Abstract
No studies to date have examined the effect of counselor techniques on smoking cessation over the course of treatment. To address this gap, we examined the degree to which the use of specific Acceptance and Commitment Therapy (ACT) counseling techniques in a given session predicted smoking cessation reported at the next session. The data came from the ACT arm of a randomized controlled trial of a telephone-delivered smoking cessation intervention. Trained raters coded 139 counseling sessions across 44 participants. The openness, awareness and activation components of the ACT model were rated for each telephone counseling session. Multilevel logistic regression models were used to estimate the predictive relationship between each component during any given telephone session and smoking cessation at the following telephone session. For every 1-unit increase in counselors’ use of openness and awareness techniques there were 42% and 52% decreases in the odds of smoking at the next counseling session, respectively. However, there was no significant predictive relationship between counselors’ use of activation techniques and smoking cessation. Overall, results highlight the theoretical and clinical value of examining therapists’ techniques as predictors of outcome during the course of treatment.
Keywords: Acceptance and Commitment Therapy, tobacco, quitline counseling, treatment components, adherence coding, therapist behavior
With 42 million cigarette smokers in the US (US Department of Health and Human Services, 2014), and 1.2 billion smokers worldwide (Mackay, Eriksen, & Shafey, 2006), smoking related deaths currently top 5 million per year, with a projected doubling to 10 million by 2025 (Hatsukami, Stead, & Gupta, 2008). The development of effective behavioral interventions to address tobacco addiction is thus a major public health need. Unfortunately, although there has been considerable innovation in pharmacotherapeutic interventions for smoking cessation over the past 25 years, behavioral interventions have seen little change during this time (Mottillo et al., 2009). Moreover, studies show that across different modalities of delivery, behavioral interventions help only 20% of smokers quit smoking (Lancaster & Stead, 2005; Stead & Lancaster, 2005; Stead, Perera, & Lancaster, 2006). Thus, innovations in behavioral interventions for smoking cessation are long overdue. One way to innovate is to investigate process-level predictors of treatment outcome in order to learn which processes hold promise for improving quit rates (e.g., Kazdin, 2007; Murphy, Cooper, Hollon, & Fairburn, 2009; Paul, 1969).
To date, the analyses of process-level predictors have focused on the study of participant-level processes. For example, in the smoking cessation literature, studies have shown that quit smoking outcomes were mediated by individuals’ self-reported self-efficacy (e.g., Bricker, Liu, et al., 2010), cravings and positive affect (e.g., Bolt, Piper, Theobald, & Baker, 2012; McCarthy et al., 2008). Another study found that quitline counseling had an effect on smoking abstinence by increasing individuals’ confidence and reducing perceived difficulty quitting (McCarthy et al., 2010). While valuable to the field, the critical limitation of this approach is that it leaves out the role of an important manipulable variable on treatment outcomes — variations in counselor-level processes. Variations in counselor-level processes are typically ignored in the analysis of randomized controlled trials that use manual-guided interventions. Therefore examining co-variation between the level of use of counselor strategies and treatment outcomes could be of great value for treatment development purposes.
With a few exceptions (e.g., Calero-Elvira, Froján-Parga, Ruiz-Sancho, & Alpañés-Freitag, in press), process analysis of counselor-level behavior are rare in the cognitive behavioral literature. A notable exception is counselor-level process analyses of Motivational Interviewing (MI). For example, observer ratings of MI counselor techniques predicted relevant client behaviors (e.g., change talk) in alcohol (Glynn & Moyers, 2010), pathological gambling (Hodgins, Ching, & McEwen, 2009), illicit drug use (Amrhein, Miller, Yahne, Palmer, & Fulcher, 2003), cocaine dependence (Aharonovich, Amrhein, Bisaga, Nunes, & Hasin, 2008) and smoking cessation interventions (Boardman, Catley, Grobe, Little, & Ahluwalia, 2006; Catley et al., 2006).
Although the degree of use of some therapeutic techniques has been directly linked with some treatment outcomes (e.g., McCambridge, Day, Thomas, & Strang, 2011), no study to date examined smoking cessation as the treatment outcome. Furthermore, to our knowledge there have been no counselor-level process analyses of Acceptance and Commitment Therapy (ACT) —an innovative intervention with the promise of improving quit rates of smoking cessation programs. ACT is a transdiagnostic model that has been utilized in a variety of populations (e.g., Bach & Hayes, 2002; Lillis, Hayes, Bunting, & Masuda, 2009; Luoma, Kohlenberg, Hayes, & Fletcher, 2012), including in the treatment of tobacco addiction (Bricker, Mann, Marek, Liu, & Peterson, 2010; Bricker, Wyszynski, Comstock, & Heffner, 2013; Gifford et al., 2004, 2011). ACT aims to increase psychological flexibility by providing clients with tools to identify their core values and strengthen their ability to experience uncomfortable thoughts, feelings and physical sensations while engaging in values-driven behaviors.
