Abstract
OBJECTIVES
To describe new users of antihypertensives and identify predictors of combination therapy initiation among older Americans.
DESIGN
Retrospective observational cohort study.
SETTING
Population-based study using U.S. Medicare fee-for-service healthcare claims (2007–2010).
PARTICIPANTS
275,493 Medicare beneficiaries >65 years of age with no recent diagnoses, procedures or medications for cardiovascular disease who newly initiated antihypertensives (210,605 initiated monotherapy and 64,888 initiated combination therapy).
MEASUREMENTS
Multivariable Poisson regression assessed factors associated with initiation of combination versus monotherapy controlling for patient characteristics, prescriber characteristics and patient encounters with healthcare system.
RESULTS
Initiation of combination therapy increased from 21.9% in 2007 to 24.7% in 2010. The most frequently initiated combinations were angiotensin-converting-enzyme inhibitor/thiazide (29.7%) and angiotensin II receptor antagonists/thiazide (18.7%). Blacks (prevalence ratio 1.48, 95% confidence interval 1.45–1.51 compared with whites), patients seeing a generalist (1.10, 1.07–1.14), patients seeing more than one doctor (3.38, 3.33–3.44), or patients with no pharmacy claims in the last six months (1.34, 1.30–1.37 compared with three or more unique drug classes) were more likely to initiate combination therapy, while patients who had more outpatient visits in the last 12 months were less likely to initiate combination therapy (per five visits 0.82, 0.80–0.83).
CONCLUSION
Nearly one in four new users of antihypertensive over the age of 65 started treatment with combination therapy. Blacks, individuals living in the South, and patients who had fewer outpatient physician office visits were more likely to initiate combination therapy. Further research is needed to determine whether this approach to managing hypertension is being well-targeted to those patients who will require combination treatment.
Keywords: Antihypertensive agents, Combination therapy, Epidemiology, Initial treatment, Medicare beneficiaries
INTRODUCTION
The prevalence of hypertension is high in older Americans, affecting more than 65% of people over the age of 65.1 The incidence of hypertension rises with increasing age, and individuals who were normotensive at age 55 have an approximate 90% lifetime risk of hypertension.2 Hypertension is an important risk factor for cardiovascular disease (CVD) and a leading risk factor for premature death and loss of disability-adjusted life-years in the United States.3 As the population is aging, the importance of managing hypertension in older adults continues to increase in terms of the impact on public health.
Advances in drug therapy have made a wide variety of blood pressure lowering antihypertensive agents available. Clinical trials have demonstrated the benefit of antihypertensives on cardiovascular events4,5 and affirmed the benefit of treating hypertension even in individuals over the age of 80.6,7 Most single antihypertensive agents can reduce blood pressure by 10 to 15%, but the majority of patients ultimately require two or more agents to achieve effective control.8
Among the many options for antihypertensive therapy, combination therapy has been gaining more attention. Combination therapy is defined as treatment with two or more agents administrated separately or in a fixed-dose combination pill.4,5 Initiating treatment with combination therapy has potential benefits including improved rate of blood pressure control and, in the case of fixed-dose combination pills, simplified treatment regimens and better adherence.9–11 Potential disadvantages include increased cost for some combinations, patients' perception of being sicker when prescribed more medications, risk of adverse effects, drug burden and lower adherence rates if two pills are required.12 Given these complex risk/benefit trade-offs, initiation of antihypertensive treatment with combination versus monotherapy remains controversial.11–15
As the evidence and guidelines are continuously evolving, little is known about the initial management of hypertension for older adults in the actual “real world” setting of clinical practice. Further, patient and health care-related factors associated with initiation of combination are not well understood. Our objectives were to describe the initial drug management of hypertension in a large cohort of older Americans without previous cardiovascular conditions and identify factors associated with the initiation of combination therapy versus monotherapy.
