Abstract
Purpose/Objectives
To explore ethnic differences in psychological distress and social withdrawal after receiving an abnormal mammogram result and to assess if coping strategies mediate ethnic differences.
Design
Descriptive correlational.
Setting
Two urban mobile mammography units and a rural community hospital in the state of Washington.
Sample
41 Latina and 41 non-Latina Caucasian (NLC) women who had received an abnormal mammogram result.
Methods
Women completed standard sociodemographic questions, Impact of Event Scale–Revised, the social dimension of the Psychological Consequences Questionnaire, and the Brief COPE.
Main Research Variables
Ethnicity, psychological distress, social withdrawal, and coping.
Findings
Latinas experienced greater psychological distress and social withdrawal compared to NLC counterparts. Denial as a coping strategy mediated ethnic differences in psychological distress. Religious coping mediated ethnic differences in social withdrawal.
Conclusions
Larger population-based studies are necessary to understand how ethnic differences in coping strategies can influence psychological outcomes. This is an important finding that warrants additional study among women who are and are not diagnosed with breast cancer following an abnormal mammogram.
Implications for Nursing
Nurses may be able to work with Latina patients to diminish denial coping and consequent distress. Nurses may be particularly effective, given cultural values concerning strong interpersonal relationships and respect for authority figures.
Keywords: breast cancer, coping, cultural competence, Hispanic, prevention, detection, quality of life
Breast cancer continues to be a leading cause of death for non-Latina Caucasian (NLC) and Latina women in the United States (American Cancer Society, 2012, 2014a). Although the incidence of breast cancer among Latinas is lower relative to NLC women, Latinas are more likely to be diagnosed at later stages (Lantz et al., 2006; Siegel, Naishadham, & Jemal, 2012) and die of diagnosed breast cancer (Jemal et al., 2004; Ooi, Martinez, & Li, 2011). Latina patients with breast cancer and survivors appear to have lower quality of life, including poorer emotional and social functioning, compared to NLC counterparts (Bickell et al., 2006; Fedewa, Ward, Stewart, & Edge, 2010). A large body of literature exists that has characterized and addressed modifiable factors associated with early detection of breast cancer, including promotion of mammography screening among Latinas (Guerra, Krumholz, & Shea, 2005; Molina, Thompson, Espinoza, & Ceballos, 2013; Purc-Stephenson & Gorey, 2008; Santiago-Rivera, Arrendondo, & Gallardo-Cooper, 2002). However, little research exists to date of quantified ethnic differences in mental health comorbidities after abnormal screening results. Psychological distress is particularly important among women who receive an abnormal mammogram result, given short- and long-term consequences related to early detection and the persistence of elevated distress as long as six months following receipt of results (Bond et al., 2013; Brewer, Salz, & Lillie, 2007; Hafslund, Espeghaug, & Nortvedt, 2012; Keyzer-Dekker et al., 2012; Salz, Richman, & Brewer, 2010).
A large body of research has characterized elevated psychological distress and anxiety among women who receive an abnormal screening result, which requires further evaluation. Most research has focused on predominantly NLC women or has not addressed racial or ethnic differences (Andrés-Hyman, Ortiz, Añez, Paris, & Davidson, 2006; Molina et al., 2013). Although the authors of the current article found no study that compared distress among Latinas and NLC women, one qualitative study with a largely Latina sample noted that psycho logical distress interfered with motivation to schedule a follow-up appointment (Allen, Shelton, Harden, & Goldman, 2008). A quantitative study found that fear of a cancer diagnosis was more strongly associated with delays in follow-up care adherence among Latina breast and cervical cancer survivors (Ashing-Giwa et al., 2010). In addition to psychological distress, receiving abnormal mammography results may also affect social functioning. Some studies have indicated that receipt of an abnormal mammogram may result in negative social consequences, including withdrawal from one's family and friends (Austin, Ahmad, McNally, & Stewart, 2002; Cockburn, De Luise, Hurley, & Clover, 1992; Lowe, Balanda, Del Mar, & Hawes, 1999). Conversely, social support has been seen as protective with regard to reduced psychological distress (Andrés-Hyman et al., 2006; Molina et al., 2013; Montgomery, 2010). Social withdrawal may be particularly problematic for Latinas, given the cultural importance placed on strong interpersonal relationships (Marin & Marin, 1991). Little research has explored social withdrawal or other aspects of psychological functioning after an abnormal mammogram among Latinas.
Coping has been linked to psychological distress and well-being across the cancer continuum (Boinon, Charles, Dauchy, & Sultan, 2011; Bond et al., 2013; Kreuter & McClure, 2004), including in response to an abnormal mammogram result (Andrés-Hyman et al., 2006; Austin et al., 2002; Molina et al., 2013; Montgomery, 2010; Moy, Park, Feibelmann, Chiang, & Weissman, 2006). Ethnic differences in coping are largely unknown in the context of the abnormal mammography experience, but hypotheses can be drawn from existing literature on Latinas’ coping strategies in other phases of the cancer continuum. Ethnic differences in coping along the cancer continuum have largely focused on coping during treatment and survivorship. Latinas are more likely to employ religious coping (e.g., prayer) (Ashing-Giwa et al., 2004; Culver, Arena, Antoni, & Carver, 2002; Culver, Arena, Wimberly, Antoni, & Carver, 2004; Lopez-Class, Gomez-Duarte, Graves, & Ashing-Giwa, 2012) and avoidant coping strategies (e.g., denial, self-distraction) (Culver et al., 2002; Umezawa et al., 2012) than their NLC counterparts. With regard to early detection, a few studies have assessed coping in relation to ethnic screening. For example, avoidant coping has been suggested to vary in its effect on mammography screening among different groups of Latinas (Kudadjie-Gyamfi & Magai, 2008).
Ethnic differences in coping may influence the amount and types of negative psychosocial consequences women face (Bond et al., 2013). Religious or spiritual (Alderete, Juarbe, Kaplan, Pasick, & Pérez-Stable, 2006) and avoidant coping strategies (Chen et al., 1996; Pakenham, Clutton, & Buckley, 1999; Heckman et al., 2004; Montgomery, 2010) have been specifically linked to psychological distress following receipt of an abnormal mammogram. In a sample including Latina and NLC women, regular attendance at religious services was related to lower levels of depressive symp toms (Alderete et al., 2006), but ethnic comparisons were not conducted. Coping may also be associated with decisions to withdraw from family and friends after receipt of abnormal screening results. One study found that NLC women undergoing diagnostic procedures relied on religious coping and simultaneously isolated themselves from family (Logan, Hackbusch-Pinto, & De Grasse, 2006).
