Abstract
Study Objectives:
To examine the sleep patterns and the role of day of the week and school break in these patterns within a primarily obese sample of children.
Methods:
Participants included 143 obese children (8-12 years) and their parents initiating treatment in a weight-management study in a community-based setting. Demographics, anthropometrics, and objectively measured sleep (i.e., with use of Sensewear Armbands) were collected prior to treatment.
Results:
Sleep duration was insufficient in our sample, as approximately 88% obtained less than 8 hours of sleep (mean = 6.92, standard deviation = 0.85). Those with lower total sleep time included older children, those identified as African American (compared to those identified as Caucasian), and those identified as Non-Hispanic (compared to those identified as Hispanic). Children on school break initiated sleep later than those in school the week of measurement. Children woke later on weekends and when on school break. There were no differences in day of the week or school break in predicting child sleep duration and total wake time (p's > 0.05).
Conclusions:
This study is one of the first to examine sleep patterns within a primarily obese sample of treatment-seeking rural children. There is a need for research to develop a better understanding of how sleep may affect health functioning and weight management, as well as quality of life and psychosocial functioning of children who are overweight or obese.
Clinical Trials Information:
Title of trial: Extension Family Lifestyle Intervention Project (E-FLIP for Kids). Clinical-Trials.gov identifier: NCT01820338. NIH/NIDDK Grant #: 1R18DK082374-01.
Citation:
Graef DM, Janicke DM, McCrae CS. Sleep patterns of a primarily obese sample of treatment-seeking children. J Clin Sleep Med 2014;10(10):1111-1117.
Keywords: sleep duration, obesity, children, treatment-seeking
The prevalence of high adiposity in children in the United States is of great health concern. Nearly 32% of children and adolescents are overweight or obese (i.e., body mass index [BMI] ≥ 85th percentile for age and gender).1 Children who are overweight or obese are at increased risk for high cholesterol, triglycerides, and glucose, as well as hypertension, metabolic syndrome, and insulin resistance.2,3 Pediatric obesity is also associated with greater risk for low self-esteem, peer victimization, and poor quality of life compared to non-overweight peers.4–6
Risk for higher weight status can be due to a variety of distal factors including genetic vulnerabilities, medical conditions, basal metabolic rate, medication regimens, and neurotransmitter activity regulating hunger and satiety. However, at the most proximate level, it is an issue of energy intake and energy expenditure.7 Sleep is one behavioral factor that can impact risk for higher weight status, as a number of studies have revealed that obese children are more likely to experience sleep problems than non-overweight peers, including sleep disordered breathing, later sleep onset, shorter sleep duration, excessive daytime sleepiness, and more fragmented sleep.8–9 Children who obtain less sleep have greater odds of concurrent and future overweight status when compared to children receiving adequate sleep.10–12 Improvement in sleep can also play an important role, as a one hour increase is associated with a 20% to 80% reduction in odds of overweight or obesity.10,12
BRIEF SUMMARY
Current Knowledge/Study Rationale: Children who are obese are more likely to experience sleep problems than non-overweight peers, which can play an important role in child psychosocial functioning. However, there is a dearth of research examining sleep duration and sleep patterns within overweight and obese samples of children.
Study Impact: This study is one of the first to examine sleep patterns within a sample of obese children and found that roughly 88% attained less than eight hours of sleep. Obesity-related sleep difficulties are likely to affect a substantial number of children in the future, suggesting there is a need to understand how sleep may impact health, weight management, quality of life, and psychosocial functioning of children who are overweight or obese.
Sleep plays an important and unique role in the overall functioning of children, as it can affect health and functioning across physical, cognitive, emotional, and social domains.13 Problematic sleep can result in physiological consequences, including increased sympathetic tone, altered glucose metabolism associated with insulin resistance, and increased hypertension and inflammatory markers associated with cardiovascular risk.10,14 Shorter sleep may result in altered cortisol release that can impact individual response to stress, suggesting that sleep can play a salient role in psychosocial functioning.15 Sleep problems are associated with behavioral difficulties such as oppositional behavior and poorer executive functioning.16,17 Childhood sleep problems are also linked to poorer emotional functioning, including greater emotional lability, increased depressive and anxiety symptoms, and lower perceived health and quality of life.16–19
While numerous advances have been made in the literature, there are still gaps in our understanding of factors that affect child sleep. Notably, there is a dearth of research examining sleep within overweight and obese populations. Research commonly focuses on sleep-related breathing disorders rather than sleep duration.18,19 Moreover, much of research in obese populations relies on subjective and single-question measures. These studies are important for establishing relationships between sleep and weight, but there is concern regarding the reliability and validity of these measures compared to objective sleep measures.20 Another limitation of the literature is the varying reference values for sleep duration, as inconsistencies fail to take into account developmental expectations for sleep and make comparison across studies difficult. Sleep duration is an important factor to consider given the impact sleep and weight can have on child health, psychosocial functioning, and QOL. The purpose of the current study was to address the limitations within the literature on weight status and sleep by examining objectively measured sleep patterns within a treatment-seeking sample of overweight and obese children.
METHODS
Description of the Larger Study
This institutional review board (IRB) approved study is part of a larger grant-funded randomized controlled trial evaluating the impact of behavioral interventions on child weight status in a rural overweight and obese sample, the Extension Family Lifestyle Intervention Project for Kids (E-FLIP for Kids).21 All data were taken from initial screening and baseline assessment visits completed with each family prior to beginning the treatment program.
