Abstract
Objectives
To understand whether nursing home (NH) introduction of culture change practices is associated with improved quality
Design
NH-level panel study using multivariate fixed-effects statistical modeling to estimate the effect of culture change introduction on quality outcomes
Setting and Participants
824 U.S. NHs with culture change practice involvement beginning between 2005 and 2010
Measurements
A culture change practice score (derived from a 2009/10 national NH survey) was used to stratify analyses by NHs with high practice implementation (scores in the top quartile; n=217) versus other NHs (n=607). NH-level outcomes included 1) prevalence of seven care practices and three resident outcomes; 2) a NH’s health-related and quality-of-life weighted survey deficiencies; and, 3) the average number of hospitalizations per resident year.
Results
For NHs with high practice implementation, introduction of culture change was associated with a significant decrease in the prevalence of restraints, tube feeding and pressure ulcers; an increase in the proportion of residents on bladder training programs; and, a small decrease in the average number of hospitalizations per resident year (coefficient −0.04, standard error (SE) 0.022; p=0.06). For NHs having lower practice implementation (practice scores in lower-three quartiles), introduction was associated with fewer health-related (coefficient −5.26; SE 3.05; p=0.09) and quality-of-life (coefficient −0.10; SE 0.049; p=0.04) survey deficiencies. However, these NHs also had small statistically significant increases in the prevalence of residents with urinary tract infections and in the average hospitalizations per resident year (coefficient 0.03; SE 0.014; p=0.02).
Conclusion
The introduction of NH culture change appears to result in significant improvements in some care processes and outcomes in NHs having high practice implementation. For other NHs, culture change introduction results in fewer survey deficiencies.
Keywords: nursing home, culture change, outcomes
INTRODUCTION
Culture change in elder care settings, such as nursing homes (NHs), involves the intentional transformation of these settings to be less institutional, increasingly centered on and directed by the residents, and more empowering of care workers. Implementation of culture change practices is rapidly spreading across the U.S. NH industry1 and research is evolving; however, evidence on how culture change relates to clinical processes and quality outcomes has remained inconclusive.2-4 Research limitations, such as inconsistent measurement of culture change practice, variation in populations studied, small sample sizes and lack of rigorous evaluation designs contribute to this lack of conclusive findings.3 Also, inadequate attention has been paid to the fact that culture change practices are often implemented incrementally5, 6 but “culture change NHs” have varying degrees of practice implementation.1, 7 Reliable evidence is necessary to inform NH stakeholders who are engaged in or considering culture change. It is also needed to guide policy, which to date has often promoted culture change based on its strong face validity. This article contributes evidence on how the introduction of culture change practices in NHs relates to changes in key care processes and quality outcomes using a more rigorous study design than most previous studies.
Comprehensive Culture Change and its Core Components
Culture change, when implemented comprehensively, entails the multidimensional reform of care practices, staff procedures, protocols, and environmental design.8, 9 Providing resident-centered care, empowering frontline staff, and making environments homelike are central culture change principles/domains; other domains include relationships, NH leadership and quality improvement.2, 10 Rather than implement culture change comprehensively, however, NHs often implement select culture change practices pertinent to their unique circumstances.5 Such practices include involving residents in determining their eating and sleeping schedules, engaging staff in quality improvement teams, and expanding dining hours and access to kitchen areas.1 Surveys with NH leaders suggest that the adoption of select culture change practices is substantially increasing, but comprehensive culture change remains rare.1, 7 The multidimensionality of culture change and its unproven value may help explain NHs’ limited uptake of such comprehensive cultural transformation, as may the challenges associated with more widespread practice implementation.11
Identified Outcomes of Culture Change
Although the evidence has been inconclusive regarding the relationship between culture change practice implementation and quality outcomes, numerous studies point to a variety of outcomes that culture change practices may positively affect. Identified benefits of culture change include reduced incidence of decline in activities of daily living,12 greater satisfaction among residents and families,12, 13 reduced feelings of boredom and helplessness among residents,14 as well as nurses’ increased job satisfaction and their improved perceptions of working conditions and of the capacity to meet the individual needs of residents with dignity and respect.8, 15 Heightened staff satisfaction16 and reductions in staff turnover17 are also apparent outcomes of staff empowerment practices. Some studies have identified adverse outcomes of culture change, such as a heightened fall risk among residents,18, 19 but it does not appear that culture change practices lead to significant negative outcomes.3
In this study we expand upon the emerging evidence base on the value of culture change by examining how the introduction of culture change practices and the degree of practice implementation are associated with changes in key care processes (e.g., bladder and bowel training, advance directives, restraints) and outcomes (e.g., falls, pressure ulcers, hospitalizations). Using national NH survey data we examine changes in study outcomes for NHs that introduced culture change involvement in different years (between 2005 and 2010), and to differing degrees. Thus, we excluded non- and early-adopters who are likely very different.20 This design allows us to control to some extent for the endogeneity between a NH’s choice to introduce culture change and its likelihood to improve quality since we compare changes in outcomes for the “middle majority” of adopters who introduced culture change in earlier versus later study years.
