Abstract
Background
Thirty day readmissions are common in general surgery patients and affect long term outcomes including mortality. We sought to determine the effect of complication timing on post-operative readmissions.
Methods
Patients from our institutional ACS NSQIP database who underwent general surgery procedures from 2006–2011 were included. The primary outcome of interest was 30 day hospital readmission.
Results
Patients diagnosed with post-discharge complications were significantly more likely to be readmitted (56%) compared with patients diagnosed with complications before discharge (7%, p<0.001). Independent predictors of post-discharge complications included laparoscopic case, short hospital stay, pre-operative dyspnea and independent functional status. GI Complications and Surgical Site Infection were the most common reasons for readmission.
Conclusions
The development of complications after hospital discharge places patients at significant risk for readmission. Early identification and treatment of GI complications and Surgical Site Infections in the outpatient setting may decrease post-operative readmission rates.
Keywords: Post-discharge complication, post-operative readmission
INTRODUCTION
Readmissions following surgical procedures are common affecting 4–25% of patients.1–5 Readmissions have been found to be associated with significantly increased mortality in vascular surgery, colon cancer, pancreatectomy, and elderly thyroid cancer patients.4, 6, 7 Standardization of the discharge process, increased patient education and outpatient follow up have improved readmission rates in both medical and surgical patients.7, 8 As more is known about which patients are at risk for readmission and what preventable diagnoses contribute to readmission, more specific interventions can be employed to further decrease post-operative readmissions.
Risk factors for readmission after surgery include older age and more comorbidities.2, 4, 6 Other factors which have been shown to increase readmission rates include later stage disease in colorectal cancer patients, need for emergent operation at index hospitalization and placement in skilled nursing facility or long term care facility at the time of discharge.2, 4 Previous studies have described longer length of stay and post-operative complications as strong predictors of readmissions.2, 4, 6, 7, 9, 10
While both complications and length of stay appear to play important roles in post-operative readmissions, little is known about the timing of complications, reasons for readmission, or which complications contribute most to readmissions. An ACS NSQIP study identified that 42% of complications occurred post-discharge and found patients diagnosed after discharge were more likely to require reoperation and more likely to die within 30 days.11 The aim of this study was to evaluate the timing of complication diagnosis in association with length of stay and hospital readmissions and to determine if complications were the primary reason for readmission in this patient population.
METHODS
Data Source
We evaluated general surgery patients at a single academic teaching center from the American College of Surgeons National Surgical Quality Improvement Project (ACS NSQIP) database between 2006 and 2011. The ACS NSQIP collects data prospectively and reports risk adjusted outcomes for the purpose of quality improvement.
Patients
All available ACS NSQIP data from a single institution was paired with the electronic medical record to accurately identify all patients readmitted within 30 days and to identify the reason for readmission. Patients who underwent elective, inpatient, general surgery procedures were included in our analysis. Patients were excluded if they died within 30 days of hospital discharge.
Outcome Variables
The primary outcome variable of interest was 30 day readmission. The reason for readmission was determined from our institutional electronic medical record. Readmissions were classified as planned readmissions, complications and other/not surgical complications. Planned readmission included scheduled readmissions for a reason unrelated to the operation.
In addition to 30 day readmissions, we also evaluated the following variables: length of stay, presence or absence of postoperative complications within 30 days and timing of complication in relation to discharge. Length of stay was divided into the following categories based on natural break points in the data: 0–2 days, 3–5 days, 6–8 days and > 8 days. These break points were established based on clinically meaningful separations, such that sample sizes were non-limiting. Complications were classified as occurring before or after discharge. Time from discharge to diagnosis of complication was also evaluated in patients diagnosed as outpatients and was divided into the following categories: ≤ 5 days, 6–12 days, > 12 days, which were clinically meaningful and resulted in non-limiting sample sizes. Finally, pre-operative patient comorbidities, pre-operative functional status, intraoperative factors and perioperative outcomes were evaluated as potential risk factors for post-discharge diagnosis of complications. Functional status was determined based on the ability to perform activities of daily living, where independent status indicated the patient did not require any assistance with activities of daily living.
