Abstract
A 73-year old man presented with abdominal pain. A tumor with central ulceration was observed in the ileum using double-balloon enteroscopy. Histological findings of the biopsy specimens were consistent with malignant lymphoma. Double-balloon enteroscopy confirmed the diagnosis of a malignant lymphoma tumor which was surgically resected. The patient is still in complete remission now.
Keywords: Malignant lymphoma, Double-balloon enteroscopy
INTRODUCTION
The small intestine, only partially accessible with push-type endoscopy, is the site of most undiagnosed lesions. Enteroscopy with the double-balloon system, an endoscopic technique developed by Yamamoto et al[1-3], enables examination of the entire small intestine with simultaneous tissue sampling and a variety of therapeutic interventions. A case is described in which double-balloon enteroscopy was used to diagnose malignant lymphoma in a patient with abdominal pain.
CASE REPORT
A 73-year old man presented with a history of abdominal pain during the previous year. The medical history was otherwise insignificant; physical examination showed a tender point in the right lower abdomen and the vital signs were within normal ranges. Laboratory test results included the following: hematocrit, 33.3% (normal: 40.4%-51.1%); Hb, 10.6 g/dL (14-18 g/dL); serum iron, 20 mcg/dL (80-170 mcg/dL); serum ferritin, 183 ng/mL (30-400 ng/mL); LDH, 133 IU/L (119-211 IU/L); and slL-2R, 1207 U/mL (188-570 U/mL); test of stools for occult blood were positive. Upper endoscopy and colonoscopy with intubation of the terminal ileum were performed, but no abnormality was detected. Computed tomography was performed revealing wall thickening and localized dilation of the ileum in the pelvis (Figure 1). In addition, gallium-67 scintigraphy was performed and collection was detected in the pelvis (Figure 2). A papillary tumor in the dilated ileum was also found using the double-contrast barium study of the small intestine (Figure 3). Enteroscopy with the double-balloon system (EN-450P5/20; Fujinon Co, Ltd, Saitama City, Japan) was performed by anal approach to evaluate the entire intestine.
Figure 1.

Computed tomography, showing localized dilation of the small intestine (arrows) in the pelvis.
Figure 2.
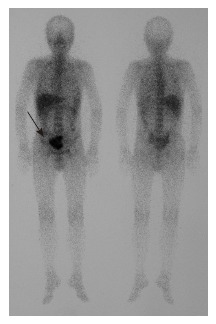
Gallium-67 scintigraphy, showing collection in the pelvis (arrow).
Figure 3.

Double-contrast barium study of the small intestine, showing a papillary tumor in the dilated ileum (arrows).
Full and informed consent was obtained from the patient before the procedure. The patient ingested 2L polyethylene glycol-based solution the day before the enteroscopic examination, which was performed with the patient under anesthesia. A papillary tumor, measuring 50 mm in diameter, was detected at 100 cm proximal to the ileocecal valve (Figure 4). It took 1 h to reach the lesion. Active bleeding was not from the tumor, thus, endoscopic treatment was not required, and no additional lesions were found in the proximal small intestine. The total time for the complete procedure was 2 h. Fluoroscopy was used to position the overtube (total radiography time: 10 min). There were no procedure-related complications. Histological findings from biopsy samples showed large atypical lymphoid lymphocytes. Immunohistochemically, these lymphocytes were positive for CD3 (Figure 5). Therefore, we confirmed the diagnosis of malignant lymphoma, diffuse large B-cell type.
Figure 4.
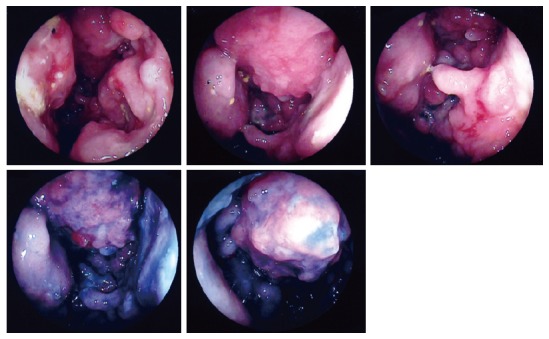
Double-balloon entero-doscopic examination, showing a papillary tumor at 100 cm proximal to the ileocecal valve.
Figure 5.