METHODS
Nursing Home Survey and Study Sample
This research is part of a larger study on the implementation of culture change practices in U.S. NHs.1 The larger study collected survey data from NH directors of nursing (DONs) and administrators (NHAs) on three central culture change domains: (1) a NH’s (physical) environment, (2) staff empowerment, and (3) resident choice and decision making (i.e., resident-centered care). The selection and cognitive-based testing of survey items are described in detail elsewhere.1, 21 Surveys were administered to a stratified, proportionate random sample of DONs and NHAs at 4,149 U.S. NHs; a contact was identified at 3,539 of these facilities. Surveys were completed between August 2009 and April 2011 (only 2.9% completed in 2011). The cooperation rate (i.e., response rate when contact was identified) was 62.6% for NHAs (n=2,215), 61.6% for DONs (n=2,164), 66.6% for either (n=2,686), and 47.8% for both (1,693). No nonresponse bias was detected.22 Some completed abbreviated surveys (5.6% of DONs and 2.5% of NHAs), and no significant differences between respondents with abbreviated versus full surveys were identified.22
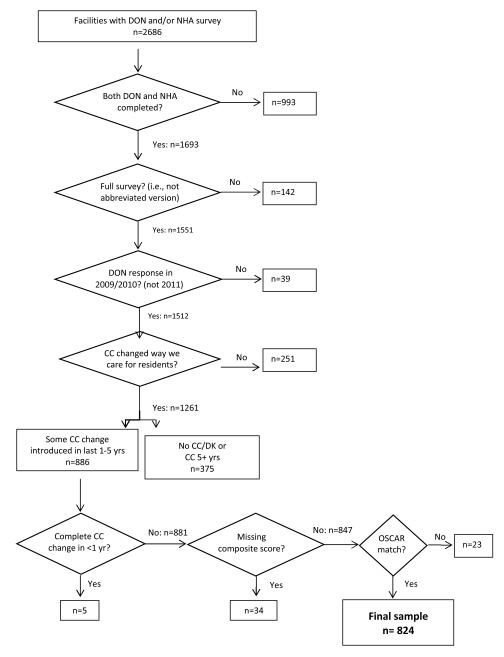
Our study sample was restricted to accommodate the study design. Thus, we included NHs with complete DON and NHA surveys (needed for composite score) and excluded those reporting no culture change involvement (nonadopters) or involvement of 5 years or more (early adopters). We also excluded NHs when the DON’s response was in 2011 given our outcomes data were through June 2010 (see Figure 1). To determine NH involvement, DONs were asked to choose a response to indicate their NH’s involvement in culture change (after being provided with a culture change definition); responses ranged from “There is NO DISCUSSION around culture change.” to “Culture change has COMPLETELY CHANGED the way we take care of residents in ALL areas of the organization.” To determine the year culture changed was introduced, DONs were also asked “How many years has your nursing home been involved in culture change activities?” We excluded NHs when responses were “Not involved,” 5 years or more or “Don’t Know ” and specified introduction year based on the following responses: “Less than 1 year” (introduction is survey year); “1 year but less than 2 years” (introduction year is year before survey); “2 years but less than 3 years” (introduction year is two years before survey); and “3 years but less than 5 years” (introduction year is four years before survey). Because of questionable validity, 5 NHs where DONs indicated that they completely changed the way they cared for residents in all areas in less than a year were removed; and, removed were NHs with missing (non-imputed) survey items and those without Online Survey Certification and Reporting (OSCAR) data during the culture change introduction year and/or in at least one year in the two years pre and post implementation (n=824; see Figure 1).
Figure 1. Study Sample Selection.
DON= director of nursing; NHA= nursing home administrator; CC= culture change; DK= don’t know; OSCAR= Online Survey, Certification and Reporting
Variables of Interest and Data Sources
Culture Change Practice Score
A culture change practice score was created to reflect a NH’s extent of practice implementation for the three central domains -- the NH environment, resident-centered care and staff empowerment. The NH environment domain included eight items, which measured facilities’ efforts at making the NH’s environment more homelike through practices such as having any residents living in self-contained (including kitchen and dining facilities) small households and/or neighborhoods, having private rooms, and having open dining policies and other homelike characteristics. The resident-centered care domain included four questions assessing residents’ involvement in determining their schedules, activities and care. The staff empowerment domain included seven items assessing staff participation in management and decision making as well as questions about staff recognition. These survey items and responses have been previously reported.1 Cronbach’s alpha showed the internal consistency reliability to be acceptable for the environment and staff empowerment items, given the small number of items within each (α = 0.61 and α = 0.62, respectively). The alpha for resident-centered care was low (α = 0.48), likely because there were only four survey items that were measured via an ordinal (not rating) scale (yes, no and working on it).23, 24 However, these items had face and construct validity.1
For each domain, item values were summed to create NH physical environment, resident-centered care and staff empowerment domain scores with total possible scores of 22, 8 and 21 respectively. In cases where one or two (scaled) items in a domain score were missing, the modal responses for the other items in the score were imputed. From these domain scores a weighted practice score was created by equally weighting each domain score and summing the proportions (resulting in a possible score of 0 to 100).
The mean practice score for the study sample was 49.4 with a standard deviation (SD) of 11.25. Since we were interested in determining how introduction of culture change was associated with quality improvement when NHs had high versus lower practice implementation, we categorized as “high” those facilities with culture change composite scores in the top quartile and as lower those with scores in the bottom three quartiles. The top quartile (n=217) had a mean practice score of 63.6 (SD 6.18) while for others (n=607) the mean score was 44.3 (SD 7.78).
