Abstract
Background:
Increasingly, older patients with severe spinal stenosis/instability undergo multiple unnecessary preoperative epidural spinal injections (ESI), despite their risks and lack of long-term benefits. Here we add to the list of risks by showing how often preoperative ESI lead to punctate cerebrospinal fluid (CSF) fistulas documented during subsequent surgery (e.g. multilevel laminectomies with non-instrumented fusions).
Methods:
A series of 39 patients with spinal stenosis/instability prospectively underwent multilevel laminectomy/non-instrumented fusion utilizing lamina autograft and NanOss Bioactive. We asked how often preoperative ESI were performed in this population and how frequently they contributed to operatively confirmed punctate cerebrospinal fluid (CSF) fistulas. Notably, CSF leaks were clearly attributed to ESI, as they were located centrally/paracentrally at the L4-L5 level, just below hypertrophied/ossified yellow ligament (OYL), and were the exact size of a Tuohy needle with clean edges.
Results:
An average of 4.1 (range 2-12) preoperative ESI were performed in 33 of 39 patients undergoing average 4.3 level laminectomies and 1.3 level non-instrumented fusions; 6 (18.2%) patients exhibited operatively confirmed, punctate CSF fistulas attributed to these ESI. The most recent injections were administered between 2 and 5 weeks prior to surgery (average 3.9 weeks). Fistulas were primarily repaired with 7-0 GORE-TEX sutures and fibrin Sealant (Tisseel).
Conclusions:
Of 33 patients undergoing multilevel laminectomies with non-instrumented fusions receiving preoperative ESI, 6 (18.2%) had operatively confirmed punctate CSF fistulas due to preoperative ESI performed an average of 4.1 times per patient.
Keywords: Epidural steroid injections, fistulas, operative confirmation, punctate cerebrospinal fluid leaks, spinal surgery
INTRODUCTION
Patients are increasingly seeking not only single, but multiple epidural spinal injections (ESI) prior to considering almost any type of lumbar surgery. This is particularly true for older patients with multilevel lumbar stenosis/instability who are hoping to avoid surgery. However, much of the literature documents that these injections are unnecessary and ineffective in providing long-term benefits, while also subjecting older patients with major comorbidities to increased risks. Here, we studied how often patients undergoing multilevel laminectomies with non-instrumented fusions exhibited operatively confirmed, punctate cerebrospinal fluid (CSF) fistulas directly attributed to their multiple preoperative ESI injections.
MATERIALS AND METHODS
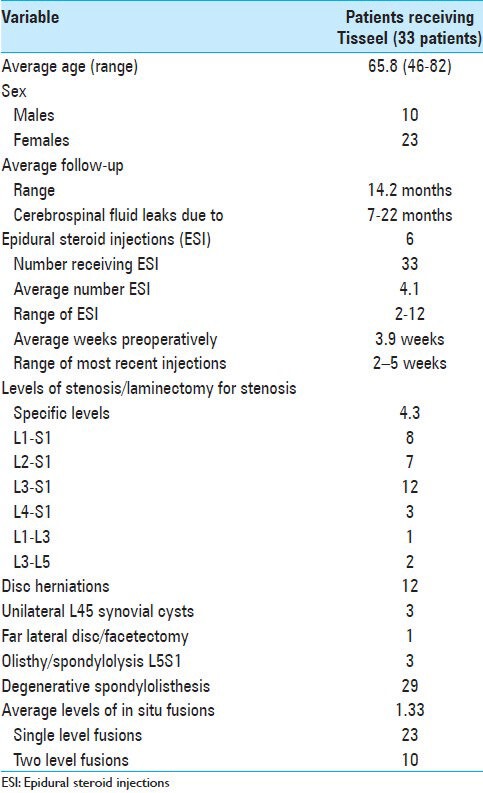
In our series, 39 patients with symptoms/signs of lumbar stenosis/instability underwent multilevel laminectomies with non-instrumented fusion utilizing lamina autograft and NanOss Bioactive (Pioneer Surgical, Marquette MI, USA) [Table 1]. We focused on the 33 patients who had undergone preoperative ESI, and asked how often they later exhibited operatively confirmed, punctate CSF fistulas that could be directly attributed to preoperative ESI. These ESI-induced punctate fistulas, were the same size as the tip of an 18-gauge Tuohy needle, had “clean” edges, and were typically located centrally/paracentrally at the L4-L5 level often initially hidden under hypertrophied/ossified yellow ligament (OYL).
