Summary
We describe three upper limb injuries admitted in one year to our institution resulting from falls from motorised mobility scooters (MMS) where all three users were novices, using their MMS for less than 6 weeks. They sustained injuries in close proximity to their homes, necessitating admission to hospital. None had received any formal training before commencing use of their respective devices. Use of MMS devices increases independence in mobility, enhances quality of life, improves self-esteem, facilitating social participation in everyday life. Use of these devices is not without risks, and no clear safety guidelines or competency testing exists for users. We believe these injuries in novice users highlights this deficiency, and should alert prescribers of these devices to advocate some form of driver training for new users.
Keywords: motorised mobility scooters, fracture, elderly, trauma, orthopaedics, rehabilitation
Introduction
The use of powered wheelchairs and other mobility scooters is a relevant societal intervention in relation to older people with limited walking ability in order to make activity and participation possible (1).
Increasing usage of MMS has been noted, and with it improved satisfaction scores for a marginalised community (2). However, these devices are frequently used by the most vulnerable, including the aged and disabled (3) and serious injuries and fatalities have been described (4).
Case series
Table 1 summarises the three cases of novice users who presented to our institution following MMS related injuries. Case 1 sustained a fall from her MMS while taking her first trip outside the home, sustaining an open comminuted fracture of her right elbow (Figure 1), for which she had closed reduction and K-wiring, followed by an extended period in a cast and convalescence prior to returning home. An independent home dweller, she had purchased the device to facilitate visiting friends and shopping.
Table 1.
The three cases with respective data regarding the injury and length of MMS usage.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age, Sex | 92, female | 69, male | 68, female |
| Injury | Open fracture right distal humerus | Closed fracture right proximal humerus | Dislocation left elbow |
| Hospital LOS | 5 days | 2 days | 3 days |
| Reason for MMS use | Lower limb arthritis | Post CVA hemiplegia | Chronic back pain |
| Location of fall | Road beside house | House driveway | House porch |
| Duration of MMS usage before injury | First use | 3 weeks | 6 weeks |
| Advice/training received | None | None | None |
Abbreviations: LOS - length of stay, MMS - motorised mobility scooter, CVA - cerebrovascular accident.
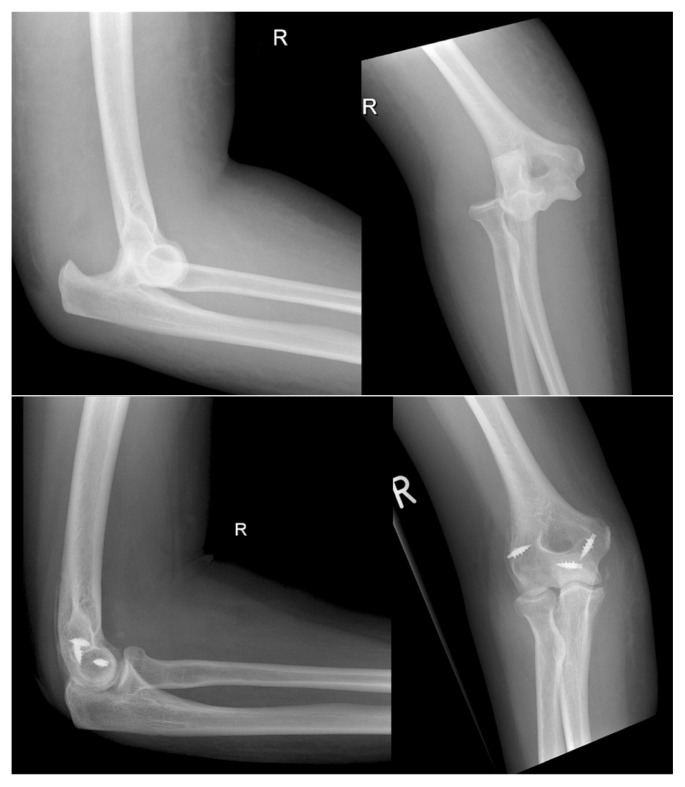
Figure 1.
Case 1: comminuted open fracture of right supracondylar humerus, treated with Kwires and an above elbow cast, with imaging at 6 months post injury.
Case 2 had been using his MMS for 3 weeks, and fell from the device while leaving his house, sustaining a fracture of his right proximal humerus (Figure 2), which was treated non-operatively. He had obtained his device to facilitate his integration into the community following a recent stroke.