Outcome Variables
Study outcome variables were from resident assessment minimum data set (MDS) data, OSCAR data, and Medicare claims data. The residential history file (RHF) which concatenates MDS, Medicare claims and vital statistics data was used to determine hospital use for NH residents since this file tracks over time residents’ NH and other health care use.25 Table 1 shows the study outcome variables, their data sources, and how variables were operationalized. For each year included in the analyses (2002 through 2010 [through June 2010]), we used yearly aggregated MDS data or OSCAR data to determine the outcome. The prevalence estimates were based on all residents in each facility on the first Thursday in April in each study year. From OSCAR data we also determined the number of health-related and quality of life survey deficiencies, which were weighted for severity and scope. For the hospitalization outcome, we first determined for each study year (first half of 2010) the number of NH days which was then divided by 365 to establish the number of resident years (the denominator). The RHF was then used to count the number of hospitalizations of Medicare fee-for-service residents that occurred directly from the NH during the calendar year (the numerator).
Table 1.
Data Sources and Definitions/Creation of Study Outcomes
| Study Outcomes | Data Source | Definition / Creation |
|---|---|---|
| Processes | ||
| % on bladder training program | OSCAR | Detailed plan of care to assist the resident to gain and maintain bladder control. |
| % on bowel training program | OSCAR | Detailed plan of care to assist the resident to gain and maintain bowel control. |
| % with preventive skin care | OSCAR | Receiving preventive skin care |
| % with advanced directives | OSCAR | Have advanced directives (i.e., living will, durable power of attorney for health care) |
| % with restraints | MDS | Use of bed rails, trunk restraint, limb restraint in the last 7 days. |
| % with antipsychotic meds | MDS | Received antipsychotics during the last 7 days. |
| % with tube feeding | OSCAR | Receive all or most nutritional requirements via a feeding tube. |
| Outcomes | ||
| % with falls in last 30 days | MDS | Fell in the past 30 days |
| % with pressure ulcers | MDS | Pressure or stasis ulcer present in the last 7 days. |
| % residents with UTI | MDS | Urinary tract infection in last 30 days. |
| Survey Deficiencies | ||
| Health deficiencies, weighted | OSCAR | All health-related deficiencies (F-series) weighted by scope and severity. |
| Quality of Life deficiencies | OSCAR | Subset of health-related deficiencies weighted by scope and severity. Codes F0240-F0258. |
| Hospital Use | ||
| Hospitalizations per resident | MDS/ | Total hospitalizations of Medicare fee-for- |
| year | Claims | service residents divided by total nursing home days for all residents in a facility during the calendar year. |
OSCAR = Online Survey, Certification and Reporting; MDS = Minimum Data Set; UTI = urinary tract infection
Covariates
Other time-varying covariates were included models to control for changes in NH occupancy and casemix, and for county-level NH competition. These variables were derived from the MDS, Medicare claims and OSCAR. Resident aggregated MDS data were used to determine a NH index of activities of daily living, ranging from 4 to 18 (all facility residents ambulatory and independent in eating, toileting and transferring [4] to all facility residents bedfast and totally dependent in eating, toileting and transferring [18]). A county-level Herfindahl index (0 to 1.0 [no competition]) derived from OSCAR data was included to control for the NH market competitiveness. Also, we included a set of dummy variables to represent calendar year to control for secular trends in the outcome variables. Of note, we did not control for time-varying NH staffing levels since any changes may be a possible result of culture change adoption; thus, controlling for staffing could potentially lead to an underestimate of the culture change introduction effect. However, staffing variables were derived from OSCAR data and summary statistics are presented.
Analyses
We used summary statistics to characterize NH and county time-varying characteristics and to compare values for study outcomes in the year prior to, of and post culture change practice introduction. Nursing home panel fixed-effect regression analyses (using the within-panel estimator) and version 12.1 of Stata software26 were used to regress each outcome on an indicator variable representing the introduction of culture change involvement. This culture change introduction variable was coded 0 for all years prior to introduction and as a 1 for the year of introduction and all years following. Panel fixed-effect regression controls for unobserved time-invariant NH characteristics that may have influenced study outcomes, and it allows for a difference-in-difference model causal interpretation of our results. Our modeling strategy estimates the change in the NH study outcomes following culture change introduction and contrasts this change with that among those NHs that did not yet introduce culture change. Thus, the derived coefficient for the culture change introduction variable can be interpreted as the effect of culture change introduction after controlling for secular time trends and the model’s time-varying covariates.
RESULTS
For the two categories of nursing homes, Table 2 describes the study covariates in the year prior to, of and culture change introduction. No large differences or changes are observed. However, NHs with the top quartile scores on average had slightly lower proportions of Medicare and Medicaid residents (and thus slightly higher proportions of private pay and/or managed care residents). Also, NHs with the top scores had on average a slightly higher proportion of residents with dementia.
Table 2.