In order to foster psychological flexibility, ACT interventions are designed to include techniques targeted at the following six processes: acceptance, defusion, present moment awareness, self-as-context, values and commitment. Acceptance and defusion techniques are conceptualized as the “openness” component; present moment and self-as-context as the “awareness” component; and finally, values and commitment as the “activation” component. This tripartite categorization has been described as the “open, aware and active” framework (Hayes, Villatte, Levin, & Hildebrandt, 2011). Table 1 includes a brief description of these processes, although a more detailed account of them can be found elsewhere (see, for example, Hayes, Strosahl, & Wilson, 2011).
Table 1.
Description of ACT components and processes
| Components | Processes | Description |
|---|---|---|
| Openness | Acceptance | Willingness to experience urges, emotions, and thoughts as they are and without any intent to change them. |
| Defusion | Recognizing thoughts, self-judgments, images, and memories as just words and pictures. | |
| Awareness | Present moment | Observation and non-judgmental description of current thoughts, feelings, sensations or other events. |
| Self-as-context | A sense of self that is flexible and distinct from the content of one’s thoughts, feelings and sensations. | |
| Activation | Values | Chosen life directions that guide actions. |
| Commitment | Engagement in activities consistent with chosen values. | |
In a previous issue of this journal, Hesser, Westin, Hayes, and Andersson (2009) examined the content of participants’ verbal statements while receiving an Acceptance and Commitment Therapy (ACT) intervention for tinnitus. Participants’ statements were coded to examine the degree to which they represented two core processes in ACT: willingness to experience the natural flow of thoughts, feelings and physical sensations (acceptance) and the ability to recognize thoughts and images as just words and pictures (defusion) and not as external events (Hayes, Strosahl, & Wilson, 2011). The authors found that the extent to which participants made acceptance and defusion statements during therapy predicted long term improvements in distress and functional impairment due to tinnitus. As pointed out by Hesser et al. (2009), a key limitation of this study was that it did not account for what elements of the intervention might have influenced those verbal statements, suggesting that future studies should examine the role of counseling techniques as agents of treatment outcome. A second limitation to this study was that it targeted a limited range of ACT processes, since it focused on the openness component but omitted both the awareness (also known as mindfulness) and activation components of ACT.
In summary, although previous work in the MI literature has examined treatment components of behavioral interventions for addiction, there is a gap in the MI and ACT literature on the predictive role of counselor behaviors with regards to smoking cessation outcomes. The current study addresses this gap by examining specific ACT counseling techniques as predictors of between-session smoking cessation. Consistent with ACT’s theoretical model, we hypothesize that higher levels of counselor use of openness, awareness and activation components of ACT prospectively predict lower probabilities of smoking at the following counseling session. According to the ACT model these three treatment components should jointly influence treatment outcomes, so we do not hypothesize specific ordering effects of such components. By examining these questions, this study will advance our understanding of the counselor-level processes of change in behavioral interventions for smoking cessation.
Method
Overview of parent trial and participants
The aim of the parent trial was to test the effectiveness of two telephone-delivered interventions for smoking cessation (ACT vs. standard telephone quitline counseling), each delivered in combination with Nicotine Replacement Therapy (NRT), in a two-arm randomized controlled pilot trial. Results of this pilot trial showed that the ACT intervention was feasible, more acceptable and had promising smoking cessation outcomes as compared to standard quitline counseling (Bricker, Bush, Zbikowski, Mercer, & Heffner, 2014). After informed consent, participants were randomized to each treatment condition using a stratified procedure that made assignments based on quit attempts in the past 12 months (yes/no) and smoking within the first 5 minutes of waking (yes/no). Participants were uninsured callers to the South Carolina State Quitline (SCSQL). Having a sample of uninsured SCSQL callers achieved the study goal of including a significant fraction of African Americans and individuals with lower socio-economic status. Both subgroups are important because of their historically low quit rates. The SCSQL is operated by Alere, a US-based company that provides smoking cessation services for 28 state quitlines.
Inclusion criteria
(a) 18 years of age or older, (b) daily smoking for at least the past 12 months, (c) desire to quit smoking in the following 30 days, (d) able to speak and read in English, (e) medically eligible to receive NRT, (e) not participating in other smoking cessation treatments. Among the 59 participants randomized to the ACT condition, 51 (86%) participated in any calls, and 44 (75%) had more than one call (which was required for this predictive session-to-session analysis). These telephone counseling participation rates are at least as good as those of other quit smoking counseling interventions (Stead, Hartmann-Boyce, Perera, & Lancaster, 2013). All 44 participants with more than one call were eligible for the session-to-session analyses of the study. These participants had a total of 139 calls. Table 2 presents descriptive data for the sample. All study procedures were approved by the Institutional Review Board of the Fred Hutchinson Cancer Research Center.
Table 2.