Exploration of ethnic differences in coping may be integral to promoting positive psychological well-being. This study draws on a conceptual framework developed by Folkman and Lazarus (1988), in which coping is conceptualized as a mediator between stressful situations and emotional reactions to stressors. In the current article, the authors posit that ethnic differences may exist in coping after receipt of an abnormal mammogram result, which is potentially because of multiple contextual factors including culture and stressors associated with socioeconomic position. Ethnic differences in coping may result in ethnic differences in emotional reactions (e.g., distress and social withdrawal) to cancer- specific stressors (e.g., an abnormal mammogram result). Previous research on patients with cancer and survivors support this conceptual framework. Ethnic differences exist in emotional responses to stressful circumstances, such as cancer treatment and survivorship (Ashing-Giwa et al., 2004; Culver et al., 2002, 2004). Other work has suggested differences in psychological well-being and quality of life, in which Latina patients with cancer and survivors exhibited lower quality of life relative to NLC counterparts (Ashing-Giwa, Padilla, Bohórquez, Tejero, & Garcia, 2006; Janz et al., 2009). Documented ethnic differences in coping may result in lower quality of life among patients and survivors. However, little research to date has examined this relationship. In addition, these relationships may begin before the cancer diagnosis, such as after receipt of an abnormal mammogram, and may exist among women who receive an abnormal mammogram result but are not diagnosed with breast cancer. Understanding the role of coping strategies in associations between ethnicity, psychological distress, and social withdrawal is warranted. If Latinas and NLC women cope differently, these differences in coping strategies may be related to ethnic variation found in psychological distress and social withdrawal and should be targeted in future interventions and in healthcare practice to improve the psychological health of ethnically diverse screening populations.
This pilot study has two primary objectives: (a) to explore ethnic differences in psychological distress, social withdrawal, and coping strategies after receipt of an abnormal mammogram result among two convenience- based samples of Latinas and NLC women and (b) to assess the mediating role of coping strategies in relation to ethnicity, psychological distress, and social withdrawal. The current study seeks to address this gap in the literature and provide pilot data for the development of psychological interventions and evidence-based nursing practices to improve the psychological well-being of Latinas who receive an abnormal mammogram result.
Methods
Procedures
The current research is part of an exploratory mixed-methods project addressing stress and coping following receipt of an abnormal mammogram among 41 Latinas and 41 NLC women living in the state of Washington. The multiphased project was reviewed and approved by the institutional review board at the Fred Hutchinson Cancer Research Center in Seattle, Washington. The authors’ study sites included two mobile mammography services within urban areas of western Washington (e.g., Seattle) and a community hospital with a radiology department within a rural area of eastern Washington (i.e., Yakima). The majority of Latina (n = 34 of 41) and NLC (n = 36 of 41) participants were recruited from the urban mobile mammography sites. The authors employed a two-step process to recruit a convenience sample of Latinas and NLC women who had received an abnormal mammogram result. For the first step, clinic staff approached potential participants during initial mammography appointments and described the study. Women who indicated interest during the initial appointment and subsequently received an abnormal mammogram result were contacted via telephone by researchers. For the second step, the authors contacted all women requiring follow-up care of some sort (e.g., diagnostic mammogram, ultrasound) with mailed materials, including a generic letter of approach from the clinic sites and a study brochure describing the project. Women were asked to initiate contact with research staff, if interested. About half of the participants (n = 48) indicated interest during the first step of the recruitment process and received mailed materials as part of the second step. The other 34 participants did not indicate interest during the initial appointment but indicated subsequent interest when recruited at the second step with mailed study materials. Strategies were used in tandem to generate a sufficient sample to test the objectives described above. Preliminary analyses revealed no significant differences in study variables of interest (i.e., ethnicity, coping, distress, and social withdrawal) by clinic or recruitment strategy (p > 0.35).
Interested women were screened according to eligibility criteria including self-identification as Hispanic, Latina, or Chicana or as European American, White, or Caucasian; being aged between 40–74 years; receipt of an abnormal mammogram result within the past month; and no prior personal history of breast cancer. Subsequent interviews were conducted for 25–35 minutes by a bicultural, bilingual interviewer and included informed consent and questionnaire administration. All study materials were available in English and Spanish. Interviews were conducted according to participants’ language preferences. Thirty-three NLC women and 33 Latinas preferred telephone interviews, four NLC women and one Latina mailed completed interview schedules, and one NLC woman and five Latinas had inperson interviews. Inperson interviews were conducted in research staff's offices or in public venues (e.g., libraries). Preliminary analyses revealed no significant differences in study variables of interest by type of interview (p = 0.31).
Measures
Sociodemographic and mammography-related variables
Standard census demographic questions were used to collect data on ethnicity, age, education, personal annual income, insurance status, nationality, and language preference. Mammography and other breast healthcare use history was ascertained from self-report and electronic medical records for women who completed Health Insurance Portability and Accountability Act forms.
Psychological distress
To address psychological distress, the authors administered the Impact of Event Scale–Revised, which has been validated in English and Spanish (Horowitz, Wilner, & Alvarez, 1979; Requena & Gil Moncayo, 2007; Weiss, 2007). The avoidance and intrusion subscales have been suggested to be relevant for different traumatic events of varying severity, in contrast to the hyperarousal subscale (Sundin & Horowitz, 2002). To minimize patient burden, the authors only administered the avoidance and intrusion subscales. Sample items of the 15 items associated with these subscales are, respectively, “I am aware that I have a lot of feelings about my results, but I haven't dealt with them” and, “I have had waves of strong feelings about my results.” Response categories included 0 indicating not at all, 1 indicating a little bit, 2 indicating moderately, 3 indicating quite a bit, and 4 indicating extremely. To create summary scores, the authors calculated summary scores for sub-scales, which were means of all items, and then added the scores together to create an overall score. The Cronbach alpha for this instrument was 0.9 in the current sample.
