Most clinicians are aware of the excellent summary on the topic of compression written by noted researchers such as Braida et al (1979), Walker and Dillon (1982), and Dillon (1988). A reasonable question is: why this paper? The fact is that over the last 10 years there has been a dramatic increase in the number of scientific papers and clinical reports on the use of compression in hearing aids. The present attitude towards compression hearing aids is certainly more positive than that expressed in previous reports. This change in interest from linear amplification with peak clipping to an alternative output limiting approach is also reflected in the increasing number of hearing aid manufacturers incorporating compression circuitry in their hearing aid design. While hearing aids using compression as output limiting offers some advantages over hearing aids using peak clipping, the use of compression is not without controversies. Some of the theoretical arguments made in favor of a particular compression approach may have practical limitations. In addition, many benefits reported with one form of compression may not be exclusive of that compression approach. This paper will review the electroacoustic specifications for compression hearing aids, and examine some theoretical and practical advantages of different compression approaches. In addition, considerations will be given to how some of the theoretical issues may require clinicians to re-evaluate their current practice of fitting such devices. Perhaps a better understanding of these issues may facilitate one's choice for a particular output limiting approach for a hearing aid wearer.
WHY LIMIT OUTPUT?
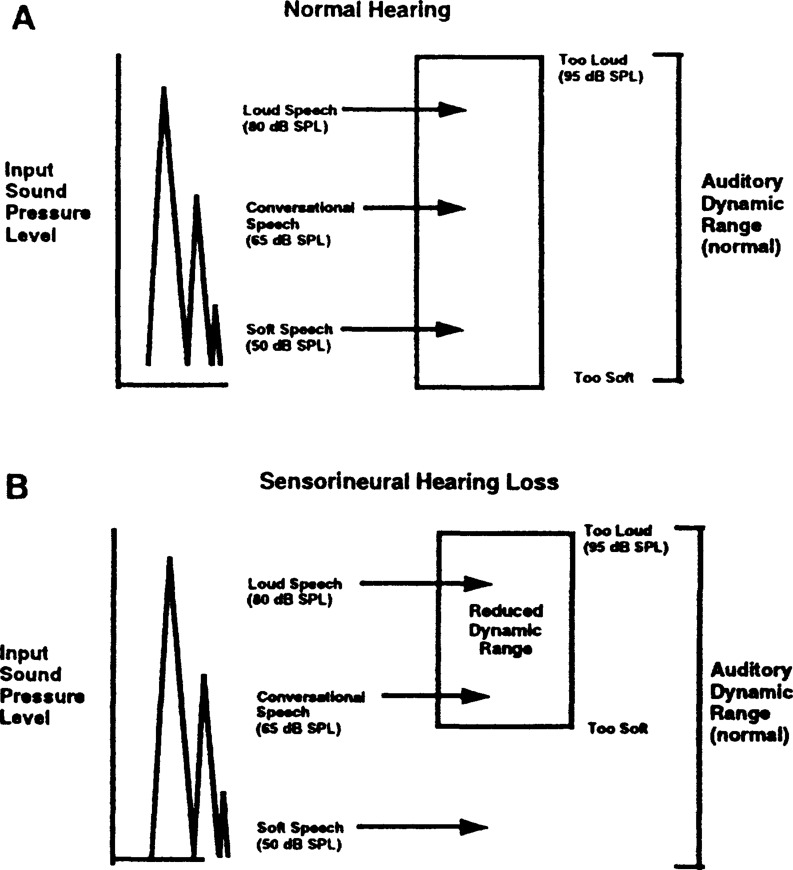
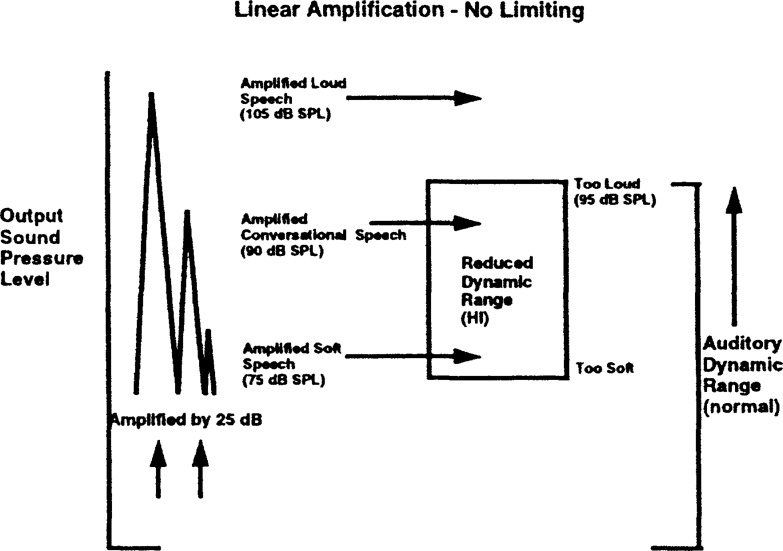
Hearing loss reduces the sensitivity of the ear to signals that are presented at low intensity levels while retaining its sensitivity to signals presented at high intensity levels. This has the effect of raising the “floor” of the auditory dynamic range while keeping the “ceiling” (or tolerance limit) at the same level as people with normal hearing. This effectively reduces the dynamic range (DR, or the difference in dB between the intensity level for “just audible” sounds and the intensity level for sounds that are “uncomfortably loud”) of the auditory system. The consequence is that low intensity sounds in the unaided condition will be inaudible, while high intensity sounds will remain loud. Figure 1 (A & B) illustrates how different levels of speech can be represented within the auditory dynamic range in a normal hearing (Figure 1A) and hearing impaired ear (Figure 1B). The rectangular box on the right represents the auditory dynamic range. The three conical-shaped symbols on the left represent the peak sound pressure levels (SPL) for three levels of speech. The highest peak represents loud speech (overall level = 80 dB SPL); the medium peak represents conversational speech (overall level = 65 dB SPL), and the lowest peak represents soft speech (overall level = 50 dB SPL). Another ramification of the reduced dynamic range is that the same gain from a hearing aid with linear amplification that makes low intensity sounds audible will make high intensity sounds uncomfortably loud. This is because the same degree of amplification (e.g., 25 dB) will place the loud speech beyond the individual's tolerance limit, which in this example, is set at 95 dB SPL (Figure 2). The immediate consequence is discomfort and a lack of satisfaction with amplification. Overamplification may result from prolonged use of the hearing aid at a high intensity output level (Macrae, 1994).
Figure 1.
Representation of soft, conversational and loud speech into the auditory dynamic range (A) normal hearing, (B) sensorineural hearing loss.
Figure 2.
Example to show how linear amplification without limiting (25 dB gain), when applied to soft, conversational and loud speech, may alter its representation in the residual auditory dynamic range of a hearing-impaired ear.
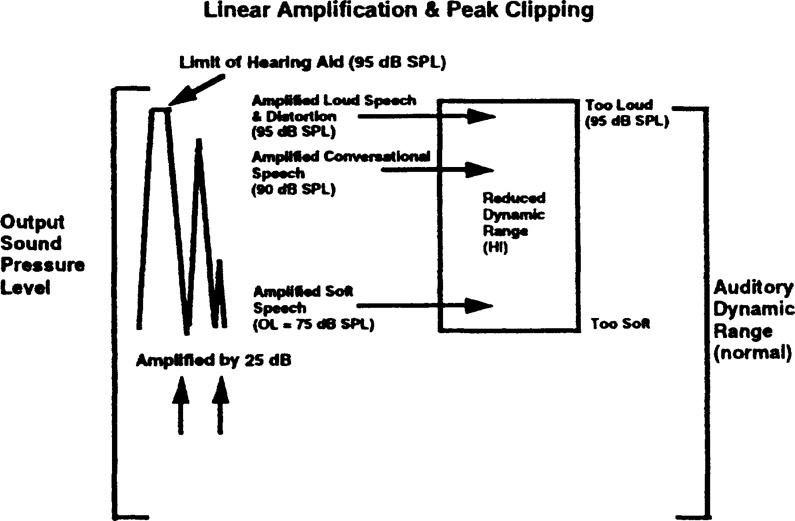
A cost-effective way to minimize the undesirable effect of amplifying high intensity sounds beyond the patient's uncomfortable loudness level is peak clipping. Using this method of output limiting, sound pressure level (SPL) at the output that exceeds a pre-set limit is “clipped.” This is illustrated in Figure 3. The peak of the highest conical symbol is clipped to reflect this change when the amplified sound pressure level of the output (i.e., gain plus input) exceeds the SSPL90 setting of the hearing aid. Typically, this limit is set to just below the loudness discomfort level (LDL) of the hearing impaired patient (95 dB SPL in this example). The result of this action is that low and moderately intense sounds will be amplified to within the patient's residual dynamic range, but all intense sounds will result in the same output sound pressure level below the patient's discomfort level.
Figure 3.
Example to show how linear amplification with peak clipping (25 dB gain), when applied to soft, conversational, and loud speech, may affect its representation in the residual auditory dynamic range of a hearing-impaired ear.
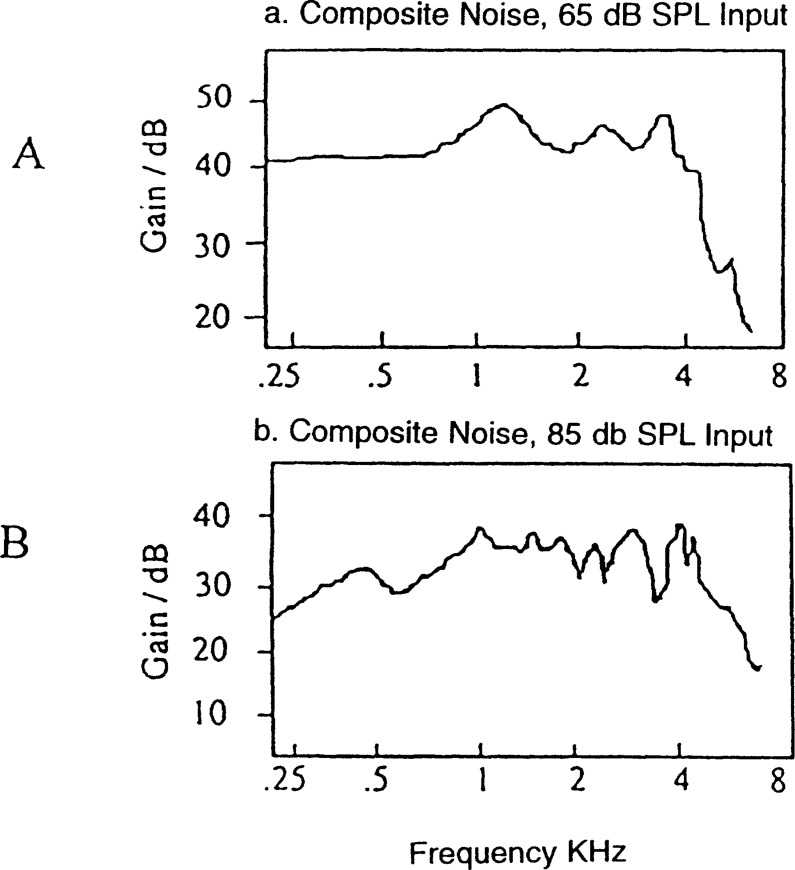
Peak clipping would be an acceptable form of output limiting if it were not for the associated saturation-induced distortion products that result from clipping. In addition to the alteration in the temporal waveform, peak clipping generates intermodulation and harmonic distortion products that are mixed with the output signal. Figure 4A shows the frequency response of a hearing aid when it is operating linearly (at 65 dB SPL input). Figure 4B shows the frequency response when the output waveform is “peak clipped” (at 85 dB SPL input). A broadband noise is used as the test stimulus. The two input levels used in this example can be approximated to the sound pressure levels recorded at the ear level when the wearer is listening to typical conversational speech and to his/her own voice when s/he vocalizes (Cornelisse et al, 1991). Note that peak clipping results in a broader frequency response (Figure 4B) and the appearance of irregularities in the frequency response. In addition, gain is also decreased. The increase in the “non-input” or distortion products would suggest a poorer signal-to-noise ratio at the output of the hearing aid when it is peak clipped than when it is not. Considering that hearing impaired individuals typically have poorer frequency selectivity (Moore, 1986) and require higher signal-to-noise ratio for speech recognition (Dirks et al, 1982), one would predict that using peak clipping to limit output level may result in poorer speech intelligibility and decrease sound quality at high input levels because of the associated saturation-induced distortion products.
Figure 4.
Frequency response curves of a hearing aid with linear amplification when tested with composite noise at (A) 65 dB SPL, and (B) 85 dB SPL (hearing aid in saturation).
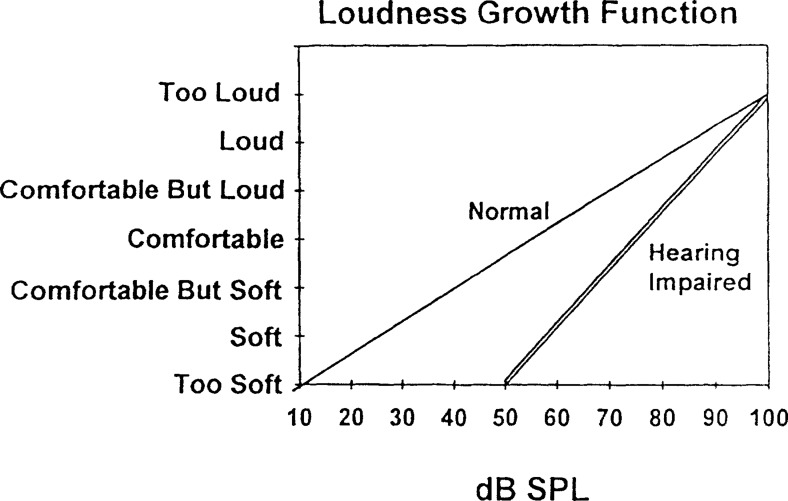
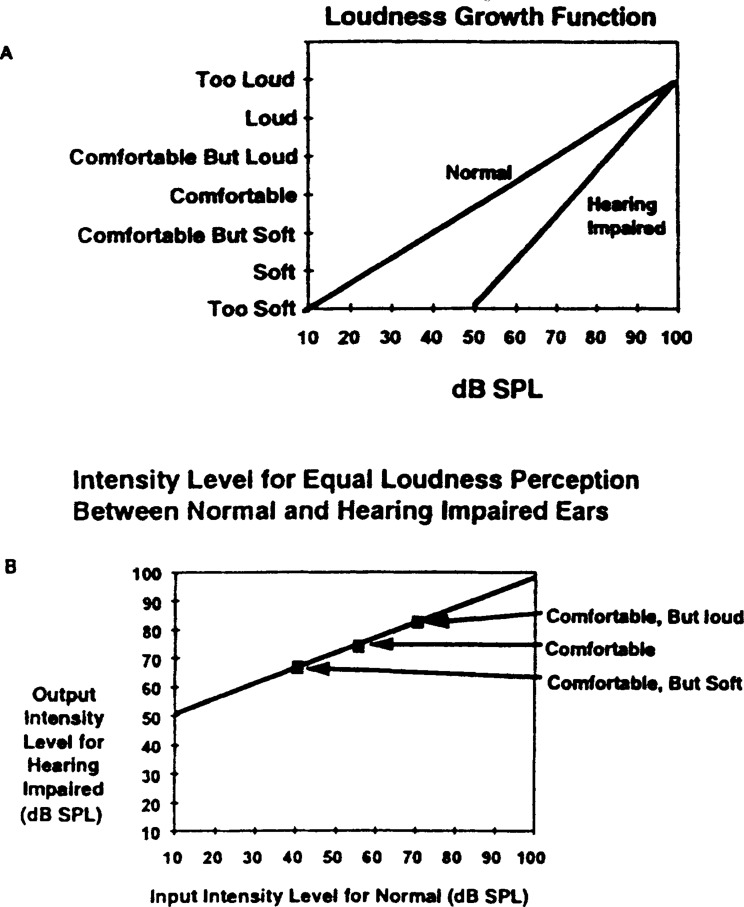
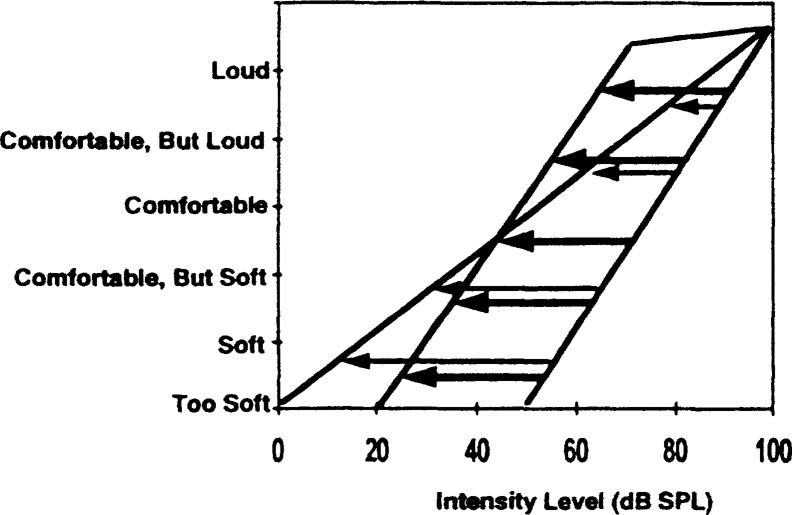
Peak clipping, while limiting output sound pressure level, does not compensate for the alteration in loudness perception associated with hearing loss. Figure 5 shows the loudness growth function of a normal hearing listener and one with a moderate sensorineural hearing loss (50 dB SPL). The reduced dynamic range in the impaired ear (i.e., 100 — 50 or 50 dB) relative to the normal ear (i.e., 100 — 10 or 90 dB) is again evident. In addition, the slope of the loudness intensity function of the hearing impaired listener is steeper than that of the normal hearing listener. This suggests that above threshold, it takes less increase in sound pressure level for the hearing impaired listener to achieve the same change in loudness perception as the normal hearing listener. It also suggests that, even if a linear hearing aid does not produce sounds that exceed the listener's discomfort level, it may generate sounds that are above the comfortable listening level of the listener unless the volume control setting is lowered.
Figure 5.
Hypothetical loudness growth functions for a normal hearing listener and hearing-impaired listener.
In order to limit the output sound pressure level of the hearing aid so that it does not result in loudness discomfort while minimizing saturation-induced distortion, one has to do more than clip the output signal. The use of compression amplification, in its various forms, may satisfy this requirement.
WHAT IS COMPRESSION?
