-economic belief, poor healthcare infrastructure and low government funding, which have resulted in a considerably higher morbidity and mortality.[3]
The objective of this descriptive article is to highlight the issues prevalent in SEA countries that preclude the optimal management of T1DM. An extensive search was conducted on the Pubmed and Cochrane databases to identify literature published between the year 1980 and 2014. Very limited studies, which focused on challenges associated with T1DM in SEA region were found. The scope of the search was then widened to identify the studies conducted globally. Snowball and gray-literature search was also conducted to supplement the results of primary database search. In view of the paucity of published literature, the authors from India, Myanmar, Bangladesh, Nepal, Pakistan and Sri Lanka narrated the challenges encountered by them in management of T1DM patients. The authors noted their observations on challenges related to diagnosis, insulin therapy, behavioral changes, lack of awareness, social and economic factors and prepared it as a descriptive article.
The article is organized in two sections. First section elaborates the challenges of managing T1DM in SEA. This is followed by a summary of issues as experienced by the authors and suggested corrective measures.
DIAGNOSTIC CHALLENGES
T1DM is often diagnosed late in SEA countries due to lack of advanced laboratories and other diagnostic facilities, which are required to confirm the disease. The presence of one or more serological markers of immune destruction of the β-cell which includes autoantibodies to islet cell, glutamic acid decarboxylase (GAD), insulinoma-associated antigens (IAs) IA-2, IA-2 β, or insulin are present in 85-90% of individuals when T1DM is initially detected.[4] Also, the disease has strong human leukocyte antigen (HLA) associations, presence of which can be either predisposing or protective. The detection of these markers, HLA typing and C-peptide measurements require a certain degree of sophistication, which is available only at select facilities in tertiary care centers. The late diagnosis results in delayed initiation of insulin and early development of complication of diabetes.
Recently, increasing prevalence of T2DM among adolescents has been realized in South Asian population.[5] Even pediatric endocrinologists in western countries have recognized T2DM in young population as an emerging epidemic among minority communities.[6] In a population based retrospective study by Harron et al., it was found that the rising incidence of T1DM in South Asians attenuated as T2DM increased after 1999. Among the diabetes of the young, 12% of patients were of T2DM. Therefore, the importance of prompt diagnosis increases as T2DM requires less intensive treatment and monitoring than T1DM. Symptom-based treatment may result in uncontrolled diabetes or treatment complications.[7] The clinical challenge in differentiating T1DM and T2DM can only be dealt by the use of autoimmune markers and HLA typing.
MANAGEMENT CHALLENGES
Insulin prescription
In SEA nations, a large proportion of patients with diabetes are treated by primary care physicians (PCPs). Their knowledge about the disease and modern treatment options including sophisticated insulin regimens is limited. Endocrinologist, diabetologist and specialist care are limited to metropolitan cities and tertiary centers. So even in cases where PCPs prescribe insulin, it is initiated late or with a sub-optimal dose. The primary concerns among PCPs towards initiation of insulin therapy are benefits vs. associated risks, patient perception towards insulin-based treatment and training on different insulin regimens available.[8]
Monitoring and therapy compliance
Self-care is an important tenet in the T1DM management. Medication compliance, self monitoring of blood glucose (SMBG), healthy eating and following optimal exercise schedule are critical to patient behaviors, which are detrimental to optimal blood glucose control.[9] T1DM patients have been found to benefit immensely by following these basic steps.[10,11,12,13] However, compliance to these is found to be lacking in chronic diseases like T1DM. A study has shown that only 30% of diabetics are compliant with the prescribed drug regimen.[14]
Anxiety arising out of frequent injections and perceived discomfort of insulin administration also plays an important role in insulin therapy non-adherence. It has been observed that patients tend to perform fewer than required SMBG, which has resulted in poorer glycemic control.[15]
Majority of T1DM patients attend regular school or colleges. They also frequently attend private coaching after regular school hours resulting in a hectic lifestyle. Compliance to insulin therapy, SMBG, regular eating hours and prescribed exercises are also negatively affected due to lack of time.