Table 1.
Clinical data for multilevel laminectomies/non-instrumented fusions with/without Tisseel
Clinical parameters
Patients (comprising 10 males and 23 females) averaged 65.8 years of age and were followed an average of 1.42 months (range 7-22 months) [Table 1]. Surgical procedures included an average of 4.3 level laminectomies and 1.3 level (range 1-2 level) non-instrumented fusions. Spinal stenosis was accompanied by ossification of the yellow ligament (all 33 patients), disc herniations (12 patients), and unilateral synovial cysts (3 patients). Instability was variously attributed to: far lateral discs warranting a unilateral full facetectomy (1 patient), spondylolisthesis/lysis (3 patients), or spondylolisthesis alone (29 patients).
RESULTS
Preoperative ESI resulted in intraoperative punctate CSF fistulas in six patients
Thirty-three patients received an average of 4.1 ESI prior to spine surgery (range 2-12 ESI/patient) [Table 1]. Six patients had punctate CSF leaks confirmed intraoperatively that were directly attributed to prior ESI; the most recent injections were performed an average of 3.9 weeks prior to surgery (range 2-5 weeks). Dural lacerations were directly repaired under an operating microscope with 7-0 GORE-TEX sutures (W. L. Gore and Associates, Newark, DE, USA) to achieve watertight closures. The fibrin sealant Tisseel (Baxter International Inc., Westlake Village, CA, USA) supplemented the dural closure utilizing the “sandwich technique.” This technique required that 5 of the 10 cc of Tisseel be evenly applied in a thin layer directly over the dura, followed by one layer of microfibrillar collagen (Duragen: Integra LifeSciences Corporation, Plainsboro Township, NJ, USA), and finally succeeded by the last and final layer of the reamining 5 cc of Tisseel.[19]
DISCUSSION
In this study, we observed that 33 patients undergoing multilevel laminectomies received an average of 4.1 ESI; 6(18.2%) patients exhibited intraoperative punctate dural fistulas directly attributed to these injections. The extraordinarily high number of ESI in these patients and the high resultant frequency of punctate CSF fistulas indicate just how often patients are being “overtreated” by too many “providers with unnecessary, ineffective, and invasive ESI that put them at increased risk. Fortunately in this series, the six punctate ESI leaks only increased the operative time by 20 min, but did not result in other major sequelae. Nevertheless, the four patients with cardiac disease/coated stents who underwent typically multiple preoperative ESI had to stop anti-platelet therapy prior to each ESI thereby putting them at increased risk of thrombosis/myocardial infarction. Furthermore, delaying surgery, often for years (e.g. one patient delayed surgery by 6 years undergoing 12 ESI), can contribute to more severe, irreversible neurological deficits that cannot be recouped.
High frequency of unnecessary lumbar ESI
Rosas et al. noted that lumbar radicular/sciatic complaints impact 13% of Americans per year, and noted that back pain is the second most common symptom-related cause for medical office visits in the United States.[14] Epstein noted that although not approved by the Food and Drug Administration (FDA), injections are being performed with an increased frequency (up 160%) and are typically short acting, are ineffective over the longer term, and expose patients to major risks/complications.[7]
18.2% Risk of intraoperative punctate dural tears secondary to preoperative ESI in patients with lumbar stenosis/instability
The incidence of durotomies occurring during spinal surgery varies from 1 to 9% for open procedures, increasing to 9.4% for minimally invasive surgery (MISS) and up to 21% for open reoperations.[5,8,10,15] To this list we now add an 18.2% risk of encountering intraoperative punctate CSF fistulas due to preoperative ESI for patients with spinal stenosis/instability undergoing multilevel laminectomies/non-instrumented fusions. For these patients, Tisseel can be applied to supplement the repair of these CSF fistulas utilizing the “sandwich technique.”[3,13,16,17,19]