Study Covariates for Years Prior to, of, and after Culture Change Introduction—By Nursing Homes with High versus Lower Culture Change Practice Implementation
| Bottom 3 Quartiles - Culture Change Composite Score |
Top Quartile - Culture Change Composite Score |
|||||
|---|---|---|---|---|---|---|
|
|
||||||
| Year Immediately Prior to Culture Change Introduction |
Year Culture Change Introduction Began |
Year Immediately Following Culture Change Introduction |
Year Immediately Prior to Culture Change Introduction |
Year Culture Change Introduction Began |
Year Immediately Following Culture Change Introduction |
|
|
|
||||||
| mean (sd) | mean (sd) | mean (sd) | mean (sd) | mean (sd) | mean (sd) | |
| Occupancy Rate (%) | 85.6 (13.3) | 85.2 (12.7) | 85.3 (13.1) | 85.2 (15.7) | 85.6 (13.6) | 86.0 (13.2) |
| Resident Payment source | ||||||
| Medicare (%) | 12.8 (11.4) | 13.2 (11.7) | 13.4 (11.2) | 11.7 (11.7) | 12.7 (12.7) | 12.3 (11.5) |
| Medicaid (%) | 60.6 (20.1) | 59.8 (20.4) | 59.9 (20.1) | 56.8 (21.2) | 56.3 (21.2) | 56.4 (20.1) |
| Residents with Dementia | 47.5 (17.3) | 48.0 (17.6) | 47.8 (16.7) | 49.4 (17.7) | 48.9 (17.6) | 50.4 (16.8) |
| (%) | ||||||
| Average ADL indexa | 10.7 (1.2) | 10.7 (1.1) | 10.7 (1.2) | 10.7 (1.0) | 10.7 (1.0) | 10.7(1.1) |
| County Herfindahl indexb | 0.2 (0.3) | 0.2 (0.3) | 0.2 (0.3) | 0.2 (0.2) | 0.2 (0.2) | 0.2 (0.2) |
ADL = activities of daily living
Range of 4 (all facility residents ambulatory and independent in eating, toileting and transferring) to 18 (all facility residents bedfast and totally dependent in eating, toileting and transferring)
Range of 0 to 1.0
Table 3 displays the unadjusted average NH values for study outcomes across the three years of interest for the two categories of NHs. With culture change introduction, NHs with high practice implementation (top quartile) had observable increases in the proportion of residents on bladder or bowel training programs and decreases in the prevalence of restraints, tube-feeding use, and pressure ulcers. Similar changes were not observed for NHs with lower culture change scores. However, the percentage of residents on bladder and bowel training was very low before culture change introduction for the high implementers (4.9% and 2.5% respectively), and then increased to 8.7% and 4.0% (respectively). Those NHs with lower culture change implementation started at a substantially higher level of bladder and bowel training (7.6% and 4.5% respectively) which was maintained with culture change implementation. Additionally, compared to NHs with lower culture change scores, NHs with high scores had higher staffing levels per resident day in the year prior to culture change introduction. Only small changes in staffing levels after culture change introduction were observed (Table 3).
Table 3.
Study Outcomes and Staffing Levels for Years Prior to, of, and after Culture Change Introduction—By Nursing Homes with High versus Lower Culture Change Practice Implementation
| Bottom 3 Quartiles - Culture Change Composite Score |
Top Quartile - Culture Change Composite Score |
|||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Year Immediately Prior to Culture Change Introduction |
Year Culture Change Introduction Began |
Year Immediately Following Culture Change Introduction |
Year Immediately Prior to Culture Change Introduction |
Year Culture Change Introduction Began |
Year Immediately Following Culture Change Introduction |
|||
|
|
||||||||
| N | mean (sd) | mean (sd) | mean (sd) | N | mean (sd) | mean (sd) | mean (sd) | |
| Processes | ||||||||
| on bladder training | 60 | 7.6 (14.7) | 7.5 (15.6) | 7.5 (14.9) | 217 | 4.9 (10.8) | 7.6 (15.1) | 8.7 (16.6) |
| program | 7 | |||||||
| 60 | 4.5 (12.5) | 4.1 (11.9) | 3.4 (9.8) | 217 | 2.5 (8.5) | 3.2 (9.6) | 4.0 (10.7) | |
| on bowel training program | 7 | |||||||
| % w/ preventive skin | 60 | 76.7 (28.0) | 78.1 (27.6) | 77.8 (28.0) | 217 | 78.9 (26.6) | 79.7 (26.3) | 78.9 (28.8) |
| care | 7 | |||||||
| 60 | 67.8 (24.7) | 68.2 (24.6) | 66.5 (26.0) | 217 | 70.6 (23.9) | 68.9 (24.8) | 71.4 (22.3) | |
| % w/ advanced directives | 7 | |||||||
| 60 | 5.0 (6.7) | 4.3 (6.1) | 3.5 (5.2) | 217 | 5.1 (6.6) | 3.8 (4.7) | 2.7 (3.9) | |
| % w/ restraints | 7 | |||||||
| 53 | 26.5 (12.2) | 26.3 (12.5) | 26.1 (12.7) | 207 | 25.2 (10.2) | 24.9 (10.0) | 24.7 (10.2) | |
| % w/ antipsychotic meds | 1 | |||||||
| 60 | 4.4 (4.8) | 4.3 (5.3) | 4.2 (4.6) | 217 | 4.1 (5.1) | 3.4 (3.4) | 3.4 (3.6) | |
| % w/ tube feeding | 7 | |||||||
| Outcomes | ||||||||
| 53 | 14.0 (6.3) | 14.3 (5.9) | 14.3 (6.0) | 207 | 14.7 (8.8) | 14.8 (6.6) | 14.7 (6.5) | |
| % w/ falls in last 30 days | 1 | |||||||
| 60 | 6.3 (4.6) | 6.4 (4.0) | 6.0 (4.0) | 217 | 6.0 (4.3) | 5.7 (3.6) | 5.4 (3.6) | |
| % w/ pressure ulcers | 7 | |||||||
