Summary
Background and aims
Although several studies have demonstrated a higher incidence of bone disorders in HCV-infected adults, the bone turnover alterations occurring in children and adolescents with chronic hepatitis C has not been thoroughly focused yet. We performed a study on a cohort of 30 HCV infected caucasian children and adolescents to assess the prevalence of osteodystrophy and evaluate a possible prophylactic and therapeutic approach.
Methods
Data regarding biochemical markers of bone metabolism were collected. Moreover, results of ultra-sonographic bone densitometry yearly performed were evaluated in comparison with data obtained from more than 500 healthy children and adolescents.
Results
Osteocalcin and telopeptide of the collagen molecule type-1, CTX, appeared higher than normal in 8/30 and in 7/30 cases respectively; the 25OH vitamin D values were normal in 25/28 cases. By densitometry osteoporosis was detected in 2 patients and osteopenia in other 5. After stratification of cases by age groups, the incidence of osteopenia/osteoporosis appeared higher among children than among adolescents. Osteocalcin levels tended to be higher in cases where hepatic fibrosis were not detected.
Conclusions
The higher number of cases of osteopenia/osteoporosis in children than in adolescents is worthy of note, although not statistically significant. Ultrasound densitometry confirmed its important early diagnostic role in asymptomatic HCV infected children; moreover, also the increase in serum levels of osteocalcin may be considered as early marker of osteodystrophy of complementary value.
Larger studies will be needed to confirm the efficacy and safety of antiviral and supportive care in these patients.
Keywords: bone disorders, childhood, chronic HCV infection
Introduction
A reduced bone mineral density (BMD) due both to a lowered physiological bone turnover and to limited osteosynthesis processes is among the extrahepatic complications most frequently identified in adults suffering from end-stage liver disease. The incidence of osteopenia and osteoporosis is particularly high in cases of primary biliary or alcoholic cirrhosis (20–60% of cases) as well as in chronic HBV or HCV related hepatopathies which have become the first cause of hepatic cirrhosis over the past decade (1–3).
Several hormonal, toxic and metabolic factors may intervene in the pathogenesis of hepatic osteodystrophy; these also combine with secondary factors (nutritional deficits, malabsorption, inactivity) and with the speed of hepatic damage progression.
In particular “low turnover” osteoporosis is determined by the reduced hepatic synthesis of IGF-1, hyperbilirubinemia and plasma retention of other substances linked to cholestasis, which can inhibit osteoblastic activity.
On the other hand in the pathogenesis of “high turnover” osteoporosis (characterized by an increased osteoclast activity) a deficit in vitamin D, calcium and serum phosphates is a determining factor and results in parathyroid hormone (PTH) hyperincretion which stimulates osteoclast function.
Recent studies show a comparable prevalence for “high- and low turnover” osteoporosis in cases of cirrhosis and also highlight a significant correlation between the rapid progression of liver disease and the onset of osteoporosis, with a reduction of bone density mainly evident at lumbar vertebrae and hip joint (3).
Only few reports have been published about bone disorders in children and adolescents with liver disease. Generally most forms of chronic hepatopathy in this population are of viral origin and represent the consequence of vertical or transfusional transmission. Available data about the prevalence of bone disorders are limited mainly because of the low number of patients evaluated, included in studies with the aim just to define the pathogenetic role of hormones (such as PTH) and their mediators with osteoblasts, such as IGF-1 and TGF-beta (4, 5).
On the contrary, our study is aimed to evaluate not only the prevalence of decreased bone mineral density in a cohort of HCV infected children, adolescents and young adults but also to define an algorithm for early diagnosis of bone disorders in people affected with chronic liver disease acquired perinatally or in the early years of life.
Patients and methods
30 caucasian patients (13 males – 17 females) aged 5–31 years (median 16.5 years) with chronic hepatitis C were followed at the Department of Infectious Diseases of the University of Pavia.
They had neither clinical or laboratory evidence of cholestasis nor had received steroid therapy or parenteral nutrition. Endocrine disorders (such as thyroid or sexual hormones dysfunctions) or gastrointestinal disease (malabsorption or celiac disease) were ruled out in all of them. Each patient followed a balanced diet with regular calcium intake.