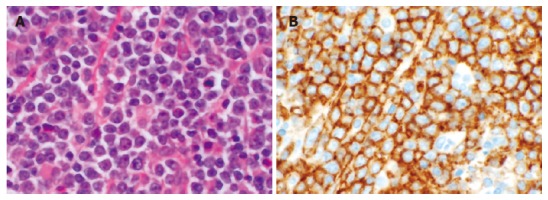
A: Histological findings demonstrated large atypical lymphoid lymphocytes, (HE, x 400); B: Immuno-histochemical analysis showed that these lymphocytes were positive for CD3. (CD3, x 400).
The patient underwent partial resection of the small intestine (180 mm in diameter). Microscopic findings of the resected small intestine showed an elevated lesion (110 mm × 85 mm × 50 mm) with central ulceration (Figure 6). Histologically, the tumor consisted of large atypical lymphoid lymphocytes. The tumor developed from the subserous mucosa and infiltrated bladder. Immunohistochemically, the tumor cells were positive for LCA, L-26, CD3 and UCHL-1. These findings were consistent with the tumor diagnosis of malignant lymphoma, diffuse large B-cell type.
Figure 6.
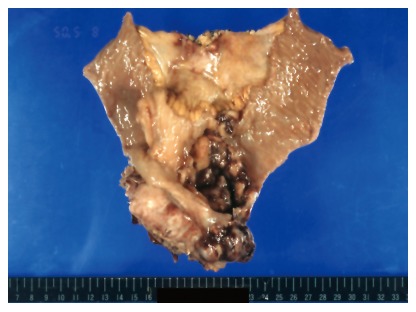
The resected specimen of ileum, showing an elevated lesion (110 mm × 85 mm × 50 mm) with central ulceration.
DISCUSSION
Although the gastrointestinal tract is the most common site of extra nodal malignant lymphoma, the small intestine (duodenum, jejunum and ileum) is reported as the site of origin for these lesions in only 15%-30% of gastrointestinal lymphomas[4]. Small-intestinal lymphomas are most often found in the duodenum 11%, jejunum 9%, ileum 29%, and ileocecal area 51%[5]. Histopathologically, B-cell lymphomas and T-cell lymphomas account for 85% and 15% of cases, respectively. Of the subtypes of B-cell lymphoma described in the new World Health Organization (WHO) classification, diffuse large B-cell lymphoma (DLBCL) is the most frequent (68.9%)[6].The overall prognosis of the more advanced stage of primary small intestinal lymphoma is only fair, with an expected 5-year survival of 25% to 30%[7]. In a retrospective analysis of 32 cases of primary small bowel lymphoma treated with either radical surgery plus polychemotherapy (early stages of IE and IIE), the overall 5-year survival was 59%[8].
Malignant lymphoma in the small intestine is difficult to diagnose in the early stages and is often found during emergency surgery in patients with a small bowel obstruction due to two reasons: First, clinical manifestations of small-intestinal lymphoma: anemia, abdominal pain, change in bowel habit, occult blood in stools, GI bleeding, obstruction and perforation (up to 25%) are not specific. Consequently the correct diagnosis is delayed[9]: Second, early diagnosis of malignant lymphoma is also delayed due to the difficulty in accessing the small intestine with conventional upper endoscopy and colonoscopy. Computed tomography (CT) as a frontline tool in the evaluation of abdominal symptoms can identify large masses but is not suitable for the diagnosis of small tumors[10]. Small-intestine radiography for the diagnosis of tumors is often difficult because of the complex looped configuration of the small intestine. CT and small-intestine radiography may be diagnostic, especially in advanced lesions, but they are relatively insensitive for early diagnosis of curable small intestinal tumors. Recently, wireless capsule endoscopy has made it possible to visualize the small intestine[11], but it has limitations such as the lack of air insufflations and the unavailability of rinsing. Consequently, neither of these examinations can be used to obtain biopsy specimens and carry out appropriate treatments.
Double-balloon enteroscopy is a new method of insertion enteroscopy that can explore the small intestine, with alternating steps of inflation and deflation of the two balloons, and alternating insertion of the endoscope and the overtube[2]. This approach enables the operator to visualize the entire small intestine, identify masses at the early stages and take biopsy specimens, the diagnosis of which is an important tool in small intestinal tumor. The exact classification(type and grade) of lymphoma can then be determined and the most suitable treatment can be administered. Consequently, the expected survival rate for patients with malignant lymphoma may increase.
