Abstract
Objective
Maternal depression is prevalent and has been associated with parenting practices that influence child weight. In this systematic review we aimed to examine the prospective association between maternal depression and child overweight.
Methods
We searched four databases (PsycINFO, PubMed, Embase, and Academic Search Premier) to identify studies for inclusion. We included studies with a prospective design with at least one year follow-up, measuring maternal depression at any stage after childbirth, and examining child overweight or obesity status, BMI z-score or percentile, or adiposity. Two authors extracted data independently and findings were qualitatively synthesized.
Results
We identified nine prospective studies for inclusion. Results were examined separately for episodic depression (depression at a single measurement occasion) and chronic depression (depression on multiple measurement occasions). Mixed results were observed for the relationship between episodic depression and indicators of child adiposity. Chronic depression, but not episodic depression, was associated with greater risk for child overweight.
Conclusions
While chronic depression may be associated with child overweight, further research is needed. Research is also needed to determine whether maternal depression influences child weight outcomes in adolescence and to investigate elements of the family ecology that may moderate the effect of maternal depression on child overweight.
Keywords: maternal depression, childhood obesity, systematic review
1. Introduction
Parents play an important role in determining child healthy lifestyles and are an important agent of change for child healthy weight (Golan and Crow, 2004). A range of parenting practices during infancy, childhood, and adolescence have been implicated in child weight development, including breastfeeding, early introduction of solid foods, physical activity parenting, screen-related parenting, and parental feeding practices (Edwardson and Gorely, 2010; Hoyos Cillero and Jago, 2010; Loprinzi et al., 2012; Rodgers et al., 2013; Sallis et al., 2000; Van der Horst et al., 2007; Weng et al., 2012). While parenting practices influence children’s diet and physical activity behaviors, and in turn child obesity risk, little is known about the broader factors that can affect parenting and subsequently child behavioral and weight outcomes.
Theoretical models of child weight development in the obeseogenic environment of high-income countries have proposed that a range of individual, family and community contextual factors influence parenting practices in this area. Such factors include parental preferences, knowledge and beliefs, family social support, chronic stress, resource shortfalls, and neighborhood social capital (Davison et al., 2012; Loprinzi et al., 2012). While the factors that influence parenting for child healthy weight are many and varied (Davison et al., 2012), parent mental health - and in particular maternal depression - may be one important element of the family ecology to consider as maternal depression has long been linked to parenting behaviors (Lovejoy et al., 2000).
Understanding the role of maternal depression in child weight development is particularly important given the prevalence of depression in both the postnatal period and beyond. A meta-analysis has estimated that up to 19% of women in developed countries experience an episode of depression in the three-month postnatal period (Gavin et al., 2005). In the 2001–2002 National Epidemiologic Survey of Alcohol and Related Conditions, approximately 10% of mothers of children <18 years of age experienced a major depressive disorder in the prior 12 month period (Ertel et al., 2011). Maternal depressive symptoms, such as negative affect and inactivity, may directly impact parenting for child healthy weight. Postnatal depression is associated with infant feeding practices, including earlier cessation of breastfeeding (Dennis and McQueen, 2009). In older children, parent depressive symptoms have been associated with physical activity parenting in low-income families (Lampard et al., 2013) and maternal depressive symptoms have been associated with increased child television viewing (Burdette et al., 2003; Conners et al., 2007; Hoyos Cillero and Jago, 2010) and lower child physical activity (Fernald et al., 2008). Despite the prevalence of maternal depression and its association with child health behaviors, its role in childhood obesity has yet to be adequately understood.
Two recent systematic reviews have investigated the relationship between perinatal depression, including depression during pregnancy and the postnatal period, and childhood obesity (Milgrom et al., 2012; Weng et al., 2012). In the most comprehensive review, three out of five studies documented a positive relationship between perinatal depression and child weight outcomes (including overall adiposity, central adiposity, overweight and obesity) between age 0 and 8 years (Milgrom et al., 2012).
As both review articles solely examined perinatal depression it is important to widen the scope of investigation to include maternal depression across the span of child development. Exposure to maternal depression at earlier and later stages of child development may be differentially associated with child weight outcomes and act via different mechanisms. Postnatal depression may influence child weight through earlier cessation of breastfeeding, impaired mother-infant feeding interactions and child feeding problems (Ertel et al., 2010). In contrast, maternal depression at later child developmental stages may influence child adiposity through parenting practices related to physical activity, food choices available in the home, and screen-related behavior. It is therefore important to examine the relationship between maternal depressive symptoms and child overweight across all child developmental stages.
Examining maternal depression across all child ages, we aimed to systematically review prospective studies to identify the association between maternal depression or depressive symptoms on excess child growth (aged 2 to 18 years), including child overweight or obesity status, BMI z-score or percentile, or alternative indicators of adiposity. We considered variation in this relationship across studies based on the timing of exposure to maternal depression, the age at which child weight outcomes were measured, the type of weight outcome examined, and income. We examined results separately for episodic depression (i.e., depression at a single point in time) and chronic depression (i.e., depression on multiple occasions). Our secondary aim was to identify evidence gaps and directions for future research to advance understanding of the role of maternal depression in childhood obesity.
2. Methods
This systematic review followed the reporting guidelines in the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (Moher et al., 2009).