Statistical Analysis
We evaluated the overall frequency of 30 day readmissions and complications. Chi-square testing was performed to evaluate for associations between timing of complication diagnosis and readmission. This analysis was done in the entire population of patients with complications and also within the length of stay categories. A similar analysis was performed to evaluate for an association between timing of complication diagnosis after discharge and readmission. We determined the frequency of each reason for readmission in all readmitted patients and within the post-discharge categories described above. Finally, we evaluated patient and perioperative factors, with chi square analyses, as potential risk factors for post-discharge complications. All factors with P value <0.1 on univariate analysis were evaluated with multivariate analysis. Two explanatory variables, preoperative sepsis and functional status, were found to be highly associated (R = 0.477) and were combined as a single variable in the multivariate analysis. All statistical analyses were performed in SPSS Statistics version 21. P values < 0.05 were considered significant and all P values were 2-tailed.
RESULTS
Patient Characteristics
A total of 3,632 patients who underwent an inpatient general surgery procedure were identified from the University of Wisconsin ACS NSQIP database. Seventy six patients (2%) died within 30 days of discharge and were therefore not included in our analysis. The study sample consisted of 3,556 patients. As demonstrated in Table 1, the most common surgical specialty in this patient population was colorectal surgery. Open procedures were more common for all surgical specialties with the exception of advanced minimally invasive surgery/foregut. The thirty day readmission rate in this patient population was 9%. The overall 30 day complication rate was 31% with 37% of complications occurring after discharge from the hospital. The average time from discharge to post-discharge complication was 10 days and the median time was 8 days.
Table 1.
Study Population by Surgical Procedure
| Surgical Specialty | Patients N = 3,556 n (%) |
Laparoscopic Approach N=1,315 n (%)* |
Open Approach N = 2,241 n (%)* |
|---|---|---|---|
| Advanced MIS/Foregut | 469 (13) | 387 (83) | 82 (17) |
| Colorectal | 1,306 (37) | 463 (35) | 843 (65) |
| Endocrine | 283 (8) | 81 (29) | 202 (71) |
| General Surgery | 853 (24) | 256 (30) | 597 (70) |
| Hepaticopancreaticobiliary | 645 (18) | 128 (20) | 517 (80) |
The percentage in the last 2 columns denotes the percentage of patients who underwent laparoscopic versus open approach within each surgical specialty.
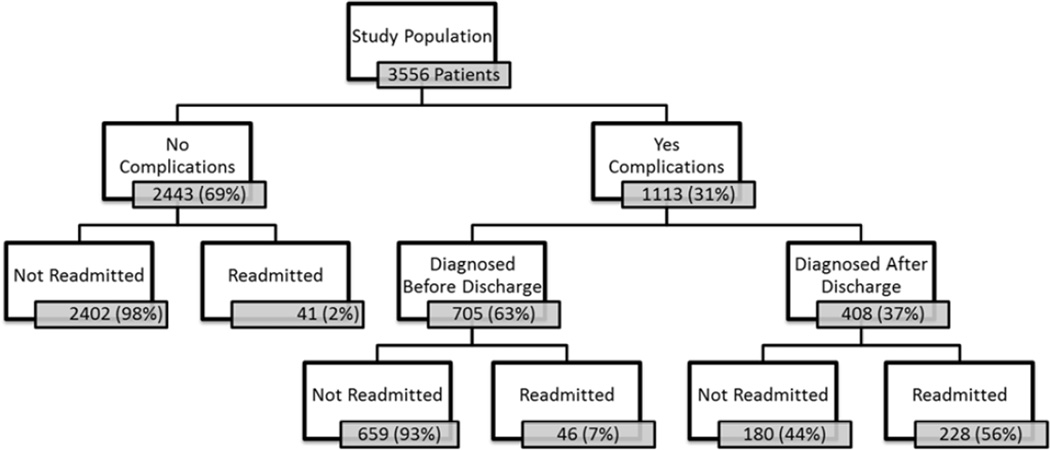
Timing of Complication Diagnosis and Readmissions
Figure 1 categorizes the study population in terms of post-operative complications and readmissions. Of note, readmission rates in patients with complications diagnosed before discharge were low at 7% and increased dramatically to 56% in patients who had complications diagnosed after discharge (P <0.001). This was further analyzed within each length of stay category (0–2 days, 3–5 days, 6–8 days and >8 days) and patients diagnosed with complications after discharge in each category had significantly higher rates of readmission (p=0.001 for each length of stay category).
