Abstract
To estimate how the Affordable Care Act's Medicaid expansions will affect demand for services, we measured ambulatory care utilization among adult patients who gained insurance during Oregon's 2008 Medicaid expansion. Using electronic health record data from 67 community health centers, we assessed pre- and postcoverage utilization among patients who gained insurance, compared with patients continuously insured or uninsured. In comparisons of the pre- and postcoverage periods, mean annual encounters among persons who gained insurance increased 22% to 35%, but declined in the comparison groups. These findings suggest that providers should expect a significant increase in demand among patients who gain Medicaid coverage through the Affordable Care Act.
Keywords: Affordable Care Act, ambulatory care utilization, insurance, Medicaid
MILLIONS OF Americans will receive new public health insurance coverage through the Affordable Care Act (ACA). Health insurance expansions will particularly impact patients who receive care in community health centers (CHCs) and other “safety net” settings. In 2011, CHCs provided primary care to more than 20 million patients, many of whom will likely benefit from new opportunities to gain health insurance under the ACA (Morgan, 2012; National Association of Community Health Centers, 2013; The White House, 2012). Although CHCs provide care regardless of patients' coverage (Hawkins & Groves, 2011), insurance status still influences care-seeking behaviors and service receipt in these settings. Uninsured persons are often less likely to receive recommended care—even if their health status indicates a heightened need for services (Gold et al., 2012; Hicks et al., 2006; Shi & Stevens, 2007; Zhang et al., 2009). Thus, it is predicted that CHCs and other primary care providers who accept Medicaid will experience increased demand when the ACA is fully enacted. There is a need to better understand how newly insured patients might utilize care subsequent to a Medicaid expansion, to help providers serving Medicaid populations anticipate ACA-related changes in demand (Sommers et al., 2013).
Policy-driven insurance expansions have been studied in the past to gain insight into how care-seeking behaviors change when a previously uninsured population receives coverage (Buchmueller et al., 2005; Decker et al., 2012; McWilliams et al., 2007; Polsky, 2011). For example, after states expanded children's coverage through the Children's Health Insurance Program, pediatric primary care utilization increased 9% to 39% (Davidoff et al., 2005; Duderstadt et al., 2006; Eisert & Gabow, 2002; Kempe et al., 2005; Kenney, 2007; Szilagyi et al., 2004). After Massachusetts' 2006 reforms, utilization increased among the newly insured (Ku, Jones, Shin, Byrne, & Long, 2011; Long & Stockley, 2011; Miller, 2012); Massachusetts' CHCs reported a 31% increase in the number of patients served between 2005 and 2009 (Ku, Jones, Shin, Byrne, & Long, 2011). However, most previous studies of postexpansion utilization used self-reported data, which is subject to biases, or claims data, which precludes comparisons with the uninsured (Buchmueller et al., 2005; Davidoff et al., 2005; Decker et al., 2012; Duderstadt et al., 2006; Finkelstein et al., 2012; Freeman et al., 2008; Hofer et al., 2011; Kempe et al., 2005; Kenney, 2007; Ku, Jones, Shin, Byrne, & Long, 2011; Long & Stockley, 2011; McWilliams et al., 2007; Miller, 2012; Szilagyi et al., 2004).
In 2008, the Oregon Health Plan expanded Medicaid coverage to approximately 10 000 previously uninsured nonelderly adults earning less than 100% of the Federal Poverty Level (FPL) (Allen et al., 2010; Baicker et al., 2013; Baicker & Finkelstein, 2011; Finkelstein et al., 2012). We used CHCs' electronic health record (EHR) data to assess utilization patterns among CHC patients in Oregon who obtained Medicaid coverage during the time of this Medicaid expansion. To estimate how demand may change among patients seeking ambulatory services after the ACA Medicaid expansions, we measured (i) utilization of CHC services among adult CHC patients who gained health insurance coverage in 2008, as documented in the EHR; (ii) how those who gained insurance utilized care compared with persons with no coverage changes (those who remained continuously insured or uninsured); and (iii) the timing of postcoverage CHC services utilization among those who gained insurance.
METHODS
Data sources
The OCHIN community health information network, a nonprofit organization, serves more than 300 CHCs in 14 states; member clinics share a single, linked, fully integrated EHR. Patients' insurance coverage status was identified in EHR data from 67 Oregon clinics that had the OCHIN EHR by July 2006; we augmented the EHR data through linkage to Medicaid coverage data. We extracted all other patient-level data from the EHR, including demographic data collected at clinic visits.