Search strategy
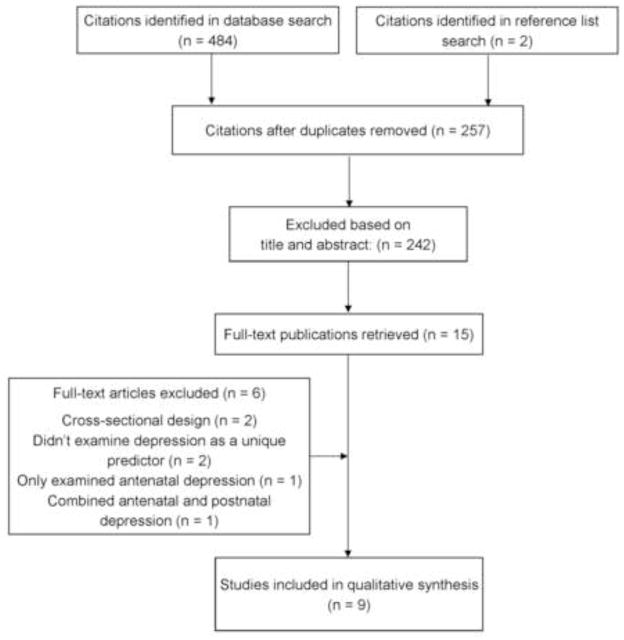
We searched four relevant databases (PsycINFO, PubMed, Embase, and Academic Search Premier) to identify eligible studies (last search on 2 January 2013). The following string of search terms were used in the database search: [(“maternal depression” OR “maternal depressive symptoms” OR “mother’s depression” OR “mother’s depressive symptoms” OR “parent depression” OR “parent depressive symptoms” OR “maternal postpartum depression” OR “maternal postpartum depressive symptoms” OR “maternal postnatal depression” OR “maternal postnatal depressive symptoms”) AND (child OR adolescent OR youth) AND (weight OR overweight OR obesity OR “body mass index” OR adiposity)]. To identify additional studies, we searched the reference lists of relevant review articles and research studies. We identified two hundred and fifty seven unique citations. Two authors independently examined the titles and abstracts of all citations. We excluded citations when both authors identified that the study did not meet inclusion criteria (n = 242). We retrieved the full-text articles of retained citations (n = 15) and two authors independently examined the full-text articles to identify studies that satisfied the inclusion criteria. Nine studies were included in the systematic review. The search strategy is illustrated in Figure 1.
Figure 1.
Literature search strategy
Study inclusion criteria
The scope of the review was limited to English language publications, published since 1980 with full text available. To qualify for inclusion, studies were required to: (i) report a quantitative analysis of the association between maternal depression or depressive symptoms (independent variable) and an indicator of excess child weight or adiposity (dependent variable), including overweight or obesity status, BMI z-score or percentile, or an alternative adiposity measure (e.g., skinfold thickness); (ii) measure maternal depression or depressive symptoms with a validated questionnaire at any period following childbirth; (iii) include children aged between 2 and 18 years at outcome assessment; and (iv) use a prospective study design with minimum one year follow-up.
Data extraction
Two authors independently pilot-tested a data extraction form on two studies, comparing extracted data and revising the form as necessary. Two authors then independently extracted data from all included studies and discrepancies in data extraction were reconciled between authors. Authors extracted the following data: study setting and population; study design; sample size; length of follow-up; measurement of exposure and outcome; and results.
Quality assessment of included studies
We examined study quality using the Newcastle-Ottawa Quality Assessment Scale for cohort studies (Wells et al., 1996) (see Appendix). This scale assesses the quality of nonrandomized studies across three domains, including the selection of exposed and non-exposed groups, the comparability of groups, and outcome assessment. Two authors independently rated study quality and discrepancies were reconciled between the authors. We used quality ratings to identify potential sources of bias and methodological areas that were poorly addressed in the included studies.
Appendix 1.
Quality review criteria for included studies based on the Newcastle-Ottawa Quality Assessment Scale for cohort studies
| Quality assessment items | Score |
|---|---|
| Selection (maximum score = 4) | |
| Representativeness of the exposed cohort | |
| Truly or somewhat representative of the average child in the community | 1 |
| Selected group of users or no description of the derivation of the cohort | 0 |
| Selection of the non-exposed cohort | |
| Drawn from the same community as the exposed cohort | 1 |
| Drawn from a different source or no description | 0 |
| Ascertainment of exposure | |
| Secure record, structured interview or administered questionnaire | 1 |
| Written self-report questionnaire or no description | 0 |
| Demonstration that the outcome was not present at the start of the study | |
| Yes | 1 |
| No | 0 |
| Comparability (maximum score = 2) | |
| Comparability of the cohorts on the basis of the design or analysis | |
| Study controls for essential confounding variables (SES indicator and maternal BMI) and additional relevant confounders | 2 |
| Study controls for some relevant confounding variables | 1 |
| Inadequate consideration of confounding variables | 0 |
| Outcome (maximum score = 3) | |
| Assessment of outcome | |
| Objective measurement of height and weight | 1 |
| Self-report or no description | 0 |
| Was follow-up long enough for outcomes to occur | |
| Yes | 1 |
| No | 0 |
| Adequacy of follow-up | |
| Complete follow-up or subjects lost to follow-up unlikely to introduce bias (small number lost or description provided of lost) | 1 |
| Inadequate follow-up rate or no description provided of those lost | 0 |
3. Results
Summary of included studies
Following the search strategy outlined in Figure 1, we identified nine prospective studies that examined the prospective association between maternal depression and child overweight (n = 6), obesity (n = 2), BMI z-score or percentile (n = 5), or alternative indicators of adiposity (n = 3). Studies were conducted in the US (n = 5), Denmark (n = 1), the Netherlands (n = 1), and Brazil (n = 1), and one study included multiple centers across Europe (n = 1). Three of the five US studies used data from the National Institute of Child Health and Human Development Study of Early Child Care and Youth Development. Only two studies examined sex-specific results.