Participants
Participants included overweight and obese children (ages 8-12 years) and their parent or legal guardian living in one of 10 rural counties in north-central Florida. Families were included in the study if the family resided in a rural county and if the child's BMI was ≥ 85th percentile for age and gender norms described by the Center for Disease Control and Prevention (CDC).22 Families were excluded if they had a medical condition that would make participating in a weight management program unsafe, had participated in another weight management program, if the parent or child did not provide informed consent or assent, and if the child was identified as having severe cognitive or developmental delays. Those families meeting eligibility at the screening visit attended a baseline assessment visit to complete questionnaires and physical assessments one to two weeks prior to the start of treatment.
Procedure
Participants were recruited through a variety of methods, including press releases, direct mailings to households and health-care providers, and brochure distribution to local schools, churches, and community events. Interested families called the research office to learn more about the program and complete a phone screening for initial eligibility criteria. In-person screening and baseline assessments were conducted at the Cooperative Extension office in the county in which they resided. At the initial screening visit, families completed informed consent and assent, as well as measures of height and weight to determine study eligibility.
A total of 305 families completed in-person eligibility screening, while 269 completed a baseline assessment, of which 250 accepted randomization and received the accelerometers. Of the 250 remaining participants, 107 children (42.8%) did not wear the armband for the required amount of time (≥ 5 nights) for useful and valid data analysis. There were no significant sociodemographic differences in those who did and did not have enough armband data to be included in the analyses.
Measures
Anthropometrics
Child height was measured to the nearest 0.1 centimeter using a Harpedon Stadiometer and weight to the nearest 0.1 kilogram using a digital scale. BMI z-scores were calculated using age and genders norms from the CDC.22
Demographic questionnaire
Parents completed a background information questionnaire during the initial screening visit. Demographic information collected included child age, gender, race or ethnicity, and household income.
Pediatric sleep duration
Children were instructed to wear a Sensewear Pro3 Armband Accelerometer (Bodymedia, Inc., Pittsburgh, PA) for 7 consecutive days, 24 hours per day as a measure of sleep.23 The Sensewear Armbands are devices worn on the back of the upper right arm that provide measures of energy expenditure and detect sleep using several biometric sensors that include heat flux, skin temperature, galvanic skin response, near-body temperature, and movement using a tri-axial accelerometer with a sampling frequency of 32 Hz.23–24 The tri-axial accelerometer provides indicators of motion and whether an individual is lying down, while changes to heat-flux and skin temperature can offer information regarding whether an individual is asleep.25 The armbands utilize a pattern recognition (i.e., machine learning) approach to estimate sleep and the algorithm was developed using lab-based polysomnography data.24,26 The demographic-specific sleep algorithms (i.e., age, gender, height, weight) were developed using a 3-step process, including a screening, analysis using PSG, and clarification of short wakeful events.26
The validity of the armband in estimating sleep-wake patterns in children and adolescents is promising. Measures of total sleep time, sleep onset latency, and sleep efficiency are not significantly different from gold-standard polysomnography; however, the armbands do slightly overestimate wake after sleep onset.24 Although there is large variability in the agreement between the 2 devices, the variation is less substantial than armband use with adults and armbands can be used for group-level comparisons.24 Strengths of the device include it having similar agreement with polysomnography across a wide range of sleep efficiencies, there being no significant effect of child gender or weight status, and it being a minimally invasive approach to obtaining sleep values over longer periods of time than possible with polysomnography.24
Sleep data were obtained using the Sensewear Professional Software (SenseWear Professional software version 7.0; Body-Media Inc). The program enables users to export the 24-h data into a spreadsheet that provides date and time-stamped 60-s epochs of data, with sleep being scored as “1” and awake being scored as “0.” Sleep onset was defined as the first minute in which there were ≥ 3 consecutive min scored as sleep and sleep offset was the last minute of ≥ 5 consecutive min scored as sleep. Sleep onset latency (SOL) was considered the number of minutes in which the child was lying down prior to sleep onset. Sleep period was defined as the number of minutes elapsed during the sleep period scored as “not asleep” (i.e., scored as “0”). Total sleep time (TST) was calculated by summing the number of minutes scored as sleep. Sleep efficiency was measured as the percentage of minutes during the sleep period that were considered sleep (i.e., [sleep minutes/sleep period] × 100). Finally, total wake time (TWT) was defined as the number of nighttime wake minutes, including SOL, WASO, and the time the child lay in bed after sleep offset. Participants were included in the current study if they had 5 nights of sleep data (i.e., 3 week-nights and 2 weekend nights).
Statistical Analyses
Bivariate correlations and t-tests were used to examine possible sociodemographic differences across child sleep variables. Means and standard deviations were calculated for each sleep variable for all measured days, weekdays, and weekends. A repeated measures ANOVA was conducted to examine whether the time of measurement (i.e., in school versus on break) and the day of the week (i.e., weekday versus weekend) predicted child sleep variables. The between-subjects factor was the time of measurement and the within-subjects factor was the day of the week. It was hypothesized that sleep patterns would differ across weekdays when compared to weekends and for children who were on school break versus attending school the week their sleep was measured. Expected differences included significantly greater SOL, shorter sleep duration, greater WASO, lower sleep efficiency, and earlier time of sleep offset on week-days (versus weekends) and during the week of school (versus school break).
