Abstract
Spinal tuberculosis is the most common manifestation of extra-pulmonary tuberculosis. It is difficult to diagnose the disease due to its insidious onset and non-specific clinical presentation. A high degree of suspicion and appropriate imaging studies are necessary for its early diagnosis and treatment. The authors report a case of lumbosacral tuberculosis in an adult patient presenting with hip pain and abscesses.
Background
Despite the improvement of public health policies and the availability of effective antitubercular drugs, tuberculosis (TB) remains a major infectious disease worldwide. According to the WHO, approximately nine million cases of TB are reported annually.1 Among the various forms of the disease, its vertebral presentation represents the main manifestation of extra-pulmonary TB, accounting for half the cases of osteoarticular TB.2
Non-specific signs and symptoms make the clinical diagnosis of spinal TB a real challenge to physicians. Delay in the diagnosis and initiation of treatment increases the risk of complications such as neurological deficit, abscesses and fistula.
We report a case of a 32-year-old patient with lumbosacral TB complicated with abscesses and fistula. At the time of the investigation, the patient had presented suppurative inflammatory lesions in the hip region. After diagnosis, the patient received medical and surgical treatment and showed significant clinical improvement.
Case presentation
In 2012, a Caucasian man aged 32, a stockist by trade, presented to our orthopaedic service with moderate pain in the right hip, and tumefaction and fistula at the level of the femoral greater trochanter with recurrent drainage of pus, even after various forms of treatment.
His history began in 2010 when, while playing sports, he fell to the ground, injuring his back. On the occasion, the blunt trauma had resulted in pain and swelling in the lumbosacral region without local skin injury.
Six months after the accident, still having pain and swelling in the lower back, he decided to seek care in another hospital. There was a worsening of symptoms, with the onset of intermittent fever and productive fistulas in the gluteal region. At that time, he was submitted to surgical drainage of the abscess in the gluteal region. Clinical treatment was introduced empirically with intravenous antibiotics. Shortly thereafter, he presented with recurrence of the frame with the emergence of new fistulas in the right hip region. MRI (figure 1) showed osteomyelitis at the right proximal femur. He was referred to our service. We chose to perform surgery at the right hip. The data analysis indicated the presence of Pseudomonas aeruginosa in the bone. With the diagnosis of bacterial osteomyelitis, treatment was performed with venous specific antibiotic therapy for a prolonged period.
Figure 1.
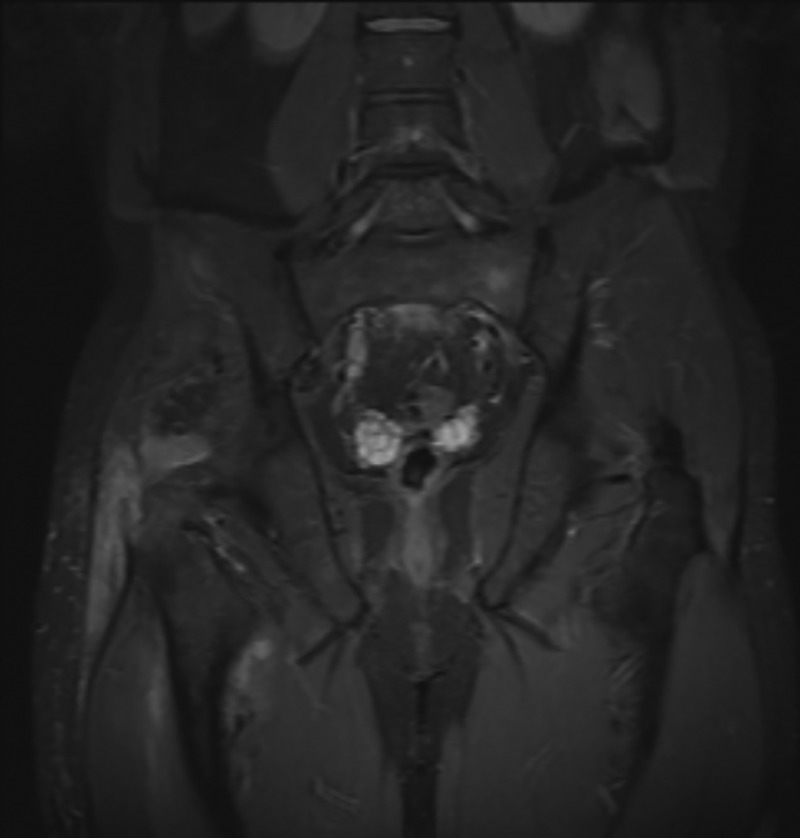
MRI identifying the peritrochanteric abscess in the right thigh and proximal femur osteomyelitis.