Demographic characteristics and smoking history of the sample (N=44)*
| Statistic | |
|---|---|
| Age, mean (SD) | 40.6 (9.6) |
| Female | 65.9% |
| Race and Ethnicity | |
| White | 77.3% |
| Black | 20.5% |
| Hispanic or Latino | 2.3% |
| Socio-economic status | |
| Unemployed | 59.1% |
| Less than a college degree | 54.6% |
| Smoking history | |
| Partner smokes | 45.5% |
| Smoked 21 or more cigarettes per day | 47.7% |
| Attempted to quit within the past year | 54.5% |
| Smoked for more than 10 years | 79.5% |
Note. SD = Standard deviation
Intervention
The ACT intervention was a five-session telephone-delivered smoking cessation protocol developed by the senior author (JB). The first session had a duration of 30 minutes, followed by four sessions of 15 minutes each. Sessions were provided on a weekly basis. The target quit date was flexible, but participants were encouraged to select a date within the planned 5-week treatment period. The length and duration of the ACT intervention matched that of the standard telephone quitline counseling comparison group. Each session included development of a committed action plan and the use of acceptance techniques, while the remainder of the ACT processes (i.e. values, defusion, present moment, and self-as-context) were the primary focus of one particular session. Counselors were instructed to flexibly apply the protocol so that each session could contain components from other sessions. The goal of allowing this flexibility was to strengthen and consolidate participants’ learning, to allow tailoring of content to the participant, and to encourage a holistic (vs. compartmentalized) approach to intervention delivery.
Participants received a 2-week course of the nicotine patch, which was the standard procedure of the South Carolina State Quitlines at the time of trial enrollment.
Counselors
Counselors were three masters-level female therapists with at least 3 years of clinical experience. Their average age was 45 years old. All counselors received 100 hours of didactic training and were supervised by a licensed clinical psychologist who is an expert ACT trainer.
Adherence coding of ACT components
Previous research has shown that ACT can be delivered with fidelity as a brief telephone intervention (Schimmel-Bristow, Bricker, & Comstock, 2012). One hundred percent of all 139 calls were coded, and a 20% random sample were coded by two raters to determine inter-rater reliability. Raters used the ACT Adherence Rater’s Manual (Bricker & Hayes, 2009), which has Cronbach α’s that range from .72 to .99. For this study, adherence coding was conducted by two bachelors-level raters who were trained and supervised by a licensed clinical psychologist with 15 years of expertise in ACT and behavioral analytic research. In order to reduce rater drift, calibration meetings were conducted monthly during the rating process.
The two raters independently coded the extent to which each treatment component was addressed during each ACT counseling telephone session. Each counseling telephone session was rated on a 5-point Likert scale. Ratings were behaviorally anchored to reflect the extent to which therapists covered acceptance, defusion, present moment, self-as-context, values and commitment skills. A rating of 1 indicated that “the variable never explicitly occurred,” a rating of 2 that “The variable was addressed by the counselor in a superficial manner,” a rating of 3 that “The variable was addressed by the counselor in a mildly in-depth manner,” a rating of 4 that “The variable was addressed by the counselor in a moderately in-depth manner,” and a rating of 5 that “The variable was addressed by the counselor in a very in-depth manner.” Raters were instructed to code only counselors’ verbal behavior and to start each section with a rating of 1 rather than at the midpoint.
Each of the three ACT treatment components (openness, awareness, and activation) were calculated by summing ratings from its two sub-components, rated on the original 5-point scale. Thus, component scores ranged from 2 to 10. Inter-rater reliability was calculated using intraclass correlation coefficients of the form ICC(3,1) (Shrout & Fleiss, 1979), and interpreted using Cicchetti (1994) standards: “poor” (below .40), “fair” (between .40 and .59), “good” (between .60 and .74), and “excellent” (between .75 and 1.00). The openness component included techniques to help individuals be open to their thoughts, feelings and physical sensations and was calculated by summing acceptance and defusion ratings. The awareness component included therapists’ use of techniques to help individuals be aware of their thoughts, feelings and physical sensations without reacting to them and adopt a more flexible sense of self (also known as mindfulness) and it was calculated by aggregating self-as-context and present moment awareness ratings. Finally, the activation component included therapists’ use of techniques to help individuals articulate their personal values and encourage them to take actions towards quitting smoking. This component was calculated by aggregating values and commitment ratings. ICCs were .91 (95% CI = .83, .95) for the openness component, .98 (95% CI = .97, .99) for the awareness component and .94 (95% CI = .88, .97) for the activation component, overall indicating excellent agreement between the two raters.
Outcome measures
Smoking cessation and number of cigarettes per day
At the beginning of each call, the participant reported to the counselor their number of cigarettes smoked during the past 7 days. The counselor recorded that number into a study database. Given that the study outcome was smoking cessation, this number was recoded as a binary outcome (i.e., smoked or not smoked). Self-report of smoking status (i.e., 7-day point prevalence abstinence) is a commonly used indicator of behavior change in smoking cessation trials (Fiore, Jaén, & Baker, 2008) that minimizes recall bias (i.e., participants are more likely to remember whether they smoked at all rather than the exact number of cigarettes they smoked). While there was no biochemical verification of smoking status, the literature suggests that false reporting of smoking status is minimal for low-intensity interventions with no face-to-face contact (Patrick et al., 1994).
Baseline cigarettes per day
Baseline smoking data were gathered during the intake survey. Participants reported their smoking levels based on four categories: 10 or less cigarettes, 11–20 cigarettes, 21–30 cigarettes, or 31 or more cigarettes.