All patients underwent clinical examination and anthropometric measurements.
The diagnosis of chronic HCV hepatitis was assessed by the evidence of plasma HCV-RNA in at least two determinations; the viral genotype was identified in every case. In a subgroup analysis the patients were divided on the basis of HCV-RNA plasma level (lower or higher than 600,000 UI/ml). In all of them the clinical outline was determined by measurement of alanine transaminases (ALT) levels (expressed as a median value drawn from the results of the previous two years of follow-up). Fibrosis score was based on histological evaluation of tissue samples obtained with liver biopsy or, alternatively, by performing ultrasound elastography (Fibroscan).
The diagnosis of osteodystrophy was based on biochemical and instrumental analysis. The former (carried out with quarterly frequency over 18 months of monitoring) included, in addition to evaluation of serum level of calcium, inorganic phosphates and alkaline phosphatase, the measurement of serum osteocalcin (as an index of osteosynthesis), of C-terminal telopeptide of the collagen molecule type 1 (CTX), selected as bone reabsorption index, and the serum 25(OH) vitamin D determination.
26/30 patients annually underwent ultrasound measurement of bone density with the Omnisense device (Sunlight Technologies, Rehovot, Israel). This analysis is based on measurement of the speed of propagation of ultrasound throughout the bone, performed at proximal phalanx of the middle finger, shin bone and radius distal segment. For patients younger than 20 years, WHO criteria for the diagnosis of osteoporosis were adopted: T-score level between +1 and −1 SD (Standard Deviation) compared to the median value calculated for the population in young-adult age was considered normal; where T-score was between −1 and −2.5 SD osteopenia was diagnosed, while T-score values <−2.5 SD indicate osteoporosis. The Omnisense device only provides a “generic” pediatric reference curve for children aged from 0 to 12 years; nevertheless, the values in childhood may differ greatly because of various factors such age, sex, race, environmental factors and bone segment examined.
Therefore the data obtained from studied children and adolescents were correctly evaluated on the basis of an Italian study carried out with the same method on a population of 533 healthy children, adolescents and young adults aged between 5 and 20 years. This study provided the first Italian reference curve for the age group, with a variation in median values for males and females which differs from the values of the Omnisense database (6).
Statistical analysis
To assess whether the percentage of osteopenia and osteoporosis was significantly different in HCV infected patients compared to controls the binomial test was used.
The non-parametric Wilcoxon test was used to assess whether or not the osteocalcin and CTX values were modified (I) in patients with osteopenia/osteoporosis, (II) in patients with different stages of the liver disease and (III) in subjects with different HCV-RNA values.
The comparison between those groups was also performed after dichotomizing values of osteocalcin and CTX in the two classes normal/altered. In this case the differences between the groups were evaluated using the chi-square test and Fisher’s exact test (when the expected counts for more than 20% of cells were lower than 5). Descriptive statistics using mean, standard deviation, range, median and quartiles were also conducted. Distributions of the variables in the different groups of subjects were visualized using the boxplot graphical technique. In a boxplot, the median is shown as a line within the box, while the lower and upper edges of the box indicate the 25th and 75th percentiles (Inter-Quartile range). The whiskers above and below the box extend to the most extreme data points that are not considered as outliers, i.e. not extending more than 1.5 times the box length from the edge of the box. Outliers, if any, are shown as individual lines.
Results
The features of cases evaluated are listed in Table 1.
Table 1.
Baseline demographic, clinical and virological characteristics of studied population. Focus on biochemical markers of bone turnover and bone mineral density.