RESULTS
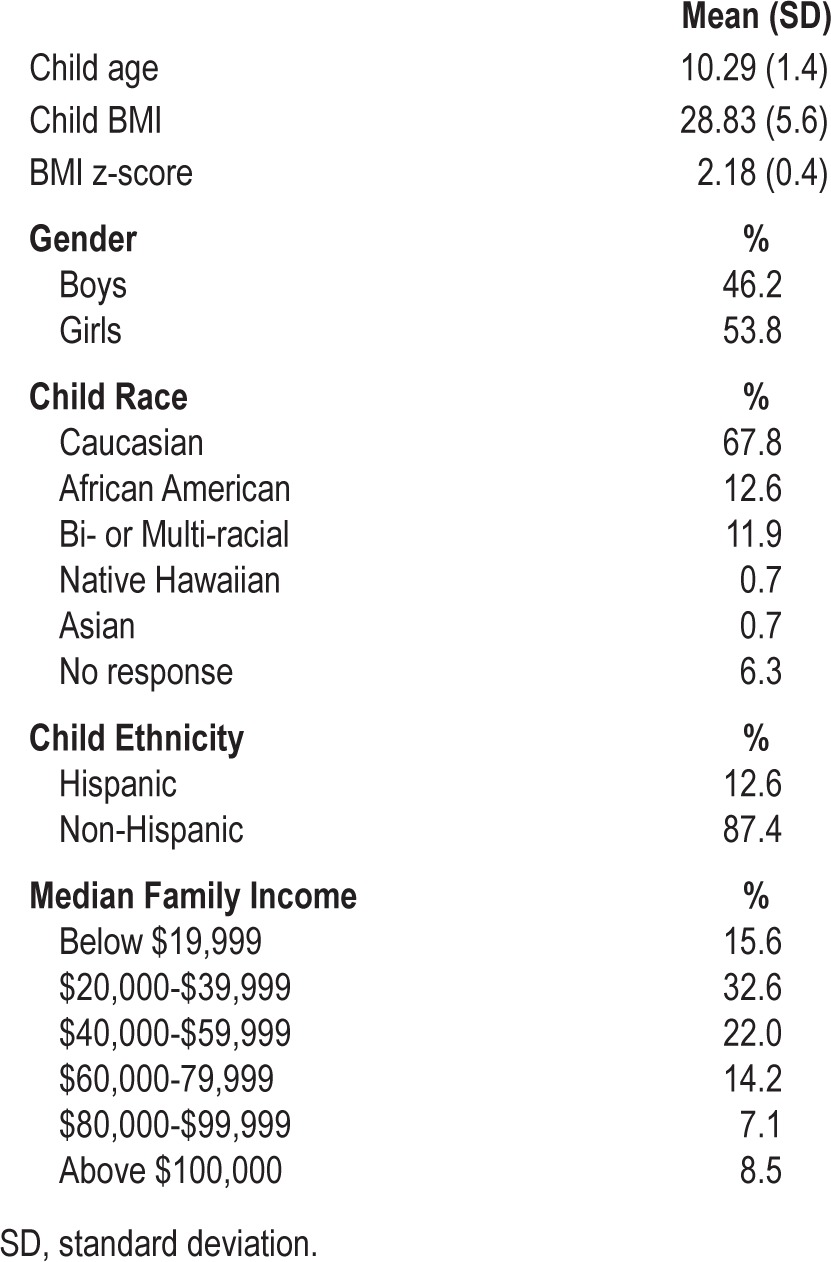
There were 143 children between the ages of 7.7 and 12.9 years (mean = 10.29, standard deviation [SD] = 1.4) who had complete data. The sample was primarily obese (i.e., 89.5%; BMI z-score ≥ 1.645), with the mean BMI being 28.83 kg/m2 (SD = 5.6) and the mean BMI z-score being 2.18 (SD = 0.4). The sample consisted of 77 girls (53.8%) and 66 boys (46.2%). The majority of the sample of parents reported their child's race as Caucasian (67.8%), while the remaining 32.2% of parents identified their child as African American (12.6%), biracial or multiracial (11.9%), no response (6.3%), Native Hawaiian (0.7%), and Asian (0.7%). Approximately 12% of parents identified their child's ethnicity as Hispanic. Participating parents or legal guardians consisted primarily of females (94.3%) and 69.2% indicated that they were married. Average parent BMI was 36.15 kg/m2 (SD = 10.6), classified as class II obesity. The median family income ranged from $40,000 to $59,999. Demographic information for the sample is presented in Table 1.
Table 1.
Demographic characteristics of sample.