Hypoglycemia
Hypoglycemia is a common and potentially dangerous side effect of insulin therapy. Irregular dietary habits, typical food preferences and erratic exercise schedule make the adolescent T1DM patients susceptible to hypoglycemia. Patients on prolonged insulin therapy have been observed to have diminished hypoglycemia perception. This has been confirmed by Pramming et al., in a study where they reported that nearly 50% of patients on long-term insulin treatment have altered awareness of hypoglycemia-related symptoms.[16] Patients who experience frequent hypoglycemic episodes are anxious and worried and may limit the insulin usage because of fear of hypoglycemia.[17]
Insulin availability and storage
A large proportion of population lives in rural areas where the healthcare infrastructure is not satisfactory. Insulin availability in these regions poses a significant challenge in meeting the treatment goals. Further, insulin is required to be stored at a specific temperature range that can be attained only through refrigeration. Storage thus requires a constant supply of electricity, which cannot be assured in rural areas and villages in these countries.
BEHAVIORAL AND PSYCHOLOGICAL ISSUES
The diagnosis of T1DM requires major alterations in lifestyle of the patient and family members of T1DM patient. Multiple daily injections (MDI) of insulin and regular SMBG necessitate a lot of discipline. Such strict dosing and monitoring requirement can become emotionally challenging. Additionally, careful dietary planning is required to keep track of calories to maintain fine balance between the growth requirements and prevention of hyperglycemia. Over the course of time, a gradual transition of responsibility of treatment is required from the parents to the child. This stage is critical and a source of added stress to the patient. As the patient approaches adolescence, there is a subtle demand for autonomy and communication between family members and the patient tends to get restricted. These changes result in reduced adaptability towards prescribed management plan. Dynamic alterations in the insulin dosage that are required to be made during the course of growth and development of the child also pose a challenge.[18,19]
The side effects of weight gain associated with insulin also leads to avoidance of insulin by the patients in this age group who due to peer pressure are overtly weight conscious. In a study conducted by Borus et al., it was found that percentage of female patients who restricted insulin dosage secondary to weight gain varies from 15% in early teens to 30% in late teens and adult females.[20] Bryden et al. in a longitudinal study observed that diabetic females frequently use insulin omission as a means for weight control, which subsequently resulted in development of microvascular complications in these patients.[21] In another study, it was shown that insulin restriction in females resulted in 3.2-fold increase in mortality over a period of 11 years as compared to patients who administered the prescribed dosage of insulins.[22]
Apart from behavioral issues, T1DM patients are also known to suffer from psychiatric maladies such as anxiety and depression triggered by strict therapy regimen. It is shown that more than 90% of patients on insulin have symptoms of anxiety and phobia.[15] The DAWN survey unveiled that 33% of patients are feared of insulin injections and more than 20% patients have to self-motivate themselves before every injection.[23] Large number of studies has shown a strong linkage between depression and T1DM patients. Depression is reportedly seen to be twice as common in patients with T1DM as in general population.[24,25,26,27] Morbid depression in T1DM patients leading to suicidal ideation has also been investigated. Goldstan et al. observed a 21.0% prevalence of suicidal ideation in T1DM with depressive symptoms. These thoughts were seen to increase to 46.0% during follow-up.[28]
SOCIO-CULTURAL FACTORS AND LACK OF AWARENESS
Lack of awareness and low literacy rates are also responsible for suboptimal management of T1DM. The patients and their caregivers do not completely understand the implications of the disease or are unable to follow proper instructions that have been provided by healthcare workers. The complications arising out of uncontrolled blood glucose level is often neglected at the outset resulting in increased morbidity and mortality. In certain population groups, diabetes is regarded as a curse for past sins and is thus incurable while in some population groups it is treated by home- grown remedies, which lack scientific rationale and testing.