| PATIENTS | n. of cases | %/total |
|---|---|---|
| Age | ||
| range | 7 – 32 | |
| 7 – 15 y | 15 | 50 |
| 16 – 25 y | 10 | 33.3 |
| > 25 y | 5 | 16.7 |
| Sex | ||
| male | 13 | 43.4 |
| female | 17 | 56.6 |
| Transmission | ||
| vertical | 20 | 66.7 |
| transfusional | 8 | 26.7 |
| Unknown | 2 | 6.6 |
| HCV-RNA | ||
| ≥ 600,000 UI/ml | 11 | 63.3 |
| < 600,000 UI/ml | 19 | 36.7 |
| Genotype | ||
| 1 | 15 | 52 |
| 2 | 3 | 10 |
| 3 | 7 | 24 |
| 4 | 4 | 14 |
| BMI | ||
| range | 15.7 – 34.1 | |
| mean ± SD | 22.09 ± 4.05 | |
| ALT (mU/ml) | ||
| range | 11 – 105 | |
| mean ± SD | 41.9 ± 23.77 | |
| Fibrosis | ||
| 0 | 19 | 70 |
| 1 | 8 | 30 |
| US-Densitometry | ||
| Normal | 20 | 74.1 |
| Osteopenia | 5 | 18.5 |
| Osteoporosis | 2 | 7.4 |
| C-terminal Telopeptyde (ng/ml) | ||
| Normal value | 0.118 – 0.504 | |
| range | 0.06 – 2.52 | |
| mean ± SD | 0.962 ± 0.613 | |
| Osteocalcin (ng/ml) | ||
| Normal value | 15 – 70 | |
| range | 6.6 – 127.7 | |
| mean ± SD | 59.4 ± 37.5 | |
| 25 OH Vitamin D (nmol/L) | ||
| Normal value | 23 – 113 | |
| range | 16.9 – 113.7 | |
| mean ± SD | 60.45 ± 27.46 | |
In all patients the clinical outline was asymptomatic while ALT levels appear above normal in more than 50% of them.
In ten cases hepatic biopsy was performed, on the basis of which mild chronic hepatitis was diagnosed at stage 0 in three of them and at stage 1 in the remaining seven; in other seventeen cases the quantitative evaluation of liver fibrosis with Echosense Fibroscan device showed hepatic elasticity corresponding to absence of fibrosis in 16 cases and one case of mild fibrosis.
About the bone metabolism analysis, the serum levels of calcium, phosphates and alkaline phosphatase resulted always normal in all cases.
Densitometry highlighted osteodystrophy in 7 patients (27% of the whole number of examined cases): osteoporosis was diagnosed in 2 and osteopenia in 5 of them respectively.
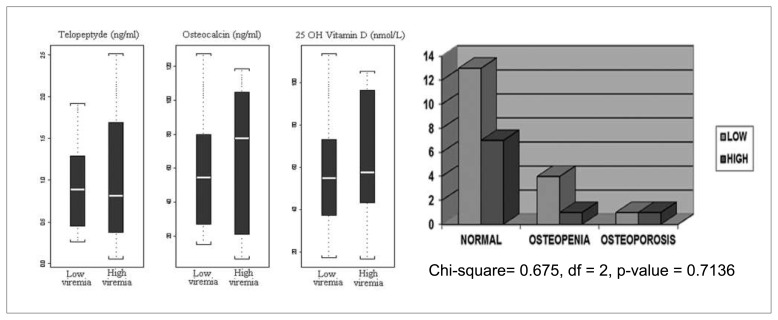
A relation between densitometric results and high serum levels of osteocalcin and CTX was observed just in one case of osteoporosis and in two cases of osteopenia. As shown in Figure 1 no relation has been found between low or high level of viremia and alterated biochemical markers of bone turnover or reduced bone mineral density (p = 0.7136); similarly, no statistical differences have been found between the activity of hepatitis (expressed by ALT value) and the incidence of bone disorders.
Figure 1.
Distribution of markers of bone turnover and bone mineral density in patients with low or high viremia (HCV-RNA respectively < or ≥ 600.000 UI/ml).
The densitometric data of the followed patients were compared with those of healthy subjects (divided into the same age bands): as shown in Table 2 statistical analysis of results did not reveal a higher incidence of altered bone mineralization in HCV-infected patients (p = 0.912). However, after stratification of cases by age groups a higher incidence of bone disorders in subjects younger than 15 years than in older ones was observed (p = 0.0577, Table 3).
Table 2.
