Abstract
Background
Closure of asylums and institutions for the mentally ill, coupled with government policies focusing on reducing the number of hospital beds for people with severe mental illness in favour of providing care in a variety of non‐hospital settings, underpins the rationale behind care in the community. A major thrust towards community care has been the development of community mental health teams (CMHT).
Objectives
To evaluate the effects of community mental health team (CMHT) treatment for anyone with serious mental illness compared with standard non‐team management.
Search methods
We searched The Cochrane Schizophrenia Group Trials Register (March 2006). We manually searched the Journal of Personality Disorders, and contacted colleagues at ENMESH, ISSPD and in forensic psychiatry.
Selection criteria
We included all randomised controlled trials of CMHT management versus non‐team standard care.
Data collection and analysis
We extracted data independently. For dichotomous data we calculated relative risks (RR) and their 95% confidence intervals (CI) on an intention‐to‐treat basis, based on a fixed effects model. We calculated numbers needed to treat/harm (NNT/NNH) where appropriate. For continuous data, we calculated weighted mean differences (WMD) again based on a fixed effects model.
Main results
CMHT management did not reveal any statistically significant difference in death by suicide and in suspicious circumstances (n=587, 3 RCTs, RR 0.49 CI 0.1 to 2.2) although overall, fewer deaths occurred in the CMHT group. We found no significant differences in the number of people leaving the studies early (n=253, 2 RCTs, RR 1.10 CI 0.7 to 1.8). Significantly fewer people in the CMHT group were not satisfied with services compared with those receiving standard care (n=87, RR 0.37 CI 0.2 to 0.8, NNT 4 CI 3 to 11). Also, hospital admission rates were significantly lower in the CMHT group (n=587, 3 RCTs, RR 0.81 CI 0.7 to 1.0, NNT 17 CI 10 to 104) compared with standard care. Admittance to accident and emergency services, contact with primary care, and contact with social services did not reveal any statistical difference between comparison groups.
Authors' conclusions
Community mental health team management is not inferior to non‐team standard care in any important respects and is superior in promoting greater acceptance of treatment. It may also be superior in reducing hospital admission and avoiding death by suicide. The evidence for CMHT based care is insubstantial considering the massive impact the drive toward community care has on patients, carers, clinicians and the community at large.
Plain language summary
Community mental health teams (CMHTs) for people with severe mental health problems
In the contemporary Western world mental health services are far more likely to be community than hospital based. In the United Kingdom, hospital and hospital‐based out‐patient clinics have been replaced with community mental health treatment teams (CMHTs) whose members are not just psychiatrists, but also nurses, psychologists, occupational therapists and social workers, and who work from a building other than a hospital, usually in a geographically defined area.
This review aims to compare CMHTs with inpatient care, hospital‐based out‐patient care or day hospital (standard care) for people living in the community with a serious mental health problem. Three randomised control trials were found that fulfilled these criteria. They included a total of 587 people, took place in urban areas of the UK and lasted from three months to one year. In the two studies that recorded it, a total of 52 people from 253 left the study early, though there was no significant difference in numbers between CMHT and control. Deaths in each study were recorded (suicide, suspicious circumstances and physical ill‐health), and although there were no significant differences between the two groups, those in the CMHT group were consistently lower than in standard care. People in CMHTs were also significantly less likely to be admitted to hospital during the period of the study, and were less likely to use social services. However, there was no significant difference between the groups in the use of accident and emergency services, general hospital services and primary care (family doctors). One study looked at satisfaction with care and found those in CMHTs were more satisfied with their care than the standard care group.
In the UK and other Western world countries, the move to CMHT has happened despite the limited evidence given above, therefore improving the evidence base is difficult. This should be borne in mind when comparing CMHTs with more specialised services such as early intervention or crisis resolution.
(Plain language summary prepared for this review by Janey Antoniou of RETHINK, UK www.rethink.org)
Background
Since the 1950's there has been an almost worldwide trend towards the closure of asylums and institutions for the mentally ill. Coupled with these closures, many government policies have focused on reducing the number of hospital beds for people with severe mental illness in favour of providing care in a variety of non‐hospital settings. The theory behind care in the community is that it enables individuals to live as independently as possible within their own homes or 'homely settings' in the community. It is hoped that this will increase the opportunities for people with serious mental illness to achieve their full 'potential' (DoH 1990) as autonomous members of society. Community care policies are also aimed at promoting choice and independence for individuals experiencing mental health difficulties.
A major thrust towards community care has been the development of community mental health teams (CMHT) (Bouras 1986, Bennett 1991). Usually the teams are comprised of several disciplines, including nurses, occupational therapists, psychiatrists, psychologists and social workers. Community mental health teams work to provide care which is less focused on hospital/institutional settings (Merson 1992b). Studies have suggested that CMHT management reduces time spent in hospital (Merson 1992b, Creed 1996) but it is uncertain, however, whether this policy leads to other benefits for seriously mentally ill people. It also remains unclear whether these policies benefit carers and society, particularly with respect to how mentally ill people function or behave in day to day life (Dowell 1993). Other controversies have surrounded the question of the quality of life of people with schizophrenia living in the community. There are suggestions that in some areas this process has lead to the development of 'psychiatric ghettos'; the direct converse of the aims of the theory driving the policies of change.
The degree to which the policy of community care and CMHT management has led to an increase in violent incidents is also the focus of controversy (Coid 1994). Those most prone to violent behaviour are those with a severe illness, such as mania or acute schizophrenia, combined with an alcohol or drug problem and deeply ingrained, maladaptive, patterns of behaviour (a disordered personality) (Miller 1993). The combination of mental illness and disordered personality ('dual diagnosis') is also associated with more self‐harm and death by suicide (Garvey 1980, Friedman 1983).
Although the original review has been criticised in peer review journals for adding little to the CMHT literature (due in part to the heterogeneity of included studies (Holloway 2001)) an update is now timely. As the activities of the community mental health team become supplemented by a range of specialised teams, such as assertive community treatment (assertive outreach ‐ Marshall 2000a), early intervention services for psychosis (Marshall 2004, Marshall 2006) and crisis resolution teams (Joy 2006), the understanding of the effects of 'core' treatment is even more important. As services are currently configured, specialised services are all extra components to the central management role performed by a community mental health team. Before we can compare the effectiveness and cost of these more specialised teams with the generic community mental health team we need to compare CMHTs to standard hospital care, as these specialist teams could potentially be based from a hospital ward, obviating the need for the community mental health team altogether. As the focus of this review is 'core' care provided, many of the papers are necessarily older as CMHTs have been functioning for up to 2 decades in some areas. The included studies have been chosen because the essential comparison is the generic CMHT with standard hospital care. Professor Graham Thornicroft has perhaps provided the best definition of a generic CMHT:
"A multidisciplinary team of mental health staff which has a lead responsibility for the provision of specialist assessment, treatment and care to a defined population, often defined by geographical catchment area or primary care registration. Such a team will usually provide the full range of functions necessary at the specialist care level, including initial assessment of general adult patients referred from other agencies and teams, consultation to primary care staff on the management of patients, the initial provision of treatment during the onset of a disorder or the early stages of a relapse, and the continuing care of patients with longer term disabilities. Generic teams may be supplemented by particular specialist teams, for example for early intervention, for home treatment in crisis, or for the assertive community treatment, but the main provision of care for the majority of patients seen by specialist mental health services."
Not only is Thornicroft's definition widely accepted and easily recognisable as describing a CMHT, it specifically differentiates the range of 'specialised teams' from generic CMHTs. Other distinctions include: crisis intervention is usually a 24 hr service, assertive community treatment works on the basis of restricted case loads and early intervention restricts its focus to patients in the early stages of their illness, usually a psychotic one. These services are therefore substantially different and excluded from this review. We have also excluded RCTs which focus on case management alone as this is not equivalent to the care from CMHTs despite some overlap (see Marshall 1998 for an in depth review of this).
Objectives
To review the effects of CMHT management, when compared to non‐team community management, for anyone with serious mental illness.
To evaluate whether those with a personality disorder as well as a serious mental illness have a substantially different response to CMHT management when compared to those with the single diagnosis of serious mental illness.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomised controlled trials.
Types of participants
We included people presenting to, or being referred to, adult psychiatric services with severe mental illness (however diagnosed). Where personality status was recorded (however diagnosed) this was noted for the purposes of the analysis outlined in 'Objectives'.
Types of interventions
1. Community Mental Health Team: management of care from a multi disciplinary, community‐based team (that is more than a single person designated to work within a team).
2. Standard or usual care: must be stated to be the normal care in the area concerned. This could be non‐team community care, outpatient care, admission to hospital (where acutely ill people were diverted from admission and allocated CMHT or in‐patient care), or day hospital.
We identified the primary question of interest as the value of CMHT management. Where this management was 'confounded' by a specific intervention, such as case‐management or a substantially different team strategy (for example, Assertive Community Team management (ACT)), we excluded studies. However, if both groups, CMHT and 'standard care', received the specific intervention, then the study was appropriate to include as this then became a dependant variable.
We specifically excluded studies looking at the effect of teams such as assertive community treatment, early intervention services and crisis intervention teams for definitional reasons (see above).
Types of outcome measures
1. Death 2. Acceptability of management as measured by loss to follow up within the study
3. Participant and carer satisfaction
4. Health Care Utilisation 4.1 admission rate 4.2 duration of admission 4.3 general hospital service use 4.4 number of visits 4.5 use of primary care
5. Social Services use
6. Symptoms of serious mental illness 6.1 general improvements 6.2 clinical outcomes
7. Social Functioning
8. Police Contacts
9. Economic costs of all care and health care.
*We chose death acceptability of management, and participant and carer satisfaction as the primary outcomes of interest. We selected outcome measures which provided global estimations of functioning. Highly specific outcomes, such as, for example, 'sense of safety' were not reported. Such specific outcomes are rarely reported in more than one study and it is difficult to assess their relevance to the effectiveness of the treatment. Other outcomes not readily falling into these categories were also recorded but were not of pre‐stated interest.
We divided outcomes into short term (less than three months) medium term (3‐12 months) and long term (over one year).
Search methods for identification of studies
1. Electronic searching We searched the Cochrane Schizophrenia Group Trials Register (March 2006) using the phrase:
[((communit* and (center* or centre* or treat*)) in title) or ((*communit* and (*team* or *cmht* or *home*)) in title, abstract or index terms of REFERENCE) or (community* or home* in intervention of STUDY)]
This register is compiled by systematic searches of major databases, hand searches and conference proceedings (see Group Module).