Parents generally do not disclose the disease state of their child to relatives due to a certain degree of stigma attached to T1DM. This is particularly true for the female patients due to marital concerns. The patients avoid going to social gatherings, as they are not comfortable with insulin administration under such circumstances.
Nutrition of the patients is also seen to be compromised, due to fears and misconceptions arising out of lack of knowledge about different aspects of the disease. Parents restrict the exercise and outings of the child due to fear of hypoglycemia.
The young patients spend a significant amount of time daily at school; however, teachers lack the knowledge about the disease and hence do not provide special considerations such as request to use urinals frequently, monitoring of blood glucose or administration of meal-time insulin to these patients.
ECONOMIC CONSTRAINTS
T1DM is a chronic disorder resulting in considerable expenditure on monitoring, therapy or hospitalization secondary to its complications. In SEA countries, there are no sustained or fixed reimbursement policies for its management. GDP spend on health is miniscule resulting in lack of government-aided infrastructure that needs to be significantly improved in these nations. Only private institutions are equipped to manage the disease and associated complications but access to these facilities is restricted due to financial constraints.
There is also a constant requirement for regular monitoring of blood glucose levels and HbA1c. Additionally monitoring of lipid profile, blood pressure, renal indices and fundus examination are also important to observe the effects of T1DM on end organs. The monitoring of these parameters adds to the overall costs of T1DM management.
CHALLENGES IN THE MANAGEMENT OF T1DM: CLINICAL EXPERIENCE FROM SEA
The challenges encountered with T1DM management in SEA region are closely linked to the socio-economic status and prevalent cultural beliefs. These countries with their modest healthcare infrastructure are not fully equipped to handle the intricate issues that are specific to T1DM. Here, we have elucidated the important obstacles operating in India, Sri Lanka, Myanmar, Nepal, Pakistan and Bangladesh. The challenges highlighted are presented as either patient or provider factors. This is followed by some suggestions, which may serve as a broad guidance to resolve the stated issues.
BANGLADESH
Patient factors
Lack of awareness about the disease and its treatment requirements is the biggest obstacle faced in T1DM management in Bangladesh. Majority of the type 1 patients are poor and require massive financial support for treatment. Patients do not disclose the T1DM condition because of certain degree of stigma attached with the disease. School authorities and employer are unaware about the patient's condition, and therefore is unable to contribute in certain situations that the patients may face difficulties themselves at school or workplace. In case of female patients, it is considered as an extra burden and hence the treatment is started late. They are forced into early marriages and subsequent pregnancy, which can have devastating effect on their health.
Provider factors
There is a dearth of trained personnel to handle T1DM. Similar to other countries from the region, PCPs are reluctant to start insulin due to the perceived complexity of insulin therapy. Although, the government tries to provide financial support for the management but with the rising costs, it is increasingly becoming difficult.
INDIA
Although, more than 95% cases in India are of T2DM, but due to large population base, the absolute number of T1DM patients is significant. On an average, the age of onset of T1DM is 5-7 years, which is an important period of life for mental and social development. The child is trying to get acclimatized to the rigorous routine and schedule of school life while the young parents are also struggling to establish themselves in their professional careers. The strict monitoring and treatment regimen of T1DM requires considerable changes in the lifestyle of parents and the young patients.
Patient factors
Insulin-based regimens require frequent daily glucose monitoring and insulin administration through either MDI or insulin pump. However, less than 0.5% patients follow this management plan. The young patients while coping with stringent treatment are also expected to compete with their peers both academically and in co-curricular activities. They start the day early, often skip breakfast and frequently enroll in private tuitions after school. This hectic schedule results in wide fluctuations and practically leaves no time for monitoring of underlying blood glucose. The support from school authorities is also not forthcoming, as the child has to monitor the sugar and self-inject insulin prior to the lunch. Their frequent request to visit the urinal is not always permitted. The patients, due to parental pressure participate in co-curricular activities like dancing, swimming and other similar high-energy consuming sports, which put extra burden to the delicately poised underlying homeostasis. Suitable dietary plan that balances the calorie need and blood glucose are not followed and patients are discouraged to do even mild exercises that may be helpful.
