Abstract
Background:
Fibrin sealants (FS)/glues (FG) are primarily utilized in spinal surgery to either strengthen repairs of elective (e.g., intradural tumors/pathology) or traumatic cerebrospinal fluid (CSF) fistulas. Here, additional roles/benefits of FS/FG in spine surgery are explored; these include increased hemostasis, reduction of scar, reduction of the risk of infection if impregnated with antibiotics, and its application to restrict diffusion and limit some of the major complications attributed to the controversial “off-label” use of bone morphogeneitc protein (rhBMP-2/INFUSE).
Methods:
We reviewed multiple studies, focusing not just on the utility of FS/FG in the treatment of CSF fistulas, but on its other applications.
Results:
FS/FG have been primarily used to supplement elective/traumatic dural closure in spinal surgery. However, FS/FG also contribute to; hemostasis, reducing intraoperative/postoperative bleeding/transfusion requirements, length of stay (LOS)/costs, reduced postoperative scar/radiculitis, and infection when impregnated with antibiotics. Nevertheless, one should seriously question whether FS/FG should be applied to prevent diffusion and limit major complications attributed to the “off-label” use of BMP/INFUSE (e.g., limit/prevent heterotopic ossification, dysphagia/respiratory decompensation, and new neurological deficits).
Conclusions:
FS/FG successfully supplement watertight dural closure following elective (e.g., intradural tumor) or traumatic CSF fistulas occurring during spinal surgery. Additional benefits include: intraoperative hemostasis with reduced postoperative drainage, reduced transfusion requirements, reduced LOS, cost, scar, and prophylaxis against infection (e.g., impregnated with antibiotics). However, one should seriously question whether FS/FG should be used to contain the diffusion of BMP/INFUSE and limit its complications when utilized “off-label”.
Keywords: Benefits, complications, fibrin sealant, hemostasis, length of stay, lumbar surgery, reduced spread BMP/INFUSE, Tisseel
INTRODUCTION
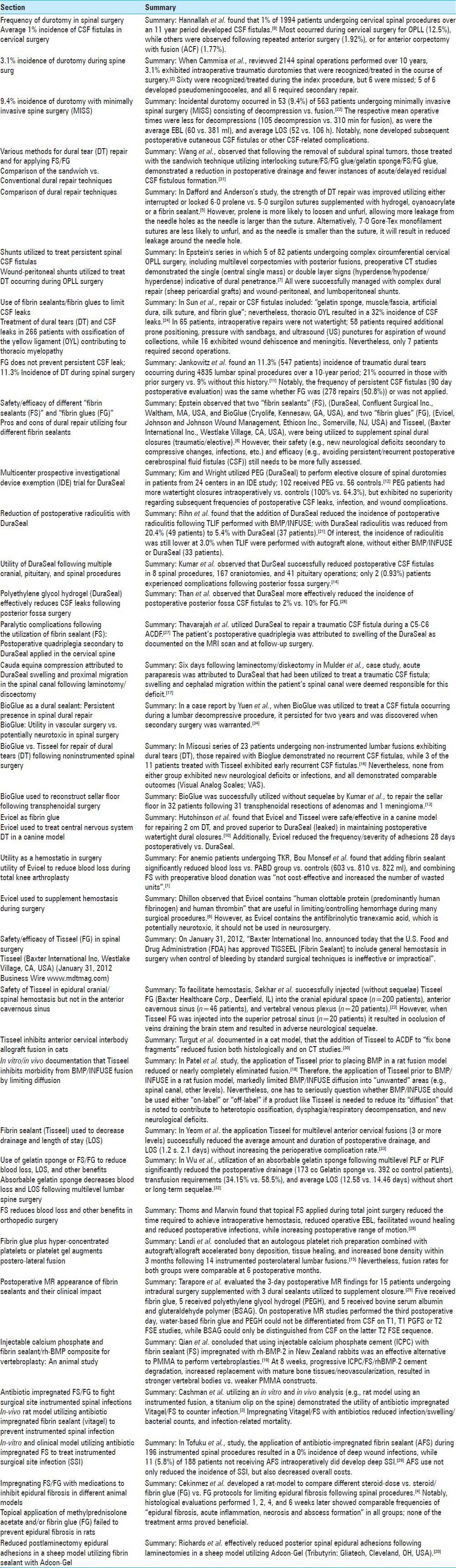
Fibrin sealants/glues (FS/FG) are now largely utilized to strengthen repairs of elective (e.g., intradural surgery for tumors/other pathology) or traumatic cerebrospinal fluid (CSF) fistulas/durotomies occurring during spinal surgery. However, other benefits of FS/FG are increasingly being established [Table 1]. One such role is increasing intraoperative hemostasis resulting in reduced postoperative drainage, reduced transfusion requirements, reduced length of hospital stay (LOS), and reduced cost. When FS/FG are mixed with antibiotics, they appear to be effectively utilized as prophylaxis against infection. Furthermore, although controversial, FS/FG have been applied to restrict the diffusion, limit the spread, and potentially reduce the complications of utilizing “off-label” rhBMP-2/INFUSE (Medtronic, Memphis, TN, USA) for various spinal procedures (e.g., complications include: ectopic/heterotopic bone formation, osteolysis, postoperative scar, radiculitis, and others).