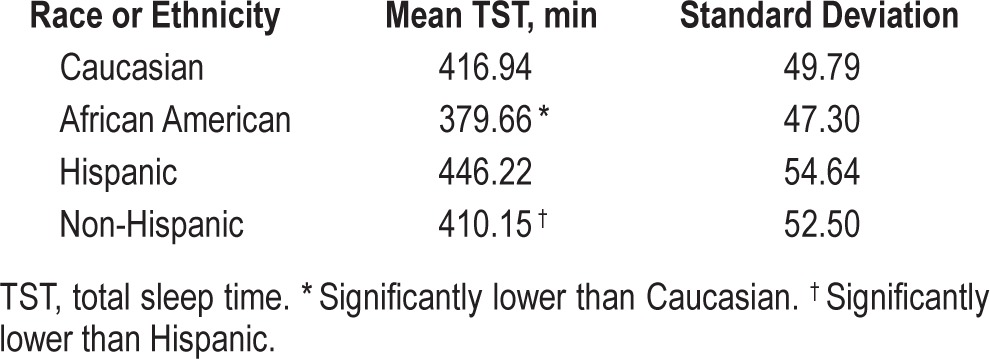
Bivariate correlations between child age and average TST was significant (r = -0.26, p < 0.01), such that older children obtained significantly less sleep than younger children. Correlations between race and TST was also significant (r = 0.23, p < 0.01). The follow-up t-test revealed that children identified as African American (i.e., both Hispanic and non-Hispanic) obtained significantly less sleep on average (mean = 379.66 min or 6.33 h) than children identified as Caucasian (mean = 416.94 min or 6.95 h; t116 = -2.95, p = 0.004). Additionally, children identified as Hispanic obtained more sleep on average (mean = 446.22 min or 7.44 h) than children identified as non-Hispanic (mean = 410.15 min or 6.84 h; t137 = -2.71, p = 0.008). Means and standard deviations for these comparisons can be found in Table 2. There were no sociodemographic variables that were significantly correlated with child TWT.
Table 2.
Total sleep time by race and ethnicity.
The aim of the study was to describe the sleep patterns of a primarily obese sample of children and examine the potential role of time of measurement (i.e., school year versus school break) and day of the week (i.e., weekday versus weekend). Means and standard deviations for sleep variables can be found in Table 3. Average time of sleep onset and offset were 23:59 and 07:15, respectively. Sleep onset latency averaged 13.73 min and WASO averaged 84.45 minutes. Children spent an average of 496.92 min (SD = 54.76) in bed from sleep onset to offset, equating to approximately 8 h 17 min. Mean TST (mean = 6.92 h, SD = 0.85) was well below the recommended quantity of 9 h sleep per night. Moreover, 88.1% of the sample averaged < 8 h of sleep per night and none of the participants averaged above 9 hours. Mean TWT ranged from 8.30 to 237.60 min (mean = 112.42, SD = 37.05). The mean sleep efficiency was 83.29% (SD = 6.54), which was below the “healthy” range of ≥ 90%. Twenty-eight percent of the sample had sleep efficiency < 80%; only 16.8% had an efficiency ≥ 90%.
Table 3.
Mean sleep variables across all days of the week and time of measurement.
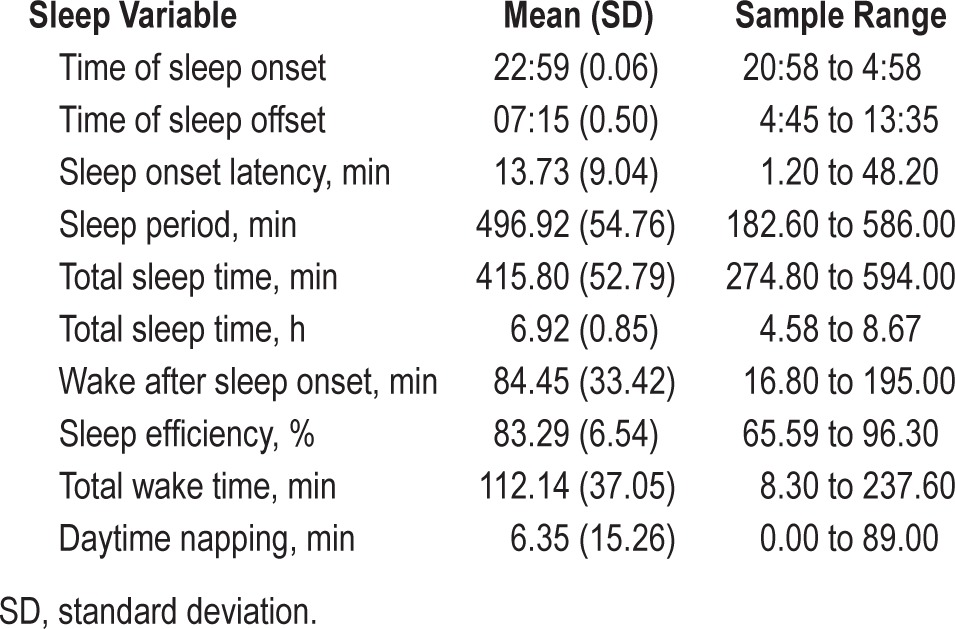
Table 4 displays the means and standard deviations of the sleep variables separately for day of the week and school break. There was a main effect of school break on the time of sleep onset, such that children on school break went to sleep much later than those in school (F1,138 = 11.54, η 2p = 0.08, p = 0.001). There were also main effects of day of the week (F1,138 = 20.99, η2p = 0.13, p < 0.001) and school break (F1,138 = 41.48, η2p = 0.23, p < 0.001) on the time of sleep offset, such that children had a later time of sleep offset on weekends (versus weekdays) and school break (versus when in school). There were no other main effects in predicting the remaining sleep variables (p's > 0.05).
Table 4.
Mean sleep variables separately across day of the week and school break.
