Abstract
Context:
India leads the world with largest number of diabetic patients and is often referred to as the diabetes capital of the world. Diabetic dyslipidemia in India is one of the main cause for Coronary Artery Disease (CAD) mortality. Although diabetes continues to be a major lifestyle condition in India, there is a lack of studies in India on whether dyslipidemia in Indian diabetics is being adequately controlled. Our study provides critical insights into the insights into proportion of diabetes patients achieving lipid goal in India.
Aims:
The primary objective of our study was to assess the control of dyslipidemia in the Indian diabetic population treated with lipid lowering drugs (LLDs), as per American Diabetes Association (ADA) 2010 guidelines.
Settings and Design:
The study was carried out in a real world Indian clinical setting involving 178 sites. This is a multicenter, noninterventional, and cross-sectional observational study.
Materials and Methods:
A total of 5400 adult subjects with established type-2 diabetes mellitus (T2DM) and dyslipidemia were recruited for the study. Patients in the study were on LLD at a stable dose for at least last 3 months before the designated study visit. Routine lipid profile tests were conducted for all patients.
Statistical Analysis Used:
Descriptive statistics was used to analyze qualitative and discrete variables. Chi-square test and t-test were conducted to assess the existence of statistically significant association between the variables.
Results:
A total of 5400 patients with T2DM from 178 centers across India were recruited. Out of the total population, 56.75% (N = 3065) of them were males. Primary end-point of low-density lipoprotein cholesterol (LDL-C) level below ADA 2010 target was achieved in a total of 48.74% (N = 2632) patients. Gender was significantly associated with lipid levels and age was significantly (P < 0.05) correlated with all lipid levels. Control rates of other lipid parameters like high-density lipoprotein cholesterol, triglyceride, and total cholesterol in the study were 60.48% (N = 3236), 57.54% (N = 3107), and 92.24% (N = 4981) respectively. Among those with overt cardiovascular disease (CVD), target LDL-C level of < 70 mg/dL was achieved in 22.87% (70 out of 306) patients. The LDL-C levels of 49.03% (N = 1768) patients who were on statin therapy were within target levels, while 53.46% (N = 634) patients who were on statin and their combinations with other LLDs had their LDL-C levels within the stipulated range.
Conclusions:
This study has reveled that dyslipidemia control in Indian T2DM patients is very poor with almost half of them not reaching their LDL -C goal. Dyslipidemia being one of the main risk factors for CVD in T2DM patients there is a need to treat dyslipidemia aggressively to reduce risk of future CV events.
Keywords: CVD, diabetes, dyslipidemia, LDL
INTRODUCTION
Diabetes mellitus is one of the most common chronic diseases globally and continues to increase in numbers. It is among the top five causes of mortality. The global prevalence of diabetes among adults is estimated to be 6.4%, affecting 285 million people, in 2010, and is expected to increase to 7.7%, affecting 439 million people by 2030. Between 2010 and 2030, it is estimated that there will be a 69% and 20% increase in number of adults with diabetes in developing countries and developed countries, respectively. Diabetes has evolved into an epidemic in India. The estimated number of patients with diabetes in India was 62.4 million in 2011 which is projected to rise to a staggering 101.2 million by 2030.[1,2,3]
Diabetes is considered a coronary heart disease (CHD)- risk equivalent and it is frequently associated with various other cardiovascular (CV) risk factors. It is well-established that dyslipidemia is a major risk factor for macrovascular complications in patients with type-2 diabetes mellitus (T2DM) and affects 10%-73% of this population.[4,5,6,7,8] Approximately, 80% of deaths in patients with diabetes are attributable to cardiovascular disease (CVD). Asian Indians have higher risk of CHD than whites.[9] Dyslipidemia in diabetes commonly manifests as raised low-density lipoprotein cholesterol (LDL-C), decreased high-density lipoprotein cholesterol (HDL-C) levels, or elevated triglyceride (TG) levels. Furthermore, data from the United Kingdom Prospective Diabetes Study suggest that both decreased HDL-C and elevated LDL-C predict CHD in diabetes.[10] All international guidelines recommend aggressive management of lipids in this population[11,12] It is very well-established that reducing LDL-C can reduce CHD events both in primary as well as secondary prevention patients.[13] Thus, lowering LDL-C level is a priority in treating diabetic dyslipidemia.