METHODS
Data Sources and Study Population
Using a de-identified random 20% sample of Medicare beneficiaries age 65 and older with feefor-service Part A, B, and D coverage simultaneously in at least one calendar month between 2007 and 2010, we identified a cohort of patients who initiated antihypertensive therapy between July 1st, 2007 and December 31st, 2010. Eligible new users had been continuously enrolled in Parts A and B for at least one year prior and in Part D for at least six months. Antihypertensive drug classes in this study included angiotensin converting enzyme inhibitors (ACEI), angiotensin II receptor antagonists (ARB), beta blockers (BB), calcium channel blockers (CCB) and thiazide (THZ). New users of antihypertensives were defined as patients who filled a prescription claim for any antihypertensive formulation of interest following six antihypertensive prescription-free months. The index date was defined as the fill date of an antihypertensive prescription. The index period ranged from the index date through the 14th day after the index date. Eligible new users who received more than one class of antihypertensive drug in form of fixed-dose combination pills or multiple single drug combinations within the index period were defined as combination therapy initiators. Patients with one unique antihypertensive drug class dispensed during the index period were defined as monotherapy initiators. We characterized patients' demographic characteristics and clinical conditions based on outpatient and inpatient claims occurring in the 12-month period prior to the index date and pharmacy claims during the six months prior to the index date.
To limit the study population to those patients who initiated antihypertensives without recent claims for CVD related diagnoses or treatments, we excluded patients who had any code for stroke, heart failure, myocardial infarction, angina, atrial fibrillation, revascularization or other CVD during the 12 months preceding the index date. We further excluded patients who had any prescription claim for warfarin, cardiac glycosides, antiplatelet drugs, nitrates or antiarrhythmics during the six months preceding the index date. The Institutional Review Board at the University of North Carolina at Chapel Hill approved this study.
Statistical Analyses
We categorized the new users in the final study cohort based on the index drug classes. The prevalence ratios (PR) and 95% confidence intervals (CI) for initiating combination therapy versus monotherapy were estimated by multivariable Poisson regression.16 Potential predictors of combination versus monotherapy initiation included demographic characteristics, comorbidities, procedures, number of prescribers for antihypertensives, prescriber's specialty, number of co-medications during six months prior to the index date, number of outpatient visits, and days of hospitalization. All analyses were conducted using SAS version 9.3 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
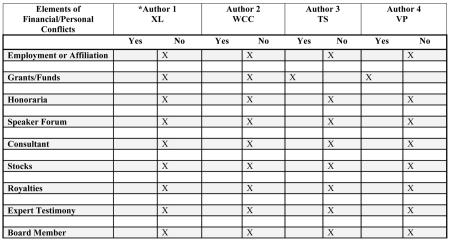
Between July 1st, 2007 and December 31st, 2010, we identified 275,493 Medicare beneficiaries without recent claims for CVD initiating an antihypertensive after at least six antihypertensive prescription-free months. As shown in Table 1, the median age of patients at initiation was 73 years (interquartile range 69–79). They were predominately female (67.0%) and white (79.8%) while blacks accounted for 10.1% of the population. A large proportion (40.4%) were from the South, 18.9% of the patients had type 2 diabetes, 55.3% had hyperlipidemia and 4.9% were prescribed antihypertensives by a cardiologist.
Table 1.
Characteristics of New Users of Antihypertensives among Medicare Beneficiaries with No Evidence of Cardiovascular Disease, United States, 2007–2010
| Percentage, % | |||
|---|---|---|---|
| All N= 275,493 | Monotherapy N= 210,605 | Combination N= 64,888 | |
| % | 100.0 | 76.4 | 23.6 |
| Female | 67.0 | 67.1 | 66.6 |
| Race/Ethnicity a | |||
| White | 79.8 | 82.0 | 72.9 |
| Black | 10.1 | 8.2 | 16.0 |