Study population
We identified 28 508 persons meeting the following criteria: aged 19 to 64 years throughout the study period; no record of insurance other than Medicaid in 2007 to 2009; 1 or more primary care visit(s) to any OCHIN CHC in Oregon before 2008, plus 1 or more visit(s) between their coverage “start date” (defined below) and December 31, 2011, to identify “established” clinic patients and ensure a minimum of continuity; and alive at the study end. We also excluded women who were pregnant at any point during the study period, as pregnancy incurs changes in both eligibility for public coverage and utilization.
Insurance group definitions
Our “cases” were persons who were continuously uninsured for 1 or more years before gaining Medicaid coverage in 2008 (precoverage) and then continuously insured for 1 or more years from the coverage start date (postcoverage) (n = 1217). We sought to compare this group with persons who had continuous Medicaid coverage, and also with persons who were continuously uninsured, in analogous time periods. To do so, all comparison group members were randomly assigned a 2008 “start date” on the basis of the distribution of Medicaid coverage start dates among those who gained insurance. (For example, 10% of those in the group who gained insurance had an actual Medicaid start date of March 11, 2008, so that start date was randomly assigned to 10% of persons in each comparison group.) The “continuously uninsured” had no coverage for 1 or more years before and 1 or more years after their assigned start date (n = 20 964); the “continuously insured” had Medicaid coverage for 1 or more years pre- and 1 or more years post–start date (n = 6327).
Utilization measurement
For the years pre- and post–start date, we measured each group's unadjusted annual utilization of (1) in-person primary care visits, excluding dental; (2) mental and behavioral health encounters; (3) all billed encounters, including those in (1) and (2); and (4) services received at any encounter, identified using standard procedure codes. Services were further stratified into labs, immunizations and injections, imaging, and referrals.
Analyses
First we used chi-square and t test analyses to conduct between-group comparisons of the study groups' demographic characteristics. Then we assessed within-group pre- versus post–start date changes in the utilization measures—the absolute change within each group—using paired t test statistics. Next we conducted adjusted comparisons of pre- and postutilization rates, expressed as rate ratios, obtained using generalized mixed models with a Poisson link that adjusted for age at coverage start date, gender, race/ethnicity, household income as percentage of FPL averaged across the study