Marriage is a source of stress to the patient and his/her family as they face a major challenge to find a suitable partner. This is specifically true for female patients where the disease status is concealed from the spouse and his family. There have been instances of the newly married girl suffering from diabetic acidosis and associated complications due to skipping of insulin.
There are other behavioral issues, which impede the successful management of T1DM. Patients do not comply with SMBG in spite of being provided with free glucometers and test strips. Prescribed regimen is not adhered because of factors related to costs, lack of awareness, fear of side effects such as weight gain/hypoglycemia. The patients tend to conceal the disease status due to employment related factors.
Provider factors
This is frequently the first point of contact in the management of T1DM. However, they are not very confident in initiating insulin due to lack of knowledge about the guidelines and complex insulin regimens. Many a time, type 1 patients are on biphasic insulin twice daily. They are continued on sub-optimal doses of insulin, which does not cause hypoglycemia or diabetic ketoacidosis, but also fails to maintain the blood glucose to accepted levels resulting in gradual development of vascular complications of diabetes, which limits their life expectancy considerably. The patients are not routinely screened for long-term complications of diabetes such as regular BP monitoring, fundus examination and lipid panel monitoring. Although, the private centers are equipped to provide a comprehensive diabetes care, due to cost factors, not many patients can afford to avail their facilities. Government infrastructure is not robust enough to provide end-to-end T1DM care.
MYANMAR
In Myanmar, prevalence of diabetes exceeds 10%. Although the accurate numbers for T1DM separately is not available, according to the estimates of the practicing physicians, T1DM account for approximately 5% cases of diabetes. With the latest population figures projected at 60 million, the total T1DM patient pool becomes sizeable for a small country like Myanmar.
Patient factors
The awareness about the disease process and its long-term effects remain low in the general population. The patients do not readily accept the insulin therapy because of the cost of monitoring and therapy, restricted availability of the insulin, electricity, requirement of refrigeration for its storage and fear of hypoglycemia and weight gain. Similar to other countries, the disease status is not revealed due to marital concerns and employment prospects. Teachers at school are not aware about the child's disease and therefore cannot be expected to co-operate.
Provider factors
As opposed to T2DM, the diagnosis of T1DM is based on HLA typing, C-peptide measurement presence of molecular markers and autoantibodies. However, specialized laboratories providing these facilities are not widely available. The treating physicians frequently initiate the patients on oral glucose lowering drugs (OGLDs), despite knowing that insulin is the mainstay of treatment. This can be attributed to lack knowledge of current treatment guidelines involving insulin-based regimens and apprehension about patient compliance to the therapy. Myanmar as a country has its own administrative and natural divisions. More than two-third of the population base is rural, where healthcare delivery is rudimentary. Due to the lack of trained personnel and availability of modern insulin, patients resort to traditional medicines.
NEPAL
Similar to other SEA countries under consideration, correct disease burden of T1DM is not available.
Patient factors
One of the biggest obstacles in adaptation to insulin-based regimen is lack of proper storage facilities. Refrigerators for preserving insulin are not widely available, and electric supply is erratic and a power failure (load shedding) may go up to 16-18 hrs a day even in the urban areas. Situation is particularly grim in rural areas where patients get discouraged to follow insulin due to these factors. Cost of therapy is another factor, which dissuades patient from regularly administering insulin, which though is provided free till the age of 16, but has to be self-financed later. SMBG is also not followed due to expenses involved. Even when affordable, insulin is avoided due to fear of needles, perceived addiction, life-time dependency and hypoglycemia. Due to lack of awareness, proper nutrition is not provided to the affected child, resulting in development and growth related abnormalities. On the social front, finding a suitable partner becomes a major challenge for the parents and so the disease status is not disclosed. The teachers at school are not fully educated and hence are mostly unaware about the diabetic status of the child due to fear of discrimination and so unable to support the child in issues related to blood glucose monitoring and insulin administration.
