Abstract
Background:
Obesity has become a worldwide epidemic and its prevalence continues to increase at a rapid rate in various populations and across all age-group. The effect of meal skipping, both behaviorally and physiologically, may have an impact on the outcome of weight-loss efforts.
Aims and Objectives:
Therefore, the aim of this study was to examine the prevalence of breakfast skipping and obesity in subjects.
Materials and Methods:
A retrospective analysis of the patients visited to a metabolic clinic of the city was done.
Results:
One hundred and eighty-six eligible subjects were included for the study. A questionnaire was used for data collection which included information regarding dietary factors and exercise schedule/physical activity. A 24-hour dietary recall method was used to assess the amount of food consumed. Anthropometric measurements were taken.
Conclusion:
The higher prevalence of overweight and obesity in the present study could be because of imbalance in the diet and faulty food habits prevalent in the region.
Keywords: Breakfast skipping, health status, obesity
INTRODUCTION
Obesity has become a worldwide epidemic and its prevalence continues to increase at a rapid rate in various populations and across all age-group.[1,2,3,4]
Obesity is a complex metabolic disorder that is thought to result from an imbalance of energy intake and energy expenditure leading to the excess accumulation of fat in various adipose tissues and organs.
Obesity as a risk factor of several major health problems including hypertension, diabetes, heart diseases, certain cancers, and other chronic diseases.[5,6] Thus, finding the factors contributing to obesity is of utmost importance.
The dramatic increase in the occurrence of overweight and obesity over the past several decades is attributed in part to changes in dietary and lifestyle habits, such as rapidly changing diets, increased availability of high-energy foods, and reduced physical activity of peoples in both developed and developing countries.[7]
The effect of meal skipping, both behaviorally and physiologically, may have an impact on the outcome of weight-loss efforts. Daily meal frequencies, and breakfast skipping in particular, have been linked to risk for overweight and obesity in UK, USA, and Australian populations, and are associated with female gender, lower socioeconomic status (SES), urban environments, and older age.[8,9,10] Cross-sectional and longitudinal studies have shown that regularly skipping breakfast is associated with greater body mass index (BMI) in all age-groups;[11,12,13,14,15,16,17] However, the mechanisms that might explain the relation between breakfast consumption and body weight are not yet well understood.[18] However, it remains unclear whether breakfast skipping plays a causal role in overweight or is associated with other factors impacting BMI such as parental involvement in food decisions.[19]
Physical activity is a component of energy balance that is particularly important in the pathogenesis of obesity and in its treatment. The components of energy expenditure are resting (basal)-energy expenditure (REE), diet-induced thermo genesis, and physical activity.[20] Preventive or therapeutic strategies to control obesity should target these abnormalities.
We could identify no published studies that examine the prevalence of breakfast skipping and its correlation with obesity in central part of India.
Therefore, the aims of this study were (1) to examine the prevalence of breakfast skipping and obesity in subjects and (2) too evaluate the hypothesis that breakfast skipping would be cross-sectionally associated with elevated odds for obesity in this sample.
MATERIALS AND METHODS
A retrospective analysis of the patients visited to a metabolic clinic of the city during a 3 month's period was done. A total of 250 patients were visited to the clinic and out of them 186 were eligible to be included. Exclusion criteria included patients on steroids or immunosuppressive drugs on past, patients with any infection, patients who were pregnant, patients with diabetes mellitus and hypothyroidism.
A predesigned questionnaire was used for data collection. The questionnaire included information regarding dietary factors and exercise schedule/physical activity. A 24-hour dietary recall method was used to assess the amount of food consumed. Standing height and weight were measured with the subjects in light clothes without shoes and BMI (kg/m2) was calculated. It was derived by dividing weight in kilogram by square of height in meters.[21] The classification of obesity was done on the basis of recommendations by World Health Organization (WHO).[22]
Breakfast skipping
Definitions of breakfast skipping vary widely across studies and feature differential methodological costs and benefits. These inconsistencies present a challenge when evaluating and comparing studies as it has been shown that whether or not an association exists between breakfast skipping and BMI can potentially depend on how breakfast skipping is defined. For example, breakfast skipping assessed on a dietary survey day may accurately represent point prevalence but not reflect seasonal or other fluctuation in dietary habits over time. Other studies assessing breakfast skipping on a specific number of days per week or other defined time period may better capture such fluctuations but are susceptible to recall biases. Lastly, studies assessing the construct in more qualitative terms34 capture participants’ self-perceptions as breakfast skippers, which may or may not accurately correspond to actual meal consumption frequency.
Statistics was done using statistical package for the social sciences (SPSS) 21.0. All the values were expressed as mean ± standard deviation (SD), percentage, Chi-square test and z test. Statistical significance was considered to be present when the two-tailed probability was less than 0.05.