The patient returned to medical examination after 6 months. He presented low back pain, suppurative fistulas in the hip and displayed lumbar radicular symptoms, including Lasègue’s signal, antalgic gait and posture. We requested MRI, which found the presence of infiltrate involving the disc space of L5 and S1 vertebrae (figure 2). We performed surgery through an anterior abdominal approach for decompression of the spinal canal, debridement, material collection and stabilisation of the spine through the arthrodesis (figure 3).
Figure 2.

MRI demonstrating the lumbar osteomyelitis, with an abscess anteriorly of the sacral bones. It is dislocating posteriorly the dural sac and the cauda equina. The signal is abnormal in the lumbosacral vertebral bodies and discs.
Figure 3.
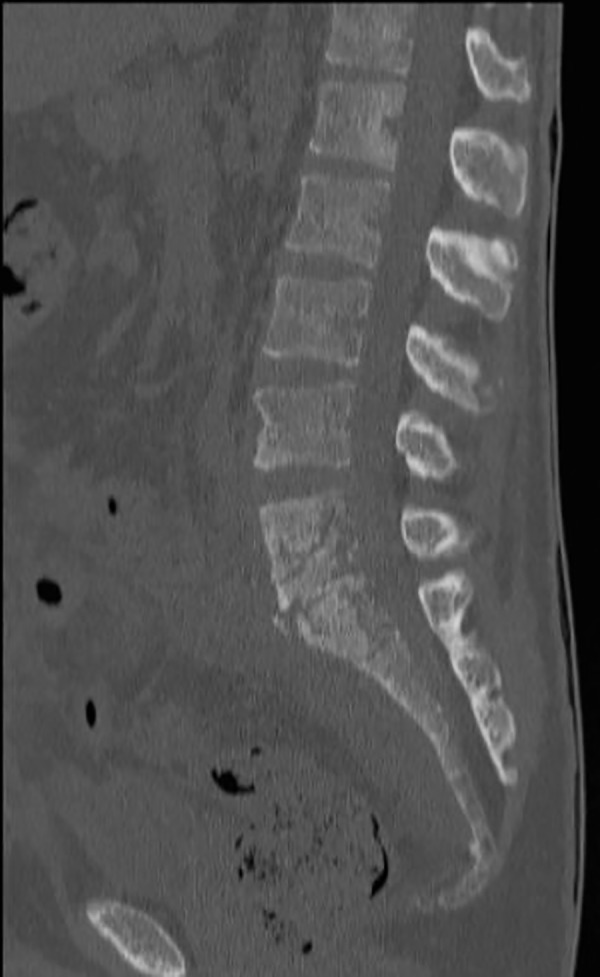
Anterior lumbosacral arthrodesis on CT scan.
The result of the histopathological examination was compatible with TB (figures 4–6). We started chemotherapy for TB with a duration plan of 6 months, to possibly be extended for up to 18 months, according to clinical development. At present, the patient has a clinical improvement and follows up with outpatient monthly reviews.
Figure 4.
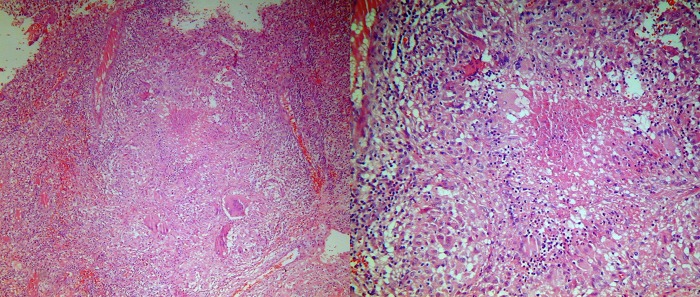
Histopathological study demonstrating the granulomatous formation in an inflammatory infiltrate, where it is possible to identify Langerhans’ giant cells and caseous necrosis.
Figure 5.
Langerhans’ giant cells with their peripherally arranged nuclei, in the left picture, and caseation (or cheesy) necrosis in the right.
