Summary
Osteoid osteoma is a benign tumor especially affecting young males generally treated with radiofrequency ablation. This is a non-invasive and safe procedure, major complications are very rare, most of them consisting in local skin burns. The present case shows a late subtrochanteric fracture in a young boy after CT guided termoablation of osteoid osteoma of proximal femur and short review of the literature.
Keywords: osteoid osteoma, radiofrequency ablation, femoral fracture
Introduction
Osteoid osteoma is a benign bone tumor consisting of a hypervascularized center (nidus) of immature osteoid surrounded by reactive sclerotic bone. The tumor primarily occurs in young males with over 90% being detected before 25 years of age (1). Typically, affected individuals experience a sharp local pain, usually at night, which responds well to non-steroidal anti-inflammatory drugs (NSAID) (2). The combination of clinical findings and typical imaging features (central radiolucent nidus, marginal sclerosis, and perifocal edema) identified in conventional radiographs, computed tomography (CT) and/or magnetic resonance imaging (MRI) allows a reliable diagnosis in most cases (3). Surgical therapy includes curettage, en-bloc resection, or wide resection and bone grafting (4). However, osteoid osteoma may occur in difficult locations and surgery may destroy significant parts of unaffected bone to reach the nidus. Minimally invasive alternative methods have become available, including radiofrequency ablation (RFA) (5) and more recently, laser ablation (LA). Success rates after one treatment session range between 83 and 100% with up to 100% success after a second session in case of failure or recurrence (4). Major complications of the procedure are very rare, most of them consisting in local skin burns. The present case shows a late subtrochanteric fracture in a young boy after CT guided termoablation of osteoid osteoma of proximal femur.
Case report
A 17-year-old Caucasian male was referred to our emergency department [after a sudden right tight pain during sport activity (long jump), functional impotential and deformity]. A pelvic and right femur x-ray were immediately performed, which showed a subtrocanteric diaphiseal fracture (Figure 1). A transcondilar traction was positioned (using a titanium wire) and the patient was admitted to our department. He was healthy and without any relevant clinical problems. The only thing he referred was a radiofrequency ablational procedure for an osteoid osteoma ten years before at the same femur. The first hypothesis was that of a fatigue fracture during an intensive training period because he was a long jumper, but the location was unusual, so the hypothesis was rejected. His relatives brought us the old clinical report and the old CT. Then we performed a new CT scan (Figure 2) and an MRI (Figure 3) with and without gadolinium contrast. The new images matched perfectly with the old ones (Figure 4) in terms of location of the previous site of osteoid osteoma and the fracture level. Moreover, the new images showed a sclerotic cortical and a narrow medullar canal. An intramedullary nailing procedure was then performed (Figure 5) with a T2 Stryker© nail (360×10mm) but we evidenced a very narrow medullar canal, so it was necessary to bore it.
Figure 1.
Fractures X-rays.
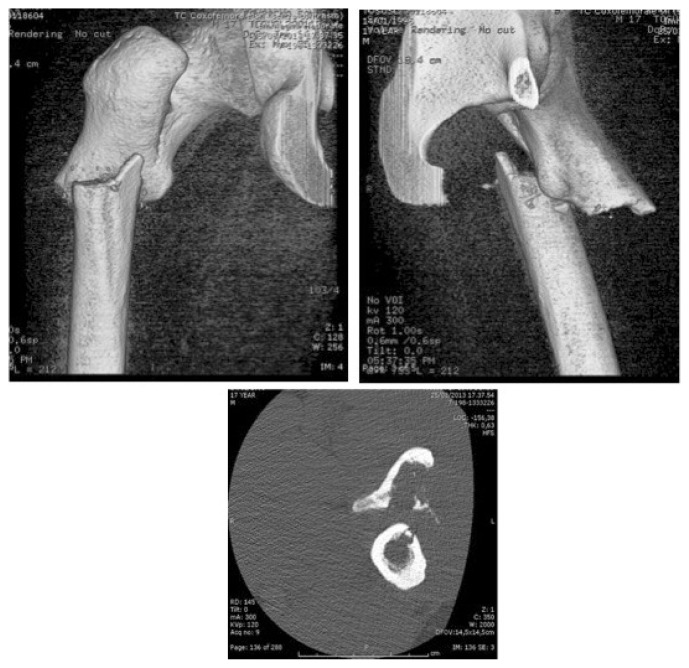
Figure 2.