| % residents w/ UTI | 53 | 8.4 (5.6) | 8.8 (5.6) | 8.9 (5.4) | 207 | 8.8 (4.9) | 9.1 (6.3) | 8.6 (5.1) |
| Survey Deficiencies | ||||||||
| 58 | 45.9 (62.7) | 43.9 (55.8) | 40.6 (46.4) | 211 | 41.2 (42.6) | 40.0 (46.0) | 41.5 (67.1) | |
| Health deficiencies | 7 | |||||||
| Quality of Life | 58 | 0.7 (1.0) | 0.7 (1.0) | 0.6 (1.0) | 211 | 0.6 (1.0) | 0.6 (0.9) | 0.5 (0.9) |
| deficiencies | 7 | |||||||
| Hospitalizations | ||||||||
| Hospitalizations per patient | 53 | 0.8 (0.4) | 0.9 (0.5) | 0.9 (0.4) | 208 | 0.8 (0.5) | 0.8 (0.5) | 0.8 (0.6) |
| year | 3 | |||||||
| 53 | 15.7 (7.1) | 16.0 (7.5) | 15.2 (8.5) | 207 | 15.0 (7.8) | 15.5 (8.5) | 16.0 (9.3) | |
| 30-day rehospitalizations | 2 | |||||||
| Staffng | ||||||||
| Registered Nurses per | 60 | 0.3 (0.4) | 0.3 (0.2) | 0.3 (0.2) | 217 | 0.4 (0.5) | 0.3 (0.4) | 0.4 (0.4) |
| resident day | 7 | |||||||
| Nursing Assistants per | 60 | 2.2 (0.9) | 2.2 (0.9) | 2.2 (1.1) | 216 | 2.4 (1.7) | 2.2 (0.8) | 2.2 (0.8) |
| resident day | 6 | |||||||
| Licensed Practical Nurses | 60 | 0.8 (0.3) | 0.8 (0.4) | 0.8 (0.4) | 217 | 0.8 (0.9) | 0.8 (0.5) | 0.8 (0.5) |
| per resident day | 6 | |||||||
UTI = urinary tract infection
For NHs with lower culture change scores, with culture change introduction there were decreases in the crude average number of weighted health-related and quality of life survey deficiencies. Of interest, however, is that these lower deficiencies post-introduction were similar to the pre-introduction deficiency averages of NHs with the top culture change scores.
Among NHs with high culture change and compared to those who had not yet introduced culture change, regression analyses showed culture change introduction was associated with a significant increase in the proportion of residents on bladder training programs (coefficient [Coef] 3.06, standard error [SE] 1.293) and significant decreases in a NH’s proportion of residents with restraints and tube feeding (Coef −1.06, SE 0.447 and Coef −0.628, SE 0.321 respectively; Table 4). There was also a significant decrease in the proportion of residents with pressure ulcers (Coef −0.63, SE 0.321). Among facilities with lower culture change scores, introduction was associated with a significant increase in the proportion of residents with urinary tract infections (Coef 0.72, SE 0.280).
Table 4.
Multivariate Results of the Association Between the Introduction of Culture Change Involvement and Study Outcomes—By Nursing Homes with High versus Lower Culture Change Practice Implementation
| Bottom 3 Quartiles - Culture Change Composite Score |
Top Quartile - Culture Change Composite Score |
|||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| N | Coefficien t |
SSE | p-value | N | Coefficien t |
SE | p-value | |
| Processes | ||||||||
| % on bladder training program | 607 | -0.57 | 0.670 | 0.40 | 217 | 3.06 | 1.293 | 0.02 |
| % on bowel training program | 607 | -0.28 | 0.536 | 0.61 | 217 | 0.04 | 0.941 | 0.96 |
| % w/ preventive skin care | 607 | 0.26 | 1.246 | 0.84 | 217 | 0.08 | 2.172 | 0.97 |
| % w/ advanced directives | 607 | 0.60 | 0.949 | 0.53 | 217 | -0.32 | 1.524 | 0.83 |
| % w/ restraints | 607 | 0.11 | 0.268 | 0.67 | 217 | -1.06 | 0.447 | 0.02 |
| % w/ antipsychotic meds | 531 | 0.33 | 0.364 | 0.37 | 207 | 0.86 | 0.575 | 0.14 |
| % w/ tube feeding | 607 | 0.11 | 0.136 | 0.41 | 217 | -0.65 | 0.241 | 0.01 |
| Outcomes | ||||||||
| % w/ falls in last 30 days | 531 | 0.09 | 0.320 | 0.78 | 207 | 0.05 | 0.624 | 0.94 |
| % w/ pressure ulcers | 607 | 0.31 | 0.190 | 0.10 | 217 | -0.63 | 0.321 | 0.05 |
| % residents w/ UTI | 531 | 0.72 | 0.280 | 0.01 | 207 | -0.06 | 0.544 | 0.92 |
| Survey Deficiencies | ||||||||
| Health deficiencies | 587 | −5.26 | 3.046 | 0.09 | 211 | −1.87 | 5.495 | 0.73 |
| Quality of Life deficiencies | 587 | −0.10 | 0.050 | 0.04 | 211 | −0.12 | 0.081 | 0.16 |
| Hospitalizations | ||||||||
| Hospitalizations per patient | 536 | 0.03 | 0.014 | 0.02 | 208 | −0.04 | 0.022 | 0.06 |
| year | ||||||||
| 30-day rehospitalizations | 535 | 0.31 | 0.420 | 0.46 | 207 | 1.08 | 0.760 | 0.16 |
UTI = urinary tract infection
For NHs with lower culture change scores, introduction (versus non-introduction) was associated with an approximate five point decrease in weighted health-related survey deficiencies (Coef −5.26, SE 3.046) and a 0.1 point significant decrease in weighted quality of life deficiencies (Coef −0.10, SE 0.050; see Table 4). Considering hospitalizations, upon introduction (compared to non-introduction) NHs with high culture change scores had a small marginally significant decrease in the number of hospitalizations per resident year (Coef −0.04, SE 0.02; p=0.06). For NHs with lower culture change scores, there was small significant increase in the number of hospitalizations per resident year (Coef 0.03, SE 0.014).