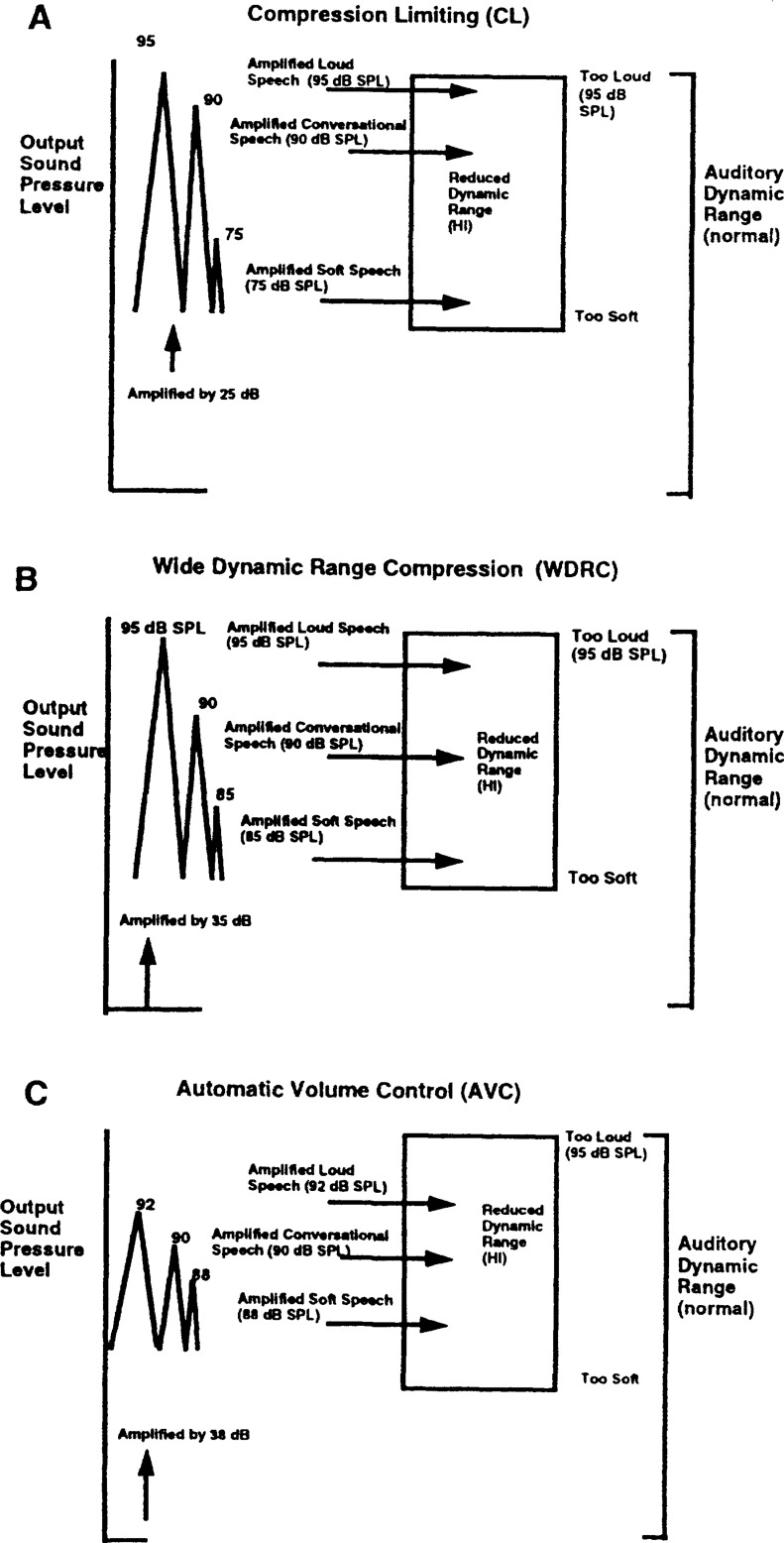
Very simply, compression is the process whereby the intensity relationship among various segments of the acoustic stimuli is altered over time. The result is that the range of SPL variation in the long-term output is reduced relative to the range at the input. In the short term, however, such intensity relationship is maintained. In theory, compression is necessary in order to “squeeze” the 30 dB range between soft and loud speech (Pearsons et al, 1977) into the residual DR of the hearing impaired listener who has a narrower DR. To accomplish that goal, amplification is applied to low intensity sounds so they are audible. Gain reduction is applied to high intensity sounds so they are not uncomfortably loud and are free from distortion. A compression hearing aid must include both of these actions (i.e., amplification and gain reduction). Figure 6 shows some of the common approaches to alter the intensity relationship among sounds in order to meet such criteria. The distances among the peaks of the three conical symbols represent the result of such intensity alteration. The numbers by the peaks represent the output SPL. For example, Fig. 6A shows that one can apply the same amount of amplification (i.e., linear) until the SPL approaches the upper limit of the auditory range. When that level is reached, gain on the hearing aid is sharply decreased (i.e., highly compressed) to prevent output SPL from reaching saturation and thus minimizing distortion. In this case the absolute intensity difference (i.e., dB between peaks) between the soft and conversational speech is preserved at 15 dB. The difference between the loud and conversational speech is reduced to 5 dB. This form of compression has been called compression limiting. Figure 6B shows that one can amplify low intensity sounds so that it is audible. Above that level, amplification is proportionately decreased with increasing input levels. Note in this case that the intensity difference between loud and conversational speech and between soft and conversational speech is reduced to 5 dB. This form of compression has been called wide (or full) dynamic range compression. Figure 6C shows that one can apply a great amount of gain to low intensity sounds so that they are amplified to a most comfortable listening (MCL) level. Above that level, one can reduce gain sufficiently so that the output SPL remains relatively close to the MCL regardless of input level. Note in this case that the absolute intensity difference between loud and conversational speech (2 dB) and between soft and conversational speech (2 dB) is further reduced. The sound pressure level at the output is clustered around 90 dB SPL, the MCL of the listener. This form of compression has been called automatic volume control.
Figure 6.
Three approaches to “compress” the entire speech range into the residual auditory dynamic range of the hearing-impaired ear: (A) compression limiting (CL), (B) wide dynamic range compression (WDRC), and (C) automatic volume control (AVC).
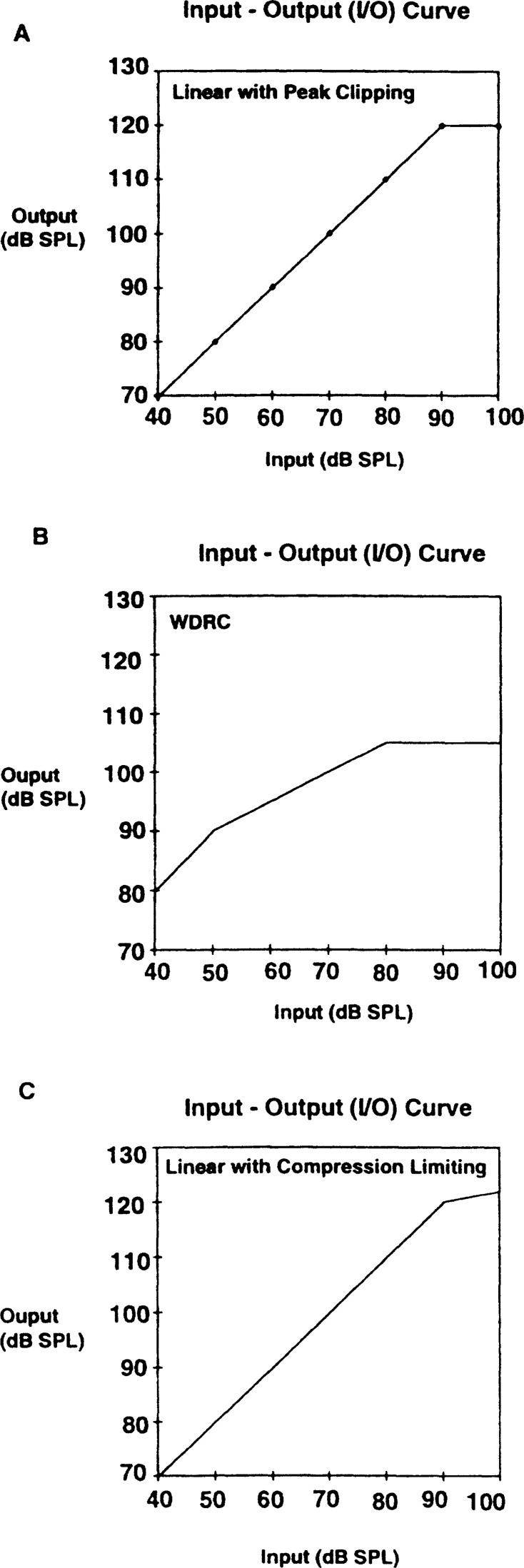
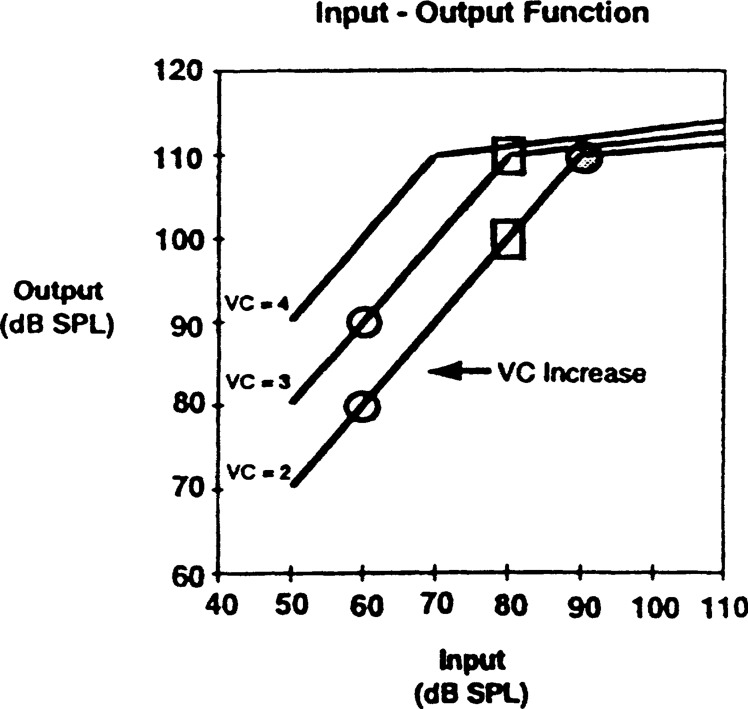
One way to determine if compression is utilized in a hearing aid is to examine the input-output (I-O) curve. This curve can be determined with a steady-state sinusoid or with a composite noise signal (ANSI, 1992). However, most reports used sinusoids as the stimulus to illustrate the static and dynamic properties of a compression hearing aid because of its simplicity. Walker and Dillon (1982) defined a hearing aid as utilizing compression when the slope of any portion of the I-O curve is greater than zero (i.e., prior to saturation) but is less than unity (i.e., one dB increase in input leads to less than one dB increase in output). Figure 7 shows the I-O curves of three limiting techniques. Figure 7A shows that when the input increases from 40 dB SPL to 90 dB SPL, the output increases from 70 dB SPL to 120 dB SPL. In this case, the slope of the I-O curve is 1 (slope = change in output/change in input = 120 – 70/90 – 40 = 1). The hearing aid is saturated at input levels exceeding 90 dB SPL. No increase in output beyond 120 dB SPL is seen with increases in input. This is classified as a linear hearing aid with peak clipping. No compression is used in this case. On the other hand, Figure 7B shows that the slope of the curve from 50 dB SPL to 80 dB SPL input is 0.5 because the change in output SPL (105 dB – 90 dB or 15 dB) is only half the magnitude of the change in input (80 dB – 50 dB or 30 dB). No increase in output level is noted beyond an input level of 80 dB SPL. By definition, Figure 7B represents compression between 50 dB SPL and 80 dB SPL. Figure 7C also reveals compression despite the fact that the I-O curve at an input level of less than 90 dB SPL has a slope of 1.0. This is because slope of the I-O curve is 0.1 when the input changes from 90 dB SPL to 100 dB SPL (121 – 120/100 – 90 or 0.1).
Figure 7.
Input-output (I-O) curves of different hearing aids. (A) Linear with peak clipping, (B) wide dynamic range compression, and (C) compression limiting.
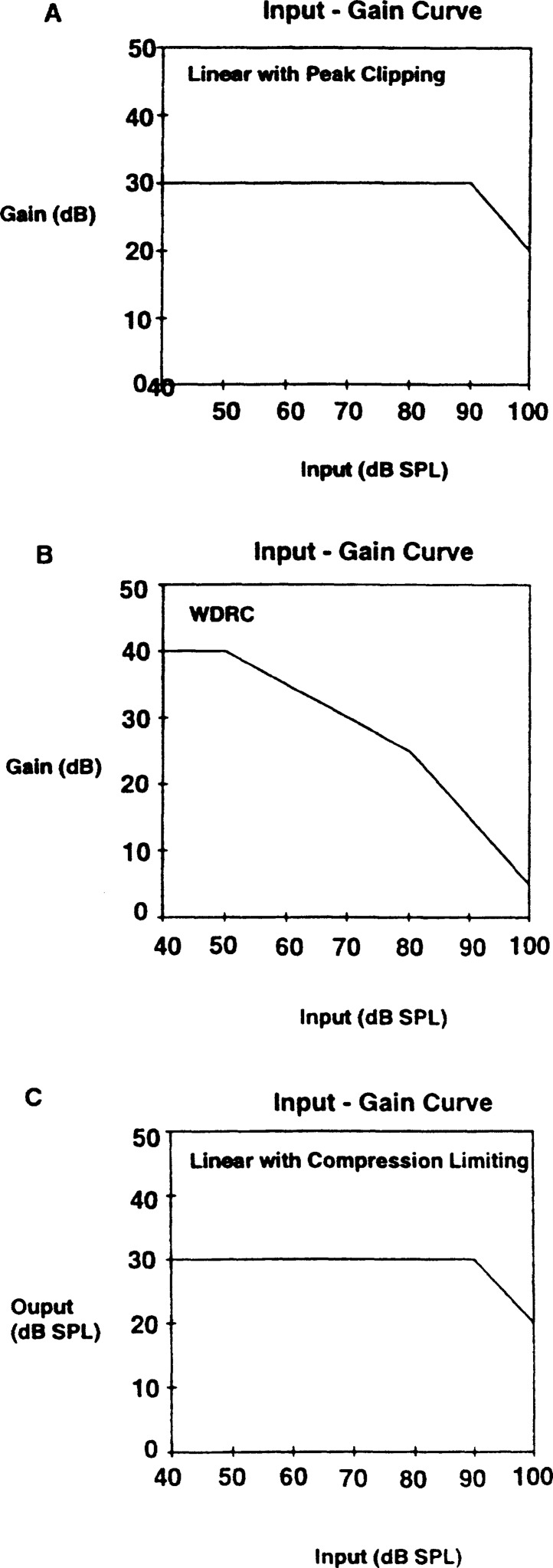
An alternative approach to determine if a hearing aid contains compression is to plot an input-gain curve (Figure 8). An input-gain curve differs from an I-O curve in that gain is plotted on the ordinate. The merit of the input-gain curve is intuitive. If a hearing aid provides diminishing increase in output when input increases, it reflects diminishing gain. Consequently, the input-gain curve of a compression hearing aid must have a portion with a negative slope that is greater than zero but is less than 1.0. That is, gain decreases slower than input increases. For example, Figure 8A shows that a linear hearing aid has a flat line (i.e., meaning constant gain for input below 90 dB SPL) prior to saturation. At and above an input level of 90 dB SPL, gain decreases at the same rate as input increases, i.e., 10 dB increases in input leads to 10 dB decrease in gain, or a negative slope of 1.0. By the above definition, no compression is used in this example. Figure 8B shows a downward slope at input greater than 50 dB SPL (reflecting gain reduction). This shows that the hearing aid is in compression at very low input level (50 dB SPL). For the compressed region (between 50 dB SPL and 80 dB SPL), gain decreases at half the rate of input increases (i.e., 10 dB increase in input leads to 5 dB decrease in gain). Above an input of 80 dB SPL, 10 dB increase in input results in 10 dB decrease in gain. This region suggests saturation rather than compression. Figure 8C shows that the hearing aid only goes into compression above an input level of 90 dB SPL. In this case, gain decreases by 9 dB for every 10 dB increase in input. Unless one examines the input-output curve (or input-gain curve) very closely, it may be difficult to distinguish between a linear peak-clipping hearing aid from a compression limiting hearing aid. One may wish to examine the curve over an extended input range (e.g., from 90 dB SPL to 120 dB SPL input instead of from 90 dB SPL to 100 dB SPL) to help decipher differences between these two types of output limiting options.
Figure 8.
Input-gain curves of the hearing aids shown in Figure 7: (A) Linear with peak clipping, (B) wide dynamic range compression, and (C) compression limiting.
CHARACTERIZATION OF COMPRESSION
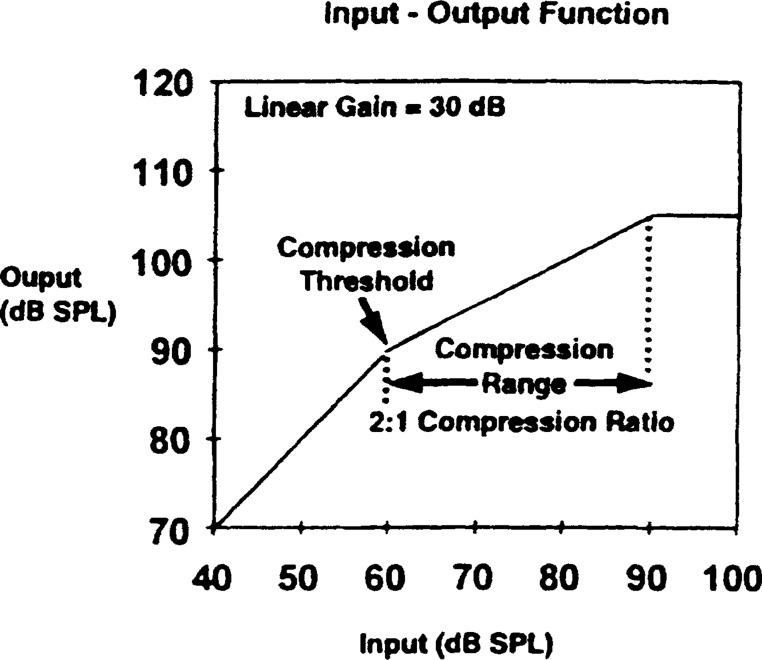
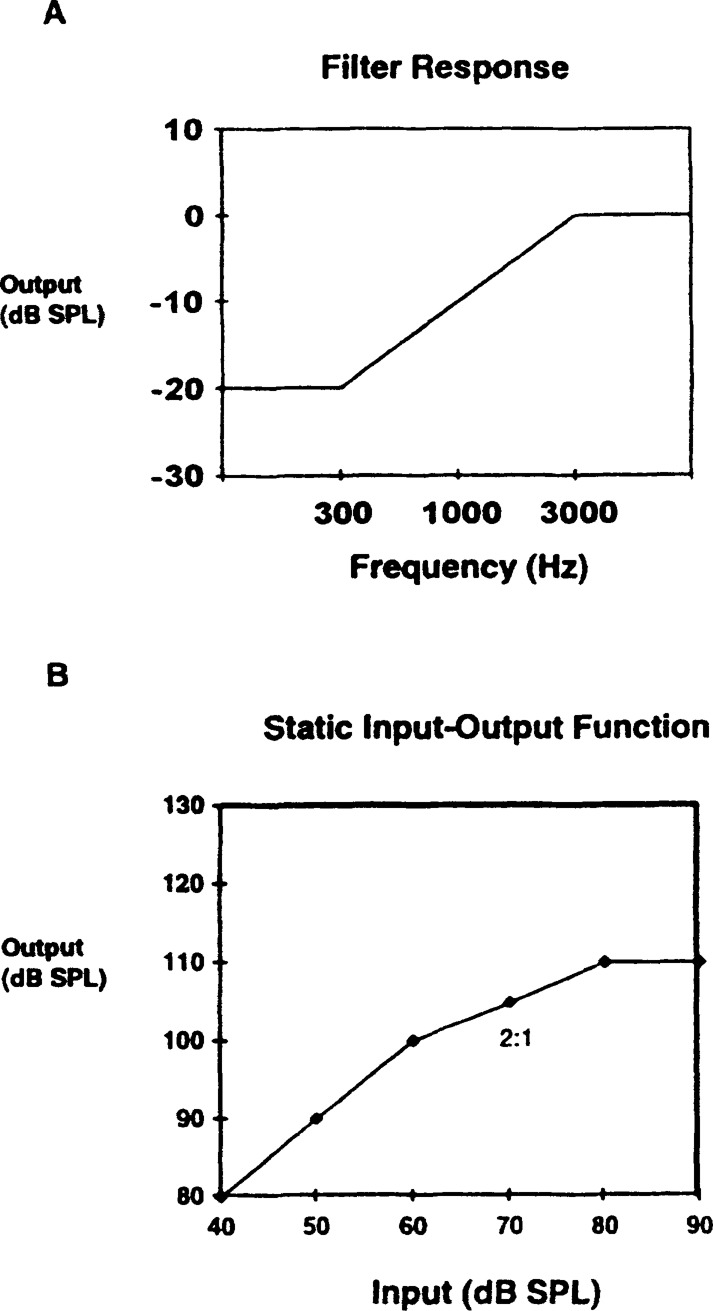
Compression systems are characterized by their static and dynamic properties when measured with steady-state 2000 Hz sinusoid (ANSI S3.22-1987). Frequently, an input-output curve is sufficient to report the static characteristics of a compression system. Figure 9 shows an I-O curve that characterizes a compression hearing aid. Details on the characterization of compression hearing aids can be found in Walker and Dillon (1982).