CT 3D reconstruction.
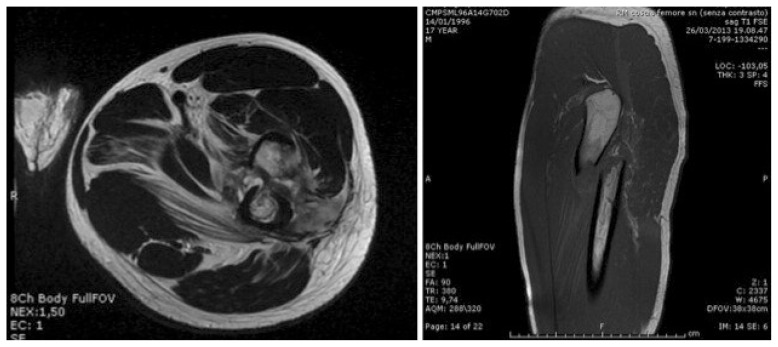
Figure 3.
MRI images.
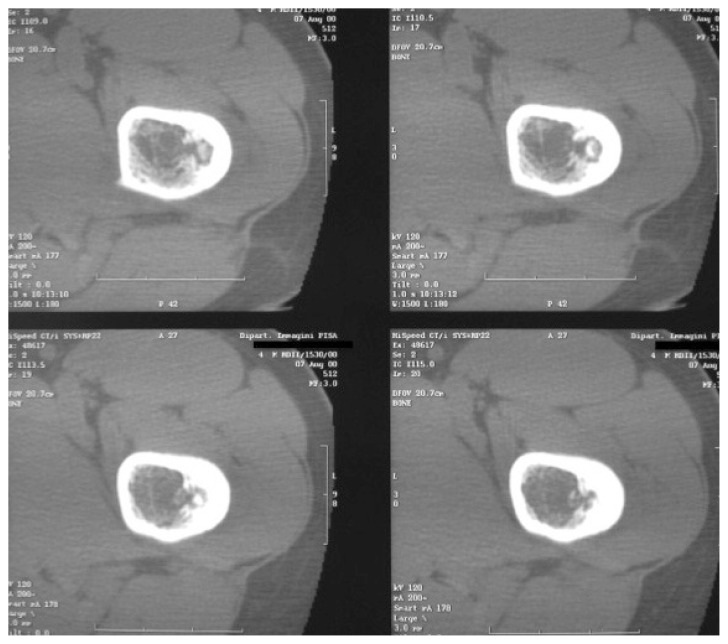
Figure 4.
Old CT images.
Figure 5.
Post-operative X-Ray.
Discussion
Osteoid osteoma is a benign and painful skeletal tumor that occurs for 10–12% of all benign tumors and 2,5% of all pediatric lesions (6). It occurs mainly in children and young adults with 90% of cases seen before the age of 25 years and a male/female ratio of more than 2:1. It is typically a small lesion (less than 1,5 cm) composed by a central nidus of osteoid tissue surrounded by a rim of reactive sclerotic bone. Osteoid osteoma can occur everywhere in the skeleton both in the cortex and medulla. However, it most commonly affects the lower extremity with 50% of all cases involving the femur or the tibia (7). CT-guided techniques for treating osteoid osteoma have recently emerged, and RFA is considered a good alternative to surgery.
During CT-guided RFA of osteoid osteoma, two basic complications may occur: 1) targeting-related complication; and 2) collateral damage of the thermal ablation. The former may lead to the perforation of vessels, nerves, the joint capsule, and growth plate due to imprecise drilling or wrong trajectory planning. Instead the latter is due to the heating of the electrode tip to 85–90°C for 4–6 min, which may result in collateral damage including cellulitis and superficial skin burn up to full-thickness skin necrosis. Fractures, as later complications, were only reported in middle aged adults who had RFA of malignant bone lesions in weight bearing bones, such as the femoral neck (8). An evaluation of fracture risk associated with this procedure requires a knowledge of material properties of the bone and biomechanics of the skeleton under physiological load. The bone is an anisotropic material that resists compressive forces better than tensile (distraction) ones. When a bone, loaded in tension, is weakened by osteoporosis, stress fracture or surgical procedures, it is more prone to fracture than a similar bone loaded in compression. This phenomenon is particularly important in the proximal femur as a result of its anatomy and biomechanics. The risk of fracture of the proximal femur following the placement of lateral metal implants is well known in orthopedic trauma. Subtrochanteric fractures, as a complication of internal fixation of femoral neck fractures with screws, have been addressed in the literature. Our femoral fracture complication occurred through a previous osteoid osteoma nidus ten years after treatment (9).