Distribution of normal, osteoporotic and osteopenic cases in HCV - negative and positive populations.
| HCV-positive subjects | Reference HCV-negative population (control) | |
|---|---|---|
| Normal | 20 | 376 |
| Osteopenia | 5 | 107 |
| Osteoporosis | 2 | 50 |
| Total | 27 | 533 |
Chi-square test = 0.1842, df = 2, p-value = 0.912
Table 3.
Stratification of bone disorders by age groups.
| Normal | Osteopenia | Osteoporosis | |
|---|---|---|---|
| ≥ 15-y-old | 15 | 1 | 1 |
| < 15-y-old | 5 | 4 | 1 |
Fisher’s exact test
p-value = 0.0577
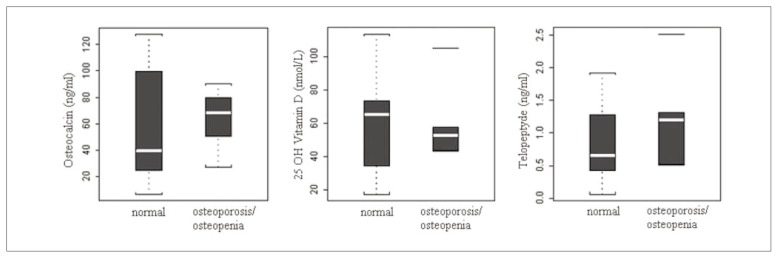
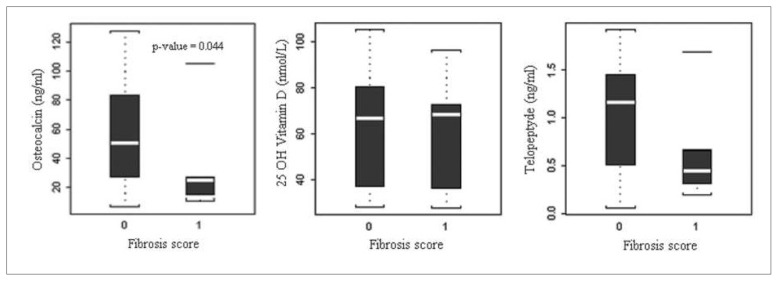
When biochemical parameters of bone metabolism are considered, no statistically significant differences appear between patients with bone loss and those with normal densitometric results (Figure 2), but osteocalcin serum levels tend to be higher in cases where the histological examination of liver biopsy or Fibroscan evaluation did not evidence fibrous areas, compared with patients with proven, although mild, alteration of hepatic structure (p=0.04, Figure 3). The degree of liver fibrosis, however, doesn’t appear to be correlated with the value of the other bone markers.
Figure 2.
Distribution of markers of bone turnover in patients with different bone mineral density.
Figure 3.
Distribution of markers of bone turnover in patients with different fibrosis score.
Discussion
Although no significant increase in the risk of osteodystrophy was found in the sample, the high number of cases of osteopenia/osteoporosis detected in the 5–15 years age band (38% of the tested subjects) is worthy of note: it includes 3 males (7–13 years) and 2 females (12–14 years) vertically infected with normal liver function, unaltered hepatic structure and no anamnestic risk factors of altered bone metabolism beyond the chronic viral infection.
Densitometry confirmed its important early role in highlighting osteopenia or osteoporosis in asymptomatic children and adolescents and its safety, because the use of ultrasound makes it possible to carry out close-up evaluation of bone mineralization even in infants and children avoiding their exposure to X-rays, on which more traditional diagnostic methods such as Dual-Energy X-ray Absorptiometry (DEXA) are based.
As in the examined cases the concentration of serum osteocalcin reached highest levels in cases where no liver fibrosis was detected we can conclude that an increased level of this marker of osteosynthesis may be considered as an early index of osteodystrophy of complementary value.
Finally, we didn’t observe any significant alteration in vitamin D metabolism in our patients, probably because of the normal liver function and parenchymal architecture detected in about 80% of them, while low serum vitamin D levels are often demonstrated in adults affected by end- stage liver disease with advanced osteoporosis (7).
The long course of chronic liver disease acquired perinatally or in early age can lead to bone disorders even in children and adolescents with a still regular liver function (2, 3), so it is possible to speculate that also in childhood and adolescence HCV infection can be related with a high risk of bone fragility fractures which often remain undiagnosed for a long time and may cause continuous functional impairment (8).