Although diabetes and dyslipidemia commonly coexist in India, there is a lack of evidence on whether dyslipidemia is adequately managed or not.[14] At present, there is lack of country wide data for meaningful analysis. Therefore, there existed a need to understand the pattern of dyslipidemia and accurately assess the control of lipids in this population in a real world setting. The primary objective of our study was to assess the control of dyslipidemia in the Indian patients with diabetes treated with lipid lowering drugs (LLDs). The secondary objectives were to assess the control of dyslipidemia by age and gender, by use of statin alone or in combination, geographical variations in dyslipidemia management (in the four zones − north, south, west, and east) and to record use of different LLDs.
MATERIALS AND METHODS
The study was conducted as per International Conference on Harmonisation Good Clinical Practice (ICH GCP) guidelines and according to the ethical code of conduct laid out by declaration of Helsinki and Indian Council of Medical Research guidelines. The study was approved by an independent ethics committee. Details about inclusion and exclusion criteria of the study are given in Table 1.
Table 1.
Inclusion and exclusion criteria
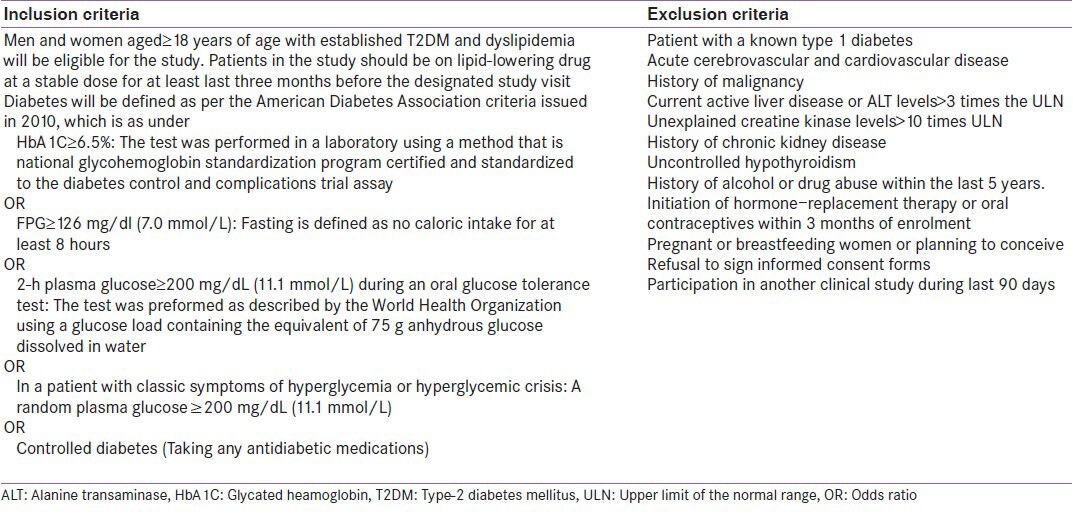
This was a multicenter, noninterventional, cross-sectional observational study. Patients with T2DM who were on stable dose of LLDs at least 3 months prior to study visit were included in the trial. Data from patients, who had signed informed consent, were collected during their first interaction with the doctor.
Statistical analysis
Patients with one or more parameters, that is, TG, HDL-C, LDL-C, or total cholesterol (TC) outside the targets recommended by American Diabetes Association (ADA) 2010 were considered to have dyslipidemia. In our study, overt CVD was defined as previous medical history of having at least one of the following: Myocardial infarction, heart failure, and ischemic or hemorrhagic stroke.
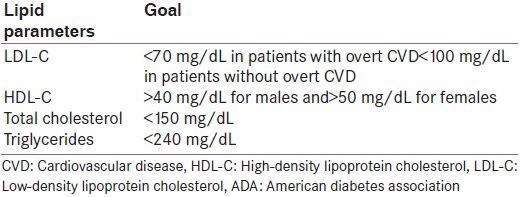
For the current analysis, LDL-C cholesterol < 70 mg/dL (1.8 mmol/L) in the overt CVD groups and < 100 mg/dL in without overt CVD group have been considered as per ADA 2010 guidelines. Details are provided in Table 2.
Table 2.
