Abstract
Background
Many vaginal dilator therapy guidelines advocate routine vaginal dilation during and after pelvic radiotherapy to prevent stenosis (abnormal narrowing of the vagina). The UK Gynaecological Oncology Nurse Forum recommend dilation “three times weekly for an indefinite time period”. The UK patient charity Cancer Backup advises using vaginal dilators from two to eight weeks after the end of radiotherapy treatment. Australian guidelines recommend dilation after brachytherapy “as soon as is comfortably possible” and “certainly within four weeks and to continue for three years or indefinitely if possible”. However, dilation is intrusive, uses health resources and can be psychologically distressing. It has also caused rare but very serious damage to the rectum.
Objectives
To review the benefits and harms of vaginal dilation therapy associated with pelvic radiotherapy for cancer.
Search methods
Searches included the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2008, Issue 4), MEDLINE (1950 to 2008), EMBASE (1980 to 2008) and CINAHL (1982 to 2008).
Selection criteria
Any comparative randomised controlled trials (RCT) or data of any type which compared dilation or penetration of the vagina after pelvic radiotherapy treatment for cancer.
Data collection and analysis
The review authors independently abstracted data and assessed risk of bias. We analysed the mean difference in sexual function scores and the risk ratio for non-compliance at six weeks and three months in single trial analyses. No trials met the inclusion criteria.
Main results
Dilation during or immediately after radiotherapy can, in rare cases, cause damage and there is no persuasive evidence from any study to demonstrate that it prevents stenosis. Data from one RCT showed no improvement in sexual scores in women who were encouraged to practice dilation. Two case series and one comparative study using historical controls suggest that dilation might be associated with a longer vaginal length but these data cannot reasonably be interpreted to show that dilation caused the change in the vagina.
Authors’ conclusions
Routine dilation during or soon after cancer treatment may be harmful. There is no reliable evidence to show that routine regular vaginal dilation during or after radiotherapy prevents the late effects of radiotherapy or improves quality of life. Gentle vaginal exploration might separate the vaginal walls before they can stick together and some women may benefit from dilation therapy once inflammation has settled but there are no good comparative supporting data.
Medical Subject Headings (MeSH): Constriction, Pathologic [etiology; therapy], Dilatation [adverse effects; *instrumentation], Pelvis, Radiotherapy [adverse effects; methods], Rupture [etiology], Time Factors, Vagina [injuries; *radiation effects]
MeSH check words: Female, Humans
BACKGROUND
Description of the condition
Cancer of the uterus and cervix often involves treatment with pelvic radiotherapy. A permanent side effect of radiotherapy is vaginal dryness, vascular and tissue damage, thinning of the epithelium, and atrophy of the vagina with a reduction in elasticity and development of fibrosis (Abitol 1974; Cartwright 1995). About a third of women suffer from vaginal stenosis (obstruction by scar tissue) after pelvic radiotherapy (Abitol 1974; Bertelesen 1983;Hartman 1972; Seibel 1982; Vasicka 1958) and altered vaginal epithelium (skin) causing sexual dysfunction (Denton 2000), but the range of reported incidence varies from 1.2% (Eltabbakh 1977) to 88% (Hartman 1972). The anatomical deformity of the vagina contributes negatively to a woman’s well-being. Any therapy that minimises the impact of radiation damage might improve sexual recovery for women after treatment. Another important reason to prevent vaginal stenosis, even for women who are not or do not plan to be sexually active, is that the vagina needs to be kept patent (open) to enable adequate examination in the five-year follow up period to detect treatable re-occurrence of the cancer.
Description of the intervention
Surveys (White 2006) show that vaginal dilation with radiotherapy is now standard British practice and the UK guidelines from the National Gynaecological Oncology Nurse Forum (UK Nurse Forum 2005) recommend dilation “three times weekly for an indefinite time period”. The UK patient charity Cancer Backup (Cancer Backup 2010) advises patients that they “can minimise or prevent stenosis by using vaginal dilators from 28 weeks after the end of their radiotherapy”. Australian practice is variable (Lancaster 2004) despite Australian guidelines that recommend encouraging dilation after brachytherapy “as soon as comfortably possible” and “certainly within four weeks” “for three years or indefinitely if possible”. USA practice guidelines are different and the NCI 2009 comment that “doctors may advise their patients not to have intercourse during radiation therapy”. Most centres offer a vaginal dilator manufactured as a medical device. Whilst some use graded glass, vulcanite or opaque plastic models, the majority provide dilator sets of four graduated sizes moulded in rigid plastic or silicone (Amielle 2010; Medintim 2010; Soul 2010).
How the intervention might work
Skin will grow when it is stretched. This is the principal behind tissue expansion plastic surgery. Observational studies of women born with no vagina (vaginal agenesis) clearly show that the vagina can be stimulated to stretch and re-grow if pressure is applied to the skin. Fingers, a dilator, stent, phallus or any other phallic shaped device can be used. It has been assumed that dilation could be used after or during radiotherapy to reduce the consequential fibrosis. Dilation might separate the adhesions formed by the denuded epithelium, thus possibly preventing stenosis (Faithfull 2003; Hassey-Dow 1992; Krumm 1993; Rice 2000). However, it is also plausible that persistently interfering with the vagina during the inflammatory phase of radiotherapy treatment might cause additional scarring and promote additional damage, both physically and psychologically. Furthermore, translating the physiology of normal young epithelial cells and assuming that this new growth potential applies to irradiated skin may be naive. It is possible that regular stretching of recently irradiated and inflamed skin causes micro tears and the associated additional inflammation could cause more (not less) scarring.
Why it is important to do this review
Routine vaginal dilation during and after radiotherapy is advocated in many guidelines, many review articles (Cartwright 1995;Crowther 1994; Davidson 2003; Gosselin 2001; Grigsby 1995;Hartman 1972; Lamberti 1979; Pountney 2005; Wilmoth 2000) and by patient advocates. For example, Cancer Backup 2010 advises patients that they “can minimise or prevent stenosis by using vaginal dilators from two to eight weeks after the end of their radiotherapy”. Routine vaginal dilation is advocated by 97% (64/ 65) of UK radiotherapy centres but only 48% of women feel they can comply with instructions (Faithfull 2003; White 2004). It is important to know if the intervention during or after radiotherapy is beneficial because the intervention is expensive in terms of nursing and therapy radiographer time. In addition, the psycho-sexual sequelae of coercing women to dilate their vagina during painful treatment may be traumatic. Finally, fistulae have occurred after treatment (Hoffman 2003). It follows that a full systematic review is required to guide clinicians who may want to prescribe adjuvant dilation associated with pelvic radiotherapy. The previous Cochrane Review (Denton 2000) relied on the paper byDecruze 1999 to conclude that dilation “was sufficient to endorse the widespread use of vaginal dilators”.
The treatment and prevention of stenosis is an important aspect of cancer care and this review examines all the available data on dilation practice to inform clinicians on the value of this strategy.
OBJECTIVES
To review the benefits and harms of different types of vaginal dilation methods offered to women treated by pelvic radiotherapy for cancer.
METHODS
Criteria for considering studies for this review
Types of studies
Initially we intended to focus on randomised controlled trials (RCTs), quasi-RCTs and cohort studies where the comparability of cohorts had been established or existing confounding factors adjusted. Subsequently, we repeated and expanded the search to capture case control retrospective studies, longitudinal surveys and case histories. A summary of studies containing any comparative data on vaginal dilation following radiotherapy or any characteristics of data on vaginal dilation following radiotherapy can be found in Table 1 and Table 2.
Table 1.