period, and the number of chronic conditions at the coverage start date. If a patient had missing FPL data, it was imputed as the average from other encounters outside of the study period, when available. The baseline count of chronic conditions was calculated using the Johns Hopkins Advanced Clinical Groups (ACG) System using diagnosis data in the EHR record in the 12 months before the start date (The Johns Hopkins ACG® System, 2011). Patients' primary clinic was entered as a random effect to account for correlation within clinics. Last, we compared pre- and postcoverage utilization patterns over time between the study groups by estimating adjusted monthly encounter rates (utilization measure 3) and 95% confidence intervals, using a Poisson mixed-effects regression model adjusted for patient and clinic characteristics as described previously.
This study was reviewed and approved by the Oregon Health & Science University institutional review board.
RESULTS
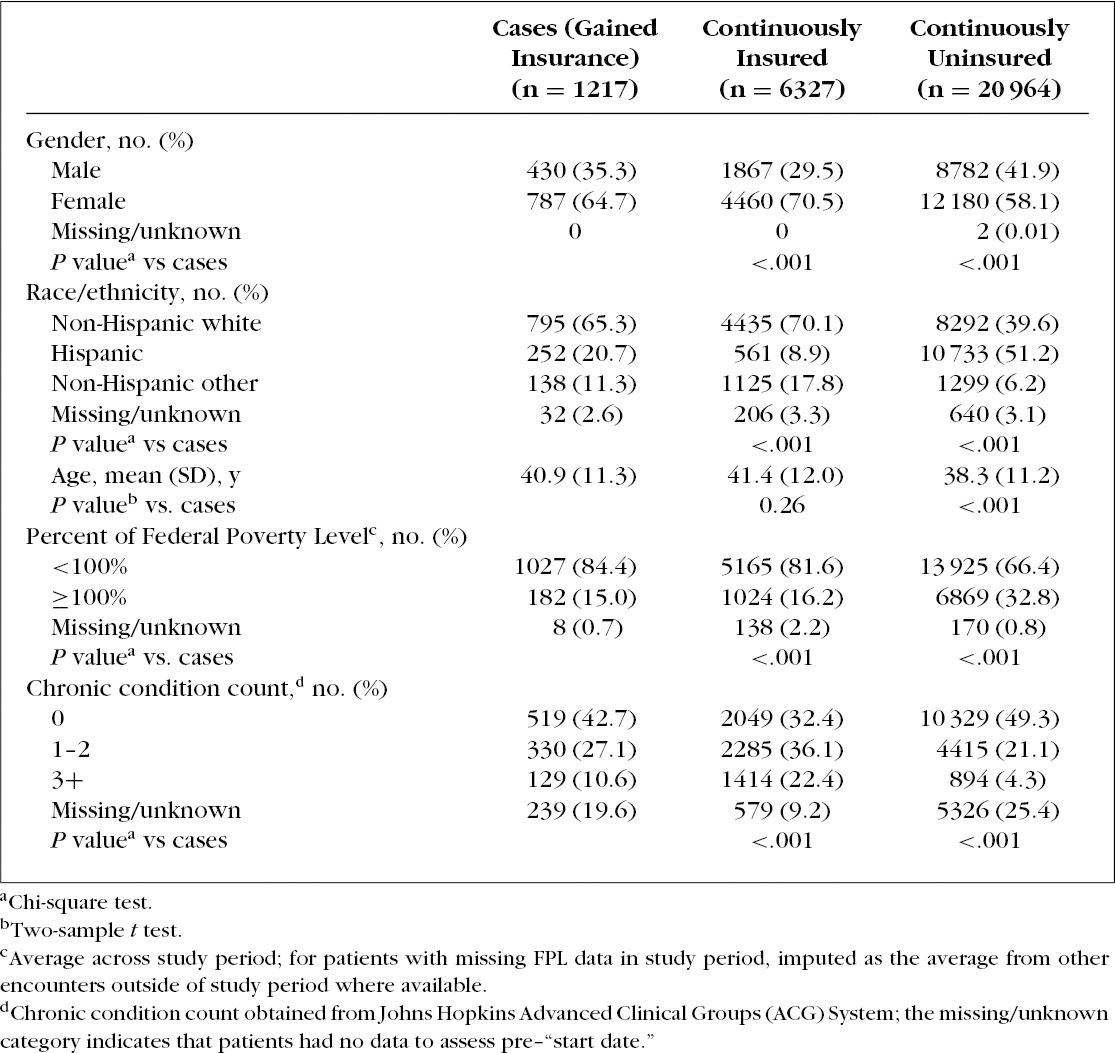
Persons who gained insurance—the study cases—differed significantly from comparison groups on gender, race/ethnicity, age (different from the continuously uninsured only), household income as percentage of FPL, and the number of chronic conditions at the coverage start date (Table 1). Notably, the cases had lower rates of chronic diseases at baseline when compared to the continuously insured, but higher rates than the continuously uninsured.
Table 1. Demographic Characteristics of Study Groups as of Coverage Start Date.
Within-group comparisons of CHC encounter and service utilization in the years before and after the coverage start date are shown in Table 2. Persons with continuous coverage had the highest overall utilization, and the continuously uninsured had the lowest. Among persons who gained insurance, the precoverage mean of 4.5 encounters rose to 6.1 in the postcoverage period, a relative increase of more than 35%; their precoverage mean of 3.8 primary care visits increased to 4.6, a relative increase of 22%. These metrics decreased for both the continuously insured and continuously uninsured comparison groups. Mean number of mental/behavioral health encounters increased in all groups, although only minimally among the continuously uninsured. Of persons who gained insurance, 19% had no primary care visit in the precoverage year, decreasing to 7% in the postcoverage year. In the comparison groups, this percentage increased (data not shown). Mean number of services ordered or received doubled among those who gained insurance; this relative change was considerably smaller in the other insurance groups.
Table 2. Within-group Comparisons of CHC Encounters and Services in the Years Pre- and Postcoverage Start Date.