Table 1.
Summary
Frequency of durotomy in spinal surgery
Average 1% incidence of CSF fistulas in cervical surgery
Hannallah et al. retrospectively evaluated the frequency of durotomy occurring during 1994 cervical spinal procedures performed over 11 years (average 5.4 years follow-up) [Table 1].[9] One percent of patients had CSF leaks; 12.5% for ossification of the posterior longitudinal ligament (OPLL), 1.92% for repeated anterior surgery, 1.77% for anterior cervical corpectomy with fusion (ACF), and 1.56% for males. Fistulas were variously/successfully treated with observation alone versus lumboperitoneal shunts; few exhibited long-term sequelae.
3.1% incidence of durotomy during spine surgery
Cammisa et al. retrospectively analyzed the incidence of traumatic durotomites occurring during 2144 spinal operations performed over a 10-year period [Table 1].[2] Intraoperative CSF fistulas were encountered in 66 (3.1%) patients; these were most frequently correlated with revision procedures. Intraoperative CSF fistulas were immediately recognized and treated in 60 patients. However, these leaks were missed during the index procedure in six cases; five subsequently developed pseudomeningocoeles. Nevertheless, all six patients required subsequent operative repair. Over the average follow-up duration of 22.4 months, none developed recurrent fistulas or further long-term sequelae.
9.4% incidence of durotomy with minimally invasive spine surgery
Ruban and O’Toole observed that 53 (9.4%) of 563 patients undergoing minimally invasive spinal surgery (MISS) developed durotomies; 2 occurred during posterior cervical procedures, and 51 were observed during posterior lumbar procedures (32 decompressions and 21 fusions) [Table 1].[22] Patients averaged 60.7 years of age (range 30-85), and exhibited mean operative times of 105 min for decompressions versus 310 min for fusions. The respective estimated blood loss (EBL) was 60 ml for the former versus 381 ml for the latter. The average LOS was, respectively, 52 versus 106 h. Of interest, all patients underwent early mobilization. Over the average postoperative 310-day follow-up period, no patient in either group developed further CSF-related complications. Risk factors for durotomy included: previous surgery at the same level (five patients; 9.4%), and lumbar procedures.
Various methods for dural tear repair and for applying FS/FG
Comparison of the sandwich versus conventional dural repair techniques
Following the excision of 54 spinal subdural tumors, Wang et al. compared the efficacy of utilizing the “sandwich” technique (e.g., three layers including; (1) interlocking suture with the first layer of FS/FG, (2) the application of a gelatin sponge, and (3) a second layer of FS/FG) versus the conventional technique (interlocking sutures/gelatin sponge) for dural repair to prevent recurrent postoperative CSF leaks [Table 1].[31] “Conventional patients” were followed an average of 11 months (range 2-34 months), and underwent surgery for 42 tumors; 23 cervical, 8 thoracic, and 11 lumbar lesions. Those treated with the “sandwich” technique were followed an average of 12 months (range 3-36 months), and had 31 tumors resected; 5 cervical, 10 thoracic, and 16 lumbar. The “sandwich” technique proved more effective; patients exhibited less total postoperative drainage (days 0-3), and fewer recurrent CSF fistulas. At 3 postoperative months, none in the “sandwich” group developed recurrent CSF fistulas, while five of those conventionally managed developed “deep hydrops under their incisions but required no treatment”.