Study location, design, population, sample size, measurement methods, and results are summarized for each included study in Table 1. In the following sections, results are synthesized based on the timing of exposure to maternal depression, the age at which child weight outcomes were measured, the type of weight outcome examined and family income status. This information is summarized in Table 2. All results pertain to episodic depression, with the exception of the subsection on chronic depression.
Table 1.
Characteristics of included studies
| First author; country; length of follow-up | Data source; sample size; sampling procedure | Maternal depression measure; operationalization; age at exposure | Child weight measure; operationalization; age at outcome | Main findings | Quality rating | ||
|---|---|---|---|---|---|---|---|
| Selection (max = 4) | Comparability (max = 2) | Outcome (max = 3) | |||||
|
Ajslev (2010) Denmark 7 year follow-up |
Danish National Birth Cohort N = 21121 Nationally representative |
3 items from the SCL-90 and GHQ Depressive symptoms 6 months postpartum |
Maternal report of height and weight Child overweight and obesity status 7 years |
MD was not associated with child overweight status (OR = 1.02; 95% CI .96, 1.08) or obesity status Sex differences were not observed |
4 | 2 | 1 |
|
Duarte (2012) USA 5 year follow-up |
Early Childhood Longitudinal Study-Kindergarten N = 21260 Nationally representative |
Abbreviated 12-item CES-D Severe depression vs. no depression K and 3rd grade |
Objectively measured height and weight BMI z-score 1st, 3rd, and 5th grade and 5th grade. MD at 3rd grade did not predict BMI z-score at 5th grade |
Girls: MD at K predicted lower BMI z-score at 3rd grade (estimate = −.27, p = .01) and greater increase in BMI z-score from K to 5th grade (estimate = .09, p < .01), but not BMI z-score at 5th grade; MD at 3rd grade predicted greater BMI z-score at 5th grade (estimate = .22, p = .05) Boys: MD at K predicted greater BMI z-score at 5th grade (estimate = .24, p = .03), but not BMI z-score at 3rd, or increase between 1st |
3 | 1 | 3 |
|
Ertel (2010) USA 2.5 year follow-up |
Project Viva N = 838 Pregnant women attending one of 8 obstetric practices in Boston, MA |
EPDS Probable depression or not depressed 6 months postpartum |
Objectively measured subscapular (SS) and triceps (TR) skinfold thickness, height and weight Adiposity (SS + TR); central adiposity (SS: TR); weight-for-height z-score; child overweight 3 years |
MD was associated with higher overall adiposity of 1.14mm (95% CI .11, 2.18) MD did not predict child overweight (OR = .87; 95% CI .45, 1.67) MD was not associated with BMI z-score, central adiposity or weight-for-height z-score |
3 | 2 | 3 |
|
Ertel (2012) Netherlands 34 month follow-up |
Generation R N = 6782 Population-based sampling of pregnant women living in Rotterdam with a delivery date between April 2002 and January 2006 |
BSI Depressive symptoms 2 and 6 months postpartum |
Objectively measured child height and weight BMI z-score; child overweight; child obesity 36 months |
Complete case analysis: MD at 2 months (β = .27; 95% CI = .08, .45) but not 6 months (β = .11; 95% CI = −.09, .30). predicted BMI z-score Multiple imputation analysis: Neither MD at 2 months (β = .10; 95% CI = −.07, .27) nor 6 months (β = .05; 95% CI = −.13, .22) predicted BMI z-score MD did not predict child overweight or obesity |
3 | 2 | 3 |
|
Grote (2010) Europe (Belgium, Germany, Italy, Poland, Spain) 2 year follow-up |
Multicenter study (11 sites) N = 1678 Infants born between October 2002 and July 2004 |
EPDS Depressed at any measurement occasion or not depressed 2, 3, and 6 months postpartum |
Objectively measured height, weight, TR and SS skinfold thickness BMI-for-age z-score; weight-for-length z-score; SS-for-age z-score; TR-for-age z-score 2 years |
BMI-for-age, weight-for-length, TR, and SS z-scores did not differ between children exposed vs not exposed to MD | 2 | 2 | 2 |
|
Lane (2013) USA 12 year follow-up |
National Institute of Child Health and Human Development Study of Early Child Care and Youth Development N = 1238 Children born at 10 hospital sites across the US in 1991; Conditional random sampling to ensure diverse study population |
CES-D Depressed or not depressed 1 month postpartum |
Objectively measured height and weight BMI percentile 24, 36, and 54 months, 1st, 3rd, 5th, and 6th grade |
MD status did not predict latent class membership (stable, steady increase, or elevated BMI percentile) MD did not predict the rate of change in BMI percentile in any latent class |
2 | 1 | 2 |
|
O’Brien (2007) USA 12 year follow-up |
National Institute of Child Health and Human Development Study of Early Child Care and Youth Development N = 1364 Children born at 10 hospital sites across the US in 1991; Conditional random sampling to ensure diverse study population |
CES-D Depressive symptoms 6, 15, 24, 36, and 54 months, 1st, 3rd, 5th and 6th grade |
Objectively measured height and weight Growth group membership based on child overweight 24, 36, and 54 months, 1st, 3rd, 5th, and 6th grade |
Five growth groups were identified (never overweight, preschool overweight, elementary overweight, and return to normal weight) MD symptoms did not differ between growth groups MD did not predict growth group membership |