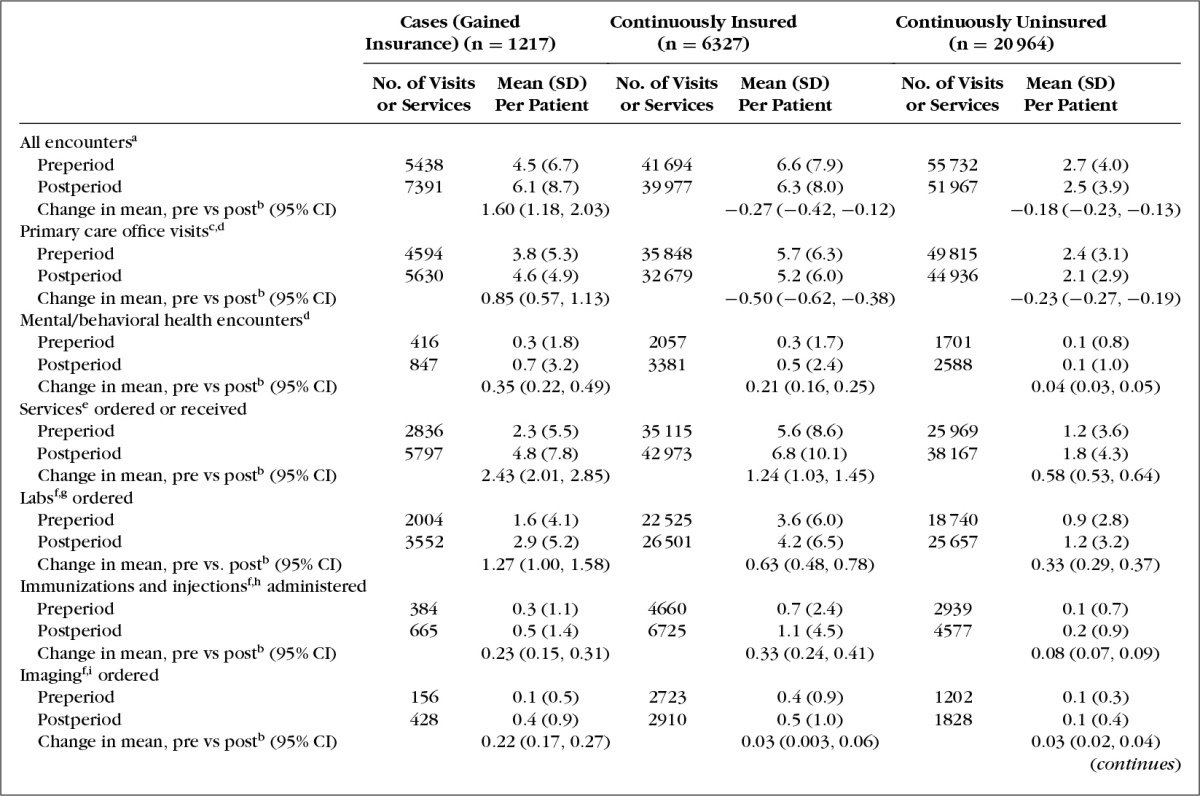
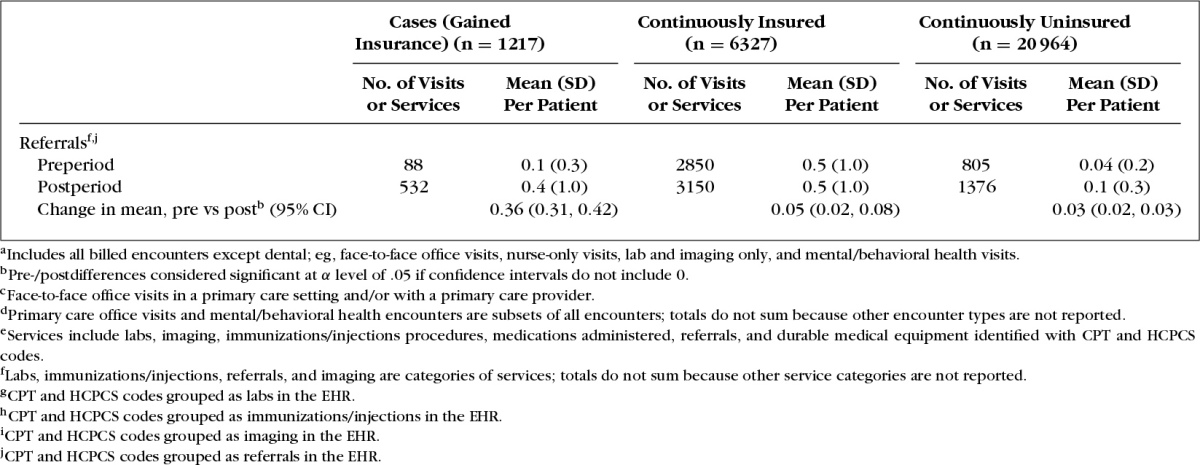
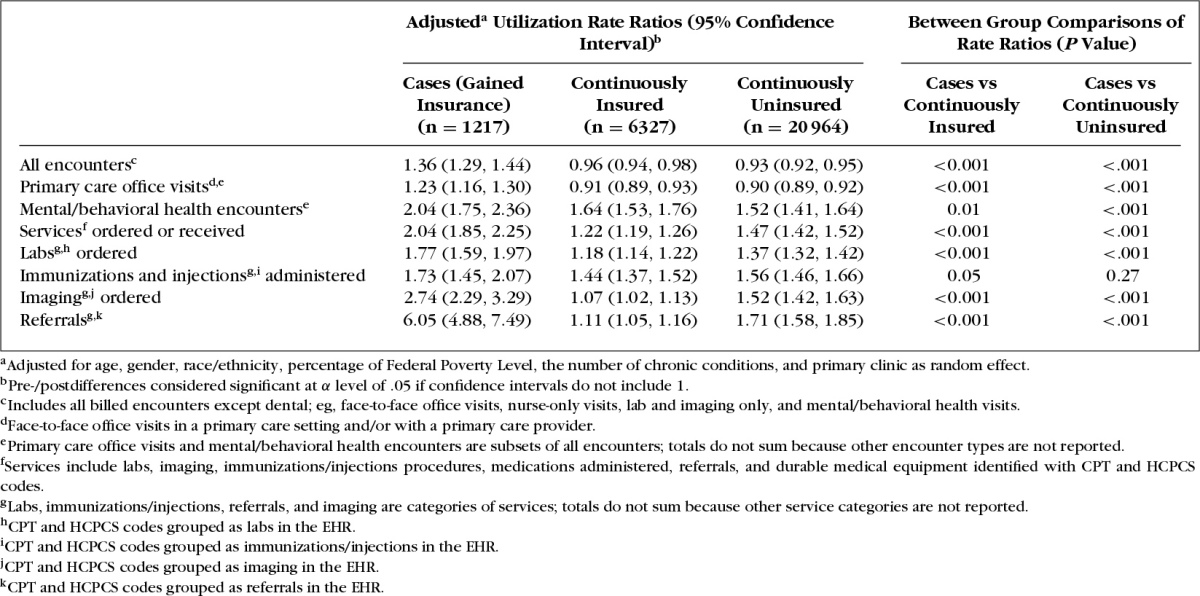
Table 3 shows the rate ratios of pre- versus postcoverage utilization for the 3 study groups, and how these differ between the groups after controlling for differences in the groups' characteristics. Similar to our unadjusted results, utilization among those who gained insurance increased for all measures. The magnitude of the change in utilization in this group significantly exceeded that in both comparison groups in all measures except immunizations and injections, even in adjusted analyses.
Table 3. Adjusted Rate Ratios Comparing Pre- and Postcoverage Start Date Utilization for the 3 Study Groups.
Adjusted monthly encounter rates over the study period are shown in Figure 1. Overall, CHC utilization among persons who gained insurance increased immediately after coverage began. Their postcoverage utilization then reached a level similar to that among the continuously insured and remained at that level throughout follow-up. All-encounter utilization among those who gained insurance was significantly higher than among the continuously insured in months 2 to 6 (significance was borderline in month 4). These results were very similar when limited to primary care office visits only (not shown).
Figure 1.
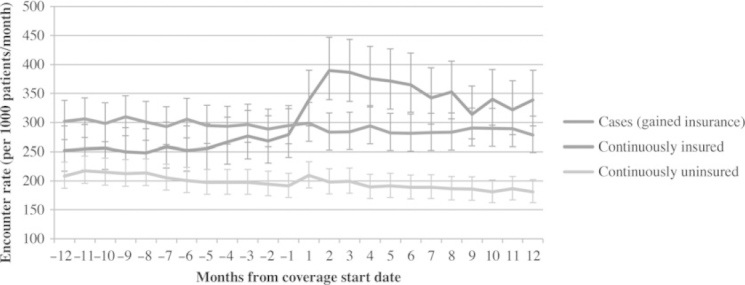