Summated findings from every study containing any data on vaginal dilation following radiotherapy
| Author/date | Outcomes | Notes | Risk of bias | Authors’ assessment |
|---|---|---|---|---|
| Poma 1980 | 5 case reports | 5 women who developed radiation stenosis who have never had treatment or intercourse during or after therapy. They were parous, aged between 47 and 55 and their radiotherapy had been between 3 and 9 years previously (5 cases at 8, 8, 9, 3 and 9 years). Women were taught to massage their vagina many years after their radiotherapy with an oestrogen cream (2 g) twice a day until vaginal depth became evident | Case histories only | Grade V Excluded study |
| Robinson 1999 | Global sexual health scores Knowledge about sexuality, cancer and vaginal dilation compliance |
The authors present a regression analysis demonstrating that intervention was associated with greater compliance but this only affected younger women. In the younger age group (less than 41.5 median age of the population), 5.6% in the control group complied compared to 44% in the intervention group. In the older group compliance was 55.6% in the control group versus 48% in the intervention group. This demonstrates that the younger women did comply and therefore randomisation has succeeded in creating 2 distinct groups, one who rarely dilated and one that complied with instructions to dilate. Mean sexual healthy scores (SD) were the same in the 2 groups. The sexual health score in the experimental group was 0.401 (0.081) compared to 0.513 (0.126) in the group who rarely dilated (control group). This was independent of age | The original paper may have been edited for brevity and did not describe how participants were randomly allocated or how contamination was minimised. However, the lead author confirms that appropriate techniques were applied. Random allocation involved sealed numbered envelopes sequenced by random number table and there were no incomplete data sets. Allocation was not concealed and the timing of sexual health score is not defined | Grade Ib Excluded study |
| Decruze 1999 | Clinical assessment of stenosis at 1 year after radiotherapy | There were 35 women in each group. 20 had stenosis who did not use a stent compared to 4 who had stenosis who did use a stent. The 4 that did use a stent who had stenosis were noteworthy because one was too frightened to use, one was confused, and 2 did not understand how to use it. Once these 4 women had been encouraged to use it properly the authors say that the stenosis improved but no further details were given | The age was different in the 2 groups with those having no stent being on average 5 years older and there is no description of how women were allocated the stent. Allocation was not concealed from the assessors and neither assessors or patients were blinded to the technique, therefore the risk of bias has to be judged as high | Grade IV Excluded study |
| Bruner 1993 | Vaginal length measured at pre-treatment, 6,12, 24 and beyond 24 months | This study shows a correlation between vaginal shortening and type of treatment. It does not provide data linking coital frequency to ultimate vaginal length. These data have been requested from the authors | No data available from the authors | Grade IV and no relevant data Excluded study |
| Jeffries 2006 | Compliance with the use of dilators | This is a randomised trial allocating psychoeducational intervention specifically designed to increase compliance with vaginal dilation. 26 women were exposed to an information-motivation-behavioural skills model of enhancing compliance with behavioural change 21 women in the control group were given 30 minutes of instruction and the appropriate equipment in the last week of therapy | The data collected were restricted to information on compliance | Grade Ia but no relevant data Excluded study |
| Sobotkowski 2006 | Vaginal length, vaginal occlusion and vaginal vault wall synechiae | Vaginal length was not different after treatment (mean length of the study group (n = 16) of 6. 5 cm +/− 2.02 and the control group (n = 15) mean 5.67 +/− 3.04. There were 4 vaginal occlusions in the control group and one in the study group. There were 4 vaginal wall synechiae in the control group and 2 in the study group. The authors concluded that the speculum and mitomycin application made no difference to vaginal length | The authors do not describe how the cases were selected, the observers and the participants were not blinded to treatment and it was not a randomised study | Grade IIIb Excluded study |
| Velaskar 2007 | Vaginal length measured before and after a programme of dilation therapy | Case series describing 89 of 100 women with stage 3 cervix cancer treated by radiotherapy. 45 also had concomitant chemotherapy. A measurement was taken 6 to 10 weeks after completing radiotherapy. Dilation therapy was taught and measurements were reassessed 4, 8 and 12 months later. Median length increased from 6 to 9 to 10 and 10 cm again over the 4 repeated measures. It is noteworthy that 46 of 89 women were able to accommodate larger dilators after 1 year of follow up | The authors do not describe how the cases were selected, how the measurements were taken, the observers and the participants were not blinded to treatment and readers are left wondering if the change in length is just a measurement artefact. It is possible that women tolerated greater penetration depth with experience and exposure to measurement and exposure to a foreign body in the vagina. The most important problem is that there is no control group | Grade IV Excluded study |
Table 2.
Characteristics of studies containing any comparative data on vaginal dilation following radiotherapy
| Author/date | Methods | Participants | Interventions | When was the intervention |
|---|---|---|---|---|
| Robinson 1999b | Randomised trial | 32 women with stage 1 or 2 cervical or endometrial carcinoma who were treated with radiotherapy |
Control arm: a clinical consultation and literature containing information on normal sexual responses, vaginal dryness, the use of lubricants, Kegel exercises, vaginal dilators and alternative positions for coitus, presumably with instruction to dilate the vagina after treatment Interventional arm: a clinical consultation and literature containing information on normal sexual responses, vaginal dryness, the use of lubricants, Kegel exercises, vaginal dilators and alternative positions for coitus presumably with instruction to dilate the vagina after treatment plus 2 separate 1.5-hour cycle education sessions guided by information motivation behavioural skills model (informing women how to use dilators, motivating them to use them and teaching them how to use them effectively) |
The stent was given to women immediately after competition of treatment Women were assessed at 6 weeks after treatment and 3 monthly thereafter |
| Decruze 1999 | Unmatched, unblinded, uncontrolled case series with historical controls | 70 women treated by either external beam radiotherapy, vaginal caesium only or combination of intrauterine vaginal caesium and external beam radiotherapy | Retrospective review of stenosis 1 year after radiotherapy in women who had used the authors own design of vaginal stent compared to uncontrolled group who never used a vaginal stent | After completion of all treatment including intracavity radiotherapy |
| Bruner 1993 | Cohort study | 90 women treated with intra-cavity radiation implants with or without external beam radiotherapy and with or without radical or total abdominal hysterectomy for either cervical or uterine carcinomas (stages 1 to 3) consecutively from 1989 to 1992 | Sexual intercourse frequency. These data have been requested from the authors but they have been unable to provide this | - |
| Sobotkowski 2006 | Non-randomised comparison | 31 women with advanced cervix cancer treated by radiotherapy and brachytherapy. Vaginal length measured before and after treatment | 16 women were chosen to have mitomycin prophylaxis applied topically to the top of the vagina. Application of the drug took place 2 and 4 weeks after completion of radiotherapy by the use of a dry speculum and the application of a mitomycin soaked gauze placed in the vaginal vault for about 4 minutes | 2 and 4 weeks after the completion of the radiotherapy |
Types of participants
The systematic examination of the literature focused on women confirmed to have a pelvic malignancy who had received pelvic radiotherapy as part of their treatment schedule. This could be either primary radiotherapy or postoperative radiotherapy, with or without chemotherapy or palliative therapy.
Types of interventions
We considered both medical devices and commercially available devices. This included all types of vaginal dilation therapy such as digital dilation with lubrication, speculums, medical devices or vibrators.
Types of outcome measures
Primary outcomes
Sexual satisfaction (Jensen 2004).
Vaginal trauma later redefined as vaginal stenosis.
Secondary outcomes
Concordance with the intervention (data extracted as non-compliance).
Any other measure of sexual function at any time.
Psychosexual morbidity at any time.
Quality of life (QoL) (EORTC 2008) at any follow-up visit.
LENT-SOMA score of stenosis (Pavy 1995) at any time.
Pain and infection were not considered as outcomes because we did not imagine any such data would be available and indeed did not find any, however these might be included as outcomes in any future update.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases:
the Cochrane Gynaecological Cancer Collaborative Review Group’s Trial Register;
the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2008, Issue 4);
MEDLINE (from 1950 to end 2008);
EMBASE (from 1980 to end 2008);
CINAHL (from 1982 to end 2008); and
Google and Google Scholar (up to November 2008).
The MEDLINE, CENTRAL and EMBASE search strategies are listed in Appendix 1, Appendix 2 and Appendix 3. Intervention terms were excluded because their inclusion might have lost some relevant papers. We conducted searches to identify RCTs and non RCTs comparing interventions related to vaginal dilation therapy and pelvic radiotherapy. The search strategy identified studies in all languages and when necessary we intended to review non-English language papers and translate them for potential inclusion in the review.
Searching other resources
Unpublished and grey literature
We contacted the main investigators of any relevant ongoing trials for further information, as well as major co-operative trials groups active in this area.
Handsearching
We handsearched reports of conferences in the following sources:
Annual Meeting of the British Gynaecological Cancer Society (BGCS);
Annual Meeting of the International Gynecologic Cancer Society (IGCS);
Annual Meeting of European Society of Medical Oncology (ESMO);
Annual Meeting of the American Society of Clinical Oncology (ASCO); and
Annual Meeting of the European Society of Gynaecological Oncology (ESGO).
Reference lists and correspondence
We checked the citation lists of included trials and contacted experts in the field to identify further reports of trials. We had personal contact with the following sources:
contact with the Cochrane Gynaecological Cancer Review Group;
contact with the Gynae Oncology Nurse Forum Dilator Subgroup;
letter (via newsletter) to gynaecology patient user group; and
direct e-correspondence with the authors of the included trials.
Data collection and analysis
Selection of studies
The two review authors independently printed and manually reviewed all titles and abstracts retrieved by electronic searching. We excluded those studies which clearly did not meet the inclusion criteria. We obtained copies of the full text of potentially relevant references and assessed these independently. We documented the reasons for exclusion. The intention was to have any disagreements resolved through discussion with a third expert. In future updates of the review we will employ the following methods.
Data extraction and management
For included studies, we will abstract data as recommended in Chapter 7 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). This will include data on the following:
author, year of publication and journal citation (including language);
country;
setting;
inclusion and exclusion criteria;
study methods (trial design, duration, setting, study inclusion criteria);
- study population;
- ○ total number enrolled;
- ○ patient characteristics;
- ○ age;
cancer details at diagnosis;
total number of intervention groups;
type of dilator interventions;
risk of bias in study (see below); and
duration of follow up.
We will extract data on outcomes as below:
For dichotomous outcomes (e.g. psychosexual morbidity, vaginal stenosis) we intend to extract the number of patients in each group who experienced the outcome of interest and the number of patients assessed at endpoint, in order to estimate a relative risk (RR).
For continuous outcomes (e.g. QoL, measure of sexual function), we intend to extract the final value and standard deviation of the outcome of interest and the number of patients assessed at endpoint in each treatment arm at the end of follow up, in order to estimate the mean difference (if trials measured outcomes on the same scale) or standardised mean difference (if trials measured outcomes on different scales) between treatment arms and its standard error.
Where possible, all data extracted will be relevant to an intention-to-treat (ITT) analysis, in which participants will be analysed in the groups to which they were assigned. We will note the time points at which outcomes were collected and reported.
Assessment of risk of bias in included studies
We will assess the risk of bias in included RCTs using the Cochrane Collaboration’s tool and the criteria specified in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). This will include assessment of:
sequence generation;
allocation concealment;
blinding (of participants, healthcare providers and outcome assessors);
incomplete outcome data;
selective reporting of outcomes; and
other possible sources of bias.
We will apply the risk of bias tool independently.
Measures of treatment effect
We will use the following measures of the effect of treatment:
for dichotomous outcomes, we will use the RR; and
for continuous outcomes, we will use the mean difference between treatment arms.
Dealing with missing data
We intend to record the proportion of participants in each intervention arm whose outcomes were not reported at the end of the study.
Assessment of heterogeneity
We will assess heterogeneity between studies by visual inspection of forest plots, by estimation of the percentage heterogeneity between trials which cannot be ascribed to sampling variation (Higgins 2003), by a formal statistical test of the significance of the heterogeneity (Deeks 2001) and, if possible, by subgroup analyses (see below). If there is evidence of substantial heterogeneity, we will investigate and report the possible reasons for this.