Social withdrawal
To address social withdrawal, the authors administered the three-item negative social consequences subscale from the Psychological Consequences Questionnaire, which has been validated in English (Cockburn et al., 1992). Bicultural, bilingual interviews were forward- and back-translated for this subscale. The subscale was then validated through cognitive interviews with 19 Latinas who had experienced an abnormal mammogram result. Exploratory factor analysis revealed comparable loadings across English and Spanish versions. Response categories included 0 indicating not at all, 1 indicating rarely, 2 indicating some of the time, and 3 indicating quite a lot of the time. One of the items for this scale is, “As a result of thoughts about my abnormal mammogram result, I have found myself noticeably withdrawing from those who are close to me.” The Cronbach alpha for this instrument was 0.6 in the current sample.
Coping
For coping strategies, the authors administered the Brief COPE, whose reliability and validity have been established for English and Spanish versions (Carver, 1997; Perczek, Carver, Price, & Pozo-Kaderman, 2000). Each of the 14 subscales for this instrument includes two items. For all items, participants could choose 1 indicating, “I haven't been doing this at all,” 2 indicating, “I've been doing this a little bit,” 3 indicating, “I've been doing this a medium amount,” 4 indicating, “I've been doing this a lot,” and 5 indicating, “I've been doing an extreme amount.” Subscales varied substantially in reliability for this sample, so the authors included only the seven scales that exhibited adequate internal consistency (Cronbach alpha ≥ 0.6). The list of seven coping scales, including one of the two items that were administered and Cronbach alpha, are self- distraction (“I've been turning to work or other activities to take my mind off things,” Cronbach alpha = 0.78), denial (“I've been saying to myself, ‘This isn't real,” Cronbach alpha = 0.77), substance use (“I've used alcohol or other drugs to make myself feel better,” Cronbach alpha = 0.99), active (“I concentrated my efforts on doing something about the situation,” Cronbach alpha = 0.61), emotional support (“I've gotten comfort and understanding from someone,” Cronbach alpha = 0.92), humor (“I've made jokes about it,” Cronbach alpha = 0.87), and religious coping (“I've prayed or meditated about my results,” Cronbach alpha = 0.87).
Analysis
To identify covariates, the authors conducted Pearson's correlations and analysis of variance (ANOVA) for age, education, income, age at first mammogram, and number of mammograms obtained throughout the past five years. The authors used chi-square tests to assess ethnic differences in place of birth (U.S.- and foreign-born), language (English-speaking or not), employment status (unemployed or not), insurance status (uninsured or not), follow-up (yes or no), and days between the initial screening and subsequent follow-up appointment. The authors conducted two multivariate analysis of covariance (MANCOVA). The first MANCOVA included psychological distress and social withdrawal summary scores as outcome variables, and the second MANCOVA included the seven coping strategies as outcome variables. The authors then conducted mediation models for each outcome using the Preacher and Hayes (2008) method (Hayes, 2009; Hayes & Preacher, 2010). This bootstrap method is a nonparametric resampling procedure that involves sampling from the data set multiple times (5,000 for this study) and generating a sampling distribution. The authors calculated standard error and 95% confidence interval of the effect of ethnicity on psychological distress and social withdrawal through coping. For comparison, the authors also employed the traditional and common Sobel (1987) test of mediation; findings were similar across methods. Given that the Preacher and Hayes (2008) method is considered superior relative for testing mediation among small-to-moderate sample sizes (Fritz & MacKinnon, 2007), the authors only report those findings in the current article.
Results
Because very few cases were missing (less than 5%), the authors used listwise case deletions to accommodate them (Schafer & Graham, 2002). Table 1 provides sociodemographic and clinical variables. All women in this study were initially classified as category 0 in the BI-RADS® Atlas. The authors did not find significant evidence of ethnic differences in time to follow-up care, receipt of procedures, or breast cancer diagnoses. Several ethnic differences emerged; Latinas were less likely to speak English and more likely to have been born outside of the United States. Latinas also appeared to be more socioeconomically disadvantaged in terms of education, income, and insurance status relative to NLC counterparts. Sociodemographic and clinical variables (e.g., mammography history, receipt of specific diagnostic procedures) were largely not associated with distress, social withdrawal, and coping. Income was negatively correlated with denial coping (r = –0.35, df = 78, p = 0.002) and substance use (r = 0.25, df = 80, p = 0.03). Of note, follow-up care adherence and time to follow-up were not associated with distress, social withdrawal, or coping. Given the findings, education, income, and insurance status (i.e., having insurance) were included as covariates in subsequent analyses.
Table 1.
Sociodemographic and Mammography-Based Characteristics (N = 82)
| Latina (n = 41) |
NLC (n = 41) |
||||
|---|---|---|---|---|---|
| Variable | X̄ | SE | X̄ | SE | Fa |
| Age (years) | 48.83 | 6.18 | 50.34 | 7.12 | 1.06 |
| Income ($)** | 10,800 | 13,470 | 29,000 | 25,700 | 15.82 |
| Age at first mammogram (years) | 40.75 | 5.96 | 39.1 | 6.45 | 1.39 |
| Number of mammograms in past five years | 2.68 | 1.93 | 2.87 | 1.79 | 0.21 |
| Days until follow-up care | 26.34 | 16.89 | 21.72 | 12.71 | 1.79 |
| Variable | n | n | χ 2 | ||
|---|---|---|---|---|---|
| Foreign-born** | 36 | 3 | 53.25 | ||
| English-speaking** | 17 | 41 | 30.44 | ||
| High school degree or less* | 24 | 6 | – | ||
| Unemployed | 13 | 9 | 0.99 | ||
| Uninsured** | 29 | 10 | 17.65 | ||
| Follow-up care | |||||
| Diagnostic mammography | 36 | 37 | 1.76 | ||
| Ultrasounds | 15 | 15 | 0.86 | ||
| Biopsies | 2 | 16 | 2.47 | ||
| Cancer diagnosis | 1 | 3 | 1.67 | ||
NLC—non-Latina Caucasian; SE—standard error
F (1, 77–80)
p < 0.05
p < 0.001
Note. Education was included as a continuous variable in all analyses.
Note. Participants could experience multiple forms of follow-up care.