| Hispanic | 3.9 | 3.7 | 4.7 |
| Other | 6.2 | 6.1 | 6.4 |
| Age b | |||
| Median (IQR) | 73 (69–79) | 73 (69–80) | 73 (69–79) |
| 66–69 | 28.8 | 28.3 | 30.4 |
| 70–74 | 27.5 | 27.1 | 28.7 |
| 75–79 | 18.8 | 18.9 | 18.5 |
| 80–84 | 13.4 | 13.8 | 12.4 |
| 85–89 | 7.6 | 7.8 | 6.8 |
| 90+ | 3.9 | 4.1 | 3.2 |
| Region | |||
| Midwest | 23.8 | 24.0 | 23.2 |
| Northeast | 16.0 | 16.5 | 14.7 |
| South | 40.4 | 39.2 | 44.1 |
| West | 19.3 | 19.9 | 17.5 |
| U.S. territories | 0.4 | 0.4 | 0.5 |
| Number of outpatient physician visits | |||
| in the last 12 months, median (IQR) | 5 (2–8) | 5 (2–9) | 4 (1–7) |
| 0 | 9.4 | 8.1 | 13.5 |
| 1–3 | 30.1 | 28.3 | 36.2 |
| 4–7 | 30.7 | 31.7 | 27.8 |
| 8+ | 29.7 | 31.9 | 22.6 |
| Comorbidities c | |||
| Chronic kidney diseases | 3.3 | 3.4 | 3.2 |
| Type 2 diabetes | 18.9 | 18.9 | 18.8 |
| Hyperlipidemia | 55.3 | 56.2 | 52.5 |
| Chronic obstructive pulmonary disease | 7.4 | 8.0 | 5.7 |
| Tobacco use | 6.0 | 6.3 | 5.0 |
| Procedures | |||
| Electrocardiography | 8.1 | 8.4 | 7.0 |
| Lipid test | 44.1 | 45.1 | 41.0 |
| Stress test | 3.9 | 4.2 | 3.1 |
| Number of Prescribers | |||
| Median (IQR) | 1 (1–1) | 1 (1–1) | 1 (1–1) |
| Prescriber Specialty d | |||
| Cardiologist | 4.9 | 4.8 | 5.3 |
| Other internist | 34.7 | 34.3 | 35.8 |
| Generalist | 34.3 | 32.9 | 38.6 |
| Other medical doctore | 7.2 | 8.5 | 2.9 |
| Nurse practitioner/Physician assistant | 5.7 | 5.6 | 5.7 |
| Other provider | 0.8 | 0.9 | 0.3 |
| Unknown | 12.5 | 12.9 | 11.5 |
| Baseline Medications f | |||
| Number of classes | |||
| 0 | 44.3 | 41.6 | 52.7 |
| 1 | 27.5 | 28.4 | 24.8 |
| 2 | 16.0 | 16.9 | 13.2 |
| 3+ | 12.2 | 13.1 | 9.3 |
| Analgesics | |||
| Nonsteroidal anti-inflammatory drugs | 12.0 | 12.4 | 10.7 |
| Opioids | 11.3 | 11.7 | 9.8 |
| Paracetamol | 9.1 | 9.5 | 7.8 |
| Antidiabetics | |||
| Insulin | 2.5 | 2.5 | 2.5 |
| Oral antidiabetics | 8.6 | 8.8 | 7.9 |
| Mental Health | |||
| Antidementia | 2.7 | 2.9 | 1.8 |
| Antidepressants | 11.8 | 12.7 | 8.6 |
| Antiparkinson | 1.7 | 1.9 | 1.1 |
| Anxiolytics | 2.3 | 2.4 | 1.8 |
| Hypnotics | 3.8 | 4.1 | 3.0 |
| Other | |||
| Antiasthma | 8.4 | 8.9 | 6.7 |
| Hormone replacement therapy | 3.9 | 4.3 | 2.9 |
| Osteoporosis treatment | 7.5 | 8.2 | 5.2 |
| Statins | 17.3 | 18.2 | 14.4 |
Note: All percentages are column percentages; IQR = Interquartile Range
From a cohort of 513,669 new users of antihypertensives, people initiated alpha blockers (N= 15,785), had claims for cardiovascular related diagnoses, procedures or medications (N= 222,391) were excluded.
From Medicare denominator file.
At time of initiation.
Clinical conditions were identified using definitions consisting of diagnoses with relevant International Classification of Diseases, Ninth Revision, Clinical Medication (ICD-9-CM) codes, and procedures with Current Procedural Terminology (CPT®) codes.
Prescriber's specialty information was extracted from the pharmacy claims file. For patients who initiated combination therapy and had multiple prescribers during the index period, the specially type of the second prescriber was used.
Other medical doctor includes physicians practicing in Emergency Medicine, Dermatology, Otolaryngology, Pain Medicine, Pathology, Pediatrics, Psychiatry and Neurology, Surgery and etc.
Data regarding prescription medication fills were extracted from Part D prescription drug event files using a crosswalk between the Anatomical Therapeutic Chemical (ATC) identifier and the National Drug Codes (NDC) adapted from First DataBank's National Drug Data File Plus.17
Among all new antihypertensive users, 23.6% (N= 64,888) initiated combination therapy. Compared with initiators of monotherapy, they were more likely to be black, younger and from the South. The counties with 30% or more combination therapy initiation were concentrated around the Southeast. Combination therapy users had fewer outpatient office visits in the last 12 months and fewer different co-medication drug classes. Their antihypertensives were more likely to be prescribed by a generalist.