1.2 Previous searches We searched the Cochrane Schizophrenia Group Trials Register (April 2002, October 2001) using the phrase:
[((COMMUNIT* and (TEAM* or CENTER* or CENTRE* or TREAT)) or #23=242 or #23=329 or #23=330 or #23=530]
[((COMMUNIT* and (TEAM* or CENTER* or CENTRE* or TREAT)) in title) or ((*communit* and (*team* or *cmht* or *home*)) in title, abstract or index terms of REFERENCE) or (Community Care or Home Care Services or Home Visits or Home‐and‐Hospital Care or Other Community Team in intervention of STUDY)]
1.2.1 We searched the Cochrane Schizophrenia Group Trials Register (August 1998) using the phrase:
[((COMMUNIT* and (TEAM* or CENTER* or CENTRE* or TREAT)) or #23=242 or #23=329 or #23=330 or #23=530]
1.3. We searched Biological Abstracts (January 1982 to January 1997) using the CSGs phrase for randomised controlled trials and schizophrenia (see Group search strategy) combined with the phrase:
[and ((COMMUNITY* near (TEAM* or CENTER* or CENTRE* or TREAT*) and MENTAL*)]
1.3.1 We re‐ran the search using only the CSGs phrase for randomised controlled trials, omitting the phrase for schizophrenia (see Group search strategy) combined with the phrase:
[and ((COMMUNIT* near (TEAM* or CENTER* or CENTRE* or TREAT*) and MENTAL*) and ((ANTISOCIAL or PSYCHOPATH* or BORDERLINE) near2 (DISORDER* or DIFFICULT* or PERSONALIT*)) or (PERSONALIT*) near2 (DISORDER* or DIFFICULT*))]
1.4 We searched the Cochrane Library (Issue 2, August 1998) using the phrase:
[COMMUNIT* and TEAM* and MENTAL*]
1.5 We searched EMBASE (January 1980 to January 1997) using the CSGs phrase for randomised controlled trials and schizophrenia (see Group search strategy) combined with the phrase:
[and (((COMMUNIT* near (TEAM* or CENTER* or CENTRE* or TREAT*) and MENTAL*) or ((COMMUNITY MENTAL HEALTH CENTER)@KMAJOR,KMIN) or ((COMMUNITY MENTAL HEALTH)@KMAJOR) and (TEAM* or (TEAMWORK)@KMAJOR,KMINOR))]
1.5.1 We re‐ran the search using only the CSGs phrase for randomised controlled trials, omitting the phrase for schizophrenia (see Group search strategy) combined with the phrase:
[and (((COMMUNIT* near (TEAM* or CENTER* or CENTRE* or TREAT*) and MENTAL*) or ((COMMUNITY MENTAL HEALTH CENTER)@KMAJOR,KMIN) or ((COMMUNITY MENTAL HEALTH)@KMAJOR) and (TEAM* or (TEAMWORK)@KMAJOR,KMINOR)) and (((ANTISOCIAL or PSYCHOPATH* or BORDERLINE) near2 (DISORDER* or DIFFICULT* or PERSONALIT*)) or (PERSONALIT*) near2 (DISORDER* or DIFFICULT*)) or (PERSONALITY DISORDER)@EX)]
1.6 We searched MEDLINE (January 1966 to January 1997) using the CSGs phrase for randomised controlled trials and for schizophrenia (see Group search strategy) combined with the phrase:
[and (((COMMUNIT* near (TEAM* or CENTER* or CENTRE* or TREAT*)) and MENTAL*) or explode COMMUNITY‐MENTAL‐HEALTH‐CENTERS/ all subheadings or ((explode COMMUNITY‐MENTAL‐HEALTH‐SERVICES/ all subheadings or explode COMMUNITY‐PSYCHIATRY/ all subheadings) and (team* or explode INSTITUTIONAL‐MANAGEMENT‐TEAMS/ all subheadings))]
1.6.1 We re‐ran the search using only the CSGs phrase for randomised controlled trials, omitting the phrase for schizophrenia (see Group search strategy) combined with the phrase:
[and (((COMMUNIT* near (TEAM* or CENTER* or CENTRE*)) and MENTAL*) or explode COMMUNITY‐MENTAL‐HEALTH‐CENTERS/ all subheadings or ((explode COMMUNITY‐MENTAL‐HEALTH‐SERVICES/ all subheadings or explode COMMUNITY‐PSYCHIATRY/ all subheadings) and (team* or explode INSTITUTIONAL‐MANAGEMENT‐TEAMS/ all subheadings)) and (((ANTISOCIAL or PSYCHOPATH* or BORDERLINE) near2 (DISORDER* or DIFFICULT* or PERSONALIT*)) or (PERSONALIT*) near2 (DISORDER* or DIFFICULT*)) or explode PERSONALITY‐DISORDERS/ all subheadings)]
1.7 We searched PsycLIT (January 1974 to January 1997) using the CSGs phrase for randomised controlled trials and schizophrenia (see Group search strategy) combined with the phrase:
[and ((COMMUNIT* near (TEAM* or CENTER* or CENTRE* or TREAT*) and MENTAL*) or (COMMUNITY‐MENTAL‐HEALTH‐CENTERS in DE) or ((explode COMMUNITY‐MENTAL‐HEALTH or COMMUNITY‐MENTAL‐HEALTH‐SERVICES IN DE or explode COMMUNITY‐PSYCHIATRY or explode COMMUNITY‐SERVICES) and (TEAM* or explode TEAMS)]
1.7.1 We re‐ran the search using only the CSGs phrase for randomised controlled trials, omitting the phrase for schizophrenia (see Group search strategy) combined with the phrase:
[and (((COMMUNIT* near (TEAM* or CENTER* or CENTRE* or TREAT*) and MENTAL*) or (COMMUNITY‐MENTAL‐HEALTH‐CENTERS in DE) or ((explode COMMUNITY‐MENTAL‐HEALTH or COMMUNITY‐MENTAL‐HEALTH‐SERVICES IN DE or explode COMMUNITY‐PSYCHIATRY or explode COMMUNITY‐SERVICES) and (TEAM* or explode TEAMS))) and (((ANTISOCIAL or PSYCHOPATH* or BORDERLINE) near2 (DISORDER* or DIFFICULT* or PERSONALIT*)) or (PERSONALIT*) near2 (DISORDER* or DIFFICULT*)) or explode PERSONALITY‐DISORDERS)]
1.8 SCISEARCH ‐ Science Citation Index We sought each of the included studies as a citation on the SCISEARCH database, and inspected reports of articles that had cited these studies in order to identify further trials.
2. Reference lists We examined references cited in all included trials in order to identify any missing studies.
3. Hand searching We searched The Journal of Personality Disorders (up to August 2006).
4. Personal contact We contacted the authors of all studies initially selected for inclusion in order to identify further relevant trials. DM contacted Professor G Thornicroft for a definition of a generic CMHT. DM and GNH again contacted the authors for further information on the included studies with the recent revision.
PT contacted colleagues on the Executive Boards of the European Network for Mental Health Service Evaluation (ENMESH) and the International Society for the Study of Personality Disorders (ISSPD) by sending them a copy of the letter outlined above.
JC also contacted all colleagues in forensic psychiatry within the UK by sending them a copy of the same letter in order to identify studies with mentally abnormal offenders which may also meet the inclusion criteria.
Data collection and analysis
1. Selection of trials Shaeda Simmonds performed the search for trials. Initial inspection and selections were undertaken by SS and PT independently. We (DM and GNH) repeated this process on the updated searches. In the original review we (SS and PT) separately evaluated the acquired studies and decided which should be included. We found overall agreement to be excellent (evaluated by the kappa statistic Cicceti 1981). Where disagreement occurred we asked (SM) to resolve the dispute. If agreement could not be reached we added the study to those awaiting assessment and the authors' were contacted for further data. We repeated this process with the updated searches with DM and GNH independently evaluating the acquired studies. Potential papers from Chinese journals reporting on Chinese provisions are awaiting classification, as we were unable to verify whether the models of care were sufficiently similar to CMHT care as defined by Thornicroft. PT resolved any disagreements and reviewed the included and excluded papers.
2. Assessment of methodological quality We (SS and PJ) assessed the methodological quality of included trials in this review using the Jadad Scale (Jadad 1996). This rated the quality of reporting of randomisation, blindness, follow‐up, and people leaving the study early. We only included trials reliably rating over two on this scale. For the updates, we (DM and GNH) assessed the methodological quality of included trials using the criteria described in the Cochrane Handbook (Higgins 2005). It is based on the evidence of a strong relationship between allocation concealment and direction of effect (Schulz 1995). Only trials in Category A or B (low or moderate risk of bias) were included in the review. We considered the paper of Soares 2004 in deciding to include category B trials into the review. When disputes arose as to which category a trial should be allocated, again resolution was attempted by discussion. When this was not possible we did not enter the data and the trial was added to the list of those awaiting assessment until further information could be obtained. The categories are defined below:
A. Low risk of bias (adequate allocation concealment) B. Moderate risk of bias (some doubt about the results) C. High risk of bias (inadequate allocation concealment).
3. Data extraction We (SS and SM) independently extracted data. Again, any disagreements were discussed, and where further clarification was needed, we contacted the authors' of trials to provide missing data.
3.1 Intention to treat analysis We excluded data from studies where more than 50% of data for any given outcome were lost to follow up. In studies with less than 50% dropout rate, we considered people leaving early to have had the negative outcome, except for the event of death. We analysed the impact of including studies with high attrition rates (25‐50%) in a sensitivity analysis. If inclusion of data from this latter group did result in a substantive change in the estimate of effect we did not add their data to trials with less attrition, but presented the data separately.
4. Data types 4.1 Dichotomous data We carried out an intention to treat analysis. This means that everyone allocated to the treatments was counted irrespective of whether they completed follow up. Where a person failed to complete treatment we assumed that they did not have a good outcome. When analysing loss of contact in studies where deaths had occurred, the size of treatment and control groups was reduced by the number of deaths. Deaths were not counted as losses of contact. We analysed data by, firstly building in the assumption that those who dropped out had a poor outcome and then analysing only completers to see if the results were substantively different. The data presented, however, were from the intention to treat analysis. We calculated the relative risk (RR) and its 95% confidence interval (CI) using a fixed effects model. Where appropriate we calculated the number needed to treat statistic (NNT) and number needed to harm (NNH).
4.2 Continuous data 4.2.1 Normal distribution Continuous data on outcomes in trials relevant to mental health issues are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data we applied the following standards to continuous final value endpoint data before inclusion: (a) standard deviations and means were reported in the paper or were obtainable from the authors, (b) when a scale started from zero, the standard deviation, when multiplied by two, should be less than the mean (otherwise the mean is unlikely to be an appropriate measure of the centre of the distribution ‐ Altman 1996), In cases with data that are greater than the mean they were entered into 'Other data' table as skewed data. If a scale starts from a positive value (such as PANSS, which can have values from 30 to 210) the calculation described above in (b) should be modified to take the scale starting point into account. In these cases skewness is present if 2SD>(S‐Smin), where S is the mean score and Smin is the minimum score.
For change data (mean change from baseline on a rating scale) it is impossible to tell whether data are non‐normally distributed (skewed) or not, unless individual patient data are available. After consulting the ALLSTAT electronic statistics mailing list, we presented change data in RevMan graphs to summarise available information. In doing this, we assumed either that data were not skewed or that the analysis could cope with the unknown degree of skew.
4.2.2 Final endpoint value versus change data Where both final endpoint data and change data were available for the same outcome category, we only presented final endpoint data. We acknowledge that by doing this much of the published change data may be excluded, but argue that endpoint data is more clinically relevant and that if change data were to be presented along with endpoint data, it would be given undeserved equal prominence. We are contacting authors of studies reporting only change data for endpoint figures.
4.2.3 Data synthesis For continuous outcomes we estimated a weighted mean difference (WMD) between groups based on a fixed effects model.
4.3 Crossover design Where trials used a crossover design, we only used data from the first stage in order to avoid the potential additive effects from the second or later stages of these trials.
4.4 Rating scales: A wide range of instruments are available to measure mental health outcomes. These instruments vary in quality and many are not valid, and are known to be subject to bias in trials of treatments for schizophrenia (Marshall 2000b). Therefore we only included continuous data from rating scales if the measuring instrument had been described in a peer‐reviewed journal.
5. General In all cases we entered the data into RevMan in such a way that the area to the left of the 'line of no effect' indicates a 'favourable' outcome for CMHT management. As well as inspecting the graphical presentations, we checked for differences between the results of each using a test of heterogeneity.
6. Sensitivity analysis Firstly, we tested the sensitivity of the results from the main outcomes for change when adding the assumption that those who did not complete the study had a poor outcome. Secondly, for the main outcomes, we investigated whether those with the dual diagnosis of severe mental illness and personality disorder differed substantively when compared to those with only severe mental illness.
7. Cluster trials Studies increasingly employ cluster randomisation (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems. Firstly, authors often fail to account for intra class correlation in clustered studies, leading to a unit‐of‐analysis error (Divine 1992) whereby p values are spuriously low, confidence intervals unduly narrow and statistical significance overestimated. This causes Type I errors (Bland 1997, Gulliford 1999).