Comparison of monthly adjusteda encounter ratesb by patient group. aAdjusted for age, gender, race/ethnicity, percentage of Federal Poverty Level, the number of chronic conditions, and primary clinic as random effect. bRates are averaged over each 1-month interval. The coverage start date begins immediately after month -1. Start dates were randomly assigned to the continuously insured and uninsured groups based on the distribution of cases' 2008 coverage start dates.
DISCUSSION
States preparing to expand Medicaid coverage to previously uninsured populations must estimate how these expansions will impact demand on CHCs and other primary care providers (Ku, Jones, Shin, Bruen, & Hayes, 2011). Previous studies using clinic-level aggregated reports, self-reported data, and claims data to report increased utilization among newly insured persons were disadvantaged by limitations associated with these data sources (Hofer et al., 2011; Ku, Jones, Shin, Byrne, & Long, 2011). The results presented here confirm prior predictions of increased utilization, and the use of EHR data addresses some of previous studies' limitations. The population of persons who gained insurance in this study is a reasonable proxy for persons who will become eligible for Medicaid under the ACA expansion: most (84%) of those in this study who gained insurance had household incomes less than 100% of the FPL, the cutoff relevant to the 2008 Oregon expansion, and 93% had incomes 138% of the FPL or less, the cutoff for Medicaid expansion under the ACA.