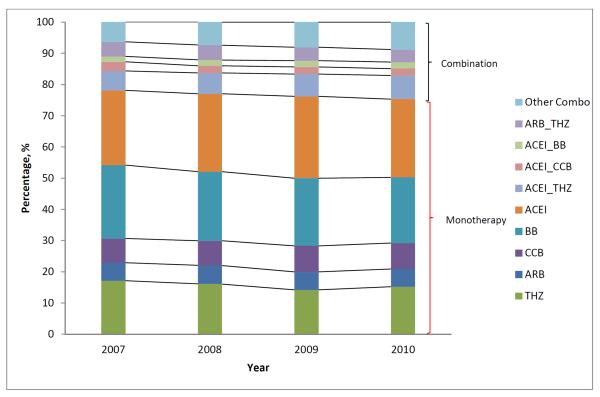
The most commonly prescribed initial monotherapy drug class was ACEI (25.2%) followed by THZ (15.4%) while the most frequently initiated combinations were ACEI/THZ (7.0%), ARB/THZ (4.4%), and ACEI/CCB (2.3%). The proportion of patients being started on combination therapy increased slightly from 21.9% in 2007 to 24.7% in 2010. The examination of trends of initial first-line antihypertensive therapy over the study period showed changes in the frequency of use (Appendix 1). Small increases were observed for the use of ACEI/THZ while the use of ARB/THZ decreased slightly. Among monotherapy options, the proportion of people initiating ACEI and CCB increased while the use of BB and THZ decreased. The use of ARBs was relatively stable.
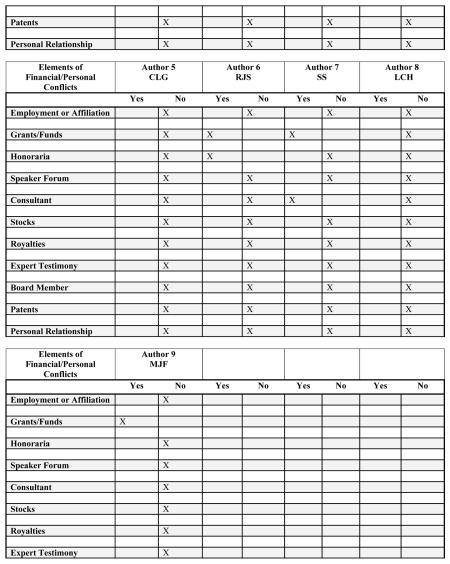
In multivariable analyses, we found no factors strongly associated (i.e., PR > 4.00) with initiation of combination versus monotherapy, but several were modestly associated with initiation of combination therapy after adjusting for other characteristics (Table 2). Among statistically significant predictors, the strongest were race, region, prescriber specialty, number of prescribers, outpatient physician visits and number of co-medications. Blacks were more likely to be prescribed a combination therapy compared with whites (PR= 1.48, 95%CI: 1.45–1.51). The effect was attenuated from a crude association (PR= 1.75, 95%CI: 1.72–1.78) when race/ethnicity was the only predictor considered in the model. Patients residing in the South, seeing more prescribers from different specialties, seeing a generalist or those with no pharmacy claims in the last six months were also more likely to initiate combination therapy. Patients who had any hospital stay or had more outpatient visits in the last 12 months were less likely to initiate combination therapy, however. Having had a lipid test or a stress test was also associated with decreased likelihood of combination therapy initiation.
Table 2.