Where clustering was not accounted for in primary studies, we presented the data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review we will seek to contact first authors of studies to obtain intra‐class correlation co‐efficients of their clustered data and to adjust for this using accepted methods (Gulliford 1999). Where clustering has been incorporated into the analysis of primary studies, we will also present these data as if from a non‐cluster randomised study, but adjusted for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a design effect. This is calculated using the mean number of participants per cluster (m) and the intraclass correlation co‐efficient (ICC) [Design effect=1+(m‐1)*ICC] (Donner 2002). If the ICC was not reported it was assumed to be 0.1 (Ukoumunne 1999). If cluster studies had been appropriately analysed taking into account intra‐class correlation coefficients and relevant data documented in the report, we synthesised these with other studies using the generic inverse variance technique.
8. Heterogeneity. Firstly, we considered all the included studies within any comparison to judge for clinical heterogeneity. Then visually inspected graphs to investigate the possibility of statistical heterogeneity. This was supplemented using, primarily, the I‐squared statistic. This provides an estimate of the percentage of variability due to heterogeneity rather than chance alone. Where the I‐squared estimate was greater than or equal to 50% we interpreted this as indicating the presence of considerable levels of heterogeneity (Higgins 2003). If inconsistency was high and clear reasons explaining the heterogeneity were found, we presented the data separately. If not, we commented on the heterogeneity of the data.
9. Addressing publication bias We entered data from all identified and selected trials into a funnel graph (trial effect versus trial size) in an attempt to investigate the likelihood of overt publication bias. A formal test for funnel‐plot asymmetry was not undertaken.
10. General Where possible, we entered data in such a way that the area to the left of the line of no effect indicated a favourable outcome for aripiprazole.
Results
Description of studies
For substantive descriptions of studies please see Included and Excluded Studies table.
1. Excluded studies We excluded eighty studies, mostly because they were non‐randomised clinical studies or focused on assertive community therapy/case management as opposed to CMHT management.
2. Awaiting assessment Two trials await assessment (Gater 1997). This is a cluster randomised trial and we are seeking further information on the number of clusters used to enable outcome data to be analysed using a design effect (see methods section 7), and Tan 2004 which requires translation.
3. Ongoing studies We are not aware of any ongoing studies.
4. Included studies We included three studies, with a total of 587 participants. All three were randomised, and compared a standard hospital based service which usually assessed patients in the outpatient clinics, with less emphasis on multidisciplinary working and usually doctor lead. The comparator intervention had more focus on community based assessments in the community and multidisciplinary working. In none of the studies were the interventions a 24 hour service, nor were there restrictions on case loads indicative on crisis intervention or assertive community treatment respectively. One of the authors (Burns 1993), during correspondence, indicated that he felt the comparison was of two CMHT and with re‐evaluation it was felt that this study still met the inclusion criteria.
4.1 Length of trials The follow‐up period between initial and final assessments vary between three months and 12 months. Burns 1993 final assessment was at 12 months, Merson 1992b at three months and Tyrer 1998 at 12 months.
4.2 Participants In all three studies schizophrenia was the most common diagnosis and all included a significant minority of those with neurotic disorders. In only one of the studies was personality status recorded before treatment (Merson 1992b). Studies all included people of both sexes, and there were slightly more females than males. All studies used operationalised diagnoses. Burns 1993 used the Present State Examination (PSE). Merson 1992b used the International Classification of Diseases (ICD‐10) and Tyrer 1998 used the Operational Criteria Checklist for Psychotic Illness (OPCRIT) diagnostic system.
4.3 Setting All studies were undertaken in the UK in community settings.
4.4 Study size Burns 1993 was the largest study to be included (n=332), although many participants dropped out shortly after randomisation. Tyrer 1998 randomised 155 participants, although this study also lost many participants at the beginning of the study. Merson 1992b included 100 participants.
4.5 Interventions The community mental heath teams in each study were involved in multidisciplinary assessments of each person, followed by regular team reviews. Care involved monitoring and prescribing medication, different forms of psychological intervention (including family intervention) and with special focus on continuity of care. Standard care was co‐ordinated from hospital based staff who assessed and treated people primarily in hospital out‐patient and in‐patient settings. Care involved psychiatrists, nurses and social workers but this was not closely co‐ordinated and was not carried out by a single team. Treatment covered the range of psychiatric interventions.
4.6 Outcomes Almost all usable data available were reported as dichotomous, i.e. psychiatric admissions, length of hospital stay, clinical outcomes, social functioning and death. Much data were rendered unusable due to inadequate reporting of essential details such as mean scores and standard deviations. Reasons for exclusion of data from other instruments are given under 'outcomes' in the 'included studies' table. Details of the scales that supplied usable data for this review are shown below.
4.6.1 Mental state 4.6.1.1 Comprehensive Psychopathological Rating Scale ‐ CPRS (Asberg 1978) The CPRS consists of 65 scaled items, covering a wide range of psychiatric symptoms. Explicit definitions in a non‐technical language are provided for items as well as scale steps. It can be used in full, or as an item pool for which subscales for different psychiatric syndromes can be designed. Subscales exist inter al., for depression, schizophrenia, obsessive‐compulsive disorder, neurasthenic syndromes and mental distress in connection with severe physical illness. The rating is based on an interview which will require less than an hour in most cases if the scale is used in full. Due to the non‐technical language used, raters without formal training in psychiatry (i.e. nurses, psychologists, general practitioners) can use the scale without reduction in reliability. Higher scores indicate a worse outcome. Merson 1992b reported data from this scale.
4.7. Missing outcomes We were unable to use much of the data from scales due to incomplete information, such as standard deviation, mean scores and 'N' values not being reported. For a fuller description of these please see included studies tables 'outcomes'.
Risk of bias in included studies
1. Randomisation Three of the four studies described the method of randomisation. In two of the studies (Merson 1992b, Tyrer 1998) randomisation was by sealed envelope method with stratification by presence or absence or previous psychiatric service contact in one group (Merson 1992b). In Burns 1993 randomisation took place at the point of referral using a random number sequence before deciding whether or not the patient satisfied the inclusion criteria (Jadad score =3). This unusual method meant that many that were randomised were never included in the study. It did, however, still allow comparison between the two large groups for some outcomes such as death. In the update of this review, two of the studies mentioned adequate concealment of allocation (Burns 1993, Tyrer 1998) while Merson 1992b, did not make this clear.
2. Blinding Only one of the studies stated that the research assessments were carried out by a psychiatrist 'blind to service allocation' (Merson 1992b).
3. Leaving the study early The follow‐up period of the studies ranged from three to 12 months. All trials had some participants that left early. However, Burns 1993 shows a large proportion of participants leaving (80 out of 148 and 130 out of 178), as randomisation occurred before inclusion criteria were imposed.
Effects of interventions
Please see Table of comparisons for more detailed data.
1. The search For the update search (February, 2006) we found 58 references, none clearly met the inclusion criteria. The October 2003 search found 71 records, none met the inclusion criteria. The July 2002 search found 61 records, and again none met the inclusion criteria. The October 2001 search found 476 records, 15 were identified as being potentially relevant. On closer inspection three fulfilled the inclusion criteria, two were duplicates of previously included records and the third (Gater 1997) is a cluster randomisation trial which awaits assessment. No further records were identified from searching references.
2. Community Mental Health Teams versus STANDARD CARE (all diagnoses)
1. Death We found no statistically significant differences in death from any cause (n=587, 3 RCTs, RR 0.47 CI 0.2 to 1.3) during medium term evaluation (3 ‐ 12 months). Fewer deaths occurred in the CMHT group (n=5), compared with the control group (n=12) although the small numbers in individual studies usually provoked no comment, collectively they amounted to a clinically, although not statistically significant difference. Death due to suicide/suspicious circumstances (n=587, 3 RCTs, RR 0.49 CI 0.1 to 2.2), and death due to physical health (n=587, 3 RCTs, RR 0.51 CI 0.1 to 2.0) were also equivocal. 2. Leaving study early Two studies (Merson 1992, Tyrer 1998) provided data and we found results from 253 participants did not reveal any statistically significant differences (RR 1.10 CI 0.7 to 1.8) in the number of people who left the study early. The data from Burns 1993 could not be included as loss to follow up data were not provided and could not be inferred.
3. Satisfaction with Service Questionnaire ‐ Not satisfied We found significantly fewer people in the CMHT group not satisfied with services compared with those given standard care (Merson 1992, n=87, RR 0.37 CI 0.2 to 0.8, NNT 4 CI 3 to 11).
4. Service use 4.1 Admission rates We found admission rates to hospital were significantly lower in the CMHT group (n=587, 3 RCTs, RR 0.81 CI 0.7 to 1.0, NNT 17 CI 10 to 104) compared with those given standard care.
4.2 Duration of hospital admission Burns 1993 reported continuous data for duration of hospital admission but outcomes contained wide confidence intervals (skewed data) and are reported in 'other data' tables.
4.3 Use of accident and emergency We found no significant difference in the use of emergency services between CMHTs and those receiving standard care (n=587, 3 RCTs, RR 0.86 CI 0.7 to 1.1).
4.4 Contact with primary care We re‐examined this section using use, rather than lack‐of‐use, of primary care. This was to more accurately reflect the data as presented in the included studies. We found no group difference (n=587, 3 RCTs, RR 0.94 CI 0.8 to 1.1).
4.5 Contact with social services No significant differences were found in the use of social services between those receiving CMHTs and standard care (n=255, 2 RCTs, RR 0.76 CI 0.6 to 1.0).
5. Mental state 5.1 Comprehensive Psychopathological Rating Scale Merson 1992b used the CPRS scale but data contained wide confidence intervals (skewed data) and are reported in 'other data' tables.
6. Social functioning 6.1 Police contacts Two studies (Merson 1992b, Tyrer 1998) provided data and we found participants in the CMHT group had significantly more contact with the police compared with those receiving standard care (n=255, RR 2.07 CI 1.1 to 4.0), although data were heterogeneous (I2 = 53%).
CMHT versus STANDARD CARE (those with serious mental illnesses and personality disorder) We have not included this analysis in the update as this is comprehensively covered elsewhere (Tyrer 2003).
Discussion
1. Generalisability All the teams reported in this review were somewhat unusual in being specially selected or being linked to a research programme. Caution should be taken in generalising from these data to non‐research community mental health teams. As community mental health care has become more widespread it is also likely that 'standard' therapy is moving closer to community mental health team management. Further studies may therefore be associated with smaller differences between the two forms of care.
2. Death Community mental health teams may reduce suicide and deaths under suspicious circumstances. The numbers of patients in this systematic review are small and because of this, the reduction in overall death and in particular death by suicide or suspicious circumstances amount to a trend, but do not reach statistical significance. Approximately twice as many patients would be needed at the rates found in the included studies to reach significance. If CMHT care does indeed help decrease rates of suicide, it would be one of the few interventions for those with serious mental illnesses to have been shown to do so. Even if this effect is modest, as this review suggests, CMHT management made available to large groups of those with serious mental health problems, could result in significant saving of life.
3. Leaving study early The original review suggested patient retention was related to CMHT management. However, reanalysis does not support this. Losses in both groups were comparable, probably reflecting a consistent finding in psychiatric research rather than a result directly related to CMHT or standard care alone. This reanalysis does not support the popular notion that CMHT dramatically improves loss to services.
4. Satisfaction with care One study (Merson 1992b) showed an improved patient satisfaction in the CMHT groups. This is, perhaps, understandable as most people would prefer to be treated at home rather than in hospital. It also correlates with the trends for improved symptomatology with less admissions and shorter hospital stays in the CMHT group.
5. Service use 5.1 Hospital admission Reanalysis of the hospitalisation data now shows those in CMHT group are statistically less likely to be admitted to hospital. This would support the received wisdom that home treatment is generally acceptable to patients and effective in managing a wide variety of crises that would have otherwise needed hospitalisation. In the initial review, the Hoult paper (Hoult 1981) had a large number of admissions, and this paper has now been excluded as it more closely represents crisis resolution, not CMHT care.
5.2 Use of accident and emergency services All three studies reported data for this outcome, however from a total sample of 587 people CMHT did not reveal any benefit over standard care.
5.3 Contact with primary care The use of primary care between CMHT and standard care showed no difference in meta‐analysis. This was reflected in the first review. CMHT input does not increase GP contact.