ESI have no long-term benefits, but correlate with major complications
Multiple studies have already demonstrated no long-term benefita of ESI, while they pose increased risks/complications. Landa et al. found that cervical and lumbar ESI demonstrated efficacy for up to 6 months of pain relief, though long-term benefits are less reliable, and acknowledged that these injections can also result in severe complications.[11] In a randomized, double-blind trial, Carette et al. showed that utilizing three ESI (methylprednisolone acetate 80 mg/8 ml of isotonic saline) versus isotonic saline (1 ml) alone were equally ineffective in managing sciatica in 158 patients at 3, 6, 12 weeks, and 1 year; there were no significant differences in outcomes for the two groups.[6] In Arden et al.'s multicenter, double-blind, randomized study of 228 patients over 1 year, the efficacy of three lumbar ESI versus three interligamentous saline injections were compared.[2] Utilizing the Oswestry Disability questionnaire (ODI), at 3 weeks, the steroid group showed a transient benefit over the placebo group; however, from 6 to 52 weeks post-injection, no benefits were demonstrated. Similarly, in Anderberg et al.'s prospective randomized study of 40 patients undergoing cervical ESI/local anesthetic versus sterile saline/local anesthetic, at five post-injection weeks, patients receiving steroid injections had less pain, but this did not last over the long term.[1]
Complications of ESI include CSF leaks/dural fistulas
Cervical or lumbar ESI may directly contribute to inadvertent CSF fistulas. In Botwin et al.'s study, complications of cervical interlaminar epidural spinal injections included[16] non-positional headaches (likely due to CSF leaks) (4.6%) and one dural puncture (0.3%).[4] In Waldman's series of 790 cervical epidural injections performed in 215 patients, there were two dural punctures.[18]
Frequency of dural puncture for ESI administered in labor/delivery
In a survey of 36 academic institutions involving 137,250 women undergoing epidural analgesia for labor/deliveries, Berger et al. found the frequency of inadvertent dural punctures ranged from 0.4-6%.[3] Webb et al. also reported a comparable maximum risk of inadvertent dural puncture utilizing a 17-gauge Tuohy needle for epidurals performed for labor/delivery.[20]
Multiple complications of ESI are often underreported
In animal models and clinical studies, ESI penetrating the dura result in a multitude of complications. In a dog model, Lima et al. performed intrathecal injections of normal saline versus methylprednisolone; the latter resulted in meningeal thickening, lymphocytic infiltrates in the blood vessels, and adhesions of pia, arachnoid, and dura mater with nerve roots surrounded by fibrosis and necrosis of the spinal cord.[12] In multiple clinical studies, ESI resulted in many more serious complications that were often underreported: infection (epidural abscess, meningitis), epidural hematoma, intravascular injections, nerve damage, CSF fistulas/headaches, air embolism, urinary retention, allergic reactions, seizures, blindness, and others.[3,9,11,20,21]
CONCLUSION
The purpose of this commentary was to highlight two major issues. First, there are too many ESI being performed prior to lumbar surgery for stenosis/instability; in this study of the 33 patients undergoing lumbar laminectomy with non-instrumented fusions, an average of 4.1 ESI were performed per patient. An average of 4.1 ESI per patient. It has been been well established that ESI are unnecessary/ineffective over the long term and unnecessarily expose these patients to increased risks/complications. Second, performing multiple preoperative ESI, as demonstrated in this series, resulted in too many intraoperative, punctate CSF fistulas [6 (18.2%)] that could have potentially increased perioperative morbidity. When does “restraint” regarding the performance of such multiple ESI begin?