Assessment of reporting biases
We will examine funnel plots corresponding to meta-analysis of the primary outcome to assess the potential for small study effects. When there is evidence of small study effects, we will consider publication bias as only one of a number of possible explanations. If these plots suggest that treatment effects may not be sampled from a symmetric distribution, as assumed by the random-effects model, we will perform sensitivity analyses using fixed-effect models.
Data synthesis
If sufficient, clinically similar studies are available we will pool their results in meta-analyses. We will use adjusted summary statistics if available; otherwise we will use unadjusted results.
For time-to-event data, we will pool hazard ratios (HRs) using the generic inverse variance facility of RevMan 5.
For dichotomous outcomes, we will calculate the RR for each study and then pool these.
For continuous outcomes, we will pool the mean differences between the treatment arms at the end of follow up if all trials measured the outcome on the same scale, otherwise we will pool standardised mean differences.
If any trials have multiple treatment groups, we will divide the ‘shared’ comparison group into the number of treatment groups and treat comparisons between each treatment group and the split comparison group as independent comparisons.
We will use random-effects models with inverse variance weighting for all meta-analyses (DerSimonian 1986).
If possible, we will use indirect comparisons, using the methods ofBucher 1997, to compare competing interventions that have not been compared directly with each other.
Subgroup analysis and investigation of heterogeneity
We will perform subgroup analyses, grouping the trials by:
disease-free interval; and
optimal cytoreduction achieved at the primary treatment.
We will consider factors such as age, stage, length of follow up and adjusted/unadjusted analysis in the interpretation of any heterogeneity.
Sensitivity analysis
We will perform sensitivity analyses (i) excluding non-randomised studies if RCTs have been included, (ii) excluding studies at high risk of bias, and (iii) using unadjusted results.
RESULTS
Description of studies
Results of the search
The electronic search identified 246 original papers and many duplicates. A further reference was retrieved by hand cascade searching and was not in the electronic searches (Velaskar 2007). Seven articles were potentially relevant after the title and abstract sift. We retrieved all in full and identified updated versions of relevant trials. The full text screening of these studies found no trials examining our primary outcomes in a high quality comparative trial of dilation versus no dilation. The relevant papers examining any measure of vaginal function are described in the Characteristics of excluded studies. We also identified and excluded two RCTs (Jeffries 2006; Robinson 1999) examining concordance with prescribed therapy. These are described in Appendix 4. Jeffries 2006 focuses on compliance (concordance) as the outcome and contains no data on vaginal anatomy or sexual function. The only value of this analysis is that it supports the primary hypothesis initially proposed by Robinson 1999. This paper shows that women who dilated more often did not improve sexual function scores.
Included studies
There are no trials comparing dilators versus no dilators.
Excluded studies
Two trials (Jeffries 2006: Robinson 1999) randomised a total of 87 women, of whom 79 were assessed at the end of the trials. Both trials come from the same group in Calgary, Alberta (Canada) and involved collaboration with clinical psychologists and oncologists. The purpose of these studies was to test the effectiveness of sophisticated and relatively intensive behaviour modification to see whether they could persuade women to use their dilator therapy more regularly.
Jeffries 2006 was a RCT of a Psychoeducational intervention specifically designed to increase compliance with vaginal dilation. The information-motivation-behavioural skills model of enhancing compliance with behavioural change was the basis for the intervention design. Forty-two sexually active women, 21 to 65 years of age, diagnosed with Stages Ic or III cervical or endometrial cancer, who received pelvic radiotherapy, were randomised to either the experimental Psychoeducational group or the information-only control group. Assessment via questionnaire occurred before treatment and at six-week, six-month, 12-month, 18-month and 24-month follow up. Assessment via interview also occurred at six-month, 12-month, 18-month and 24-month follow up. These data support the strategy that investing in health resources to support women during this phase of their cancer journey does change the uptake of the prescribed therapy.
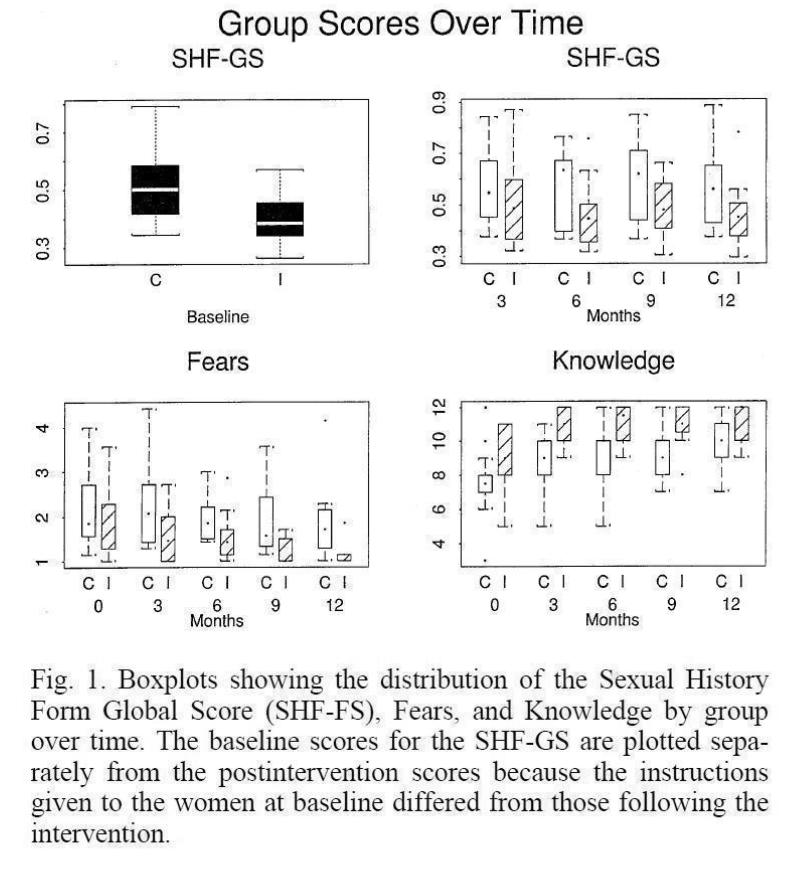
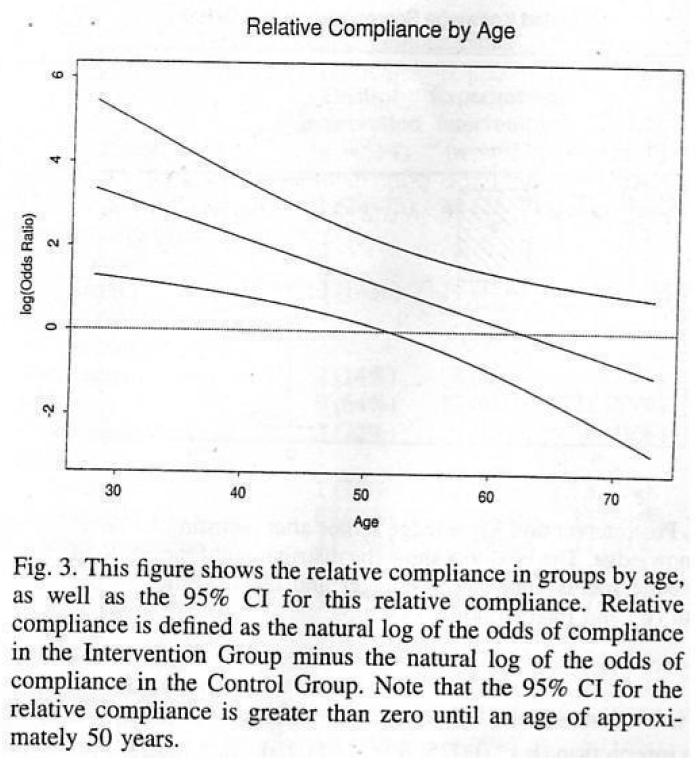
Robinson 1999 measured vaginal dilation compliance but also reported on measures of global sexual health, knowledge about sexuality and cancer, and fears about sexuality after cancer. In this study, 32 women with Stage I or II cervical or endometrial carcinoma who were being treated with radiotherapy were randomised and received either written information and brief counselling or a more intensive Psychoeducational programme based on the information-motivation-behavioural skills model of behaviour change. Women were randomised based on a random number table. The allocation was concealed in opaque sealed envelopes. The post hoc analysis subdivided the groups into older and younger women. This RCT also showed that it is possible to encourage and support women successfully to dilate their vagina. This means that we have a comparison of sexual health scores in women who rarely dilated compared to a group who were more likely to dilate. Admittedly, sexual function is not the authors primary outcome, the sample size is small and over half of the intervention group still failed to comply with the protocol. In addition, this is not a trial where the outcome is measured vaginal length. However, it is sexual function not length that is important to most women (Figure 1; Figure 2).
Figure 1.
Sexual function data extracted from the paper by Robinson 1999, reproduced with permission of the International Journal of Radiation Oncology, Biology, and Physics.
Figure 2.
Compliance data plotted by age extracted from the paper by Robinson 1999, reproduced with permission of the International Journal of Radiation, Oncology, Biology, and Physics.
There are five observational studies that comment on vaginal length but they have been excluded from the formal analysis for one of the following reasons:
no relevant data was available (Bruner 1993);
historical controls were used to compare with the intervention group (Decruze 1999);
was a case series of only five women (Poma 1980);
there is no control group and therefore we do not know what would have happened if dilation had not been suggested (Velaskar 2007);
the focus was on the application of mitomycin with a speculum (Sobotkowski 2006).