5.4 Contact with social services The initial review did not comment specifically on this. Analysis of the two studies that reported social services use suggests an increased use among the control group. This is somewhat surprising, as it would be expected that integrated teams would be able to provide a more streamlined delivery of social care to patients. Conversely this may reflect the multidisciplinary nature of CMHTs and their ability to undertake some of the work that was social work in the control arm. It is not possible to test these assumptions further with the data presented.
6. Social functioning 6.1 Police Contacts This was not included in the results of the initial review although is clearly a proxy marker for social functioning. Analysis showed a significantly higher rate of police contact in the CMHT group but data are heterogeneous (!2 =53%) which may be due to group differences between the two sets of pooled data. In addition, the standard care groups spent longer in hospitals, an environment in which police contact is significantly less likely.
Authors' conclusions
Implications for practice.
1. For people with serious mental illness and their carers CMHT management may reduce suicide and be more acceptable to those with mental illness than a non‐team standard care approach. It is also likely that a person managed within a CMHT is more likely to avoid hospital admission and to spend less time as an in‐patient. CMHT care may lead to police contact and may mean less social services contact is necessary. There is, however, no substantial data supporting or refuting the use of CMHT management with respect to mental state or social functioning.
2. For clinicians This review is significantly more robust in that only studies clearly defined, as CMHTs are included. Health care professionals concerned at maintaining contact with individuals, particularly those at risk of suicide, should consider a CMHT. Much of the presumed benefits of CMHT care (e.g. lower cost, improved social functioning, greater patient, carer satisfaction, loss to follow up) are not supported by primary research. This makes implementing improvements on CMHTs with more highly specialised services, such as (Crisis Resolution Teams CRT, difficult to justify from an evidenced based perspective of benefits. In assessing models of care, it is important to recognise that CMHT, which is now becoming the control arm in many trials, is clearly described, but not clearly proven effective.
3. For policy makers and commissioners of care The finding from this update of CMHT care versus hospital based treatment suggests the evidence to support the commissioning of CMHTs as superior to hospital based management is scanty. It does appear, however that there is a trend towards improvements in some clinical areas, with no indication of deterioration (other than police contacts) at no increased cost. CMHTs do not reduce the cost of caring for patients with serious mental illness. This lack of evidence for the superiority of CMHTs undermines the drive towards CMHTs with a special focus, such as Crisis Resolution Teams (CRTs) or assertive outreach services.
Implications for research.
1. General The primary difficultly in the meta‐analysis of the data in this area is the breadth of instruments used to measure outcomes, both clinical and non clinical. This makes combination of the data difficult, and very often impossible, reducing the power of any conclusions that can be drawn. The evidence for CMHT based care is supported by only three reviewed research papers and this evidence base is surprisingly shallow, considering the massive impact the drive toward community care has on patients, carers, clinicians and the community at large. We are now implementing ever more specialised types of community care teams, without clear evidence that generic CMHTs fulfil their requirements in all areas. However, more studies in this area would now be difficult to rectify this as hospital based care is now phased out from most of the western world. Clear and strict adherence to the CONSORT statement (Moher 2001) for all outcomes would have resulted in a more informative review.
2. Future Trials This would clearly be difficult to achieve in the western world, as there is little social or political will to implement hospital based care. Although this type of trial could be carried out in the developing would, it is not clear if these results would be generalisable to a western setting considering the complex interaction of society, culture and presentation as factors in CMHT care.
Such a trial may, however, contain the components as listed in Table 1.
1. Suggestions for trial design.
| Methods | Participants | Interventions | Outcomes | Notes |
| Allocation: randomised, with sequence generation and concealment of allocation clearly described. Blindness: single. Duration: 12 months at least. Raters: independent. | Diagnosis: SMI with a clear definition of SMI from the outset. N=300.* History: in need of psychiatric admission. Sex: both. Age: any. | 1. Standard Hospital care: focus on outpatient appointments and only occasional emergency domicillary visits. A 9 till 5 service with little team working with or without care management. N=150. 2. CMHT: community and multidisciplinary team focus. A 9 till 5 service and not primarily emergency assessments. N=150. | Death. Serious harm to self and others. Service outcomes: hospital admission, readmissions. Leaving the study early. Global and mental state (CGI, binary outcome).** Use scales as used by Merson a 92 and Tyrer 98. Satisfaction: family burden, patient satisfaction, relative satisfaction, staff burden (binary data) Economic data. | * Size of study with sufficient power to highlight ˜10% difference between groups for primary outcome. ** Primary outcome. |
3. Well described participants and interventions The constituents of effective community team management remain unclear following this update and reanalysis. Several factors may be relevant, including the (i) size of case load, (ii) clarity of operational policies, (iii) qualification of the care workers, (iv) degree of continuity of care and (v) specific illnesses/disorders from which clients of CMHT may suffer. More trials incorporating these elements would help to clarify the effects of this approach.
What's new
| Date | Event | Description |
|---|---|---|
| 21 May 2018 | Amended | Review update is underway, new team assigned and the title will be amended to 'Community mental health teams for people with severe mental illnesses'. |
History
Protocol first published: Issue 1, 1997 Review first published: Issue 4, 1998
| Date | Event | Description |
|---|---|---|
| 15 February 2010 | Amended | Contact details updated. |
| 25 April 2008 | Amended | Converted to new review format. |
| 21 May 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Many thanks to Jeremy Coid and Peter Joseph for their contributions to the original version of this review.
Clive Adams, John Rathbone, Mark Fenton and Tessa Grant of the Cochrane Schizophrenia Group for their support and assistance.
Data and analyses
Comparison 1. CMHT versus STANDARD CARE (all diagnoses).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Death ‐ medium term (up to 12 months) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 any cause | 3 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.17, 1.34] |
| 1.2 suicide or suspicous circumstances | 3 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.11, 2.21] |
| 1.3 due to 'physical' ill health | 3 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.13, 1.95] |
| 2 Leaving study early ‐ medium term (up to 12 months) | 2 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.68, 1.78] |
| 3 Satisfaction with Service Questionnaire ‐ Not satisfied ‐ medium term (up to 12 months) | 1 | 87 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.18, 0.79] |
| 4 Service use: 1. Admitted to hospital ‐ medium term (up to 12 months) | 3 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.67, 0.97] |
| 5 Service use: 2. Duration of psychiatric hospital admission ‐ medium term (up to 12 months) | Other data | No numeric data | ||
| 6 Service use: 3. Use of Accident and Emergency and general hospital ‐ medium term (up to 12 months) | 3 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.66, 1.12] |
| 7 Service use: 4. Contact with Primary Care ‐ medium term (up to 12 months) | 3 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.80, 1.11] |
| 8 Service use: 5. Contact with social services ‐ medium term (up to 12 months) | 2 | 255 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.58, 1.01] |
| 9 Mental state. Average endpoint scores ‐ medium term (up to 12 months) (CPRS, high score = bad) | Other data | No numeric data | ||
| 10 Social functioning. Police contacts ‐ medium term (up to 12 months) | 2 | 255 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.07 [1.08, 3.97] |
1.1. Analysis.
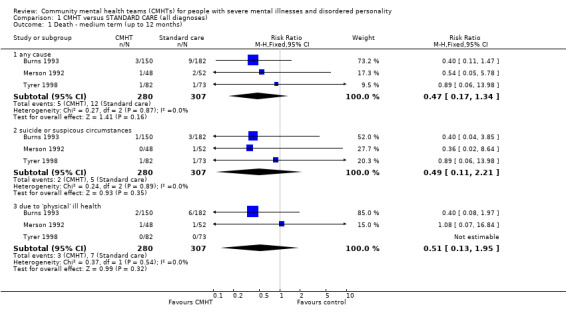
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 1 Death ‐ medium term (up to 12 months).
1.2. Analysis.
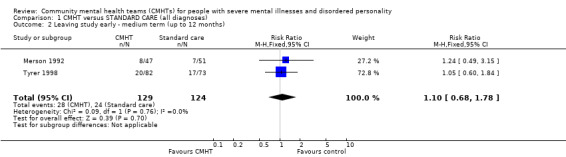
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 2 Leaving study early ‐ medium term (up to 12 months).
1.3. Analysis.
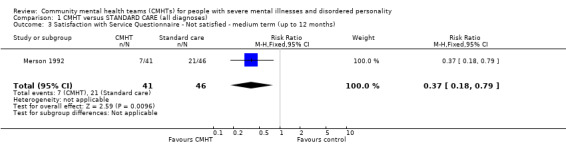
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 3 Satisfaction with Service Questionnaire ‐ Not satisfied ‐ medium term (up to 12 months).
1.4. Analysis.
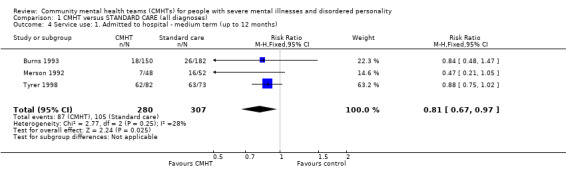
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 4 Service use: 1. Admitted to hospital ‐ medium term (up to 12 months).
1.5. Analysis.
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 5 Service use: 2. Duration of psychiatric hospital admission ‐ medium term (up to 12 months).
| Service use: 2. Duration of psychiatric hospital admission ‐ medium term (up to 12 months) | |||||
|---|---|---|---|---|---|
| Study | Intervention | Mean | SD | N | notes |
| Burns 1993 | CMHT | 35.2 | 46.7 | 94 | This data is not intention to treat numbers, original N's are CMHT150, SC 182. |
| Burns 1993 | Standard care | 41.3 | 29.8 | 78 | |
1.6. Analysis.
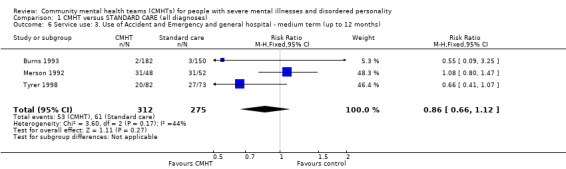
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 6 Service use: 3. Use of Accident and Emergency and general hospital ‐ medium term (up to 12 months).
1.7. Analysis.
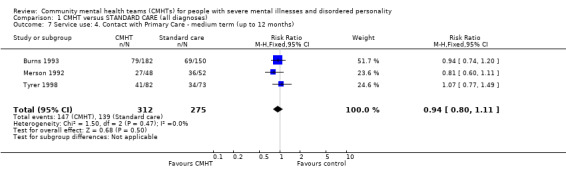
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 7 Service use: 4. Contact with Primary Care ‐ medium term (up to 12 months).
1.8. Analysis.
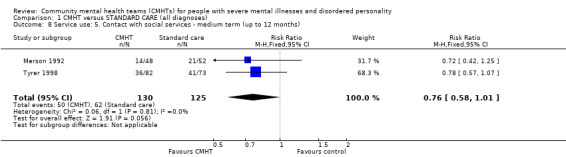
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 8 Service use: 5. Contact with social services ‐ medium term (up to 12 months).
1.9. Analysis.
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 9 Mental state. Average endpoint scores ‐ medium term (up to 12 months) (CPRS, high score = bad).
| Mental state. Average endpoint scores ‐ medium term (up to 12 months) (CPRS, high score = bad) | ||||
|---|---|---|---|---|
| Study | Intervention | mean | SD | N |
| Merson 1992 | CMHT | 22.8 | 11.00 | 48 |
| Merson 1992 | Standard care | 23.60 | 14.10 | 52 |
1.10. Analysis.
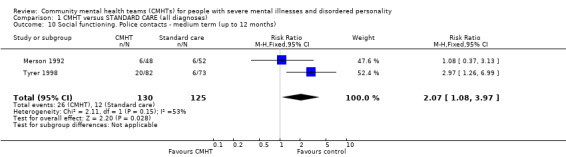
Comparison 1 CMHT versus STANDARD CARE (all diagnoses), Outcome 10 Social functioning. Police contacts ‐ medium term (up to 12 months).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Burns 1993.
| Methods | Allocation: randomised, using a random number sequence, before applying inclusion criteria. Blindness: single (researchers). Follow up: 12 months. Analysis: ITT. | |
| Participants | Diagnosis: psychotic disorders 55/158 (35%), (PSE, CATEGO). History: 79 had previous psychiatric history. N=332*. Age: mean 40 years. Sex: 75 M, 97 F. Race: 157 white. Setting: inner city. | |
| Interventions | 1. Community treatment teams: multi‐disciplinary community teams, home based assessment within two weeks of referral, joint visits; not crisis intervention and no mention of 24 hour cover; no restriction on case loads. N=94 'entering study'. 2. Standard hospital treatment: usually OPD with occasional home visits. N=78 'entering' study. |
|
| Outcomes | Death.