Figure 1.
Flow chart of complications and readmission rates in entire study population.
Laparoscopic approach, private insurance, short length of stay, pre-operative dyspnea, independent functional status, lower American Society of Anesthesiologists Classification (1–2), and younger age (<65) correlated with post-discharge complications on univariate analysis. Patients with lack of the following pre-operative conditions were more likely to develop post-discharge complications: Diabetes, Chronic Obstructive Pulmonary Disease, Hypertension, Open Wound, and Sepsis. The variables listed in Table 2 were found to be independent predictors of post-discharge diagnosis of complications (c statistic = 0.742). In patients who underwent laparoscopic procedures, short length of stay was the only variable found to be significantly associated with post-discharge diagnosis of complications (p<0.001).
Table 2.
Risk Factors for Post-Discharge Diagnosis of Complications (Multivariate Analysis)
| Variable | Odds Ratio | Confidence Interval |
|---|---|---|
| Laparoscopic | 1.888 | 1.363–2.615 |
| Length of Stay | ||
| 3–5 days | 0.402 | 0.249–0.650 |
| 6–8 days | 0.359 | 0.221–0.584 |
| >8 days | 0.124 | 0.076–0.204 |
| Preoperative Dyspnea | 1.985 | 1.218–3.233 |
| Functional Status/Preoperative Sepsis* | ||
| Independent with sepsis | 0.481 | 0.308–0.752 |
| Dependent with sepsis | 0.523 | 0.298–0.905 |
Baseline comparison was independent functional status and lack of preoperative sepsis
We found that as length of stay increased the proportion of complications diagnosed before discharge from the hospital also increased. Patients who were hospitalized for <3 days and developed complications were diagnosed after discharge 71% of the time as compared with 18% of patients who remained in the hospital >8 days (p<0.001).
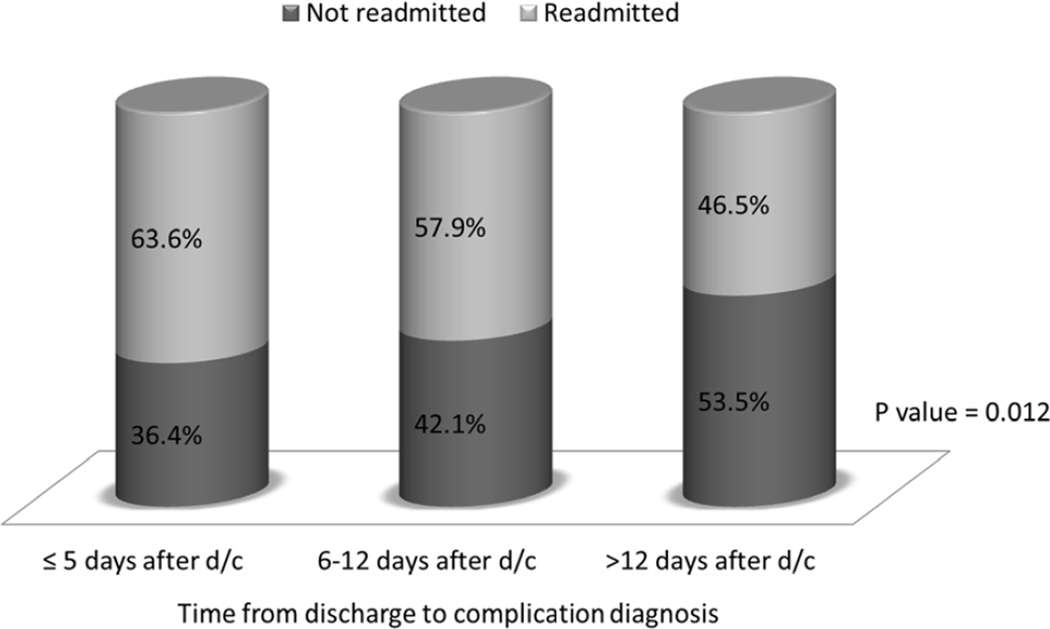
Figure 2 demonstrates readmission rates in association with timing of complication diagnosis after discharge. Although, readmission risk decreases as complications are diagnosed farther from discharge, there is still approximately 50% risk of readmission with diagnosis of complications > 12 days after discharge.