In conclusion, double-balloon enteroscopy is a very useful method for the diagnosis of small intestinal tumors. Double-balloon enteroscopy represents an important diagnostic and therapeutic tool for small-intestine disease in combination with computed tomography and double-contrast barium study. The present case of anemia and abdominal pain demonstrates its diagnostic value before surgery for obtaining biopsy specimens. Using this method, it may be possible to diagnose small-intestinal lymphoma at the early stages more frequently and administer the most effective treatment based on diagnosis. As a result, the expected survival rate for patients with malignant lymphoma may increase.
Footnotes
S- Editor Liu Y L- Editor Alpini GD E- Editor Ma WH
References
- 1.Yamamoto H, Sugano K. A new method of enteroscopy--the double-balloon method. Can J Gastroenterol. 2003;17:273–274. doi: 10.1155/2003/309532. [DOI] [PubMed] [Google Scholar]
- 2.May A, Nachbar L, Wardak A, Yamamoto H, Ell C. Double-balloon enteroscopy: preliminary experience in patients with obscure gastrointestinal bleeding or chronic abdominal pain. Endoscopy. 2003;35:985–991. doi: 10.1055/s-2003-44582. [DOI] [PubMed] [Google Scholar]
- 3.Yamamoto H, Yano T, Kita H, Sunada K, Ido K, Sugano K. New system of double-balloon enteroscopy for diagnosis and treatment of small intestinal disorders. Gastroenterology. 2003;125:1556; author reply 1556–1557. doi: 10.1016/j.gastro.2003.03.004. [DOI] [PubMed] [Google Scholar]
- 4.Amer MH, el-Akkad S. Gastrointestinal lymphoma in adults: clinical features and management of 300 cases. Gastroenterology. 1994;106:846–858. doi: 10.1016/0016-5085(94)90742-0. [DOI] [PubMed] [Google Scholar]
- 5.Kohno S, Ohshima K, Yoneda S, Kodama T, Shirakusa T, Kikuchi M. Clinicopathological analysis of 143 primary malignant lymphomas in the small and large intestines based on the new WHO classification. Histopathology. 2003;43:135–143. doi: 10.1046/j.1365-2559.2003.01659.x. [DOI] [PubMed] [Google Scholar]
- 6.Nakamura S, Matsumoto T, Takeshita M, Kurahara K, Yao T, Tsuneyoshi M, Iida M, Fujishima M. A clinicopathologic study of primary small intestine lymphoma: prognostic significance of mucosa-associated lymphoid tissue-derived lymphoma. Cancer. 2000;88:286–294. doi: 10.1002/(sici)1097-0142(20000115)88:2<286::aid-cncr7>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 7.Liang R, Todd D, Chan TK, Chiu E, Lie A, Kwong YL, Choy D, Ho FC. Prognostic factors for primary gastrointestinal lymphoma. Hematol Oncol. 1995;13:153–163. doi: 10.1002/hon.2900130305. [DOI] [PubMed] [Google Scholar]
- 8.Zinzani PL, Magagnoli M, Pagliani G, Bendandi M, Gherlinzoni F, Merla E, Salvucci M, Tura S. Primary intestinal lymphoma: clinical and therapeutic features of 32 patients. Haematologica. 1997;82:305–308. [PubMed] [Google Scholar]
- 9.PAGTALUNAN RJ, MAYO CW, DOCKERTY MB. PRIMARY MALIGNANT TUMORS OF THE SMALL INTESTINE. Am J Surg. 1964;108:13–18. doi: 10.1016/0002-9610(64)90072-8. [DOI] [PubMed] [Google Scholar]
- 10.Gill SS, Heuman DM, Mihas AA. Small intestinal neoplasms. J Clin Gastroenterol. 2001;33:267–282. doi: 10.1097/00004836-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 11.de Mascarenhas-Saraiva MN, da Silva Araújo Lopes LM. Small-bowel tumors diagnosed by wireless capsule endoscopy: report of five cases. Endoscopy. 2003;35:865–868. doi: 10.1055/s-2003-42625. [DOI] [PubMed] [Google Scholar]