3 | 1 | 2 |
|
Santos (2010) Brazil 3 year follow-up |
Prospective cohort N = 4287 All hospital births from mothers living in the city of Pelotas, from January 2004 to December 2004 |
EPDS Never depressed, depressed 1–2 occasions, or depressed 3 occasions 12, 24, and 48 months postpartum |
Objectively measured height and weight Overweight status; weight for height z-score 48 months |
MD on 1–2 occasions did not predict overweight relative to no depression (OR = 1.0; 95% CI = .8–1.3) MD on 3 occasions was marginally associated with overweight relative to no depression (OR = 1.6; 95% CI 1.0, 2.5) Non-significant linear trend for depression chronicity (p = .210) The interaction between MD and income predicting child overweight was not significant MD was not associated with weight-for-height z-score |
3 | 2 | 2 |
|
Wang (2013) USA 12 year follow-up |
National Institute of Child Health and Human Development Study of Early Child Care and Youth Development N = 1090 Children born at 10 hospital sites across the US in 1991 |
CES-D Depressed or not depressed; Number of occurrences of depression (0, 1, 2, or 3) 1, 24, and 36 months postpartum |
Objectively measured height and weight Child overweight status 1st, 3rd, and 5th grade |
3 occasions of MD predicted greater risk of overweight than no MD (OR = 2.13; 95% CI 1.05, 4.31) MD at 1, 24, or 36 months did not predict overweight at grade 1, 3 or 6 |
3 | 1 | 3 |
BMI, Body Mass Index; CES-D, Center for Epidemiological Studies Depression Scale; BSI, Brief Symptom Inventory; EPDS, Edinburgh Postpartum Depression Scale; GHQ, General Health Questionnaire; MINI, Mini International Neuropsychiatric Interview; SCL-90, Symptom Distress Checklist; MD, maternal depression; OR, odds ratio
Table 2.
Summary of observed associations between exposure to maternal depression and child weight outcomes
| Attribute | Positive association | Null or negative association |
|---|---|---|
| Child age: maternal depression exposure | ||
| Infancy (<6 months) | 3, 4 | 1, 5, 9* |
| Preschool or middle childhood | 2 | 9* |
| Child age: weight outcome assessment | ||
| Preschool (2 to 5 years) | 3, 4 | 5 |
| Middle childhood | 2, 9* | 1 |
| Growth patterns across childhood | - | 6*, 7* |
| Weight outcome measure | ||
| Overweight or obesity | 9* (chronic depression) | 9* (episodic depression) 1, 3, 4, 7*, 8 |
| BMI z-score or percentile | 2 (mixed associations) 4 (mixed associations) |
2 (mixed associations) 4 (mixed associations) 3, 5, 6* |
| Alternative indicators | 3 (overall adiposity) | 3 (central adiposity, weight-for-height z-score) 5 (weight-for-length z-score, SS skinfold thickness z-score, TR skinfold thickness z-score) 8 (weight-for-height z-score) |
| Chronicity of maternal depression | ||
| Chronicity | 9* | 8 (marginal significance) |
| Country | ||
| US | 2, 3, 9* | 6*, 7* |
| Non-US | 4 | 1, 5, 8 |
1, Ajslev et al. (2010); 2, Duarte et al. (2012); 3, Ertel et al. (2010); 4, Ertel et al. (2012); 5, Grote et al. (2010); 6, Lane et al. (2013); 7, O’Brien et al. (2007); 8, Santos et al. (2010); 9, Wang et al. (2013);
studies used data from the same cohort (National Institute of Child Health and Human Development Study of Early Child Care and Youth Development)
Does the developmental period at which children are exposed to maternal depression influence the association with child weight?
Maternal depression was predominantly measured in the first 6 months following childbirth (n = 6), but was also examined as a unique predictor later in childhood in two studies. In addition, three studies combined exposure across developmental periods (1, 24, and 36 months of age; 12, 24, and 36 months; and 6 months to 6th grade). Notably, maternal depression was not examined as a unique predictor past 3rd grade. Within this restricted range, the timing of the measurement of maternal depression did not appear to influence results.
Up to 6 months postpartum
Both positive (Ertel et al., 2012; Ertel et al., 2010) and null (Ajslev et al., 2010; Ertel et al., 2012; Ertel et al., 2010; Grote et al., 2010; Lane et al., 2013; Wang et al., 2013) associations were observed between maternal depression in the first 6 months of life and child weight outcomes. In a US sample, Ertel et al. (2010) observed that children exposed to maternal depression had greater overall adiposity (sum of subscapular skinfold and triceps skinfold thickness) of 1.14mm, but not BMI z-score, central adiposity, or risk for overweight, compared to those not exposed to maternal depression. In a sample of Dutch children, Ertel et al. (2012) found that maternal depressive symptoms at 2 months but not 6 months postpartum were associated with greater child BMI z-score, but not child overweight or obesity. While this positive association was observed in complete-case analysis, this effect was not observed when multiple-imputation methods were employed. The remaining studies failed to find an association between postpartum maternal depression and child weight outcomes, including child overweight (Ajslev et al., 2010; Wang et al., 2013), obesity (Ajslev et al., 2010), growth in child BMI percentile (Lane et al., 2013), or weight-for-length, triceps skinfold thickness, and subscapular skinfold thickness z-score (Grote et al., 2010).