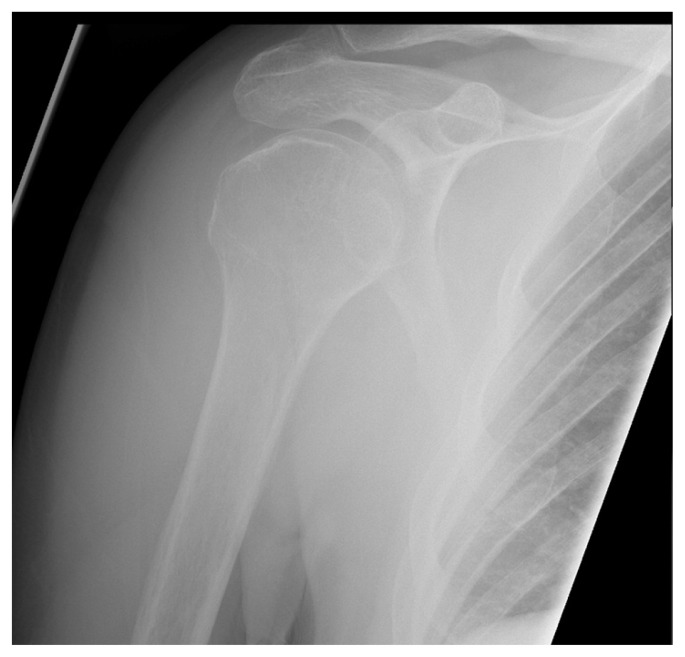
Figure 2.
Case 2: undisplaced right proximal humerus fracture, treated non-operatively.
Case 3 sustained a fall after slipping from her MMS while pulling away from her front door, causing a hyperextension injury to her right arm in which she sustained a dislocated elbow with ligamentous disruption which required surgical stabilisation (Figure 3). She had multiple locomotor complaints, and used the device to facilitate painless travelling between her home, local shops and the doctor’s office.
Figure 3.
Case 3: closed dislocation right elbow with ligamentous disruption, treated with closed reduction and ligamentous repair.
Discussion
MMS are three or four wheeled vehicles designed for people with mobility related challenges with regards to walking distances, and are a popular mode of transport allowing users maintain active, independent lifestyles. Two studies report medical indication for MMS usage. In the first study based on an Australian cohort indications included in decreasing frequency: arthritis, heart condition, hip or knee joint replacement, high blood pressure and spinal cord injury (5). In the second study, from America, indications quoted were disabling arthritis, chronic lung disease, neurologic disorders, and heart failure (6).
A recent Australian cross-sectional study of 202 power wheelchair and scooter users reported that one fifth of participants aged 18–98 years had had an accident using their mobility device in the previous year. The most common accidents described were running into doors and walls, tipping over, being hit by a car or colliding with objects, knocking over shop displays. 11% of this sample population had been hospitalised for MMS-related injuries which although unspecified ranged from “broken bones, lacerations and bruising” (5).
Research undertaken in Victoria in 2006 showed that motorised mobility scooters, a relatively new product, have had a rapid uptake by vulnerable populations (particularly the very old). They noted a substantial emerging upward trend in related deaths and serious injuries among persons aged 60 years and over. The major problem, as with most product-related injuries, appears to be largely at the user/machine interface, though some actual product failures have also been reported. Most reported deaths tend to be result from collisions with other motor vehicles, and are due to head injuries (4).
Although use of these devices improves self-perceived quality of life, usage of MMS is not without its risks. MMS prescribers should be aware that detrimental long-term effects have been reported by increasing cardiovascular risk, particularly insulin resistance (6).
Even in able bodied subjects, MMS driving skill is not intuitive, and only improves with practice. In another Australian study thirty-three of the fifty healthy local community participating subjects (mean age 34 years) failed at least one test item. Basic skills of reversing, weave and zigzag, and all traffic and performing multiple simultaneous tasks produced failures. The author advocates that basic driving skills including weaving, steering in reverse and traffic and multiple tasking need to be taught and tested for all new users of this equipment (7).