Because of the availability of diagnostic instruments that can early highlight bone turnover alterations, preventive strategies are to be adopted in all HCV-infected children and adolescents.
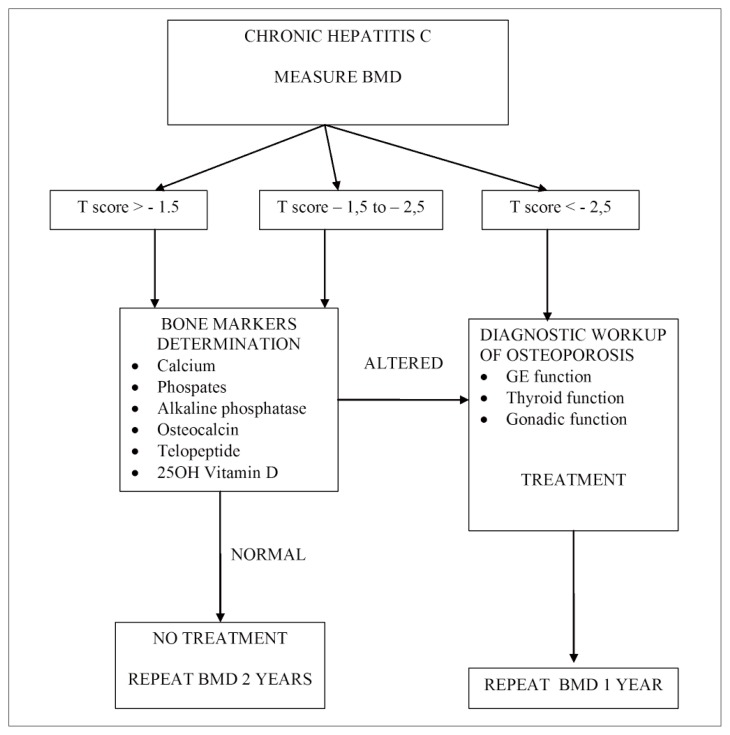
Figure 4 shows a summary of possible strategies for the diagnosis and management of bone disorders in children and adolescents with chronic hepatitis. Bone metabolism parameters should be monitored at least twice a year while ultrasound bone densitometry should be performed once a year as from the first year of life in all of them. Moreover, careful attention to dietary calcium intake, regular physical activity and vitamin D levels are the key points to observe.
Figure 4.
Algorithm of proposed strategy for diagnosis and treatment of bone disorders in children and adolescents with chronic hepatitis.
Clear guidelines for the management of osteopenia and osteoporosis in children and adolescents are not widely accepted yet because only few data regarding cases of bone density reduction in pediatric population are still available, but it is possible to assess a program to better monitor these patients by drawing some indications from recent multicenter studies.
First of all, an increased weight bearing physical activity during 12–18 years of age has been demonstrated to be correlated with bone mass formation; moreover, the effects of activity on bone health become more evident and lasting when the daily oral intake of calcium and proteins is adequate and the composition of entire diet improve the ingested calcium absorption (9, 10).
Although no direct correlation between low vitamin D serum levels and fracture risk was demonstrated in children with osteodystrophy, a vitamin D supplementation is advisable and may reduce morbidity in these subjects (11).
With regard to the pharmacological treatment of bone disorders in children, bisphosphonate therapy must be seen as an essential component of a complex therapeutic regimen for primary or secondary osteoporosis. Recently the use of these drugs is increasing even in pediatric population and their positive effect in improving bone mineral density is encouraging; nevertheless, the optimal duration of oral or intravenous therapies is unknown and their effectiveness in fracture prevention and their long-term efficacy and safety is still uncertain (12).
Finally, in HCV infected young patients the most effective strategy against the underlying disease is based on the combination of Pegylated Interferon (PEG-IFN) and Ribavirin and may contribute to the secondary osteopenia and osteoporosis management. These drugs, administered following specific protocols, are expected to give effective results in reducing the incidence of osteodystrophy not only on the basis of their antiviral activity but also because of the IFN demonstrated property to inhibit the synthesis of osteoclast-like cells in vivo and to reduce the urinary excretion of polypeptides deriving from collagen break-up in HCV infected subjects (2, 13).