Data analytic strategy
Following the “open, aware and active” framework of ACT (Hayes, Villatte, et al., 2011), our goal was to examine the extent to which each treatment component prospectively predicted smoking cessation over the course of treatment. Accordingly, our analytic strategy was to examine how much the extent of use of each of the treatment components described above in any given counseling session (Componentt) was prospectively associated with the likelihood that participants had achieved smoking abstinence in the next counseling session (Smoking Statust+1).
To account for the repeated measures within subjects, we utilized a logistic regression with random intercepts (Gelman & Hill, 2007). Our regression models adjusted for all ACT components, baseline levels of smoking, and for number of cigarettes smoked per day at the current counseling session. To rule out the potential cumulative effects of participants’ exposure to ACT techniques from previous calls, we also adjusted for number of counseling sessions. Our adjusted model was of the form,
| (1) |
where i indexes individuals and t measurement occasion. A second set of analyses was conducted to examine the effect of each component without adjusting for baseline levels of smoking, number of cigarettes smoked per day at the previous counseling session, and number of counseling calls. These unadjusted models have been recommended in the literature (Austin, Manca, Zwarenstein, Juurlink, & Stanbrook, 2010). Statistical significance was set at the α = .05 level. Regression models were conducted with the lme4 package (Bates, Maechler, & Bolker, 2011) and graphics with the rmeta (Lumley, 2012) and ggplot2 packages (Wickham, 2009) in R-3.0.1 (R Core Team, 2013).
Results
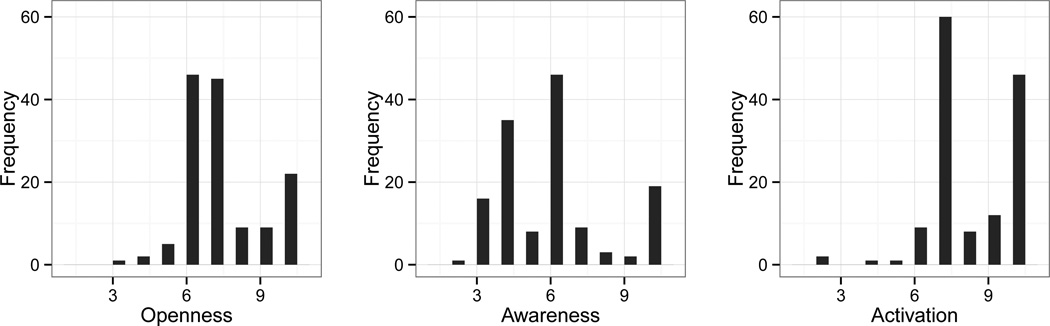
Counselors conducted a total of 139 calls. The average number of counseling sessions per person was 3.2, each with an average duration of 23.6 minutes. All adherence ratings were on a 10-point scale. The openness component had an average extensiveness rating of 7.2 (SD=1.6), the awareness component an average rating of 5.8 (SD=2.2), and the activation component an average rating of 8.1 (SD=1.7). For the activation component 47.5% of ratings were 8 or above. Visual inspection of histograms (see Figure 1) confirmed that as compared to the other variables, the activation component had low variability and a negatively skewed distribution.
Figure 1.
Histograms of adherence ratings to each ACT treatment component.
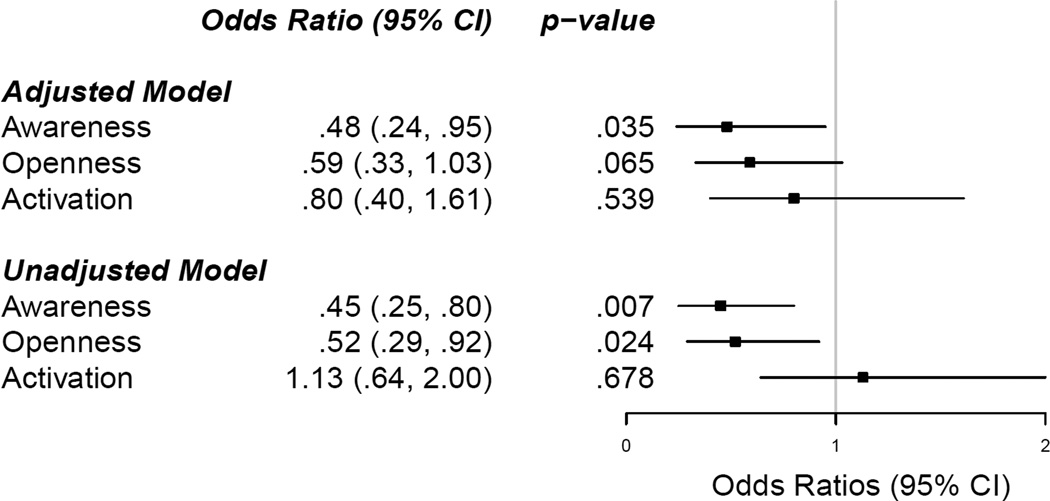
Our regression model indicated that a 1-unit increase in counselors’ use of exercises to promote awareness predicted a 52% lower odds of smoking at the following counseling session (OR = .482; 95% CI = .238, .977; p = .043). Similarly, a 1-unit increase in counselors’ use of openness techniques in one session predicted a non-significant trend of 42% lower odds of smoking at the following counseling session (OR = .585; 95% CI = .338, 1.011; p = .055). Finally, the extent of use of activation techniques did not significantly predict smoking at the following counseling session (OR = .804; 95% CI = .362; 1.784; p = .592). The results of the unadjusted model were consistent with the main model, but in this case, both openness (OR = .515; 95% CI = .31, .855; p = .01) and awareness (OR = .447; 95% CI = .27, .742; p = .002) reached statistical significance, and the activation component remained non-significant (OR = 1.129; 95% CI = .599, 2.13; p = .707). Figure 2 presents a summary of these findings and the results of the unadjusted model.