Determinants of Combination versus Monotherapy Antihypertensive Therapy Initiation among Medicare Beneficiaries with No Evidence of Cardiovascular Disease, United States, 2007–2010
| Combination versus Monotherapy | ||||||
|---|---|---|---|---|---|---|
| Prevalence Ratio (95% Confidence Interval) | ||||||
| Unadjusted | Multivariable Adjusted | |||||
| Year | ||||||
| 2007 | 1.00 | 1.00 | ||||
| 2008 | 1.05 | 1.02 | 1.07 | 1.03 | 1.01 | 1.06 |
| 2009 | 1.09 | 1.06 | 1.11 | 1.06 | 1.04 | 1.09 |
| 2010 | 1.12 | 1.10 | 1.15 | 1.08 | 1.06 | 1.11 |
| Sex | ||||||
| Male | 1.00 | 1.00 | ||||
| Female | 0.98 | 0.97 | 1.00 | 1.03 | 1.02 | 1.05 |
| Race/Ethnicity a | ||||||
| White | 1.00 | 1.00 | ||||
| Black | 1.75 | 1.72 | 1.78 | 1.48 | 1.45 | 1.51 |
| Hispanic | 1.30 | 1.26 | 1.34 | 1.21 | 1.17 | 1.26 |
| Other | 1.14 | 1.11 | 1.17 | 1.12 | 1.09 | 1.15 |
| Age b | ||||||
| per 5 years older | 0.96 | 0.95 | 0.96 | 0.96 | 0.95 | 0.96 |
| Region | ||||||
| West | 1.00 | 1.00 | ||||
| Midwest | 1.08 | 1.06 | 1.10 | 1.08 | 1.06 | 1.11 |
| Northeast | 1.01 | 0.99 | 1.03 | 1.03 | 1.00 | 1.05 |
| South | 1.21 | 1.18 | 1.23 | 1.18 | 1.16 | 1.21 |
| U.S. territories | 1.30 | 1.19 | 1.42 | 1.25 | 1.11 | 1.40 |
| Hospitalization in the last 12 months | ||||||
| None | 1.00 | 1.00 | ||||
| Hospitalized in the last year | 0.84 | 0.81 | 0.86 | 0.94 | 0.91 | 0.97 |
| Per one more day in the hospitalc | 1.00 | 0.99 | 1.00 | 1.00 | 0.99 | 1.00 |
| Outpatient Visit | ||||||
| None | 1.00 | 1.00 | ||||
| Had 1+ visit in the last 30 days | 0.90 | 0.89 | 0.91 | 0.85 | 0.83 | 0.86 |
| Per five visits in the last 12 monthsd | 0.70 | 0.69 | 0.71 | 0.82 | 0.80 | 0.83 |
| Comorbidities | ||||||
| Chronic kidney diseases | 0.96 | 0.92 | 1.00 | 1.00 | 0.96 | 1.04 |
| Type 2 diabetes | 1.00 | 0.98 | 1.02 | 1.06 | 1.04 | 1.08 |
| Hyperlipidemia | 0.89 | 0.88 | 0.90 | 1.06 | 1.04 | 1.08 |
| Chronic obstructive pulmonary disease | 0.75 | 0.73 | 0.77 | 0.92 | 0.89 | 0.95 |
| Tobacco use | 0.83 | 0.80 | 0.85 | 0.93 | 0.90 | 0.96 |
| Procedures | ||||||
| Electrocardiography | 0.86 | 0.83 | 0.88 | 1.00 | 0.97 | 1.03 |
| Lipid test | 0.88 | 0.87 | 0.89 | 0.94 | 0.93 | 0.96 |
| Stress test | 0.77 | 0.74 | 0.81 | 0.89 | 0.85 | 0.93 |
| Prescriber | ||||||
| One prescriber | 1.00 | 1.00 | ||||
| Two or more prescribers | 3.54 | 3.49 | 3.59 | 3.38 | 3.33 | 3.44 |
| Prescriber Specialties | ||||||
| Cardiologist | 1.00 | 1.00 | ||||
| Other internists | 0.96 | 0.93 | 0.99 | 1.03 | 1.00 | 1.06 |
| Other medical doctore | 0.38 | 0.36 | 0.40 | 0.39 | 0.37 | 0.41 |
| Generalist | 1.05 | 1.02 | 1.09 | 1.10 | 1.07 | 1.14 |
| Nurse practitioner/Physician assistant | 0.94 | 0.90 | 0.98 | 0.98 | 0.94 | 1.02 |
| Other provider | 0.33 | 0.29 | 0.38 | 0.31 | 0.27 | 0.35 |
| Number of Co-medication classes | ||||||
| None | 1.57 | 1.53 | 1.60 | 1.34 | 1.30 | 1.37 |
| One | 1.18 | 1.15 | 1.21 | 1.11 | 1.08 | 1.14 |
| Two | 1.09 | 1.05 | 1.12 | 1.05 | 1.02 | 1.08 |
| Three or more | 1.00 | 1.00 | ||||
Poisson models for unadjusted prevalence ratios and 95% confidence intervals included only the variables under consideration. Poisson models for multivariable adjusted prevalence ratios and 95% confidence interval adjusted for all the variables listed in the table.
From Medicare denominator file.
At time of initiation, included as a linear continuous variable in the model.
Modeled as a continuous variable with a linear term and a quadratic term.
Modeled as a continuous variable with a linear term, a quadratic term and a cubic term.