Figure 2.
Timing of complication after discharge and readmission.
Reasons for Readmissions
The reasons for readmission for the 315 patients readmitted within 30 days are displayed in Table 3. The most common reasons for readmission were GI Complications and Surgical Site Infection/Wound Disruption, accounting for over one half of all readmissions. Table 3 further describes the readmission diagnoses for the 93 patients included in GI Complications and the 83 patients within Surgical Site Infection/Wound Disruption. The majority of readmissions due to Surgical Site Infection/Wound Disruption were secondary to Organ Space Infections (57%). Reason for readmission was also differentiated between patients who underwent laparoscopic and open procedures (Table 3).
Table 3.
Reason for Readmission
| Reason for Readmission | Total N= 315 n (%) |
Laparoscopic N = 104 n (%)* |
Open N = 211 n (%)* |
|---|---|---|---|
| GI Complications | 93 (29.5) | 28 (26.9) | 65 (30.8) |
| Ileus/Constipation | 40 (43.0) | 10 (9.6) | 30 (14.2) |
| Bowel Obstruction | 26 (28.0) | 12 (11.5) | 14 (6.6) |
| Dehydration/Electrolyte Abnormality | 23 (24.7) | 6 (5.8) | 17 (8.1) |
| Delayed Gastric Emptying | 2 (2.2) | 0 (0) | 2 (0.9) |
| Gastroenteritis | 2 (2.2) | 0 (0) | 2 (0.9) |
| SSI | 83 (26.3) | 18 (17.3) | 65 (30.8) |
| Organ Space | 47 (56.6) | 12 (11.5) | 35 (16.6) |
| Superficial | 21 (25.3) | 4 (3.8) | 17 (8.1) |
| Deep | 13 (15.7) | 2 (1.9) | 11 (5.2) |
| Dehiscence | 2 (2.4) | 0 (0) | 2 (0.9) |
| Post-operative Pain (unknown etiology) | 14 (4.4) | 5 (4.8) | 9 (4.3) |
| Bleeding/Anemia | 13 (4.1) | 6 (5.8) | 7 (3.3) |
| Sepsis | 12 (3.8) | 5 (4.8) | 7 (3.3) |
| Deep Vein Thrombosis/Pulmonary Embolism | 9 (2.9) | 6 (5.8) | 3 (1.4) |
| Urinary Tract Infection | 9 (2.9) | 3 (2.9) | 6 (2.8) |
| Cellulitis | 9 (2.9) | 4 (3.8) | 5 (2.4) |
| Pneumonia | 7 (2.2) | 3 (2.9) | 4 (1.9) |
| Congestive Heart Failure/Fluid Overload | 6 (1.9) | 1 (1.0) | 5 (2.4) |
| Pancreatitis | 5 (1.6) | 2 (1.9) | 3 (1.4) |
| Planned Readmission | 5 (1.6) | 2 (1.9) | 3 (1.4) |
| COPD/Bronchitis | 4 (1.3) | 2 (1.9) | 2 (0.9) |
| Fever (unknown etiology) | 4 (1.3) | 1 (1.0) | 3 (1.4) |
| Clostridium difficile Infection | 3 (1.0) | 3 (2.9) | 0 (0) |
| Catheter/Shunt Dysfunction | 3 (1.0) | 2 (1.9) | 1 (0.5) |
| Renal Insufficiency | 2 (0.6) | 0 (0) | 2 (0.9) |
| Cerebral Vascular Accident | 2 (0.6) | 0 (0) | 2 (0.9) |
| Chest Pain (unknown etiology) | 2 (0.6) | 1 (1.0) | 1 (0.5) |
| Adrenal Insufficiency | 2 (0.6) | 2 (1.9) | 0 (0) |
| Enterocutaneous Fistula | 2 (0.6) | 0 (0) | 2 (0.9) |
| Other (not complications) | 26 (8.3) | 10 (9.6) | 16 (7.6) |
The percentage in the last 2 columns denotes the proportion of patients who underwent laparoscopic or open procedures within each reason for readmission category.