Leaving study early.
Time in hospital.
Duration of hospital care. Unable to use ‐ Satisfaction of care. (no data). Psychiatric symptoms: PSE, BPRS, and clinical interview (no SD). Social functioning. (no SD). Social services use. (no usable data). Costs of care. (no usable data). |
|
| Notes | *Randomisation of all referrals to mental health services randomised, routine or urgent. 172 'entered study'. Not in treatment with psychiatric services in previous 12 months. Substantial numbers excluded, dropped or lost after randomisation but before first assessment. Six people died from natural causes (4 standard care group; 2 CMHT group) ‐ subtracted from original number randomised. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Merson 1992.
| Methods | Allocation: randomised, sealed envelopes, stratified by previous contacts with psychiatric services. Blindness: double; blinding tested +3 = no blinding, ‐ 3 = perfect blinding: mean 1.95. N=87. Follow up: 3 months. Analysis: ITT. | |
| Participants | Diagnosis: schizophrenia (38), mood disorders (32), neurotic (25), other (5). Personality disordered 50 (ICD‐10), 35 (PAS)**. History: 51% previous psychiatric contact. N=100*. Age: median 32. Sex: 40 M, 60 F. Setting: inner city. | |
| Interventions | 1. Community focused multidisciplinary team, open referral, in‐home assessments, collaboration maintained with already involved agencies, clinical decisions by team consensus. N=48. 2. Standard hospital treatment : usually outpatient clinic assessments with occasional home visits. N=52. |
|
| Outcomes | Death.
Leaving study early.
Satisfaction with care (Satisfaction with Service Questionnaire, displayed as not very satisfied with care).
Hospital admission.
Duration of hospital care.
Team utilisation (mean visits).
Social functioning/networks (Network Schedule, SFQ).
Police contacts. Unable to use ‐ Psychiatric symptoms: BAS, MADRAS (no SD). |
|
| Notes | *Randomisation at point of referral to psychiatric emergency services (A&E presentations, urgent GP or social work referrals), not currently in contact with psychiatric services. Additional diagnosis of personality disorder made & data presented on this subgroup. 2 'natural cause' deaths subtracted from original number randomised. **Data relating to those with personality disorder presented in separate comparison. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Tyrer 1998.
| Methods | Allocation: randomised, sealed envelopes. Blindness: single (researchers). Follow up: 12 months. | |
| Participants | Diagnosis: schizophrenia (86), bipolar affective disorder (20), depressive disorder (24), other (25) (DSM‐III, ICD‐10, OPCRIT). History: >1 admission in last 3 years. N=155*. Age: range 16‐65 years. Setting: urban. | |
| Interventions | 1. 'Community team': multidisciplinary community based team, treatment at home\other appropriate setting. N=82. 2. Standard hospital treatment: care plans & reviews organised from hospital base. N=73. |
|
| Outcomes | Death**.
Hospital admission.
Leaving the study early.
Days in hospital.
Police contacts. Unable to use ‐ Mental state: BAS, CPRS, HADS, MADRAS (no SD). Social Function: SFQ (no SD). Global assessment: GAF (no SD). Costs of care. (no usable data). |
|
| Notes | * Randomisation at point of discharge from hospital.
** 1 accidental death considered 'suspicious circumstances' for this review.
Contact reviewer = trial author. No data collected on patient satisfaction. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
General F1 psychosis = Medical Subject Heading Codes. ICD‐10 = 10th revision of the International Classification of Diseases. OPD = Out patient department. SCL ‐ Syndrome Check List SCALES
Mental state BAS = Brief Rating Scale for Anxiety. BPRS = Brief Psychiatric Rating Scale. CPRS = Comprehensive Psychpathological Rating Scale. MADRAS = Montgomery and Asberg Depression Rating Scale. OPCRIT = Operational Criterea for diagnosing Severe Mental Illness. PEF = Psychiatric Evaluation Form. PSE = Present State Examination (to measure clinical symptoms).
Family buden FEF = Family Evaluation Form.
Functioning GAF = Global Assessment of Functioning HSRS = Health Sickness Rating Scale (to measure a persons functioning). PEF = Psychiatric Evaluation Form. SFQ = Social Functioning Questionaire. SFS = Social Functioning Schedule.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Audini 1994 | Allocation: randomised. Participants: people with serious mental illness. Intervention: assertive community treatment versus standard care. |
| Bedell 1989 | Allocation: not randomised, matched controls. |
| Bond 1988 | Allocation: randomised. Participants: people with serious mental illness. Intervention: assertive community treatment versus standard care. |
| Bond 1990 | Allocation: randomised. Participants: people with serious mental illness. Intervention: assertive community treatment versus 'drop in' centre. |
| Cannon 1985 | Allocation: randomised. Participants: people with schizophrenia. Intervention: hospital care versus residential programme. |
| Coelho 1993 | Allocation: randomised. Participants: people with mild to moderate developmental disability, together with a DSM III diagnosis of mental illness. Interventions: intensive case management versus standard care. |
| Connolly 1996 | Allocation: not randomised. |
| Crosby 1993 | Allocation: not randomised. |
| Cuffel 1994 | Allocation: not randomised. |
| Curtis 1998 | Allocation: randomised. Participants: people discharged from an inpatient psychiatry service. Intervention: case management, not CMHT. |
| De‐Cangas 1995 | Allocation: randomised. Participants: people with serious mental illness. Interventions: assertive community treatment versus standard care. |
| Dean 1993 | Allocation: not randomised. |
| Dick 1991 | Allocation: randomised. Participants: people with severe depression or anxiety. Intervention: day hospital versus out patient treatment. |
| Dixon 1997 | Allocation: randomised. Participants: people with mental illnesses. Intervention assertive community treatment, not CMHT. |
| Essock 1995 | Allocation: randomised. Participants: people with serious mental illness. Interventions: assertive community treatment versus case management. |
| Fenton 1979 | Allocation: randomised. Participants: people with serious mental illness. Interventions: crisis intervention versus standard hospital care. |
| Ferguson 1992 | Allocation: not randomised, case control study. |
| Ford 1995 | Allocation: randomised. Participants: people with severe mental illness. Intervention: intensive case management versus standard care. |
| Franklin 1987 | Allocation: randomised. Participants: people with chronic mental illness. Interventions: case management versus standard care. |
| Friedman 1964 | Allocation: not randomised, series of preliminary project reports |
| Griffiths 1974 | Allocation: randomised. Participants: people with psychotic illness and work problems. Interventions: rehabilitation unit versus standard care. |
| Hargreaves 2006 | Allocation: unclear. Participants: people with severe mental illness. Intervention assertive community treatment, not CMHT |
| Harrison‐Read 2002 | Allocation: randomised. Participants: people with serious mental illness and heavy service users. Interventions: enhanced case management/assertive community treatment versus standard CMHT care. |
| Heitger 1995 | Allocation: not randomised. |
| Hoult 1981 | Allocation: randomised. Participants: serious mental illness. Interventions: crisis intervention versus standard hospital care. |
| Huf 2002 | Allocation: randomised. Participants: people with mental illnesses requiring IMI. Intervention: medication, not CMHT. |
| Husted 1994 | Allocation: not randomised, repeated measures within subject design. |
| Jerrell 1995 | Allocation: randomised. Participants: people with serious mental illness. Intervention: intensive case management versus program of assertive treatment versus standard CMHT. |
| Kluiter 1990 | Allocation: randomised. Participants: people with serious mental illness. Interventions: day hospital versus standard care. |
| Knapp 1994 | Allocation: randomised. Participants: people with serious mental illness. Intervention: assertive community treatment. |
| Kovess 1988 | Allocation: not randomised. |
| Krupinski 1984 | Allocation: not randomised. |
| Kuldau 1977 | Allocation: randomised. Participants: people with mental illness. Interventions: therapeutic community type approach versus rapid discharge with pre‐discharge planning (both inpatient treatment programmes). |
| Kwakwa 1995 | Allocation: not randomised. |
| Lafave 1996 | Allocation: randomised. Participants: people with mental illness. Interventions: assertive community treatment versus hospital based care. |
| Leff 1996 | Allocation: not randomised. |
| Linn 1977 | Allocation: randomised. Participants: people with mental illness. Interventions: foster care preparation and placement versus continued hospitalisation. |
| Linszen 2001 | Allocation: unclear. Participants: people with first episode schizophrenia. Intervention: two forms of psychosocial interventions with medication. |
| Littrell 1995 | Allocation: not randomised. |
| Locker 1984 | Allocation: not randomised, case control design. |
| Macias 1994 | Allocation: randomised. Participants: people with serious mental illness. Interventions: case management and psychosocial rehabilitation versus psychosocial rehabilitation. |
| Marks 1994 | Allocation: randomised. Participants: people with serious mental illness. Interventions: assertive community treatment versus hospital based care. |
| Marshall 1995 | Allocation: randomised. Participants: people with serious mental illness. Intervention: case management versus standard care. |
| McClary 1989 | Allocation: not randomised. |
| McCrone 1994 | Allocation: randomised. Participants: people with serious mental illness. Interventions: community intensive support team versus generic CPN care. |
| Modcrin 1988 | Allocation: randomised. Participants: people with chronic mental illness. Interventions: developmental aquisition model of case management versus standard case management. |
| Muijen 1992a | Allocation: randomised. Participants: people with serious mental illness. Interventions: assertive community treatment versus standard care. |
| Muijen 1992b | Allocation: randomised. Participants: people with serious mental illness. Interventions: assertive community treatment versus standard care. |
| Muijen 1994 | Allocation: randomised. Participants: people with serious mental illness. Intervention: intensive CPN support versus generic CPN care. |
| Nordentoft 2002 | Allocation: randomised. Participants: people with a first diagnosis of schizophrenia. Intervention: modified assertive community treatment. |
| Pasamanick 1964 | Allocation: randomised. Participants: people with schizophrenia. Intervention: drugs versus placebo, with home care. |
| Paykel 1982 | Allocation: randomised. Participants: people with serious mental illness. Interventions: CPN care versus standard out patient care. |
| Piper 1993 | Allocation: randomised. Participants: people with mental illnesses. Interventions: day treatment versus no treatment, not CMHT. |
| Polak 1976 | Allocation: randomised. Participants: people requiring psychiatric hospitalisation. Interventions: community based therapeutic environments versus standard hospital care. |
| Power 2002 | Allocation: randomised. Participants: people with early psychosis. Interventions: assertive community treatment versus standard care. |
| Quinlivin 1995 | Allocation: randomised. Participants: serious mental illness. Interventions: intensive case management versus traditional case management versus standard care. |
| Rosenheck 1995 | Allocation: randomised. Participants: people with a mental illness. Interventions: intensive psychiatric community care versus standard care. |
| Ruphan 1992 | Allocation: randomised. Participants: people with serious mental illness. Interventions: day hospital treatment versus standard care. |
| Rushton 1990 | Allocation: not randomised, review. |
| Sands 1994 | Allocation: not randomised, case control study. |
| Santiago 1985 | Allocation:randomised. Participants: people with a major mental illness. Interventions: treatment network team versus standard care (inpatient and CMHT). |
| Schene 1993 | Allocation: randomised. Participants: people referred for inpatient treatment. Interventions: day treatment versus inpatient care. |
| Sellwood 1999 | Allocation: randomised. Participants: people with schizophrenia. Interventions: outpatient rehabilitation versus home based rehabilitation, not CMHT. |
| Slavinsky 1982 | Allocation: randomised. Participants: people receiving long term psychiatric care. Interventions: nurse lead social support programme versus medication. clinics. |
| Smith 1974 | Allocation: not randomised, matched pairs design. |
| Smith 1975 | Allocation: not randomised. |
| Solomon 1994 | Allocation: randomised. Participants: people with serious mental illness. Interventions: assertive community treatment versus intensive case management versus standard care. |
| Solomon 1995a | Allocation: randomised. Participants: people with major mental illness. Interventions: consumer case management versus professional case management. |
| Solomon 1995b | Allocation: randomised. Participants: people with severe mental illness. Interventions: assertive community treatment versus forensic intensive case management versus standard care. |
| Solomon 1995c | Allocation: randomised. Participants: major mental illness diagnosis. Interventions: consumer case management versus professional case management. |
| Stein 1975 | Allocation: randomised. Participants: people with chronic mental illness. Interventions: training in community living case versus standard care. |
| Tyrer 1995 | Allocation: randomised. Participants: people with vulnerable psychiatric patients. Interventions: care programming approach versus standard follow up. |
| vanMinnen 1997 | Allocation: randomised. Participants: people with mental retardation and mental illness. Intervention: assertive community treatment versus hospital care. |
| Walsh 2001 | Allocation: randomised. Participants: people with established psychotic illness. Intervention: intensive case management versus standard case management. |
| Wiersma 1991 | Allocation: randomised. Participants: people with schizophrenia. Interventions: specialised day centre versus hospital care. |
| Wilkinson 1995 | Allocation: not randomised, cohort study. |
| Wirshing 2001 | Allocation: randomised. Participants: people with schizophrenia. Interventions: two types of psycho‐education programmes. |
| Wood 1995 | Allocation: not randomised, matched group design. |
| Zhang 1994 | Allocation: not randomised, case control study. |
| Zimmer 1985 | Allocation: randomised. Participants: elderly chronically ill / terminally ill. |
ACT‐ Assertive Community Treatment CPN ‐ Community Psychiatric Nurse. CMHT‐ community mental health team. IMI‐ intramusular medication injection.