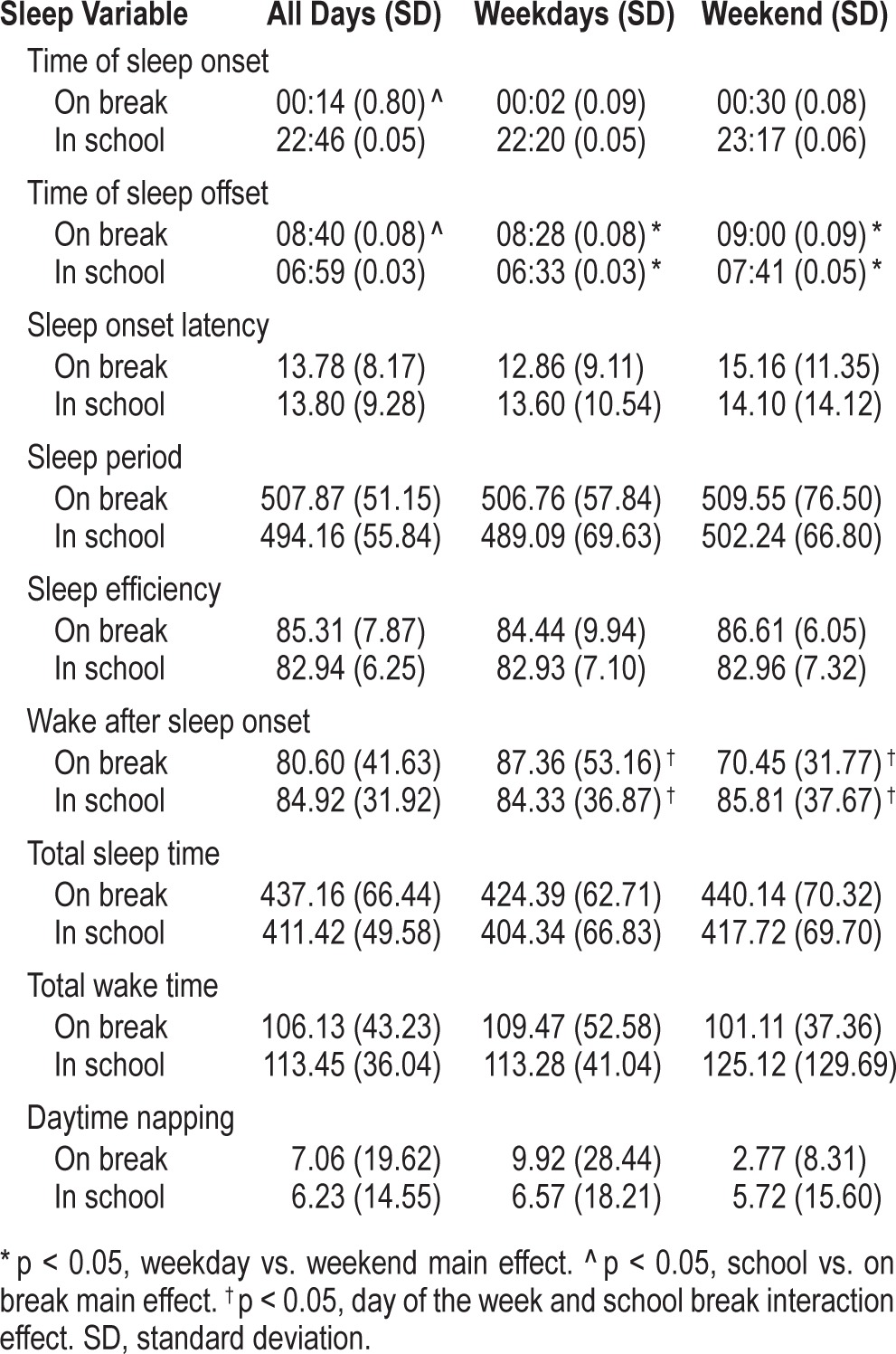
There were few significant findings when examining the potential role of the interaction between the day of the week and school break. There was a significant interaction effect detected in predicting WASO (F1,138 = 4.13, p = 0.044). Children on school break spent fewer minutes awake after sleep onset on weekends (mean = 87.36, SE = 8.48) than on week-days (mean = 70.46, SE = 7.85), while children in school had a similar WASO for both weekdays (mean = 84.33, SE = 3.66) and weekends (mean = 85.81, SE = 37.67).
DISCUSSION
The current study is one of the first to examine sleep patterns within a strictly treatment-seeking overweight and obese sample of children. Most notably, a vast majority of the children exhibited sleep insufficiencies, as approximately 88% of children averaged eight or fewer hours of sleep per night, spent a large amount of time awake at night, and only about 17% of the sample had optimal sleep efficiency. These findings are consistent with research examining the trend towards shorter sleep in a large, nationally representative sample of children.27 However, it is noteworthy that 11% of the national sample obtained less than 8 hours of sleep and is in contrast to the approximately 88% of our sample.27
The percentage of children experiencing insufficient TST in our sample is even greater than reported by Beebe and colleagues, who compared objectively measured sleep of obese adolescents attending a weight management clinic (Mage = 13.1 years; BMI ≥ 95th percentile) to a control group of healthy weight and overweight adolescents (Mage = 12.6 years; RangeBMI = 24th to 92nd percentile).8 Beebe found that 26% of healthy weight and overweight adolescents (MBMIz = 0.26, SD = 0.61) and 56% obese adolescents (MBMIz = 2.48, SD = 0.30) averaged less than 8 hours of sleep.8 The proportion of obese children in the current study obtaining inadequate sleep compared to those in the Beebe study suggests that trends towards decreased sleep may be more substantial in rural obese samples. It is possible that children in rural areas may need to travel further to school and rise earlier in the morning than non-rural samples. It is also possible that differences in sleep found between both studies reflect the younger child age and lower child weight status in the current sample. However, this is contrary to research that has reported later time of sleep onset and shorter sleep duration in older children.28 Although obese children in both samples exhibited low percentages of children achieving 8 hours of sleep per night, the sleep period for children in the current study (mean = 496.92 min, SD = 54.76) was greater than the obese sample in the Beebe study (mean = 469.00 min, SD = 50; t142 = 6.01, p < 0.001). This difference in mean numbers but not in percentage achieving 8 hours of sleep may be due to the greater variability in the sleep data in the current study.