Figure 2.
Odds of not smoking by the next counseling session with and without adjusting for baseline smoking, cigarettes per day at the current counseling session, and number of counseling sessions.
Discussion
Process analyses of counselor-level behavior are rare in the cognitive behavioral literature, and no studies to date have examined the effect of counselor techniques on smoking cessation over the course of treatment. To address this gap, the study examined the degree to which specific ACT counseling techniques prospectively predicted smoking cessation at the subsequent counseling session. Mostly supporting our hypothesis, counselors’ use of awareness and openness (at a trend level) techniques prospectively predicted smoking cessation at the following counseling session. In contrast, activation techniques did not contribute significantly to the odds of being abstinent from smoking. Finally, the magnitude and direction of our estimates were robust to the adjustment of number of cigarettes smoked the prior week, baseline levels of smoking, and number of ACT counseling sessions. The persistence of these predictive patterns reflects on the importance of the counselor-level processes examined in this study.
This study is the first to investigate the direct role of key modifiable variables, such as the use of counseling techniques, on smoking cessation during the course of treatment. Previous studies only targeted the content of participants’ statements (e.g., Amrhein et al., 2003) or the effect of therapists’ techniques on clients’ statements (e.g., Boardman et al., 2006). In addition, this study builds upon the results of a previous study published in this journal (Hesser et al., 2009) by exploring the full range of processes of change proposed by the ACT model, and by prospectively focusing on a fine-grained analysis of counselor-level session-to-session components and participant outcomes. Furthermore, as discussed by others (Forman et al., 2012; Hesser et al., 2009), overreliance on global self-report measures to assess processes of change limits our ability to understand key factors responsible for behavior change, and therefore this study adds to the growing body of literature examining the role of adherence to counseling techniques in behavior change processes and outcomes (e.g., Amrhein et al., 2003; Calero-Elvira et al., in press; Tollison et al., 2013). Lastly, the fact that the study population consisted of a sample of uninsured and low socio-economic status individuals shows the promise of ACT counseling techniques in predicting smoking cessation in a challenging treatment population.
The lack of a predictive relationship between activation and smoking might be explained by a number of possibilities. First, a low range of activation techniques in ACT could have led to consistently high adherence ratings and lack of variability in this component. For example, if commitment was conceptualized as simply encouraging participants to take specific steps towards values-driven behaviors, this could easily lead to high ratings in this category. However, values-driven behaviors can be promoted in a variety of ways, such as creating a hierarchy of actions consistent with patient’s values, or the application of principles of behavior change to promote successive approximations towards those values-driven behaviors. This possibility needs to be further examined in future studies, since our adherence rating scale did not take into account those counselor behaviors. Second, although not part of our initial hypothesis, a possible interpretation is that activation techniques are more likely to succeed when awareness and openness skills have already been established, since those skills could be helping individuals to cope effectively with the discomfort of being put in contact with their own personal values and the discrepancy between their values and actions; a process suggested by recent Relational Frame Theory research (Hooper, Stewart, Duffy, Freegard, & McHugh, 2012). Finally, while there is an increasing number of ACT studies examining the important role of activation in individual’s functioning (e.g., Chase et al., 2013; Kashdan & McKnight, 2013), there is still a small number addressing the role of values and commitment as compared to other ACT processes (Levin, Hildebrandt, Lillis, & Hayes, 2012). Thus, these non-significant findings should motivate further study of activation — a central process of the ACT model.