Comparison of dural repair techniques
Dafford and Anderson observed that dural tears (DTs) occur in between 1% and 17% of lumbar procedures [Table 1].[5] These are typically repaired in a watertight fashion utilizing a combination of sutures and FS/FG. They compared the hydrostatic strength of dural repair utilizing different suturing/closure techniques (e.g., looking at different sutures/sizes and sealants (hydrogel, cyanoacrylate, and FG)) in a calf spine model. They compared the efficacy of sutured-repair for 5-0 surgilon (Covidien, Mansfield, MA, USA) versus 6-0 prolene (Ethicon, Bridgewater, NJ, USA), and also analyzed whether continuous locked versus interrupted sutures provided better closures. They found that 6-0 prolene significantly reduced leakage versus 5-0 surgilon; although leaks were largely attributed to the needle holes surrounding the sutures, the results were comparable for interrupted versus continuous locked sutures. Their study also compared the efficacy of three supplemental adhesives: hydrogel, cyanoacrylate, and FG. Although there was an “80% reduction in leak area with the hydrogel and cyanoacrylic sealants compared with only a 38% reduction with FG, there was no statistical difference between the leak rates using any of the sealants.” Notably, had 7-0 Gore-Tex (Elkton, MD, USA) sutures been utilized instead of the two above, leakage around the suture would likely have been reduced as the needle is smaller than the suture.
Shunts utilized to treat persistent spinal CSF fistulas
Wound-peritoneal shunts utilized to treat DT occurring during OPLL surgery
In Epstein's series, she diagnosed multilevel OPLL utilizing the magnetic resonance imaging/computed tomography (MRI/CT) studies of 82 patents; they required multilevel anterior corpectomy fusion (ACF: average 2.6 levels) and simultaneous posterior fusion (PF: average 6.6 levels) [Table 1].[7] Preoperative CT studies for the five patients who developed DT due to OPLL demonstrated either the single-layer sign (two patients: large central mass with/without lateral “C” signs), or the double-layer sign (three patients: hyperdense/hypodense/hyperdense layers). Complex dural repairs included the use of sheep pericardial grafts, FS, microfibrillar collagen (Duragen: Integra LifeSciences, Plainsboro, NJ, USA), and wound-peritoneal (WP)/lumboperitoneal shunts (LP). The wound-peritoneal shunt utilized a low-pressure valve (Uni-Shunts, Codman, Johnson and Johnson, Dorchester, Mass), and the proximal tip was applied lateral/parallel to the fibula strut graft/anterior cervical plate, while the distal catheter was tracked into the peritoneum (right upper quadrant). Note that in such multilevel OPLL cases, all patients are presumptively prepared and draped for the potential necessity of placing a WP shunt.
Use of fibrin sealants/fibrin glues to limit CSF leaks
Treatment of dural tears and CSF Leaks in 266 patients with ossification of the yellow ligament contributing to thoracic myelopathy
In Sun et al. retrospective analysis, management/outcomes of 226 patients with thoracic ossification of the yellow ligament (OYL), with ossified dura (25.2% of patients) resulted in a 32% incidence of CSF leaks (85/266 patients) [Table 1].[24] Repair of CSF fistulas included the application of a: “gelatin sponge, muscle/fascia, artificial dura, silk suture, and FG”. Nevertheless, intraoperative repairs were inadequate (did not fix the leaks) in 65 of 85 patients; 58 required “protracted prone positioning, continuous pressure by sandbag, ultrasound-guided puncture, and aspiration”, while 16 developed wound dehiscence and meningitis. Of interest, only seven patients required secondary surgery.