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2014/5/8/325/139622
REFERENCES
- 1.Anderberg L, Annertz M, Persson L, Brandt L, Säveland H. Transforaminal steroid injections for the treatment of cervical radiculopathy: A prospective and randomized study. Eur Spine J. 2007;16:321–8. doi: 10.1007/s00586-006-0142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arden NK, Price C, Reading I, Stubbing J, Hazelgrove J, Dunne C, et al. A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: The WEST study. Rheumatology (Oxford) 2005;44:1399–406. doi: 10.1093/rheumatology/kei028. [DOI] [PubMed] [Google Scholar]
- 3.Berger CW, Crosby ET, Grodecki W. North American survey of the management of dural puncture occurring during labor epidural analgesia. Can J Anaesth. 1998;45:110–4. doi: 10.1007/BF03013247. [DOI] [PubMed] [Google Scholar]
- 4.Botwin KP, Castellanos R, Rao S, Hanna AF, Torres-Ramos FM, Gruber RD, et al. Complications of fluoroscopically guided interlaminar cervical epidural injections. Arch Phys Med Rehabil. 2003;84:627–33. doi: 10.1016/s0003-9993(02)04862-1. [DOI] [PubMed] [Google Scholar]
- 5.Cammisa FP, Jr, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2000;25:2663–7. doi: 10.1097/00007632-200010150-00019. [DOI] [PubMed] [Google Scholar]
- 6.Carette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierre A, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997;336:1634–40. doi: 10.1056/NEJM199706053362303. [DOI] [PubMed] [Google Scholar]
- 7.Epstein NE. The risks of epidural and transforaminal steroid injections in the Spine: Commentary and a comprehensive review of the literature. Surg Neurol Int. 2013;(4 Suppl 2):S74–93. doi: 10.4103/2152-7806.109446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hannalah D, Lee J, Khan M, Donaldson WF, Kang JD. Cerebrospinal fluid leaks following cervical spine surgery. J Bone Joint Surg Am. 2008;90:1101–5. doi: 10.2106/JBJS.F.01114. [DOI] [PubMed] [Google Scholar]
- 9.Huntoon MA. Epidural abscess and meningitis after epidural corticosteroid injection. Mayo Clin Proc. 2004;79:682–6. doi: 10.4065/79.5.682. [DOI] [PubMed] [Google Scholar]
- 10.Jankowitz BT, Atteberry DS, Gerszten PC, Karausky P, Cheng BC, Faught R, et al. Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J. 2009;18:1169–74. doi: 10.1007/s00586-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Landa J, Kim Y. Outcomes of interlaminar and transforminal spinal injections. Bull NYU Hosp Jt Dis. 2012;70:6–10. [PubMed] [Google Scholar]
- 12.Lima RM, Navarro LH, Carness JM, Barros GA, Marques ME, Solanki D, et al. Clinical and histological effects of the intrathecal administration of methylprednisolone in dogs. Pain Physician. 2010;13:493–501. [PubMed] [Google Scholar]
- 13.Patel VV, Zhao L, Wong P, Pradhan BB, Bae HW, Kanim L, et al. An in vitro and in vivo analysis of fibrin glue use to control bone morphogenetic protein diffusion and bone morphogenetic protein-stimulated bone growth. Spine J. 2006;6:397–403. doi: 10.1016/j.spinee.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Rosas HG, Lee KS. Performing fluoroscopically guided interlaminar lumbar epidural injections. AJR Am J Roentgenol. 2012;199:419. doi: 10.2214/AJR.12.8541. [DOI] [PubMed] [Google Scholar]
- 15.Ruban D, O’Toole JE. Management of incidental durotomy in minimally invasive spine surgery. Neurosurg Focus. 2011;31:E15. doi: 10.3171/2011.7.FOCUS11122. [DOI] [PubMed] [Google Scholar]
- 16.Sekhar LN, Natarajan SK, Manning T, Bhagawati D. The use of fibrin glue to stop venous bleeding in the epidural space, vertebral venous plexus, and anterior cavernous sinus: Technical note. Neurosurgery. 2007;61(3 Suppl):E51. doi: 10.1227/01.neu.0000289711.95426.50. [DOI] [PubMed] [Google Scholar]
- 17.Turgut M, Erkuş M, Tavus N. The effect of fibrin adhesive (Tisseel) on interbody allograft fusion: An experimental study with cats. Acta Neurochir (Wien) 1999;141:273–8. doi: 10.1007/s007010050298. [DOI] [PubMed] [Google Scholar]
- 18.Waldman SD. Complications of cervical epidural nerve blocks with steroids: A prospective study of 790 consecutive blocks. Reg Anesth. 1989;14:149–51. [PubMed] [Google Scholar]
- 19.Wang HR, Cao SS, Jiang YQ, Li JN, Li XL, Fu YG, et al. A comparison between “sandwich” and conventional methods of repairing spinal dura rupture. Orthop Surg. 2012;4:233–40. doi: 10.1111/os.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Webb CA, Weyker PD, Zhang L, Stanley S, Coyle DT, Tang T, et al. Unintentional dural puncture with a Tuohy needle increases risk of chronic headache. Anesth Analg. 2012;115:124–32. doi: 10.1213/ANE.0b013e3182501c06. [DOI] [PubMed] [Google Scholar]
- 21.Zimmerer SM, Conen A, Müller AA, Sailer M, Taub E, Flückiger U, et al. Spinal epidural abscess: Etiology, predisponent factors and clinical outcomes in a 4-year prospective study. Eur Spine J. 2011;20:2228–34. doi: 10.1007/s00586-011-1838-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