The Characteristics of excluded studies table gives details of all the excluded observational studies. In summary, two are reports describing a series of women who dilated their vagina, one report correlates vaginal shortening with type of treatment but does not provide data linking coital frequency to ultimate vaginal length, one is a comparison of outcomes with a new stent compared tohistorical controls, and the other is a study describing the impact of mitomycin applied with a speculum. All examine dilation practice after radiotherapy.
The report by Poma 1980 consists of five case reports. The authors suggest that dilation can work when used for a median of eight years after radiotherapy. These women never had any vaginal penetration following or during their radiotherapy until they were recruited. The five women were able to achieve some vaginal patency after dilation. Poma’s paper may offer limited support for the practice of dilation many years after radiation but offers no evidence to support dilation during cancer treatment. It is not appropriate to translate these data and claim that dilation during or immediately after radiotherapy is beneficial.
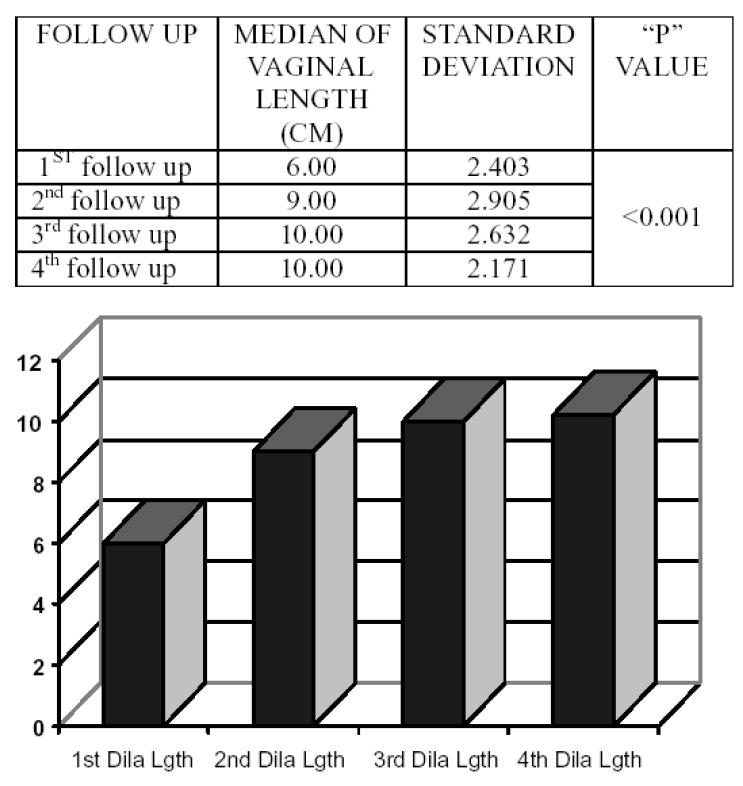
Velaskar 2007 observed vaginal length in 89 of 100 women after radiotherapy for cervix cancer and found that the median vaginal length was 6 cm six to 10 weeks after treatment. It was 9 cm four months later following the introduction of dilation practice. No further significant vaginal length was achieved with continued dilation four and eight months later (median length = 10 cm at these assessments) (Figure 3). Women tolerated a 6 cm measurer on the first vaginal assessment after radiotherapy and tolerated a larger one after four months of dilation experience. The main limitation of these data is that there is no control group to determine outcomes if dilation had not been suggested and we do not know if the reason women accepted a larger measurer in their vagina many months after the treatment was tolerance, familiarity or the resolution of inflammatory radiation oedema.
Figure 3.
Vaginal length data extracted from the paper by Velaskar 2007, reproduced with permission of the the Indian Journal of Occupational Therapy and thanks to Ms. Shruti M. Velaskar.
Bruner 1993 measured vaginal length before treatment, and then six to 12 months, 12 to 24 months and more than 24 months after radiotherapy. This study shows a correlation between vaginal shortening and type of treatment. It does not provide data linking coital frequency to ultimate vaginal length. These data would potentially link natural vaginal dilation frequency (penetrative vaginal sex) with ultimate vaginal length. These data have been requested from the authors but to date they have been unable to provide them.
Decruze 1999 studied 35 women who used a stent designed by the trialists and compared a clinical assessment of stenosis at one year after radiotherapy in a group of 35 historical controls. Twenty historical controls who did not use the same stent had stenosis compared to four who did. The four that did use a stent who had stenosis were noteworthy because one was too frightened to use it, one was confused, and two did not understand how to use it. Once these four women had been encouraged to use it properly the authors reported that stenosis improved, however no further details were given. The report is valuable but limited because the study is not blinded and the control groups are not comparable. They state that their stent made a significant difference to the stenosis rate but stenosis was assessed by the authors who knew that their design of stent had been used. There was no record describing how these women were selected or why they were selected. Bias is compounded because there is a difference in the comparative groups in age, tumour site and type of radiotherapy. Those having no stent were on average five years older. Allocation was not concealed from the assessors and neither assessors nor patients were blinded to the technique. Therefore the risk of bias is probably high. This report is useful but does not meet the criteria to be included in any evidence-based review.
The study by Sobotkowski 2006 is a comparison of 62 women treated by radiotherapy for gynaecological cancer. An unspecified half received the chemotherapeutic drug mitomycin applied to the top of the vagina with a speculum. Mitomycin C prevents DNA cross-linkage and this might affect scarring. However, it is also relevant that it would have been applied via a speculum stretching the vagina on two separate occasions and this might be interpreted to be a form of dilatation soon after radiotherapy. It may have helped prevent any epithelial adhesions. There was no difference in vaginal length with this treatment. This is not a study evaluating dilatation but it is the only one that actually measures vaginal length after an intervention. There is no apparent difference between the control and intervention group (mean length of the study group (n = 16) of 6.5 cm +/− 2.02 and the control group (n = 15) mean 5.67 +/− 3.04). There were four vaginal occlusions in the control group and one in the study group, four vaginal wall synechiae in the control group and two in the study group. The authors concluded that the speculum and mitomycin application made no difference to vaginal length. We do not know how the cases were selected but we do know that the observers and the participants were not blinded to treatment and it was not a RCT.
Risk of bias in included studies
No trials were found and therefore the risk of bias tool was not applied.
Effects of interventions
It was not possible to carry out a meta-analysis from the data collected.
DISCUSSION
Summary of main results
There are no data which unequivocally report that dilation therapy improves any meaningful outcomes for women after pelvic radiotherapy for gynaecological cancer. It is worth exploring why dilation in the acute phase of treatment might be unhelpful. There are five obvious reasons why dilation should be discouraged:
psychological trauma;
trauma during healing increases fibrosis;
anatomical damage;
lack of data to support its use; and
health economics.
The psychological trauma induced by dilation is very variable and cannot be measured in any meaningful qualitative way by a quantitative study. However, simple anecdotes are sufficient to demonstrate that dilation can inflict psychological damage. There is no doubt that genital cancer, particularly cervical carcinoma, is associated with significant psychological distress in some women. This may include unpleasant imagery and fears and they may associate it with a sexually transmitted disease. Anecdotal reports (Hull 2008; Miles 2007) offer a catalogue of testimonies confirming that some women are affected by the psychological stress of being told to dilate their vagina (American Psychiatric Association 2000) and some feel that the ultimate fibrosis is their fault for failing to comply with the instructions of their doctor. Rare but serious physical damage has been reported following dilatation, with case reports of the dilators causing fistula (Hoffman 2003). The health economic consequences are important. Vaginal dilation uses a significant amount of therapy radiographer or nurse specialist time and the cost of vaginal dilators is also an issue. Although this would probably be absorbed in the day to day work of healthcare professionals and may not require additional finances from the purchasing health authorities, it does divert important time resources from other areas of care. Even those with a strong conviction that dilation might be valuable must now accept that there appears to be no evidence to show that the treatment is of benefit.
The studies formally excluded from our protocol are presented in this review to demonstrate the exhaustive nature of the literature search. The objective of this is to demonstrate that persuasive but low quality reports have not been overlooked. None showed an advantage to dilation during or soon after radiotherapy. Of course, the comparison of dilation verses no dilation is unrealistic in the real clinical world. What matters to clinicians is whether women benefit from the recommendation to use dilators. Two trials randomised 79 women and compared Psychoeducational support with standard care in women receiving pelvic radiotherapy for treatment of cervical or endometrial cancer. It was not possible to combine the findings of these two trials with meta-analysis but Baysian principles allow us to conclude that psychological support probably does encourage more women to use their dilator. This means that trials comparing different ways of administering the dilation therapy are probably examining the effect of dilation therapy and we can place more reliance on the conclusions from Robinson 1999. The absence of any difference in sexual function scores in this paper means either that there is no beneficial effect on sexual function from dilation, or if one does exist science has failed to detect it.
Overall completeness and applicability of evidence
We have done everything reasonably possible to identify all studies relevant to this subject. We expanded the search strategy to include data of any sort and included case reports to demonstrate the exhaustive nature of our enquiries. Chinese and Japanese literature has not been trawled or cascade searched but communication with colleagues suggests that there are no relevant studies. The Chinese papers we were able to identify did not contain any relevant data. We would encourage readers who might be aware of further studies to use The Cochrane Library feedback system to bring these to our attention. Robinson 1999 is the only study that we have been able to locate that has any reliable, non-biased data examining sexual function in women who were randomly allocated to more dilation therapy compared to less. This paper does not support dilation therapy. If this systematic review is confirmed to be exhaustive then it follows that there are no reliable data to support the current national recommendations: the practice of adjuvant dilation therapy with radiotherapy is not supported by high quality scientific research.