RESULTS AND DISCUSSION
Table 1 shows the classification of adults according to body mass index (BMI).
Table 1.
Classification of adults according to body mass index
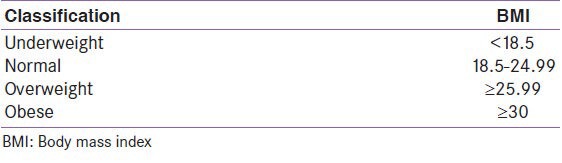
Table 2 shows the prevalence of obesity was found to be 58.6% in the study population at the confidence interval of 51.52–65.68. [Figure 1]
Table 2.
Distribution of study subjects according to weight status
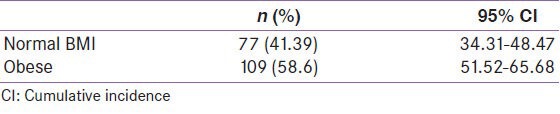
Figure 1.
Percentage prevalence of the study subjects according to body mass index (BMI)
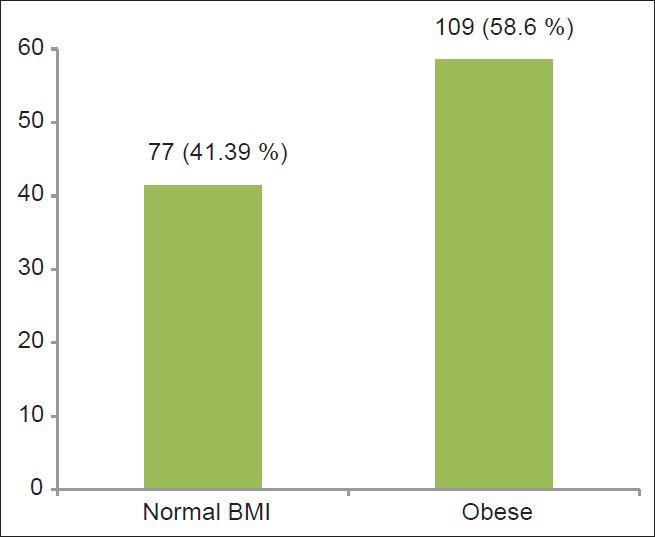
In the present study, normal BMI patients mean age was 48.96 ± 9.6 where as obese had 43.8 ± 7.7 years. [Table 3 and Figure 2]
Table 3.
Clinical status of normal weight and obese patients
Figure 2.
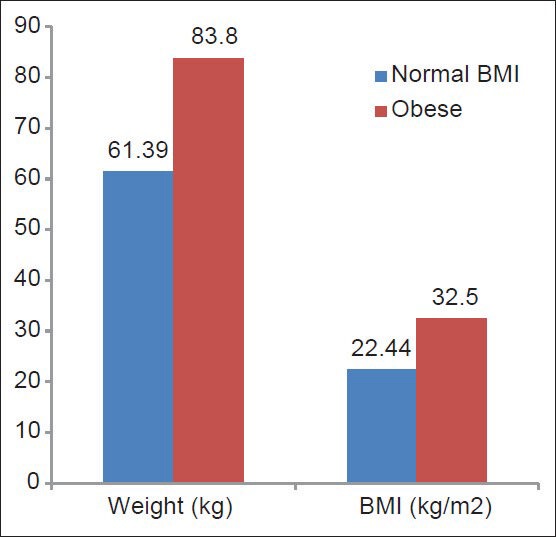
Mean weight and body mass index (BMI) of the subjects
Table 4 shows the general breakfast consumption status of participants; about 132 (71%) patients reported that they don’t consume breakfast regularly. Out of these 84 (63.6%) falls in obese group and 48 (36.3%) falls in normal BMI group.
Table 4.
Breakfast habits of study population
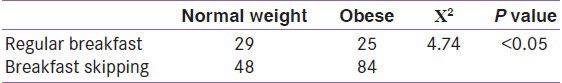
A BMI-specific multivariate analysis was used to determine the relationship between breakfast consumption practices and body weight profile. In both groups, frequent breakfast eaters had significantly lower levels of BMI (X2 = 4.74, P = < 0.05) compared to those of infrequent breakfast eaters.
Table 5 shows the exercise routine of the participants; about 95 (51%) patients reported that they don’t exercise regularly. Out of these, 78 (72%) are obese (X2 = 4.21, P = < 0.01)
Table 5.