Larger studies will be required focusing on the natural history of the HCV infection perinatally transmitted or acquired early in life to better assess the actual incidence of HCV related risk of bone disease; further data about the efficacy and safety of the treatment of infected children and adolescents with antiviral drugs and the use of different bisphosphonates (which vary in potency and method of administration) will allow to optimize the multi-disciplinary prophylactic and therapeutic approach to these subjects.
Footnotes
Disclosures
The authors have no conflicts of interest or funding to disclose.
References
- 1.Gallego-Rojo FJ, Gonzalez-Calvin JL, Munoz-Torres M, Mundi JL, Fernandez-Perez L, Rodrigo-Moreno D. Bone mineral density, serum insulin-lìke growth factor I and bone turnover markers in viral cirrhosis. Hepatology. 1998;28:695–99. doi: 10.1002/hep.510280315. [DOI] [PubMed] [Google Scholar]
- 2.Rouillard S, Lane NE. Hepatic osteodystrophy. Hepatology. 2001;33:301–07. doi: 10.1053/jhep.2001.20533. [DOI] [PubMed] [Google Scholar]
- 3.Crawford BA, Kam C, Donaghy AJ, McCaughan GW. The eterogeneity of bone disease in cirrhosis: a multivariate analysis. Osteoporosis Int. 2003;14:987–94. doi: 10.1007/s00198-003-1495-z. [DOI] [PubMed] [Google Scholar]
- 4.Seibel MJ. Bone metabolism, mineral homeostasis and its pharmacological modulation. Clin Lab. 2004;50:255–64. [PubMed] [Google Scholar]
- 5.Mahdy KA, Ahmed HH, Manaa F, Abdel-Shaheed A. Clinical benefits of bìochemical markers of bone turnover in Egyptian children with chronic liver disease. World J Gastroenterol. 2007;13:785–90. doi: 10.3748/wjg.v13.i5.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pedrotti L, Bertani B, Tuvo G, Barone F, Crivellari I, Lucanto S, et al. Evaluation of bone density in infancy and adolescence. Review of medical lìterature and personal experience. Clin Cases Min Bone Metab. 2010;7:102–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Crosbie OM, Freaney R, McKenna MJ, Hegarty JE. Bone density, vitamin D status and disordered bone remodelling in end-stage chronic liver disease. Calcif Tissue Int. 1999;64:295–300. doi: 10.1007/s002239900622. [DOI] [PubMed] [Google Scholar]
- 8.Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271–8. doi: 10.1002/hep.21852. [DOI] [PubMed] [Google Scholar]
- 9.Rideout CA, McKay HA, Barr SI. Self-reported lifetime physical activity and areal bone mineral density in healthy postmenopausal women: the importance of teenage activity. Calcif Tissue Int. 2006;79:2014–22. doi: 10.1007/s00223-006-0058-7. [DOI] [PubMed] [Google Scholar]
- 10.Chevalley T, Bonjour JP, Ferrari S, Rizzoli R. High protein intake enhances the positive impact of physical activity on BMC in prepubertal boys. J Bone Mineral Res. 2008;23:131–42. doi: 10.1359/jbmr.070907. [DOI] [PubMed] [Google Scholar]
- 11.Bowden SA, Robinson RF, Carr R, Mahan JD. Prevalence of Vitamin D deficiency and insufficiency in children with osteopenia or osteoporosis referred to a pediatric metabolic bone clinic. Pedìatrics. 2008;121:e1585–90. doi: 10.1542/peds.2007-2111. [DOI] [PubMed] [Google Scholar]
- 12.Uziel J, Zifman E, Hashkes PJ. Osteoporosis in children: pediatric and pediatric rheumatology perspective: a review. Pediatric Rheumatology. 2009;7:7–16. doi: 10.1186/1546-0096-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miki T, Yoshida H, Shioi A. Effect of interferon alpha on bone metabolism in patients with chronic hepatitis. J Bone Miner Metab. 1993;11:39–44. [Google Scholar]