Quality of the evidence
There appears to be no evidence to form a robust conclusion on the efficacy of dilation therapy. One small trial suggests that dilation therapy does not improve sexual function but the sample size is small, the participants are a mixture of older and younger women and the pathologies are a mixture of cervical and uterine cancer. Sexual function is difficult to measure with any precision, the analysis by intention-to-treat is contaminated by cross-over and the control group received a good standard of care. These features of the trial might have contributed to minimise any potential difference associated with the intervention. Moreover, the power of the trial was probably insufficient to detect any small differences in the groups.
It is pertinent to examine why this review concluded that there is no useful data to support or refute dilation. The likely explanation for the significant paucity of data is the fact that it is uncomfortable for research workers to carry out scientific evaluations of the vagina during radiation treatment. It is a field dominated by nurse specialists and therapy radiographers who, until recently, have had minimal training in research methodology. It is not a field that is exploited by radiation oncologists and it has been particularly difficult in the United Kingdom to suggest a comparative trial to an ethics committee given the current national standard recommending dilation for all women Miles 2010.
There are a handful of observational reports that support adjuvant dilation practice. The main thrust of these reports is that dilation enables a woman to tolerate a larger measurer in her vagina at the end of therapy. This does not mean that the practice works. The increase in apparent vaginal length might occur naturally with the healing process. It is also possible that dilation therapy simply teaches women to accommodate and tolerate larger measuring devices and the reported improvements might be artificial. For these reasons, observations of cases should not be used to conclude that routine dilation practice offers any clinically useful advantage.
Potential biases in the review process
It is important for us to state that we began this review with the prior belief that dilation of the vagina during and after radiotherapy was appropriate management. Numerous texts, guidelines, recommendations and opinions support the practice and we assumed that it prevented vaginal scaring. We had accepted this without critical thought and it has always been the practice in our cancer centre to promote this therapy. On reflection, and with the benefit of hindsight, we were probably biased at the outset of this review and were looking to examine the magnitude of benefit, rather than challenge the premise behind standard UK care. However, this potential bias had the unintended effect of making the authors of this review search all data thoroughly and then repeat the process.
One other potential bias is the heterogeneity of studies with respect to the timing of dilation therapy. The results of asking a woman to dilate her vagina during the acute inflammatory phase, the healing phase and the resolution phase after radiotherapy must be different. For example, Miles 2010a follows national guidelines and this trial involves dilation during and after radiotherapy treatment. Robinson 1999 and Decruze 1999 began dilation therapy with completion of radiotherapy (during the acute inflammatory phase). Sobotkowski 2006 began therapy two and four weeks after the completion of the radiotherapy (in the early healing phase). Finally, Poma 1980 waited a median of eight years before offering dilation (once all inflammation had resolved). It is very difficult to justify combining any data from such heterogenous observations. It is probably important to separate the effects of dilation therapy into dilation therapy either during the time of radiotherapy or dilation months later, once the inflammatory phase has subsided. Theoretically, dilation and associated trauma in the inflammatory phase could exacerbate fibrosis and scarring and there are no reassuring data to oppose this theory. In contrast, the pathophysiology of healing demands that the vagina will respond very differently to dilation years after radiotherapy.
Agreements and disagreements with other studies or reviews
Previous opinion supported the use of routine vaginal dilation. This review challenges this. The obvious counter-claim from the supporters of routine vaginal dilation is that the lack of good evidence is not evidence of no effect. Our failure to show a difference does not mean that one does not exist. Therefore it is worth turning to other data and re-examining the basic principles of healing pathophysiology to examine the current practice of routine vaginal dilation during or immediately after pelvic radiotherapy. One important point is that it is commonly practised. Numerous clinical reviews recommend routine dilation (Cartwright 1995;Crowther 1994; Davidson 2003; Grigsby 1995; Gosselin 2001;Hartman 1972; Lamberti 1979; Pountney 2005; Wilmoth 2000) but do not offer supporting data.
The incidence of stenosis quoted in the literature ranges from just above 1% to just below 90% (Lancaster 2004). This implies that there are differing definitions of stenosis. It is said that vaginal damage from radiotherapy can be minimised by encouraging women to dilate their vagina during and after radiotherapy. It is known that stretching healthy skin stimulates mitosis and the development of new epithelial cells. Plastic surgeons use tissue expanders with good effect in the breast and scalp. Even the vagina can be rebuilt with tissue expansion techniques (Johnson 1991). It is known that girls born without a vagina (Rokitansky syndrome/Mayer-Rokitansky-Küster-Hauser Syndrome or mullerian agenesis) can stimulate it to grow by applying pressure on the mullerian pit (vestibule) (Johnson 1990). However, there is no evidence and no suggestion that this applies to irradiated tissue and the skin of a teenager’s vaginal stem cells has no resemblance to epithelial cells after radical radiation. An alternative argument is to use the basic principles attributable to healing during inflammation. Radiotherapy is associated with cellular damage, subsequent inflammation and moist desquamation. The physical trauma associated with dilation during the healing peri-inflammatory phase is unquantifiable but potentially real. Many woman report bleeding and pain presumably due to tearing of the epithelium. Further trauma induced by dilatation during healing will cause more inflammation and this will recruit more fibroblasts and may induce further scarring. The pathophysiology of dilating the vagina during or soon after radiotherapy is different from dilating many months or years after therapy but it is reasonable to argue that stretching and tearing inflamed skin during or soon after radiotherapy could cause more harm and more scarring.
Numerous clinical reviews recommend routine dilation but do not offer supporting data. It is possible that these recommendations have been uncritical in their acceptance of past teachings based on the observation that dilation helps women born with no vagina and may help women with vaginismus. However, some reviewers do reference their recommendation. Examples includeBurke 1996 who refers the readers to a comparison of American and French practice. This reference is a commentary on the variations between nations and does not offer supporting data for the practice. Krumm 1993 and Lamberti 1979 also advocate dilation and they support their recommendation by referring readers to the 1986 guidelines on implant therapy from Ellis Fischel State cancer centre, Columbia. This reference is a description of local practice and has no supporting data. The previous Cochrane Review (Denton 2000) relied on the paper by Decruze 1999 to conclude that dilation “was sufficient to endorse the widespread use of vaginal dilators”. Decruze 1999 implies that dilation prevents stenosis but critical appraisal reveals that the study examined historical controls who still might have used a dilator and the 35 cases in each arm were not blinded nor perfectly matched.
Not all reviewers accept that dilation is effective. The review byAbitol 1974 is more analytical than most text books. They say that “mechanical dilation of the vagina and the use of topical oestrogens appear to be of doubtful value”. Australian practice is less protocol-driven than UK practice. A survey shows that local practice tends to be dominated by the non-scientific opinion of the leading clinician (Lancaster 2004). USA practice guidelines (NCI 2009) comment that “Doctors may advise their patients not to have intercourse during radiation therapy” and American practice guidelines do not promote dilation therapy.
AUTHORS’ CONCLUSIONS
Implications for practice
The UK Nurse Forum 2005 will question their guidelines advocating dilation as regular routine standard national practice during or soon after radiotherapy because there is no good evidence to support it. It is costly in terms of healthcare time, plausibly associated with greater scar formation rather than less, is associated with case reports of very serious damage following its treatment and is undeniably associated with psychological sequelae for some women. However, gentle exploration of the vagina soon after treatment might identify epithelial adhesions and it is plausible that separation might prevent the fusion of the vaginals walls. It might be reasonable to address the topic of vaginal dilation once the acute inflammatory phase of radiotherapy has settled. This would give the attending practitioner an opportunity to focus on survivorship, especially sexual survivorship.
Implications for research
There are no good data examining the benefits of routine dilation of the vagina during or soon after pelvic radiotherapy. The research and development committee of the Royal United Hospital, Bath, UK has recently funded a multi-centre cohort study examining the variables that might influence sexual function and vaginal anatomy after gynaecological cancer radiotherapy. This should provide the data to inform practice and direct resources towards designing and funding the most appropriate comparative randomised trial. Miles 2010a has completed the data collection from a randomised trial comparing static with vibrating dilation therapy and the future analysis of these data may help inform the debate. The results of a preference trial have limited applicability but are expected at the 13th Biannual Meeting of the International Society for Gynaecological Oncology. However, as far as we know, there are no currently planned randomised trials of dilation practice during the recovery phase and these data are badly needed to help inform practice. However, any trial would need to stratify cases of young and old, stratify cervix cancer from uterine and anal cancer and separate dilation during, soon after and long after radiotherapy. The outcome would need to be an objective measure of sexual function or vaginal physiology. As a minimum, vaginal length must be defined by the pressure applied to the measuring device.
PLAIN LANGUAGE SUMMARY.
Vaginal dilator therapy for women receiving pelvic radiotherapy
Pelvic radiotherapy for gynaecological and anorectal cancer damages the vagina. It causes the vagina to shrink and can make the sides stick together. It has become established practice in the UK to recommend regular vaginal dilation during and after radiotherapy to try and prevent this. Dilation involves placing and rotating a phallus shaped appliance in the vagina approximately three times a week for about five minutes to stretch the skin. This review appraised all the literature and retrieved all available data on this topic to see if there was any evidence to support this practice. These data showed that dilation of the vagina was linked to a rare but serious risk of vaginal rupture and could trigger psychological damage in some women. There was no reliable data to show that dilation had any beneficial impact on sexual function or vaginal anatomy. However, there are case reports suggesting that dilation months or years after radiotherapy is associated with lengthening of the vagina and there is one study (with a high risk of bias) that implies that stenosis rates can be reduced by a stent (plastic phallus shaped tube) compared to a dilator. Other data imply that dilation does not reduce vaginal damage. We conclude that there are data to show that dilation may be harmful in rare cases and that there are insufficient data to confer benefit, so we cannot recommend its routine regular use. However, this is not the same as saying that occasional gentle vaginal examinations or intercourse during or soon after treatment will not prevent the vaginal walls sticking together and dilation after the inflammatory phase has settled may improve vaginal length.