Figure 9.
Input-output curve showing the different static compression characteristics.
Static Compression Characteristics
Gain—the gain of a linear hearing aid is calculated as the difference between the output level and the input level when the hearing aid is in linear operation (i.e., prior to saturation). In the case of a compression hearing aid, a fixed gain value may be difficult to establish because the gain of such a device decreases with increasing input level. To meet quality assurance purpose in electroacoustic specification, most manufacturers report gain at a low input level (i.e., 50 dB SPL) or when the hearing aid is in linear amplification. An input-output curve (ANSI, 1987), or a series of output frequency gain curves at different input levels (ANSI, 1992) will be needed to determine gain at various inputs. Figure 9 shows that the gain is 30 dB (80 dB – 50 dB = 30 dB) below an input of 60 dB SPL. However, gain becomes 25 dB at an input of 70 dB SPL and 20 dB at an input of 80 dB SPL.
Compression threshold (CT)—represents the lowest input SPL at which the hearing aid changes from linear amplification to nonlinear amplification (i.e., slope less than 1, but not zero). This is frequently described as the kneepoint on the I-O curve. In Figure 9, the CT is 60 dB SPL.
Compression ratio (CR)—represents the ratio of the change in input levels to the corresponding change in output levels when the SPL of the input is within the compression range (CR = change in input/change in output). The nominal CR is calculated when the output reaches its steady-state value. The CR can also be calculated as the inverse of the slope of the I-O curve within the compression range. In this example, the CR is calculated to be 2:1 (90 – 60/105 – 90 = 2) whereas the slope of the I-O curve is 0.5 (105 – 90/90 – 60 = 0.5).
Dynamic Compression Characteristics
Attack and release times
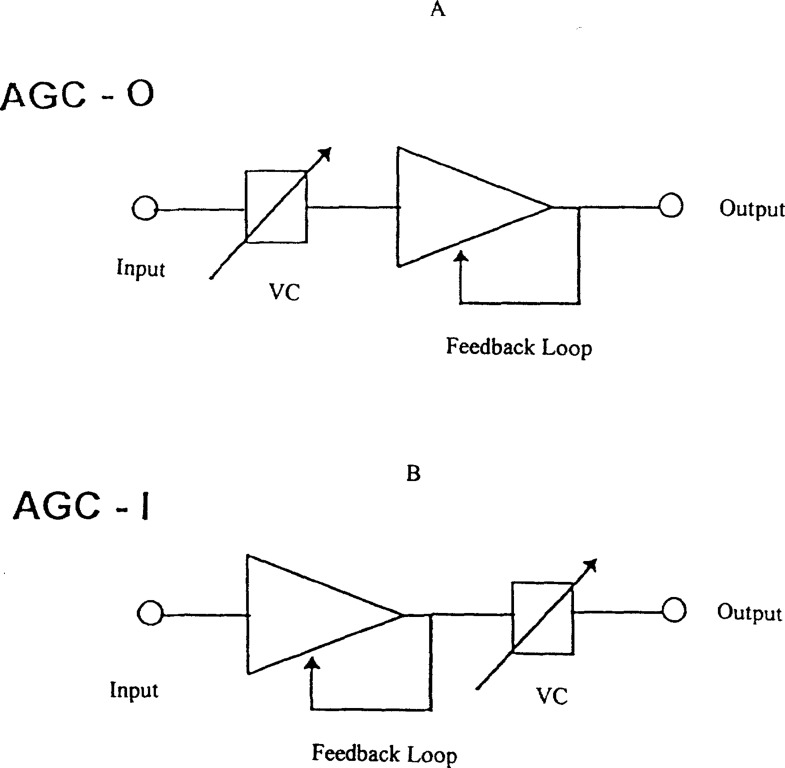
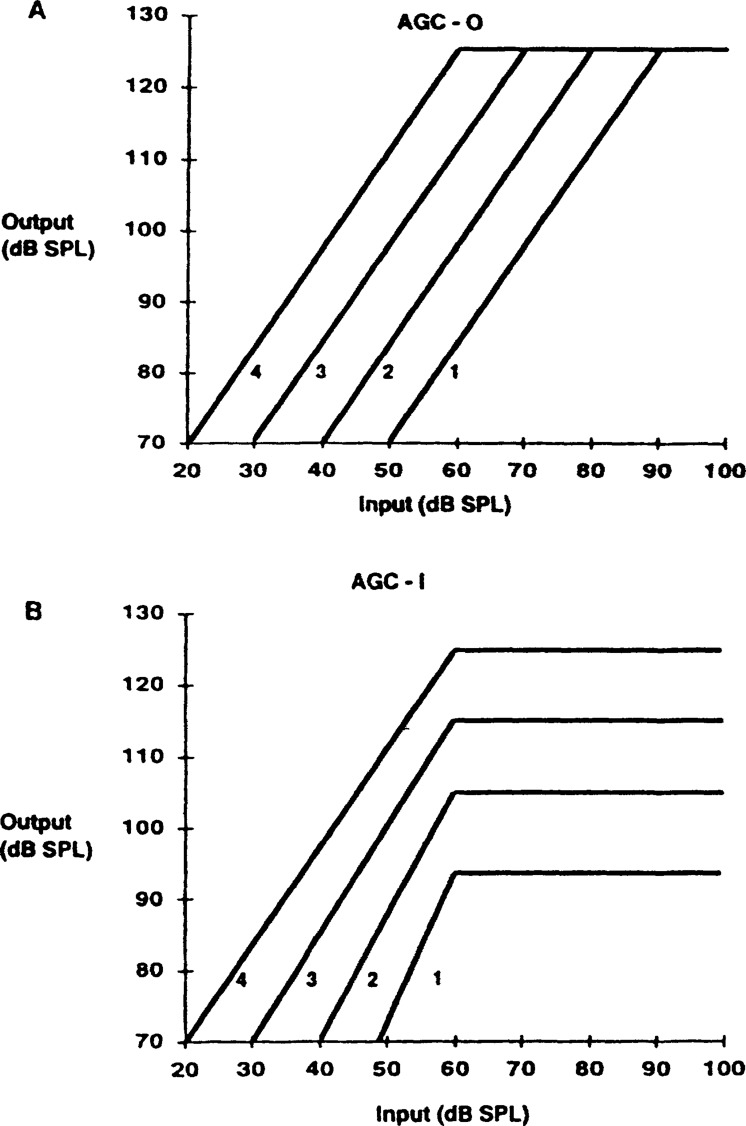
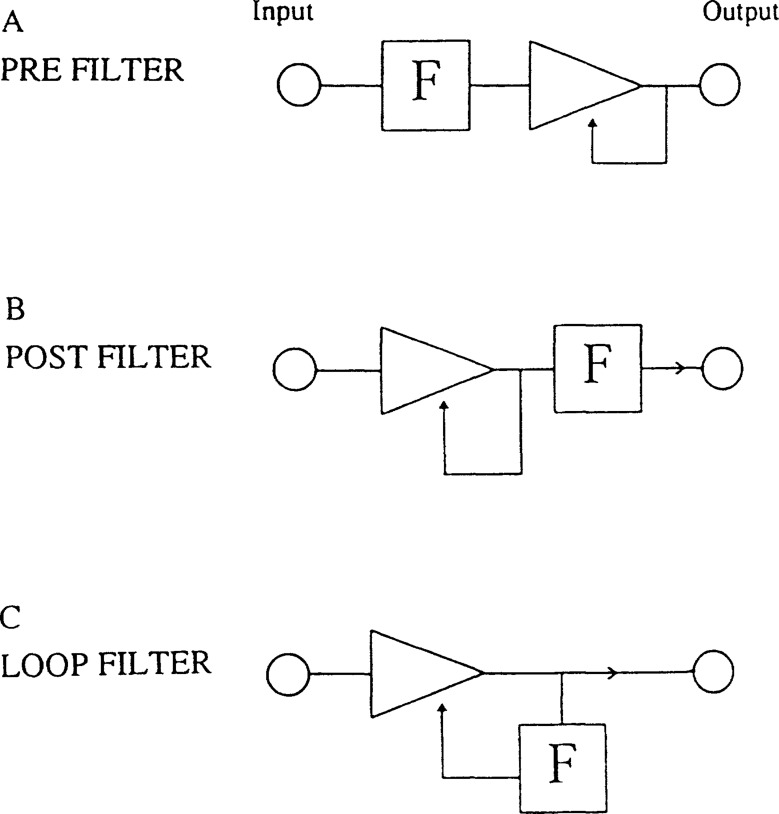
Compression circuits operate through the use of feedback loops. Figure 10 is a schematic diagram illustrating its action. A monitoring network measures the voltage or current level of the signal that is fed back. A decision is made on whether the signal level exceeds the compression threshold. If it does, a return signal goes to the amplifier to signal gain reduction. Otherwise, no gain reduction occurs.
Figure 10.
Schematic diagram of a compression circuit.
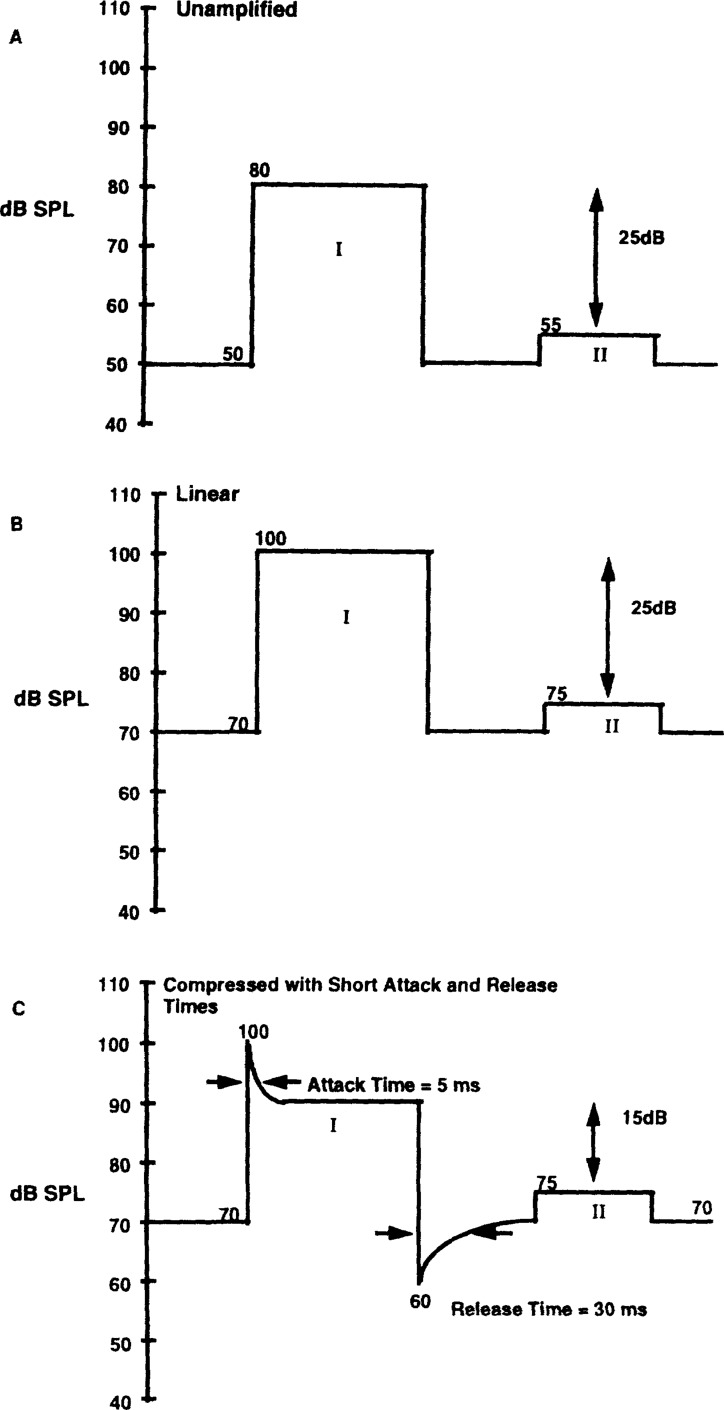
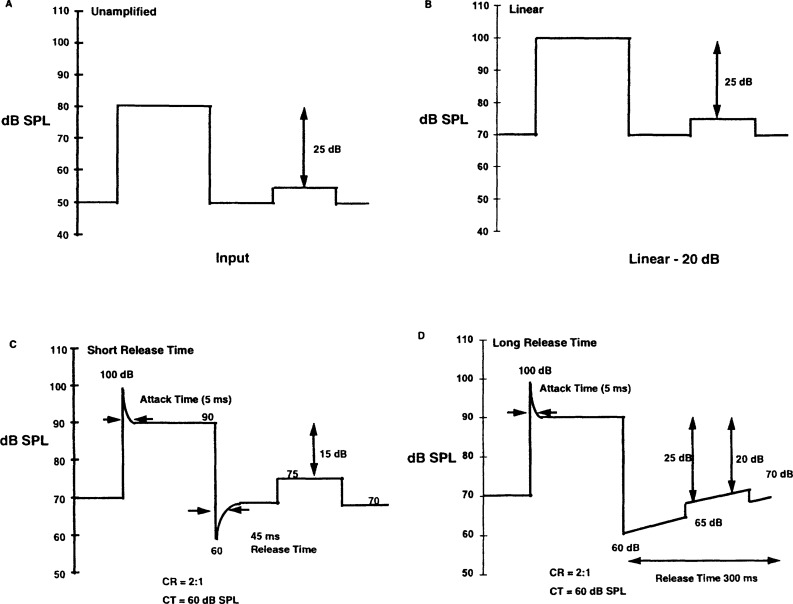
The time taken for the compression hearing aid to change from linear gain to within 2 dB of the compressed steady state (i.e., reduced gain) is called the attack time. The time taken for the compression hearing aid to return from the compressed state to within 2 dB of the linear steady state (i.e., full gain) is called the release time. Figure 11 is a simplified representation to illustrate the waveform changes with attack and release times. Figure 11A shows the unamplified signal with two bursts of energy peaks (I) and (II). Figure 11B shows the signal after it has been amplified linearly. Figure 11C shows the signal after it has been amplified by a compresssion hearing aid with a CT at 60 dB SPL, a CR of 2:1, and a gain of 20 dB. With linear amplification (Fig. 11B), the steady state output of (I) is at 100 dB SPL and the steady state output of (II) is at 75 dB SPL. The floor of the signal is amplified to 70 dB SPL. Figure 11C shows how the output waveform is modified with compression. Because the CT is at 60 dB SPL, signal (II) will be amplified by 20 dB to 75 dB SPL. Signal (I), however, is only amplified by 10 dB to 90 dB SPL. The time for the hearing aid to reduce gain so that the 100 dB SPL output is changed to within 2 dB of the 90 dB SPL steady-state output is the attack time (or 5 ms in this case). Because gain on the hearing aid is still at 10 dB when the input falls from 80 dB SPL to 50 dB SPL, the instantaneous output of the hearing aid is 60 dB SPL (50 dB + 10 dB). The time it takes for the hearing aid to return from 60 dB SPL to within 2 dB of the 70 dB SPL steady state output (i.e., full 20 dB gain) is the release time (30 ms in this case). In addition, the SPL difference between the two signals (I and II) is reduced from 25 dB (100 – 75) in the unamplified and linear amplification modes to 15 dB (90 – 75) in the compression mode.
Figure 11.
Illustration of attack and release times and associated output waveform from a compression hearing aid: (A) unamplified signal (B) linearly amplified output, and (C) compressed output.
The ANSI S3.22-1987 standard (ANSI, 1987) specifies that attack and release times be measured with a 2000 Hz sinusoid that abruptly changes from 55 dB SPL to 80 dB SPL. The sinusoid remains at that level for 2 seconds before it returns back to 55 dB SPL. The use of 2 signals with different steady-state durations is required to test compression hearing aids with adaptive and/or multiple release times. The assumption for using the 55–80 dB SPL signal level is that 80 dB SPL is typically above the compression threshold and 55 dB SPL is typically below the compression threshold. This choice of intensity levels is not uncommon with compression devices using compression limiting or automatic volume control. These types of compression hearing aids typically have a high compression threshold (above 60–65 dB SPL). The use of the same signal to measure the dynamic characteristics of a wide dynamic range compression hearing aid may be questionable. This is because the threshold of such hearing aid is often between 45 dB SPL-50 dB SPL. This shows that the hearing aid is in compression even for the 55 dB SPL portion of the test signal. A different signal level is needed if one wishes to characterize the dynamic aspects of compression hearing aids with low CT. Unfortunately, the most recent ANSI standard (ANSI, 1992) does not provide additional specification for evaluating the attack and release times of a non-linear hearing aid using composite noise signals.
The attack and release times of a compression hearing aid are designed to meet specific purposes. Typically, attack time is below 10 ms in order that the hearing aid can respond quickly to impulsive signals. The choice of release time may be less straightforward. Frequently, the choice is dependent on the specific purpose that the compression hearing aid is designed to serve. In so doing, some compromises may be inevitable. Short release time (< 50 ms) is used if the compression hearing aid is designed to follow the intensity variation encountered at the phonemic or syllabic level of speech. Longer release time is used to reduce distortion and/or maintain a comfortable listening level (Walker and Dillon, 1982).