Children in our study went to sleep significantly later when on school break and woke up significantly later on weekends and when on school break. These findings are generally consistent with the literature examining sleep patterns in childhood and adolescence.29,30 As expected, children on school break spent fewer minutes awake after sleep onset (WASO) on weekends when compared to weekdays, while there were no significant differences in WASO across the day of the week for children who were in school the week of measurement. Differences in sleep patterns across days of the week and school attendance are important to consider given that irregularities in the sleep schedule and timing are frequently associated with shorter sleep duration.31 The time of sleep onset, regardless of the day of the week, was late for the age group of our sample (22:59) and may be a possible area for intervention to address concerns with inadequate sleep duration.
Contrary to our hypothesis, there were no significant main or interaction effects of day of the week (weekday versus weekend) and school break across the remaining sleep variables (SOL, TST, TWT, and sleep efficiency). An additional unexpected finding was the delayed sleep preference (time of sleep onset and offset increased by one hour on weekends) in children who were attending school during measurement, such that the sleep-wake shift did not result in weekend sleep extension or greater sleep efficiency. This is contrary to research with adolescents that indicate that a shift to later and more preferred bedtimes on weekends is associated with improved SOL, TST, and sleep efficiency.30,31 One potential explanation for the limited differences across sleep variables is the degree of variability of sleep in our sample. Although a smaller range of data can limit detection of significant relationships, highly variable data (i.e., higher standard deviation) may indicate that the sample mean does not accurately represent the variable being measured due to higher random error.32 However, the majority of participants fell within two standard deviations of the mean, suggesting that this was not the case in this study.
Comparison of weekday versus weekend TST and sleep efficiency between the current study sample relative to the obese and control groups in the Beebe study are noteworthy. Beebe and colleagues found that sleep duration and efficiency differences between the control group (non-overweight and over-weight) and obese group were more pronounced on weekends due to a later time of sleep onset in the obese group.8 Similarly, children in the current sample averaged significantly less weekend sleep (t142 = -8.77, p < 0.001) and weekend sleep efficiency (t142 = -7.93, p < 0.001) than the Beebe control group. These findings are in contrast to group comparisons for weekday sleep. Average weekday sleep was not significantly different between our sample and the Beebe non-obese group (t142 = -1.12, p = 0.27). However, our sample had significantly lower sleep efficiency (t142 = -6.26, p < 0.001). This is noteworthy given the dearth of research examining sleep duration and efficiency in children of varying weight status. The finding that obese children obtain poorer sleep efficiency despite non-significantly different overall weekday sleep than non-obese children suggests that focusing on the negative effects of lower sleep duration in obese populations does not necessarily equate with sleep efficiency. Sleep efficiency takes into account wake time during the night, suggesting that the amount of time spent awake is important to examine. Future research should also consider factors that may contribute to poor sleep efficiency in these children, including anxiety or stress related to peer victimization or low self-esteem and screen time use (i.e., TV, phone, computer).
In the current study there was a negative association between child sleep time and child age. Moreover, African American children obtained less sleep than Caucasian children. These findings are consistent with previous research examining child age and ethnic/minority status.33,34 Contrary to the findings of previous research, there continued to be significant differences in TST between Caucasian (mean = 423.47 min) and African American children (mean = 385.34 min) when sleep also included time spent in daytime napping.33 There were also significant ethnic differences in sleep, as children identified as Non-Hispanic obtained less sleep than those identified as Hispanic. Silva and colleagues noted that sleep patterns and risk for higher weight status vary by ethnicity, such that Hispanics were at greater risk of shorter sleep and obesity compared to Non-Hispanics at follow-up, regardless of sleep duration.35 Although the findings of the current study indicated that sleep patterns vary by ethnicity, findings were contrary to what was noted by Silva et al., and there were no significant differences in weight status between ethnic groups. Additional research is needed to examine potential social and environmental influences of sleep patterns across racial and ethnic groups, as well as whether the impact of short sleep on subsequent weight gain varies by ethnicity. There were no sociodemographic variables that were significantly associated with child TWT.
The current study had several strengths, including the use of an objective measure of sleep duration in a strictly overweight and obese treatment-seeking sample of children and their parents. However, there were several methodological limitations of the study. One limitation was the cross-sectional design that limited our ability to make causal statements in our results. An additional limitation was the treatment-seeking sample that included a highly restricted range of weight status (89.5% obese), which may have precluded our ability to make them distinguishable from the general population of children who are overweight or obese. However, the main goal of the study was to elucidate the sleep patterns within obese samples by examining the role of objectively measured sleep.