FG does not prevent persistent CSF leaks following 11.3% incidence of DT during spinal surgery
Jankowitz et al. found an 11.3% (547 patients) incidence of traumatic DTs occurring during 4835 lumbar spinal procedures over a 10-year period [Table 1].[11] The only variable that correlated with an increased risk of intraoperative traumatic DT (2.8 times greater) was a history of prior surgery; 21% had prior surgery versus 9% who had no prior surgery. Persistent CSF leaks, defined as occurring within the first 3 postoperative months, occurred in 64 patients (11.7%); these did not resolve with bed rest, over-sewing, or with other conservative measures. Notably, the frequency of persistent CSF fistulas was the same whether FG (278 repairs (50.8%)) was or was not applied. Of further interest, no complications were attributed to FG.
Safety/efficacy of different “fibrin sealants” and “fibrin glues”
Pros and cons of dural repair utilizing four different fibrin sealants
In 2010, Epstein noted that in spinal surgery, traumatic dural fistulas or deliberate durotomies for intradural pathology were increasingly supplemented with “FS” or “FG” to strengthen these closures [Table 1].[8] However, few spinal surgeons had reviewed the manufacturers’ inserts/flyers regarding the indications, “pros and cons”, and risks and complications, for utilizing these different products. The two FS included DuraSeal (Confluent Surgical Inc., Waltham, MA, USA) and BioGlue (Cryolife, Kennesaw, GA, USA). The two FG included Evicel (Johnson and Johnson Wound Management, Ethicon Inc., Somerville, NJ, USA) and Tisseel (Baxter International Inc., Westlake Village, CA, USA). To establish the safety and efficacy of these four FS/FG products, the incidence of risks/complications (e.g., new neurological deficits secondary to compressive changes, infections, and persistent/recurrent postoperative CSF fistulas) were assessed.
Multicenter prospective investigational device exemption trial for DuraSeal
Kim and Wright performed a prospective, multicenter, randomized, investigational device exemption (IDE) study to evaluate the safety/efficacy of polyethylene glycol (PEG) hydrogel spinal sealant (DuraSeal Spinal Sealant, Confluent Surgical, Waltham, MA) to supplement sutured spinal dural closure following elective spinal durotomy [Table 1].[12] PEG was applied following careful closure/suturing of the dura in patients in 24 centers; patients were randomized 2:1, with 102 receiving PEG versus 56 undergoing standard treatment. Those receiving PEG had more watertight closures versus controls (100% versus 64.3%) intraoperatively, but exhibited similar frequencies of postoperative CSF leaks, infections, and wound complications. Of note, however, PEG contributed to no new postoperative neurological deficits. They concluded PEG was “safe and effective” in producing watertight closure when used to supplement sutured dural repair during spinal surgery. However, its “superiority” in achieving long-term dural closure and avoiding subsequent complications was not clearly established.
Reduction of postoperative radiculitis with DuraSeal
Utilizing medical records, dynamic lumbar X-rays, and select CT studies, Rihn et al. assessed whether DuraSeal would reduce postoperative radiculitis attributed to transforaminal lumbar interbody fusions (TLIF) performed with BMP/INFUSE (86 patients) versus autograft (33 patients) [Table 1].[21] For the 119 patients in this study, clinical follow up averaged 27.6 months, and radiographic follow-up averaged 19.1 months. Duraseal was applied in 37 of the 86 patients receiving BMP/INFUSE to reduce postoperative radiculitis. Although the complication rate for those receiving autograft versus BMP/INFUSE was higher, this difference was not statistically significant. However, different complications were observed. Autograft complications included; donor-site pain (30.3%), donor-site infection (3.1%), lumbar wound infection (6.1%), pseudarthrosis 3.0%, and radiculitis (3.0%). Alternatively, BMP/INFUSE-related complications included; vertebral osteolysis (5.8%), ectopic bone formation (2.3%), pseudarthrosis (3.5%), and lumbar wound infection (3.5%). Additionally, the incidence of postoperative radiculitis was 20.4% for those receiving BMP/INFUSE without DuraSeal (49 patients), but was reduced to 5.4% where DuraSeal was added to BMP/INFUSE PLIF (37 patients).