Preschool or middle childhood
Similarly, positive (Duarte et al., 2012) and null (Wang et al., 2013) associations were observed between later measurements of maternal depression and child weight outcomes. Duarte et al. (2012) observed sex-specific results for the association between severe maternal depressive symptoms and child BMI z-score. Maternal depression at kindergarten was associated with greater BMI z-score at 5th grade for boys but not girls. Conversely, maternal depression at 3rd grade was associated with greater BMI z-score at 5th grade for girls but not boys. A negative association was also observed, whereby maternal depression at kindergarten was associated with lower BMI z-score in girls at 3rd grade. In contrast, Wang et al. (2013) did not observe an association between episodic maternal depression at 24 months or 36 months and risk for child overweight.
Does child age at weight outcome measurement influence the association between episodic maternal depression and child weight?
Child weight outcomes were examined during preschool years (n = 3) and middle childhood (n = 3). In addition, two studies examined growth patterns between ages 2 and 12 years. No studies examined the association between maternal depression and child weight outcomes in later adolescence (i.e., between the ages of 12 and 18 years).
Preschool years (age 2 to 5 years)
Three studies examined the association between episodic depression and weight outcomes among preschool-aged children. Two of these studies identified a positive association between maternal depression and child adiposity or BMI z-score (Ertel et al., 2012; Ertel et al., 2010). The remaining study did not observe an association between maternal depression and child weight outcomes (Grote et al., 2010).
Middle childhood
Three studies examined child weight outcomes in middle childhood (age 7 to 12 years). One of these studies observed a positive association between maternal depression and BMI z-score (Duarte et al., 2012). The two remaining studies did not observe a positive association between episodic maternal depression and child overweight (Ajslev et al., 2010; Wang et al., 2013).
Growth patterns from preschool years to middle childhood
Two studies examined the association between maternal depression and child growth patterns between the ages of 2 and 12 years using data from the National Institute of Child Health and Human Development Study of Early Child Care and Youth Development. Neither study identified an association between maternal depression and child growth. O’Brien et al. (2007) identified groups based on the patterns of transitioning into and out of child overweight status between age 2 and 12 years. Maternal depression did not predict group membership (“never overweight”, “ever overweight”, “preschool overweight”, or “elementary overweight”). Lane et al. (2013) examined change in child BMI percentile between age 2 and 12 years, identifying three distinct classes of BMI percentile growth. Maternal depression did not predict whether a child was a member of the “stable”, “steady increase”, or “elevated” growth class. In addition, maternal depression was not associated with the rate of change in child BMI percentile within each growth pattern.
Does the chronicity of maternal depression influence the association between maternal depression and child weight outcomes?
While results up to this point have examined episodic depression, two studies examined the relationship between chronic maternal depression and child outcomes. Wang et al. (2013) observed an effect for chronicity, finding that maternal depression on three occasions was associated with a twofold increase in risk for child overweight status relative to no maternal depression; one or two occurrences of maternal depression did not exhibit this association. Similarly, Santos et al. (2010) found that maternal depression at three occasions was associated with greater child risk for overweight with marginal significance (OR = 1.6, 95% CI = 1.0, 2.5), relative to no depression.
Is maternal depression differentially associated with alternative indicators of child weight outcome?
Three studies examined the association between maternal depression and BMI z-score (Duarte et al., 2012; Ertel et al., 2012; Ertel et al., 2010). A positive association was observed in two of these studies (Duarte et al., 2012; Ertel et al., 2012). Six studies examined the association between maternal depression and child overweight (n = 6) or obesity (n = 2) (Ajslev et al., 2010; Ertel et al., 2012; Ertel et al., 2010; O’Brien et al., 2007; Santos et al., 2010; Wang et al., 2013). None of these studies observed a positive association with episodic depression, but Wang et al. observed a positive association between chronic depression and child overweight. Alternative adiposity and anthropometric indices were also examined. A positive association was observed for overall adiposity (Ertel et al., 2010), but not central adiposity (Ertel et al., 2010), weight-for-height z-score (Santos et al., 2010), weight-for-length z-score (Grote et al., 2010), subscapular skinfold thickness z-score (Grote et al., 2010), or triceps skinfold thickness z-score (Grote et al., 2010).
Does family income influence the association between maternal depression and child anthropometric outcomes?
Only two studies examined family income as a moderator of the relationship between maternal depression and child weight outcomes. Ertel et al. (2012) did not observe an interaction between income and maternal depression predicting child BMI z-score at age 36 months. Similarly, Santos et al. (2010) found that family income did not interact with maternal depression predicting child overweight at age 4 years. As both studies measured maternal depression exposure early in child life, it has yet to be tested whether income moderates the effect of maternal depression on child weight at later child developmental periods, including middle childhood and later adolescence.
