Summary
In elderly patients frequent episodes of joint pain of lower limbs exacerbated by stress and resistant to treatment occur frequently. This paper reports a case of a long lasting bilateral atraumatic knee pain with a final diagnosis of bilateral stress fractures of proximal tibia in osteoporotic postmenopausal woman.
The distinctive trait of this case is that the fracture has set in bilaterally and associated with an isthmic L4–L5 spondylolisthesis in a patient afflicted by a decline in mood. This particular clinical picture has delayed the diagnosis and the suitable treatment for 3 years. Therapy for this type of patients must aim in the acute phase at pain relief and only after must be settled in a long term antiosteoporotic therapy. We choose clodronate acyd for pain relief and after strontium ranelate for osteoporosis prevention.
Keywords: osteoporosis, stress fracture, knees, spondilolistesys, clodronic acid
Introduction
The frequency of osteoporosis is quickly and consistently increasing. Osteoporotic fracture often cause disability, loss of independence and pain (1).
In elderly patients frequent episodes of joint pain of lower limbs exacerbated by stress and resistant to treatment occur frequently. These episodes are attributed to degenerative arthritis pathology and patients usually just undergo conventional radiology. In most cases the conventional radiology only shows a clinical picture of articular degeneration. The appearance and persistence of an atraumatic knee pain, in a negative radiograph exam, should alert the specialist to consider other diagnostic tests (as CT or MRI) (2–4).
Case report
This paper reports a case of a long lasting bilateral atraumatic knee pain with a final diagnosis of bilateral stress fractures of proximal tibia in a postmenopausal osteoporotic woman.
The distinctive trait of this case is that the fracture has set in bilaterally and associated with an isthmic L4–L5 spondylolisthesis.
This particular clinical picture has delayed the diagnosis and the suitable treatment for 3 years.
Patient: D.P.; Caucasian woman: 70 years old. Anthropometric parameters: h=160 cm; w=58 Kg; BMI= 22,6.
Physiological anamnesis: non smoker patient; no reported use of alcohol; menarche at 12 years old; menopause at 50 years old; two full term pregnancies; no allergy reported. Past medical history: hypothyroidism treated with levothiroxyne 125 microgr, urinary incontinence, mood disorder treated with paroxetine. No history of fractures reported or cardiovascular disease. Previous surgery: tonsillectomy and appendicectomy during childhood. Right mastectomy to treat a breast cancer (10 years ago), actually in remission. This event was followed by a prosthetic breast reconstruction.
In June 2007 the patient went to her general practitioner for a bilateral knee pain during the ambulation associated with bilateral ankle pain. At that time pain was tolerable and controlled by painkillers. For this reason no medical examination was taken up.
During the following months the pain became worse and worse and started to be continuous; it could be localized by patient at the antero-medial side of knee and she couldn’t find relief not even with painkillers.
In April 2009 the patient reached orthopaedic specialist observation complaining, as prime problem, the pain during ambulation. The orthopaedic ordered to do x-rays of lower limb and lumbosacral spine.
Knees and ankles x-rays didn’t reveal any recent bone lesion. Spine x-ray instead showed a low-grade isthmic spondylolisthesis at the L4–L5 level. The following MRI confirmed the clinical picture of spondylolisthesis associated to a bulging spinal disc.
Taking into account the clinical picture, the medical imaging and the highly frequency of spinal disease, the diagnosis of spondylolisthesis seemed to justify the symptoms of the patient.
In July 2009 the patient was evaluated by the neurosurgeon and underwent a surgical operation of spinal stabilization L4–L5 level with peduncular screws by posterior way. Furthermore has been set anti-osteoporosis therapy with 400 mg clodronic acid per os daily.
At the end of August 2009, the patient underwent a new neurosurgical control and went on complaining her knees pain.
At the same time the patient reported a decline in mood (with insomnia and depression) and the appearance of hip pain (with x-ray evidence of hip osteoarthritis).
At the end of November 2009 the clinical picture didn’t improve and the patient comes to our observation. We evaluated again the patient, decided to increase anti-osteoporosis therapy, continuing clodronic acid but IM, and ordered a right knee MRI (at that moment the right knee was the most painful).
In January 2010 the exam detected a proximal intraspongious tibial fracture with a widespread edema and vascular suffering of surrounding bone. Some days after the right knee MRI, the patient underwent a left knee MRI that showed the same anatomopathological situation of contralateral knee.