These findings are directly applicable to estimating how ACA expansions will impact demand for ambulatory care services from providers serving Medicaid populations. In this study, utilization of all encounters increased 35% or more among newly insured, established CHC patients in the year after Oregon's 2008 Medicaid expansion; in-person primary care visit utilization increased 22%; and services ordered or received doubled. These results are consistent with those from a survey conducted in a subset of patients who received coverage through Oregon's 2008 expansion, who reported increases in the number of office visits made after receiving coverage (Baicker et al., 2013).
In this study, utilization among the continuously insured and continuously uninsured comparison groups was relatively stable compared with utilization among the newly insured, suggesting that postcoverage utilization changes among those who gained insurance were likely related to their gaining coverage, and not attributable to secular trends or concurrent initiatives. However, even after we adjusted for baseline characteristics, including the difference in baseline health status described previously, utilization rates among persons who gained coverage through Oregon's Medicaid expansion were significantly greater than rates among the continuously uninsured in the 4 months prior to the Medicaid expansion. This suggests that persons with greater medical need may have been particularly motivated to sign up for coverage during Oregon's Medicaid expansion. This is consistent with previous reports that persons potentially eligible for Medicaid through the ACA have fewer chronic conditions than those already enrolled in Medicaid, but have worse control over their existing conditions (Decker et al., 2013). Thus, persons who seek enrollment through the ACA may have greater unmet need for care than those who remain uninsured, so the health status of previously uninsured patients must be considered when estimating how ACA expansions will affect care utilization among safety net patients.
The “pent-up demand hypothesis” posits that utilization increases soon after patients gain insurance (Eisert & Gabow, 2002; State Health Access Data Assistance Center, 2005); some have shown that this initial increase tends to decline the longer a person is enrolled in Medicaid (Ku et al., 2009). Similarly, our study population of established safety net patients had a brief postcoverage “spike” in utilization, which declined somewhat over time. However, we found that postcoverage utilization among the newly insured stayed higher than their precoverage utilization for at least 12 months past the coverage start date, and became similar to utilization rates among continuously insured persons.
These findings suggest that providers who care for Medicaid-insured patients, and CHC-based primary care providers in particular, may be able to predict how demand will change post-ACA Medicaid expansions by assuming that postcoverage utilization among currently uninsured patients will rise rapidly in the first few months, and then will be sustained at a level similar to that among their currently insured patients. This knowledge may help CHCs estimate the extent to which ACA-related changes constrain their capacity to meet demand. It may also help policy makers consider approaches to supporting the safety net in the initial postcoverage period, such as continued expansion funding. While different populations will be affected, these results may also inform thinking about how demand for CHC services will change with the expansion of private insurance exchanges.
LIMITATIONS
This study was designed to assess how utilization changed in CHCs after a policy-driven expansion of Medicaid coverage—an expansion that was closely analogous to the ACA. We compared established CHC patients who gained new coverage (ie, not persons who sought CHC services only after gaining coverage) to established CHC patients whose insurance status was consistent during the study periods (ie, insured or uninsured throughout the entire pre- or postperiods). Further research is needed to estimate how demand may change among discontinuously insured patients, and among new CHC patients; these populations may also affect CHCs' capacity to meet demand, discussed previously.
While most of the persons who gained insurance in this study did so because of Oregon's 2008 Medicaid expansion, some likely gained coverage because of eligibility changes caused by changes in their health, socioeconomic status, or another life event. As noted previously, persons who gained insurance may have had greater medical need that motivated them to seek coverage. However, as Oregon's 2008 expansion was based on poverty level, changes in coverage eligibility due to qualified health conditions should have been similar among persons who gained insurance and those who remained uninsured. Furthermore, in our population, by definition, those who gained coverage sought at least some care in CHCs even when they were uninsured; therefore, their postcoverage utilization might be higher than it would be for those who never sought care while uninsured. The demographic characteristics of the newly insured differed significantly from those of the comparison groups; notably, the continuously uninsured have the highest percentage of Hispanic persons, likely including immigrants who are ineligible for Medicaid. We addressed these limitations by adjusting our between-group analyses for baseline health status (the number of chronic conditions), race/ethnicity, socioeconomic status, and other factors, and accounting for correlation within clinic populations. Additional adjustment might help to further isolate how gaining insurance impacts utilization; nevertheless, our findings likely yield an accurate depiction of post-Medicaid expansion utilization patterns.
Our use of CHCs' EHR data is a strength but did not allow us to assess the extent to which established CHC patients sought care at settings other than the study CHCs, once they were insured; further research is needed to understand this better. In studies of a similar policy-driven expansion in Massachusetts, newly insured CHC patients were more likely to increase demand at a CHC where they had previously been seen, rather than seeking new primary care providers (Ku, Jones, Shin, Byrne, & Long, 2011). To ensure a minimum level of care continuity in our analyses, we limited our study to CHC patients with 1 or more visits to an OCHIN CHC in both the pre- and postcoverage periods, thus excluding patients who left the CHC after gaining coverage.