Ethnic Differences in Psychological Distress, Social Withdrawal, and Coping Strategies
Table 2 provides ethnic differences in psychological distress and coping strategies, after adjusting for the covariates noted previously. Latinas reported greater psychological distress and social withdrawal (Wilks’ lamda = 0.9, F[2, 73] = 4.12, p = 0.02). Most women appeared to employ active, emotional support, and spiritual or religious coping in response to an abnormal mammogram. After adjusting for education, income, and insurance status, Latinas and NLC women differed in coping (Wilks’ lamda = 0.65, F[7, 64] = 4.9, p < 0.0001). Subsequent analysis revealed that Latinas were more likely to employ denial and religious coping following receipt of an abnormal mammogram. A nonsignificant trend also occurred in which NLC women appeared to be marginally more likely to employ humor in coping (p = 0.09).
Table 2.
Ethnic Differences in Study Variables of Interest After Adjusting for Education, Income, and Insurance Status (N = 82)
| Latina (n = 41) |
NLC (n = 41) |
aOR (95% CI) | |||
|---|---|---|---|---|---|
| Variable | n | n | |||
| Scheduled follow-up care | 28 | 36 | 0.31 [0.0, 1.3] | ||
| Variable | X̄ | SE | X̄ | SE | F(1, 74) |
|---|---|---|---|---|---|
| Psychological distress** | 3.03 | 0.25 | 2.01 | 0.24 | 7.4 |
| Social withdrawal* | 2.95 | 0.41 | 1.65 | 0.4 | 4.31 |
| Variable | X̄ | SE | X̄ | SE | F(1, 70) |
|---|---|---|---|---|---|
| Coping strategies | |||||
| Self-distraction | 3.92 | 2.15 | 3.26 | 2.27 | 0.06 |
| Denial*** | 2.73 | 2.32 | 0.47 | 0.92 | 18.17 |
| Substance abuse | 0.05 | 0.33 | 0.21 | 1.02 | 0.001 |
| Active | 3.38 | 2.19 | 3.34 | 2.26 | 0.13 |
| Emotional support | 3.78 | 2.5 | 3.55 | 2.38 | 1.29 |
| Religious or spiritual | 4.65 | 2.5 | 2.71 | 2.6 | 11.41 |
| Humor | 0.49 | 1.26 | 1.42 | 2.07 | 2.89 |
p < 0.05
p < 0.01
p < 0.001
aOR—adjusted odds ratio; CI—confidence interval; NLC—non-Latina Caucasian; SE—standard error
Note. Psychological distress was measured using the Impact of Event Scale–Revised, social withdrawal was measured using the Psychological Consequences Questionnaire subscale, and coping strategies were measured using the Brief COPE.
Mediation Model
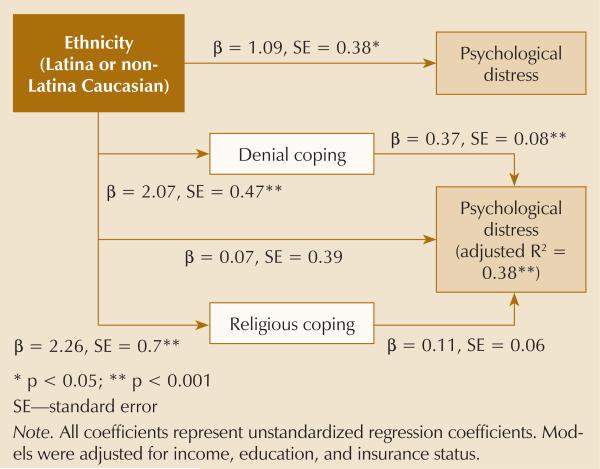
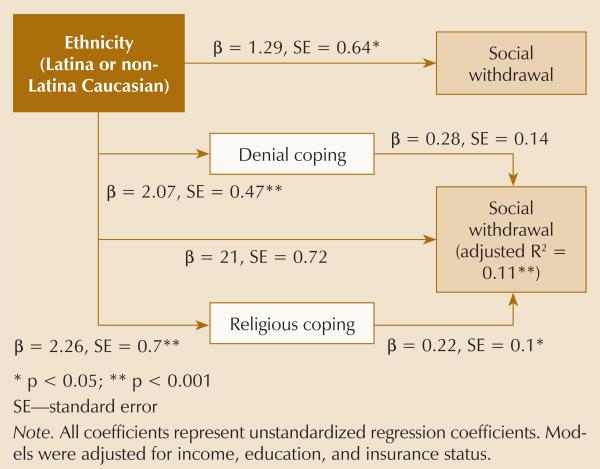
The authors conducted two mediation models to assess the role of denial and religious coping in ethnic differences in psychological distress and social withdrawal. Denial coping appeared to fully mediate differences between ethnicities in psychological distress (see Table 3 and Figure 1), and Latinas appeared to exhibit greater psychological distress as a result of employing more denial coping. Religious coping emerged as a significant mediator of ethnic differences in social withdrawal; Latinas were more likely to be socially withdrawn following receipt of an abnormal mammo-gram because of religious coping (see Figure 2).
Table 3.
Mediation of the Effects of Ethnicity on Denial and Religious Coping After Adjusting for Education, Income, and Insurance Status (N = 70)
| Model | Mediation Effect (A × B) | Bootstrap Results (95% CI) |
|---|---|---|
| Psychological distress | ||
| Denial copinga | 0.77 | [0.49, 1.71] |
| Religious coping | 0.25 | [0.0, 0.67] |
| Total indirect effectsa | 1.02 | [0.38, 1.98] |
| Social withdrawal | ||
| Denial coping | 0.58 | [–0.05, 1.57] |
| Religious copinga | 0.49 | [0.08, 1.18] |
| Total indirect effectsa | 1.08 | [0.32, 2.14] |
Significant effect as determined by 95% CI
CI—confidence interval
Figure 1.
Multiple Mediation Model of the Relationship of Ethnicity and Psychological Distress
Figure 2.
Multiple Mediation Model of the Relationship of Ethnicity and Social Withdrawal
Discussion
This exploratory study is among the first to assess ethnic differences in negative psychosocial outcomes following an abnormal mammogram and to assess the role of coping strategies as mediators in ethnic differences. The findings provide preliminary evidence that Latinas experience greater psychological and social withdrawal following receipt of an abnormal mammogram result compared to NLC counterparts. This pilot study suggests that these differences should be considered in the context of coping with abnormal mammogram results. Latinas appeared to experience greater psychological distress and negative social withdrawal through greater use of denial and religious coping, respectively. These findings are important first steps toward future projects with larger samples that may further assess differences in psychosocial factors following an abnormal mammogram and their relationship to cancer disparities. Understanding differences in psychosocial functioning and the role of coping strategies in response to the stressful situation of receiving an abnormal screening result will help to inform the design and content of future interventions and programs dedicated to improving the well-being of traditionally underserved and vulnerable populations (e.g., Latinas). Nurses and other healthcare professionals may alleviate patient distress through counseling with regard to coping strategies in a culturally tailored manner.