Utility of DuraSeal following multiple cranial, pituitary, and spinal procedures
Kumar et al. evaluated the frequency of residual postoperative CSF leaks following the application of DuraSeal in 210 patients (216 procedures) over a 22-month period [Table 1].[14] Procedures included; 114 supratentorial craniotomies (52.7%), 53 infratentorial craniotomies (24.5%), 41 transphenoidal adenohypophysectomies (18.9%), and 8 spinal procedures (3.7%). Postoperatively, there were no complications other than two (0.93%) cases of persistent CSF fistulas following posterior fossa craniotomies.
Polyethylene glycol hydrogel (DuraSeal) effectively reduces CSF leaks following posterior fossa surgery
Than et al. utilized DuraSeal (Confluent Surgical, Waltham, MA) to address the 4-17% incidence of CSF fistulas that follow posterior fossa surgery [Table 1].[26] They applied DuraSeal in 100 patients to supplement closure of posterior fossa craniotomies versus craniectomies, and followed the incidence of postoperative “leak, pseudomeningocele, meningitis, wound infection, and interventions required to treat a CSF leak or pseudomeningocele”. Data were then compared with “controls” consisting of a comparable retrospective cohort of 100 patients managed with FG. Although 2 patients treated with DuraSeal had CSF leaks versus 10% with FG, the rates of “pseudomeningocele, meningitis, or other postoperative interventions” were comparable.
Paralytic complications following the utilization of fibrin sealant: DuraSeal
Despite its subsequent Food and Drug Administration (FDA) approval for application in the brain and spine (2009), DuraSeal has been noted to expand into a mass resulting in neural compression, contributing to instances of quadriplegia and paraplegia.
Postoperative quadriplegia secondary to DuraSeal applied in the cervical spine
In a retrospective case report, Thavarajah et al. utilized DuraSeal to repair a traumatic CSF fistula occurring during a C5-C6 anterior cervical diskectomy/fusion (ACDF) utilizing a Polyetheretherketone (PEEK) cage [Table 1].[27] During the procedure, a small CSF leak occurred when excising the posterior longitudinal ligament; this was repaired with both Surgicel and DuraSeal. Postoperatively, the patient's quadriparesis was attributed to swelling of the DuraSeal as documented on the MRI scan, and as confirmed during operative reexploration.
Cauda equina compression attributed to DuraSeal swelling and proximal migration in the spinal canal following laminotomy/discectomy
Mulder et al. observed the evolution of a cauda equina syndrome 6 days following a laminotomy/discectomy utilizing DuraSeal to supplement closure of a traumatic CSF fistula [Table 1].[17] On the first postoperative day, the patient noted increasing radiculopathy (first day); 6 days later, after bending, the patient developed an acute paraparesis. Operative exploration 10 days postoperatively (4 days later) documented not only swelling but also significant cephalad migration of DuraSeal proximal to the original site of dural repair. Although previous reports cited its potential for volume expansion in the posterior fossa resulting in neural compromise, few studies cited extensive migration of DuraSeal within the spinal canal.
BioGlue as a dural sealant: Persistent presence in spinal dural repair
BioGlue: Utility in vascular surgery versus potentially neurotoxic in spinal surgery
BioGlue (CyroLife, Kennesaw, GA, USA), comprised of bovine serum albumin and glutaraldehyde, has been successfully utilized in vascular surgery. Recently it was utilized to augment closure of CSF fistulas despite the absence of large studies documenting its safety/efficacy in neurosurgery. Additionally, the manufacturers’ insert/flyer states BioGlue is “neurotoxic”, and should not be applied in neurosurgical cases. In a case report by Yuen et al., when BioGlue was utilized to treat a CSF fistula occurring during a lumbar decompressive procedure, it persisted for 2 postoperative years as discovered during a second surgical procedure [Table 1].[34]
BioGlue versus Tisseel for repair of dural tears following non-instrumented spinal surgery
Misusci et al. compared the short/long-term (e.g., 3 months, 1 year) safety/efficacy (e.g., postoperative recurrent CSF fistulas, new neurological deficits, infections) of utilizing BioGlue versus Tisseel to repair DTs occurring during non-instrumented lumbar fusions (23 patients) [Table 1].[16] All DTs were directly repaired with a suture with/without a dural patch; 12 patients received BioGlue (FS), while 11 received Tisseel (FG) (Tissucol®; Baxter, Inc., IL, USA). All patients were followed postoperatively at 3 months and 1 year. Although all eventually exhibited successful CSF repairs, 3 of the 11 in the Tisseel group demonstrated early postoperative recurrent CSF fistulas versus no such complications utilizing BioGlue. Notably, none exhibited new neurological deficits or infections, and all demonstrated comparable outcomes (Visual Analog Scales; VAS).