Consensus on the issues surrounding MMS usage is far from easy. A group of Canadian rehabilitation practitioners seeking to develop a client-centred guideline for power mobility use within an ageing care context conducted a qualitative study of the meaning of powered mobility and safety concerns. They identified by 19 participants from 8 stakeholder groups (which included powered mobility users, relatives of users, non-power mobility residents, their relatives, power mobility prescribers, and residential home staff), and noted four main themes; i) the meaning of power mobility; ii) learning the rules; iii) concerns about safety; and iv) potential solutions (8).
A study commissioned by the Australian Competition and Consumer Commission (ACCC) of injury data involving motorised mobility devices was performed by Monash University Department of Forensic Medicine and Accident Research Centre. Commenting on the pattern of injury among Queensland emergency department presentations, almost all injury cases occurred in persons aged 60–89 years, with falls being the most common cause of both admitted (75%) and non-admitted cases (67%). The most common location of injury was the road, street and highway, (58% of admissions and 50% of non-admitted cases), followed by the home (17% and 20% respectively) (4).
Tools do exist to assist and improve driver skills. A Canadian study recently compared two power mobility training protocols in residential facilities for the elderly. Using a Power-Mobility-Indoor-Driving-Assessment (PIDA) tool to assess power wheelchair and scooter driving performance, results suggest that training can impact significantly on optimal driving performance (9). A similar study showed that the Power-Mobility-Community-Driving-Assessment (PCDA) can also enhance access to powered devices by potentially unsafe drivers, and identify specific learning needs to promote independent living for drivers of power-mobility devices (10).
Conclusion
Use of MMS devices increases independence in mobility and ease of mobility-related participation in everyday life. Older people with limited locomotion may benefit considerably from devices such as MMS. Given the importance of these devices, safety measures need to address both the mobility drivers and those around them. Education and support regarding optimal usage of such devices in addition to specific training of basic driving skills would seem to be an important components to improve safety concerns for the stakeholders involved.
References
- 1.Brandt A, Iwarsson S, Stahle A. Older people’s use of powered wheelchairs for activity and participation. J Rehabil Med. 2004;36:70–7. doi: 10.1080/16501970310017432. [DOI] [PubMed] [Google Scholar]
- 2.Evans S, Frank AO, Neophytou C, de Souza L. Older adults’ use of, and satisfaction with, electric powered indoor/outdoor wheelchairs. Age Ageing. 2007;36(4):431–5. doi: 10.1093/ageing/afm034. [DOI] [PubMed] [Google Scholar]
- 3.Cassell E, Clapperton A. Consumer product-related injury(2): injury related to the use of motorised mobility scooters. Hazard. 2006;62:1–12. [Google Scholar]
- 4.Gibson K, Ozanne-Smith J, Clapperton A, Kitching F, Cassell E. Targeted Study of Injury Data Involving Motorised Mobility Scooters. A report commissioned by the Australian Competition and Consumer Commission. 2011. http://www.productsafety.gov.au.
- 5.Edwards K, McCluskey A. A survey of adult power wheelchair and scooter users. Disabil Rehabil Assist Technol. 2010;5:411–9. doi: 10.3109/17483101003793412. [DOI] [PubMed] [Google Scholar]
- 6.Zagol BW, Krasuski RA. Effect of motorized scooters on quality of life and cardiovascular risk. Am J Cardiol. 2010;105:672–6. doi: 10.1016/j.amjcard.2009.10.049. [DOI] [PubMed] [Google Scholar]
- 7.Nitz JC. Evidence from a cohort of able bodied adults to support the need for driver training for motorized scooters before community participation. Patient Educ Couns. 2008;2:276–80. doi: 10.1016/j.pec.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 8.Mortenson WB, Miller WC, Boily J, Steele B, Odell L, Crawford EM, et al. Perceptions of power mobility use and safety within residential facilities. Can J Occup Ther. 2005;72:142–52. doi: 10.1177/000841740507200302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hall K, Partnoy J, Tenenbaum S, Dawson D. Power Mobility Driving Training for Seniors: A Pilot Study. Asst Technology. 2005;17:47–56. doi: 10.1080/10400435.2005.10132095. [DOI] [PubMed] [Google Scholar]
- 10.Letts L, Dawson D, Bretholz I, Kaiserman-Goldenstein E, Gleason J, McLellan E, et al. Reliability and validity of the power-mobility community driving assessment. Assist Technol. 2007;19:154–63. doi: 10.1080/10400435.2007.10131872. [DOI] [PubMed] [Google Scholar]