Differences in psychological distress and social withdrawal following an abnormal mammogram are perhaps not surprising in the context of documented differences in distress among Latina and NLC women with breast cancer and survivors (Ashing-Giwa et al., 2006; Janz et al., 2009) and the importance of social functioning for quality of life among Latinas (Buki et al., 2008; Sammarco & Konecny, 2008). The authors found no research that explored ethnic differences during early detection and diagnostic evaluation; the current study contributes to a growing body of work that suggests psychosocial disparities exist across the cancer continuum. The differences in psychological distress and social withdrawal noted in the authors’ work may warrant attention because previous work has suggested emotional distress is linked to diagnostic delays among Latinas (Allen et al., 2008; Ashing-Giwa et al., 2010).
A substantial amount of literature concerns ethnic differences in coping among patients with cancer and survivors, and the current findings support that work. This study con tributes to existing research concerning relationships between coping strategies and psychological distress. Recent comprehensive reviews have indicated a wide range of coping strategies used following an abnormal mammogram result, and they have also indicated the need for more research to characterize associations between coping and psychosocial outcomes (Andrés-Hyman et al., 2006; Bond et al., 2013; Molina et al., 2013; Montgomery, 2010). In contrast to previous literature (Alderete et al., 2006), religious coping was not affiliated with psychological distress in the current study. Differences in findings may be because of differences in study samples as well as measurement of religious coping (e.g., Brief COPE versus measurement of weekly attendance at religious services). Religious coping may vary across ethnicities with regard to associations to psychological distress and other forms of coping. A study by Umezawa et al. (2012) indicated belief in the divine was negatively related to avoidance coping among low-acculturated Latinas but not other ethnic groups. Additional studies are needed to characterize the association between different forms of coping and psychological distress across multiethnic samples. Findings about denial coping and distress also suggest a need to distinguish between types of avoidant coping and compare the effects on mental health outcomes. For example, cognitive distraction has been noted to be protective for mental health during an abnormal mammogram experience, and behavioral distraction and substance use have been positively related to anxiety symptoms (Andrés-Hyman et al., 2006; Bond et al., 2013; Montgomery, 2010).
The authors’ mediation models also support future characterization of different coping strategies. Denial coping was significantly associated with psychological distress, and religious coping was significantly associated with social withdrawal. These findings provide preliminary evidence concerning the importance of denial coping for future longitudinal studies and counseling interventions for Latinas in terms of psychological distress. The findings suggest that Latinas may be more socially withdrawn because of a greater reliance on religious coping. Latinas may be employing spiritual resources more than social resources because of fear of burdening the family and causing the family to worry. This would coincide with qualitative literature suggesting that women do not rely on social resources to protect family and friends from undue stress (Austin et al., 2002; Logan et al., 2006). Reliance on spiritual coping should be addressed in future studies to better understand how strategies, such as prayer and reliance on spiritual beliefs, may influence the abnormal mammography experience for Latinas.
Distress, social withdrawal, and coping were not associated with follow-up care adherence among Latinas and NLC women, which is in contrast to previous research with larger sample sizes that has documented associations between cancer worry and delay among Latinas (Ashing-Giwa et al., 2010). Additional studies will help to elucidate these conflicting findings. This study also provides preliminary findings that call for future research concerning the influence of psychological sequelae following an abnormal mammogram on subsequent screening practices to determine the long-term consequences of elevated distress among Latinas. Elevated distress and social withdrawal fol lowing an abnormal screening result may be particularly important with regard to subsequent distress and quality of life among women diagnosed with breast cancer and for cancer worry among women not diagnosed with breast cancer. Researchers must conduct studies concerning the relationship between ethnic differences in distress and social withdrawal following an abnormal mammogram result to disparities in psychological health among patients with cancer and survivors (Ashing-Giwa et al., 2006; Janz et al., 2009). That research will help to inform the need for future psychosocial interventions for Latinas who receive an abnormal result.
Limitations
This study had several limitations. This was a pilot study with relatively small samples of Latinas and NLC women. Women were recruited through convenience sampling, and the findings are not likely to be representative of broader Latina and NLC samples. For example, women in the current sample are relatively young compared to current recommended guidelines by the U.S. Preventive Services Task Force (2009). However, the women were within the range of guidelines per the American Cancer Society (2014b) and the National Comprehensive Cancer Network (Bevers et al., 2009). Although the current sample included women living in rural and urban areas, the sample was underpowered to test differences in rural and urban women's experiences. The majority of women from the sample were recruited from mobile mammography services, which may have influenced the generalizability of the findings.
Another important confounder is the effect of study participation on linguistic barriers, which have been documented to influence diagnostic resolution following receipt of an abnormal mammogram result. A recent study found that the majority of clinics distributing screening mammogram results only provide letters in English (Marcus, Koru-Sengul, Miao, Yepes, & Sanders, 2014); the majority of the patients in the current sample came from sites with this type of protocol. Linguistic barriers and comprehension of abnormal screening results have been noted to influence diagnostic delays and patient satisfaction among Latinas and women with English-limited proficiency (Allen et al., 2008; Marcus et al., 2014; Mojica, Bastani, Ponce, & Boscardin, 2007; Poon et al., 2004). Women who were recruited to participate in this project were able to interact with bilingual research staff and, therefore, were potentially more likely to understand that they had received an abnormal mammogram result and needed to schedule follow-up care.
Several of the survey instruments demonstrated adequate, but low, internal consistency (e.g., social withdrawal, active coping). The authors used instruments that had multiple items with psychometrically robust properties. Future research could use instruments used in research and clinical settings (e.g., National Comprehensive Cancer Network Distress Thermometer) to better inform practice. The majority of baseline surveys were conducted prior to administration of biopsies and cancer diagnoses, which are likely to influence coping strategies and distress (Steffens, Wright, Hester, & Andrykowski, 2011). The authors did not collect data on the history of previous receipt of abnormal results, which may have influenced distress and coping strategies.