ACKNOWLEDGEMENTS
The authors would like to thank the following.
Dr John Robinson for providing raw data from his and from Dr Jeffries’s study.
The staff from the University of the West of England for critical comments given during the supervision of Tracie Miles’ PhD thesis.
The Cochrane Gynaecological Cancer Review Group, particularly Jane Hayes for supporting the searches and Gail Quinn and Clare Jess for their editorial expertise during the development of the protocol through to the review. We would also like to thank Andy Bryant for his methodological advice.
The British Journal of Obstetric and Gynaecology for allowing us to reproduce sections of the paper by Johnson 2010, the Canadian Journal of Human Sexuality for allowing us to reproduce the figure from the paper by Robinson 1999 and the Indian Journal of Occupational Therapy for allowing us to reproduce the data from Velaskar 2007.
SOURCES OF SUPPORT
Internal sources
No sources of support supplied
External sources
Department of Health, UKNHS Cochrane Collaboration Programme Grant Scheme CPG-506, UK.
CHARACTERISTICS OF STUDIES
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bruner 1993 | There are no data provided of any measure of vaginal or sexual function and no data were available from the authors |
| Decruze 1999 | This comparative study used historical controls that were not perfectly matched and the care in the control group are not defined, but it seems that some form of dilation therapy was available |
| Jeffries 2006 | Did not meet the inclusion criteria |
| Poma 1980 | This is a case series of 5 selected cases treated many years after cancer therapy |
| Robinson 1999 | Did not meet the inclusion criteria, flawed methodology and prone to bias |
| Sobotkowski 2006 | This is a good comparative study but the focus is on the application of mitomycin with a speculum. Whilst it is reasonable to assume that the treatment group had 2 additional examinations with a speculum that must have stretched the vagina, the absence of any difference in the groups could be due to numerous factors including the possibility that both groups were receiving some form of dilation care from another source |
| Velaskar 2007 | Case series with unblinded measurements, the measuring tool is not disclosed and altered vaginal length might represent a different tolerance to being measured due to experience, rather than changes in anatomy |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Trial comparing 2 techniques of vaginal dilation therapy for women receiving radiotherapy, to determine patient satisfaction and effectiveness |
|---|---|
| Methods | Randomised controlled trial |
| Participants | 15 women with stage I or II cervical or endometrial cancer treated with radiotherapy |
| Interventions | Clinical nurse specialist support and motivation and either a standard static dilator (Amielle Comfort Vaginal Dilators from Owen Mumford Ltd of Oxford, UK) or a vibrator (Sh! emporium of 57 Hoxton Square, London) |
| Outcomes | Vaginal anatomy and sexual function |
| Starting date | 2005 |
| Contact information | tracie.miles@ruh.nhs.uk |
| Notes | NHS research ethics application 04/Q2001/227 |
| Trial name or title | A comparison of static and vibrating vaginal dilators to evaluate sexual morbidity in women receiving radiotherapy for carcinoma of the cervix or uterus |
|---|---|
| Methods | Full programme of research |
| Participants | Women with stage I to 3 genital cancer treated with radiotherapy |
| Interventions | Commercially available vaginal vibrator |
| Outcomes | Vaginal anatomy and sexual function and quality of life |
| Starting date | 2003 |
| Contact information | tracie.miles@ruh.nhs.uk |
| Notes | A thesis to be submitted in accordance with the requirements for the degree of Doctor of Philosophy to The University of the West of England Bristol, Faculty of Health and Social Care, Bristol |
DATA AND ANALYSES
This review has no analyses.
Appendix 1. MEDLINE search strategy
1950 to November Week 3 2008
exp Vagina/
vagina*.mp.
1 or 2
exp Radiotherapy/
“radiotherapy”.fs.
“radiation effects”.fs.
radiotherap*.mp.
radiation.mp.
4 or 5 or 6 or 7 or 8
dilat*.mp.
vibrator*.mp.
device*.mp.
lubricat*.mp.
stent*.mp.
cream*.mp.
massage*.mp.
stenos*.mp.
fibros*.mp.
scarring.mp.
10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19
3 and 9 and 20
key: mp = title, original title, abstract, name of substance word, subject heading word
fs = floating subheading
Appendix 2. CENTRAL search strategy
The Cochrane Library 2008, Issue 4
#1 MeSH descriptor Vagina explode all trees
#2 vagina*
#3 (#1 OR #2)
#4 MeSH descriptor Radiotherapy explode all trees
#5 Any MeSH descriptor with qualifier: RT
#6 Any MeSH descriptor with qualifier: RE
#7 radiotherap*
#8 radiation
#9 (#4 OR #5 OR #6 OR #7 OR #8)
#10 dilat*
#11 vibrator*
#12 device*
#13 lubricat*
#14 stent*
#15 cream*
#16 massage*
#17 stenos*
#18 fibros*
#19 scarring
#20 (#10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19)
#21 (#3 AND #9 AND #20)
Appendix 3. EMBASE search strategy
1980 to 2008 week 50
exp Vagina/
vagina*.mp.
1 or 2
exp Radiotherapy/
radiotherap*.mp.
radiation.mp.
4 or 5 or 6
dilat*.mp.
vibrator*.mp.
device*.mp.
lubricat*.mp.
12 stent*.mp.
cream*.mp.
massage*.mp.
stenos*.mp.
fibros*.mp.
scarring.mp.
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17
3 and 7 and 18
key: mp = title, original title, abstract, name of substance word, subject heading word
fs = floating subheading
Appendix 4. Compliance data for Jeffries 2006 and Robinson 1999
| Methods | RCT |
| Participants | 42 sexually active women, 21 to 65 years of age, diagnosed with Stages Ic to III cervical or endometrial cancer, who received pelvic radiotherapy. There were 23 (49%) women with stage I disease, 16 (34%) with stage II and 8 (17%) with stage III disease The mean age of women in the trial was 43 years (SD= 10.3 years, range: 21 to 65). Two (4%) women had a marital status of single, 31 (66%) were married, 3 (6.5%) were divorced and 11 (19%) women had common law as their status. There were 13 (28%) women educated to high school level, 21 (45%) women had a secondary education and 13 (28%) women had at least an undergraduate degree. 38 (81%) women were diagnosed with cervical cancer and 9 (19%) women had endometrial carcinoma |
| Interventions | Intervention: psychoeducational intervention specifically designed to increase compliance with vaginal dilation Comparison: information-only control group Dilation began in the last week of therapy |
| Outcomes | Assessment of vaginal dilation compliance was made by questionnaire before treatment and at 6 week, 6 month, 12 month, 18 month, and 24 month follow-up. Assessment via interview also occurred at 6-month, 12-month, 18-month, and 24-month follow up. No data are available on vaginal or sexual function |
| Notes | This randomised trial is from the same group as the one led by John Robinson. It focused on compliance with treatment and no data on sexual scores were collected. The data are heterogeneous and the likely cause of the heterogeneity is the difference in ages |
Risk of bias table
| Item | Judgement | Description |
|---|---|---|
| Adequate sequence generation? | Yes | Direct communication from one of the authors (JR) confirms that the block randomisation protocol was constructed using random number tables generated by Microsoft Excel Version 6.0. The block randomisation protocol was designed to randomly assign approximately equal numbers of groups of women to either the control or experimental interventions for both centres |
| Allocation concealment? | Yes | As the author both designed the random assignment protocol and was the recruiter for the Calgary arm of the trial. Special precautions were undertaken to ensure she was blind to the assignment. First, the random assignment was based on relatively large blocks so that the next random assignment could not be predicted from the previous assignments. Second, the random assignment protocol was designed very early in the experimental design to minimise the chance that she would remember the assignment order. Each assignment was then sealed into numbered envelopes that were not opened until the small groups of women were accrued. Sealed assignment envelopes were also supplied to the research assistant in Edmonton |
| Blinding? | No | The control group knew they were not receiving additional psychoeducational support |
| Incomplete outcome data addressed? | Yes | 100% of women analysed: 47/47 |
| Free of selective reporting? | Yes | There is no suggestion of selective reporting |
| Free of other bias? | Yes | This was a well-conducted trial given the potentials for bias |
| Methods | Random allocation was directed by a random number table concealed in sealed opaque envelope |
| Participants | 32 women with Stage I or II cervical or endometrial cancer treated with radiotherapy. 24 (75%) women were diagnosed with stage I/II cervical carcinoma and 8 (25%) women had endometrial carcinoma. Radiotherapy was the sole treatment in 9 (28%) women, the other 23 (72%) had a combination of radiotherapy with surgery and/or chemotherapy. 20 women (63%) were taking hormone replacement therapy The mean age of women in the trial was 46.5 years (range = 28 to 73 years). There were 3 (9%) women with an education grade 1 to 8, 11 (34%) women with grade 9 to 12 and 18 (56%) women had at least some post-secondary education |
| Interventions |
Intervention: psychoeducational programme using an information-motivation-behavioural skills’ model to influence compliance Women randomised to the experimental intervention arm attended two 1.5-hour psychoeducational group sessions co-facilitated by the lead and last author using the information-motivation-behavioural skills model described by Fisher 1996. Information about sexuality in general and sexuality and cancer was presented using a variety of teaching aids and techniques: a three-dimensional (3D) model of the female pelvis was utilised; women were shown and able to feel different kinds of vaginal lubricants; explicit instruction for vaginal dilation was given; and the women were shown and able to handle a vibrator. In addition to receiving a copy of Sexuality and Cancer (Schover 1988), the participants were given a handout on the additional material covered in the meetings. The motivational component of the intervention was designed to enhance the women’s view of their sexuality and to promote the idea that sex can be pleasurable despite cancer treatment. The group format allowed for social comparisons, normalisation of feelings, and social connections. For example, the women were encouraged to go together to “sexuality” shops to purchase vibrators and lubricants. They were encouraged to discuss their experience and fears. Issues such as changes in body image and fears about painful intercourse and vaginal bleeding were raised by the facilitators if they were not raised by the women. The behavioural skills component focused on teaching women how to effectively use dilators and lubricants, and Kegal exercises Comparison: standard care Women in the control arm met with a counsellor and were given a copy of Sexuality and Cancer: For the Women Who Has Cancer, and her partner (Schover 1988). This booklet provides a very frank description of both the “normal” sexual response and sex-related consequences of cancer and its treatments. It covers topics such as vaginal dryness and the use of lubricants; painful intercourse and strategies for managing this problem, such as Kegel exercises, vaginal dilators, and alternative positions for intercourse: managing anxiety; and changes in body image. During the counselling session, women’s questions about cancer and sexuality were answered by referring to the appropriate sections of the booklet. The attention of all women was drawn to the sections of the booklet related to dilation and the use of lubricants |
| Outcomes | Global sexual health, knowledge about sexuality and cancer, fears about sexuality after cancer and vaginal dilation compliance. No attempt was made to measure vaginal anatomy |
| Notes | - |
Risk of bias table
| Item | Judgement | Description |
| Adequate sequence generation? | Yes | Randomisation involved a random number table |
| Allocation concealment? | Yes | Direct communication from the first author confirms that random allocation was directed by a random number table concealed in sealed opaque envelopes |
| Blinding? | Unclear | It would have been impossible to conceal the group allocation from participants. It was unclear whether the outcome assessor was blinded |
| Incomplete outcome data addressed? | Yes | When the authors began to analyse the data, they became aware that 8 of the 40 participants recruited to the study had dropped out after randomisation. These data were excluded in the analysis (20% of women analysed: 32/40). This means that the analysis did not use the intention-to-treat principle |
| Free of selective reporting? | Yes | An honest critique of the limitations of the data and the wiliness to openly share the data impressed us to conclude that the paper was not selectively reported |
| Free of other bias? | No | The authors claim that the intervention increased compliance in the young but critical review of the paper makes it difficult to assess this conclusion. Data are available from 1 in 5 young women aged below the median age who continued dilating at the 3-month assessment compared to 3 in 4 who were given encouragement. However, there were 14 subjects in the control group and 18 who were allocated the intervention so data should have been available in 7 and 9 cases respectively under the median age Also, the authors gave data on the number of responses to questioning about compliance and their table includes 36 responses in the control group out of 18 cases but 45 responses out of 14 women. It is likely that the scores for the same women have been repeated and this requires a prior hypothesis and more complex statistical modelling taking the analysis of variance and repeated measures into account |
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
The protocol was designed with the expectation that data existed to support current practice and this review was expected to quantify the strength and magnitude of the effect from the intervention. The absence of data surprised the authors and we then expanded the search criteria to provide an exhaustive literature trawl.