Conclusions
One major concern of en bloc surgical nidus excision is the weakening of the bone and subsequent higher risk of fracture. In theory, a percutaneous method of nidus ablation through a small drill hole would reduce this risk and have less morbidity, thus increasing the margin of safety for children undergoing this procedure. We have found that RFA is an efficacious way of osteoid osteoma treatment; however, the risk of fracture is not entirely eliminated by this minimally invasive procedure. As for the material properties of bone, the biomechanics of the proximal femur and the risks of stress risers, the lateral proximal femur should be approached with caution when treating osteoid osteoma lesions with RFA. Moreover, the risk is not just in the early post-operative period due to the localized osteoporosis, but even in the late period. In fact, the bone could react making a sclerotic area, which is harder, but is not consequently stronger. This area is considered a locus minoris resistentiae, especially for the lower limbs. Restrictions in jumping, in running and in torsional activities in the post-procedural setting are also strongly recommended, although we are unable to make a definitive statement on the proper duration and to recognize that compliance is difficult in this young, active patient population. We believe our experience demonstrates the efficacy of RFA in the treatment of osteoid osteoma while raising awareness of the risk, albeit rare, of fracture of the proximal femur.
Footnotes
Conflict of interest
The Authors declare no conflict of interest.
References
- 1.Mirra JM, Gold RH, Picci P. Osseous tumors of intramedullary origin. In: Mirra JD, editor. Bone tumors: clinical, radiologic, and pathologic correlations. Philadelphia: Lea&Febiger; 1989. pp. 248–438. [Google Scholar]
- 2.Ilyas I, Younge DA. Medical managment of ostoid osteoma. Canadian Journal of Surgery. 2002;45(6):435–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Greenspan A. Benign bone-forming lesions: ostoid osteoma. Canadian journal of Surgery. 2002;45(6):435–7. [Google Scholar]
- 4.Cantwell CP, Obyrne J, Eustace S. current trends in treatment of osteoid osteoma with an emphasis on radiofrequency ablation. Eur Radiol. 2004;14(4):607–17. doi: 10.1007/s00330-003-2171-6. [DOI] [PubMed] [Google Scholar]
- 5.Rosenthal DI, Alexander A, Rosenberg AE, Springfield D. Ablation of osteoid osteoma: percutaneous laser ablation and follow-up in 114 patients. Radiology. 2007;242(1):293–301. doi: 10.1148/radiol.2421041404. [DOI] [PubMed] [Google Scholar]
- 6.Healey JH, Ghelman B. Osteoid osteoma and osteoblastoma: current concepts and recent advances. Clin Orthop Rel Res. 1986;204:76–85. [PubMed] [Google Scholar]
- 7.Kransdorf MJ, Murphey MD. In: Osseus tumors, in Imaging of bone tumors and tumor-like lesions: techniques and applications. Davies AM, Sundaram M, James SL, editors. Springer; Berlin, Germany: 2009. pp. 251–304. [Google Scholar]
- 8.Dierselhuis EF, Jutte PC, van der Eerden PJ, Suurmeijer AJ, bulstra SK. Hip fracture after radiofrequency ablation therapy for bone tumors: two case report. Skeletal Radiol. 2010;39(11):1139–43. doi: 10.1007/s00256-010-1013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Earhart J, Wellman D, Donaldson J, Chesterton J, King E, Janicki JA. Radiofrequency ablation in the treatment of osteoid osteoma: results and complications. Pediatr Radiol. 2013;43:814–819. doi: 10.1007/s00247-013-2636-y. [DOI] [PubMed] [Google Scholar]