DISCUSSION
For NHs with the most reported culture change practice implementation (top quartile of 2009/10 survey scores), the introduction of culture change was associated with improvements in selected care processes and resident outcomes, including a small reduction in hospitalizations. Among NHs with lower reported practice implementation, culture change introduction was associated with lower health-related and quality of life survey deficiencies. Findings support the value of the numerous efforts underway to further disseminate NH culture change practices, and demonstrate the need for future research to consider the extent of practice implementation when studying how NH culture change practice may affect quality outcomes.
Findings showing the introduction of culture change (for high practice adopters) is associated with increases in the proportion of residents on bladder training programs and decreases in the proportion with restraints and feeding tubes are consistent with recent research in Veterans Administration (VA) NHs showing decreased unfavorable events in NHs with greater culture change practice implementation.27 Additionally, upon introduction of culture change, these NHs had a significant decrease in the proportion of residents with pressure ulcers and a small but marginally significant decrease in hospitalizations per resident year. With regard to pressure ulcers, a large study of Dutch NHs similarly found development of a resident council, which is an artifact of culture change, along with implementation of other quality initiatives, was associated with significant reduction in pressure ulcers.28 Furthermore, regarding hospitalizations, previous research suggests culture change may contribute to NH staff paying greater attention to early warning signs of an impending hospitalization, helping to deter hospitalizations.29
Among NHs with lower culture change practice implementation, the introduction of culture change was associated with significant decreases in survey deficiencies and quality of life deficiencies; this agrees with previous research.30 Notably, in the year prior to culture change implementation, these NHs also had high health and quality of life deficiencies (45.9 and 0.7, respectively) compared to NHs with high culture change implementation (41.2 and 0.6). Thus, these reductions in deficiencies brought them in line with the deficiency levels of NHs with higher implementation. The associations between culture change introduction and reductions in survey deficiencies are consistent with findings from qualitative interviews in that many NHAs described their implementation efforts as being aligned with surveyor oversight.11 Although regulatory oversight has previously been reported as a barrier to culture change implementation in NHs,31 bringing alignment between culture change efforts and surveyor oversight has also been a target of national and state efforts.32 While our national findings suggest some level of alignment has been achieved, future studies examining these issues by states or in regions within states are needed because of known variation in regulatory oversight.33
For NHs with lower culture change implementation, we found the introduction of culture change was associated with a small but significant increase in the number of resident hospitalizations. Thus, although culture change may contribute to NH staff paying greater attention to early warning signs of an impending hospitalization,29 this may not be occurring in NHs with lower implementation. However, examining the extent and types of culture change practices implemented over time together with the changes in hospitalization rates may help to clarify this.
LIMITATIONS
This study has limitations that deserve comment. First, while the study was designed to address the probable endogeneity between a NH’s choice to introduce culture change and its likelihood of having improvements in quality, this may not have been totally accomplished since NHs who introduced culture change earlier in years (2005-2010) may still have differed (perhaps in unmeasured ways) from NHs introducing it in later years. Still, it is likely we eliminated much potential endogeneity bias by excluding NH non-adopters (i.e., in this study the 14% with no involvement)1 and early adopters (i.e., the 22% who introduced culture change 5+ years prior to the survey).20 Also, the extent of culture change practice implementation was self-reported and subject to social desirability bias;34 and, we surveyed only DONs and NHAs and responses may have differed had we asked other NH staff. Additionally, when interpreting results readers should consider that the Cronbach’s alpha for the resident-centered care domain was low. This is likely due to the small number of items in this domain and its ordinal measurement. When adding items and repeating measurement, it would be appropriate to consider ours and similar survey collection efforts as reflecting indices of practice rather than measures of an underlying domain. As such, high internal consistency (via Cronbach’s alpha) would not be relevant given that NHs implement practices incrementally and thus item agreement is not necessarily an expectation.4, 5 Importantly, we previously found good correspondence between survey responses and qualitative interviews;1 therefore, the validity of the survey data appears sound. Last, we focused on only three of the six culture change domains,35 and within each included only between four and eight items. Nonetheless, the domains studied are central to culture change implementation2 and supported by construct validity analyses. 1, 36, 37
Conclusion
This study supports the positive association between the introduction of NH culture change and quality improvements. However, we found quality improvements beyond a reduction in survey deficiencies occurred only for those NHs with greater culture change practice implementation (i.e., those with culture change practice scores in the top quartile). As such, these findings may help to explain some of the previous equivocal findings from quality studies when the extent of culture change practice implementation was not considered or measured. Future longitudinal study examining the association between the extent and types of culture change practices implemented and changes in quality indicators is recommended. Numerous ongoing efforts are underway to promote greater implementation of culture change practices in NHs. This study supports the value of these efforts.