Provider factors
PCPs often are the first point of contact for these patients and are not fully equipped to manage this complex and chronic disorder. Pediatricians are primarily associated with the management of T1DM, due to lack of available endocrinologists.
PAKISTAN
Pakistan has a large population with low literacy level and poverty. This makes the management of chronic disorders like T1DM extremely challenging.
The support of the government is insufficient with a 1% share of the Gross Domestic Product allocated for health, where only fraction of which is dedicated for diabetes. The health delivery care is substandard, especially in the rural areas with inadequate Basal Health Units and not all manned by doctors. Poverty can prevent the parents from taking the child to the next city to consult a medical professional, due to not being able to bear travel expenses. Specialized care is largely confined to urban areas and managed by private centers with limited population accessibility due to financial constraints.
Patient factors
There is a widespread lack of awareness among the patient population and their care providers. T1DM is regarded as a punishment for past sins of the parents or as an effect of an evil eye and so there is poor social support. Parents often turn to traditional healers, who prescribe measures and local medications, which have no scientific backing and many parents are forced to believe that a miracle cure will come for their child one day. As there is an evident lack of support group, the type 1 patients may find it extremely difficult to be selected for a job.
The low acceptability of insulin is also related to affordability of insulin-based regimens, as the requisite equipments are mainly imported from other countries. Schools do not have special provisions for the patients and prevent them from participating in active sports. Due to lack of knowledge and training of the teachers, a child can be denied emergency treatment as for hypoglycemia during school hours. This at times can prove to be dangerous.
Social issues are many; marriage again is a major hurdle, specifically for female patients. There is a strong belief that girls with T1DM would not be able to conceive or have a normal pregnancy. They would not be able to carry out the routine household chores and would be an added financial burden due the cost of insulin, monitoring and visits to the doctor.
Provider factors
PCPs are not keen to initiate insulin because of lack of knowledge about the complex insulin based therapy and insufficient time that has be devoted to an individual patient.
Lack of continued medical education facilities especially in smaller cities and rural areas, takes away the confidence of the general practitioner to prescribe insulin and monitor the results. This can deny a child with T1DM, the benefits of a good glycemic control.
SRI LANKA
The correct epidemiological data from Sri Lanka is not available. However, unverified estimates based on clinical evidence and experience states T1DM prevalence between 1-2%.
Patient factors
Insulin therapy and accompanied monitoring requirements are considered as non-essential measures. This lack of awareness amongst the patients makes insulin acceptance and compliance unsatisfactory. The patients are denied the required diet comprising of specific nutrients because of misconceptions about the disease. Moderate exercise helps in keeping blood glucose under check, but this is not encouraged by the family members due to fear of developing hypoglycemia. Likewise, the patients are not allowed to participate in routine physical activities and games at schools. Teachers at school do not co-operate fully when the patient is required to perform a blood glucose monitoring or administer insulin. The patients do not reveal the disease condition to employers because of the perception that T1DM patients cannot withstand the pressures of full-time job. Significant challenges are faced in marrying off the patients resulting in concealment of disease to prospective partners and their families.
Provider factors
T1DM is sometimes diagnosed late because the signs and symptoms may be masked by accompanied infections such as malaria, typhoid and other infectious diseases. This results in either misdiagnosis or delayed diagnosis, which can have potentially serious consequences. The patient and provider factors influencing T1D management in SEA Countries are listed in Figure 1.
Figure 1.