Other medical doctor includes physicians practicing in Emergency Medicine, Dermatology, Otolaryngology, Pain Medicine, Pathology, Pediatrics, Psychiatry and Neurology, Surgery and etc.
After controlling for other factors, the year of initiation of antihypertensive therapy remained modestly predictive of combination therapy use, indicating that the observed increase in prevalence was not fully explained by changes in the population. Patients with type 2 diabetes or hyperlipidemia were more likely to initiate combination therapy, but patients with a code for tobacco use or chronic obstructive pulmonary disease were less likely to initiate combination therapy.
DISCUSSION
In this large, national sample of older Americans without recent claims related to CVD who began antihypertensive treatment, we found that one in four patients initiated combination therapy. The use of combination therapy as first-line treatment increased slightly from 2007 to 2010. Nationally, counties in which at least 30% of new users received combination therapy were concentrated in the Southeast and overlapped, to some extent, with the “stroke belt” where higher rates of stroke and other CVD cluster.18
Among patients initiating combination therapy, the three most frequent combinations were ACEI/THZ, ARB/THZ, and ACEI/CCB. These combinations have demonstrated synergistic or complementary effects: ACEI/THZ,19 ARB/THZ,20 and ACEI/CCB,21 and have been recommended as preferred choice of two-drug combinations.8 They are also available in single-pill form, making them easier to manage and may reduce out-of-pocket patient costs.
The choice of antihypertensive therapy is normally based on blood pressure, stage of hypertension, age, gender, race or ethnic group, coexisting conditions and the response to previously used drugs, including the presence or absence of adverse reactions.15 In this population of patients starting antihypertensives, with blood pressure and stage of hypertension unobserved, we found the strongest predictors of combination therapy included black race, number of co-medication classes and living in the South. These findings are consistent with other research studies.14,22 Compared with whites, blacks are more likely to have stage 2 hypertension which typically requires two or more agents to achieve blood pressure control.4,23,24 Chronic conditions are common among older adults with more than a third of Medicare beneficiaries having four or more chronic conditions,25 and many of these require medication. Concerns about additional pill burden leading to difficulty with adherence and potential drug interactions may underlie the inverse association between the number of other medications used by the patient and the initiation of combination (rather than mono-) therapy.
In addition to the demographic characteristics, patients' encounters with the healthcare system were also associated with initiation of combination therapy. Compared to one prescriber, patients seeing multiple prescribers were more than twice as likely to start on a combination therapy. Among patients initiating combination therapy, 8.2% received different prescriptions within 14 days from different prescribers. While the use of another drug class in the index period might be due to adverse side effects of the initial therapy, we think it is unlikely as most of these patients filled another prescription of the initial therapy after adding the second drug class. It is possible that the initial therapy was not sufficient to reach target blood pressure level and additional drug classes were deemed necessary. Alternatively, concurrent initiation may have been inadvertent if the providers were not aware of other interactions with the healthcare system.
Our findings should be interpreted in light of the inherent limitations of claims data. These data do not include blood pressure levels or stage of hypertension, which should affect the choice of first-line treatment.4,15,23 Because the indication for the prescription is not reported on the claim, some individuals who we identified as new users of antihypertensives may be treated for reasons other than blood pressure control. We limited the impact of this by excluding patients who were likely to be prescribed antihypertensives for secondary prevention as well as new users of antihypertensive medications with known primary targets other than blood pressure control (e.g., alpha blockers). Thirdly, the Medicare pharmacy drug claims only capture dispensed prescriptions reimbursed by insurance. It is possible that the cohort included patients who were not truly new initiators either because they previously were prescribed an antihypertensive or in the event that the patient was a current user who recently changed from paying out of pocket to using the Medicare drug benefit.26,27 However, we do not expect this to adversely impact the interpretation of our findings. Moreover, Medicare data, as an administrative claims data, are lacking information on alternative approaches to manage hypertension with some being used as complementary to these pharmaceutical agents. Lastly, our findings would not generalize to other populations, such as those with recent cardiovascular complications. Compared with Medicare beneficiaries in general, this is a relatively healthier cohort. For instance, the average number of comedication classes is lower than that reported in other studies of the elderly population.28 Given that we excluded patients with any prevalent use of cardiovascular drugs (the top prescribed therapeutic class in the elderly29), this is expected.