Lipid goals as per ADA 2010 Guidelines
Control rates of dyslipidemia in T2DM patients were analyzed by age and gender, statins alone or in combination, and across the four zones in India. Statistical hypotheses testing using Chi-square test and likelihood ratio Chi-square test were conducted to assess the existence of statistically significant association between the variables tested. We considered 5% level of significance as statistically significant. Pearson's correlation test was performed to find the correlation between various demographic variables and CV risk factors such as age > 55 years with lipid profiles (i.e. LDL-C, HDL-C, TG, and TC). T-test was performed to test the significance of association between family history of premature CHD, coronary artery disease, cerebrovascular disease, (i.e. ischemic stroke, peripheral vascular disease, carotid artery atherosclerosis, and diabetes mellitus), previous medical history (hypertension, angina, myocardial infarction, heart failure, or ischemic stroke) with lipid profiles (i.e. LDL-C, HDL-C, TG, and TC).
RESULTS
A total of 5400 patients were recruited from 178 sites distributed across country with 40.91% patients recruited from south zone followed by 31.76%, 20.09%, and 7.24% of patients from west zone, north zone, and east zone, respectively. Out of the total population, 56.42% were males and 43.58% were females. The mean age of the study population was 54.03 (±11.57) years and mean (standard deviation, SD) body mass index was 26.81 (±4.46) kg/m2. Out of the total study population, 10.45% were smokers, 8.98% were alcohol consumers, and 12.60% had reported family history of premature CHD. Mean (SD) baseline values for systolic and diastolic blood pressures were 133.05 (14.62) mm Hg and 83.38 (8.85) mm Hg, respectively. High LDL-C (63.09% patients) was found to be the most common reason for initiating LLDs. Angina (7.20%) was the highest reported previous medical history in the study population.
Our study showed that 2632 (48.74%) patients had achieved LDL-C goals as per the ADA 2010 guideline. Similarly, 3266 (60.48%) patients had their HDL-C levels within the target range. Table 3 gives achievement of ADA 2010 goal of lipid parameters in study population.
Table 3.
American diabetes association 2010 goal achievement in study population
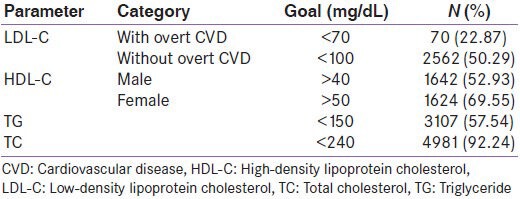
Among those with overt CVD (N = 306), target LDL-C level of < 70 mg/dL was achieved in 13.76% (15 out of 109) of the female patients and in 27.92% (55 out of 197) of the male patients. Among those without overt CVD (N = 5094), target LDL-C level of < 100 mg/dL was achieved in 48.61% (1082 out of 2226) and 51.60% (1480 out of 2868) of the female and male patients, respectively. Chi-square test showed that gender was significantly associated with levels of LDL-C, HDL-C, TG, and TC.
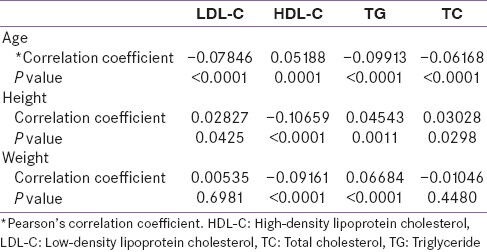
Of the total study population, 49.78% patients were aged ≥ 55 years, followed by 38.93% in the range of 40-54 and 11.30% below 40 years. Pearson's correlations test showed that age was significantly correlated (P ≤ 0.05) with all lipid profile parameters. Table 4 gives details about correlation of various demographic variables with lipid parameters. P value of less than 0.05 indicates statistically significant correlation between two variables.
Table 4.
Correlation of various demographic variables with lipid parameters
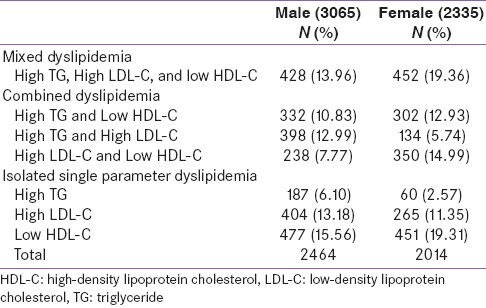
As shown in Table 5, the most common pattern among males was isolated single parameter dyslipidemia with low HDL-C, followed by mixed dyslipidemia. Almost the same pattern was observed among the female population as well; however, slightly higher occurrence of mixed dyslipidemia was seen. Control rates of dyslipidemia with all four parameters (LDL-C, HDL-C, TG, and TC) at goal were 5.98% overall with no major difference in zonewise data − North (5.16%), South (5.17%), West (7.0%), and East (6.14%).