Based on patient’s clinical conditions and the instrumental findings we prescribed:
- Magnet therapy (4–5 hours per day)
- Clodronic acid 100 mg IM, 1/die for 7 days, after 1/week for 6 months
- Calcium 1500 mg associated with vitamin D3 400 U.I. 1/die
- Ambulation with crutches
- New MRI after 2 months.
In the same period the dual-energy x-ray absorptiometry (DEXA) examination showed: L1–L4=−2,4 DS; at femoral neck −3,8 DS.
In April 2010 the patient is hospitalized and underwent a new MRI revealed an initial reduction of intraspongious edema. From the clinical point of view, the patient reported an improving of her life quality with a clear decrease of her pain.
Furthermore the patient underwent a bone scintigraphy and tumor markers are also tested to dismissed the presence of bone metastatic disease, linked to her past medical history, and no specific medical problems were detected.
During the hospitalization and till the end of June, the patient continued with the therapy prescribed in January. At the end of June patient began a therapy with strontium ranelate for osteoporosis treatment.
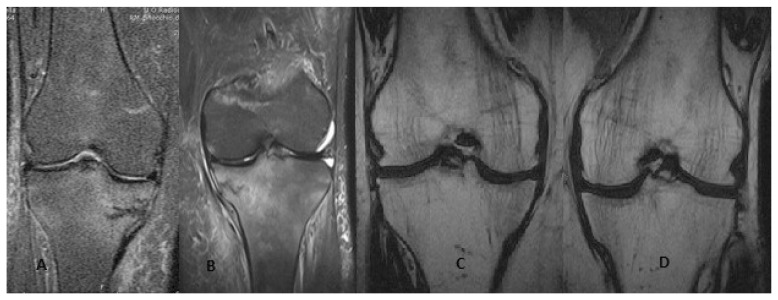
Two years later, in March 2012, the patient performed a bilateral knee MRI that confirmed the complete clinical and radiographic remission (Figures 1, 2).
Figure 1A–D.
A, B) R e L knee MRI at the time of diagnosis. C, D) MRI after resolution of pain.
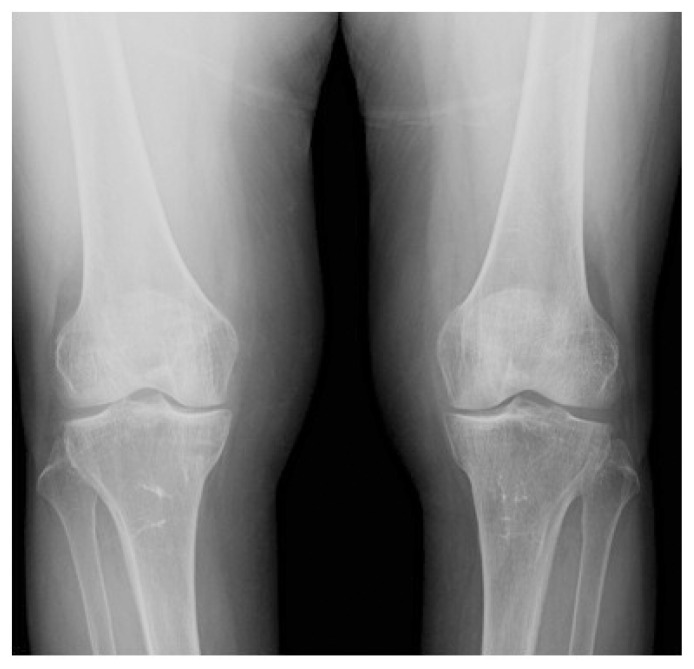
Figure 2.
Knee X-ray after two years of treatment.
Discussion
Considering international literature we found many works about stress fractures in athletes (especially in endurance athletes), instead we found a lower number of articles about stress fracture in elderly patients (5, 6).
Stress fractures result from an unsuccessful bone adaptation to mechanical changes induced by repetitive overload determining the prevalence of osteoclastic bone resorption phenomenon in bone remodeling.
These type of fractures are made in two ways: direct mechanical damage where repeated sudden overloads don’t act progressively on the stimulation of osteoblastic activity and exceed the mechanical strength of the bone; repetitive microtraumatism that, despite having activated the compensatory mechanism of the osteoblastic activity, tip the balance towards the resorption and the osteoclastic activity (7).
We believe that the mechanism that leads to traumatic stress fracture in the elderly is the same mechanism of stress fracture in younger patients. In the elderly, however, the poor bone quality reduces the entity of the stimulus necessary to produce fracture and low energy trauma is often enough to produce fracture.