Another limitation was the use of Sensewear Armbands (SWA) as a sleep measure. Although the SWA has the advantage of unobtrusive and extended monitoring, there is scant research examining its use in pediatric sleep. The only study to date examining agreement between SWA and PSG in children found no systematic bias in estimating sleep (TST, SOL, and sleep efficiency).24 However, the large variability of the agreement resulted in substantial random error and suggests that SWA is recommended only for group-level analyses.24,30 An additional limitation was the number of excluded participants (N = 107, 42.8%) due to the lack of adequate sleep data for useful and valid analysis, resulting in analyses being conducted with less power. While this suggests possible biases in the study findings, there were no significant sociodemographic differences between those who did and did not have enough sleep data.
Despite the limitations noted in the use of Sensewear Arm-bands, each approach to assessing pediatric sleep provides unique information and carries different strengths and weaknesses. Polysomnography (PSG) is considered the “gold standard” for sleep physiology and for diagnosing sleep related breathing disorders and periodic limb movement disorder.36 Actigraphy is an objective measure that can be used within the home environment that provides information about sleep-wake behaviors.23,37 However, actigraphy has poor specificity when compared to PSG and there is a lack of consistency in the device, epoch length, and algorithm used across studies.38 Daily sleep diaries are the “gold standard” measure of insomnia and allow for correction of sleep artifacts associated with actigraphy (e.g., external movements in vehicles).36,39 The Sensewear Armbands are a novel objective sleep measure that have a similar agreement with PSG across a wide range of sleep efficiencies and show no significant effect of child gender or weight status.24 A single time point measurement, regardless of the measure, has limitations due to the variability of sleep behavior. It is therefore important for assessment to include multiple measures that can complement one another and address individual weaknesses.36,40
Clinical Implications and Future Directions
Given the current prevalence of high child adiposity in the U.S., the strong association between short sleep and weight status, and the potential negative long-term impact of each, obesity-related sleep difficulties are likely to affect a substantial number of children and adolescents in the future. There is, therefore, a need for research to develop a better understanding of how sleep may impact not only health functioning and weight management, but also quality of life and psychosocial functioning of children who are overweight or obese.
Future research should include a multi-method and longitudinal assessment approach to examine child- and parent-reported child sleep problems, well-validated objective sleep measures (e.g., actigraphy or accelerometry and PSG), and sleep diaries to account for artifacts of the objective measures. This information is needed to obtain more conclusive information about the direction of the relationship between sleep and weight, as well as sleep and child psychosocial functioning in an obese population. Given the degree of insufficient sleep in our study and the impact it can have on child functioning, it is reasonable to speculate that improved sleep may be associated with improvements in child well-being. Prospective research using a larger sample size and use of well-validated measures of sleep duration, as well as perceived sleep problems or sleep quality are needed before drawing more definitive conclusions on these relationships.
DISCLOSURE STATEMENT
This was not an industry supported study. This study was funded by NIDDK grant 1R18DK082374-01. The funding organization had no role in data extraction and analysis, writing the manuscript, or the decision to submit the manuscript for publication. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307:483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175–82. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 3.Garnett SP, Baur LA, Srinivasan S, Lee JW, Cowell CT. Body mass index and waist circumference in midchildhood and adverse cardiovascular disease risk clustering in adolescence. Am J Clin Nutr. 2007;86:549–55. doi: 10.1093/ajcn/86.3.549. [DOI] [PubMed] [Google Scholar]
- 4.Janicke DM, Marciel KK, Ingerski LM, et al. Impact of psychosocial factors on quality of life in overweight youth. Obesity. 2007;15:1799–807. doi: 10.1038/oby.2007.214. [DOI] [PubMed] [Google Scholar]
- 5.McClure AC, Tanski SE, Kingsbury J, Gerrard M, Sargent JD. Characteristics associated with low self-esteem among US adolescents. Acad Pediatr. 2010;10:238–44. e2. doi: 10.1016/j.acap.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zeller MH, Saelens BE, Roehrig H, Kirk S, Daniels SR. Psychological adjustment of obese youth presenting for weight management treatment. Obes Res. 2004;12:1576–86. doi: 10.1038/oby.2004.197. [DOI] [PubMed] [Google Scholar]
- 7.Hill JO. Understanding and addressing the epidemic of obesity: an energy balance perspective. Endocr Rev. 2006;27:750–61. doi: 10.1210/er.2006-0032. [DOI] [PubMed] [Google Scholar]
- 8.Beebe DW, Lewin D, Zeller M, et al. Sleep in overweight adolescents: shorter sleep, poorer sleep quality, sleepiness, and sleep-disordered breathing. J Pediatr Psychol. 2007;32:69–79. doi: 10.1093/jpepsy/jsj104. [DOI] [PubMed] [Google Scholar]