The study has key limitations. First, and as discussed earlier, the restricted range of the activation component had an impact on the reliability of the regression estimates and their interpretation. Second, we cannot rule out the possibility that a third, unmeasured variable, both influenced the use of counselor techniques and smoking cessation outcomes, thereby leading to potentially inflating the observed association between counseling techniques and smoking outcomes. Possible examples of third variables include participants’ self-efficacy and/or intention to reduce smoking the following week. Both variables might lead to greater engagement with ACT techniques following and ACT counseling session and to higher likelihood of quitting before the following session, raising the question of to what extent counselor behaviors had a causal influence on participants’ smoking behavior. Third, although the aim of this study was to examine the effect of manipulable variables (i.e., ACT counseling techniques) on treatment outcomes, statistical power limited alternative analytic strategies, such as the analysis of moderating or mediating variables. One such variable could have been participants’ willingness to experience smoking urges and cravings in response to the ACT intervention. In addition, the use of openness, awareness and activation techniques could be driven by participants’ responses to such techniques in prior sessions. Future studies with more statistical power might consider examining these associations or the identification of alternative variables influencing the outcomes. Fourth, coding openness, awareness and activation components in the non-ACT arm of this randomized controlled trial would have shed light into the use of these treatment components in standard telephone quitline counseling. However, coding standard telephone quitline counseling was not possible for security reasons, since state quitline call recordings are only kept on file for 30 days as part of their operating procedures. Fifth, this observational design was limited by the lack of experimental manipulation of independent variables. This lack of experimental manipulation limits the interpretation of the time effects inherent in our intervention. Our model indicated that adjusting for prior exposure to these ACT components (i.e., counseling calls) did not change the pattern of relationships observed in the unadjusted models. However, adjusting to number of calls does not inform about the role of specific ordering of effects. A more rigid treatment protocol could have helped us understand these effects, but it would have also limited its “real-world” clinical utility. Future research might consider alternative methodological strategies that can address these questions more directly, such as dismantling studies, single case designs (Hayes, 1981), SMART designs (in which specific ACT components are switched and their effects observed in the following sessions; Collins, Murphy, & Strecher, 2007), or the use of moderated-mediation process analyses in larger samples.
Tobacco addiction is a serious public health problem that calls for the development of more effective behavioral interventions. A better understanding of the processes of change of behavioral smoking cessation treatments helps meet this need. This study provided a prospective evaluation of the effects of manipulable treatment components and adjusted for important covariates, such as number of cigarettes smoked during the previous counseling session, baseline level of smoking, and counseling calls. This is the first study to suggest that a counselor’s focus on ACT’s openness and awareness processes has the potential to improve the effectiveness of behavioral interventions for smoking cessation. Overall, results hightlight the theoretical and clinical value of examining therapists’ techniques as predictors of outcomes during the course of treatment.
No studies have examined the effect of counselor techniques on smoking outcomes
ACT openness and awareness techniques predict smoking cessation
Examining counselor-level processes has important theoretical and clinical value
Acknowledgment
This study was, supported by the National Institutes of Health (T32MH082709 to RV, K23DA026517 to, JLH, R21DA030646 to JB) and the Fred Hutchinson Cancer Research Center
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Roger Vilardaga, University of Washington & Fred Hutchinson Cancer Research Center
Jaimee L. Heffner, Fred Hutchinson Cancer Research Center
Laina D. Mercer, Fred Hutchinson Cancer Research Center & University of Washington
Jonathan Bricker, Fred Hutchinson Cancer Research Center & University of Washington
References
- Aharonovich E, Amrhein PC, Bisaga A, Nunes EV, Hasin DS. Cognition, commitment language, and behavioral change among cocaine-dependent patients. Psychology of Addictive Behaviors. 2008;22(4):557. doi: 10.1037/a0012971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. Journal of consulting and clinical psychology. 2003;71(5):862. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- Austin PC, Manca A, Zwarenstein M, Juurlink DN, Stanbrook MB. A substantial and confusing variation exists in handling of baseline covariates in randomized controlled trials: a review of trials published in leading medical journals. Journal of clinical epidemiology. 2010 Feb;63(2):142–153. doi: 10.1016/j.jclinepi.2009.06.002. (PMID: 19716262) [DOI] [PubMed] [Google Scholar]
- Bach P, Hayes SC. The use of acceptance and commitment therapy to prevent the rehospitalization of psychotic patients: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2002;70(5):1129–1139. doi: 10.1037//0022-006x.70.5.1129. PMID:12362963. [DOI] [PubMed] [Google Scholar]