BioGlue used to reconstruct sellar floor following transphenoidal surgery
Kumar et al. used BioGlue to repair the sellar floor in 32 patients following transphenoidal surgery (e.g., 31 pituitary adenomas and 1 meningioma) [Table 1].[13] He noted that CSF fistulas arising from these procedures could present as: rhinorrhea, pneumocephalus, meningitis, granulomas, or other complications. Utilizing BioGlue to repair the sella floor avoided these postoperative complications.
Evicel as fibrin glue
Evicel, one of the “FG”, has been proven to be clinically effective in orthopedic, cardiac, vascular, general, and plastic surgical procedures. However, predominantly animal studies have documented its safety/efficacy in neurosurgery (e.g., for the treatment of cranial/spinal dural fistulas).
Evicel used to treat central nervous system DT in a canine model
Hutchinson et al. noted that closing DT occurring during cranial/spinal neurosurgical procedures is critical, and that different adjuncts may be utilized to supplement these watertight closures [Table 1].[10] They compared the efficacy of utilizing Evicel versus Tisseel versus DuraSeal in avoiding subsequent CSF fistulas following the creation of 2.0 cm DT in a canine model (27 mongrel dogs; 28-day duration). All three sealants effectively avoided CSF leakage during surgery (up to 15 mmHg.), but only two (Evicel, Tisseel, not DuraSeal) effectively prevented recurrent postoperative CSF leaks. Of interest, microscopic anatomical postoperative tissue changes produced by Evicel and Tisseel at the DT site were comparable; only DuraSeal produced “foamy macrophages”. Additionally, Evicel reduced the frequency/severity of adhesions 28 days postoperatively versus DuraSeal.
Evicel as a hemostatic in surgery
Utility of Evicel to reduce blood loss during total knee arthroplasty
Bou Monsef et al. compared the efficacy of utilizing the FS Evicel versus the cell saver to eliminate preoperative autologous blood donation for anemic patients undergoing total knee replacement (TKR) [Table 1].[1] In 176 anemic patients (Hb < 13.5 g/dl) undergoing TKR, they evaluated how four factors impacted perioperative blood loss and transfusion requirements. These included: preoperative autologous blood donation (PABD: 21 patients), intraoperative use of the cell saver (26 patients), application of FS (5 ml Evicel®, Johnson and Johnson Wound Management, Ethicon, Somerville, NJ; 45 patients), and no intervention (40 control patients). Transfusion rates were comparable for all three interventions; all demonstrated a significant reduction in intraoperative blood loss/transfusion requirements versus control patients. Adding Evicel significantly reduced blood loss versus PABD group (603 vs. 810 ml) and Evicel significantly reduced blood loss versus the control group (603 vs. 822 ml). Furthermore, they noted that combining FS with preoperative blood donation was “not cost-effective and increased the number of wasted units”.
Evicel used to supplement hemostasis during surgery
Dhillon observed that Evicel, containing “human clottable protein (predominantly human fibrinogen) and human thrombin”, may be utilized to control hemorrhage during surgical procedures (e.g., retroperitoneal or intraabdominal surgery, endonasal surgeries, and tonsillectomies and/or adenoidectomies, and orthopedic surgeries) where standard measures are “ineffective or impractical” [Table 1].[6] Additionally, since bovine aprotinin has been removed from Evicel, it may be safely used in surgery without risking a hypersensitivity reaction. Nevertheless, as it does contain the antifibrinolytic tranexamic acid that is potentially neurotoxic, it should not be used in neurosurgery.