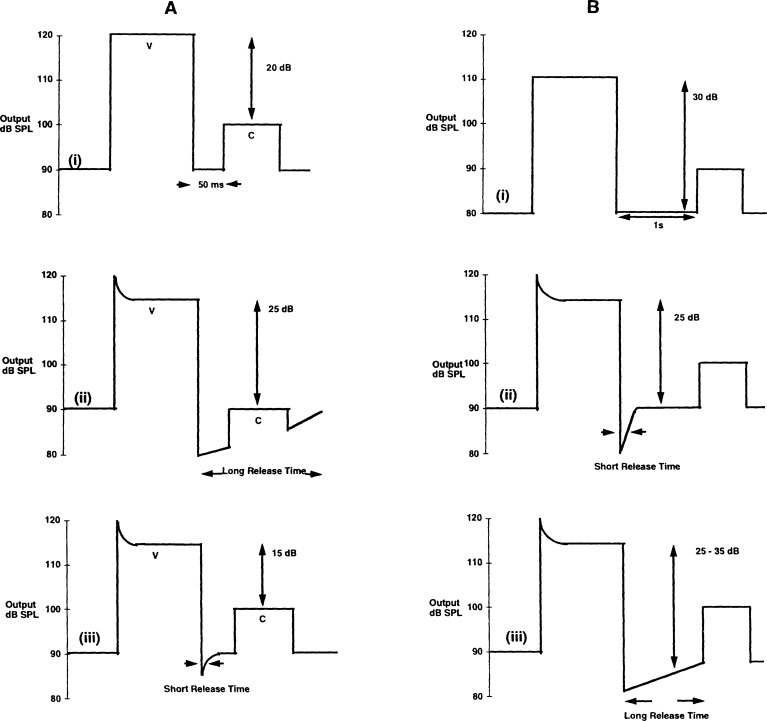
A compression hearing aid with a fixed release time may be problematic in some situations. Figure 12A-i is a simplified illustration of the envelope of a vowel-consonant (VC) syllable with short intra-syllabic interval when it is amplified linearly. Figure 12A-ii represents the output when a long release time is used. In this case, the hearing aid is still in the recovery phase when the consonant occurs. This suggests that the consonant will receive less than the full linear gain (level of consonant at 90 dB SPL). This may render the consonant inaudible. A shorter release time will return the hearing aid to full linear gain before the consonant. The level of the consonant is returned to 100 dB SPL (Figure 12A-iii). On the other hand, Figure 12B shows that a fixed short release time may be problematic when speech segment with long silent interval is encountered. Figure 12B-i again shows the output with linear amplification. It is assumed that the silent interval between the two speech segments is inaudible (80 dB SPL). Figure 12B-ii shows the output from a compression hearing aid with short release time. Note that the gain is higher than the linear hearing aid. Because linear gain quickly returns after compression, the silent interval between the syllabic structures is now amplified to 90 dB SPL. If the wearer's hearing sensitivity is better than 90 dB SPL (but poorer than 80 dB SPL), the interval which is previously inaudible will now be perceived as “pumping”, “breathy”, and/or “noisy”. The longer release time (Figure 12B-iii) will keep the silent interval in the recovery phase longer. The result is that the silent interval will be amplified to around 80 dB SPL. This may reduce the perception experienced with the shorter release time. Increasing the release time, and/or decreasing the gain of the compression hearing aid may help reduce the “breathy” or “noisy” perception.
Figure 12.
Effect of long and short release times on the output waveform when the input has (A) short intra-syllabic interval, and (B) long inter-syllabic interval. “V” represents vowel and “C” stands for consonant.
One attempt to solve this dilemma is the use of multiple release times and/or adaptive release time. A short release time may be used if the activating stimulus is a short, high intensity signal (e.g., impulsive sound). A long release time may be used if the activating signal is a long, moderately intense signal. It must be emphasized that the duration of the release time varies with the intensity and duration of the stimulus. It does not vary with the duration of the interval after the activating stimulus (which, of course, cannot be predicted precisely). The assumption is that short duration, high intensity sounds are probably impulsive in nature and do not occur regularly in daily situations. Consequently, when these stimuli are present, the circuit needs to return to linear gain as quickly as possible. One further assumes that the short duration impulsive sounds would typically not be followed by long, silent intervals. On the other hand, since daily acoustic signals (including speech) typically have a finite duration, longer release time is employed in daily situations (Moore et al, 1991) to minimize “breathiness” perception. As discussed earlier, a long release time also suggests that the hearing aid is in a “reduced gain” state longer. Release time that changes with the duration of the activating stimulus has been called adaptive release time. Many manufacturers utilize adaptive release time in their compression hearing aids (e.g., Phonak supercompression, K-Amp, Telex) to minimize the perceptual effects of “noisiness” and “breathiness” while reducing saturation-induced distortion.
Although not described as an adaptive release time circuit, Moore and Glasberg (1988), and Moore et al (1991) reported a laboratory based, prototype compression system which they called the “dual front-end AGC” circuit. Rather than having one feedback loop, this circuit has two voltage generators (fast control and slow control) to which the input signal is measured and compared. The voltage generator with the larger voltage feeds the signal to the AGC amplifier to determine its compression characteristics. The fast control voltage generator has a higher compression threshold than the slow control voltage generator. It has a short attack time and a release time of 100 ms. The slow control voltage generator has a long attack time (few hundred milliseconds) and a long release time of several seconds. Effectively, the two release times used in this circuit is able to handle both short, impulsive and long, steady state signals.
While one can describe a compression hearing aid by its static and dynamic characteristics, in reality, such clear demarcation seldom exists. The static compression characteristics describing a compression hearing aid will be modified by its dynamic properties. One such static characteristic, the compression ratio, is modified by the attack and release times of the hearing aid and their interaction with the acoustic signals. Such interactions are described in the following section.
Effective compression ratio
The compression ratio that is determined by measuring the steady-state response of the compression circuit to sinusoids (i.e., nominal CR) may not reflect the actual or effective compression ratio in the real world. In other words, the ability of the compression circuit to provide more amplification to low intensity sounds (re: conversational speech) and less amplification to high intensity sounds (re: conversational speech) may be poorer than is indicated by its nominal values. In such cases, the theoretical advantages offered by a compression hearing aid will be jeopardized. Furthermore, the need to precisely determine “the best” compression ratio will be questionable. Factors that can affect the effective compression ratio have been studied using modulation transfer functions (Viemeister, 1979). These factors include the pre-compressor gain on the hearing aid, the peak-to-valley ratio of the input signals, the overall input level, the time constants of the compression circuit, and the intervals between different acoustic peaks (Stone and Moore, 1992). Because daily acoustic signals (including speech) fluctuate greatly in intensity levels, peak-to-valley ratios, and inter-stimulus intervals, such factors can interact with the time constants of the compression hearing aid to yield a lower compression ratio.
Figure 13 illustrates how the release time may affect the effective compression ratio. Let us assume that an input signal (Figure 13A) has a constant 50 dB SPL noise floor and two segments that are separated by 100 ms. The more intense segment is at 80 dB SPL and the less intense segment is at 55 dB SPL (difference of 25 dB). Figure 13B shows the output from a linear amplifier with 20 dB gain. The output sound pressure level is thus 20 dB higher than the input signal. The uniform increase in SPL across all segments suggests that the 25 dB difference between the intense and the less intense segments is maintained. In Figure 13C, this signal is presented to a compression system with a CT at 60 dB SPL, a CR of 2:1, a linear gain of 20 dB, an attack time of 5 ms, and a release time of 45 ms. Five ms (i.e., attack time) after the compressor is activated, the intense portion will have a steady-state output of 90 dB SPL (within 2 dB). The less intense portion will have a steady-state output of 75 dB SPL because the full 20 dB gain is available. Full gain is available because the release time of the hearing aid is short enough to return to linear gain before the less intense segment. The intensity difference between the intense and less intense segments becomes 15 dB (90 – 75). This signifies a reduction of 10 dB in level difference between the intense and less intense segments of the acoustic input.
Figure 13.
Example to illustrate the reduction in compression ratio from the interaction between release time and inter-syllabic interval. (A) Unamplified signal, (B) linearly amplified signal, (C) short release time, and (D) long release time.
A different outcome is seen when the release time of the compression circuit is extended to 300 ms. Rather than returning to the full 20 dB gain for the less intense segment (i.e., 55 dB SPL portion), Figure 13D shows that gain prior to the onset of the less intense segment is only 10 dB. Gain restoration is not complete until 300 ms after the offset of the intense segment. This means that the intensity level of the less intense segment is at 65 dB SPL (55 dB + 10 dB). The intensity difference between the intense and less intense segments remains at 25 dB. This is 10 dB greater than the case when the release time is short. Thus, although the nominal compression ratio is 2:1, the measured compression ratio is unity (i.e., 1.0). In this case, only gain reduction occurs.
Various authors have indicated that the effective compression ratio is dependent on the magnitude of the release time to the magnitude of the intersyllabic interval (Blesser, 1969; Stone and Moore, 1992). The longer the release time (for the same fixed intersyllabic interval), the more likely the effective compression ratio deviates from the nominal value. Blesser (1969) proposed the following equation to relate the effective compression ratio to the release time.
where
Ke = effective compression ratio K0 = static compression ratio
k = hardware constant
T = period of activating pulse
tr = release time
The interval “T” in Blesser's equation can be used to represent the syllabic and intersyllabic intervals typically found in daily speech. For everyday speech, “T” may vary from 20 ms to 300 ms, although the typical duration of a syllable is between 200 to 300 ms. Additionally, these intervals may vary among speakers, listening environments, and different parts of the speech segment. For this reason, nominal CR will necessarily deviate from the effective CR at some time.
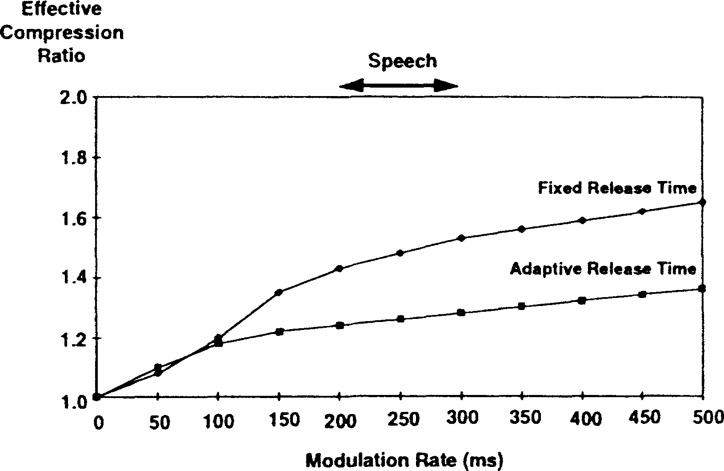
One may speculate that the disagreement between nominal and effective compression ratio should be minimal for hearing aids with adaptive release time. This is because such hearing aids adapt to the duration of the signal. Baechler (1995) measured the effective compression ratio of a commercial single-channel compression hearing aid (CT = 45 dB SPL, CR = 2:1) using modulation transfer studies. The effective compression ratio was determined using both fixed and adaptive release times. Figure 14 shows that in the fixed release time condition, the effective compression ratio ranged from 1.4 to 1.6 when the modulation interval was similar to that found in conversational speech (with a duration of 200 ms to 300 ms). The effective CR decreased to approximately 1.3 when adaptive release time was used. This illustrates that adaptive release time, rather than maintaining the nominal CR, may actually decrease the CR further and “linearize” a compression hearing aid (i.e., make it work like a linear hearing aid). This may be due to the fact that daily acoustic stimuli require the use of a long release time. Moore et al (1991) also commented that despite the fact that their “dual-front-end AGC” circuit has two time constants, “normally, the operation of the AGC amplifier is determined by the slow-acting control voltage,” meaning that the longer release time is typically used in the normal operation of the AGC amplifier.
Figure 14.
Effective compression ratio of a commercially available compression circuit with fixed release time of 50 ms, and adaptive release time.
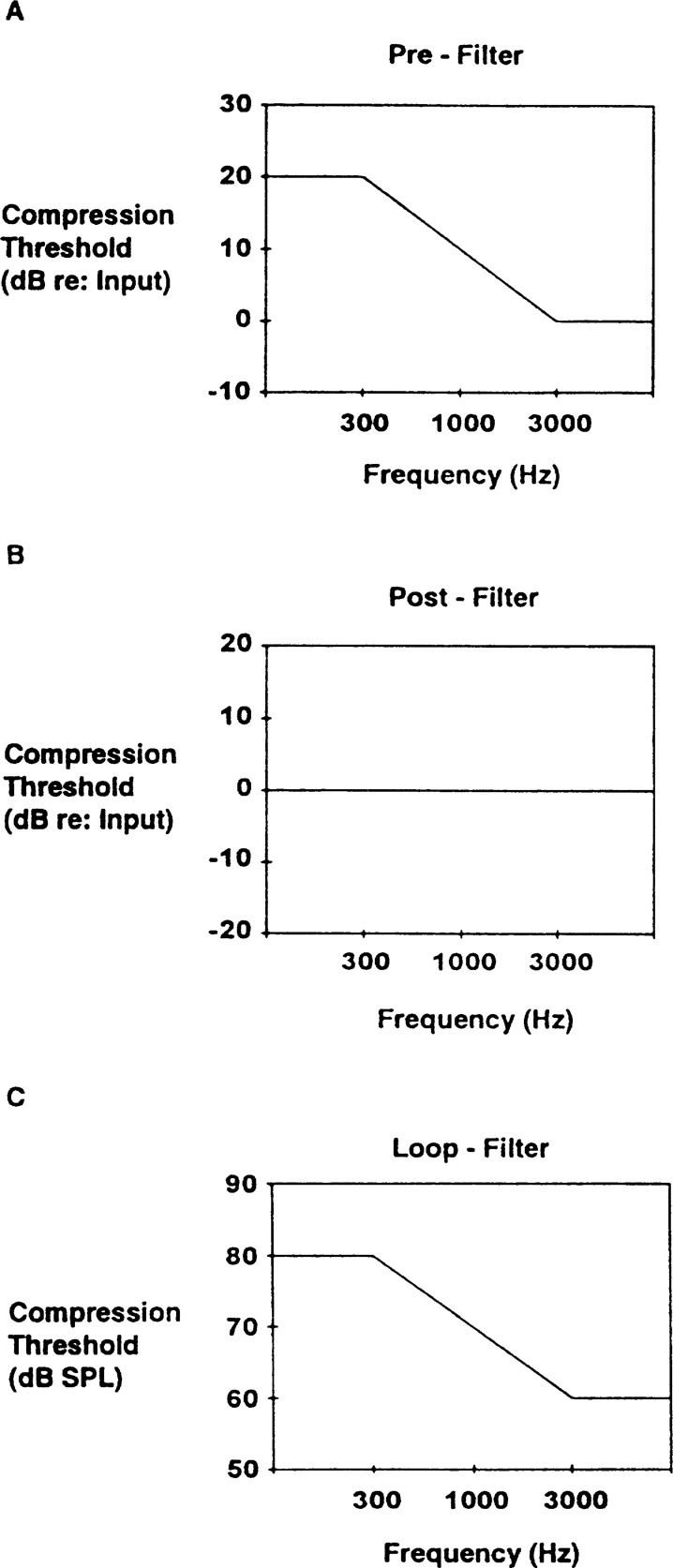
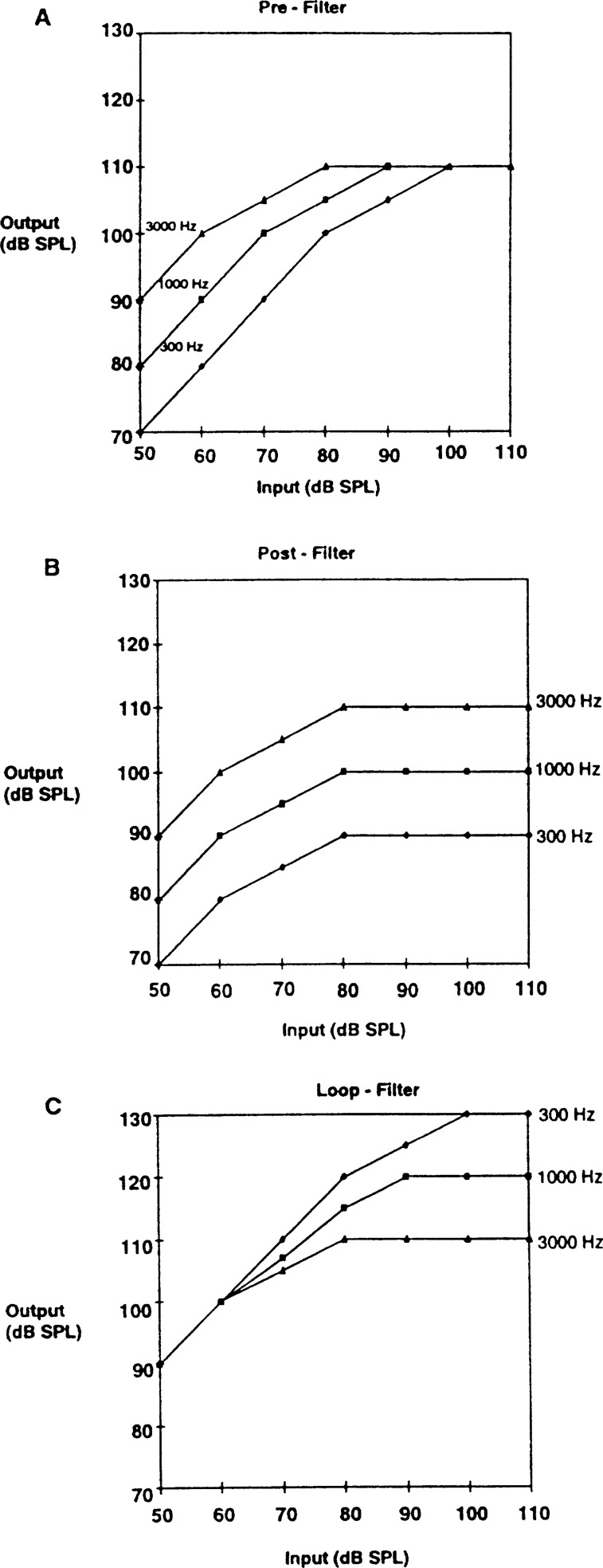
CLASSIFICATION OF COMPRESSION CIRCUITS
Compression hearing aids are broadly classified into three types based on their intended functions and compression characteristics (Braida et al, 1979; Walker and Dillon, 1982; King and Martin, 1984). This section gives a brief description of the three common types of compression, followed by a summary table comparing their features. These three types of compression include: compression limiting (CL), wide dynamic range compression (WDRC), and automatic volume control (AVC).
Compression Limiting (CL)
A difficulty in using peak clipping to limit the output SPL is the occurrence of saturation-induced distortion products (i.e., harmonic and intermodulation distortion) when the output SPL exceeds the saturation limit of the hearing aid. Logically, saturation-induced distortion will never occur if output SPL never saturates the amplifier. This is the basis for a compression limiting (CL) or output compression limiting (OCL) hearing aid. Specifically, a CL hearing aid is designed to (1) prevent the acoustic output from exceeding a preset level (thereby ensuring loudness tolerance); (2) minimize the distortion products that may be generated at a moderate to high input level, while (3) minimizing temporal and spectral distortion of the acoustic input at low and intermediate levels by providing linear amplification for these input levels.
In order that the amplifier remains in linear amplification for as long as possible, a low to moderate gain CL hearing aid typically has a high compression threshold (greater than 75 dB SPL). On the other hand, a high gain CL hearing aid may have the CT as low as 60 dB SPL. In addition, a high compression ratio (greater than 5:1) is used in order to keep the already high output SPL from reaching saturation. Moreover, a short attack time (less than 5 ms) and a moderately long release time (about 100 ms) is used in order to quickly respond to and recover from high intensity sounds. Adaptive release time has been used by several manufacturers in their CL hearing aids. This combination of compression characteristics suggests that the hearing aid amplifies linearly for most input levels. It only goes into compression when the combination of VC setting and input level result in a high output SPL that exceeds the preset maximum output level.
Compression limiting hearing aids have been used commercially since the 1950s (Lynn and Carhart, 1963). They have been fitted in a manner similar to the fitting of conventional linear peak clipping hearing aids. The output threshold level is typically set below the wearer's loudness discomfort level and expressed in dB SPL (not dB HL). Many current conventional and programmable hearing aids utilize this form of compression.
There have been research studies comparing the relative benefits of linear hearing aids with peak clipping versus compression limiting. These studies showed that a speech recognition score was higher with compression limiting in comparison to peak clipping when the stimuli were presented at the level near the compression threshold (Davis et al, 1947; Hudgins et al, 1948). This finding is possibly due to the reduction of saturation-induced distortion products from compression limiting. Other studies, although with less convincing results, suggest the possibility that changes in the compression values used in the studies may alter the outcome. For example, in a study by Blegvad (1974), a shorter release time (less than 200 ms) may yield results that can support the use of compression limiting. In a study by Sung and Sung (1982), it was demonstrated that a higher compression threshold (60 dB SPL and 70 dB SPL) yielded a higher speech recognition score than a lower (50 dB SPL) compression threshold.