Quality assessment of included studies
Selection of groups
Across included studies, the ascertainment of exposure to maternal depression was generally weak. Five studies relied on self-report measures and the remaining studies administered questionnaires via interview. No studies utilized a structured diagnostic interview, which is the gold standard for assessing clinical depression. For example, the most commonly used instrument was the Center for Epidemiological Studies – Depression (CES-D) scale. In a sample of US adults the CES-D has shown a predictive value of 15% for current major depression ascertained by structured diagnostic interview (specificity = 73%; sensitivity = 87.5%) (Breslau, 1985).
Comparability of exposed and non-exposed groups
Socio-economic status, maternal BMI, and ethnicity are key confounding variables in the association between maternal depression and child weight status. All studies controlled for at least one indicator of socio-economic status (income, maternal education or a combined indicator of socio-economic status). However, four studies did not adjust for maternal BMI and three studies did not adjust for maternal race. Of these three studies, one was conducted in the US (Lane et al., 2013), and it is likely that race is a particularly relevant confounding variable in US samples. All studies controlled for some relevant confounding variables and seven studies extensively controlled for relevant confounding variables, including maternal age, smoking, parity, gestational weight gain, paternal BMI, child sex, gestational age at birth, and marital status.
Outcome assessment
Methods for measuring child weight outcomes were of good quality; only one study relied on maternal self-report of child height and weight. The length of study follow-up was adequate, ranging from 1 to 12 years. The greatest potential source of bias in outcome assessment was related to the adequacy of the retention of the cohorts. Five studies reported inadequate retention of participants or failed to adequately describe loss to follow-up.
4. Discussion
The primary aim of this systematic review was to determine whether maternal depression is associated with child overweight or adiposity. We identified nine studies that examined the prospective association between maternal depression and child weight outcomes. All six studies that tested the association between episodic maternal depression and risk for child overweight or obesity failed to observe an effect, indicating that episodic maternal depression is not associated with child overweight or obesity status. However, results from this review suggest that chronic depression may play an important role in child overweight. This finding is in line with theories linking maternal depression to child weight through parenting practices. If maternal depression influences child weight through parenting practices related to child diet, screen behaviors, and physical activity, then more prolonged depression will have a more prolonged impact on parent and child behavior, and therefore a greater likelihood of influencing child weight in the long-term. Episodic depression may not influence parenting practices in a sustained manner needed to influence child weight over time. As only two studies have examined the prospective effect of chronic maternal depression on child overweight, further research is needed in this area.
In relation to maternal depression and child BMI z-score or adiposity, there was heterogeneity in results. Three studies observed a positive association between episodic maternal depression and overall adiposity or greater BMI z-score. However, the remaining three studies failed to observe an association between maternal depression and BMI z-score or alternative indicators of child adiposity. Results did not systematically differ according to tested sources of heterogeneity, including the timing of the measurement of maternal depression or the timing of the measurement of child weight outcome. The inconsistent results indicate that there may be additional factors that modify the association between maternal depression and these child weight outcomes.
In evaluating the strength of the evidence in this review, it is important to consider the methodological quality of included studies. First, as maternal depression and child weight are both associated with a range of social, economic and ecological characteristics within families and neighborhoods, it is essential for studies to control for confounding variables in analyses in order to identify the unique contribution of maternal depression to child overweight. Importantly, the extent to which studies controlled for confounding variables did not systematically differ between those observing a positive or null association between maternal depression and child weight outcomes. The four studies that did observe a positive association used adequate controlling for confounding variables, with the exception that two of these studies did not control for maternal BMI.
Second, despite the importance of controlling for confounding variables, it is possible that some of the confounding factors controlled for in these studies may also lie on the causal pathway between maternal depression and child overweight. For example, two studies controlled for breastfeeding as a confounding variable, despite the possibility that a shorter duration of breastfeeding may mediate the association between maternal depression and child overweight. By controlling for certain factors as confounding variables, without considering their potential role as mediating variables, studies may have underestimated the association between maternal depression and child overweight.
Third, loss to follow-up and the presence of missing data are also important considerations. If chronic maternal depression is associated both with loss to follow-up and child weight status, studies may underestimate the association between maternal depression and child weight outcomes. A number of studies were limited by poor retention rates and inadequate description of those lost to follow-up. Related to this, there was some evidence to suggest that the method of dealing with missing data influenced results (e.g., Ertel et al., 2012). It is recommended that in future studies examining the relationship between maternal depression and child weight outcomes, researchers provide a more rigorous description of those participants lost to follow-up, consider the effect of attrition on study results, and thoughtfully apply appropriate methods for dealing with missing data.
Finally, in determining exposure to maternal depression, all studies employed self-report or administered questionnaires; no studies used instruments for the diagnosis of clinical depression. This method of ascertaining exposure is a problem to the extent that misclassification of depression exposure is related to child weight outcomes, which is unclear.
In line with the secondary aim of this study, we identified clear opportunities for future research to advance understanding in this area. Few studies have examined exposure to maternal depression in later periods of child development, beyond the postnatal period. There was also a notable gap in outcome assessment, whereby child weight outcomes were not examined past 12 years of age. Given that excess weight and adiposity accumulate over time, longer follow-up periods are necessary to fully assess the impact of maternal depression. There were also few studies examining sex differences in the role of maternal depression on child weight. Given that sex differences were observed in one study, and that maternal parenting practices can differ for girls and boys, this may be an important consideration for future research.
