Abstract
Corticosteroids, one of the most widely prescribed topical drugs, have been used for about six decades till date. However, rampant misuse and abuse down the years has given the drug a bad name. Topical steroid abuse may lead to two major problems which lie at the opposing ends of the psychosomatic spectrum. Topical steroid addiction, a phenomenon that came to be recognized about a decade after the introduction of the molecule is manifested as psychological distress and rebound phenomenon on stoppage of the drug. The rebound phenomenon, which can affect various parts of the body particularly the face and the genitalia has been reported by various names in the literature. TC phobia which lies at the opposite end of the psychiatric spectrum of steroid abuse has been reported particularly among parents of atopic children. Management of both conditions is difficult and frustrating. Psychological counseling and support can be of immense help in both the conditions.
Keywords: Addiction, phobia, topical corticosteroids
What was known?
Topical corticosteroids misuse leads to psychological problems.
These problems lie at opposite ends of a spectrum causing both addiction and phobia.
Addiction results in psychological distress and rebound phenomenon on stoppage of the drug.
Phobia occurs particularly among parents of atopic children.
Introduction
The introduction of topical hydrocortisone in 1952 marked a revolution in dermatologic therapy. Subsequent research led to more and more potent corticosteroids making way into the dermatologist's armamentarium. However, topical corticosteroids (TC) soon proved to be a double-edged sword, with the very properties which made it a useful therapeutic agent becoming the cause for its rampant misuse. Reports of cutaneous adverse effects of TC misuse started emerging almost a decade after its introduction.[2] However, its addictive potential was realized much later.[3] Kligman and Frosh first described in detail the condition for which they coined the term “Steroid addiction”.[4] The condition may have various manifestations which have been described in the literature as light-sensitive seborrheid,[5] red skin syndrome,[6] steroid-induced rosacea-like dermatitis[7] and topical corticosteroid-damaged face.[8] “Topical corticosteroid addiction/dependence” implies the cutaneous and psychological dependence of the patient on the drug (TC), which results in rebound phenomenon and psychological distress on stoppage of its application. It is this psychological aspect which differentiates this condition from the other TC-induced skin reactions. On the other extreme of the psychological spectrum of topical steroid abuse lies the entity known as “steroid phobia” where sub-therapeutic amounts of TC are used due to fear or prejudice against “steroids” even at the cost of therapeutic efficacy.
Addiction
Addiction essentially means an excessive liking for something, leading to its repeated use of it followed subsequently by overuse and misuse. This finally leads to dependence on that particular item, in many cases. Dependence on a psychoactive substance is a condition which is characterized by a set of distinctive features. The person might lose control of amount and duration of intake once he starts it. An unavoidable and intensely strong desire for its intake, commonly denoted as craving, is common in these people. A set of demonstrable withdrawal symptoms, both physiological and psychological are associated. There would be an evidence of tolerance of the substance i.e. progressive increase in requirement of the substance to produce the same physiological and psychological effect. A person is said to be dependent on a psychoactive substance, when he shows some characteristic features. Another characteristic feature of dependence is persistent use of the substance despite being aware of its harmful physical, social or legal consequences. For some time if three or more of these features are present together, a person would be officially diagnosed with dependence on that substance.[9] The various terminologies like dependence, addiction, abuse or harmful use essentially convey the same meaning—the person is harmfully and helplessly attached to the substance for a substantial period.[10]
Topical Corticosteroid Addiction (TCA)
The condition results from chronic misuse of TC which results in psychological and physical (cutaneous) dependence on the drug. Any attempt to stop the offending drug leads to a rebound or flare in the symptoms which becomes both physically and psychologically distressing to the patient. Thus, in order to maintain normal or near normal social functioning, the individual continues using the drug. Any attempt to withdraw it fails or is resisted by the patient. Although there have been no population-based study to measure the prevalence of TC misuse in the population a large number of clinic or hospital-based studies are available. However, in most of these studies only the magnitude of TC misuse or the incidence of the common adverse effects of TC among OPD patients has been measured. How many of these patients of chronic TC misuse actually develop the rebound phenomenon characteristic of TCA is difficult to assess. In a multicentric study conducted in India on TC misuse on face 15% of chronic abusers of TC were found to be addicted to it.[8] A hospital-based study in Iraq found 94% patients with steroid-induced rosacea to experience a rebound.[11] The face is the most common site of TCA. However, other sites of the body such as the flexures, perianal area and genital area in both males and females—sites which are prone to develop other adverse effects of TC—may also show symptoms due to topical steroid addiction. The basic clinical features of the condition are the same irrespective of the site of involvement, though the presentation varies slightly depending on the site.