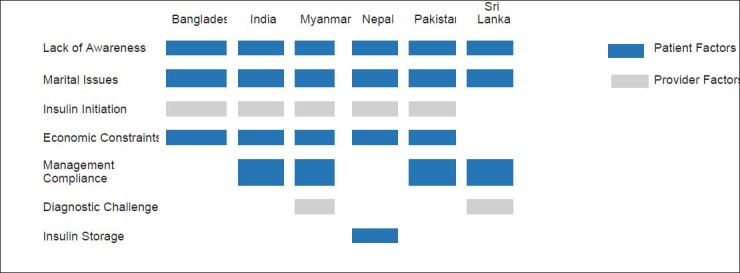
Patient and provider factors influencing T1D management in SEA Countries
Suggested corrective measures for issues and challenges seen in T1DM
Issues like delayed or suboptimal initiation of insulin therapy by PCPs can be overcome by placing special emphasis on clinical orientation in medical school curriculum towards insulin-based management of type 1 diabetes. Forums and platforms for continued medical education and regular interaction among PCPs, endocrinologists and diabetologists should be encouraged. Specific workshops on comprehensive diabetes care and insulin treatment including insulin pumps should be held periodically. Comprehensive type 1 diabetes program algorithm that stress on updated management, incorporating some of the common concepts, which doctors should ideally follow such as basal bolus therapy, insulin pump therapy, glucose-monitoring techniques,[29] mandatory vaccinations,[30] Continuous Glucose Monitoring etc., may be formulated.
Compliance to the different aspects of T1DM can be improved by placing thrust on self-management education programs. The treating physician can identify patients who are prone to non-adherence to prescribed therapy. A brief counseling of these patients by the physician will help in improving the treatment compliance.
Hypoglycemic episodes can be reduced by ensuring that patients clearly understand the hypoglycemic symptoms. They should be instructed to self-monitor the blood glucose in the wake of symptoms and take remedial measure in instances of low blood glucose readings. Insulin dosing should be titrated or the regimen should be altered in consultation with the physician when hypoglycemic events become more frequent.
T1DM being a life-long disease, requires constant support and motivation so that patient can meet the challenges of the disease and strict treatment and monitoring regimen. Periodic counseling by trained psychologist is required, which can ease the psychological burden associated with chronic diseases. The family and the treating physician should understand that T1DM and adolescence are two complex issues and closely linked and complicated by one another. The misconceptions about insulin therapy should be removed. Parents of adolescent patients should be sensitized towards the mood changes that these patients might be susceptible to.
To counteract the challenges arising out of lack of awareness, special programs targeting the patients and their close relatives should be designed to promote understanding about T1DM. They should be specifically educated about the importance of maintaining the glycemic control in preventing the dreaded long-term complications of retinopathy, nephropathy and neuropathy.
Governmental agencies should specifically focus on this dreaded disease and increase the resource allocation. Special diabetic clinics with adequate trained staff including laboratory facilities should be opened in remote areas to cater to the rural T1DM population pool. The rising incidence of diabetes is a challenge and the support by non-governmental agencies is also imperative. The Insulin Bank of the Diabetes Association of Sri Lanka provides a total care package free of charge to 578 needy Type I Children and Young Adults. Diabetic Association of Bangladesh currently provides care free of cost to poor patients. Life for A Child (LFAC) and Changing Diabetes in Children (CDIC) are also in the forefront to lighten the burden by providing support to 3000 children.
CONCLUSION
Management of T1DM requires a strong commitment from the patients, their family, treating physicians and government bodies. SEA harbors a significant percentage of T1DM cases; however, its management in these countries is suboptimal. On the therapeutic front, there has been a considerable progress with the introduction of safer and flexible insulin regimens, but this has not translated into improved patient outcomes. The problem is more acute in SEA because of the local factors that restrict the timely initiation of insulin. Factors such as lack of comprehensive awareness about the disease in the patient population and fear of multiple daily insulin injections and associated side effects have led to limited acceptance by patients and prescription by physicians. The socio-economic status of these countries also does not sometimes permit required insulin therapy and the related blood glucose monitoring. To overcome these factors, it is therefore imperative to spread awareness about the disease and strengthening the government healthcare infrastructure.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.van Belle TL, Coppieters KT, von Herrath MG. Type 1 diabetes: Etiology, immunology, and therapeutic strategies. Physiol Rev. 2011;91:79–118. doi: 10.1152/physrev.00003.2010. [DOI] [PubMed] [Google Scholar]
- 2.IDF 2013 Atlas. Sixth Edition. 2013. [Last cited on 2014 Feb 12]. Available From: http://www.idf.org/sites/default/files/DA6_Regional_factsheets_0.pdf .