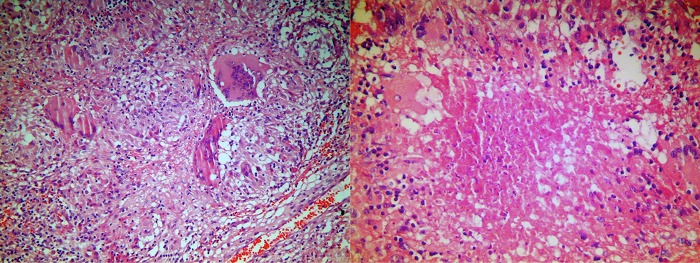
Figure 6.
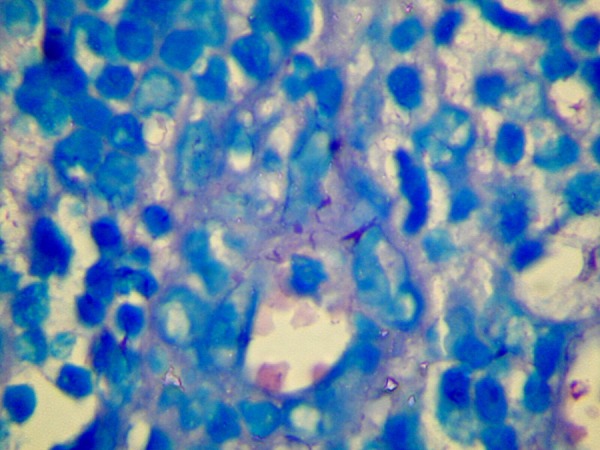
The Wade stain technique to identify acid-fast bacilli.
Investigations
Laboratory tests that may be used in the investigation of spinal TB are: Montoux Test (PPD Skin Test), erythrocyte sedimentation rate, ELISA and PCR.
The most frequently used imaging methods for the investigation of spinal TB include planar radiography, CT scan and MRI. The X-ray is the most used method for initial screening when infectious spondylitis is suspected. This examination, however, is often normal in the early stages of the disease. Calcifications in paraspinal abscesses are highly suggestive of TB3 and are well demonstrated by CT. Additionally, CT is considered the best method to guide percutaneous spinal biopsy. MRI is the gold standard method to evaluate spinal infection, combining high sensitivity and satisfactory specificity.4 In the images, it is possible to identify lesions of vertebral bodies with structural collapse, kyphotic deformity, retroperitoneal abscess formation, invasion of soft tissue and vertebral discs.
The diagnosis of tuberculous infection cannot be established based on imaging methods alone. Nevertheless, imaging studies are useful to assess the extent of the lesions, guide the aspiration biopsy, assist surgery planning and contribute to follow-up.
The biopsy of the initial focus of infection and the microorganism culture define the aetiological diagnosis and guide the treatment. However, culturing atypical pathogens takes much time and can lead to frequent false-negative results. The histopathological study can show the presence of granulomatous inflammatory infiltrate with caseous necrosis and Langerhans’ giant cells. The Ziehl-Neelsen stain can demonstrate acid-fast bacilli.
The main differential diagnoses that should be considered include pyogenic spondylodiscitis, actinomycosis, brucellosis, Salmonella osteomyelitis, syphilis, systemic fungal infections, and benign and malignant tumours of the vertebral column.2 5 6
Discussion
Clinical presentation of spinal TB is varied and basically depends on: the disease’s stage, the patient’s age, the affected site, and the presence or absence of complications. In the early stages, the most common symptoms are back pain and systemic symptoms such as asthaenia, anorexia, weight loss and fever. The reported average duration of symptoms before diagnosis of spinal TB is 4 months but can be considerably longer.7 This delay in diagnosis can be catastrophic since the progression of the disease can lead to severe complications such as spinal deformity, neurological weakness, cold abscesses and sinus tracts.4
Spinal TB mainly affects the thoracic and lumbar spine.2 7 8 The progressive bone destruction leads to vertebral collapse and kyphosis, especially in the thoracic spine.2 Furthermore, the extension of the infectious zones to adjacent structures is common, resulting in formation of abscesses in approximately 75% of cases.9 Usually, these abscesses seem to grow slowly and do not manifest any symptoms, which allows them to reach high volumes and to cause compression of the nerve structures leading to severe neurological sequelae. However, neurological deficit is not so common in cases of TB lumbosacral, such as in our patient, being more frequent when the thoracic spine is affected.7
Abscesses may be located in all paraspinal regions and their spread follows the paths of least resistance. In the lumbar region, they usually spread inferiorly through the intermuscular planes, mainly through the psoas sheath. Thus, purulent material can be found in different anatomical areas far away from the initial site of lesion. The main sites mentioned in the literature are: ischiorectal fossa; gluteal region; along the psoas sheath; lumbodorsal region (though the triangle of Petit); medial side of the thigh; femoral triangle; and popliteal fossa.5 Our patient had a history of gluteal and lumbar abscesses; nevertheless, when he came to us he only presented abscesses over the greater trochanter area.