The initial protocol included a strategy for meta-analysis but data were not synthesised and heterogeneity was not explored because the comparisons were restricted to single trial analyses.
Footnotes
DECLARATIONS OF INTEREST: None.
The authors have an academic research grant from the Royal United Hospital NHS Trust to correlate vaginal dilator use with vaginal anatomy. The findings of this review helped inform the trial rationale and design. The lead author has received educational grants, equipment for research and a travel grant to attend the IGCS in Santa Monica in 2007 from Owen Mumford, manufacturers of Amielle 2010.
CONTRIBUTIONS OF AUTHORS: TPM: original idea; NJ and TPM: analysis; NJ and TPM: writing protocol and review.
NOTES: A version of this review will be available in the BJOG, 2010 (Johnson 2010).
WHAT’S NEW Last assessed as up-to-date: 15 July 2010.
| Date | Event | Description |
|---|---|---|
| 27 March 2014 | Amended | Contact details updated. |
References to studies excluded from this review
- Bruner 1993 {published data only (unpublished sought but not used)} .Bruner DW, Lanciano R, Keegan M, Corn B, Martin E, Hanks GE. Vaginal stenosis and sexual function following intracavitary radiation for the treatment of cervical and endometrial cancer. International Journal of Radiation Oncology, Biology, Physics. 1993;27(4):825–30. doi: 10.1016/0360-3016(93)90455-5. [DOI] [PubMed] [Google Scholar]
- Decruze 1999 {published data only} .Decruze SB, Guthrie D, Magnani R. Prevention of vaginal stenosis in patients following vaginal brachytherapy. Clinical Oncology. 1999;11:46–8. doi: 10.1053/clon.1999.9008. [DOI] [PubMed] [Google Scholar]
- Jeffries 2006 {published and unpublished data} .Jeffries SA, Robinson JW, Craighead PS, Keats MR. An effective group psychoeducational intervention for improving compliance with vaginal dilation: a randomized controlled trial. International Journal of Radiation Oncology, Biology, Physics. 2006;65(2):404–11. doi: 10.1016/j.ijrobp.2005.12.009. [DOI] [PubMed] [Google Scholar]
- Poma 1980 {published data only} .Poma PA. Postirradiation vaginal occlusion: nonoperative management. International Journal of Gynaecology and Obstetrics. 1980;18(2):90–2. doi: 10.1002/j.1879-3479.1980.tb00252.x. [DOI] [PubMed] [Google Scholar]
- Robinson 1999 {published and unpublished data} .Robinson JW, Faris PD, Scott CB. Psychoeducational group increases vaginal dilation for younger women and reduces sexual fears for women of all ages with gynecological carcinoma treated with radiotherapy. International Journal of Radiation Oncology Biology and Physics. 1999;44(3):497–506. doi: 10.1016/s0360-3016(99)00048-6. [DOI] [PubMed] [Google Scholar]
- Sobotkowski 2006 {published data only} .Sobotkowski J, Markowska J, Fijuth J, Pietraszek A. Preliminary results of mitomycin C local application as post-treatment prevention of vaginal radiation-induced morbidity in women with cervical cancer. European Journal of Gynaecological Oncology. 2006;27(4):356–8. [PubMed] [Google Scholar]
- Velaskar 2007 {published data only} .Velaskar SM, Martha R, Mahantashetty U, Badakare JS, Shrivastava SK. Use of indigenous vaginal dilator in radiation induced vaginal stenosis. Indian Journal of Occupational Therapy. 2007;34(1):3–6. [Google Scholar]
References to ongoing studies
- Miles 2005 {published and unpublished data} .Miles TP, Johnson N. Vaginal elasticity and viscosity after pelvic radiotherapy and implications for practice. International Journal of Gynecological Cancer. 2006;16(S3):712. [Google Scholar]
- Miles 2010a {unpublished data only} .Miles TP. A comparison of static and vibrating vaginal dilators to evaluate sexual morbidity in women receiving radiotherapy for carcinoma of the cervix or uterus. (to be submitted in accordance with the requirements for the degree of Doctor of Philosophy) The University of the West of England Bristol, Faculty of Health and Social Care; Bristol, UK: 2010. [Google Scholar]
Additional references
- Abitol 1974 .Abitol MM, Davenport JH. Sexual dysfunction after therapy for cervical carcinoma. American Journal of Obstetrics and Gynaecology. 1974;119:181–9. doi: 10.1016/0002-9378(74)90031-3. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association 2000 .American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Sexual and Gender Identity Disorders. Fourth Edition, Text Revision. American Psychiatric Association; Washington DC, USA: 2000. Sexual Aversion Disorder 302.79. http://www.psychiatryonline.com/content.aspx?aID=9929&searchStr=sexual+aversion+disorder. [Google Scholar]
- Amielle 2010 .Owen Mumford Ltd. Brook Hill. Woodstock. Oxford OX20 1TU Amielle Comfort. http://www.owenmumford.com/en/range/21/amielle-comfort.html.
- Bertelesen 1983 .Bertelesen K. Sexual dysfunction after treatment of cervical cancer. Danish Medical Bulletin. 1983;Vol. 30:31–4. [PubMed] [Google Scholar]
- Best Clinical Practice Guidelines 2009 .GMCT Gynaecological Oncology Guidelines Review Group . Best Clinical Practice Gynaecological Cancer Guidelines [Vaginal stenosis] NSW Department of Health; Sydney: 2009. p. 16. http://www.health.nsw.gov.au/resources/gmct/gynaeonc/pdf/goclinicalguidelines.pdf. [ISBN 978–1–74187–444–0] [Google Scholar]
- Bucher 1997 .Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. Journal of Clinical Epidemiology. 1997;50:683–91. doi: 10.1016/s0895-4356(97)00049-8. [DOI] [PubMed] [Google Scholar]
- Burke 1996 .Burke L. Sexual dysfunction following radiotherapy for cancer of the cervix. British Journal of Nursing. 1996;5(4):239–44. doi: 10.12968/bjon.1996.5.4.239. [DOI] [PubMed] [Google Scholar]
- Cancer Backup 2010 .Cancer Backup [last accessed 6 July 2010]; http://www.macmillan.org.uk.