More broadly, the literature is lacking a strong theory to guide the assessment and timing of measurements, and the examination of mediating and moderating models. Two studies included in this review offer some analyses that pertain to possible mechanisms of the association between maternal depression and child weight. It has been proposed that earlier cessation of breastfeeding may be one mechanism that could explain a link between maternal depression and child overweight, since mothers with postnatal depression report a shorter duration of breastfeeding (Dennis and McQueen, 2009). One study in this review tested this hypothesis, and found that the observed association between postnatal depression and child adiposity was not mediated by breastfeeding duration or the early introduction of solid food (Ertel et al., 2010). It is also possible that maternal depression may influence child weight through its effect on parenting practices and child behavior related to feeding, screen-viewing, and physical activity. This hypothesis is partially supported by results from the Duarte et al. study, which found that, in boys, unhealthy eating habits at grade 5 mediated the relationship between maternal depression in kindergarten and greater BMI z-score at grade 5. However, further research is needed in this area to elucidate the mechanisms of the association between maternal depression and child weight outcomes.
In addition, while all studies controlled for maternal income, education, or socioeconomic status as a confounding variable, few studies examined the role of income or other indicators of social circumstance in modifying the association between maternal depression and child growth. This is an important oversight, as maternal depression might have a stronger effect on child weight in families with fewer resources and limited access to services. For example, maternal depression may be more strongly associated with child overweight for a single mother with a low income, limited access to health services and social support, poorer neighborhood social capital, and fewer neighborhood resources to support child physical activity and healthy eating, compared to a mother with greater income and greater access to resources that may buffer the effect of maternal depression on child weight. Mental health treatment status may also modify the effect of maternal depressive symptoms on child weight. In order to inform the targeting of obesity prevention efforts, research is therefore needed to identify whether aspects of the family and neighborhood context modify the effect of maternal depression and place certain families at greater risk of child overweight.
This is the first systematic review to examine the prospective association between exposure to maternal depression and child excess weight across the span of child development. It should be noted that the studies included in this review were conducted in high-income countries, with the exception of one study conducted in Brazil, and the relationship between maternal depression and child overweight may be different in lower income countries. Limitations at the review level include the possibility of incomplete identification of relevant studies. One prospective study was excluded from this review, which measured maternal depression in the postnatal period but did not examine the unique association between postnatal depression and child weight outcomes, instead combining exposure with pre-natal depression (Wojcicki et al., 2011). This study did not observe a positive association between perinatal depression and child overweight. In addition, reviewed studies were conducted across four different locations, including a multi-country European study, and this source of variability is a potential limitation of the current review. Finally, we did not attempt to meta-analyze quantitative data in the current study, given the vast heterogeneity between studies in the measurement and categorization of maternal depression exposure, child age at exposure and child age at outcome.
5. Conclusion
In summary, we identified mixed findings for the association between maternal depression and child weight outcomes. Importantly, preliminary evidence suggests that chronic maternal depression, but not episodic depression, may increase risk for child overweight. This finding indicates that initiatives to prevent childhood obesity may need to incorporate efforts to identify, involve, and support mothers experiencing chronic depression. Beyond a focus on chronic depression, we identified clear priorities for future research. Research in this field is still in its infancy, as demonstrated by the recent time span of the studies identified in this review (2007–2013). Studies with longer follow-up periods are needed to identify the long-term effect of exposure to maternal depression into adolescence and beyond. Similarly, exposure to maternal depression at later periods of child development should be examined. Finally, theory-driven investigations of the mediating and moderating factors that may explain and influence the relationship between maternal depression and child weight outcomes, such as family income, family access to resources, and parenting practices, are needed. Given the prevalence of maternal depression, understanding its impact on child weight development within the context of family and neighborhood conditions may lead to important insights for obesity prevention efforts.
Highlights.
Episodic maternal depression was not associated with child overweight or obesity
Chronic maternal depression, however, may increase risk for child overweight
Mixed findings were observed for child BMI z-score
Footnotes
The authors declare that there are no conflicts of interest.