- Bates D, Maechler M, Bolker B. lme4: Linear mixed-effects models using s4 classes. r package version 0.999375-42. 2011 Retrieved from http://CRAN.R-project.org/package=lme4. [Google Scholar]
- Boardman T, Catley D, Grobe JE, Little TD, Ahluwalia JS. Using motivational interviewing with smokers: Do therapist behaviors relate to engagement and therapeutic alliance? Journal of substance abuse treatment. 2006;31(4):329–339. doi: 10.1016/j.jsat.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Bolt DM, Piper ME, Theobald WE, Baker TB. Why Two Smoking Cessation Agents Work Better Than One: Role of Craving Suppression. Journal of Consulting and Clinical Psychology. 2012;80(1):54–65. doi: 10.1037/a0026366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bricker JB, Bush T, Zbikowski SM, Mercer LD, Heffner JL. In 20th Annual Meeting of the Society for Research on Nicotine and Tobacco. Seattle, WA: 2014. Feb, Randomized trial of telephone-delivered acceptance and commitment therapy vs. cognitive behavioral therapy for smoking cessation: A pilot feasibility study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bricker JB, Hayes SC. Adherence raters’ manual for the "act now" telephone smoking cessation intervention. 2009 (Unpublished manuscript) [Google Scholar]
- Bricker JB, Liu J, Comstock BA, Peterson AV, Kealey KA, Marek PM. Social cognitive mediators of adolescent smoking cessation: results from a large randomized intervention trial. Psychology of addictive behaviors: journal of the Society of Psychologists in Addictive Behaviors. 2010 Sep;24(3):436–445. doi: 10.1037/a0019800. (PMID:20853929) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bricker JB, Mann SL, Marek PM, Liu J, Peterson AV. Telephone-delivered acceptance and commitment therapy for adult smoking cessation: a feasibility study. Nicotine & Tobacco Research. 2010;12(4):454–458. doi: 10.1093/ntr/ntq002. (PMID:20142417) [DOI] [PubMed] [Google Scholar]
- Bricker JB, Wyszynski C, Comstock B, Heffner JL. Pilot randomized controlled trial of web-based acceptance and commitment therapy for smoking cessation. Nicotine & Tobacco Research. 2013;ntt056 doi: 10.1093/ntr/ntt056. (PMID:23703730) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calero-Elvira A, Froján-Parga MX, Ruiz-Sancho EM, Alpañés-Freitag M. Descriptive study of the socratic method: Evidence for verbal shaping. Behavior Therapy. (in press). [Google Scholar]
- Catley D, Harris KJ, Mayo MS, Hall S, Okuyemi KS, Boardman T, Ahluwalia JS. Adherence to principles of motivational interviewing and client within-session behavior. Behavioural and Cognitive Psychotherapy. 2006;34(1):43. [Google Scholar]
- Chase JA, Houmanfar R, Hayes SC, Ward TA, Vilardaga JP, Follette V. Values are not just goals: Online ACT-based values training adds to goal setting in improving undergraduate college student performance. Journal of Contextual Behavioral Science. 2013;2(3âӐŞ4):79–84. [Google Scholar]
- Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994;6(4):284–290. [Google Scholar]
- Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. American journal of preventive medicine. 2007;32(5 Suppl):S112–S118. doi: 10.1016/j.amepre.2007.01.022. (PMID:17466815 PMCID: PMC2062525) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore M, Jaén C, Baker T. Treating tobacco use and dependence: 2008 update U.S. public health service clinical practice guideline executive summary. Respiratory care. 2008;53(9):1217–1222. (PMID:18807274) [PubMed] [Google Scholar]
- Forman EM, Chapman JE, Herbert JD, Goetter EM, Yuen EK, Moitra E. Using session-by-session measurement to compare mechanisms of action for acceptance and commitment therapy and cognitive therapy. Behavior Therapy. 2012;43(2):341–354. doi: 10.1016/j.beth.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical models. Cambridge; New York: Cambridge University Press; 2007. [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Antonuccio DO, Piasecki MM, Rasmussen-Hall ML, Palm KM. Acceptance-based treatment for smoking cessation. Behavior Therapy. 2004;35(4):689–705. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Pierson HM, Piasecki MP, Antonuccio DO, Palm KM. Does acceptance and relationship focused behavior therapy contribute to bupropion outcomes? a randomized controlled trial of functional analytic psychotherapy and acceptance and commitment therapy for smoking cessation. Behavior therapy. 2011;42(4):700–715. doi: 10.1016/j.beth.2011.03.002. (PMID:22035998) [DOI] [PubMed] [Google Scholar]
- Glynn LH, Moyers TB. Chasing change talk: The clinician’s role in evoking client language about change. Journal of substance abuse treatment. 2010;39(1):65–70. doi: 10.1016/j.jsat.2010.03.012. [DOI] [PubMed] [Google Scholar]
- Hatsukami DK, Stead LF, Gupta PC. Tobacco addiction. Lancet. 2008;371(9629):2027–2038. doi: 10.1016/S0140-6736(08)60871-5. (PMID:18555914) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC. Single case experimental design and empirical clinical practice. Journal of Consulting and Clinical Psychology. 1981 Apr;49(2):193–211. doi: 10.1037//0022-006x.49.2.193. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy, second edition: The process and practice of mindful change. New York, NY, USA: Guilford Press; 2011. [Google Scholar]
- Hayes SC, Villatte M, Levin M, Hildebrandt M. Open, aware, and active: Contextual approaches as an emerging trend in the behavioral and cognitive therapies. Annual Review of Clinical Psychology. 2011;7(1):141–168. doi: 10.1146/annurev-clinpsy-032210-104449. (PMID:21219193) [DOI] [PubMed] [Google Scholar]