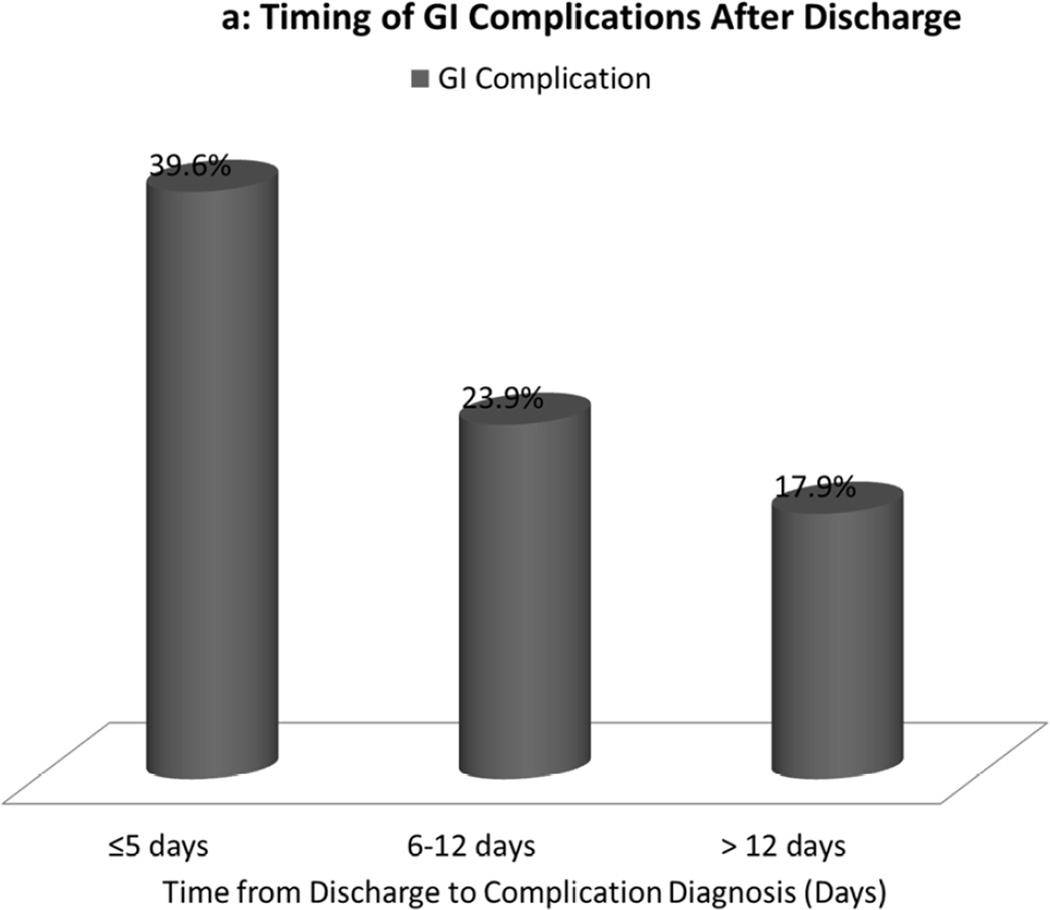
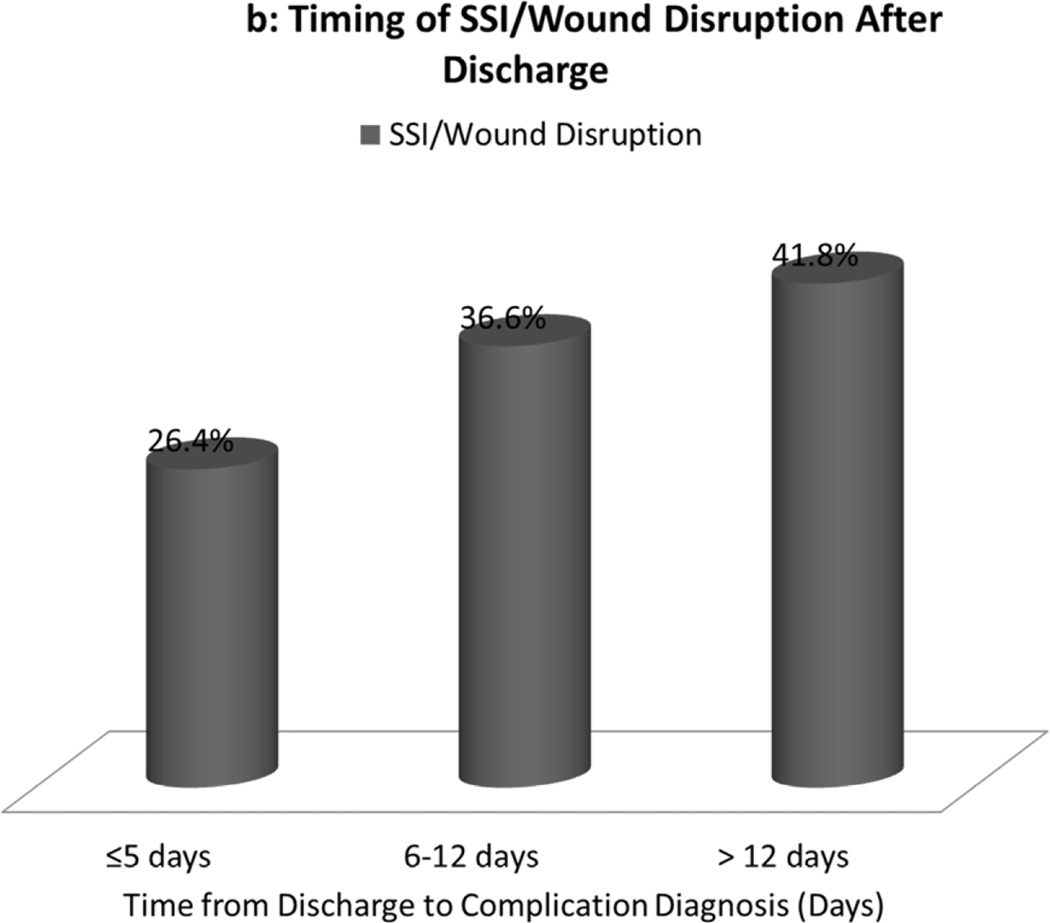
Within the group of patients at highest risk for readmission (those diagnosed with complications after discharge), GI Complications and Surgical Site Infection/Wound Disruption remained the most common causes of readmission. As demonstrated in Figure 3a, GI Complication was a common cause for readmission in the first five days after discharge (40%) after which rates decreased (18% at >12 days). As shown in Figure 3b, Surgical Site Infection/Wound Disruption was less common immediately following discharge (26%) and increased in frequency by >12 days after discharge (42%). This suggests that general surgery patients are at risk for GI complications in the early post-discharge period and the risk for Surgical Site Infection increases one week after discharge.
Figure 3.
a: Proportion of readmissions due to GI Complications in post-discharge complication categories.
b: Proportion of readmissions due to SSI/Wound Disruption in post-discharge complication categories.
DISCUSSION
We found that patients diagnosed with complications after discharge were much more likely to be readmitted and that although readmissions decreased as time from discharge to complication diagnosis increased, patients diagnosed with complications within 2 weeks after discharge still had a 50% risk for readmission. GI Complications and Surgical Site Infection /Wound Disruption were the most common causes of readmission with a high incidence of GI Complications early after discharge and increasing incidence of Surgical Site Infection /Wound disruption later after discharge.