The cause of stress fractures is often multifactorial (8, 9) and various modifiable and non-modifiable factors have been proposed to play a role: white race (10), high bone turnover (11), vitamin D insufficiency (12), nicotine and alcohol abuse, steroid use, low adult weight (13), low bone density (14), anorexia (15), or bisphosphonate therapy (16, 17).
Furthermore, female gender has been identified as an important risk factor and thus sex-specific effects appear to play a role in the pathogenesis of stress fractures (11).
The risk of fractures in women increases by a factor of 2,6 for each additional year from menarche and by a factor of 1,7 for every 1% decrease in lean body mass of lower limb (18).
In our patient, in addition to the risk factors described above, we find a comorbidity for hypothyroidism that may have influenced the clinical picture, (19) although the patient is receiving hormone therapy and presents normal values of blood tests at the time of fractures: FT4 11,7 pg/ml; FT3 2,89 pg/ml; TSH 2,88 mU/ml; Ca++ 1,25 mmol/L; PTH 60 pg/ml; VIT D 44,1 ng/ml.
International literature is not univocal on the correlation between a deficiency of thyroid hormones and an alteration of bone metabolism.
For some Authors there is no association between TSH or FT4 and bone loss, and fracture risk did not differ significantly by thyroid function (20).
According to some other Authors fracture risk is increased in hyperthyroidism and hypothyroidism especially in post-menopausal women (21).
Therapy for this type of patients must aim in the acute phase at pain relief and only after must be settled in a long term anti-osteoporotic therapy. For this reason we used clodronate acid as a first choice and strontium ranelate in a second time.
Clodronic acid has been shown to be effective in the maintenance or improvement of bone mineral density in patients with osteoporosis. Use of the drug is also associated with reductions in fracture risk. Intramuscular clodronic acid in particular has also been associated with improvements in osteoarticular pain (22).
It is important to increase awareness of this problem. Elderly patients often present complex osteoarticular clinical pictures (hip and knee osteoarthritis, spondyloarthritis and lumbar spinal stenosis) that make the diagnostic process hard.
In our patients for example varus deformity of the knee (Figure 2), with a medial compart overloading, leads to an early osteoarthritis of the knee.
Unfortunately stress fractures often goes unrecognized both for the lack of a pathognomonic and clear symptoms and for the non-high specificity of the first level medical tests (x-rays). In this patient the pain into the anterior medial region of thigh linked by an isthmic spondylolisthesis at the L4–L5 level make the diagnosis harder.
Knee X-ray rarely demonstrates alterations suggestive of a spontaneous fracture. The presence of occult fractures of knee segments should be suspected even in the absence of evident radiographic alteration in the elderly of knee pain resistant to treatment.
We believe that a well-defined diagnosis pathway is necessary in elderly patients with a long time non traumatic lower limb pain, without discharge these patients always with a diagnosis of osteoarthritis.
In particular, in presence of endocrinopathies, second level imaging tests of the painful area should be included in the diagnosis pathway.
Footnotes
Disclosure
No disclosures or conflict of interests. The patients gave the informed consent prior being included into the study; the study was authorized by the local ethical committee and was performed in accordance with the Ethical standards of the 1964 Declaration of Helsinki as revised in 2000.
References
- 1.Tarantino U, et al. Strontium Ranelate and bone healing: report of two cases. Clin Cases Miner Bone Metab. 2010 Jan-Apr;7(1):65–68. [PMC free article] [PubMed] [Google Scholar]
- 2.Sambataro md, Gonzaga do PMR. A Non-Traumatic Stress Fracture of the Tibial Plateau. 2009 Jul;1(7):691–3. doi: 10.1016/j.pmrj.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Luria S, Liebergall M, Elishoov O, Kandel L, Mattan Y. Osteoporotic tibial plateau fractures: an underestimated cause of knee pain in the elderly. Am J Orthop (Belle Mead NJ) 2005 Apr;34(4):186–8. [PubMed] [Google Scholar]