The authors used a simplistic conceptual model that focused on ethnicity, coping, distress, and withdrawal in the context of the abnormal mammogram experience. Variation in coping after an abnormal mammo-gram experience may be because of several factors that were not included in this study, such as family history of breast cancer, previous experience with breast biopsies, and unrelated stressors (e.g., financial stress, work history). The current study focused on mediating roles of coping strategies, but recent qualitative research on coping following an abnormal mammogram has suggested coping strategies may depend on other sociodemographic and personality characteristics (Austin et al., 2002; Umezawa et al., 2012). The sample size did not have sufficient statistical power to assess the moderating role of coping strategies or the influence of these factors on coping. Future population-based research with larger sample sizes should include the variables in more complicated models. Future research is warranted to elucidate this study's findings as well as the broader literature on coping following an abnormal mammogram. Future studies with larger samples and those that do not affect standard delivery of care are important to confirm differences in psychological and social withdrawal following receipt of an abnormal mammogram result as well as to clarify relationships between disparities in negative psychosocial outcomes and receipt of recommended follow-up care guidelines.
Implications for Practice and Research
Additional research is warranted to address the role of psychological sequelae (e.g., distress, social withdrawal) on follow-up care adherence as well as other long-term behavioral consequences (e.g., screening practices). Research is needed concerning the effect of distress and social withdrawal following an abnormal mammogram on subsequent breast cancer worry and quality of life for women diagnosed with breast cancer and those who are not. Future interventions should target denial coping to mitigate distress among Latinas. To improve access to social support resources, interventions may also incorporate religious coping strategies. The benefits of disclosure to family about abnormal results and reliance on social support may be described through noting the emphasis of family in religious contexts for Latinas.
Coping interventions may be particularly well received by Latinas when they are administered by nurses because of cultural values that emphasize strong interpersonal relationships as well as respecting and attending to authority figures (Marin & Marin, 1991). Practitioners working with Latinas who receive abnormal results may be ideally suited to mitigate distress within this population through addressing coping skills. Oncology nurses may wish to address coping strategies to mitigate distress and social withdrawal among Latina patients with cancer because coping strategies used during receipt of an abnormal mammo-gram result may also be used upon receipt of a cancer diagnosis and throughout treatment (Ashing-Giwa et al., 2004; Culver et al., 2002, 2004).
Conclusions
The current study provides important contributions to the existing body of research addressing ethnic disparities along the cancer continuum. This preliminary work suggests that Latinas experience poorer psychosocial outcomes, including elevated psychological distress and social withdrawal. The additional psychosocial distress experienced by Latinas was found to be linked to types of coping. Additional studies should be conducted to understand the mechanisms used to diminish psychological distress and to develop interventions and improve clinical practice to assist women who receive an abnormal mammogram.
Knowledge Translation.
Latinas are more likely to exhibit greater distress and social withdrawal than non-Latina Caucasian (NLC) women after an abnormal mammogram.
Latinas appear to exhibit greater distress than NLC women because of greater denial coping.
Latinas appear to exhibit greater social withdrawal than NLC women because of greater religious coping.
Acknowledgments
This work was supported by grants (Nos. P50CA148143 and R25CA92408) from the National Cancer Institute.
Contributor Information
Yamile Molina, Division of Public Health Sciences.
Shirley A.A. Beresford, Department of Epidemiology and senior associate dean, both at the University of Washington.
Noah Espinoza, Northwest Kidney Centers.
Beti Thompson, Fred Hutchinson Cancer Research Center, all in Seattle, WA..
References
- Alderete E, Juarbe TC, Kaplan CP, Pasick R, Pérez-Stable EJ. Depressive symptoms among women with an abnormal mammogram. Psycho-Oncology. 2006;15:66–78. doi: 10.1002/pon.923. doi:10.1002/pon.923. [DOI] [PubMed] [Google Scholar]
- Allen JD, Shelton RC, Harden E, Goldman RE. Follow-up of abnormal screening mammograms among low-income ethnically diverse women: Findings from a qualitative study. Patient Education and Counseling. 2008;72:283–292. doi: 10.1016/j.pec.2008.03.024. [DOI] [PubMed] [Google Scholar]
- American Cancer Society Cancer facts and figures for Hispanics/ Latinos, 2012–2014. 2012 Retrieved from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/docu ment/acspc-034778.pdf.
- American Cancer Society Cancer facts and figures, 2014. 2014a Retrieved from http://www.cancer.org/acs/groups/content/@research/documents/webcontent/acspc-042151.pdf.
- American Cancer Society Detailed guide: Breast cancer. 2014b Retrieved from http://www.cancer.org/Cancer/BreastCancer/DetailedGuide.