TCA of Face
Iatrogenic TC misuse on face often occurs in cases of chronic atopic dermatitis or seborrheic dermatitis.[6] There is a history of long-term use of TC, for control of a rash which becomes increasingly resistant. The patient or treating physician may step up the potency of the TC or increase the frequency of application to control this “resistant rash”. A vicious cycle ensues and the patient becomes increasingly addicted to the TC. The face is also the most common site of misuse of TC by the lay public who use it as a fairness cream, anti-acne cream, beauty cream etc [Figure 1].[8] The skin which was relatively normal at first starts developing pustules, acneform lesions and erythematous papules [Figure 2]. These lesions have a tendency to flare up on stopping the drug. Clinically the patient presents with diffuse facial erythema with papules, pustules, dryness and telangiectasia [Figure 3]. Photosensitivity is present in most of the cases.[12] Sometimes the rebound phenomenon may involve an area larger than the area of TC misuse. Distant sites may also be affected.[6] Some patients may also present with symptoms resembling status cosmeticus, or repeated flares of photosensitivity with erythema resembling chronic actinic dermatitis.[6]
Figure 1.

Tinea incognito on face due to repeated use of high potency topical corticosteroid on face as a fairness cream
Figure 2.

Hypertrichosis on face of a child due to prolonged use of topical corticosteroid
Figure 3.

Post-steroid erythema, acne and hypertrichosis
TCA of Genitalia And Perianal Area
TCA of the scrotum, inguinal and penile area have been described by various authors.[4,6] It is manifested as burning erythema of the entire region, scrotal pain and in the later stages atrophy of the glans. The condition known as red scrotum syndrome has also been attributed to topical steroid abuse.[6] The erythema and pain flares on stopping the TC and forces the patient back to TC application. The condition can be accompanied by intense psychological depression and anxiety which in some cases may even lead to impotence. TC is often used on the female genitalia for control of nonspecific discomfort or pruritus due to various reasons. Repeated use may result in addiction leading to persistent pruritus vulvae and vulvodynia which worsens on withdrawal. The labia and vestibule appear glazed and erythematous. This condition can affect the normal daily functioning of the patient.[6] TCA of the perianal area presents as persistent perianal erythema and burning occurring as a manifestation of rebound phenomenon. The continued TC use might lead to perianal atrophoderma.[6]
Pathogenesis
Although the more potent topical corticosteroids are the molecules which have a greater potential for causing TCA, even the long term use of the milder so-called safe ones are not completely without risks. However, the duration of use required for developing TCA varies with the potency of the TC. The more potent the molecule, the shorter is the duration of usage which can result in dependence. Likewise the withdrawal and management of cases of TCA caused by more potent molecules is more difficult and requires a longer period of time. Still it has been reported that a period of about 4 months or 2 months on average of TC misuse precedes development of this condition.[7,12] A reactive fixed vasodilatation occurring on withdrawal of the vaso-constrictive effect of the TC is the possible mechanism underlying the fixed erythema that characterizes rebound. This is possibly mediated by Nitric oxide (NO).[6] Repeated application of TC results in chronic vasoconstriction due to inhibition of action of NO. Release of the endothelial NO stores on withdrawal of TC hence results in hyperdilatation of the blood vessel, which is perhaps worsened by the TC-induced dermal atrophy and lack of support to the cutaneous vasculature.[12] Another hypothesis regarding the pathogenesis of the rebound phenomenon incriminates the immunosuppressive effect of TC. Possibly the chronic immunosuppression caused by the TC causes overgrowth of micro-organisms which may act as super-antigens. Withdrawal of the TC-induced immunosuppression then results in an antigen mediated inflammatory reaction of the skin, which manifests as the inflammatory papules and pustules seen on rebound.[12] Atopic individuals are more prone to developing TCA because of inherent vasomotor instability and chances of long-term misuse because of their dermatologic condition. In the study of Rappaport et al. involving more than 800 patients of TC of face, 90% of the patients were atopic.[6]
Management
Treatment aims at complete stoppage of the TC and reversal of the skin damage. Patients need to be counseled regarding the rebound on withdrawal. A lot of psychological support is often required at this stage. While some advocate a sudden complete cessation of TC with supportive measures,[6] others prefer a slower form of withdrawal with tapering potency of TC, to prevent the extremely distressing rebound.[7,13] Corticosteroid withdrawal is characterized by a mild erythema and flare for 2 weeks followed by desquamation [Figure 4]. The eruythema resolves but recurs within a fortnight. A second flare usually occurs within 2 weeks followed again by resolution. A number of such flares with decreasing intensity followed by resolutions of longer durations occur before complete cure – the duration of the withdrawal period depends on the duration of use of the topical corticosteroid [Figure 5]. This pattern of flare and resolution repeats itself but each time smaller duration of flares and longer resolution periods.[6]
Figure 4.