The EHR data also allowed us to assess demand for ambulatory care visits and services only. Utilization of care at hospitals or emergency departments may decrease as newly insured patients access better preventive care; conversely, utilization of some hospital-based services (eg, nonurgent surgeries) may increase as payment barriers decrease (Ku, Jones, Shin, Byrne, & Long, 2011). Providers of specialty care, laboratory services, medical imaging, etc, also may experience increased demand post-ACA, as few CHCs have such resources in-house. Our finding that ordered/received services (labs, imaging, and referrals) almost doubled among the newly insured supports this assumption, and suggests that both primary care providers and those who see patients referred from primary care settings need to prepare for insurance expansion. Community health centers may want to work with other community providers to prepare for changing demand for such services.
CONCLUSIONS
This study greatly informs estimates of how demand for ambulatory care services might change among newly insured patients post-ACA Medicaid expansions. In sum, demand for primary care services provided by CHCs and other providers who serve Medicaid populations may increase 22% to 35%; after a short-term spike, demand among the newly insured will likely be sustained at a level higher than their precoverage rates and similar to that among other insured patients.
Footnotes
The authors thank the OCHIN practice-based research network health centers.
This study was supported by grant R01HL107647 from the National Heart, Lung, and Blood Institute.
The authors have no conflicts of interest to report.
REFERENCES
- Allen H., Baicker K., Finkelstein A., Taubman S., Wright B. J. (2010). What the Oregon health study can tell us about expanding Medicaid. Health Affairs (Millwood), 29(8), 1498–1506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicker K., Finkelstein A. (2011). The effects of Medicaid coverage—Learning from the Oregon experiment. New England Journal of Medicine, 365(8), 683–685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicker K., Taubman S. L., Allen H. L., Bernstein M., Gruber J. H., Newhouse J. P., Smith J. (2013). The Oregon experiment—effects of Medicaid on clinical outcomes. New England Journal of Medicine, 368(18), 1713–1722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmueller T. C., Grumbach K., Kronick R., Kahn J. G. (2005). The effect of health insurance on medical care utilization and implications for insurance expansion: A review of the literature. Medical Care Research and Review, 62(1), 3–30 [DOI] [PubMed] [Google Scholar]
- Davidoff A., Kenney G., Dubay L. (2005). Effects of the State Children's Health Insurance Program Expansions on children with chronic health conditions. Pediatrics, 116(1), e34–e42 [DOI] [PubMed] [Google Scholar]
- Decker S. L., Doshi J. A., Knaup A. E., Polsky D. (2012). Health service use among the previously uninsured: Is subsidized health insurance enough? Health Economics, 21(10), 1155–1168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker S. L., Kostova D., Kenney G. M., Long S. K. (2013). Health status, risk factors, and medical conditions among persons enrolled in Medicaid vs uninsured low-income adults. JAMA, 309(24), 2579–2586 [DOI] [PubMed] [Google Scholar]
- Duderstadt K. G., Hughes D. C., Soobader M. J., Newacheck P. W. (2006). The impact of public insurance expansions on children's access and use of care. Pediatrics, 118(4), 1676–1682 [DOI] [PubMed] [Google Scholar]
- Eisert S., Gabow P. (2002). Effect of Child Health Insurance Plan enrollment on the utilization of health care services by children using a public safety net system. Pediatrics, 110(5), 940–945 [DOI] [PubMed] [Google Scholar]
- Finkelstein A., Taubman S., Wright B., Bernstein M., Gruber J., Newhouse J. P., Baicker K. Oregon Health Study Group. (2012). The Oregon health insurance experiment: Evidence from the first year. The Quarterly Journal of Economics, 127(3), 1057–1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman J. D., Kadiyala S., Bell J. F., Martin D. P. (2008). The causal effect of health insurance on utilization and outcomes in adults: A systematic review of US studies. Medical Care, 46(10), 1023–1032 [DOI] [PubMed] [Google Scholar]
- Gold R., DeVoe J. E., McIntire P. J., Puro J. E., Chauvie S. L., Shah A. R. (2012). Receipt of diabetes preventive care among safety net patients associated with differing levels of insurance coverage. Journal of the American Board of Family Medicine, 25(1), 42–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins D., Groves D. (2011). The future role of community health centers in a changing health care landscape. The Journal of Ambulatory Care Management, 34(1), 90–99 [DOI] [PubMed] [Google Scholar]