ACKNOWLEDGMENTS
This project was funded by a grant from The Retirement Research Foundation (2008-086) and from the Shaping Long Term Care in America Project funded by the National Institute on Aging (1P01AG027296). During study data collection Dr. Lepore was funded through the Agency for Healthcare Research and Quality (AHRQ) National Research Services Awards (NRSA) Post doctoral fellowship training grant (5T32HS000011-24).
Sponsor’s Role: The funding institutions had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of manuscript or in the decision to submit the manuscript for publication.
Funding: This project was funded by a grant from The Retirement Research Foundation (2008-086) and from the Shaping Long Term Care in America Project funded by the National Institute on Aging (1P01AG027296). During study data collection Dr. Lepore was funded through the Agency for Healthcare Research and Quality (AHRQ) National Research Services Awards (NRSA) Post doctoral fellowship training grant (5T32HS000011-24).
Footnotes
A paper on this study was presented at the Academy Health 2013 Annual Research Meeting in Baltimore, MD in June 2013.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: Susan C. Miller: Study concept and design, acquisition of data, analysis and interpretation of data, and drafting the manuscript.
Michael Lepore: Acquisition of data and drafting the manuscript.
Julie C. Lima: Acquisition of data, analysis and interpretation of data, and revising the manuscript critically for important intellectual content.
Renee R. Shield: Acquisition of data and revising the manuscript critically for important intellectual content.
Denise A. Tyler: Acquisition of data and revising the manuscript critically for important intellectual content.
Contributor Information
Susan C. Miller, Center for Gerontology & Health Care Research, Department of Health Services, Policy and Practice, Brown University School of Public Health, Providence, RI
Michael Lepore, Planetree, Inc., Derby, CT Department of Health Services, Policy and Practice, Brown University School of Public Health, Providence, RI
Julie C. Lima, Center for Gerontology & Health Care Research, Brown University School of Public Health, Providence, RI
Renee Shield, Center for Gerontology & Health Care Research, Department of Health Services, Policy and Practice, Brown University School of Public Health, Providence, RI
Denise A. Tyler, Center for Gerontology & Health Care Research, Department of Health Services, Policy and Practice, Brown University School of Public Health, Providence, RI
REFERENCES
- [1].Miller SC, Looze J, Shield R, et al. Culture Change Practice in U.S. Nursing Homes: Prevalence and Variation by State Medicaid Reimbursement Policies. Gerontologist. 2014;54:434–45. doi: 10.1093/geront/gnt020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Koren MJ. Person-centered care for nursing home residents: The culture-change movement. Health Aff (Millwood) 2010;29:312–317. doi: 10.1377/hlthaff.2009.0966. [DOI] [PubMed] [Google Scholar]
- [3].Shier V, Khodyakov D, Cohen L, et al. What does the evidence really say about culture change in nursing homes? Gerontologist. 2014 Feb;54(Suppl 1):S6–S16. doi: 10.1093/geront/gnt147. [DOI] [PubMed] [Google Scholar]
- [4].Rahman AN, Schnelle JF. The nursing home culture-change movement: Recent past, present, and future directions for research. Gerontologist. 2008;48:142–148. doi: 10.1093/geront/48.2.142. [DOI] [PubMed] [Google Scholar]
- [5].Chapin M. Creating Innovative Places: Organizational and Architectural Case Studies of the Culture Change Movement in Long-Term Care. University of Wisconsin-Milwaukee; 2006. [Google Scholar]
- [6].Miller SC, Lima JC, Mitchell SL. Hospice care for persons with dementia: The growth of access in US nursing homes. Am J Alzheimers Dis Other Demen. 2010;25:666–673. doi: 10.1177/1533317510385809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Doty MM, Koren MJ, Sturla EL. Findings from the Commonweath Fund 2007 National Survey of Nursing Homes. Volume 91. The Commonwealth Fund; 2008. Culture Change in Nursing Homes: How Far Have We Come? [Google Scholar]
- [8].Brownie S, Nancarrow S. Effects of person-centered care on residents and staff in aged-care facilities: A systematic review. Clin Interv iAging. 2013;8:1–10. doi: 10.2147/CIA.S38589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Misiorski S, Kahn K. Changing the culture of long-term care: Moving beyond programmatic change. J Soc Work Long-Term Care. 2008;3:137–146. [Google Scholar]
- [10].Holistic Approach to Transformational Change (HATCh): An Overview. New Mexico Medical Review Association; Albuquerque, NM: 2005. Quality Partners of Rhode Island. [Google Scholar]
- [11].Shield RR, Looze J, Tyler DA, et al. Why and how do nursing homes implement culture change practices? Insights from qualitative interviews in a mixed methods study. J Appl Gerontol. 2013 Jul 19; doi: 10.1177/0733464813491141. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kane RA, Lum TY, Cutler LJ, et al. Resident outcomes in small-house nursing homes: a longitudinal evaluation of the initial green house program. J Am Geriatr Soc. 2007;55:832–839. doi: 10.1111/j.1532-5415.2007.01169.x. [DOI] [PubMed] [Google Scholar]