Post-steroid erythema and acne
Figure 5.
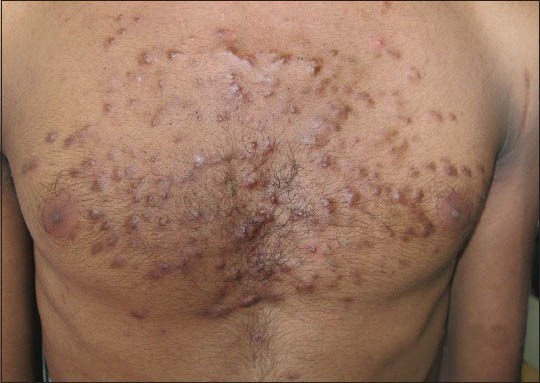
Truncal acne following prolonged use of high potent corticosteroid applied for tinea corporis
Therapeutic intervention in such cases is quite difficult. There is some controversy regarding the use of topical calcineurin inhibitors. Some workers found it to be quite useful.[14,15] However, Rapaport et al. in their study found them to be ineffective along with further increase of the burning sensation.[6] Oral antibiotics such as doxycycline or minocycline and other drugs such as metronidazole can be helpful.[16] Other supportive measures include repeated ice compress, Burrows compress for wet weepy lesions and use of bland emollients to alleviate dryness.[6] Oral antihistaminics may be required to control the associated pruritus.[12] Anxiolytics may be required in some patients. In general the duration required for complete withdrawal of the steroid and the patient to become symptom-free depends on the duration and the potency of the TC misuse, with more potent TC and longer duration of use taking more time to clear.[6]
Phobia
Phobia denotes an extreme aversion, avoidance and fear. One of the basic tenets of the concept of phobia is the fear is irrational leading to a deliberate avoidance of the item producing it, and the condition leads to gross socio-occupational dysfunction. That the fear is irrational is sometimes even acknowledged by the patient himself but when exposed to it, he cannot help avoiding it.[10]
TC Phobia
TC phobia (TCP) occupies a position at the extreme opposite end of the spectrum of TC-addiction. TCP is defined as a fear vis-à-vis the TC, rational or not.[17] Although this fear is difficult to grade, it is an important factor that affects compliance adversely. In fact TCP is a new phenomenon that has emerged probably because of rampant TC abuse. In 1992 TC phobia, among patients as well as doctors, was first reported from Germany. TC therapy has been discredited by physicians because of the perils of indiscriminate use.[18] TCP is commonly encountered in chronic inflammatory skin disorders, especially atopic dermatitis. Charman et al. published the first study of TCP in patients of atopic dermatitis.[19] Further reports confirmed this phenomenon among parents of children with atopic dermatitis. A recent study of TCP conducted on caregivers of these patients showed that 38.3% were reluctant to use TC. Predictive factors for steroid phobia included female sex, paternal history of atopic dermatitis and frequent change of clinics.[20] Another study of childhood eczema found that 50% parents requested non-steroidal prescriptions due to concerns regarding skin atrophy and growth retardation.[21] Recently, Moret et al. have developed a scale called TOPICOP to measure TC phobia among parents of children with atopic dermatitis.[22]
Management
TC phobia leads to refusal to apply, irregular application (haphazardly as and when the patient feels) or less than useful application (e.g. only one application per day when the patient is asked to apply the TC twice). To ensure TC therapy compliance, the health care provider should aim to establish a strong patient-doctor relationship to allay the anxiety of the patients and their guardians. They should clearly communicate to them about the risk-benefit issues of TC. This would go a long way in improving compliance and reducing morbidity and mortality.[17]
What is new?
Although the more potent topical corticosteroids are the molecules which have a greater potential for causing TCA, even the long-term use of the milder so-called safe ones are not completely without risks.
Recently, a scale called TOPICOP has been developed to measure TC phobia among parents of children with atopic dermatitis.