Table 5.
Pattern of dyslipidemia
Out of the total 5400 study patients for whom data on LLDs was available 75.25% (N = 3606) were prescribed statin alone and 24.75% (N = 1186) were on combination of statin with other LLDs drugs. The LDL-C levels of 49.03% (N = 1768) patients who were on statin therapy were within target levels, while 53.46% (N = 634) patients who were on statin and their combinations with other LLDs had their LDL-C levels within the stipulated range. Similarly control rates of all the lipid parameters (LDL-C, HDL-C, TG, and TC) was 6.26% and 5.73% in those who were on statin alone and those who were on statin and their combination with other LLDs, respectively. Control rates of each key lipid parameter in the four different zones are shown in Figure 1 along with the percentage of patients at goal for all four lipid parameters combined.
Figure 1.
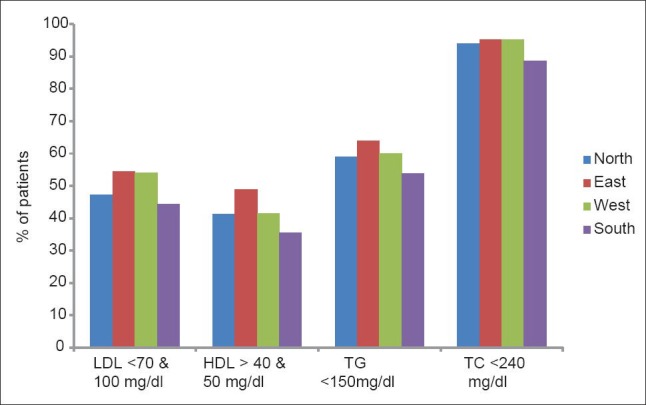
Zone-wise control rate of different lipid parameters American Diabetes Association 2010 lipid goals: Low-density lipoprotein cholesterol (LDL-C) <70 mg/dL in With overt cardiovascular disease and <100 mg/dL without overt patients; High-density lipoprotein cholesterol (HDL-C) ≥40 mg/dL in males and ≥50 mg/dL in females patients; triglyceride (TG) <150 mg/dL; total cholesterol (TC) <240 mg/dL
Top four molecules used in the study were atorvastatin (52.70%), rosuvastatin (28.99%), combination of atorvastatin and fenofibrate (8.41%), and rosuvastatin and fenofibrate (2.86%).
DISCUSSION
Our research reveals critical information on the control rates of dyslipidemia in Indian diabetic population. We believe this study provides significant data, taking into consideration the scale and nationwide sample pool of patients. Our study shows that 48.74% of the patients had their LDL-C levels within the target range. These results are comparable to the data from Kennady et al.,[15] who found that 45% of those with diabetic dyslipidemia are at LDL-C goal. Similarly, Jayaram et al., have recently shown that 43.91% patients achieved LDL-C goal, in a study from India.[15]
In our cohort control of LDL-C was worst in those with overt CVD with only 22.87% of them reaching LDL-C goal, whereas Kennady et al.,[15] demonstrated that a slightly lower proportion (only 15%) of the high-risk study population reached LDL-C level < 70 mg/dL. We found that LDL-C goal achievement was similar in those on statin alone compared with those on combinations of LLDs. Both age and gender were found to be associated with control of all lipid parameters. We observed that lipid control rates went down with increasing age.
Control of other lipid parameters was also inadequate in our study population with less than 40% and 60% of the patients reaching HDL-C and TG goals, respectively. Combined dyslipidemia was the most common dyslipidemia pattern observed in our study and this accounted for a third of the study population. Jayaram et al.,[16] in a single center study in about 800 patients reported that 44.2% males and 42.97% females had combined dyslipidemia. The control rates for dyslipidemia when all the four lipid parameters are considered together, showed a grim picture with approximately 6% of the total population achieving goals. There was no significant difference between control rates of lipid levels across the four zones in India.