- [13].Lum TY, Kane RA, Cutler LJ, et al. Effects of Green House nursing homes on residents’ families. Health Care Financ Rev. 2008;30:35–51. [PMC free article] [PubMed] [Google Scholar]
- [14].Bergman-Evans B. Beyond the basics. Effects of the Eden Alternative model on quality of life issues. J Gerontol Nurs. 2004;30:27–34. doi: 10.3928/0098-9134-20040601-07. [DOI] [PubMed] [Google Scholar]
- [15].Ashburner C, Meyer JE, Johnson B, et al. Using action research to address loss of personhood in a continuing care setting. Illness Crisis Loss. 2004;12:23–37. [Google Scholar]
- [16].Bishop CE, Squillace MR, Meagher J, et al. Nursing home work practices and nursing assistants’ job satisfaction. Gerontologist. 2009;49:611–622. doi: 10.1093/geront/gnp040. [DOI] [PubMed] [Google Scholar]
- [17].Anderson RA, Corazzini KN, McDaniel RR., Jr. Complexity science and the dynamics of climate and communication: Reducing nursing home turnover. Gerontologist. 2004;44:378–388. doi: 10.1093/geront/44.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Coleman MT, Looney S, O’Brien J, et al. The Eden Alternative: Findings after 1 year of implementation. J Gerontol A Biol Sci Med Sci. 2002;57:M422–427. doi: 10.1093/gerona/57.7.m422. [DOI] [PubMed] [Google Scholar]
- [19].Chenoweth L, King MT, Jeon YH, et al. Caring for Aged Dementia Care Resident Study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: A cluster-randomised trial. Lancet Neurol. 2009;8:317–325. doi: 10.1016/S1474-4422(09)70045-6. [DOI] [PubMed] [Google Scholar]
- [20].Rogers EM. Diffusion of Innovations. 5th ed Free Press; New York, NY: 2003. [Google Scholar]
- [21].Tyler DA, Shield RR, Rosenthal M, et al. How valid are the responses to nursing home survey questions? Some issues and concerns. Gerontologist. 2011;51:201–211. doi: 10.1093/geront/gnq095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Clark MA, Roman A, Rogers ML, et al. Surveying Multiple Health Professional Team Members within Institutional Settings: An Example from the Nursing Home Industry. Evaluation and the Health Professions. 2014 doi: 10.1177/0163278714521633. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].McDowell I, Newell C. Measuring Health: A Guide to Rating Scales and Questionnaires. 2nd edn Oxford University Press, Inc.; NY: 1996. pp. 41–42. [Google Scholar]
- [25].Intrator O, Hiris J, Berg K, et al. The Residential History File: Studying nursing home residents’ long-term care histories. Health Serv Res. 2011;46:120–137. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Stata: Data Analysis and Statistical Software. 12 edn StataCorp LP; College Station, TX: 2012. [Google Scholar]
- [27].Sullivan JL, Shwartz M, Burgess JF, Jr, et al. Person-centered care practices and quality in Department of Veterans Affairs nursing homes: Is there a relationship? Med Care. 2013;51:165–171. doi: 10.1097/MLR.0b013e3182763230. [DOI] [PubMed] [Google Scholar]
- [28].Wagner C, Klein Ikkink K, van der Wal G, et al. Quality management systems and clinical outcomes in Dutch nursing homes. Health Policy. 2006;75:230–240. doi: 10.1016/j.healthpol.2005.03.010. [DOI] [PubMed] [Google Scholar]
- [29].Lamb G, Tappen R, Diaz S, et al. Avoidability of hospital transfers of nursing home residents: Perspectives of frontline staff. J Am Geriatr Soc. 2011;59:1665–1672. doi: 10.1111/j.1532-5415.2011.03556.x. [DOI] [PubMed] [Google Scholar]
- [30].Grabowski DC, O’Malley AJ, Afendulis CC, et al. Culture change and nursing home quality of care. Gerontologist. 2014;54(Suppl 1):S35–45. doi: 10.1093/geront/gnt143. [DOI] [PubMed] [Google Scholar]
- [31].Miller SC, Miller EA, Jung HY, et al. Nursing home organizational change: The “Culture Change” movement as viewed by long-term care specialists. Med Care Res Rev. 2010;67:65S–81S. doi: 10.1177/1077558710366862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Stone RI, Bryant N, Barbarotta L. Supporting culture change: Working toward smarter state nursing home regulation. Issue Brief (Commonw Fund) 2009;68:1–10. [PubMed] [Google Scholar]
- [33].Miller EA, Mor V. Balancing regulatory controls and incentives: Toward smarter and more transparent oversight in long-term care. J Health Polit Policy Law. 2008;33:249–279. doi: 10.1215/03616878-2007-055. [DOI] [PubMed] [Google Scholar]
- [34].Tourangeau R, Smith TW. Asking sensitive questions: The Impact of data collection mode, question format, and question context. Public Opin Quarterly. 1996;60:275–304. [Google Scholar]
- [35].Colorado Foundation for Medical Care . Measuring Culture Change: Literature Review. Colorado Foundation for Medical Care; 2006. [Google Scholar]
- [36].Bott M, Dunton N, Gajewski B, et al. Culture Change and Turnover in Kansas Nursing Homes. Kansas Department on Aging; Topeka, KS: 2009. [Google Scholar]
- [37].Mueller C. Nursing Leadership and Nursing Home Culture Change. Gerontological Society of America 60th Annual Scientific Meeting; San Francisco, CA: Gerontologist; 2007. [Google Scholar]