- Andrés-Hyman RC, Ortiz J, Añez LM, Paris M, Davidson L. Culture and clinical practice: Recommendations for working with Puerto Ricans and other Latinas(os) in the United States. Professional Psychology: Research and Practice. 2006;37:694–701. [Google Scholar]
- Ashing-Giwa KT, Gonzalez P, Lim JW, Chung C, Paz B, Somlo G, Wakabayashi MT. Diagnostic and therapeutic delays among a multiethnic sample of breast and cerivcal cancer survivors. Cancer. 2010;116:3195–3204. doi: 10.1002/cncr.25060. [DOI] [PubMed] [Google Scholar]
- Ashing-Giwa KT, Padilla G, Tejero J, Kraemer J, Wright K, Coscarelli A, Hills D. Understanding the breast cancer experience of women: A qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psycho-Oncology. 2004;13:408–428. doi: 10.1002/pon.750. doi:10.1002/pon.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashing-Giwa KT, Padilla GV, Bohórquez DE, Tejero JS, Garcia M. Understanding the breast cancer experience of Latina women. Journal of Psychosocial Oncology. 2006;24:19–52. doi: 10.1300/J077v24n03_02. doi:10.1300/J077v24n03_02. [DOI] [PubMed] [Google Scholar]
- Austin LT, Ahmad F, McNally MJ, Stewart DE. Breast and cervical screening in Hispanic women: A literature review using the Health Belief Model. Women's Health Issues. 2002;12:122–128. doi: 10.1016/s1049-3867(02)00132-9. [DOI] [PubMed] [Google Scholar]
- Bevers TB, Anderson BO, Bonaccio E, Buys S, Daly MB, Dempsey PJ, Yankeelov T. NCCN clinical practice guidelines in oncology: Breast cancer screening and diagnosis. Journal of the National Comprehensive Cancer Network. 2009;7:1060–1096. doi: 10.6004/jnccn.2009.0070. [DOI] [PubMed] [Google Scholar]
- Bickell NA, Wang JJ, Oluwole S, Schrag D, Godfrey H, Hiotis K, Guth AA. Missed opportunities: Racial disparities in adjuvant breast cancer treatment. Journal of Clinical Oncology. 2006;24:1357–1362. doi: 10.1200/JCO.2005.04.5799. doi:10.1200/jco.2005.04.5799. [DOI] [PubMed] [Google Scholar]
- Boinon D, Charles C, Dauchy S, Sultan S. Effects of emotional expression on adjustment to cancer: A systematic review of research. Psycho-Oncologie. 2011;5:173–190. [Google Scholar]
- Bond M, Pavey T, Welch K, Cooper C, Garisde D, Dean S, Hyde C. Systematic review of the psychological consequences of false-positive screening mammograms. Health Technology Assessment. 2013;17(13):1–170. doi: 10.3310/hta17130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Salz T, Lillie S. Systematic review: The long-term effects of false-positive mammograms. Annals of Internal Medicine. 2007;146:502–510. doi: 10.7326/0003-4819-146-7-200704030-00006. doi:10.7326/0003-4819-146-7-200704030-00006. [DOI] [PubMed] [Google Scholar]
- Buki LP, Garcés DM, Hinestrosa MC, Kogan L, Carrillo IY, French B. Latina breast cancer survivors’ lived experiences: Diagnosis, treatment, and beyond. Cultural Diversity and Ethnic Minority Psychology. 2008;14:163–167. doi: 10.1037/1099-9809.14.2.163. doi:10.1037/1099-9809.14.2.163. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol's too long: Consider the brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. doi:10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Chen CC, David A, Thompson K, Smith C, Lea S, Fahy T. Coping strategies and psychiatric morbidity in women attending breast assessment clinics. Journal of Psychosomatic Research. 1996;40:265–270. doi: 10.1016/0022-3999(95)00529-3. doi:10.1016/0022-3999(95)00529-3. [DOI] [PubMed] [Google Scholar]
- Cockburn J, De Luise T, Hurley S, Clover K. Develop ment and validation of the PCQ: A questionnaire to measure the psychological consequences of screening mammography. Social Science and Medicine. 1992;34:1129–1134. doi: 10.1016/0277-9536(92)90286-y. [DOI] [PubMed] [Google Scholar]
- Culver JL, Arena PL, Antoni MH, Carver CS. Coping and distress among women under treatment for early stage breast cancer: Comparing African Americans, Hispanics and non-Hispanic Whites. Psycho-Oncology. 2002;11:495–504. doi: 10.1002/pon.615. doi:10.1002/pon.615. [DOI] [PubMed] [Google Scholar]
- Culver JL, Arena PL, Wimberly SR, Antoni MH, Carver CS. Coping among African-American, Hispanic, and non-Hispanic White women recently treated for early stage breast cancer. Psychology and Health. 2004;19:157–166. [Google Scholar]
- Fedewa SA, Ward EM, Stewart AK, Edge SB. Delays in adjuvant chemotherapy treatment among patients with breast cancer are more likely in African American and Hispanic populations: A national cohort study 2004–2006. Journal of Clinical Oncology. 2010;28:4135–4141. doi: 10.1200/JCO.2009.27.2427. doi:10.1200/jco.2009.27.2427. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. Coping as a mediator of emotion. Journal of Personality and Social Psychology. 1988;54:466–475. [PubMed] [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. doi:10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra CE, Krumholz M, Shea JA. Literacy and knowledge, attitudes and behavior among mammography in Latinas. Journal of Health Care for the Poor and Underserved. 2005;16:152–166. doi: 10.1353/hpu.2005.0012. [DOI] [PubMed] [Google Scholar]
- Hafslund B, Espeghaug B, Nortvedt MW. Effects of false-positive results in a breast screening program on anxiety, depression and health-related quality of life. Cancer Nursing. 2012;35:E26–E35. doi: 10.1097/NCC.0b013e3182341ddb. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. doi:10.1080/03637750903310360. [Google Scholar]
- Hayes AF, Preacher KJ. Quantifying and testing indirect effects in simple mediation models when the constituent paths are nonlinear. Multivariate Behavioral Research. 2010;45:627–660. doi: 10.1080/00273171.2010.498290. [DOI] [PubMed] [Google Scholar]
- Heckman BD, Fisher EB, Monsees B, Merbaum M, Ristvedt S, Bishop C. Coping and anxiety in women recalled for additional diagnostic procedures following an abnormal screening mammogram. Health Psychology. 2004;23:42–48. doi: 10.1037/0278-6133.23.1.42. doi:10.1037/0278-6133.23.1.42. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Janz NK, Mujahid MS, Hawley ST, Griggs JJ, Alderman A, Hamilton AS, Katz SJ. Racial/ethnic differences in quality of life after diagnosis of breast cancer. Journal of Cancer Survivorship. 2009;3:212–222. doi: 10.1007/s11764-009-0097-y. doi:10.1007/s11764-009-0097-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal A, Clegg LX, Ward E, Ries LA, Wu X, Jamison PM, Edwards BK. Annual report to the nation on the status of cancer, 1975–2001, with a special feature regarding survival. Cancer. 2004;101:3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- Keyzer-Dekker CM, van Esch L, de Vries J, Ernst MF, Nieuwenhuijzen GA, Roukema JA, van der Steeg AF. An abnormal screening mammogram causes more anxiety than a palpable lump in benign breast disease. Breast Cancer Research and Treatment. 2012;134:253–258. doi: 10.1007/s10549-012-2025-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter MW, McClure SM. The role of culture in health communication. Annual Review of Public Health. 2004;25:439–455. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- Kudadjie-Gyamfi E, Magai C. The influence of coping styles on mammography screening in a multiethnic sample. Cultural Diversity and Ethnic Minority Psychology. 2008;14:183–192. doi: 10.1037/1099-9809.14.3.183. [DOI] [PubMed] [Google Scholar]