Contributions of authors
Sheda Simmonds ‐ protocol formulation, searching, study selection, data extraction and assimilation, report writing, review maintenance.
Peter Tyrer ‐ acquisition of funding, protocol formulation, study selection, data extraction and assimilation, report writing, review maintenance.
Sarah Marriot ‐ protocol formulation, study selection, report writing.
Jeremy Coid ‐ protocol formulation, author contact, study selection, report writing.
Peter Joseph ‐ protocol formulation, author contact, study selection.
Sources of support
Internal sources
Imperial College School of Medicine, London, UK.
North West London Mental Health Services NHS Trust, London, UK.
St Bartholomew's Hospital, London, UK.
Royal London School of Medicine and Dentistry, London, UK.
External sources
North Thames Regional Health Authority, London, UK.
Declarations of interest
None.
Edited (no change to conclusions)
References
References to studies included in this review
Burns 1993 {published data only}
- Burns T, Beadsmoore A, Bhat AV, Oliver A. A controlled trial of home‐based acute psychiatric services: I. Clinical and social outcome. British Journal of Psychiatry 1993;163:49‐54. [DOI] [PubMed] [Google Scholar]
- Burns T, Raftery J. Cost of Schizophrenia in a randomized trial of home‐based treatment. Schizophrenia bulletin 1991;17(3):407‐10. [DOI] [PubMed] [Google Scholar]
- Burns T, Raftery J, Beadsmoore A, McGuigan S, Dickson M. A controlled trial of home‐based acute psychiatric services. II: Treatment patterns and costs. British Journal of Psychiatry 1993;163:55‐61. [DOI] [PubMed] [Google Scholar]
Merson 1992 {published and unpublished data}
- Merson S, Tyrer P, Carlen D, Johnson T. The cost of treatment of psychiatric emergencies: a comparison of hospital and community services. Psychological Medicine 1996;26:727‐34. [DOI] [PubMed] [Google Scholar]
- Merson S, Tyrer P, Onyett S, Lack S, Birkett P, Lynch S, Johnson T. Early intervention in psychiatric emergencies: A controlled clinical trial. Lancet 1992;339:1311‐4. [DOI] [PubMed] [Google Scholar]
- Tyrer P, Merson S, Onyett S, Johnson T. The effect of personality disorder on clinical outcome, social networks and adjustment: a controlled clinical trial of psychiatric emergencies. Psychological Medicine 1994;24:731‐40. [DOI] [PubMed] [Google Scholar]
Tyrer 1998 {published data only}
- Gandhi N, Tyrer P, Evans K, McGee A, Lamont A, Harrison‐Read P. A randomized controlled trial of community‐oriented and hospital oriented care for discharged psychiatric patients: influence of personality disorder on police contacts. Journal of Personality Disorders 2001;15(1):94‐102. [DOI] [PubMed] [Google Scholar]
- Tyrer P, Evans K, Gandhi N, Lamont O, Harrison‐Reed P, Johnson T. Randomised controlled trial of two models of care for discharched psychiatric patients. BMJ 1998;316:106‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Audini 1994 {published data only}
- Audini B, Marks IM, Lawrence RE, Connolly J. Home‐based versus out‐patient/in‐patient care for people with serious mental illness: Phase II of a controlled study. British Journal of Psychiatry 1994;165:204‐10. [DOI] [PubMed] [Google Scholar]
Bedell 1989 {published data only}
- Bedell J, Ward JC. An intensive community‐based treatment alternative to state hospitalization. Hospital and Community Psychiatry 1989;40:533‐5. [DOI] [PubMed] [Google Scholar]
Bond 1988 {published data only}
- Bond GR, Miller LD, Krumwied RD, Ward RS. Assertive case management in three CMHCs: A controlled study. Hospital and Community Psychiatry 1988;39:411‐8. [DOI] [PubMed] [Google Scholar]
Bond 1990 {published data only}
- Bond GR, Witheridge TF, Dincin J, Wasmer D, Webb J, Graaf Kaser R. Assertive community treatment for frequent users of psychiatric hospitals in a large city: a controlled study. American Journal of Community Psychology 1990;18:865‐91. [DOI] [PubMed] [Google Scholar]
Cannon 1985 {unpublished data only}
- Cannon N. A cost effectiveness analysis of a controlled experiment comparing treatment alternatives for chronically mentally ill patients. PhD dissertation submited to the Brandeis University, USA 1985:156.
Coelho 1993 {published data only}
- Coelho RJ, Kelley PS, Deatsman‐Kelley C. An experimental investigation of an innovative community treatment model for persons with a dual diagnosis (DD/MI). Journal of Rehabilitation 1993;59:37‐42. [Google Scholar]
Connolly 1996 {published data only}
- Connolly J, Marks I, Lawrence R, McNamee G, Muijen M. Observations from community care for serious mental illness during a controlled study. Psychiatric Bulletin 1996;20:3‐7. [Google Scholar]
Crosby 1993 {published data only}
- Crosby C. Health Services Research Unit (HSRU) University College of North Wales: Evaluation of the strategy for mental illness services in North Wales. Journal of Mental Health UK 1993;2:85‐8. [Google Scholar]
Cuffel 1994 {published data only}
- Cuffel BJ. Violent and destructive behavior among the severely mentally ill in rural areas: evidence from Arkansas' community mental health system. Community Mental Health Journal 1994;30:495‐504. [DOI] [PubMed] [Google Scholar]
Curtis 1998 {published data only}
- Curtis JL, Millman EJ, Struening EL, D'Ercole A. Does outreach case management improve patients quality of life. Psychiatric services 1998; March;49:351‐54. [DOI] [PubMed] [Google Scholar]
Dean 1993 {published data only}
- Dean C, Phillips J, Gadd EM, Joseph M, England S. Comparison of community based service with hospital based service for people with acute, severe psyciatric illness. British Medical Journal 1993; August;307(6902):473‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
De‐Cangas 1995 {published data only}
- De‐Cangas JPC. Psychiatric nursing assertive case management: a comprehensive evaluation of the effectiveness and outcomes of hospital based treatment versus a nurse directed assertive case management program. International Journal of Psychiatric Nursing Research 1995;1:72‐81. [Google Scholar]
Dick 1991 {published data only}
- Dick PH, Sweeney ML, Crombie IK. Controlled comparison of day‐patient and out‐patient treatment for persistent anxiety and depression. British Journal of Psychiatry 1991;158:24‐7. [DOI] [PubMed] [Google Scholar]
Dixon 1997 {published data only}
- Dixon L, Weiden P, Torres M, et al. Assertive community treatment and medication compliance in the homeless mentally ill. American J of Psychiatry 1997;154(9):1302‐04. [DOI] [PubMed] [Google Scholar]
Essock 1995 {published data only}
- Essock SM, Kontos N. Implementing assertive community treatment teams. Psychiatric Services 1995;46:679‐83. [DOI] [PubMed] [Google Scholar]
Fenton 1979 {published data only}
- Fenton FR, Tessier L, Contandriopoulos AP, Nguyen H, Struening EL. A comparative trial of home and hospital psychiatric treatment: financial costs. Canadian Journal of Psychiatry 1982;27:177‐87. [DOI] [PubMed] [Google Scholar]
- Fenton FR, Tessier L, Struening EL. A comparative trial of home and hospital psychiatric care: One‐year follow‐up. Archives of General Psychiatry 1979;36:1073‐9. [DOI] [PubMed] [Google Scholar]
- Fenton FR, Tessier L, Struening EL, Smith FA, Benoit C, Contandriopoulos AP. A two‐year follow‐up of a comparative trial of the cost‐effectiveness of home and hospital psychiatric treatment. Canadian Journal of Psychiatry 1984;29:205‐11. [DOI] [PubMed] [Google Scholar]
- Smith F, Fenton F, Benoit C, Barzell E, Tessier L. Home care treatment of acutely ill psychiatric patients. Canadian Psychiatric Association Journal 1978;23(2):73‐6. [DOI] [PubMed] [Google Scholar]
Ferguson 1992 {published data only}
- Ferguson B, Cooper S, Brothwell J, Markantonakis A. The clinical evaluation of a new community psychiatric service based on general practice psychiatric clinics. British Journal of Psychiatry 1992;160:493‐7. [DOI] [PubMed] [Google Scholar]
Ford 1995 {published data only}
- Ford R, Beadsmoore A, Ryan P, Repper J, Craig T, Muijen M. Providing the safety net: Case management for people with a serious mental illness. Journal of Mental Health 1995;4:91‐7. [Google Scholar]
Franklin 1987 {published data only}
- Franklin JL, Solovitz B, Mason M, Clemons JR, Miller GE. An evaluation of case management. American Journal of Public Health 1987;77:674‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Friedman 1964 {published data only}
- Friedman T, Becker A, Weiner L. The psychiatric home treatment service: Preliminary report of five years of clinical experience. American Journal of Psychiatry 1964;120:782‐8. [DOI] [PubMed] [Google Scholar]
Griffiths 1974 {published data only}
- Griffiths RD. Rehabilitation of chronic psychotic patients. Psychological Medicine 1974;4:316‐25. [MEDLINE: ; PMID 4427978] [PubMed] [Google Scholar]
Hargreaves 2006 {published data only}
- Hargreaves WA, Ja DY, Gee M. Assertive community treatment can be cost‐effective for schizophrenia. 39th Annual Meeting of the American College of Neuropsychopharmacology. 2000; Dec.