It needs to be recognized that the difference between a linear hearing aid with peak clipping and a hearing aid with compression limiting is the manner in which they handle the high output sound pressure level (occurring from high input and/or high gain). A fair comparison between these two types of hearing aids must be made at high input and output SPLs. In addition, evaluative techniques such as subjective judgment of sound quality and preference may be used. These criteria may be more sensitive than speech recognition scores because the difference between peak clipping and compression limiting is not one of audibility, but of sound quality. This is reported by Dillon (1988) who showed that hearing impaired listeners expressed higher clarity judgments for compression limiting in comparison to peak clipping. Hawkins and Naidoo (1993) compared subjective preference for peak clipping and compression limiting using paired comparisons of sound quality and clarity. All twelve subjects with moderate degree of hearing loss preferred compression limiting when the input stimuli were presented at a high intensity level. At such an intensity level, saturation was reached with the peak clipping hearing aid, but not with the compression limiting hearing aid.
Dawson et al (1991) studied the subjective preference of 76 subjects with severe-to-profound hearing loss between peak clipping and compression limiting hearing aids. These hearing aids were matched in frequency response. 43 of the 44 subjects with pure tone averages (PTA) less than 90 dB HL favored the compression limiting hearing aid. Only 16 of 32 subjects with PTA greater than 90 dB HL favored the compression limiting hearing aid. These subjects preferred the higher output SPL from the peak clipping hearing aid. The authors concluded that peak clipping may be useful for those with profound loss who use their hearing aids at saturation. Compression limiting, they contend, may be useful for listeners with up to a severe-to-profound hearing loss. Killion (1995) also recommended compression limiting for his Type III patients who have severe-to-profound sensorineural hearing loss.
The general research findings suggest that compression limiting is preferable over peak clipping. This is because of its ability to reduce distortion while maintaining the temporal and spectral integrity of the signal most of the time. Dillon (1988) suggests that such benefits can be enjoyed by hearing impaired patients with mild-to-moderate degree of hearing loss. Additionally, patients with severe-to-profound hearing loss who have sufficient residual frequency selectivity may also benefit from reduced distortion. It is unclear if patients with profound hearing loss would indeed prefer peak clipping over compression limiting. The observation in Dawson et al (1991) on the preference for peak clipping over compression limiting may reflect the reduced output SPL in the compression limiting hearing aid. Perhaps an increase in output sound pressure level (from increased gain) and an increase in SSPL90 setting may change this observation.
Reduction of distortion products that result from peak clipping may not always prove beneficial. Some hearing impaired listeners with precipitous high frequency hearing loss may depend on the intermodulation distortion products (that are produced during saturation) as cues to aid in speech perception (Ingelstam et al, 1971). Reduction of distortion in a compression limiting hearing aid reduces this cue and can decrease intelligibility. Some patients may report a loss of “naturalness” in sound quality. More work is necessary to determine if a compression limiting hearing aid is more acceptable for people with profound hearing loss. One aspect of compression limiting may be readily accepted. It yields less saturation-induced distortion than peak clipping at high input level, while maintaining the temporal and spectral contrast of input signals at low to moderate intensity levels. These benefits can improve speech recognition score or enhance subjective preference if such factors as distortion and temporal integrity have deleteriously affected the hearing impaired person's performance with the peak clipping hearing aid.
Wide Dynamic Range Compression (WDRC)
The hypothetical advantages of compression hearing aids are not limited to the reduction of distortion. By varying the compression settings from those used in a compression limiting hearing aid, additional advantages may also be realized. When the compression hearing aid is designed with short attack time (less than 5 ms), short release times (from 20 ms to 100 ms), low compression threshold (less than 50 dB SPL), and low compression ratio (less than 5:1), it is referred to as wide (or full) dynamic range compression (WDRC) or syllabic (or phonemic) compression (Dillon, 1988). Such nomenclature has been suggested because the low compression threshold ensures that the full range of speech (from soft to loud) will be “compressed” most of the time (thus WDRC). It is called syllabic (or phonemic) compression because the short release time would allow the compression hearing aid to follow the envelope fluctuation among syllables or phonemes typically seen in conversational speech. Using Dillon's (1988) criterion of short release time for WDRC, a compression hearing aid with long release time or adaptive release time should not be labelled as WDRC. The following is a discussion of how different hypothetical advantages can be achieved with WDRC.
Normalization of Loudness Contour
Figure 15A shows the loudness growth function of a normal ear and a moderately impaired ear. It is obvious that while hearing loss raises the thresholds (i.e., 10 dB SPL for the normal ear and 50 dB SPL for the impaired ear are judged to be “too soft”), high intensity sounds appear equally loud to a normal and an impaired ear (i.e., both rated the 100 dB SPL signal as “loud”). If one can assume that the difference in intensity levels for the normal and the impaired ear to reach the same loudness perception would indeed represent the gain value to restore normal loudness perception to the impaired ear (Figure 15B), loudness normalization can be accomplished by providing significantly more gain at the low input level and decreasing gain for the higher input level. For example, Figure 15B shows that 40 dB SPL is necessary for the normal ear to report a “soft” perception while the impaired ear needs a level of 65 dB SPL. Thus the gain at an input level of 40 dB SPL is 25 dB (65 – 40). On the other hand, the gain is 20 dB (75 – 55) for the impaired ear to reach “comfortable” loudness when such perception requires an intensity level of 55 dB SPL in the normal ear and 75 dB SPL in the impaired ear. In order that “normal loudness” is achieved in the impaired ear, the rate of output level increase with input level increase (i.e., slope, which is the inverse of CR) as seen in an input-output function (Figure 7B) should be equal to the slope of the curve generated between the difference in loudness-growth functions for the normal hearing and the hearing impaired ear (Figure 15B). By providing greater gain at low intensity inputs, WDRC can ensure that such sounds are audible. By providing a low compression ratio (e.g., < 5:1), one can ensure that adequate output SPL is available.
Figure 15.
(A) Hypothetical loudness growth function of normal hearing ear and moderately hearing-impaired ear. (B) Output intensity levels for normal hearing and hearing-impaired ears to reach the same loudness perception. The SPL difference between the normal and impaired ears represent the desired gain in the hearing aid to achieve “normal” loudness for the impaired ear.
There are also physiological observations that suggest the use of WDRC for hearing impaired people with mild-to-moderate sensorineural hearing loss. Brownell et al (1985) suggested that the outer hair cells (OHC) in the normal cochlea, because of their electromotile properties, amplify the amplitude of the basilar membrane vibration at low input level. The result is that the inner hair cells (IHC), which make direct synaptic connection with the auditory fibers, can be stimulated even at low input SPL (IHC, because of their lack of coupling to the tectorial membrane, are not easily stimulated until high input SPL). The effect of the OHC on the IHC at high intensity inputs may be minimal, since high intensity sounds result in sufficient vibration of the basilar membrane to stimulate both the OHC and IHC. This magnification function of the low intensity sounds is a non-linear property of the normal cochlea. This property diminishes with OHC loss. The result is that the IHC cannot be stimulated and no auditory sensation results for low intensity signals. In humans, it is estimated that a sensorineural hearing loss of 60 dB could result from complete OHC damage without damage to the IHC (Norton, 1992).
A WDRC hearing aid has been suggested as a mechanism to compensate for the loss of non-linearity in the auditory system that results from the loss of OHC (Killion, 1995). For a cochlea without any OHC, basilar membrane displacement is a linear function of input at all intensity levels. That is, unit increase in stimulus intensity leads to unit increase in basilar membrane vibration. Consequently, in order to provide more displacement of the basilar membrane at low input levels (so that the IHC of the impaired ear can still be stimulated), a hearing aid must provide more amplification at low intensity input than at high intensity input. The magnitude of the basilar membrane vibration at high input level should be sufficient to stimulate the IHC. A WDRC hearing aid meets this differential gain requirement.
Although the concept of loudness normalization with compression is of practical and theoretical interest, there are several issues that must be considered carefully. First, what is the user benefit of loudness normalization? Is there any evidence to suggest that loudness normalization implies improved speech intelligibility and/or sound quality? Second, is it necessary to perform loudness scaling in order to define the compression threshold and compression ratio on a WDRC hearing aid? Third, can the result of loudness scaling be directly applied to commercially available WDRC hearing aids to achieve “normal” loudness perception across all frequencies? Last, is there any relationship between the compression ratios determined during loudness scaling and the effective compression ratio in daily situations?
Does Loudness Normalization Result in Improved Speech Intelligibility?
One must accept the premise that an inaudible signal is an unintelligible signal. However, once a signal is audible, there is no direct evidence to suggest that loudness normalization results in enhanced speech intelligibility. Kuk and Lau (1995) correlated perceived loudness and perceived intelligibility ratings. Subjects listened to discourse passages presented at different overall intensity levels under two signal-to-noise ratios (SNR). When the SNR = +5, a mild positive correlation (r = 0.26) was observed between perceived loudness and perceived intelligibility. A stronger correlation was seen at the lower intensity level than at the higher intensity level (from r = −0.1 at an input level of 75 dB SPL to r = 0.54 at an input level of 55 dB SPL). On the other hand, when the SNR = −5, the correlation between perceived loudness and perceived intelligibility was negligible (r = −0.15). There are at least two implications. First, at least for perceived intelligibility, loudness and intelligibility are not strongly related when audibility is ensured. Second, even when loudness and intelligibility are correlated, the correlation is dependent on the SNR of the listening condition and not simply its overall level.
Another study may also add doubt to the relationship between loudness normalization and intelligibility. Nabelek (1983) compared word recognition scores on the modified rhyme test in eight hearing impaired subjects with three compression systems that differed in their compression thresholds. One is termed a “whole range compression” in which most of the variation in speech levels is in the range of compression (i.e., similar to WDRC). One is termed a “high level compression” in which only the high level segments of speech are compressed (i.e., similar to compression limiting). The last is termed “low level compression” in which lower levels of speech are compressed and higher levels are amplified linearly. A CR of 1.7:1 was used with short attack and release times (Ta = 1 ms, Tr = 30 ms). Three SNR (quiet, +5, 0) were used. No significant difference in word recognition score was found among the three systems.
In the same study, Nabelek (1983) also compared word recognition scores in noise where there was no compression, and at CR of 2.5:1, 5:1, and 10:1. Word recognition score was poorer in the compressed mode than in the no compression mode. No difference in word recognition score was noted between a CR of 2.5:1 and a CR of 5:1. The lowest word score was found with the CR at 10:1.
One must remember that loudness scaling addresses only psychophysical processing in the intensity domain. Processing abilities in other psychophysical domains, like frequency (spectral) and time (temporal) are not considered in loudness scaling. At this time, many authors feel that the slope of the loudness growth function (and similarly, the compression ratio) may have minimal effect on speech recognition provided that (a) audibility is ensured, (b) the maximum output sound pressure level is within the wearer's tolerance limit, and (c) the hearing aid output is free of distortion products (e.g., Nabelek, 1983; Dillon, 1988; Moore, 1990; and Van Tasell, 1993). This is not to say, however, that hearing impaired subjects are insensitive to the compression ratio of a compression hearing aid (e.g., Neuman et al, 1994). The use of speech recognition tests may not be sensitive enough to differentiate among compression ratios. Hearing impaired subjects may find subjective sound quality difference among compression systems that achieve various degrees of loudness normalization. Future research in this area may consider the inclusion of subjective criteria.
Is Loudness Scaling Necessary to Set Compression Parameters?
Loudness scaling procedures have been used in order to determine the optimal compression settings for restoration of “normal” loudness perception (Pluvinage, 1989; Allen and Jeng, 1990; IHAFF, 1994). One of the implicit assumptions behind loudness scaling is that the results will define the loudness growth characteristics of the impaired ear. The goal is to select compression settings that can result in an I-O curve having the same characteristics as the loudness growth curve. From the previous section one cannot but wonder the efficacy of using the results of loudness scaling to adjust compression settings. This is because a substantial difference in compression threshold or a difference in compression ratio did not result in any significant difference in word recognition score. A tentative conclusion is that the implementation of individual loudness growth information may not provide additional enhancement of speech recognition ability in comparison to the information available from computational methods based on the individual's dynamic range considerations (Killion, 1994; Cornelisse et al, 1995). Further research is necessary to examine this hypothesis.
There are two qualifications to the above speculation. First, speech intelligibility alone is considered. Matching the compression characteristics to the individual's loudness growth function may have other advantages, e.g. improvement of subjective comfort or ease of listening (Moore et al, 1992). Such improvement is also important to a hearing aid wearer in the acceptance of hearing aids. Second, CR based on the consideration of dynamic range information may be appropriate for the “average” hearing impaired listener, but may fall short of meeting the individual loudness requirement of every hearing impaired person. Rather than determining the compression settings based on calculations alone (which is efficient but may not be individualized) or from the loudness growth curve (which is individualized but may not be as efficient as calculation), a compromise is to use the dynamic range information of the individual listener to determine CR initially. In addition, based on the listener's reaction to the initial setting, further fine-tuning of the compression settings may be necessary. This approach may improve the efficiency of the fitting process while accounting for individual differences. Additional research is necessary to examine the validity of this approach.
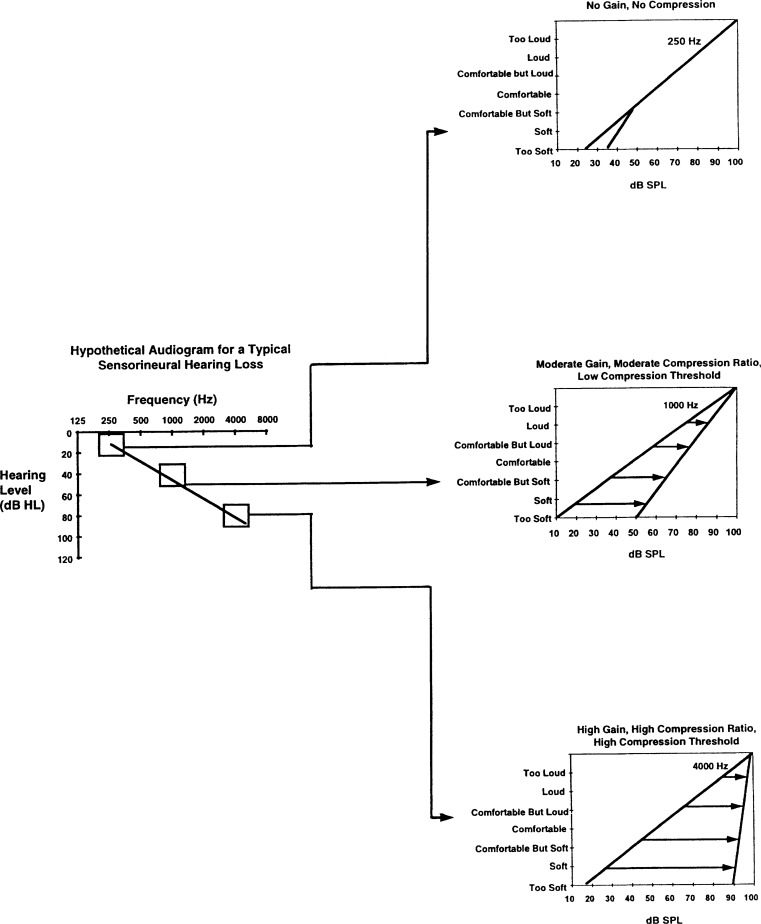
Do Commercial WDRC Hearing Aids Achieve Normal Loudness Growth across All Frequencies?
Current methods of loudness scaling may only provide an approximate match to the loudness growth functions of the impaired ear. Although there are commercial units that allow adjustment in up to thirteen frequency channels, for practical reasons, most scaling procedures are restricted to two to six frequencies. The average loudness growth curves of these frequencies is used to determine the compression ratio for a single or multiple channel compression system. In other words, a single compression ratio is used for more than one frequency region. On the other hand, if one wishes to fully compensate for the loudness difference between normal and impaired ear, it is necessary to normalize this perception at all frequency regions. Because of the differential sensitivity at each frequency region, each may have its own dynamic range, and thus requires a different compression ratio. Figure 16 uses a typical sloping high frequency sensorineural hearing loss to illustrate the point. In the normal low-frequency region (250 Hz), no gain nor compression is required to restore normal loudness. In the mid-frequency region (1000 Hz) where a moderate loss is seen, a moderate amount of gain, coupled with a compression ratio of 1.8:1 (100 – 10/100 – 50 = 1.8) and low compression threshold may be appropriate. In the high-frequency region (4000 Hz) where a profound loss is seen, high gain, high compression ratio of 8:1 (100 – 20/100 – 90 = 8), and perhaps a high compression threshold will be needed. Intermediate gain and compression settings are needed for intermediate frequencies. Complete loudness normalization is possible only when different compression settings are used at different frequency regions. An exception may be that of a flat loss where the same dynamic range may be assumed for all frequency regions. A single channel compressor, and to a certain extent, those with two or three channels cannot be expected to restore normal loudness at all frequencies. At least in theory, the use of a multiple channel compression system that has as many frequency channels as there are “critical auditory regions” or “critical bands” is needed. Additionally, each of these channels must allow independent adjustment of compression parameter. The optimal number of channels in a compression hearing aid to achieve complete loudness normalization needs further examination.
Figure 16.
Hypothetical audiogram showing the difference in dynamic range (and thus compression) characteristics across frequencies.
What Is the Effective Compression Ratio in Daily Situations?
Recall that the effective compression ratio is a factor of the interaction between the time constants used and the inter-syllabic and intra-syllabic intervals (for speech stimuli), peak-to-valley aspect of the stimulus, and gain prior to compression (Stone and Moore, 1992). Because daily speech fluctuates widely in intensity level and syllabic intervals, the effective compression ratio will be lower than the one calculated from data obtained using loudness scaling of steady-state sinusoids or narrow-band noise. The implication is that even if one has an infinite number of channels in a compression system and can achieve normal loudness perception at all frequency regions in the clinic, one still may not achieve perfect loudness normalization for all input stimuli in daily listening environments.
These issues certainly raise questions on the necessity of determining loudness growth functions in order to set a compression hearing aid properly. However, they should not discourage one from attempting to set compression parameters properly. Rather, they are raised as a reminder that the theoretical advantage of WDRC in loudness normalization may not be fully achievable with current hearing aids. Use of compression hearing aids with sufficient number of channels to cover all frequency regions, and compensation for the effective CR in real life will be necessary to achieve complete loudness normalization.
Reduction of Intensity Difference among Syllables
Speech sounds vary widely in intensity level even at normal vocalization (Pearsons et al, 1977). By applying the same gain to all speech components (vowels and consonants), the more intense vowels will become louder while the less intense consonants may still be inaudible. Furthermore, weaker speech sounds may be masked by the higher intensity sounds in a forward or backward manner (i.e., temporal masking; Festen and Plomp, 1983; Moore et al, 1985) which may result in decreased speech intelligibility.
Compression hearing aids with high gain and a low compression threshold (45 dB SPL) would ensure that the more intense vowel sounds receive less gain than the less intense consonant sounds. The result may be similar to a linear hearing aid with high frequency emphasis. This could reduce the intensity difference between the more intense vowels and the less intense consonants and thus increase the consonant-to-vowel ratio (Montgomery and Edge, 1988; Preves, 1991). In order that gain during one syllable is minimally affected by gain during preceding syllables, the release time must be short (e.g., 50 ms). This is important in order to recover from compression (of the more intense vowels) so that the weaker consonants can be amplified with more gain. However, the release time cannot be so short that any silent interval between syllables or within a syllable is amplified to produce unacceptable subjective perception (e.g., noisiness, breathiness, pumping). Various investigators have studied the effect of release time on speech intelligibility (e.g., Lynn and Carhart, 1963; Johansson, 1973; Ahren et al, 1977; Schweitzer and Causey, 1977; and Jerlvall and Lindblad, 1978). In general, release times between 30 ms to 100 ms were shown to have minimal deleterious effects on speech intelligibility.