- 4.Cabitza Paolo, Tamim Hassan. Occult fractures of tibial plateau. Detected employing magnetic resonance imaging. Arch Orthop Trauma Surg. 2000;120:355–357. doi: 10.1007/s004020050483. [DOI] [PubMed] [Google Scholar]
- 5.Mattila VM, Niva M, Kiuru M, Pihlajamaki H. Risk factors for bone stress injuries: a follow-up study of 102,515 person-years. Med Sci Sports Exerc. 2007;39:1061–1066. doi: 10.1249/01.mss.0b013e318053721d. [DOI] [PubMed] [Google Scholar]
- 6.Breer S, Krause M, Marshall RP, Oheim R, Amling M, Barvencik F. Stress fractures in elderly patients. International Orthopaedics (SICOT) 2012;36:2581–2587. doi: 10.1007/s00264-012-1708-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benazzo F, Mosconi M, Beccarisi G, Galli U. Use of capacitive coupled electric fields in stress fractures in athletes. Clin Orthop Relat Res. 1995 Jan;(310):145–9. [PubMed] [Google Scholar]
- 8.Pepper M, Akuthota V, McCarty EC. The pathophysiology of stress fractures. Clin Sports Med. 2006;25:1–16. vii. doi: 10.1016/j.csm.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Bennell KL, Malcolm SA, Thomas SA, Reid SJ, Brukner PD, Ebeling PR, Wark JD. Risk factors for stress fractures in track and field athletes. A twelve-month prospective study. Am J Sports Med. 1996;24:810–818. doi: 10.1177/036354659602400617. [DOI] [PubMed] [Google Scholar]
- 10.Pegrum J, Crisp T, Padhiar N. Diagnosis and management of bone stress injuries of the lower limb in athletes. BMJ. 2012;344:e2511. doi: 10.1136/bmj.e2511. [DOI] [PubMed] [Google Scholar]
- 11.Mattila VM, Niva M, Kiuru M, Pihlajamaki H. Risk factors for bone stress injuries: a follow-up study of 102,515 person-years. Med Sci Sports Exerc. 2007;39:1061–1066. doi: 10.1249/01.mss.0b013e318053721d. [DOI] [PubMed] [Google Scholar]
- 12.McClellan JWr, Vernon BA, White MA, Stamm S, Ryschon KL. Should 25-Hydroxyvitamin D and bone density using DXA be tested in adolescents with lumbar stress fractures of the Pars Interarticularis? J Spinal Disord Tech. 2011 doi: 10.1097/BSD.0b013e31823f324f. [DOI] [PubMed] [Google Scholar]
- 13.Lappe JM, Stegman MR, Recker RR. The impact of lifestyle factors on stress fractures in female Army recruits. Osteoporos Int. 2001;12:35–42. doi: 10.1007/s001980170155. [DOI] [PubMed] [Google Scholar]
- 14.Marx RG, Saint-Phard D, Callahan LR, Chu J, Hannafin JA. Stress fracture sites related to underlying bone health in athletic females. Clin J Sport Med. 2001;11:73–76. doi: 10.1097/00042752-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Teng K. Premenopausal osteoporosis, an overlooked consequence of anorexia nervosa. Cleve Clin J Med. 2011;78:50–58. doi: 10.3949/ccjm.78a.10023. [DOI] [PubMed] [Google Scholar]
- 16.Koh JS, Goh SK, Png MA, Kwek EB, Howe TS. Femoral cortical stress lesions in long-term bisphosphonate therapy: a herald of impending fracture? J Orthop Trauma. 2010;24:75–81. doi: 10.1097/BOT.0b013e3181b6499b. [DOI] [PubMed] [Google Scholar]
- 17.Isaacs JD, Shidiak L, Harris IA, Szomor ZL. Femoral insufficiency fractures associated with prolonged bisphosphonate therapy. Clin Orthop Relat Res. 2010;468:3384–3392. doi: 10.1007/s11999-010-1535-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bennelle KL, Malcolm SA, Thomas SA, Wark JD, Brukner PD. The incidence and distribution of stress fractures in competitive track and field athlete. A twelve month prospective study. Am J Sports Mea. 1996;24:211–217. doi: 10.1177/036354659602400217. [DOI] [PubMed] [Google Scholar]
- 19.Tárraga López Pedro J, et al. Osteoporosis in patients with subclinical hypothyroidism treated with thyroid hormone. Clinical Cases in Mineral and Bone Metabolism. 2011;8(3):44–48. [PMC free article] [PubMed] [Google Scholar]
- 20.Waring Avantika C. et al. A prospective study of thyroid function, bone loss, and fractures in older men: The MrOS study. Journal of Bone and Mineral Research. 2013;28(3):472–479. doi: 10.1002/jbmr.1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vestergaard P, Mosekilde L. Fractures in patients with hyperthyroidism and hypothyroidism: a nationwide follow-up study in 16,249 patients. Thyroid. 2002 May;12(5):411–9. doi: 10.1089/105072502760043503. [DOI] [PubMed] [Google Scholar]
- 22.Frediani B, Cavalieri L, Cremonesi G. Clodronic acid formulations available in Europe and their use in osteoporosis: a review. Clin Drug Investig. 2009;29(6):359–79. doi: 10.2165/00044011-200929060-00001. [DOI] [PubMed] [Google Scholar]