Our study also has several strengths. The existing literature on the “real world” practice of antihypertensive management in the older Americans is restricted to regional12 and specific groups of patients.22 Using the Medicare claims, the largest nationally representative data source in the United States, we were able to examine the use of antihypertensive therapy and provide an update of the existing literature on current clinical practice in older adults on a large scale. Unlike data from electronic medical records, dispensed prescriptions represent medications that patients actually received. With extensive information captured in the claims, we were able to study new users of antihypertensives and assess the relationship between combination therapy as initial treatment and patients' demographic, comorbidities and co-medications, encounters with the healthcare system, and prescriber characteristics. Some of the predictors such as comorbidities and prescriber characteristics were lacking in the previous studies.12,22 While controlling for potential confounding with this multivariable regression, this study identifies several important predictors of choice of initial antihypertensive treatment among many potential factors.
In summary, nearly one in four new users of antihypertensives over age 65 started treatment with combination therapy. Blacks were more likely to initiate combination therapy. More research is needed to determine whether this approach to managing hypertension is being well-targeted and results in better outcomes.
ACKNOWLEDGMENTS
The authors thank Dr. Stacie B. Dusetzina for helpful comments.
Funding sources and related paper presentations: This project was supported by a competitive Gillings Innovation Laboratory award (GIL 200811.0010) from the UNC Gillings School of Global Public Health, grant number K02HS017950 from the Agency for Healthcare Research and Quality, and R01 AG023178 from the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Conflict of Interest: XL is a recipient of the Amgen Pre-doctoral Fellowship in Pharmacoepidemiology. WCC is currently a joint postdoctoral fellow in the Department of Environmental Health Sciences, Johns Hopkins Bloomberg School of Public Health, Baltimore MD and the Center for Health Research, Geisinger Health System (Danville PA, USA). RS has received research support from Merck, and honoraria from Merck and Pfizer. Salary support is provided by investigator initiated grants from Sanofi (TS, VP), Merck (TS, VP) and Amgen (VP), NIA (LCH, TS, R01 AG023178), AHRQ (MJF, K02HS017950), PCORI (TS, MJF, VP, PFA 12001), Johnson and Johnson (SS). SS serves on advisory board for Novartis and Affymax and is supported by AHRQ Mid-Career Awards. MJF and TS receive salary support from the Center for Pharmacoepidemiology which is currently funded by GlaxoSmithKline, UCB Biosciences and Merck.
Sponsor's Role: The grant sponsors had no input on the design, methods, analysis, or preparation of this paper.
Appendix 1.
Trend of Initiation of Antihypertensives by Drug Class among Medicare Beneficiaries with No Evidence of Cardiovascular Disease, United States, 2007–2010.
(ACEI = angiotensin converting enzyme inhibitors; ARB = angiotensin II receptor antagonists; BB = beta blockers; CCB = calcium channel blockers; THZ = thiazide; Combo = combination therapy)
Footnotes
A poster presentation based on an abstract of the study was presented at the 29th International Conference on Pharmacoepidemiology and Therapeutic Risk Management, August 25–28, 2013, Montreal, Canada.
Author Contributions: Study concept and design: XL, WCC, TS, CLG, MJF; Data analysis: XL, VP; Interpretation of data: XL, WCC, TS, RJS, SS, LCH, MJF; Preparation of the manuscript: XL, MJF; Critical revision of the manuscript for important intellectual content: XL, WCC, TS, CLG, RJS, SS, LCH, MJF.