Although syllabic compression may minimize the long-term intensity difference among syllables and can increase consonant-to-vowel ratios, such ability is not a sole property of compression hearing aid. Indeed, linear hearing aids which are fitted in a high-pass mode (i.e., more amplification to high frequency sounds than to low frequency sounds) can achieve the same outcome. The difference between a linear high frequency emphasis hearing aid and a WDRC hearing aid is that the linear hearing aid may result in distortion at moderately intense input levels (70 dB SPL to 80 dB SPL) whereas the WDRC may have less distortion at the same input level. At high input levels (i.e., greater than 90 dB SPL), WDRC is just as likely to introduce distortion as a linear hearing aid. Even so, it is questionable if the resulting distortion with linear amplification may be objectionable to the wearer. Horwitz et al (1991) compared syllable recognition and subjective preference among linear, high-pass, and “treble increase at low level” (or TILL) processing. No significant difference in syllabic recognition score was evidenced among the three methods of processing. However, there was a strong preference for linear processing.
Research data on the efficacy of WDRC have been mixed. Braida et al, (1979), based on a review of research data from 1952 to 1976, concluded that there is no conclusive evidence to suggest this type of compression is beneficial for persons with sensorineural hearing loss. Walker and Dillon (1982), based on a review of the literature up to that time, reported that there may be some “tentative support” for WDRC. Hickson (1994), based on a review of more recent research findings, reported more positively on the efficacy of such a circuit design, although the generalization of such findings may still be questionable.
There are a few recent studies to suggest that WDRC hearing aids may be superior to linear amplification. In general, the test conditions that were most likely to show a positive effect of WDRC over linear amplification included (1) testing in quiet; (2) stimulus presented at a low intensity level, and (3) fixed volume control setting. Dreschler (1989) compared consonant recognition between a compression hearing aid with short attack and release times (Ta = 5 ms, Tr = 55 ms) and a linear hearing aid with similar frequency response. The compression hearing aid improved the recognition of plosive sounds over that of the linear hearing aid when the stimuli were presented in quiet. In noise, no difference between the two hearing aids was noted. Tyler and Kuk (1989) also failed to find any significant improvement in consonant recognition score between a single channel syllabic compressor (CR = 2:1, release time = 36 ms) and its linear version.
Moore et al (1992) reported on the comparison between a two-channel WDRC hearing aid and the same hearing aid adjusted to amplify linearly. The hearing aids were adjusted to have the same frequency response but different gain characteristics at different input levels. The linear version was fitted with the fixed NAL-R gain; whereas the WDRC version was adjusted based on the results of loudness scaling using the Loudness Growth of Octave Band (LGOB) test (Pluvinage, 1989). Subjects were tested at different input levels (50 dB SPL, 65 dB SPL, and 80 dB SPL) in quiet and in noise. Subjects were not allowed to adjust volume on the hearing aids during testing. In quiet and at a low intensity input (50 dB SPL), speech recognition score was significantly higher in the WDRC mode than in the linear mode. However, at a higher input level and in the presence of noise, no significant difference was reported between the two modes of amplification.
The difference in performance between WDRC and linear amplification may be explained from the standpoint of audibility. Figure 17 compares the amount of gain prescribed for an impaired ear between a WDRC hearing aid (thin arrows) and a linear hearing aid (thick arrows). In order to restore “normal” loudness, the WDRC hearing aid supplies greater gain at lower input levels and less gain at higher input levels. As a linear hearing aid is fitted primarily to optimize performance at conversational level, the same amount of gain is applied regardless of input level. When these gain values are compared, one sees that both hearing aids provide similar gain at conversational level (65 dB SPL). However, the WDRC hearing aid supplies more gain at low input levels and less gain at high input levels than the linear hearing aid. If no volume adjustment is allowed, subjects will receive more gain from the WDRC hearing aid than from the linear hearing aid at low input level. More gain from a hearing aid would ensure greater chance for audibility when the input level is low, speech recognition score resulting from the use of a WDRC hearing aid will be predictably higher than that from the linear hearing aid. As the output SPL from both hearing aids (WDRC and linear) are similar at conversational level, similar speech recognition scores can be expected. Because less gain is available to a WDRC hearing aid than to a linear hearing aid at high input level, a wearer of such device may find loud sounds more bearable with WDRC. This may account for the increased comfort associated with the use of WDRC hearing aids in daily environments (e.g. Moore et al, 1992).
Figure 17.
Amount of gain (shown by the length of the arrows) provided by a WDRC (←) and a CL (←) circuit as illustrated on a loudness growth function.
Figure 17 also shows that a linear hearing aid can provide the same amount of gain as the WDRC hearing aid if the wearer can adjust the volume control setting. This may be one reason for the negative results in the Tyler and Kuk (1989) study where subjects were allowed to adjust the VC setting on their hearing aids when comparing compression and linear hearing aids. This suggests that the advantage of a WDRC hearing aid over a linear hearing aid at this time is possibly one of ensuring audibility for low intensity sounds in quiet and reducing gain for high intensity sounds without VC adjustment, and not necessarily one of enhancing signal-to-noise ratio or restoration of the normal loudness growth function. This advantage alone may be sufficient to warrant the purchase and use of WDRC hearing aids for some wearers. However, given that the main difficulty that hearing impaired listeners experience daily is that of poor speech understanding in noise, improving audibility and increasing comfort alone even without VC adjustment may not be sufficient to meet the communication needs of hearing impaired listeners. Every effort must be made to improve the signal-to-noise ratio of the listening environments also. Unfortunately, conclusive evidence to suggest that WDRC can achieve SNR improvement is scarce. Technologies like directional microphones and direct audio input must be employed to provide such benefits.
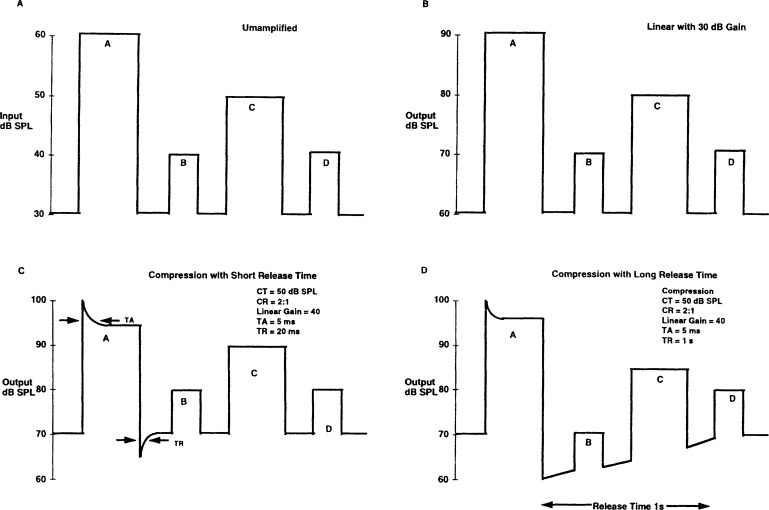
An important consideration that has often been overlooked when fitting a WDRC hearing aid is that this type of processing may alter the temporal and spectral structure of the input signal. By successfully altering the intensity relationship among the various segments of the input signal, one is also distorting its temporal envelope (Plomp, 1988; Van Tasell, 1993). Figure 18 is a simplified representation of the temporal envelope of an acoustic input marked by four bursts of energy at A, B, C, and D (Figure 18A). When the input is amplified linearly, the overall output level of the signal is increased. However, the intensity difference between A and B, between C and D, or that among A, B, C, and D remains the same (Figure 18B). In other words, the same temporal envelope is preserved at the output. Figure 18C shows the temporal envelope at the output of a WDRC hearing aid with short release time. In contrast to the observation in Figure 18B, the intensity difference between A and B, A and C, and A and D is reduced. More reduction in intensity difference would occur as the compression ratio is increased. Indeed, for a compression hearing aid with an infinite compression ratio, there may not be any intensity fluctuation in the temporal envelope of the output waveform. By the same token, a long release time can also vary the intensity relationship among A, B, C, and D, although in a slightly different way (Figure 18D).
Figure 18.
Illustration of how compression can affect the temporal intensity relationship among acoustic segments. (A) No amplification, (B) linear amplification, (C) compression with short release time, and (D) compression with long release time.
The above example shows that compression, depending on the release time used in its design, may alter the temporal relationship among acoustic signals in different ways. For some hearing aid wearers with good residual frequency resolution, this temporal alteration may not result in noticeable deleterious effect on speech intelligibility. However, for hearing aid wearers with poor frequency resolution, WDRC and its associated temporal alteration among speech segments, although ensuring audibility, may decrease the available cues for speech recognition (Van Tasell, 1993). This may be another reason why some studies evaluating the efficacy of WDRC hearing aids result in negative findings. Perhaps the benefits of this type of processing are masked by the negative effects of temporal distortion. Choice of this type of processing would require consideration of temporal and frequency resolution of the listener. Loudness scaling procedures are not designed to provide insights to these aspects of psychophysical processing of the hearing impaired listeners. Psychophysical studies like gap detection, tuning curves (from masking studies) are necessary to characterize such capabilities. In today's clinics, these studies are not conducted prior to any hearing aid evaluation because of their time involvement (a tuning curve for one frequency may take up to 2 hours to obtain). An efficient method to determine psychophysical ability may be needed to properly characterize the psychophysical ability of the hearing impaired listener. Such information may improve hearing aid fitting. Alternatively, the use of paired comparison technique may hold promise in determining the optimal output limiting approach (and associated compression settings) without elaborate measurement of psychophysical abilities. At this time, paired comparison has been applied mostly to the selection of frequency gain responses in linear hearing aids (exception: Neuman et al, 1994 applied this technique to examine compression ratios). Its application in the fitting of non-linear hearing aids would require further research and validation. An overview of this technique can be found in Kuk (1994).
Automatic Volume Control (AVC)
Rather than mapping the full range of speech into the hearing impaired listener's full residual auditory range, a compression hearing aid with automatic volume control is designed to map the full range of speech onto a restricted region within the residual dynamic range. An example may be the region where the most comfortable listening (MCL) level is reported. By so doing, a relatively constant output level is maintained despite fluctuations in input levels. The advantage of such manipulation is that all acoustic stimuli are presented at a constant level of maximum comfort (or maximum intelligibility). Additionally, because the output level is maintained at a comfortable level, the need to adjust VC is minimized. Such hearing aid has also been called an automatic gain control (AGC) hearing aid.
In order for an AVC compression hearing aid to achieve its objectives, it is designed with moderate compression threshold (60 dB SPL-65 dB SPL) so that low intensity sounds will not activate the compression hearing aid. A high compression ratio is used in order to keep the output level within a restricted range (greater than 5:1). One characteristic of this circuit is its long attack and release times. The attack time can be several hundred milliseconds and the release time can be several seconds. This suggests that the hearing aid remains in the compressed, reduced gain state most of the time (Walker and Dillon, 1982). This ensures that the temporal envelope of the acoustic signal is preserved while the long-term intensity range of the input signal is restricted to within a region of the individual's auditory area. Because of the long time constants, these hearing aids are also called slow-acting compression hearing aids.
Because the output SPL at high input is also reduced, an AVC hearing aid also minimizes loudness discomfort and reduces saturation-induced distortion at moderate to high input levels. While a compression limiting hearing aid typically compresses at high input level (exception: high gain compression limiter), both WDRC and AVC hearing aids are in the compressed state most of the time. The difference between WDRC and AVC is the relative frequency in which they go in and out of compression. A hearing aid with WDRC goes in and out of compression frequently in order to minimize intensity fluctuation. A hearing aid with AVC stays in compression longer (i.e., reduced gain state). This maintains the short-term intensity relations among speech segments while reducing the overall long-term intensity fluctuation in the output. This suggests that consonant-to-vowel ratio enhancement, which is achieved by minimizing intensity fluctuations in WDRC, may not be possible with AVC. Whereas the WDRC hearing aid matches the speech range (> 30 dB) to within the listener's full residual auditory range, an AVC hearing aid ensures that all input levels fall within a small region of the listener's auditory range (e.g., MCL). The long release time used in AVC would also argue that such hearing aid may not effectively compress all acoustic signals to the degree indicated by its nominal compression ratios.
Reduction for Long-term Intensity Difference
Despite the theoretical advantage of enhanced comfort, AVC circuits are not used in hearing aids frequently. Dillon (1988) speculated that the long time constants mean that excessive output level cannot be prevented at the start of impulsive signals. Additionally, a low intensity signal following an intense one may be inaudible with the long release time. This suggests that an AVC circuit may be acceptable to ensure overall comfort in situations where speech intelligibility is not of the major concern, and only in situations where extreme fluctuations in the signals (e.g., impulsive sounds followed by low intensity sounds) are not common.
Relatively few studies were conducted to examine the efficacy of AVC hearing aids. King and Martin (1984) compared the subjective preference between a linear hearing aid and an AVC hearing aid (CR – 5:1, CT = 65 dB SPL, Ta = 1 ms, Tr = > 90 ms). For speech materials presented in quiet and at input levels less than 65 dB SPL, no strong preference was seen for either type of processing. However, when speech was presented in noise, and at a high input level (85 dB SPL) in quiet, 16 of 17 subjects commented that the AVC hearing aid was clearer and more comfortable. Changes in compression ratio (20:1 vs. 3:1), or where the VC is placed in the compression hearing aid did not result in any difference in preference.
Peterson et al (1990) compared linear amplification with peak clipping and an AVC hearing aid with a CT at 60 dB SPL, a CR at 10:1, a Ta of 15 ms, and a Tr of 180 ms using the Nonsense Syllable Test. The AVC hearing aid yielded significantly higher syllable recognition scores in comparison to linear amplification when the test was conducted in quiet. On the other hand, better performance was seen with linear amplification when the test was conducted in noise.
Neuman et al (1994) evaluated subjective preferences for five compression ratios using an AVC hearing aid (CT = 65 dB SPL; Ta = 5 ms; Tr = 200 ms). The compression ratios were compared in a round robin format and included 1.5, 2.0, 3.0, 5.0, and 10.0:1. Twenty hearing impaired subjects listened to female discourse fixed at 85 dB SPL. The speech was processed by different compression ratios and the processed passages were presented in a pairwise manner. Subjects selected the sample that was more preferable. All comparisons were completed at the subject's MCL. Loudness was equalized for various speech segments (including linear). At a low intensity noise background (vent and apartment noise, about 50 dB SPL), seven to eight of the twenty subjects preferred linear amplification. The remaining subjects were equally divided in their preference among compression ratios. For the high intensity noise background (cafeteria noise, 71 dB SPL), 13 of the 20 subjects preferred the linear hearing aid. Of the remaining seven subjects, six preferred a compression threshold of 1.5:1, and the remaining subject preferred a compression ratio of 3:1. This suggests that when using subjective preference judgment, individuals are varied in their preference for compression in a quiet or low noise (less than 50 dB SPL) background. However, in a high intensity noise background, most of the subjects preferred processing with none or minimal compression. The preservation of the temporal envelope and intensity contrast in such condition (while maintaining the gain and output at MCL) may account for this finding.
It should be clear that the three types of compression hearing aids share the same objective—gain reduction with increasing input level. They differ in their settings of CT, CR, and release time. Given that, it may be meaningful to describe compression hearing aids by their compression settings and not simply by their names (i.e., compression limiting, WDRC, AVC). For example, a compression hearing aid with a wide range of adjustments can be easily adjusted to function like WDRC or compression limiting by varying its CT and CR. The choice of the compression parameters, rather than the name assigned to the type of compression, is most important when selecting a compression system. In addition, the ability to select different compression parameters may be useful to meet the different listening criteria in various listening situations.
It is reasonable to ask how different compression approaches can be used effectively to meet the needs of hearing impaired individuals. Despite the research effort in the past twenty years, a clear answer is not yet available. From that standpoint, it is gratifying to note that the Veterans Administration Medical Center (VAMC) and the National Institute on Deafness and other Communicative Disorders (NIDCD) are collaborating in a joint effort to examine the relative efficacy of three types of amplification strategies—linear with peak clipping, compression limiting, and wide dynamic range compression. In addition to a large subject base (360 subjects in eight geographic regions in the USA), the study examines both laboratory and real-life benefits of these devices using objective as well as subjective measures. Such data should provide a basis for selecting the type of hearing aid for a particular hearing impaired patient.
Table 1 summarizes the similarities and differences among the different modes of amplification as discussed in this section—their electroacoustic characteristics, their advantages, limitations, and applications. Obviously, this is simply a summary based on the interpretation of available report. New data, e.g., from the VA/NIDCD study, will no doubt alter the application of this summary.
Table 1:
Summary table comparing the compression charactenstics, advantages, limitations and applications of linear peak clipping (PC), compression limiting (CL), wide dynamic range compression (WDRC) and automatic volume control (AVC) hearing aids.
| Compression Characteristics | ||||
| PC | CL | WDRC | AVC | |
| a. CR | not applicable | high | low | intermediate to high |
| b. CT | not applicable | typically high | low | intermediate |
| c. Release Time | not applicable | intermediate | short | long |
| Advantages | ||||
| PC | CL | WDRC | AVC | |
| a. Limit Output | yes | yes | yes | yes |
| b. Saturation Distortion | yes | minimal | minimal | minimal |
| c. Loudness Normalization | no attempt | no attempt | attempt to normalize | no attempt |
| d. Need to Adjust VC for Soft & Loud Sounds | yes | yes | minimal | minimal |
| e. Effect of Lowering VC | output ☟, distortion ☟, maintain SSPL | output ☟, distortion ☟, maintain SSPL, CT ☝ (AGC-O onlv) | output ☟, distortion ☟, maintain CT, SSPL ☟ (AGC-I onlv) | output ☟, distortion ☟, maintain CT, SSPL ☟, (AGC-I onlv) |
| Limitations | ||||
| PC | CL | WDRC | AVC | |
| a. Output Level | sufficient even for profound loss | may be insufficient output for profound loss | may be insufficient output for severe loss | may be insufficient output for severe loss |
| b. Distortion | saturation-induced at moderate input level | temporal & spectral at high input | temporal & spectral at all input | temporal & spectral above moderate input |
| Applications | ||||
| PC | CL | WDRC | AVC | |
| a. Hearing Loss | all degrees, especially profound & precipitous or experienced PC users | all degrees, except profound | mild-to-moderate | moderate |
| b. Evaluative Criteria | intelligibility, quality (least comfort, least natural) most aversive & distortion | intelligibility, quality (some comfort) | intelligibility, quality, comfort, ‘normal’ loudness | intelligibility, quality, most comfort. |
| c. Optimal Listening Condition | low to moderate input, quiet | low to high input, quiet and noise | low to high input; quiet | low to high input, quiet |
| d. Non-Candidate | all except experienced PC users | none | poor frequency resolution | poor frequency resolution |
COMPONENT CONSIDERATION IN COMPRESSION CIRCUITS
Compression hearing aids are classified according to how frequently compression is invoked and the intended functions for compression. However, the placement of electronic components within the hearing aid may alter the effective use of compression. The placement of these components are based on thorough consideration by design engineers. It is worthwhile to understand how such design may affect the use of compression and the implications of such decisions. The effects of VC and filter placement within the hearing aid, and the issue of multiple channels will be considered in this section.