- 3.Ramachandran A, Snehalatha C, Ma RC. Diabetes in south-east Asia: An update. Diabetes Res Clin Pract. 2014;103:213–7. doi: 10.1016/j.diabres.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;35(Suppl 1):S64–71. doi: 10.2337/dc12-s064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bajaj S, Jawad F, Islam N, Mahtab H, Bhattarai J, Shrestha D, et al. South Asian women with diabetes: Psychosocial challenges and management: Consensus statement. Indian J Endocrinol Metab. 2013;17:548–62. doi: 10.4103/2230-8210.113720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenbloom AL, Joe JR, Young RS, Winter WE. Emerging epidemic of type 2 diabetes in youth. Diabetes Care. 1999;22:345–54. doi: 10.2337/diacare.22.2.345. [DOI] [PubMed] [Google Scholar]
- 7.Harron KL, Feltbower RG, McKinney PA, Bodansky HJ, Campbell FM, Parslow RC. Rising rates of all types of diabetes in south Asian and non-south Asian children and young people aged 0-29 years in West Yorkshire, U.K., 1991-2006. Diabetes Care. 2011;34:652–4. doi: 10.2337/dc10-1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hayes RP, Fitzgerald JT, Jacober SJ. Primary care physician beliefs about insulin initiation in patients with type 2 diabetes. Int J Clin Pract. 2008;62:860–8. doi: 10.1111/j.1742-1241.2008.01742.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.AADE. AADE7 Self-Care Behaviors. Diabetes Educ. 2008;34:445–9. doi: 10.1177/0145721708316625. [DOI] [PubMed] [Google Scholar]
- 10.Povey RC, Clark-Carter D. Diabetes and healthy eating: A systematic review of the literature. Diabetes Educ. 2007;33:931–59. doi: 10.1177/0145721707308408. [DOI] [PubMed] [Google Scholar]
- 11.Boule NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: A meta-analysis of controlled clinical trials. JAMA. 2001;286:1218–27. doi: 10.1001/jama.286.10.1218. [DOI] [PubMed] [Google Scholar]
- 12.American Diabetes Association. Standards of Medical Care in Diabetes-2009. Diabetes Care. 2009;32(Suppl 1):S13–61. doi: 10.2337/dc09-S013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Odegard PS, Capoccia K. Medication taking and diabetes: A systematic review of the literature. Diabetes Educ. 2007;33:1014–29. doi: 10.1177/0145721707308407. [DOI] [PubMed] [Google Scholar]
- 14.Kotwani A, Ewen M, Dey D, Iyer S, Lakshmi PK, Patel A, et al. Prices and availability of common medicines at six sites in India using a standard methodology. Indian J Med Res. 2007;25:645–54. [PubMed] [Google Scholar]
- 15.Berlin I, Bisserbe JC, Eiber R, Balssa N, Sachon C, Bosquet F, et al. Phobic symptoms, particularly the fear of blood and injury, are associated with poor glycemic control in type I diabetic adults. Diabetes Care. 1997;20:176–8. doi: 10.2337/diacare.20.2.176. [DOI] [PubMed] [Google Scholar]
- 16.Pramming S, Thorsteinsson B, Bendtson I, Binder C. Symptomatic hypoglycaemia in 411 type 1 diabetic patients. Diabet Med. 1991;8:217–22. doi: 10.1111/j.1464-5491.1991.tb01575.x. [DOI] [PubMed] [Google Scholar]
- 17.Gonder-Frederick LA, Fisher CD, Ritterband LM, Cox DJ, Hou L, DasGupta AA, et al. Predictors of fear of hypoglycemia in adolescents with type 1 diabetes and their parents. Pediatr Diabetes. 2006;7:215–22. doi: 10.1111/j.1399-5448.2006.00182.x. [DOI] [PubMed] [Google Scholar]