REFERENCES
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics-2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287:1003–1010. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJL, Abraham J, Ali MK, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 5.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC8) JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 6.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 7.Briasoulis A, Agarwal V, Tousoulis D, et al. Effects of antihypertensive treatment in patients over 65 years of age: a meta-analysis of randomised controlled studies. Heart. 2014;100(4):317–323. doi: 10.1136/heartjnl-2013-304111. [DOI] [PubMed] [Google Scholar]
- 8.Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Clin Hypertens (Greenwich) 2011;13:146–154. doi: 10.1111/j.1751-7176.2010.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Epstein M, Bakris G. Newer approaches to antihypertensive therapy. Use of fixed-dose combination therapy. Arch Intern Med. 1996;156(17):1969–1978. [PubMed] [Google Scholar]
- 10.Giles TD. Rationale for combination therapy as initial treatment for hypertension. J Clin Hypertens (Greenwich) 2003;5(4 Suppl 3):4–11. doi: 10.1111/j.1524-6175.2003.02673.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor AA. Combination drug treatment of hypertension: have we come full circle? Curr Cardiol Rep. 2004;6(6):421–426. doi: 10.1007/s11886-004-0049-0. [DOI] [PubMed] [Google Scholar]
- 12.Elliott WJ. Is fixed combination therapy appropriate for initial hypertension treatment? Curr Hypertens Rep. 2002;4(4):278–285. doi: 10.1007/s11906-996-0005-z. [DOI] [PubMed] [Google Scholar]
- 13.Gradman AH. Strategies for combination therapy in hypertension. Curr Opin Nephrol Hypertens. 2012;21(5):486–491. doi: 10.1097/MNH.0b013e328356c551. [DOI] [PubMed] [Google Scholar]
- 14.Egan BM, Bandyopadhyay D, Shaftman SR, et al. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension. 2012;59(6):1124–1131. doi: 10.1161/HYPERTENSIONAHA.112.194167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.August P. Initial treatment of hypertension. N Engl J Med. 2003;348:610–617. doi: 10.1056/NEJMcp010357. [DOI] [PubMed] [Google Scholar]
- 16.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 17.FDB MEDKNOLWEDGE. http://www.fdbhealth.com/fdb-medknowledge/
- 18.National Heart, Lung, and Blood Institute [Assessed Dec 10, 2013];Stroke Belt Initiative: project accomplishments and lessons learned. http://www.nhlbi.nih.gov/health/prof/heart/other/sb_spec.pdf.
- 19.Padilla MC, Armas-Hernández MJ, Hernández RH, et al. Update on diuretics in the treatment of hypertension. Am J Ther. 2007;14(2):154–160. doi: 10.1097/01.pap.0000249938.05382.d0. [DOI] [PubMed] [Google Scholar]
- 20.Sowers JR, Neutel JM, Saunders E, et al. Antihypertensive efficacy of Irbesartan/HCTZ in men and women with the metabolic syndrome and type 2 diabetes. J Clin Hypertens (Greenwich) 2006;8(7):470–480. doi: 10.1111/j.1524-6175.2006.05486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hair PI, Scott LJ, Perry CM. Fixed-dose combination lercanidipine/enalapril. Drugs. 2007;67(1):95–106. doi: 10.2165/00003495-200767010-00007. [DOI] [PubMed] [Google Scholar]
- 22.Monane M, Glynn RJ, Gurwitz JH, et al. Trends in medication choices for hypertension in the elderly. The decline of the thiazides. Hypertension. 1995;25(5):1045–1051. doi: 10.1161/01.hyp.25.5.1045. [DOI] [PubMed] [Google Scholar]
- 23.Aronow WS, Fleg JL, Pepine CJ, et al. ACCF Task Force ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2011;123:2434–2506. doi: 10.1161/CIR.0b013e31821daaf6. [DOI] [PubMed] [Google Scholar]
- 24.Flack JM, Sica DA, Bakris G, et al. on behalf of the International Society on Hypertension in Blacks Management of high blood pressure in blacks: an update of the International Society on Hypertension in Blacks. Hypertension. 2010;56:780–800. doi: 10.1161/HYPERTENSIONAHA.110.152892. [DOI] [PubMed] [Google Scholar]
- 25.Lochner KA, Cox CS. Prevalence of multiple chronic conditions among Medicare beneficiaries, United States, 2010. Prev Chronic Dis. 2013;10:E61. doi: 10.5888/pcd10.120137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li X, Brookhart MA. Evidence of free sample use among new users of branded statins: implications for pharmacoepidemiology. Am J Epidemiol. 2013;177(S11):S–136. [Google Scholar]
- 27.Polinski JM, Schneeweiss S, Levin R, et al. Completeness of retail pharmacy claims data: implications for pharmacoepidemiologic studies and pharmacy practice in elderly patients. Clin Ther. 2009;31(9):2048–2059. doi: 10.1016/j.clinthera.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tulner LR, Kuper IM, Frankfort SV, et al. Discrepancies in reported drug use in geriatric outpatients: relevance to adverse events and drug-drug interactions. Am J Geriatr Pharmacother. 2009;7(2):93–104. doi: 10.1016/j.amjopharm.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 29.Stagnitti MN. Statistical Brief #153. Agency for Healthcare Research and Quality; Rockville, MD: Dec, 2006. [Assessed March 10, 2014]. The top five therapeutic classes of outpatient prescription drugs ranked by total expense for the Medicare population age 65 and older in the US civilian noninstitutionalized population, 2004. DOI: http://dx.doi.org/10.5888/pcd10.120137. [Google Scholar]