Exercise schedule of study population
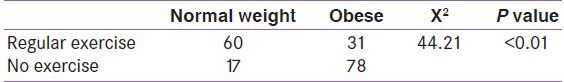
Table 6 shows the prevalence of obesity was higher in the females than males. The difference was statistically significant (X2 = 14.46, P < 0.01) [Table 7].
Table 6.
Classification of study population as per gender
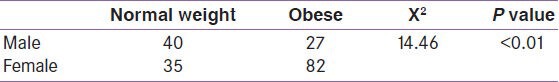
Table 7.
Weight status of study subjects according to oil and protein consumption
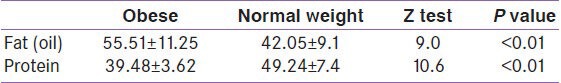
On observing the effect of dietary factors, it was found that the prevalence of overweight and obesity was higher among those who consumed more than recommended amount of fat (oil) than those who were taking recommended or less amount of fat (oil). The difference was found to be statistically significant (z = 9.0, P < 0.01). Whereas the protein consumption was also significantly associated with the obesity (z = 10.6, P < 0.01)
DISCUSSION
The higher prevalence of overweight and obesity in the present study could be because of imbalance in the diet and faulty food habits prevalent in the region.
Gender is one of the biological factors affecting the weight status. It was observed in the present study that the prevalence of overweight is generally higher in females than males. Finding of studies conducted in India by Gopinath et al., Gopalan, Mohan et al., Mishra et al., Ramchandran et al., Reddy et al., Shukla et al., revealed a much higher percentage for obesity/overweight in females that in males. In females, extra energy gets converted into fat. This pattern of energy usage, or “nutrient partitioning,” in females contributes to further positive energy balance and fat deposition. Due effort should be undertaken to decrease overweight or obesity in females to make an impact on overall prevalence.
We lack a strong scientific basis for answering the question of how much physical activity is required to prevent weight gain in the population. There is a lack of prospective, randomized trials that address the question of how much, what type, what intensity, and what duration of physical activity are required to prevent weight gain. Furthermore, the amount of physical activity required to prevent weight gain may differ in different populations and may differ at different times during the life span.
Dietary energy intake is one end of the energy balance equation. The intake of calories more than our body requirement leads to positive energy balance and so obesity. This fact was confirmed in the present study. It was found that the prevalence of overweight was higher among those who consumed more than recommended calories than those who were taking recommended or fewer calories per day. The difference was found to be statistically significant.
Among other factors in dietary consumption, the skipping of breakfast impacted overweight positively while eating habits either vegetarian or both (vegetarian and non vegetarian) did not affect the weight status of subjects significantly.
The average intake of fat and protein by the study subjects was quite less than the recommended intake of these food items. Also, there was a difference in the amount of consumption of these foods in overweight and normal weight groups. The amount of fat (oil) intake was more among overweight than normal weight subjects and mean intake of protein was less among the overweight subjects than their normal weight counterparts. Thus, there was positive association between fat (oil) intake and overweight status and a negative association between protein intake and overweight status which was statistically significant. Similar findings were observed in the study of National Foundation of India (1998) which indicated that the consumption of refined oil and saturated fats (ghee and vanaspati) was significantly higher among the obese individuals (P < 0.05) [Figure 3].
Figure 3.
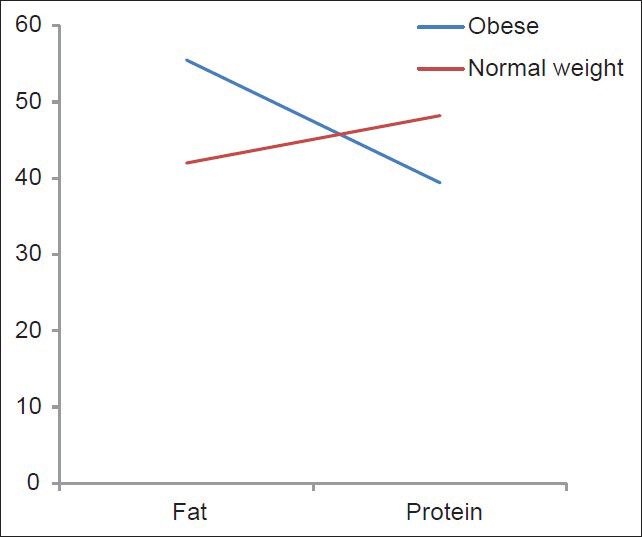
Protein and fat consumption of the subjects
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Geneva: WHO; 2003. WHO. Joint WHO/FAO Expert Consultation on diet, nutrition and the prevention of chronic diseases: Report of a joint WHO/FAO expert consultation. [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2007;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Monteiro C, Popkin BM. Trends of overweight in children and adolescents in the United states, Brazil, China, and Russia. Am J Clin Nutr. 2002;75:971–7. doi: 10.1093/ajcn/75.6.971. [DOI] [PubMed] [Google Scholar]