Volume Control (VC)
Placement of the VC in a hearing aid with compression affects the compression threshold and the SSPL90 of the hearing aid. Figure 19 shows two possible placement sites of the VC in relation to the feedback loop. If the VC is placed before the feedback loop, the SSPL90 from the hearing aid will be determined by the threshold level set at the feedback loop regardless of the VC position. In this situation, activation of the feedback loop is determined by the output voltage (or current) prior to the hearing aid receiver. Consequently, this type of compression is called output compression or AGC-O (Figure 19A). In this design, a fixed SSPL90 level is achieved regardless of VC setting. On the other hand, the level of the input signal would directly affect activation of the feedback loop if the VC is placed after it. Output SPL after the feedback loop can be further changed by the VC setting. This type of compression is called input compression or AGC-I (Figure 19B). In this type of circuit, the SSPL90 of the hearing aid is tied to the VC setting.
Figure 19.
Placement of volume control in a compression circuit: (A) AGC-O, and (B) AGC-I.
Figure 20 shows the I-O curves of an AGC-O and an AGC-I hearing aid as the VC setting is lowered in 10 dB steps from maximum (VC = 4) to minimum (VC = 1). Several observations are apparent. First, when the VC is set at maximum, the I-O curve of both the AGC-I and the AGC-O hearing aids reveal identical gain and SSPL90. However, as the VC is lowered, differences between these two hearing aids appear. The SSPL90 of the AGC-O hearing aid remains at 125 dB SPL, but the SSPL90 of the AGC-I hearing aid decreases systematically as the VC is lowered. On the other hand, the compression threshold of the AGC-O hearing aid increases from 60 dB SPL to 90 dB SPL as the VC is lowered; whereas the compression threshold of the AGC-I hearing aid remains at 60 dB SPL regardless of VC setting.
Figure 20.
Effect of volume control rotation on the input-output function of an (A) AGC-O hearing aid, and (B) AGC-I hearing aid.
Some may find it paradoxical that an increase in VC is associated with a decrease in compression threshold in an AGC-O hearing aid (or lowering the VC is associated with an increase in compression threshold). Lowering of compression threshold would mean that the input signal will be compressed at a lower level. At first glance, one may conclude that this could result in lower sound pressure level at the output. Figure 21 shows how these two actions are not antagonistic. This figure shows I-O curves at different VC settings on an AGC-O hearing aid. If the wearer uses the hearing aid at VC = 2 (CT = 90 dB SPL), turning the VC up to the next step (VC = 3) will increase the output by 10 dB whether the input is at 60 dB SPL or at 80 dB SPL. Consequently, despite lowering the compression threshold to 80 dB SPL with higher VC setting (VC = 3), no reduction in output sound pressure level results. On the other hand, raising the VC when the input level is high may not result in noticeable increase in output sound pressure level. This is seen at an input level of 90 dB SPL, where changing the VC from 2 to 3 leads to only a one dB increase in output SPL because the compression range (CR = 10:1) is reached. In this case, increasing the SSPL90 setting on the hearing aid is necessary to increase the output SPL.
Figure 21.
Effect of volume control rotation on the output of an AGC-O hearing aid: Increasing VC leads to an increase in output despite reducing the compression threshold except where saturation is reached.
The dependence of the SSPL90 on VC setting in an AGC-I hearing aid may be problematic. First, most manufacturers' specification reports SSPL90 of a hearing aid at the maximum VC setting. For a linear peak clipping hearing aid, or for a compression hearing aid with AGC-O, the clinician can easily read off such information from the specification and adjust the SSPL90 setting to below the loudness discomfort level (LDL) of the hearing aid wearer. No consideration needs to be made of the VC setting, since SSPL90 is independent of VC setting in such hearing aids. However, because the VC is tied to the SSPL90 in an AGC-I hearing aid, the clinician must also determine the VC setting where the wearer will use the hearing aid in order to set the SSPL90 properly. Adjusting the SSPL90 on an AGC-I hearing aid simply based on the specification sheet (which shows SSPL90 at full-on VC) will likely result in a lower SSPL90 in real-life use. Typically, hearing aid wearers are taught not to wear their hearing aids at full volume.
Another theoretical consideration is the issue of headroom (HR). Headroom is defined as the SPL difference between the output intensity level at which saturation or peak clipping occurs and the instantaneous output SPL. Typically, the intensity level at which saturation occurs is reflected by the magnitude of the SSPL90 setting on a hearing aid. (Exception: in a compression hearing aid, the saturation level may be higher than the SSPL90 level. However, for the sake of simplicity in this illustration, we will assume that the SSPL90 level is the same as the saturation level). Figure 22 shows the available headroom for an AGC-O (Figure 22A) and an AGC-I (Figure 22 B) hearing aid (both with the same CR of 2:1) when the VC is adjusted downward. Figure 22A shows that as the VC is turned down by 10 dB, the output sound pressure level of the AGC-O hearing aid decreases from 95 dB SPL to 85 dB SPL. If the hearing aid saturates at 105 dB SPL, lowering the VC will result in an increase in headroom from 10 dB (105–95) to 20 dB (105–85). In the AGC-I hearing aid, lowering the VC by 10 dB also lowers the output sound pressure level from 95 dB SPL to 85 dB SPL. However, the SSPL90 of the system is also lowered from 105 dB SPL to 95 dB SPL. In this case, lowering the VC to reduce gain also reduces the level at which saturation occurs. This suggests that the same amount of headroom is experienced regardless of VC setting (i.e., 105 – 95 = 10; and 95 – 85 = 10).
Figure 22.
Effect of volume control rotation on the available headroom (HR) in an (A) AGC-O and (B) AGC-I hearing aid.
Lowering or raising the VC on an AGC-O hearing aid may change the mode of operation of the compression circuit (i.e., linear or non-linear). This is illustrated in Figure 23. Let us assume that a hearing aid wearer uses a compression hearing aid (CR – 5:1; CT – 70 dB SPL) to listen to conversational speech (60 dB SPL to 70 dB SPL). When the gain is set at 40 dB, the output of the hearing aid will fluctuate between 100 dB SPL and 110 dB SPL (circles) for both AGC-I and AGC-O hearing aids. The 10 dB intensity fluctuation at the input (70 — 60 = 10) is preserved at the output (110 – 100 = 10). When the input level is raised by 10 dB to 70 dB SPL-80 dB SPL (as in loud speech), output SPL from both hearing aids is increased to 110 dB SPL-112 dB SPL (squares), or a 2 dB range. The absolute output intensity range has been reduced by 8 dB (10 −2 = 8). The difference between the AGC-I and the AGC-O hearing aids is revealed as the wearer turns the VC down to offset the increase in output sound pressure level. For the AGC-O hearing aid, lowering the VC by 10 dB lowers the output to the 100 dB SPL-110 dB SPL range (shown with X). The original intensity difference of 10 dB is restored. For the AGC-I hearing aid, lowering the VC to 2 lowers the output level to between 100 dB SPL and 102 dB SPL (shown with X). This range is 8 dB (110 – 102 = 8) less than the output range for the lower input because the intensity fluctuation is compressed to 2 dB from the original 10 dB. In this example, lowering the VC has the potential of restoring the intensity fluctuation in the input signal in an AGC-O hearing aid; but maintaining the reduced intensity range in an AGC-I hearing aid. If temporal and intensity fluctuations in the speech signal serve as cues for speech perception in the hearing impaired individuals (Plomp, 1988; Van Tasell, 1993); or form a basis for subjective impression of the acoustic input, an AGC-O hearing aid may be more preferable than an AGC-I hearing aid if the wearers use the VC effectively.
Figure 23.
Effect of volume control rotation on the absolute output intensity range in an (A) AGC-O and (B) AGC-I hearing aid. The symbols represent the output level for specific input and VC setting. “O” represents an input from 60 dB SPL to 70 dB SPL and VC = 3. “□” represents an input from 70 dB SPL to 80 dB SPL and VC = 3. “X” represents an input from 70 dB SPL to 80 dB SPL when the volume is turned down to VC = 2.
Along the same line, raising or lowering the VC may differentially affect the long-term signal-to-noise ratio (SNR) between the output of an AGC-O hearing aid and the output of an AGC-I hearing aid. However, it is important to point out that the instantaneous SNR at the output of a single channel AGC-O or AGC-I hearing aid remains the same as the input, because both speech and noise are affected at the same time. Figure 24 illustrates how the long-term SNR can be affected. Let us assume that a speech signal (70 dB SPL) that is 20 dB above the background noise (50 dB SPL) is presented to a compression hearing aid (CT = 70 dB SPL, CR – 5:1). At a VC = 3 (or 40 dB gain), the output from the hearing aid will have the noise at 90 dB SPL and the speech at 110 dB SPL (Figure 24A). The SNR at the input is seen at the output. If now both the noise and speech levels are increased by 10 dB (noise = 60 dB SPL, speech – 80 dB SPL), output from the hearing aid will range from 100 dB SPL to 112 dB SPL (Figure 24B). The SNR at the output is now reduced to 12 dB (112 – 100 – 12). The SNR at the output is 8 dB less (20 – 12 = 8) than that at the input. Typically, a hearing aid wearer lowers the VC setting when s/he is in a loud noise background. For the AGC-I hearing aid (Figure 24C), lowering the VC from 3 to 2 results in a lowered speech output (from 112 dB SPL to 102 dB SPL). The SNR, however, is unchanged from the higher VC setting because the compression threshold remains the same. On the other hand, Figure 24D shows that as the VC is lowered from 3 to 2 in an AGC-O hearing aid, the speech output of the hearing aid decreases from 112 dB SPL to 110 dB SPL but the noise output decreases from 100 dB SPL to 90 dB SPL. The SNR present at the input is now restored. Further lowering of the VC will not lead to additional enhancement of SNR.
Figure 24.
Effect of VC rotation on the long term signal-to-noise ratio. (A) Signal (S) and noise (N) not sufficient to reach the compression threshold. The SNR at the input is preserved. (B) Reduction in output SNR at higher input level. (C) SNR is maintained at a reduced value in an AGC-I hearing aid when the VC is lowered, and (D) SNR at the input is restored in an AGC-O hearing aid with VC reduction.
These differences suggest that while an AGC-I and an AGC-O hearing aid may behave similarly at one fixed VC setting, their behavior can be very different as the VC is changed. Clinically, it suggests that clinicians need to run I-O curves at two VC settings in order to fully appreciate the action of a compression hearing aid.
The decision to choose AGC-O or AGC-I has been one of design consideration. In some compression hearing aids, the VC can be placed either before or after the feedback loop. Walker and Dillon (1982) suggest the use of AGC-O for a compression limiting circuit and AGC-I for an AVC circuit. For WDRC circuit, either input or output compression circuits can be used. Fabry (1991) indicated that most syllabic compression or WDRC hearing aids use input compression. Commercially, some compression hearing aids also place the VC before and after the feedback loop. In such hearing aids, a simple prediction of the I-O characteristics can not be easily made.
Filters
Whereas the SSPL90 and compression threshold of a compression hearing aid vary with placement of the VC, the position of the filter within the compression hearing aid affects the output spectrum of the signal, and the frequency dependence of the compression threshold (Walker and Dillon, 1982). A filter element can be placed before, after, or within the feedback loop (Figure 25).
Figure 25.
Possible placement of filter within a compression hearing aid: (A) pre-filter, (B) post-filter, and (C) loop filter. “F” represents the filter.
Pre-filter
The filter is placed before the feedback loop of the compression hearing aid. Because the frequency response of the filter shapes the input signal prior to the feedback loop, the effective input level to activate compression is altered by the frequency response of the filter. Therefore, the frequency response at the output varies with the input level. For this reason, a compression hearing aid with a pre-filter is also called a frequency-dependent compression hearing aid.
Post-filter
The filter is placed after the feedback loop in a post-filter compression hearing aid. Because of this placement, the frequency response of the filter cannot affect the compressor. The frequency response at the output does not change with input levels. For this reason, a compression hearing aid using post-filter is also called a frequency-independent compression hearing aid.
Loop-filter
The filter is placed within the feedback loop in a loop-filter. Because the feedback loop is triggered only when the input signal exceeds the compression threshold, the effect of a loop filter is not active as long as the input level is below the compression threshold. Thus, if a high compression threshold is set, the frequency response at the output will not vary with the inputs at low to moderate input levels. The effect of frequency shaping will be evident at high input levels.
The effect of filter position on the output of a compression hearing aid may be better understood with the use of the same filter placed at different points of the compression hearing aid. Let us assume that a high-pass filter is used in a compression hearing aid that has a linear gain of 40 dB below 60 dB SPL and a static compression ratio of 2:1 from 60 dB SPL to 80 dB SPL. A fixed output is maintained above 80 dB SPL input. The filter response (Figure 26A) and the I-O curve at 3000 Hz (Figure 26B) used in the compression hearing aid are illustrated in Figure 26.
Figure 26.
(A) Frequency response of the filter and (B) I-O curve of the compression circuit used in the illustration.
Figure 27 (A–C) illustrates the effect of the three filter positions on the compression threshold. For the pre-filter (Figure 27A), because the low frequency signal is attenuated 20 dB relative to the high frequency signal (Figure 26A), a greater amount of low frequency signal is needed to reach the compression threshold than the high frequency signal. Consequently, the compression threshold is lower for the high frequency region than for the low frequency region. Because the filter is placed after the feedback loop in the post-filter (Figure 27B), the compression threshold is not affected by the filter response. Finally, the effect of placing the filter within the feedback loop (Figure 27C) is somewhat similar to the pre-filter condition once the compression threshold is reached. The feedback loop is not activated below 60 dB SPL, thus no frequency shaping is seen. Above the compression threshold (60 dB SPL, Figure 26B), a higher compression threshold is required for the low frequency than for the high frequency because of the filter response (i.e., more low frequency is needed to activate compression than high frequency).
Figure 27.
Effect of filter position on compression threshold: (A) pre-filter, (B) post-filter, and (C) loop-filter.
The effect of filter position on the I-O curves is summarized in Figure 28 (A–C). For the pre-filter (Figure 28A), two immediate observations are apparent. First, the output at the higher frequencies (3000 Hz) is greater than that at the lower frequencies (300 Hz). Second, CT decreases as input frequency increases. These observations can be explained with the frequency response and static compression characteristics of the filter (Figure 26). For example, the I-O curve at 3000 Hz should be identical to the one shown in Figure 26B, because this frequency is in the bandpass region of the filter. On the other hand, the I-O curve for 300 Hz is shifted by the amount of its attenuation (Figure 26A). This yields a CT at 80 dB SPL and a compression range from 80 dB SPL to 100 dB SPL. The I-O curve for the 1000 Hz signal is intermediate. For the post-filter position (Figure 28B), filter response has no effect on the compression threshold, but to shift the output level at each frequency by the amount of attenuation (Figure 26B). In this case, a 3000 Hz signal has the highest output, while the 300 Hz signal has the lowest output. For the loop-filter (Figure 28C), filter response changes the compression threshold and the SSPL90 at each frequency. In this case, the CT for the lower frequencies is shifted by the amount of attenuation (i.e., 20 dB, from 60 dB SPL to 80 dB SPL in Figure 26B). The shift in compression threshold suggests that the low frequency region will have a higher output than the high frequency region. In this case, a 20 dB difference is seen between 300 Hz and 3000 Hz.
Figure 28.
Effect of filter position on input-output curve: (A) pre-filter, (B) post-filter, and (C) loop-filter.
Figure 29 (A–C) summarizes the output frequency response curves as a function of input levels (50 dB SPL to 100 dB SPL) for the three filter positions. Because a high-pass filter is used, a high-pass response is seen in the pre- and post-filter positions (i.e., greater output as frequency increases). For the pre-filter position (Figure 29A), output increases linearly at 300 Hz (i.e., looking vertically) until 80 dB SPL is reached. However, at 3000 Hz, output increases by 5 dB for every 10 dB increase in level above 60 dB SPL. This is because the CT is reached earlier for the 3000 Hz than for the 300 Hz. In other words, a differential frequency effect is seen for the pre-filter position. The post-filter response (Figure 29B) shows a 5 dB increase in output for every 10 dB increase in input above 60 dB SPL. The same change is seen at all frequencies since the CT is the same for all frequencies (Figure 27B). For the loop filter position (Figure 29C), the frequency response shows a flat frequency response for input levels below 60 dB SPL. Above 70 dB SPL, a low-pass response is seen with less output for 3000 Hz than for 300 Hz as input level increases.
Figure 29.
Effect of filter position on frequency response curve at 300 Hz, 1000 Hz, and 3000 Hz: (A) pre-filter, (B) post-filter, and (C) loop-filter. The input levels are indicated as parameter.
Another way to examine the effect of filter position on frequency response is to re-plot the frequency response curves as frequency-gain curves (Figure 30, A–C). For the pre-filter position (Figure 30A), a high-pass response with maximum gain is seen for inputs below 60 dB SPL. As input level increases, gain at the high frequencies begins to initially decrease, until a flat gain curve results at an input of 100 dB SPL. For the post-filter position (Figure 30B), a high-pass response is once again seen. Unlike the pre-filter position, no differential frequency effect is seen as input level increases. For the loop-filter position (Figure 30C), there is a broad frequency gain response at the low-input level (i.e., 50 dB SPL). As input level increases, the frequency gain curve reveals gain reduction initially in the high frequencies and then extends to the lower frequencies. Unlike the pre-filter position where a flat response is seen at high input level (100 dB SPL), a low pass response is seen for the loop-filter position.
Figure 30.
Effect of filter position on frequency-gain curve at 300 Hz, 1000 Hz, and 3000 Hz: (A) pre-filter, (B) post-filter, and (C) loop-filter. The input levels are indicated as parameter.
These observations are based on theoretical considerations where headroom is not an issue and where only one filter response is considered. Use of other filter responses will change the output and gain response of the compression hearing aid. Additionally, these figures are generated with the use of sweep sinusoids for ease of comparison. The use of a complex signal like speech may not produce the “blooming” effect seen in the pre- and loop-filter positions with increases in input level. However, complex signals may produce different outcomes depending on the spectrum of the signal. Albeit these precautions, these observations reveal that although most specifications for compression hearing aids show a general I-O curve, the actual I-O performance of the hearing aid may be quite different depending on the response and position of the filter in the compression hearing aid. Because the output response varies with input level, compression hearing aids must be tested at multiple input levels in order that its dynamics can be more fully understood (Preves et al, 1989). The current ANSI standard (ANSI, 1992) recommends testing non-linear hearing aids with a broadband signal at multiple input levels.
Number of Channels
The discussion so far has focused on single channel compression hearing aids. A multiple channel compression hearing aid is one in which the input signal is split into more than one frequency channels. The output from each channel is acted upon by a feedback loop. Figure 31 (A and B) shows the schematics of a single channel compression hearing aid (A) and a three-channel compression hearing aid (B). In theory, a multiple channel compression hearing aid can be adjusted so that each channel assumes a different set of compression characteristics. In practice, most commercial analog or programmable multiple channel compression hearing aids are limited in their flexibility.
Figure 31.
Schematic illustration between a (A) single-channel compression hearing aid, and (B) three-channel compression hearing aid.
A rationale for a multiple-channel compression hearing aid is the flexibility that such hearing aid offers in matching the dynamic range (i.e., threshold to the tolerance limit) of the hearing impaired listener at multiple frequency regions. This would include ensuring audibility at more frequency regions (depending on the number of channels) and the application of differential gain to each frequency region to enhance its relative salience. Additionally, one may argue that by having multiple channels, the intense low frequency noise may be processed by a separate channel from the high frequency speech in order to prevent unnecessary compression of the higher frequencies. This may further ensure audibility of the high frequency sounds.