- 18.Clarke WL. Behavioral challenges in the management of childhood diabetes. J Diabetes Sci Technol. 2011;5:225–8. doi: 10.1177/193229681100500203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wysocki T, Harris MA, Greco P, Bubb J, Danda CE, Harvey LM, et al. Randomized, controlled trial of behavior therapy for families of adolescents with insulin-dependent diabetes mellitus. J Pediatr Psychol. 2000;25:23–33. doi: 10.1093/jpepsy/25.1.23. [DOI] [PubMed] [Google Scholar]
- 20.Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: Prevention and intervention. Curr Opin Pediatr. 2010;22:405–11. doi: 10.1097/MOP.0b013e32833a46a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bryden KS, Neil A, Mayou RA, Peveler RC, Fairburn CG, Dunger DB. Eating habits, body weight, and insulin misuse. A longitudinal study of teenagers and young adults with type 1 diabetes. Diabetes Care. 1999;22:1956–60. doi: 10.2337/diacare.22.12.1956. [DOI] [PubMed] [Google Scholar]
- 22.Goebel-Fabbri AE, Fikkan J, Franko DL, Pearson K, Anderson BJ, Weinger K. Insulin restriction and associated morbidity and mortality in women with type 1 diabetes. Diabetes Care. 2008;31:415–9. doi: 10.2337/dc07-2026. [DOI] [PubMed] [Google Scholar]
- 23.Peyrot M, Rubin RR, Lauritzen T, Skovlund SE, Snoek FJ, Matthews DR, et al. International DAWN Advisory Panel. Resistance to insulin therapy among patients and providers: Results of the cross-national Diabetes Attitudes, Wishes, and Needs (DAWN) study. Diabetes Care. 2005;28:2673–9. doi: 10.2337/diacare.28.11.2673. [DOI] [PubMed] [Google Scholar]
- 24.Pouwer F, Geelhoed-Duijvestijn PH, Tack CJ, Bazelmans E, Beekman AJ, Heine RJ, et al. Prevalence of comorbid depression is high in out-patients with Type 1 or Type 2 diabetes mellitus. Results from three out-patient clinics in the Netherlands. Diabet Med. 2010;27:217–24. doi: 10.1111/j.1464-5491.2009.02903.x. [DOI] [PubMed] [Google Scholar]
- 25.Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. Gen Hosp Psychiatry. 2003;25:246–52. doi: 10.1016/s0163-8343(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 26.Van Tilburg MA, McCaskill CC, Lane JD, Edwards CL, Bethel A, Feinglos MN, et al. Depressed mood is a factor in glycemic control in type 1 diabetes. Psychosom Med. 2001;63:551–5. doi: 10.1097/00006842-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A metaanalysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 28.Goldston DB, Kovacs M, Ho VY, Parrone PL, Stiffler L. Suicidal ideation and suicide attempts among youth with insulin-dependent diabetes mellitus. J Am Acad Child Adolesc Psychiatry. 1994;33:240–6. doi: 10.1097/00004583-199402000-00013. [DOI] [PubMed] [Google Scholar]
- 29.Kesavadev J, Das AK, Unnikrishnan R, 1st, Joshi SR, Ramachandran A, Shamsudeen J, et al. Use of insulin pumps in India: Suggested guidelines based on experience and cultural differences. Diabetes Technol Ther. 2010;12:823–31. doi: 10.1089/dia.2010.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kesavadev J, Misra A, Das AK, Saboo B, Basu D, Thomas N, et al. Suggested use of vaccines in diabetes. Indian J Endocrinol Metab. 2012;16:886–93. doi: 10.4103/2230-8210.102982. [DOI] [PMC free article] [PubMed] [Google Scholar]


