Sir,
Blepharochalasis is a rare disorder characterized by laxity of the eyelid skin due to a defect in the elastic tissue. Blepharochalasis is usually bilateral; unilateral cases are extremely rare. We report a rare case of unilateral blepharochalasis.
A 14-year-old female presented with gradually progressing laxity and wrinkling of right upper eyelid since 6 years. At the age of 8, she noted a painless swelling of the right upper eyelid. The swelling persisted for 3 days and subsided without any medication. Such attacks of asymptomatic swelling occurred repeatedly over a period of 4 years. After that, the frequency of attacks gradually decreased; the last episode was 6 months before presentation. There was no history of any prior drug intake and no history of chronic or recurrent dermatitis of eyelids or urticarial lesions. There was no enlargement of thyroid. None in her family had a similar history. The cutaneous examination revealed thin, lax, wrinkled, and atrophic skin of the right upper eyelid with rounding of the medial canthal angle and nasal fat pad atrophy [Figure 1]. The patient was investigated thoroughly for other causes of eyelid edema. Color Doppler study was done to rule out any pathological cause of eyelid edema [Figure 2]. A diagnosis of unilateral blepharochalasis was made. We plan to wait for 6 more months and undertake blepharoplasty if no further episodes of swelling occur.
Figure 1.
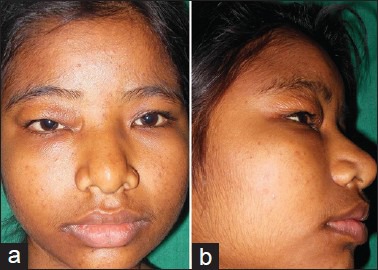
Thin, lax, wrinkled, and atrophic skin of right upper eyelid with rounding of the medial canthal angle and nasal fat pad atrophy
Figure 2.
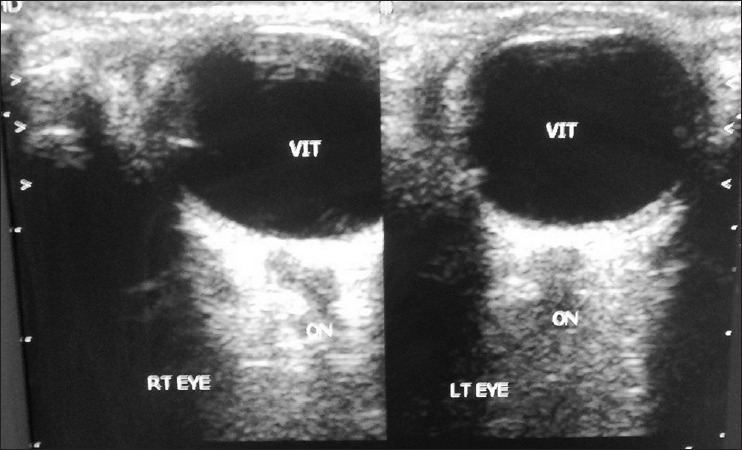
Color Doppler study showing normal images of bilateral eyes
There are three stages of blepharochalasis. In the primary edema stage, there is intermittent painless and transient swelling of eyelids with mild redness of skin resembling angioedema. In the second (atonic ptosis) stage, the skin becomes discolored, reddish brown, heavily venular, flabby, and hangs over the lashes. The power to lift the eyelid is decreased. In the third (ptosis adipose) stage, there is relaxation of the tissues of the orbital septum with subsequent prolapse of orbital fat and lacrimal glands, resulting in drooping of the affected eyelid. Most of the reported cases had presented in the second stage. Incidentally, our case also presented in the second stage.
In individuals with atypical clinical presentations, ultrasonography, computed tomography (CT) scanning, or magnetic resonance imaging (MRI) may be performed to exclude dysthyroid orbitopathy, idiopathic orbital inflammation, or other processes that could result in eyelid edema. In the present case, we performed color Doppler to rule out any other possible ocular or orbital cause.
Ascher’s syndrome (Laffer–Ascher syndrome) is a rare combination of blepharochalasis, double lip, and nontoxic thyroid enlargement generally noted in adolescence. There are occasional reports of blepharochalasis showing significant improvement with oral acetazolamide with or without topical steroid.[1] The only effective treatment of blepharochalasis is surgical correction, that is, blepharoplasty. The frequency of edema decreases with age. Hence, surgery should be deferred at least for 1 year from the last attack of eyelid edema. Otherwise, subsequent attacks of lid edema may interfere with the results. We decided to wait for another 6 months before undertaking blepharoplasty.
There are reports of blepharochalasis in the Indian literature as early as 1985.[2] Most cases had involvement of upper eyelids bilaterally. Reports of unilateral blepharochalasis in the world literature are rare.[3,4,5] To the best of our knowledge (after an extensive search in Pubmed, we could not get a single Indian case report), this is the first report of unilateral blepharochalasis from India.
References
- 1.Lazaridou MN, Sandinha T, Kemp EG. Oral acetazolamide: A treatment option for blepharochalasis? Clin Ophthalmol. 2007;1:331–3. [PMC free article] [PubMed] [Google Scholar]
- 2.Ranjini G, Janaki C, Premalatha S, Zahra A. Blepharochalasis: A case report. Indian J Dermatol. 1984;29:35–8. [PubMed] [Google Scholar]
- 3.Brazin SA, Stem LJ, Taylor-Johnson W. Unilateral blepharochalasis. Arch Dermatol. 1979;115:479–81. [PubMed] [Google Scholar]
- 4.Langley KE, Patrinely JR, Anderson RL, Thiese SM. Unilateral blepharochalasis. Ophthalmic Surg. 1987;18:594–8. [PubMed] [Google Scholar]
- 5.Collin JR. Blepharochalasis. A review of 30 cases. Ophthal Plast Reconstr Surg. 1991;7:153–7. doi: 10.1097/00002341-199109000-00001. [DOI] [PubMed] [Google Scholar]