We found that GI Complications and Surgical Site Infection /Wound Disruption accounted for over 50% of all readmissions due to complications. These remained the most common reasons for readmission when patients who underwent laparoscopic and open procedures were evaluated separately. Other authors have described similar findings. Greenblatt and colleagues4 evaluated the SEER Medicare database and found that 36% of readmissions after colectomy were due to GI complications or infections. In patients who underwent laparoscopic colectomy, most complications (43%) were due to abdominal pain with an additional 29% of complications due to infection.3 Reddy et al. described readmissions in patients with pancreatic adenocarcinoma and found 80% were due to “operative complications” (abscess, sepsis, hemorrhage and pancreatic fistula).10 Paradoxically, in the Medicare fee-for-service program Jencks et al. found that 73% of readmissions in surgical patients were due to “medical reasons” as opposed to “surgical reasons”.5 However, medical reasons included conditions such as GI complications which may have been associated with the index operation and may partially explain this discrepancy.
Patients in this study were much more likely to be readmitted if complications were diagnosed after discharge as compared with patients diagnosed prior to discharge. Thirty seven percent of all complications were diagnosed after discharge from the hospital. Kazaure et al. described a similar rate with 42% of complications occurring post-discharge11. We also found the reason for readmission differed in patients diagnosed with complications early after discharge as compared with later after discharge. This information will act as guide for more specific patient education, appropriate timing of follow up appointments and clinics aimed at identifying complications early to prevent readmissions.
While previous studies have found an association between longer length of stay and high readmission rates,2, 4, 9 we found higher readmission rates in patients who had post-discharge complications and that short length of stay was independently correlated with post-discharge complications. This difference may be explained by differences in study inclusion criteria and timeframe for readmission. Smith et al.9 evaluated veteran medical patients who were readmitted within 90 days of discharge, while we evaluated surgical patients within 30 days. The other two studies,2, 4 only evaluated colorectal patients and included patients who underwent emergent operations, while we assessed all general surgery patients and excluded patients who had emergency surgery. Kelly and colleagues2 defined prolonged length of stay as >24 days and Greenblatt et al.4 defined prolonged length of stay as >15 days; this high cutoff for prolonged length of stay is most likely due to longer length of stay in emergency surgery patients who are also more likely to be readmitted.2, 4 Therefore, our study provides new information about complications and readmissions in the non-emergent general surgery patient population.
We expected to find that short length of stay was associated with outpatient complication diagnosis and that the majority of patients were readmitted for post-discharge complications. However, we were surprised to find that regardless of length of stay and timing of complication after discharge, diagnosis of complications after discharge placed patients at high risk of readmission. Laparoscopic surgery, preoperative dyspnea and independent functional status were also risk factors for post-discharge complications. When we evaluated patients who underwent laparoscopic procedures independently, short hospital stay correlated with post-discharge complications. Shorter length of stay in laparoscopic patients most likely explains why laparoscopic surgery is a risk factor for post-discharge complications. Knowledge of these risk factors will help identify patients who may benefit from earlier and more frequent postoperative clinic follow up.
Patient education prior to discharge has been shown to decrease readmission rates.8 Given the results of this study, we propose general surgery patients at our institution should have teaching regarding GI complications prior to discharge. Also, knowing the median time from discharge to complication diagnosis is 8 days and that 40% of GI complications occur in the first 5 days following discharge, we propose outpatient follow up should occur within one week of discharge. In clinic, patients should be evaluated for GI complications and Surgical Site Infection and further teaching regarding signs and symptoms of infection should occur.
Limitations of this study include that it utilizes retrospective ACS NSQIP data. This study was performed at a single center and therefore may not be generalizable to other centers. Also, this study was not powered to evaluate the timing of procedure specific complications and their effects on readmission. We believe this will be an important next step in better understanding which complications contribute to post-operative readmissions. We only considered readmissions in this study and therefore may have underestimated post-discharge hospital utilization. Kind and colleagues12 have described “complicated transitions” in medical patients, which describe any movement to more intensive care and include ED visits, transition to skilled nursing facility and new need for home care in addition to hospital readmissions. The rate of readmission may also be underestimated in this patient population as patients have been found to be readmitted at a different hospital from the index hospital in 13–22% of cases4, 13 and it is likely that many patients are readmitted outside 30 days.