The potential advantage of a multiple-channel compression system may also be, interestingly, a major disadvantage. As previously pointed out, compression can result in distortion of the input signal. The long-term effect of compression is an increase in the level of the low intensity signal and a decrease in the level of the high intensity signals. This results in a reduction of the temporal and spectral contrasts among speech components. This may be problematic for hearing-impaired people with poor frequency resolution (Plomp, 1988). Indeed, for a compression system with an infinite number of channels and each with an infinitely high compression ratio, the output waveform will contain no “peaks and valleys”. This is because all intensity fluctuations will be “smoothed” by the compressor (Bustamante and Braida, 1987; Plomp, 1988; and Moore, 1991). For a single channel system, the possibility of complete “smoothing” is low because any one frequency in the input signal may trigger the compressor and lead to a decrease in overall level across all frequencies. Thus, the peak-to-valley ratio among speech components may still be preserved with the single channel compressor. In a multichannel compression system, independent compression and amplification at different frequency regions may restore audibility across all frequency regions. However, it may also introduce severe temporal distortion so that any cues that the hearing-impaired listeners rely on for speech perception may be lost. The optimal number of channels, the dependence of these channels, the compression characteristics of each channel, and the type of processing algorithm are important design parameters which must be carefully considered to ensure acceptable performance of a multiple channel compression system. As in programmable hearing aids, multiple-channel compression hearing aids differ. The fact that a compression hearing aid has multiple channels does not guarantee its performance over a single channel system. Differences among multichannel compression hearing aids will be an emerging topic of clinical interest in the future.
Hickson (1994) summarized the findings of twenty-one studies that examined the efficacy of multichannel compression hearing aids. Of the twenty-one studies, ten reported support for multiple channel compression, while the others were less supportive of its efficacy. The readers are urged to refer to Hickson (1994) for a summary. In addition to the studies cited by Hickson (1994), several recent publications may also shed light on the efficacy of multiple-channel compression.
Hohmann and Kollmeier (1995) evaluated a compression system with twenty-three independent compression channels (Ta = 5 ms, Tr = 50 ms) using normal hearing subjects. Compression ratios that were evaluated included 1.0, 2.0, 2.5, and 3.0:1. Three SNRs (−2, −6, and −8) were tested with a monosyllabic word list. At a poor SNR (−8), intelligibility decreased as the CR increased. At the high SNR (−2), compression had no significant effect on intelligibility but the sound quality was reportedly poorer.
Yund and Buckles (1995 a, b) compared the relative syllabic recognition score of linear hearing aid with flat frequency response; linear hearing aid with frequency shaping; four-channel wide dynamic range compression system and the same WDRC system with 6, 8, 12 and 16-channels of compression. Hearing impaired and normal hearing subjects were used. For the hearing impaired subjects, syllabic recognition improved 1% as the number of channels increased from 4 to 6, and improved 2% as the number of channels increased from 6 to 8 channels. Overall, syllable recognition improved 3–4% as the number of channels increased from 4 to 8. This difference was reported to be statistically significant. No further improvement was seen as the number of channels increased beyond eight. On the other hand, syllabic recognition score for the single-channel linear hearing aid was only 1% poorer than that of the eight-channel compression system. This finding is similar to Barfod's (1978) who reported that the speech recognition score for a linear single channel hearing aid was similar to that of the four-channel compression hearing aid. In addition, the performance of the four-channel system was better than the two-channel system. Of the sixteen hearing impaired subjects who were tested by Yund and Buckles (1995a), seven reported better performance with the eight-channel compression system, four reported better performance on the single-channel linear system and five subjects reported no difference between the systems. On the other hand, the normal hearing subjects reported a 4–5% decrease in intelligibility with the eight-channel compression system over the single-channel linear system.
In general, while multichannel compression hearing aids do exhibit theoretical advantages, research to date has not uniformly confirmed its superiority over single-channel compression system. Levitt (1993) also pointed out that the superiority of multichannel compression hearing aid over well-designed linear hearing aid has not been demonstrated. Indeed, some of the advantages argued for multichannel compression system (e.g., differential compression threshold) can easily be achieved with a properly designed single-channel compression hearing aid using pre-filtering or loop-filtering. At this point, a generally agreed advantage of multichannel compression hearing aid is its ability to ensure audibility at more frequency regions (depending on the number of filters and filter characteristics). Improvement in speech intelligibility, or that of enhancing signal-to-noise ratio, which is desirable for hearing impaired listeners, has not been reported as an undisputed advantage of multichannel compression hearing aid. Better processing strategies are needed in order to improve speech intelligibility in noise. In addition, the possibility of learning effect on evaluating the efficacy of multiple-channel compression system cannot be overlooked (e.g., Yund and Buckles, 1995c).
CONCLUDING REMARKS
A logical question to ask, given what has been discussed, is the accepted benefit of compression hearing aids. One can easily understand the benefit if one remembers that compression is simply a mechanism to control gain of an amplification device so that the output of the device does not increase as rapidly as the input. One immediate benefit of this action is the prevention of sounds from being uncomfortably loud or from reaching saturation to cause distortion. This view would suggest that compression is not a way of improving speech intelligibility unless speech intelligibility has been degraded by distortion, or that audibility has not been achieved with conventional hearing aid fitting. Speech intelligibility may be enhanced but possibly as a secondary outcome to increase comfort or decrease distortion. This is true even when “normal” loudness growth is not completely achieved. Sammeth and Ochs (1991) also concluded that the advantages of compression or adaptive high-pass response hearing aids are the reduction of distortion and improvement in overall comfort. The enhancement of SNR, a desired goal to achieve for people with hearing loss, may not be achievable with this processing.
On the other hand, it is important to recognize that there are differences among the various forms of output limiting approaches. Linear amplification with peak clipping is the simplest form of output limiting approach, while retaining the gain provided by the hearing aid. Although the associated distortion products may decrease intelligibility for some hearing aid users, not all wearers may be negatively affected by distortion. Indeed, some hearing aid wearers who are longtime linear hearing aid users may be satisfied only with such a hearing aid. Linear amplification with compression limiting maintains linearity of the hearing aid until the output level approaches saturation. It is perhaps the only form of limiting approach that minimizes temporal, spectral, and saturation-induced distortion at low to moderate input levels. Individuals whose speech intelligibility can be easily affected by any distortion in the input signal should consider this form of output limiting option. Syllabic or wide dynamic range compression, when fitted properly, allows audibility for soft sounds and less gain for sounds above conversational level without volume control adjustment. This ensures consistent intelligibility over a wider range of input intensities in quiet and provides listening comfort over a wide range of input. On the other hand, this type of compression is associated with temporal and spectral distortion even at low and moderate input levels. Together with the reduced output SPL, this form of compression may be inappropriate for those (1) who have difficulties with frequency resolution, (2) who are sensitive to temporal cues for speech reception and (3) who require high output SPL from a hearing aid. Automatic volume control hearing aid ensures that a wide range of stimulus intensities can be heard at a restricted region (e.g., MCL) of the user's residual dynamic range. Additionally, it maintains the relative temporal relationship among the speech segments. This would ensure comfort in hearing aid use. The readers are referred to Table 1 for review.
The relative merit of each output limiting option suggests that no one option is ideal for all listening situations and for all hearing aid wearers. One must guard against the temptation of assigning one form of output limiting option exclusively for all hearing impaired listeners simply based on the degree of hearing loss and dynamic range information. These two indices do not reflect the psychophysical limitation of the impaired ear. Furthermore, other factors like the cognitive level, physical limitation and preference of the hearing aid wearer must also be considered in the hearing aid evaluation process. Such factors would also affect the choice of output limiting option for a hearing aid wearer. The availability of different output limiting options and the choice of different compression parameters on some programmable hearing aid allow the possibilities for a better match between hearing aid characteristics and individual needs for various acoustic environments. Perhaps such matching can further improve the hearing aid wearers' satisfaction with their hearing aids.
REFERENCES
- Ahren T, Arlinger S, Holmgren S, Jerlvall L, Johansson B, Lindblad A, Persson L, Petterson A, Sjogren H. (1977). Automatic Gain Control in Hearing Aids: The Influence of Different Attack and Release Times on Speech Intelligibility for Hearing Impaired with Recruitment (Report TA 84). Stockholm: Karolinska Institute [Google Scholar]
- Allen J, Jeng P. (1990). Loudness growth in 1/2 octave bands (LGOB): a procedure for the assessment of loudness. J Acoust Soc Amer 88: 745–753 [DOI] [PubMed] [Google Scholar]
- American National Standards Institute. (1987). Specification of Hearing Aid Characteristics. ANSI S3.22–1987. American National Standards Institute, New York [Google Scholar]
- American National Standards Institute. (1992). Testing Hearing Aids with a Broadband Noise Signal. ANSI S3.42–1992.
- Baechler H. (1995). Unpublished data.
- Barfod J. (1978). Multichannel compression hearing aids: Experiments and consideration on clinical applicability. Scand Audiol (suppl 6): 315–339 [PubMed]
- Blegvad B. (1974). Clinical evaluation of behind-the-ear hearing aids with compression amplification. Scand Audiol 3: 57–60 [Google Scholar]
- Blesser B. (1969). Audio dynamic range compression for minimum perceived distortion. IEEE Trans Audio Electroacoustics 17: 78–84 [Google Scholar]
- Braida L, Durlach N, Lippman R, Hicks B, Rabinowitz W, Reed C. (1979). Hearing aids—A review of past research on linear amplification, amplitude compression, and frequency lowering. ASHA Monograph No. 19, Rockville, MD: [PubMed] [Google Scholar]
- Brownell W, Bader C, Bertrand D, Ribaauplene Y. (1985). Evoked mechanical responses of isolated cochlear outer hair cells. Science 227: 194–196 [DOI] [PubMed] [Google Scholar]
- Bustamante D, Braida L. (1987). Multiband compression limiting for hearing-impaired listeners. J Rehab Res Dev 24 (4): 149–160 [PubMed] [Google Scholar]
- Cornelisse L, Gagne J, Seewald R. (1991). Ear level recordings of the long term average spectrum of speech. Ear Hear 12: 47–54 [DOI] [PubMed] [Google Scholar]
- Cornelisse L, Seewald R, Jamieson D. (1995). The input/output formula: A theoretical approach to the fitting of personal amplification devices. J Acoust Soc Amer 97 (3): 1854–1864 [DOI] [PubMed] [Google Scholar]
- Davis H, Stevens S, Nichols R, Hudgins C, Peterson G, Marquis R, Ross D. (1947). Hearing Aids—An Experimental Study of Design Objectives. Cambridge, MA: Harvard University Press [Google Scholar]
- Dawson P, Dillon H, Battaglia J. (1991). Output limiting compression for the severe-profoundly deaf. Austral J Audiol 13 (1): 1–12 [Google Scholar]
- Dillon H. (1988). Compression in hearing aids. In: Sandlin R. (ed) Handbook of Hearing Aid Amplification, vol. I, Theoretical and Technical Considerations. College-Hill Press [Google Scholar]
- Dirks D, Morgan D, Dubno J. (1982). A procedure for quantifying the effects of noise on speech recognition. J Speech Hear Dis 47: 114–123 [DOI] [PubMed] [Google Scholar]
- Dreschler W. (1989). Phoneme perception via hearing aids with and without compression and the role of temporal resolution. Audiol 28: 49–60 [DOI] [PubMed] [Google Scholar]
- Fabry D. (1991). Hearing aid compression. Amer J Audiol 1 (1): 11–13 [DOI] [PubMed] [Google Scholar]
- Festen J, Plomp R. (1983). Relations between auditory functions in impaired hearing. J Acoust Soc Amer 73: 652–662 [DOI] [PubMed] [Google Scholar]
- Hawkins D, Naidoo S. (1993). Comparison of sound quality and clarity with asymmetrical peak clipping and output limiting compression. J Amer Acad Audiol 4: 221–228 [PubMed] [Google Scholar]
- Hickson L. (1994). Compression amplification in hearing aids. Amer J Audiol 3: 51–65 [DOI] [PubMed] [Google Scholar]
- Hohmann V, Kollmeier B. (1995). The effect of multichannel dynamic compression on speech intelligibility. J Acoust Soc Amer 97: 1191–1195 [DOI] [PubMed] [Google Scholar]
- Horwitz A, Turner C, Fabry D. (1991). Effects of different frequency response strategies upon recognition and preference for audible speech stimuli. J Speech Hear Res 34: 1185–1196 [DOI] [PubMed] [Google Scholar]
- Hudgins C, Marquis R, Nichols R, Peterson G, Ross D. (1948). The comparative performance of an experimental hearing aid and two commercial instruments. J Acoust Soc Amer 20: 241–258 [Google Scholar]
- IHAFF, Independent Hearing Aid Fitting Forum. (1994). The unveiling of a comprehensive hearing aid fitting protocol for the 21st century. Presented at the Jackson Hole Rendezvous, Jackson Hole, WY.
- Ingelstam R, Johansson B, Petterson A, Sjogren H. (1971). The Effect of Non-Linear Amplitude Distortion, an Investigation by Variation of the Quadratic and Cubic Components. (Report TA 64). Stockholm: Karolinska Institute [Google Scholar]
- Jerlvall L, Lindblad A. (1978). The influence of attack and release time on speech intelligibility. A study of the effects of AGC on normal hearing and hearing impaired subjects. Scand Audiol (suppl 6): 341–353 [PubMed]
- Johansson B. (1973). The hearing aid as a technical audiological problem. Scand Audiol (Suppl 3): 55–76
- Killion M. (1994). Fig6.exe software: Hearing aid fitting targets for 40, 65 & 95 dB SPL inputs (version 1.01D). Etymotic Research, Elk Grove Village, IL [Google Scholar]
- Killion M. (1995). Talking hair cells: what they have to say about hearing aids. In Berlin C. (ed) Hair Cells and Hearing Aids. Singular Press, San Diego [Google Scholar]
- King A, Martin M. (1984). Is AGC beneficial in hearing aids? Bri J Audiol 18: 31–38 [DOI] [PubMed] [Google Scholar]
- Kuk F. (1994) Use of paired comparison in hearing aid fitting. In: Valente M. (ed) Strategies for Selecting and Verifying Hearing Aid Fittings. Thieme Medical Publishers, NY, p. 108–135 [Google Scholar]
- Kuk F, Lau C. (1995). Criteria considerations in subjective rating tasks. Paper presented at Third International Hearing Aid Conference in Iowa City, IA, 1995
- Levitt H. (1993). Future directions in hearing aid research. J Speech-Lang Path & Audiol 1: 107–124 [Google Scholar]
- Lynn G, Carhart R. (1963). Influence of attack and release in compression amplification on understanding of speech by hypoacusics. J Speech Hear Dis 28: 124–140 [DOI] [PubMed] [Google Scholar]
- Macrae J. (1994). Prediction of asymptotic threshold shift caused by hearing aid use. J Speech Hear Res 37: 1450–1458 [DOI] [PubMed] [Google Scholar]
- Montgomery A, Edge R. (1988). Evaluation of two speech enhancement techniques to improve intelligibility for hearing impaired adults. J Speech Hear Res 31: 386–393 [DOI] [PubMed] [Google Scholar]
- Moore B. (1986). Frequency Selectivity in Hearing. London: Academy Press [Google Scholar]
- Moore B. (1990). How much do we gain by gain control in hearing aids? Acta Otolaryng (supp 469): 250–256 [PubMed]
- Moore B. (1991). Characterization and simulation of impaired hearing: Implications for hearing aid design. Ear Hear 12: 154S–161S [DOI] [PubMed] [Google Scholar]
- Moore B, Laurence R, Wright D. (1985). Improvements in speech intelligibility in quiet and in noise produced by two-channel compression hearing aids. Bri J Audiol 19: 175–187 [DOI] [PubMed] [Google Scholar]
- Moore B, Glasberg B. (1988). A comparison of four methods of implementing automatic gain control (AGC) in hearing aids. Bri J Audiol 22: 93–104 [DOI] [PubMed] [Google Scholar]
- Moore B, Glasberg B, Stone M. (1991). Optimization of a slow-acting automatic gain control system for use in hearing aids. Bri J Audiol 25: 171–182 [DOI] [PubMed] [Google Scholar]
- Moore B, Johnson J, Clark T, Pluvinage V. (1992). Evaluation of a dual channel full dynamic range compression system for people with sensorineural hearing loss. Ear Hear 13: 349–370 [DOI] [PubMed] [Google Scholar]
- Nabelek I. (1983). Performance of hearing-impaired listeners under various types of amplitude compression. J Acoust Soc Amer 74: 776–791 [DOI] [PubMed] [Google Scholar]
- Neuman A, Bakke M, Hellman S, Levitt H. (1994). Effect of compression ratio in a slow-acting compression hearing aid: paired comparison judgments of quality. J Acoust Soc Amer 96 (3): 1471–1478 [DOI] [PubMed] [Google Scholar]
- Norton S. (1992). Cochlear function and otoacoustic emissions. Seminars in Hearing 13: 1–14 [Google Scholar]
- Pearsons K, Bennett R, Fidell S. (1977). Speech Levels in Various Noise Environments. EPA report 600/1–77–025. Washington, D.C [Google Scholar]
- Peterson M, Feeney P, Yantis P. (1990). The effect of automatic gain control in hearing-impaired listeners with different dynamic ranges. Ear Hear 11: 185–194 [DOI] [PubMed] [Google Scholar]
- Plomp R. (1988). The negative effect of amplitude compression in multichannel hearing aids in the light of the modulation-transfer function. J Acoust Soc Amer 83: 2322–2327 [DOI] [PubMed] [Google Scholar]
- Pluvinage V. (1989). Clinical measurement of loudness growth. Hear Instrum 39 (4): 19–22 [Google Scholar]
- Preves D. (1991). Output limiting and speech enhancement. In: Studebaker G, Bess F, Beck L. (eds), The Vanderbilt Hearing Aid Report II. Parton, MD: York Press, 35–51 [Google Scholar]
- Preves D, Beck L, Burnett E, Teder H. (1989). Input stimuli for obtaining frequency responses of automatic gain control hearing aids. J Speech Hear Res 32: 189–194 [DOI] [PubMed] [Google Scholar]
- Sammeth C, Ochs M. (1991). A review of current “noise reduction” hearing aids: A rationale, assumptions, and efficacy. Ear Hear 12: 116S–124S [DOI] [PubMed] [Google Scholar]
- Schweitzer H, Causey G. (1977). The relative importance of recovery time in compression hearing aids. Audiol 16: 61–72 [PubMed] [Google Scholar]
- Stone M, Moore B, (1992). Syllabic compression: effective compression ratios for signals modulated at different rates. Bri J Audiol 26: 351–161 [DOI] [PubMed] [Google Scholar]
- Sung R, Sung G. (1982). Compression amplification: its effect on speech intelligibility in noise. Hear Aid J 35 (11): 20–24 [Google Scholar]
- Tyler R, Kuk F. (1989). The effects of “noise suppression” hearing aids on consonant recognition in speech babble and low frequency noise. Ear Hear 10 (4): 243–249 [DOI] [PubMed] [Google Scholar]
- Van Tasell D. (1993). Hearing loss, speech, and hearing aids. J Speech Hear Res 36: 228–244 [DOI] [PubMed] [Google Scholar]
- Viemeister N. (1979). Temporal modulation transfer function based on modulation thresholds. J Acoust Soc Amer 66: 1364–1380 [DOI] [PubMed] [Google Scholar]
- Walker G, Dillon H. (1982). Compression in Hearing Aids: An Analysis, a Review, and Some Recommendations (report No. 90). Canberra, Australia: Australian Government Publishing Service [Google Scholar]
- Yund E, Buckles K. (1995a). Multichannel compression hearing aids: Effect of number of channels on speech discrimination in noise. J Acoust Soc Amer 97: 1206–1223 [DOI] [PubMed] [Google Scholar]
- Yund E, Buckles K. (1995b). Enhanced speech perception at low signal-to-noise ratios with multichannel compression hearing aids. J Acoust Soc Amer 97: 1224–1240 [DOI] [PubMed] [Google Scholar]
- Yund E, Buckles K. (1995c). Discrimination of multichannel-compressed speech in noise: long term learning in hearing impaired subjects. Ear Hear 16: 417–427 [DOI] [PubMed] [Google Scholar]