References
- Ajslev TA, Andersen CS, Ingstrup KG, Nohr EA, Sorensen TI. Maternal postpartum distress and childhood overweight. PLoS One. 2010;5:e11136. doi: 10.1371/journal.pone.0011136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N. Depressive symptoms, major depression, and generalized anxiety: a comparison of self-reports on CES-D and results from diagnostic interviews. Psychiatry Res. 1985;15:219–29. doi: 10.1016/0165-1781(85)90079-4. [DOI] [PubMed] [Google Scholar]
- Burdette HL, Whitaker RC, Kahn RS, Harvey-Berino J. Association of maternal obesity and depressive symptoms with television-viewing time in low-income preschool children. Arch Pediatr Adolesc Med. 2003;157:894–99. doi: 10.1001/archpedi.157.9.894. [DOI] [PubMed] [Google Scholar]
- Conners N, Tripathi S, Clubb R, Bradley R. Maternal characteristics associated with television viewing habits of low-income preschool children. J Child Fam Stud. 2007;16:415–25. [Google Scholar]
- Davison KK, Jurkowski JM, Lawson HA. Reframing family-centred obesity prevention using the Family Ecological Model. Public Health Nutr Epub. 2012 doi: 10.1017/S1368980012004533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis CL, McQueen K. The relationship between infant-feeding outcomes and postpartum depression: a qualitative systematic review. Pediatrics. 2009;123:e736–e51. doi: 10.1542/peds.2008-1629. [DOI] [PubMed] [Google Scholar]
- Duarte CS, Shen S, Wu P, Must A. Maternal depression and child BMI: longitudinal findings from a US sample. Pediatr Obes. 2012;7:124–33. doi: 10.1111/j.2047-6310.2011.00012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwardson CL, Gorely T. Parental influences on different types and intensities of physical activity in youth: a systematic review. Psychol Sport Exerc. 2010;11:522–35. [Google Scholar]
- Ertel KA, Kleinman K, van Rossem L, Sagiv S, Tiemeier H, Hofman A, Jaddoe VWV, Raat H. Maternal perinatal depression is not independently associated with child body mass index in the Generation R Study: methods and missing data matter. J Clin Epidemiol. 2012;65:1300–09. doi: 10.1016/j.jclinepi.2012.05.013. [DOI] [PubMed] [Google Scholar]
- Ertel KA, Koenen KC, Rich-Edwards JW, Gillman MW. Antenatal and postpartum depressive symptoms are differentially associated with early childhood weight and adiposity. Paediatr Perinat Epidemiol. 2010;24:179–89. doi: 10.1111/j.1365-3016.2010.01098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertel KA, Rich-Edwards JW, Koenen KC. Maternal depression in the United States: nationally representative rates and risks. J Womens Health. 2011;20:1609–17. doi: 10.1089/jwh.2010.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernald LCH, Jones-Smith JC, Ozer EJ, Neufeld LM, DiGirolamo AM. Maternal depressive symptoms and physical activity in very low-income children. J Dev Behav Pediatr. 2008;29:385–93. doi: 10.1097/DBP.0b013e318182a98e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106:1071–83. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Golan M, Crow S. Parents are key players in the prevention and treatment of weight-related problems. Nutr Rev. 2004;62:39–50. doi: 10.1111/j.1753-4887.2004.tb00005.x. [DOI] [PubMed] [Google Scholar]
- Grote V, Vik T, von Kries R, Luque V, Socha J, Verduci E, Carlier C, Koletzko B. Maternal postnatal depression and child growth: a European cohort study. BMC Pediatr. 2010;10:14. doi: 10.1186/1471-2431-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyos Cillero I, Jago R. Systematic review of correlates of screen-viewing among young children. Prev Med. 2010;51:3–10. doi: 10.1016/j.ypmed.2010.04.012. [DOI] [PubMed] [Google Scholar]
- Lampard AM, Jurkowski JM, Lawson HA, Davison KK. Family ecological predictors of low-income parents’ support for children’s physical activity. Beh Med. 2013;39:97–103. doi: 10.1080/08964289.2013.802215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane SP, Bluestone C, Burke CT. Trajectories of BMI from early childhood through early adolescence: SES and psychosocial predictors. Br J Health Psychol. 2013;18:66–82. doi: 10.1111/j.2044-8287.2012.02078.x. [DOI] [PubMed] [Google Scholar]
- Loprinzi PD, Cardinal BJ, Loprinzi KL, Lee H. Parenting practices as mediators of child physical activity and weight status. Obes Facts. 2012;5:420–30. doi: 10.1159/000341097. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. 2000;20:561–92. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Milgrom J, Skouteris H, Worotniuk T, Henwood A, Bruce L. The association between ante- and postnatal depressive symptoms and obesity in both mother and child: a systematic review of the literature. Women’s Health Issues. 2012;22:e319–e28. doi: 10.1016/j.whi.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman D The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien M, Nader PR, Houts RM, Bradley R, Friedman SL, Belsky J, Susman E. The ecology of childhood overweight: a 12-year longitudinal analysis. Int J Obes. 2007;31:1469–78. doi: 10.1038/sj.ijo.0803611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers R, Paxton S, Massey R, Campbell K, Wertheim E, Skouteris H, Gibbons K. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: a prospective study. Int J Behav Nutr Phys Act. 2013;10:24. doi: 10.1186/1479-5868-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32:963–75. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- Santos IS, Matijasevich A, Domingues MR, Barros AJD, Barros FCF. Long-lasting maternal depression and child growth at 4 years of age: a cohort study. J Pediatr. 2010;157:401–06. doi: 10.1016/j.jpeds.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Horst K, Oenema A, Ferreira I, Wendel-Vos W, Giskes K, Van Lenthe FJ, Brug J. A systematic review of environmental correlates of obesity-related dietary behaviors in youth. Health Educ Res. 2007;22:203–26. doi: 10.1093/her/cyl069. [DOI] [PubMed] [Google Scholar]
- Wang L, Anderson JL, Dalton WT, III, Wu T, Liu X, Zheng S. Maternal depressive symptoms and the risk of overweight in their children. Matern Child Health J. 2013;17:940–8. doi: 10.1007/s10995-012-1080-1. [DOI] [PubMed] [Google Scholar]
- Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa Hospital Research Institute; Ottawa: 1996. [Google Scholar]
- Weng SF, Redsell SA, Swift JA, Yang M, Glazebrook CP. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch Dis Child. 2012;97:1019–26. doi: 10.1136/archdischild-2012-302263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojcicki JM, Holbrook K, Lustig RH, Epel E, Caughey AB, Munoz RF, Shiboski SC, Heyman MB. Chronic maternal depression is associated with reduced weight gain in latino infants from birth to 2 years of age. PLoS One. 2011;6:e16737. doi: 10.1371/journal.pone.0016737. [DOI] [PMC free article] [PubMed] [Google Scholar]