In conclusion, patients diagnosed with complications after discharge were much more likely to be readmitted to the hospital within 30 days. While readmission rates decreased as complications were diagnosed later after discharge, almost half of patients diagnosed with complications 2 weeks after discharge required readmission. GI Complications and Surgical Site Infection/Wound Disruption accounted for over one half of all readmissions in this patient population. These results highlight the importance of complication timing after discharge and identifying the reason for readmissions to provide targets for quality improvement with the goal of preventing readmissions in general surgery patients.
Acknowledgments
This study was supported by a National Institute of Health T32 training grant (CA090217).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflict of interest
References
- 1.Podulka J, Barrett M, Jiang HJ. Steiner C. 30-Day Readmissions following Hospitalizations for Chronic vs. Acute Conditions, 2008: Statistical Brief #127. 2006 Feb; [PubMed] [Google Scholar]
- 2.Kelly M, Sharp L, Dwane F, Kelleher T, Comber H. Factors predicting hospital length-of-stay and readmission after colorectal resection: a population-based study of elective and emergency admissions. BMC Health Serv Res. 2012;12:77. doi: 10.1186/1472-6963-12-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Down SK, Nicolic M, Abdulkarim H, Skelton N, Harris AH, Koak Y. Low ninety-day re-admission rates after emergency and elective laparoscopic cholecystectomy in a district general hospital. Ann R Coll Surg Engl. 2010 May;92(4):307–310. doi: 10.1308/003588410X12664192075053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenblatt DY, Weber SM, O'Connor ES, LoConte NK, Liou JI, Smith MA. Readmission after colectomy for cancer predicts one-year mortality. Ann Surg. 2010 Apr;251(4):659–669. doi: 10.1097/SLA.0b013e3181d3d27c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009 Apr 2;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 6.Greenblatt DY, Greenberg CC, Kind AJ, et al. Causes and implications of readmission after abdominal aortic aneurysm repair. Ann Surg. 2012 Oct;256(4):595–605. doi: 10.1097/SLA.0b013e31826b4bfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tuggle CT, Park LS, Roman S, Udelsman R, Sosa JA. Rehospitalization among elderly patients with thyroid cancer after thyroidectomy are prevalent and costly. Ann Surg Oncol. 2010 Nov;17(11):2816–2823. doi: 10.1245/s10434-010-1144-7. [DOI] [PubMed] [Google Scholar]
- 8.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009 Feb 3;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith DM, Giobbie-Hurder A, Weinberger M, et al. Predicting non-elective hospital readmissions: a multi-site study. Department of Veterans Affairs Cooperative Study Group on Primary Care and Readmissions. J Clin Epidemiol. 2000 Nov;53(11):1113–1118. doi: 10.1016/s0895-4356(00)00236-5. [DOI] [PubMed] [Google Scholar]
- 10.Reddy DM, Townsend CM, Jr, Kuo YF, Freeman JL, Goodwin JS, Riall TS. Readmission after pancreatectomy for pancreatic cancer in Medicare patients. J Gastrointest Surg. 2009 Nov;13(11):1963–1974. doi: 10.1007/s11605-009-1006-4. discussion 1974–1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kazaure HS, Roman SA, Sosa JA. Association of postdischarge complications with reoperation and mortality in general surgery. Arch Surg. 2012 Nov 1;147(11):1000–1007. doi: 10.1001/2013.jamasurg.114. [DOI] [PubMed] [Google Scholar]
- 12.Kind AJ, Smith MA, Frytak JR, Finch MD. Bouncing back: patterns and predictors of complicated transitions 30 days after hospitalization for acute ischemic stroke. J Am Geriatr Soc. 2007 Mar;55(3):365–373. doi: 10.1111/j.1532-5415.2007.01091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kind AJ, Bartels C, Mell MW, Mullahy J, Smith M. For-profit hospital status and rehospitalizations at different hospitals: an analysis of Medicare data. Ann Intern Med. 2010 Dec 7;153(11):718–727. doi: 10.1059/0003-4819-153-11-201012070-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]