- Hicks L. S., O'Malley A. J., Lieu T. A., Keegan T., Cook N. L., McNeil B. J., Guadagnoli E. (2006). The quality of chronic disease care in U.S. community health centers. Health Affairs (Millwood), 25(6), 1712–1723 [DOI] [PubMed] [Google Scholar]
- Hofer A. N., Abraham J. M., Moscovice I. (2011). Expansion of coverage under the Patient Protection and Affordable Care Act and primary care utilization. Milbank Quarterly, 89(1), 69–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempe A., Beaty B. L., Crane L. A., Stokstad J., Barrow J., Belman S., Steiner J. F. (2005). Changes in access, utilization, and quality of care after enrollment into a state child health insurance plan. Pediatrics, 115(2), 364–371 [DOI] [PubMed] [Google Scholar]
- Kenney G. (2007). The impacts of the State Children's Health Insurance Program on children who enroll: findings from ten states. Health Services Research, 42(4), 1520–1543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku L., Jones E., Shin P., Byrne F. R., Long S. K. (2011). Safety-net providers after health care reform: Lessons from Massachusetts. Archives of Internal Medicine, 171(15), 1379–1384 [DOI] [PubMed] [Google Scholar]
- Ku L., Jones K., Shin P., Bruen B., Hayes K. (2011). The states' next challenge—securing primary care for expanded Medicaid populations. New England Journal of Medicine, 364(6), 493–495 [DOI] [PubMed] [Google Scholar]
- Ku L., MacTaggart P., Pervez F., Rosenbaum S. (2009). Improving Medicaid's continuity and quality of care. Retrieved August 31, 2013, from http://www.communityplans.net/Portals/0/ACAP%20Docs/ACAP%20MCQA%20Report.pdf
- Long S. K., Stockley K. (2011). The impacts of state health reform initiatives on adults in New York and Massachusetts. Health Services Research, 46(1 Pt 2), 365–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McWilliams J. M., Meara E., Zaslavsky A. M., Ayanian J. Z. (2007). Use of health services by previously uninsured Medicare beneficiaries. New England Journal of Medicine, 357(2), 143–153 [DOI] [PubMed] [Google Scholar]
- Miller S. (2012). The effect of the Massachusetts reform on health care utilization. Inquiry, 49(4), 317–326 [DOI] [PubMed] [Google Scholar]
- Morgan D. (2012). Health centers for poor, uninsured see ranks swell. Retrieved January 21, 2013, from http://www.reuters.com/article/2012/05/01/us-usa-healthcare-centers-idUSBRE8401JL2012050
- National Association of Community Health Centers. (2013). United States health center fact sheet. Retrieved November 1, 2013, from http://www.nachc.com/client/US12.pdf
- Polsky D. (2011). How the newly insured use health services: A lesson for the U.S. from Medicare. LDI Issue Brief, 17(4), 1–4 [PubMed] [Google Scholar]
- Shi L., Stevens G. D. (2007). The role of community health centers in delivering primary care to the underserved: Experiences of the uninsured and Medicaid insured. Journal of Ambulatory Care Management, 30(2), 159–170 [DOI] [PubMed] [Google Scholar]
- Sommers B. D., Arntson E., Kenney G. M., Epstein A. M. (2013). Lessons from early Medicaid expansions under health reform: Interviews with Medicaid officials. MMRR, 3(4). http://dx.doi.org/10.5600/mmrr.003.04.a02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- State Health Access Data Assistance Center. (2005). Pent-up demand for health care services among the newly insured. Retrieved May 14, 2013, from http://www.azahcccs.gov/reporting/Downloads/HRSAgrant/publications/SHADAC_FINAL_REPORT.pdf
- Szilagyi P. G., Dick A. W., Klein J. D., Shone L. P., Zwanziger J., McInerny T. (2004). Improved access and quality of care after enrollment in the New York State Children's Health Insurance Program (SCHIP). Pediatrics, 113(5), e395–e404 [DOI] [PubMed] [Google Scholar]
- The Johns Hopkins ACG® system. (2011). (Version 10) Baltimore, MD: Johns Hopkins Bloomberg School of Public Health [Google Scholar]
- The White House. (2012). The Obama administration and community health centers. Retrieved June 5, 2012, from http://www.whitehouse.gov/sites/default/files/05-01-12_community_health_center_report.pdf
- Zhang J. X., Huang E. S., Drum M. L., Kirchhoff A. C., Schlichting J. A., Schaefer C. T., Chin M. H. (2009). Insurance status and quality of diabetes care in community health centers. American Journal of Public Health, 99(4), 742–747 [DOI] [PMC free article] [PubMed] [Google Scholar]