- Hesser H, Westin V, Hayes SC, Andersson G. Clients? in-session acceptance and cognitive defusion behaviors in acceptance-based treatment of tinnitus distress. Behaviour research and therapy. 2009;47(6):523–528. doi: 10.1016/j.brat.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Ching LE, McEwen J. Strength of commitment language in motivational interviewing and gambling outcomes. Psychology of Addictive Behaviors. 2009;23(1):122. doi: 10.1037/a0013010. [DOI] [PubMed] [Google Scholar]
- Hooper N, Stewart I, Duffy C, Freegard G, McHugh L. Modelling the direct and indirect effects of thought suppression on personal choice. Journal of Contextual Behavioral Science. 2012;1(1–2):73–82. [Google Scholar]
- Kashdan TB, McKnight PE. Commitment to a purpose in life: An antidote to the suffering by individuals with social anxiety disorder. Emotion. 2013 doi: 10.1037/a0033278. (PMID:23795592) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. The Cochrane database of systematic reviews. 2005;(2):CD001292. doi: 10.1002/14651858.CD001292.pub2. (PMID:15846616) [DOI] [PubMed] [Google Scholar]
- Levin ME, Hildebrandt MJ, Lillis J, Hayes SC. The impact of treatment components suggested by the psychological flexibility model: A meta-analysis of laboratory-based component studies. Behavior Therapy. 2012;43(4):741–756. doi: 10.1016/j.beth.2012.05.003. doi: http://dx.doi.org/10.1016/j.beth.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 2009;37(1):58–69. doi: 10.1007/s12160-009-9083-x. (PMID:19252962) [DOI] [PubMed] [Google Scholar]
- Lumley T. rmeta: Meta-analysis [Computer software manual] 2012 Retrieved from http://CRAN.R-project.org/package=rmeta (R package version 2.16) [Google Scholar]
- Luoma JB, Kohlenberg BS, Hayes SC, Fletcher L. Slow and steady wins the race: A randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. Journal of Consulting and Clinical Psychology. 2012;80(1):43–53. doi: 10.1037/a0026070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackay J, Eriksen M, Shafey O. The tobacco atlas (2nd ed) American Cancer Society. 2006 [Google Scholar]
- McCambridge J, Day M, Thomas BA, Strang J. Fidelity to motivational interviewing and subsequent cannabis cessation among adolescents. Addictive behaviors. 2011;36(7):749–754. doi: 10.1016/j.addbeh.2011.03.002. (PMID 21440994) [DOI] [PubMed] [Google Scholar]
- McCarthy DE, Piasecki TM, Jorenby DE, Lawrence DL, Shiffman S, Baker TB. A multi-level analysis of non-significant counseling effects in a randomized smoking cessation trial. Addiction. 2010 Dec;105(12):2195–2208. doi: 10.1111/j.1360-0443.2010.03089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy DE, Piasecki TM, Lawrence DL, Jorenby DE, Shiffman S, Baker TB. Psychological mediators of bupropion sustained-release treatment for smoking cessation. Addiction. 2008;103(9):1521–1533. doi: 10.1111/j.1360-0443.2008.02275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mottillo S, Filion KB, Bélisle P, Joseph L, Gervais A, O’Loughlin J, Eisenberg MJ. Behavioural interventions for smoking cessation: a meta-analysis of randomized controlled trials. European heart journal. 2009;30(6):718–730. doi: 10.1093/eurheartj/ehn552. (PMID:19109354) [DOI] [PubMed] [Google Scholar]
- Murphy R, Cooper Z, Hollon SD, Fairburn CG. How do psychological treatments work? investigating mediators of change. Behaviour Research and Therapy. 2009;47(1):1–5. doi: 10.1016/j.brat.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. American journal of public health. 1994;84(7):1086–1093. doi: 10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul G. Behavior modification research: Design and tactics. In: Franks CM, editor. Behavior therapy: Appraisal and status. Oxford: McGraw-Hill; 1969. pp. 29–62. [Google Scholar]
- R Core Team. Vienna, Austria: 2013. R: A language and environment for statistical computing [Computer software manual] Retrieved from http://www.R-project.org/ [Google Scholar]
- Schimmel-Bristow A, Bricker JB, Comstock B. Can acceptance & commitment therapy be delivered with fidelity as a brief telephone-intervention? Addictive behaviors. 2012;37(4):517–520. doi: 10.1016/j.addbeh.2011.11.015. (PMID:22192865) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Stead LF, Hartmann-Boyce J, Perera R, Lancaster T. Telephone counselling for smoking cessation. The Cochrane database of systematic reviews. 2013;8:CD002850. doi: 10.1002/14651858.CD002850.pub3. (PMID:23934971) [DOI] [PubMed] [Google Scholar]
- Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. The Cochrane database of systematic reviews. 2005;(2):CD001007. doi: 10.1002/14651858.CD001007.pub2. (PMID:15846610) [DOI] [PubMed] [Google Scholar]
- Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. The Cochrane database of systematic reviews. 2006;(3):CD002850. doi: 10.1002/14651858.CD002850.pub2. (PMID:16855992) [DOI] [PubMed] [Google Scholar]
- Tollison SJ, Mastroleo NR, Mallett KA, Witkiewitz K, Lee CM, Ray AE, Larimer ME. The relationship between baseline drinking status, peer motivational interviewing microskills, and drinking outcomes in a brief alcohol intervention for matriculating college students: a replication. Behavior therapy. 2013;44(1):137–151. doi: 10.1016/j.beth.2012.09.002. (PMID:23312433) [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services. The health consequences of smoking-50 years of progress: A report of the surgeon general. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014. Retrieved 2014-02-25, from http://www.ncbi.nlm.nih.gov/books/NBK179276/ (PMID:24455788) [Google Scholar]
- Wickham H. ggplot2: elegant graphics for data analysis. Springer New York: 2009. Retrieved from http://had.co.nz/ggplot2/book. [Google Scholar]