Moreover, the study reveals that patients with diabetes and overt CVD are not achieving guideline recommended target LDL-C levels. Considering the rising prevalence and changing epidemiology of both diabetes and CVD and the higher likelihood of their coexistence in India, this data provide important insights on control of dyslipidemia in this vulnerable population. Therefore, this calls for immediate attention by the medical community to resort to a more aggressive approach to manage dyslipidemia, especially in those with diabetes and overt CVD.
Based on the study results, it is clear that aggressive dyslipidemia management is the need of the hour in patients with diabetes. We hope our study will pave the way for future research in this area and also help the medical fraternity in consciously taking measures to address these burning issues.
We must admit that this research has some limitations. Due to the real world setting of the study, some of the key challenges were in terms of lack of proper medical screening, high dependency on patient reported medical history, and availability of laboratory reports. Though a controlled clinical trial would have helped address these challenges, as our aim was to obtain real world Indian data in a cross-sectional setting, we opted for this study design. While we acknowledge the limitations of the study, we believe the data are valuable given the high magnitude of diabetic dyslipidemia in the country. Further research is needed to gather more information and insights.
We conclude that over half of patients with diabetic dyslipidemia are not achieving the LDL-C goal as defined in the ADA 2010 guidelines despite being on treatment with LLDs. Moreover, overall control rate of dyslipidemia is alarmingly low. Though this data provide important insights on the subject, there is need to generate more local Indian data in this area.
ACKNOWLEDGMENTS
We thank Dr. Shiva Patil and Amit Kumar for their contribution in execution of the study. We also acknowledge BioQuest Solutions for their services in data management and manuscript writing. We would like to also thanks all principal investigators of SOLID: A non-interventional, cross sectional, observational study on the management of dyslipidemia in adult Type 2 diabetes mellitus patients in India. Study Investigator's list-, Andhra Pradesh: Jayaraju B, Padmavathi Devi C, Tirupathi Rao DC, Girisesh G, Haricharan G, Camoens L, Manju Bhargavi M, Papa Rao N, Sudhakar Reddy P, Usha Bala P, Deb P, Rama Reddy S, Venkateshwarlu S, and Chandrasekhar V. Delhi: Manchanda AK, Ajmani AK, Gupta AK, Grover A, Siddiqui AA, Katyal A, Kohli GS, Sawhney GS, Kumar G, Mahar MS, Kawatra P, Lalwani RK, Marya RK, Sinha RSK, Bansal R, Gupta R, Gogia R, Gupta R, Gupta R, Rastogi SS, Kalra SP, and Sabharwal V. Gujarat: Parekh AM, Mehta A, Saboo B, Trivedi BK, Joshi CP, Patel DC, Mankad H, Shah J, Prajapati J, Bhatt JL, Shah KR, Sharma K, Tibrewala KD, Shah KR, Singhavi M, Vithalani M, Shah N, Yajnik NV, Kurmi PH, Desai P, Shah RB, Mehta SP, Phatak SR, Shah SJ, Marwah T, Dhruv U, Abichandani VK, and Bharsar V. Karnataka: Baliga BG, Ramesh D, Changkakoti DD, Siddappa MD H, Pai KNN, Sreenivasa Murthy L, Satyanarayana PK, Ranganath S, and Javaz SAA. Kerala: Kannampilly JJ, Koya MA, Moideen MA, Sunil NS, Ramachandra Menon PK, Zacharia PS, Mohamed R, Krishna Kumar S, Rasheed SA, Sadakkathulla, Chandran S, Sulaiman SC, Shijoy MN, Menon SK, Ummer Koya T, Ramaswamy TS, Thankachan T, Anand Kumar V, Jayapal V, Abdul Jaleel V, Haridas VM, and Chemmanam V. Madhya Pradesh: Sharma MK, and Sharma N. Maharashtra: Mutha A, Joshi AS, Harshe BB, Punatar D, Shah D, Damle G, Thacker H, Shah K, Samudra K, Joshi PK, Sanghavi P, Kulkarni RB, Dargad RR, Bakshi S, Kolke SS, Phadke UK, and Kadam Y. Pondicherry: Gopinath S. Punjab: Singh N, Goyal R. Rajasthan: Sharma SK, Jain VK. Tamil Nadu: Sethuraman A, Franklin Joseph A, Panneer Selvam A, Bosco B, Pandian B, Periyandavar I, Krishnan J, Srinivas K, Meenakshi Sundaram L, Chellamariappan M, Deepak MC, Prasad NS, Dharmarajan P, Selva Pandian P, Srinivasan R, Murthy S, Ram Mohan Rau U, Jinadas V, and Sundaram V. Uttar Pradesh: Awasthi AK, Rai A, Parti A, Taneja AK, Johri A, Singh BK, Sinha DK, Mohan M, Rastogi P, Goel P, Yakhmi R, Awasthi R, Shukla R, Gupta S, and Jain S. West Bengal: Ojha AK, Roy D, Das KK, Paul K, Chakraborty K, Guha MK, Mukhopadhyay MK, Bhansali ML, Chakravarty N, Chatterjee P, Joshi LR, Saraogi RK, Mukharjee S, Mandal S, Godbole S, Kothari SK, Satpathy SC, Bhattacharya S, Chattopadhyay TK, and Rahman T.