- Cartwright 1995 .Cartwright-Alcarese F. Addressing sexual dysfunction following radiation therapy for gynaecologic malignancy. Oncology Nursing Forum. 1995;22(8):1227–31. [PubMed] [Google Scholar]
- Crowther 1994 .Crowther ME, Corney RH, Shepherd JH. Editorial. Psychosexual implications of gynaecological cancer. BMJ. 1994;308:869–70. doi: 10.1136/bmj.308.6933.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson 2003 .Davidson SE, Burns M, Routledge J, Swindell R. The impact of radiotherapy for carcinoma of the cervix on sexual function assessed using the LENT SOMA scales. Radiotherapy and Oncology. 2003;68(3):241–7. doi: 10.1016/s0167-8140(03)00190-7. [DOI] [PubMed] [Google Scholar]
- Deeks 2001 .Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Davey Smith G, Altman DG, editors. Systematic Reviews in Health Care: Meta-Analysis in Context. 2nd edition BMJ Publication Group; London: 2001. [Google Scholar]
- Denton 2000 .Denton AS, Bond SJ, Mathews S, Bentzen SM, Maher EJ. National audit of the management and outcome of carcinoma of the cervix treated with radiotherapy in 1993. Clinical Oncology. 2000;12:347–53. doi: 10.1053/clon.2000.9192. [DOI] [PubMed] [Google Scholar]
- DerSimonian 1986 .DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Eltabbakh 1977 .Eltabbakh GH, Piver MS, Hempling RE, Shin KH. Excellent long term survival and absence of vaginal recurrences in 332 patients with low risk stage I endometrial adenocarcinoma treated with hysterectomy and vaginal brachytherapy without formal staging lymph node sampling: report of a prospective trial. International Journal of Radiation Oncology, Biology, Physics. 1977;32(2):373–80. doi: 10.1016/s0360-3016(97)00040-0. [DOI] [PubMed] [Google Scholar]
- EORTC 2008 .EORTC . 2008. http://groups.eortc.be/qol/eortc-qlq-c30. [Google Scholar]
- Faithfull 2003 .Faithfull S, Wells M. Supportive Care in Radiotherapy. Churchill Livingstone; Edinburgh: 2003. [Google Scholar]
- Fisher 1996 .Fisher J, Fisher W, Misovich S, Kimble D, Malloy T. Changing AIDS risk behaviour: effects of an intervention emphasizing AIDS risk reduction information, motivation and behaviour skills in a college student population. Health Psychology. 1996;14:120–8. doi: 10.1037//0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]
- Gosselin 2001 .Gosselin T, Waring J. Nursing management of patients receiving brachytherapy for gynecologic malignancies. Clinical Journal of Oncology Nursing. 2001;5(2):59–63. [PubMed] [Google Scholar]
- Grigsby 1995 .Grigsby PW, Russell A, Bruner D, Eifel P, Koh WJ, Spanos W, et al. Late injury of cancer therapy on the female reproductive tract. International Journal of Radiation Oncology, Biology, Physics. 1995;31(5):1281–99. doi: 10.1016/0360-3016(94)00426-L. [DOI] [PubMed] [Google Scholar]
- Hartman 1972 .Hartman P, Diddle AW. Vaginal stenosis following irradiation therapy for carcinoma of the cervix uteri. Cancer. 1972;30(2):426–42. doi: 10.1002/1097-0142(197208)30:2<426::aid-cncr2820300219>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Hassey-Dow 1992 .Hassey-Dow K. Nursing Care in Radiation Oncology. WB Saunders; Philadelphia: 1992. Altered patterns of sexuality. [Google Scholar]
- Higgins 2003 .Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins 2008 .Higgins JPT, Green S, editors. The Cochrane Collaboration. [updated February 2008]. 2008. Cochrane Handbook for systematic Reviews of Interventions Version 5.0.0. Available from www.cochrane-handbook.org. [Google Scholar]
- Hoffman 2003 .Hoffman MS, Wakeley KE, Cardosi RJ. Risks of rigid dilation for a radiated vaginal cuff: Two related rectovaginal fistulas. Obstetrics and Gynecology. 2003;101(5 (Suppl):1125–6. doi: 10.1016/s0029-7844(02)02624-8. [DOI] [PubMed] [Google Scholar]
- Hull 2008 .Hull A, Brennan J, Murdoch J, Radford S. British Gynaecological Cancer Society Spring Conference: Quality of Life Assessment in Gynaecological Oncology. Kent; Canterbury: 2008. Psychological factors mediating use of vaginal dilators following brachytherapy for endometrial cancer; p. 8. [Google Scholar]
- Jensen 2004 .Jensen PT, Klee MC, Thranov I, Groenvold M. Validation of a questionnaire for self-assessment of sexual function and vaginal changes after gynaecological cancer. Psycho-Oncology. 2004;13:577–92. doi: 10.1002/pon.757. [DOI] [PubMed] [Google Scholar]
- Johnson 1990 .Johnson N, Lilford RJ. Chapter 25: The surgical treatment of gynaecological congenital malformations. In: Studd J, editor. Progress in Obstetrics and Gynaecology 8. Churchill Livingstone; Edinburgh: 1990. pp. 413–31. [Google Scholar]
- Johnson 1991 .Johnson N, Batchelor A, Lilford RJ. Experience with tissue expansion vaginoplasty. British Journal of Obstetrics and Gynaecology. 1991;98:564–8. doi: 10.1111/j.1471-0528.1991.tb10371.x. [DOI] [PubMed] [Google Scholar]
- Krumm 1993 .Krumm S, Lamberti J. Changes in sexual behaviour following radiation therapy for cervical cancer. Journal of Psychosomatic Obstetric Gynaecology. 1993;14(1):51–63. doi: 10.3109/01674829309084430. [DOI] [PubMed] [Google Scholar]
- Lamberti 1979 .Lamberti J. Sexual adjustment after radiation therapy for cervical carcinoma, a brief guide to office counselling. Medical Aspects of Human Sexuality. 1979;13:87–8. [Google Scholar]
- Lancaster 2004 .Lancaster L. Preventing vaginal stenosis after brachytherapy for gynaecological cancer: an overview of Australian practices. European Journal of Oncology Nursing. 2004;8(1):30–9. doi: 10.1016/S1462-3889(03)00059-0. [DOI] [PubMed] [Google Scholar]
- Medintim 2010 .MEDintim Personal Healthcare [accessed 2 July 2010];Vaginal Dehnungshilfen aus Silikon. http://medintim-shop.de/Fuer-die-Frau/Vaginal-Dilatoren/Dilator-Set.html?gclid=CKKuwIGHjZ8CFU0B4wodtGTfIQ.
- Miles 2007 .Miles TP. Annual National Meeting of the British Society for the Study of Vulval Disease. University of Cardiff; Apr, 2008. Vagina monologues. [Google Scholar]
- Miles 2010 .Miles TP, Johnson N. Systematic literature review, a randomised trial and a preference trial challenging the practice of vaginal dilation during radiotherapy. 13th Biennial Meeting of the International Gynaecological Cancer Society (IGCS 2010); Prague. Czech Republic; 2010. [Google Scholar]
- NCI 2009 .National Cancer Institute: US National Institutes of Health [accessed 2 July 2010];Cancer of the uterus. http://www.cancer.gov/cancertopics/wyntk/uterus.
- Pavy 1995 .Pavy JJ, Denekamp J, Letschert J, Littbrand B, Mornex F, Bernier J, et al. EORTC Late Effects Working Group. Late effects toxicity scoring: the SOMA scale. Radiotherapy and Oncology. 1995;35:11–5. doi: 10.1016/0167-8140(95)97448-m. [DOI] [PubMed] [Google Scholar]
- Pountney 2005 .Pountney D. From clinic to commerce. Cancer Nursing Practice. 2005;4:9. [Google Scholar]
- Rice 2000 .Rice A. Sexuality in cancer and palliative 1: effects of disease and treatment. International Journal of Palliative Nursing. 2000;6(8):392–7. doi: 10.12968/ijpn.2000.6.8.9064. [DOI] [PubMed] [Google Scholar]
- Schover 1988 .Schover LR. Sexuality & cancer: for the woman who has cancer, and her partner. American Cancer Society; 1988. [Google Scholar]
- Seibel 1982 .Seibel M, Freeman M, Graves W. Sexual function after surgical and radiation therapy for cervical carcinoma. Southern Medical Journal. 1982;75:1195–7. doi: 10.1097/00007611-198210000-00010. [DOI] [PubMed] [Google Scholar]
- Soul 2010 .Soul Source Enterprises [accessed 2 July 2010];Soul Source Silicone Dilators. http://www.soulsource.com/products/silicone-vaginal-dilators/
- UK Nurse Forum 2005 .National Forum of Gynaecological Oncology Nurses. Owen Mumford; Oxon: Jul, 2005. Best practice guidelines on the use of vaginal dilators in women receiving pelvic radiotherapy. http://www.jotrust.co.uk/files/PDF%20to%20download/23198DilatorsA4fnlAW.pdf. [Google Scholar]
- Vasicka 1958 .Vasika A, Popovitch NR, Brausch CC. Post radiation course of patients with cervical carcinoma. Obstetrics and Gynaecology. 1958;11:403–14. [PubMed] [Google Scholar]
- White 2004 .White I, Faithfull S. UK survey of current practice in vaginal dilatation associated with pelvic radiotherapy. European Institute of Health and Medical Sciences; 2004. [Google Scholar]
- White 2006 .White ID, Faithfull S. Vaginal dilation associated with pelvic radiotherapy: a UK survey of current practice. International Journal of Gynecological Cancer. 2006;16:11406. doi: 10.1111/j.1525-1438.2006.00452.x. [DOI] [PubMed] [Google Scholar]
- Wilmoth 2000 .Wilmoth MC, Spinelli A. Sexual implications of gynecologic cancer treatments. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2000;29(4):413–21. doi: 10.1111/j.1552-6909.2000.tb02064.x. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Denton 2003 .Denton AS, Maher EJ. Interventions for the physical aspects of sexual dysfunction in women following pelvic radiotherapy. Cochrane Database of Systematic Reviews. 2003;(Issue 1) doi: 10.1002/14651858.CD003750. [Art. No.: CD003750. DOI: 10.1002/ 14651858.CD003750] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson 2010 .Johnson N, Miles TP, Cornes P. Dilating the vagina to prevent damage from radiotherapy; systematic review of the literature. British Journal of Obstetrics and Gynaecology. 2010;117(5):522–31. doi: 10.1111/j.1471-0528.2010.02502.x. [DOI] [PubMed] [Google Scholar]
- * Indicates the major publication for the study