- 5.Bray GA, Bellanger T. Epidemiology, trends, and morbidities of obesity and the metabolic syndrome. Endocrine. 2006;29:109–17. doi: 10.1385/ENDO:29:1:109. [DOI] [PubMed] [Google Scholar]
- 6.Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. American Heart Association, Obesity Committee of the Council on Nutrition, Physical Activity, Metabolism, Obesity, and Cardiovascular Disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 7.Popkin BM. The nutrition transition and its health implications in lower income countries. Public Health Nutr. 1988;1:5–21. doi: 10.1079/phn19980004. [DOI] [PubMed] [Google Scholar]
- 8.Siega-Riz AM, Popkin BA, Carson T. Trends in breakfast consumption for children in the United States from 1965 to 1991. Am J Clin Nutr. 1998;67:748S–56. doi: 10.1093/ajcn/67.4.748S. [DOI] [PubMed] [Google Scholar]
- 9.Delva J, O’Maley PM, Johnston LD. Racial/ethnic and socioeconomic status differences in overweight and health-related behaviours among American students: National trends 1986-2003. J Adolesc Health. 2006;39:536–45. doi: 10.1016/j.jadohealth.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 10.Utter J, Scragg R, Mhurchu CN, Schaaf D. At-home breakfast consumption among New Zealand children: Associations with body mass index and related nutrition behaviors. J Am Diet Assoc. 2007;107:570–6. doi: 10.1016/j.jada.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 11.Ma Y, Bertone ER, Stanek EJ, 3rd, Reed GW, Hebert JR, Cohen NL, et al. Association between eating patterns and obesity in a free-living US adult population. Am J Epidemiol. 2003;158:85–92. doi: 10.1093/aje/kwg117. [DOI] [PubMed] [Google Scholar]
- 12.Song WO, Chun OK, Obayashi S, Cho S, Chung CE. Is consumption of breakfast associated with body mass index in US adults? J Am Diet Assoc. 2005;105:1373–82. doi: 10.1016/j.jada.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Cho S, Dietrich M, Brown CJ, Clark CA, Block G. The effect of breakfast type on total daily energy intake and body mass index: Results from the Third National Health and Nutrition Examination Survey (NHANES III) J Am Coll Nutr. 2003;22:296–302. doi: 10.1080/07315724.2003.10719307. [DOI] [PubMed] [Google Scholar]
- 14.Stockman NK, Schenkel TC, Brown JN, Duncan AM. Comparison of energy and nutrient intakes among meals and snacks of adolescent males. Prev Med. 2005;41:203–10. doi: 10.1016/j.ypmed.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Sjöberg A, Hallberg L, Höglund D, Hulthén L. Meal pattern, food choice, nutrient intake and lifestyle factors in the Göteborg Adolescence Study. Eur J Clin Nutr. 2003;57:1569–78. doi: 10.1038/sj.ejcn.1601726. [DOI] [PubMed] [Google Scholar]
- 16.Berkey CS, Rockett HR, Gillman MW, Field AE, Colditz GA. Longitudinal study of skipping breakfast and weight change in adolescents. Int J Obes Relat Metab Disord. 2003;27:1258–66. doi: 10.1038/sj.ijo.0802402. [DOI] [PubMed] [Google Scholar]
- 17.Affenito SG, Thompson DR, Barton BA, Franko DL, Daniels SR, Obarzanek E, et al. Breakfast consumption in African-American and white adolescent girls correlates positively with calcium and fiber intake and negatively with body mass index. J Am Diet Assoc. 2005;105:938–45. doi: 10.1016/j.jada.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Rampersaud GC. The benefits of breakfast for children and adolescents: update and recommendations for practitioners. Am J Lifestyle Med. 2009;3:86–103. [Google Scholar]
- 19.Videon TM, Manning CK. Influences on adolescent eating patterns: The importance of family meals. J Adolesc Health. 2003;32:365–73. doi: 10.1016/s1054-139x(02)00711-5. [DOI] [PubMed] [Google Scholar]
- 20.Westerterp KR. Assessment of physical activity: A critical appraisal. Eur J Appl Physiol. 2009;105:823–8. doi: 10.1007/s00421-009-1000-2. [DOI] [PubMed] [Google Scholar]
- 21.Park K. Obesity. In: Park K, editor. Park's Textbook of Preventive and Social Medicine. 19th ed. Jabalpur: Bhanot Publishers; 2007. pp. 332–6. [Google Scholar]
- 22.Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253. [PubMed] [Google Scholar]