- Lantz PM, Mujahid M, Schwartz K, Janz NK, Fagerlin A, Salem B, Katz SJ. The influence of race, ethnicity, and individual socioeconomic factors on breast cancer stage at diagnosis. American Journal of Public Health. 2006;96:2173–2178. doi: 10.2105/AJPH.2005.072132. doi:10.2105/ajph.2005.072132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan J, Hackbusch-Pinto R, De Grasse CE. Women undergoing breast diagnostics: The lived experience of spirituality. Oncology Nursing Forum. 2006;33:121–126. doi: 10.1188/06.ONF.121-126. [DOI] [PubMed] [Google Scholar]
- Lopez-Class M, Gomez-Duarte J, Graves K, Ashing-Giwa K. A contextual approach to understanding breast cancer survivorship among Latinas. Psycho-Oncology. 2012;21:115–124. doi: 10.1002/pon.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe JB, Balanda KP, Del Mar C, Hawes E. Psychologic distress in women with abnormal findings in mass mammography screening. Cancer. 1999;85:1114–1118. doi: 10.1002/(sici)1097-0142(19990301)85:5<1114::aid-cncr15>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Marcus EN, Koru-Sengul T, Miao F, Yepes M, Sanders L. How do breast imaging centers communicate results to women with limited English proficiency and other barriers to care?. Journal of Immigrant and Minority Health. 2014;16:401–408. doi: 10.1007/s10903-012-9771-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin G, Marin BV. Research with Hispanic populations. Vol. 23. Sage; Newbury Park, CA: 1991. [Google Scholar]
- Mojica CM, Bastani R, Ponce NA, Boscardin WJ. Latinas with abnormal breast findings: Patient predictors of timely diagnostic resolution. Journal of Women's Health. 2007;16:1468–1477. doi: 10.1089/jwh.2006.0324. [DOI] [PubMed] [Google Scholar]
- Molina Y, Thompson B, Espinoza N, Ceballos R. Breast cancer interventions serving US-based Latinas: Current approaches and directions. Women's Health. 2013;9:335–348. doi: 10.2217/whe.13.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery M. Uncertainty during breast diagnostic evaluation: State of the science. Oncology Nursing Forum. 2010;37:77–83. doi: 10.1188/10.ONF.77-83. [DOI] [PubMed] [Google Scholar]
- Moy B, Park ER, Feibelmann S, Chiang S, Weissman JS. Barriers to repeat mammography: Cultural perspectives of African-American, Asian, and Hispanic women. Psycho-Oncology. 2006;15:623–634. doi: 10.1002/pon.994. [DOI] [PubMed] [Google Scholar]
- Ooi SL, Martinez ME, Li CI. Disparities in breast cancer characteristics and outcomes by race/ethnicity. Breast Cancer Research and Treatment. 2011;127:729–738. doi: 10.1007/s10549-010-1191-6. doi:10.1007/s10549-010-1191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakenham KI, Clutton SJ, Buckley BM. Predictors of emotional well-being following a ‘false positive’ breast cancer screening result. Psychology and Health. 1999;14:263–275. [Google Scholar]
- Perczek R, Carver CS, Price AA, Pozo-Kaderman C. Coping, mood, and aspects of personality in Spanish translation and evidence of convergence with English versions. Journal of Personality Assessment. 2000;74:63–87. doi: 10.1207/S15327752JPA740105. doi:10.1207/s15327752jpa740105. [DOI] [PubMed] [Google Scholar]
- Poon EG, Haas JS, Puopolo A, Gandhi TK, Burdick E, Bates DW, Brennan TA. Communication factors in the follow-up of abnormal mammograms. Journal of General Internal Medicine. 2004;19:316–323. doi: 10.1111/j.1525-1497.2004.30357.x. doi:10.1111/j.1525-1497.2004.30261.x-i1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Purc-Stephenson RJ, Gorey KM. Lower adherence to screening mammography guidelines among ethnic minority women in America: A meta-analytic review. Preventive Medicine. 2008;46:479–488. doi: 10.1016/j.ypmed.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Requena GC, Gil Moncayo FL. Propiedades psicométricas de la escala revisada del impacto del evento estresante (IES-R) en una muestra española de pacientes con cáncer. Análisis y Modificación de Conducta. 2007;33(149):311–331. [Google Scholar]
- Salz T, Richman AR, Brewer NT. Meta-analyses of the effects of false-positive mammograms on generic and specific psychosocial outcomes. Psycho-Oncology. 2010;19:1026–1034. doi: 10.1002/pon.1676. [DOI] [PubMed] [Google Scholar]
- Sammarco A, Konecny LM. Quality of life, social support, and uncertainty among Latina breast cancer survivors. Oncology Nursing Forum. 2008;35:844–849. doi: 10.1188/08.ONF.844-849. doi:10.1188/08.ONF.844-849. [DOI] [PubMed] [Google Scholar]
- Santiago-Rivera AL, Arrendondo P, Gallardo-Cooper M. Counseling Latinos and la familia: A practical guide. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Siegel R, Naishadham D, Jemal A. Cancer statistics for Hispanics/Latinos, 2012. CA: A Cancer Journal for Clinicians. 2012;62:283–293. doi: 10.3322/caac.21153. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Direct and indirect effects in linear structural equation models. Sociological Methods and Research. 1987;16:155–176. [Google Scholar]
- Steffens RF, Wright HR, Hester MY, Andrykowski MA. Clinical, demographic, and situational factors linked to distress associated with benign breast biopsy. Journal of Psychosocial Oncology. 2011;29:35–50. doi: 10.1080/07347332.2011.534024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundin EC, Horowitz MJ. Impact of Event Scale: Psycho-metric properties. British Journal of Psychiatry. 2002;180:205–209. doi: 10.1192/bjp.180.3.205. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- Umezawa Y, Lu Q, You J, Kagawa-Singer M, Leake B, Maly RC. Belief in divine control, coping, and race/ethnicity among older women with breast cancer. Annals of Behavioral Medicine. 2012;44:21–32. doi: 10.1007/s12160-012-9358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D. The Impact of Event Scale: Revised. In: Wilson J, So-Kum Tang C, editors. Cross-cultural assessment of psychological trauma and PTSD. Springer; New York, NY: 2007. pp. 219–238. [Google Scholar]