Psychological counseling and support can be of immense help in both the conditions.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Sulzberger MB, Witten VH. The effect of topically applied compound F in selected dermatoses. J Invest Dermatol. 1952;19:101–2. doi: 10.1038/jid.1952.72. [DOI] [PubMed] [Google Scholar]
- 2.Epstein NN, Epstein WL, Epstein JH. Alrophic striae in patients with inguinal intertrigo. Arch Dermatol. 1963;87:450–7. [Google Scholar]
- 3.Burry JN. Topical drug addiction: Adverse effects of fluorinated corticosteroid creams and ointments. Med J Austr. 1973;1:393–6. doi: 10.5694/j.1326-5377.1973.tb118065.x. [DOI] [PubMed] [Google Scholar]
- 4.Kligman AM, Frosch PJ. Steroid addiction. Int J Dermatol. 1979;18:23–31. doi: 10.1111/j.1365-4362.1979.tb01905.x. [DOI] [PubMed] [Google Scholar]
- 5.Frumess GM, Lewis HM. Light-sensitive seborrheid. AMA Arch Derm. 1957;75:245–8. doi: 10.1001/archderm.1957.01550140089014. [DOI] [PubMed] [Google Scholar]
- 6.Rapaport MJ, Rapaport V. The red skin syndromes: Corticosteroid addiction and withdrawal. Expert Rev Dermatol. 2006;1:547–61. [Google Scholar]
- 7.Rathi SK, Kumrah L. Topical corticosteroid-induced rosacea-like dermatitis: A clinical study of 110 cases. Indian J Dermatol Venereol Leprol. 2011;77:42–6. doi: 10.4103/0378-6323.74974. [DOI] [PubMed] [Google Scholar]
- 8.Saraswat A, Lahiri K, Chatterjee M, Barua S, Coondoo A, Mittal A, et al. Topical corticosteroid abuse on the face: A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160–6. doi: 10.4103/0378-6323.77455. [DOI] [PubMed] [Google Scholar]
- 9.Geneva: WHO; 1993. The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic Criteria for Research. [Google Scholar]
- 10.American Psychiatric Association. 5th ed. Arlington, VA: American Psychiatric Association; 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 11.Hameed AF. Steroid dermatitis resembling rosacea: A clinical evaluation of 75 patients. ISRN Dermatol. 2013;2013:491376. doi: 10.1155/2013/491376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen AY, Zirwas MJ. Steroid-induced rosacea like dermatitis: Case report and review of the literature. Cutis. 2009;83:198–204. [PubMed] [Google Scholar]
- 13.Ljubojeviae S, Basta-Juzbasiae A, Lipozenèiae J. Steroid dermatitis resembling rosacea: Aetiopathogenesis and treatment. J Eur Acad Dermatol Venereol. 2002;16:121–6. doi: 10.1046/j.1468-3083.2002.00388_2.x. [DOI] [PubMed] [Google Scholar]
- 14.Goldman D. Tacrolimus ointment for the treatment of steroid-induced rosacea: A preliminary report. J Am Acad Dermatol. 2001;44:995–8. doi: 10.1067/mjd.2001.114739. [DOI] [PubMed] [Google Scholar]
- 15.Chu CY. An open-label pilot study to evaluate the safety and the efficacy of topically applied pimecrolimus cream for the treatment of steroid-induced rosacea-like eruption. J Eur Acad Dermatol Venereol. 2007;21:484–90. doi: 10.1111/j.1468-3083.2006.01991.x. [DOI] [PubMed] [Google Scholar]
- 16.Narang T, Kumaran MS, Dogra S, Saikia UN, Kumar B. Red scrotum syndrome: Idiopathic neurovascular phenomenon or steroid addiction? Sex Health. 2013;10:452–5. doi: 10.1071/SH13052. [DOI] [PubMed] [Google Scholar]
- 17.Aubert H, Barbarot S. Non adherence and topical steroids. Ann Dermatol Venereol. 2012;(139 Suppl 1):S7–12. doi: 10.1016/S0151-9638(12)70102-3. [DOI] [PubMed] [Google Scholar]
- 18.Drosner M. Paths to a rational cortisone therapy via urea supplements-countering cortisone phobia. Hautarzt. 1992;(43 Suppl 11):23–9. [PubMed] [Google Scholar]
- 19.Charman CR, Morris AD, Williams HC. Topical corticosteroid phobia in patients with atopic eczema. Br J Dermatol. 2000;142:931–6. doi: 10.1046/j.1365-2133.2000.03473.x. [DOI] [PubMed] [Google Scholar]
- 20.Kojima R, Fujiwara T, Matsuda A, Narita M, Matsubara O, Nonoyama S, et al. Factors associated with steroid phobia in caregivers of children with atopic dermatitis. Pediatr Dermatol. 2013;30:29–35. doi: 10.1111/j.1525-1470.2012.01808.x. [DOI] [PubMed] [Google Scholar]
- 21.Hon KL, Kam WY, Leung TF, Lam MC, Wong KY, Lee KC, et al. Steroid fears in children with eczema. Acta Paediatr. 2006;95:1451–5. doi: 10.1080/08035250600612298. [DOI] [PubMed] [Google Scholar]
- 22.Moret L, Anthoine E, Aubert-Wastiaux H, Le Rhun A, Leux C, Mazereeuw-Hautier J, et al. TOPICOP©: A new scale evaluating topical corticosteroid phobia among atopic dermatitis outpatients and their parents. PLoS One. 2013;8:e76493. doi: 10.1371/journal.pone.0076493. [DOI] [PMC free article] [PubMed] [Google Scholar]