We are indebted to Dr Sanjay Kalra for reviewing manuscript and providing valuable suggestions.
Footnotes
Source of Support: This study was supported by Astra Zeneca
Conflict of Interest: None declared.
REFERENCES
- 1.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 2.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. ICMR–INDIAB Collaborative Study Group. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-India Diabetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 4.Taskinen MR. Strategies for the management of diabetic dyslipidemia. Drugs. 1999;58:47–51. doi: 10.2165/00003495-199958001-00011. [DOI] [PubMed] [Google Scholar]
- 5.Turner RC, Millns H, Neil HA, Stratton IM, Manley SE, Matthews DR, et al. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23) BMJ. 1998;316:823–8. doi: 10.1136/bmj.316.7134.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farmer JA. Diabetic dyslipidemia and atherosclerosis: Evidence from clinical trials. Curr Diab Rep. 2008;8:71–7. doi: 10.1007/s11892-008-0013-2. [DOI] [PubMed] [Google Scholar]
- 7.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291:335–42. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 8.Mukhopadhyay J, Kanjilal S, Biswas M. Diabetic dyslipidemia-priorities and targets in India. [Last accessed on 2013 Aug 23];Medicine Update. 2010 20 Available from: http://www.apiindia.org/content_mu_2010.html . [Google Scholar]
- 9.O’Keefe JH, Jr, Miles JM, Harris WH, Moe RM, McCallister BD. Improving the adverse cardiovascular prognosis of Type 2 diabetes. Mayo Clin Proc. 1999;74:171–80. doi: 10.4065/74.2.171. [DOI] [PubMed] [Google Scholar]
- 10.Ethnicity and cardiovascular disease. The incidence of myocardial infarction in white, South Asian, and Afro-Caribbean patients with type 2 diabetes (U.K. Prospective Diabetes Study 32) Diabetes Care. 1998;21:1271–7. doi: 10.2337/diacare.21.8.1271. [DOI] [PubMed] [Google Scholar]
- 11.American Diabetes Association. Standards of medical care in diabetes-2009. Diabetes Care. 2009;32(Suppl 1):S13–61. doi: 10.2337/dc09-S013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brunzell JD, Davidson M, Furberg CD, Goldberg RB, Howard BV, Stein JH, et al. American Diabetes Association, American College of Cardiology Foundation. Lipoprotein management in patients with cardiometabolic risk: Consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care. 2008;31:811–22. doi: 10.2337/dc08-9018. [DOI] [PubMed] [Google Scholar]
- 13.Rosenson RS. Statins: Can the new generation make an impression? Expert Opin Emerg Drugs. 2004;9:269–79. doi: 10.1517/14728214.9.2.269. [DOI] [PubMed] [Google Scholar]
- 14.American Diabetes Association. Standards of Medical Care in Diabetes-2010. Diabetes Care. 2010;33(Suppl 1):S11–61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kennady AG, MacLean CD, Littenberg B, Ades PA, Pinckney RG. The challenge of achieving national cholesterol goals in patients with diabetes. Diabetes Care. 2005;28:1029–34. doi: 10.2337/diacare.28.5.1029. [DOI] [PubMed] [Google Scholar]
- 16.Jayarama N, Reddy M, Lakshmaiah V. Prevalence and pattern of dyslipidemia in type 2 diabetes mellitus patients in a rural tertiary care centre, southern India. Glob J Med Public Health. 2012;1:24–8. [Google Scholar]