Nowadays, there have been few reports about the management of lumbosacral TB and there is no established guideline for its treatment. According to a recent review article, the most currently used chemotherapy regimen is similar to that indicated for pulmonary TB, which includes rifampicin, isoniazid, pyrazinamide and ethambutol for 2 months, followed by another 4 months on rifampin and isoniazid. However, there is no consensus on the duration of treatment.
Depending on the clinical, laboratory and radiological findings, some physicians prefer longer treatment duration.10 Recent studies have shown increased use of treatment combining a clinical as well as surgical approach.8 10 The main indications for surgical treatment are neurological deficit, spinal deformity with instability or pain, failure of drug treatment and bulky paravertebral abscess. The goals of surgery are debridement and removal of the septic focus, sample collection for laboratorial examination, decompression of the spinal canal with stabilisation and restoration of the infected segment and subsequent bony fusion. When debridement is performed optimally, studies have shown that this procedure can increase the effectiveness of chemotherapy.10 There are also disagreements about the surgical approach to be adopted. Notwithstanding, in situations like the one described, we observed that the anterior approach is more appropriate. This is a safe approach that allows bone fusion, direct debridement of the paravertebral and intraspinal focus of infection.11 12
Finally, our case highlights that when a source of low back pain is elusive to work up, spinal TB should also be considered.
Learning points.
Vertebral tuberculosis is not an uncommon disease and must be considered.
Retroperitoneal abscesses can drain to the hip and manifest as symptoms.
Spinal fusion is important when there is vertebral deformity or instability.
Long-term specific antibiotics are necessary to treat bone tuberculosis.
Secondary infections can be found in the abscesses.
Acknowledgments
The authors are grateful for the histopathological study performed by Professors Porphirio José Soares Filho and Albino Fonseca Júnior.
Footnotes
Contributors: VSG performed the surgery and followed up the patient. DdSFJ and LdREJ reviewed the theme and collected data. GCSdA helped on diagnostic evaluation, and organised and edited the text. All authors took part in the text writing and revision.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.WHO. Global tuberculosis report 2013. Geneva: WHO Press, 2013 [Google Scholar]
- 2.Chauhan A, Gupta B. Spinal tuberculosis. J Indian Acad Clin Med 2007;8:110–14 [Google Scholar]
- 3.Tali ET Spinal infections. Eur J Radiol 2004;50:120–33 [DOI] [PubMed] [Google Scholar]
- 4.Rivas-Garcia A, Sarria-Estrada S, Torrents-Odin C, et al. Imaging findings of Pott's disease. Eur Spine J 2013;22(Suppl 4):567–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sankaran B Tuberculosis of bones & joints. Indian J Tuberc 1993;40:109–18 [Google Scholar]
- 6.Mete B, Kurt C, Yilmaz MH, et al. Vertebral osteomyelitis: eight years’ experience of 100 cases. Rheumatol Int 2012;32:3591–7 [DOI] [PubMed] [Google Scholar]
- 7.Turgut M Spinal tuberculosis (Pott's disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev 2001;24:8–13 [DOI] [PubMed] [Google Scholar]
- 8.Fuentes Ferrer M, Gutierrez Torres L, Ayala Ramirez O, et al. Tuberculosis of the spine. A systematic review of case series. Int Orthop 2012;36:221–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindahl S, Nyman RS, Brismar J, et al. Imaging of tuberculosis. IV. Spinal manifestations in 63 patients. Acta Radiol 1996;37:506–11 [DOI] [PubMed] [Google Scholar]
- 10.Varatharajah S, Charles YP, Buy X, et al. Update on the surgical management of Pott's disease. Orthop Traumatol Sur Res 2014;100:229–35 [DOI] [PubMed] [Google Scholar]
- 11.Li M, Du J, Meng H, et al. One-stage surgical management for thoracic tuberculosis by anterior debridement, decompression and autogenous rib grafts, and instrumentation. Spine J 2011;11:726–33 [DOI] [PubMed] [Google Scholar]
- 12.Luk KD Commentary: instrumentation in the treatment of spinal tuberculosis, anterior or posterior? Spine J 2011;11:734–6 [DOI] [PubMed] [Google Scholar]