Harrison‐Read 2002 {published data only}
- Harrison‐Read P, Lucas B, Tyrer P, Ray J, Shipley K, Simmonds S, Knapp M, Lowin A, Patel A, Hickman M. Heavy users of acute psychiatric beds: randomized controlled trial of enhanced community management in an outer London borough. Psychological Medicine 2002;32(3):403‐16. [MEDLINE: ; 11989986] [DOI] [PubMed] [Google Scholar]
Heitger 1995 {published data only}
- Heitger B, Saameli W. Effectiveness of treatment in a psychiatric day hospital [Wirksamkeit einer psychiatrischen Tagesklinikbehandlung. Eine empirische Untersuchung aus den Psychiatrischen Diensten des Regionalspitals Thun]. Schweizer Archiv fur Neurologie und Psychiatrie 1995;146:33‐8. [PubMed] [Google Scholar]
Hoult 1981 {published data only}
- Hoult J. Psychiatric hospital versus community treatment: The results of a randomised trial. Australian and New Zealand Journal of Psychiatry 1983;17:160‐7. [DOI] [PubMed] [Google Scholar]
- Hoult J, Reynolds I. Schizophrenia: A comparative trial of community orientated and hospital orientated psychiatric care. Acta Psychiatrica Scandinavica 1984;69:359‐72. [DOI] [PubMed] [Google Scholar]
- Hoult J, Reynolds I, Charbonneau C, Powis M, Coles P, Briggs J. A controlled study of psychiatric hospital versus community treatment ‐ the effect on relatives. Australia and New Zealand Journal of Psychiatry 1981;15:323‐8. [DOI] [PubMed] [Google Scholar]
- Hoult J, Rosen A, Reynolds I. Community orientated treatment compared to psychiatric hospital orientated treatment. Social Science and Medicine 1984;18:1005‐10. [DOI] [PubMed] [Google Scholar]
- Reynolds I, Hoult JE. The relatives of the mentally ill: A comparative trial of community‐oriented and hospital‐oriented psychiatric care. Journal of Nervous and Mental Disease 1984;172:480‐9. [PubMed] [Google Scholar]
Huf 2002 {published data only}
- Huf G, Coutinho ESF, Adams CE. TREC III. The protocol and progress of TREC. Schizophrenia Research 2002;53(3 Suppl.1):187. [MEDLINE: ; PMID 11479066]11479066 [Google Scholar]
Husted 1994 {published data only}
- Husted J, Wentler SA, Bursell A. The effectiveness of community support programs for persistently mentally ill in rural areas. Community Mental Health Journal 1994;30:595‐600. [DOI] [PubMed] [Google Scholar]
Jerrell 1995 {published data only}
- Jerrell JM. Toward managed care for persons with severe mental illness: implications from a cost‐effectiveness study. Health Affairs 1995;14(3):197‐207. [MEDLINE: ; PMID 7498892] [DOI] [PubMed] [Google Scholar]
Kluiter 1990 {published data only}
- Kluiter H, Giel R, Nienhuis FJ, Ruphan M, Wiersma D. Feasibility of a day‐treatment program for the severely mentally ill; first results of a randomized experiment [Hallbaarheid van dagbehandeling voor de opnamepopulatie van een algemeen psychiatrisch ziekenhuis. Berichten vanuit het substitutieproject drenthe]. Tijdschrift voor Psychiatrie 1990;32:625‐39. [Google Scholar]
Knapp 1994 {published data only}
- Knapp M, Beecham J, Koutsogeorgopoulou V, Hallam A, Fenyo A, Marks I, Connolly J, Audini B, Muijen M. Service use and costs of Home‐based versus hospital‐based care for people with serious mental illness. British Journal of Psychiatry 1994;165(6):506‐12. [DOI] [PubMed] [Google Scholar]
Kovess 1988 {published data only}
- Kovess V, Lafleche M. How do teams practise community psychiatry?. Canada's Mental Health 1988;36:9‐16. [PubMed] [Google Scholar]
Krupinski 1984 {published data only}
- Krupinski J, Lippmann L. Multidisciplinary or nondisciplinary: Evaluation of staff functioning in a community mental health centre. Australian and New Zealand Journal of Psychiatry 1984;18:172‐8. [DOI] [PubMed] [Google Scholar]
Kuldau 1977 {published data only}
- Kuldau JM, Dirks SJ. Controlled evaluation of a hospital‐originated community transitional system. Archives of General Psychiatry 1977;34:1331‐40. [DOI] [PubMed] [Google Scholar]
Kwakwa 1995 {published data only}
- Kwakwa J. Alternatives to hospital‐based mental health care. Nursing Times 1995;91:38‐9. [PubMed] [Google Scholar]
Lafave 1996 {published data only}
- Lafave HG, Souza HR, Gerber GJ. Assertive community treatment of severe mental illness: A Canadian experience. Psychiatric Services 1996;47:757‐9. [DOI] [PubMed] [Google Scholar]
Leff 1996 {published data only}
- Leff J, Trieman N, Gooch C. Team for the assessment of psychiatric services (TAPS) project 33: Prospective follow‐up study of long‐stay patients discharged from two psychiatric hospitals. American Journal of Psychiatry 1996;153:1318‐24. [DOI] [PubMed] [Google Scholar]
Linn 1977 {published data only}
- Linn MW, Caffey EM, Klett CJ, Hogarty G. Hospital vs community (foster) care for psychiatric patients. Archives of General Psychiatry 1977;34:78‐83. [DOI] [PubMed] [Google Scholar]
Linszen 2001 {published data only}
- Linszen D, Dingemans P, Lenior Marie. Early intervention and a five year follow up in young adults with a short duration of untreated psychosis: ethical implications. Schizophrenia Research 2001;51(1):55‐61. [MEDLINE: ; PMID 11479066] [DOI] [PubMed] [Google Scholar]
Littrell 1995 {published data only}
- Littrell KH, Freeman LY. Maximizing psychosocial interventions. Journal of the American Psychiatric Nurses Association 1995;1:214‐8. [Google Scholar]
Locker 1984 {published data only}
- Locker D, Rao B, Weddell JM. Evaluating community care for the mentally handicapped adult: A comparison of hostel, home and hospital care. Journal of Mental Deficiency Research 1984;28:189‐98. [DOI] [PubMed] [Google Scholar]
Macias 1994 {published data only}
- Macias C, Kinney R, Farley OW, Jackson R, Vos B. The role of case management within a community support system: partnership with psychosocial rehabilitation. Community Mental Health Journal 1994;30:323‐39. [DOI] [PubMed] [Google Scholar]
Marks 1994 {published data only}
- Marks IM, Connolly J, Muijen M, Audini B, McNamee G, Lawrence RE. Home‐based versus hospital‐based care for people with serious mental illness. British Journal of Psychiatry 1994;164:179‐94. [DOI] [PubMed] [Google Scholar]
Marshall 1995 {published data only}
- Marshall M, Lockwood A, Gath D. Social services case‐management for longterm mental disorders: A randomised controlled trial. Lancet 1995;345:409‐12. [DOI] [PubMed] [Google Scholar]
McClary 1989 {published data only}
- McClary S, Lubin B, Evans C, Watt B. Evaluation of a community treatment program for young adult schizophrenics. Special Issue: Post‐traumatic stress disorder. Journal of Clinical Psychology 1989;45:806‐8. [DOI] [PubMed] [Google Scholar]
McCrone 1994 {published data only}
- McCrone P, Beecham J, Knapp M. Community psychiatric nurse teams: cost‐effectiveness of intensive support versus generic care. British Journal of Psychiatry 1994;165:218‐21. [DOI] [PubMed] [Google Scholar]
Modcrin 1988 {published data only}
- Modrcin M, Rapp CA, Poertner J. The evaluation of case management services with the chronically mentally ill. Evaluation and Program Planning 1988;11:307‐14. [DOI] [PubMed] [Google Scholar]
Muijen 1992a {published data only}
- Muijen M, Marks IM, Connolly J, Audini B. The Daily Living Programme: Preliminary comparison of community versus hospital‐based treatment for the seriously mentally ill facing emergency admission. British Journal of Psychiatry 1992;160:379‐84. [DOI] [PubMed] [Google Scholar]
Muijen 1992b {published data only}
- Muijen M, Marks I, Connolly J, Audini B. Home based care and standard hospital care for patients with severe mental illness: a randomised controlled trial. British Medical Journal 1992;304:749‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Muijen 1994 {published data only}
- Muijen M, Cooney M, Strathdee G, Bell R, Hudson A. Community psychiatric nurse teams: intensive support versus generic care. British Journal of Psychiatry 1994;165:211‐7. [DOI] [PubMed] [Google Scholar]
Nordentoft 2002 {published data only}
- Nordentoft M, Jeppesen P, Kassow P, Abel M, Petersen L, Thorup A, Cristensen T, Øhlenschlæger J, Jørgensen P. Opus‐project: a randomised controlled trial of integrated psychiatric treatment in first‐episode psychosis‐clinical outcome improved. Schizophrenia Research 2002;53(3 Suppl.1):51. [MEDLINE: ; PMID 11479066]11479066 [Google Scholar]
Pasamanick 1964 {published data only}
- Pasamanick B, Scarpitti F, Lefton M, Dinitz S, Wernert J, McPheeters H. Home versus Hospital care for schizophrenics. The Journal of the American Medical Association 1964;187(3):177‐81. [DOI] [PubMed] [Google Scholar]
Paykel 1982 {published data only}
- Paykel ES, Mangen SP, Griffith JH, Burns TP. Community psychiatric nursing for neurotic patients: A controlled trial. British Journal of Psychiatry 1982;140:573‐81. [DOI] [PubMed] [Google Scholar]
Piper 1993 {published data only}
- Piper WE, Rosie JS, Azim HFA, Joyce AS. A randomized trial of psychiatric day treatment for patients with affective and personality disorders. Hospital and Community Psychiatry 1993;44:757‐63. [DOI] [PubMed] [Google Scholar]
Polak 1976 {published data only}
- Polak PR, Kirby MW. A model to replace psychiatric hospitals. Journal of Nervous and Mental Disease 1976;162:13‐22. [DOI] [PubMed] [Google Scholar]
Power 2002 {published data only}
- Power P, Craig T, Garety P, Rahaman N, Fornells‐Ambrojo M, Colbert S. A randomised controlled trial of assertive community follow‐up in early psychosis: preliminary results. Schizophrenia Research 2002;53(3 Suppl.1):42. [MEDLINE: ; PMID 11479066]11479066 [Google Scholar]
Quinlivin 1995 {published data only}
- Quinlivan R, Hough R, Crowell A, Beach C, Hofstetter R, Kenworthy K. Service utilization and costs of care for severely mentally ill clients in an intensive case management program. Psychiatric Services 1995;46:365‐71. [DOI] [PubMed] [Google Scholar]
Rosenheck 1995 {published data only}
- Rosenheck R, Neale M, Leaf P, Milstein R, Frisman L. Multisite experimental cost study of Intensive Psychiatric Community Care. Schizophrenia Bulletin 1995;21:129‐40. [DOI] [PubMed] [Google Scholar]
Ruphan 1992 {published data only}
- Ruphan M, Kluiter H, Nienhuis FJ, Wiersma D, Giel R. Day‐treatment versus inpatient treatment for psychiatric patients in need of admission: Longitudinal effects on social role‐functioning studied by means of randomized trial [Opnamevervangende dagbehandeling bij psychiatrische patienten: Effecten op het sociale functioneren, twee jarr na de start van een gecontroleerd experiment]. Tijdschrift voor Psychiatrie 1992;34:571‐83. [Google Scholar]
Rushton 1990 {published data only}
- Rushton A. Community‐based versus hospital‐based care for acutely mentally ill people. British Journal of Social Work 1990;20:373‐83. [Google Scholar]
Sands 1994 {published data only}
- Sands RG, Cnaan RA. Two modes of case management: assessing their impact. Community Mental Health Journal 1994;30:441‐57. [DOI] [PubMed] [Google Scholar]
Santiago 1985 {published data only}
- Santiago JM, McCall‐Perez F, Bachrach LJ. Integrated services for chronic mental patients: theoretical perspective and experimental results. General Hospital Psychiatry 1985;7:309‐15. [MEDLINE: ; PMID 4065549] [DOI] [PubMed] [Google Scholar]
Schene 1993 {published data only}
- Schene AH, Wijngaarden B, Poelijoe NW, Gersons BPR. The Utrecht comparative study on psychiatric day treatment and inpatient treatment. Acta Psychiatrica Scandinavica 1993;87:427‐36. [DOI] [PubMed] [Google Scholar]
Sellwood 1999 {published and unpublished data}