- 9.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knutson KL. Impact of sleep and sleep loss on glucose homeostasis and appetite regulation. Sleep Med Clin. 2007;2:187–97. doi: 10.1016/j.jsmc.2007.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lumeng JC, Somashekar D, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics. 2007;120:1020–9. doi: 10.1542/peds.2006-3295. [DOI] [PubMed] [Google Scholar]
- 12.Landhuis CE, Poulton R, Welch D, Hancox RJ. Childhood sleep time and long-term risk for obesity: a 32-year prospective birth cohort study. Pediatrics. 2008;122:955–60. doi: 10.1542/peds.2007-3521. [DOI] [PubMed] [Google Scholar]
- 13.Mindell JA, Owens JA. Sleep 101. In: Mindell JA, Owens JA, editors. A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems. Philadelphia: Lippincott Williams & Wilkins; 2010. pp. 1–11. [Google Scholar]
- 14.Meier-Ewert HK, Ridker PM, Rifai N, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43:678–83. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- 15.Spiegel K, Leproult R, L'Hermite-Baleriaux M, Copinschi G, Penev PD, Van Cauter E. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89:5762–71. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]
- 16.Anderson B, Storfer-Isser A, Taylor HG, Rosen CL, Redline S. Associations of executive function with sleepiness and sleep duration in adolescents. Pediatrics. 2009;123:e701–7. doi: 10.1542/peds.2008-1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moore M, Kirchner HL, Drotar D, et al. Relationships among sleepiness, sleep time, and psychological functioning in adolescents. J Pediatr Psychol. 2009;34:1175–83. doi: 10.1093/jpepsy/jsp039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crabtree VM, Varni JW, Gozal D. Health-related quality of life and depressive symptoms in children with suspected sleep-disordered breathing. Sleep. 2004;27:1131–8. doi: 10.1093/sleep/27.6.1131. [DOI] [PubMed] [Google Scholar]
- 19.Carno MA, Ellis E, Anson E, et al. Symptoms of sleep apnea and polysomnography as predictors of poor quality of life in overweight children and adolescents. J Pediatr Psychol. 2008;33:269–78. doi: 10.1093/jpepsy/jsm127. [DOI] [PubMed] [Google Scholar]
- 20.Hart CN, Cairns A, Jelalian E. Sleep and obesity in children and adolescents. Pediatr Clin North Am. 2011;58:715–33. doi: 10.1016/j.pcl.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Janicke DM, Lim CS, Perri MG, et al. The extension family lifestyle intervention project (E-FLIP for Kids): design and methods. Contemp Clin Trials. 2011;32:50–8. doi: 10.1016/j.cct.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 23.van Wouwe NC, Valk PJ, Veenstra BJ. Sleep monitoring: A comparison between three wearable instruments. Mil Med. 2011;176:811–6. doi: 10.7205/milmed-d-10-00389. [DOI] [PubMed] [Google Scholar]
- 24.Soric M, Turkalj M, Kucic D, Marusic I, Plavec D, Misigoj-Durakovic M. Validation of a multi-sensor activity monitor for assessing sleep in children and adolescents. Sleep Med. 2013;14:201–5. doi: 10.1016/j.sleep.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Teller A. A platform for wearable physiological computing. Interact Comput. 2004;16:917–37. [Google Scholar]
- 26.Sunseri M, Liden CB, Farringdon J, et al. Pittsburgh: BodyMedia Inc; 2002. The SenseWear armband as a sleep detection device [Internet] [cited 2014 Feb 3]. Available from: http://www.bodymedia.com/Professionals/Whitepapers/The-SenseWear-armband-as-a-Sleep-Detection-Device. [Google Scholar]
- 27.Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 2007;78:309–23. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 28.Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Dev Psychol. 2000;36:291–301. doi: 10.1037//0012-1649.36.3.291. [DOI] [PubMed] [Google Scholar]
- 29.Hansen M, Janssen I, Schiff A, Zee PC, Dubocovich ML. The impact of school daily schedule on adolescent sleep. Pediatrics. 2005;115:1555–61. doi: 10.1542/peds.2004-1649. [DOI] [PubMed] [Google Scholar]
- 30.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 31.Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep, and daytime behaviour in adolescence. J Sleep Res. 2002;11:191–9. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- 32.Field A, editor. Discovering statistics using SPSS. London: Sage; 2009. Everything you ever wanted to know about statistics; pp. 35–43. [Google Scholar]
- 33.Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics. 2005;115:225–32. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spilsbury JC, Storfer-Isser A, Drotar D, et al. Sleep behavior in an urban US sample of school-aged children. Arch Pediatr Adolesc Med. 2004;158:988–94. doi: 10.1001/archpedi.158.10.988. [DOI] [PubMed] [Google Scholar]
- 35.Silva GE, Goodwin JL, Parthasarathy S, et al. Longitudinal association between short sleep, body weight, and emotional and learning problems in Hispanic and Caucasian children. Sleep. 2011;34:1197–205. doi: 10.5665/SLEEP.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 37.Littner M, Kushida CA, Anderson WM, et al. Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: an update for 2002. Sleep. 2003;26:337–41. doi: 10.1093/sleep/26.3.337. [DOI] [PubMed] [Google Scholar]
- 38.Meltzer LJ, Montgomery-Downs HE, Insana SP, Walsh CM. Use of actigraphy for assessment in pediatric sleep research. Sleep Med Rev. 2012;16:463–75. doi: 10.1016/j.smrv.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–92. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- 40.Morin CM. Measuring outcomes in randomized clinical trials of insomnia treatments. Sleep Med Rev. 2003;7:263–79. doi: 10.1053/smrv.2002.0274. [DOI] [PubMed] [Google Scholar]