- Seiiwood W, Thomas C, Tarrier N, Jones S, Clewes J, James A, Welford M, Palmer J, McCarthy E. A randomized controlled trial of home‐based rehabilitation versus outpatient based rehabilitation for patients suffering from chronic schizophrenia. Social Psychiatry and Psychiatric Epidemiology 1999;34(5):250‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Sellwood W, Thomas C, Tarrier N, Jones S, Clewes J, James A, Welford M, Hilton J, McCarthy E. A randomized controlled trial of home based rehabilitation versus outpatient based rehabilitation for patients suffering from chronic schizophrenia. unpublished manuscript. [MEDLINE: ] [DOI] [PubMed]
Slavinsky 1982 {published data only}
- Slavinsky AT, Krauss JB. Two approaches to the management of long‐term psychiatric outpatients in the community. Nursing Research 1982;31:284‐9. [PubMed] [Google Scholar]
Smith 1974 {published data only}
- Smith WG, Kaplan J, Siker D. Community mental health and the seriously disturbed patient: First admission outcomes. Archives of General Psychiatry 1974;30:696. [DOI] [PubMed] [Google Scholar]
Smith 1975 {published data only}
- Smith WG. Evaluation of the clinical services of a regional mental health center. Community Mental Health Journal 1975;11:47‐57. [DOI] [PubMed] [Google Scholar]
Solomon 1994 {published data only}
- Solomon P, Draine J, Meyerson A. Jail recidivism and receipt of community mental health services. Hospital and Community Psychiatry 1994;45:793‐7. [DOI] [PubMed] [Google Scholar]
Solomon 1995a {published data only}
- Solomon P, Draine J. Consumer case management and attitudes concerning family relations among persons with mental illness. Psychiatric Quarterly 1995;66:249‐61. [DOI] [PubMed] [Google Scholar]
Solomon 1995b {published data only}
- Solomon P, Draine J. One ‐year outcomes of a randomized trial of case management with seriously mentally ill clients leaving jail. Evaluation Review 1995;19:256‐73. [Google Scholar]
Solomon 1995c {published data only}
- Solomon P, Draine J. One‐year outcomes of a randomized trial of consumer case management. Evaluation and Program Planning 1995;18:117‐27. [Google Scholar]
Stein 1975 {published data only}
- Stein LI, Test MA, Marx AJ. Alternative to the hospital: A controlled study. American Journal of Psychiatry 1975;132:517‐22. [DOI] [PubMed] [Google Scholar]
Tyrer 1995 {published data only}
- Tyrer P, Morgan J, Horn E, Jayakody M, Evans K, Brummell R. A randomised controlled study of close monitoring of vulnerable psychiatric patients. Lancet 1995;345:756‐9. [DOI] [PubMed] [Google Scholar]
vanMinnen 1997 {published data only}
- Minnen A, Hoogduin C, Broekman T. Hospital vs outreach treatment of patients with mental retardation and psychiatric disorders: a controlled study. Acta Psychiatrica Scandinavica 1997;95(6):515‐22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Walsh 2001 {published data only}
- Walsh E, Gilvarry C, Samele C, Harvey K, Manley C, Tyrer P, Creed F, Murray R, Fahy T. Reducing violence in severe mental illness: randomised controlled trial of intensive case management compared with standard care. BMJ 2001;323:1093‐6. [MEDLINE: ; PMID 11701572] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiersma 1991 {published data only}
- Wiersma D, Kluiter H, Nienhuis FJ, Ruphan M. Costs and benefits of day treatment with community care for schizophrenic patients. Schizophrenia Bulletin 1991;17:411‐9. [DOI] [PubMed] [Google Scholar]
Wilkinson 1995 {published data only}
- Wilkinson G, Piccinelli M, Falloon I, Krekorian H, McLees S. An evaluation of community‐based psychiatric care for people with treated long‐term mental illness. British Journal of Psychiatry 1995;167:26‐37. [DOI] [PubMed] [Google Scholar]
Wirshing 2001 {published data only}
- Wirshing DA, Wirshing WC, Rossoto E, Gonzalez L, Watson J, Ballon J, McNally C. The community re‐entry program for schizophrenia: correlates of treatment response. Annual Meeting of the American Psychiatric Association; 2001 May 5‐10; LA, USA. Marathon Multimedia, 2001. [MEDLINE: ; PMID 11290639]11290639
Wood 1995 {published data only}
- Wood K, Anderson J. The effect on hospital admissions of psychiatric case management involving general practitioners: preliminary results. Australia and New Zealand Journal of Psychiatry 1995;29:223‐9. [DOI] [PubMed] [Google Scholar]
Zhang 1994 {published data only}
- Zhang M, Yan H, Phillips MR. Community‐based psychiatric rehabilitation in Shanghai. Facilities, services, outcome, and culture‐specific characteristics. British Journal of Psychiatry 1994;165(supplement):70‐9. [PubMed] [Google Scholar]
Zimmer 1985 {published data only}
- Zimmer JG, Groth‐Juncker A, McCusker J. A randomized controlled study of a home health care team . . . physician, nurse practitioner, and social worker. American Journal of Public Health 1985;75:134‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Gater 1997 {published and unpublished data}
- Gater R, Goldberg D, Jackson G. The care of patients with chronic schizophrenia: a comparison between two services. Psychological medicine 1997;27:1325‐36. [DOI] [PubMed] [Google Scholar]
Tan 2004 {published data only}
- Tan B. The Analysis of curative effect of schizophrenia patients treated in the community. Journal of Hubei Institute for nationalities meical edition 2004;21(4):17‐19. [Google Scholar]
Additional references
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313:1200. [CMHT020600] [DOI] [PMC free article] [PubMed] [Google Scholar]
Asberg 1978
- Asberg M, Montgomery SA, Perris C, Schalling D, Sedvall GA. Comprehensive Psychopathological Rating Scale. Acta Psychiatrica Scandinavica 1978;27(Suppl 271):5‐27. [DOI] [PubMed] [Google Scholar]
Bennett 1991
- Bennett D, Freeman H. Principles and prospect. In: Bennett D, Freeman H editor(s). Community Psychiatry. Edinburgh: Churchill Livingstone, 1991:1‐39. [Google Scholar]
Bland 1997
- Bland JM. Statistics notes. Trials randomised in clusters. BMJ 1997;315:600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bouras 1986
- Bouras N, Turnell G, Brough DI, Watson JP. Model for integration of community psychiatric and primary care. Journal of the Royal College of General Practitioners 1986;36:62‐6. [PMC free article] [PubMed] [Google Scholar]
Cicceti 1981
- Cicceti D, Sparrow SS. Developing criteria for the rating of specific items in a given inventory. American Journal of Mental Deficiency 1981;86:127‐37. [PubMed] [Google Scholar]
Coid 1994
- Coid J. Failure in community care: psychiatry's dilemma. BMJ 1994;308:805‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Creed 1996
- Creed F. Evaluation of community treatments for acute psychiatric illness. In: Tyrer P, Creed F editor(s). Community Psychiatry in Action: Analysis and Prospects. Cambridge: Cambridge University Press, 1996:11‐27. [Google Scholar]
Divine 1992
- Divine GW, Brown JT, Frazier LM. The unit of analysis error in studies about physicians' patient care behavior. Journal of General Internal Medicine 1992;7(6):623‐9. [DOI] [PubMed] [Google Scholar]
DoH 1990
- Department of Health. Community care in the next decade and beyond. London: HMSO, 1990. [Google Scholar]
Donner 2002
- Donner A, Klar N. Issues in the meta‐analysis of cluster randomized trials. Statistics in Medicine 2002;21:2971‐80. [DOI] [PubMed] [Google Scholar]
Dowell 1993
- Dowell DA, Ciarlo JA. Overview of the community mental health centres program from an evaluation perspective. American Journal of Psychiatry 1983;19:95‐125. [DOI] [PubMed] [Google Scholar]
Friedman 1983
- Friedman RC, Aronoff MS. History of suicidal behaviour in depressed borderline in‐patients. American Journal of Psychiatry 1983;140:1023‐6. [DOI] [PubMed] [Google Scholar]
Garvey 1980
- Garvey MJ, Spoden F. Suicide attempts in antisocial personality disorder. Comprehensive Psychiatry 1980;21:146‐9. [DOI] [PubMed] [Google Scholar]
Gulliford 1999
- Gulliford MC. Components of variance and intraclass correlations for the design of community‐based surveys and intervention studies: data from the Health Survey for England 1994. American Journal of Epidemiology 1999;149:876‐83. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2005
- Higgins JPT, Green S editors. Cochrane Collaboration Handbook. Cochrane Handbook for systematic reviews of interventions. 4.2.5. Cichester UK: John Wiley and sons Ltd, May 2005. [Google Scholar]
Holloway 2001
- Holloway F. Invited commentary on: Community mental health team management in severe mental illness. British Journal of Psychiatry 2001;178:503‐5. [DOI] [PubMed] [Google Scholar]
Jadad 1996
- Jadad A, Moore A, Carroll D, Jenkinson C, Reynolds DJM, Gavanagh DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary?. Controlled Clinical Trials 1996;17:1‐12. [DOI] [PubMed] [Google Scholar]
Joy 2006
- Joy CB, Adams CE, Rice K. Crisis intervention for people with severe mental illnesses. Cochrane Database of Systematic Reviews 2006, Issue 4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Marshall 1998
- Marshall M, Gray A, Lockwood A, Green R. Case management for people with severe mental disorders (Cochrane Review). Cochrane Database of Systematic Reviews 1998, Issue 2. [DOI] [PubMed] [Google Scholar]
Marshall 2000a
- Marshall M, Lockwood A. Assertive community treatment for people with severe mental disorders. Cochrane Database of Systematic Reviews 2000, Issue 2. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Marshall 2000b
- Marshall M, Lockwood A, Bradley C, Adams C, Joy C, Fenton M. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. British Journal of Psychiatry 2000;176:249‐52. [DOI] [PubMed] [Google Scholar]
Marshall 2004
- Marshall M, Lockwood A. Early Intervention for psychosis. Cochrane Database of Systematic Reviews 2004, Issue 2. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Marshall 2006
- Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database of Systematic Reviews 2006, Issue 4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Merson 1992b
- Merson S, Tyrer P, Onyett S, Lack S, Birkett P, Lynch S, et al. Early intervention in psychiatric emergencies: a controlled clinical trial. Lancet 1992;339:1311‐4. [DOI] [PubMed] [Google Scholar]
Miller 1993
- Miller RJ, Zadolinnyj K, Hafner RJ. Profiles and predictors of assaultiveness for different psychiatric ward populations. American Journal of Psychiatry 1993;150:1368‐73. [DOI] [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman D. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomized trials. JAMA 2001;285:1987‐91. [DOI] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
Soares 2004
- Soares, H.P. Daniels, S, Kumar. A, et al. (2004). Bad reporting does not mean bad methods for randomised trials: observational study of randomised trials performed by the Radiation Therapy Oncology Group. British Medical Journal 2004;328:22‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tyrer 2003
- Tyrer P, Simmonds S. Treatment models for those with severe mental illness and comorbid personality disorder. British Journal of Psychiatry 2003;182(suppl 44):s15‐s18. [DOI] [PubMed] [Google Scholar]
Ukoumunne 1999
- Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ. Methods for evaluating area‐wide and organistation‐based intervention in health and health care: a systematic review. Health Technology Assessment 1999;3(5):1‐75. [PubMed] [Google Scholar]
References to other published versions of this review
Simmonds 2001
- Simmons S, Coid J, Joseph P, Marriott S, Tyrer P. Community mental health team management in severe mental illness: a systematic review. British Journal of Psychiatry 2001;178:497‐502. [DOI] [PubMed] [Google Scholar]
Tyrer 2000
- Tyrer P, Coid J, Simmonds S, Joseph P, Marriott S. Community mental health teams (CMHTs) for people with severe mental illnesses and disordered personality. Cochrane Database of Systematic Reviews 2000, Issue 2. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