Safety/efficacy of Tisseel (FG) in spinal surgery
Tisseel (Baxter International Inc, Westlake Village, CA, USA) (January 31, 2012 Business Wire www.mdtmag.com)
On January 31, 2012, “Baxter International Inc. announced that the U.S. FDA has approved Tisseel (FS) to include general hemostasis in surgery when control of bleeding by standard surgical techniques are ineffective or impractical” [Table 1]. As documented in a peripheral vascular Phase III clinical study, Tisseel mimicked the “clotting cascade”, producing “a clot that adheres to the wound surface and helps achieve hemostasis”. Prior to this, it avoided leakage following colon procedures (e.g., reversal of colostomies).
Safety of FS in epidural cranial/spinal hemostasis but not in the anterior cavernous sinus
Sekhar et al. injected Tisseel FG (Baxter Healthcare Corp., Deerfield, IL) into the cranial epidural space (n = 200 patients), anterior cavernous sinus (n = 46 patients), vertebral venous plexu (n = 20 patients), and superior petrosal sinus (n = 20 patients) to facilitate hemostasis [Table 1].[23] Effective hemostasis and no complications were encountered for the first three, but injection into the superior petrosal sinus resulted in occlusion of veins draining the brain stem with resultant adverse neurological sequelae.
Tisseel inhibits anterior cervical interbody allograft fusion in cats
Turgut et al. assessed the impact of Tisseel on anterior cervical interbody allograft fusion at the C5-C6 level in cats (12 received Tisseel, 12 did not) to determine whether it should be utilized as “an adhesive to augment bone grafting operations” [Table 1].[30] However, at 6 postoperative months, they noted better CT-documented fusion (more voluminous fusion mass) occurred in the untreated animals versus those treated with Tisseel. Histopathology similarly showed increased vascularization of the graft and greater new bone formation in those not receiving Tisseel. The authors, therefore, concluded that the local application of Tisseel was not suitable for ““fixation of bone fragments” for ACDF in this cat model.
In vitro/in vivo documentation that Tisseel inhibits morbidity from BMP/INFUSE fusion by limiting diffusion
Patel et al. evaluated whether Tisseel would effectively inhibit unwanted diffusion and heterotopic ossification (unwanted bone formation: HO) during spinal fusions performed with rh-BMP2 (recombinant human bone morphogenetic protein-2) [Table 1].[18] It is already known that BMP/INFUSE diffuses/extravasates beyond where it is applied, thereby contributing to: increased soft-tissue swelling, heterotopic ossification, dysphagia/respiratory decompensation, and new neurological deficits. In this study, Tisseel, an “amorphous FG”, was effectively utilized to control the spread of BMP/INFUSE, thus limiting its in vitro and in vivo morbidity. The in vivo arm of the study involved evaluating changes in rats at 60 days; spines were harvested, and tested for fusion/bone growth, utilizing a manual examination, X-rays, and micro-CT scans. For those treated with BMP alone, there were no new neurological deficits, while X-rays showed partial, and manual testing confirmed 100% intertransverse process fusion. Alternatively, for those receiving Tisseel prior to applying BMP impregnated sponges, only one “possible” fusion occurred. The authors concluded that in this model, those treated with Tisseel prior to the application of BMP/INFUSE exhibited significantly reduced fusion rates. Additionally, however, one has to seriously question whether BMP/INFUSE should be used either “on-label” or “off-label” if a product like Tisseel is needed to reduce its “diffusion” noted to contribute to the multiple complications cited.
Use of fibrin sealants/fibrin glues to limit CSF leaks
Fibrin sealant (Tisseel) used to decrease drainage and length of stay
Yeom et al. evaluated the impact of FS (Tisseel) on postoperative drainage and length of stay (LOS) following multilevel anterior cervical fusion.[33] Thirty patients had anterior fusions of 3 or more levels and utilized 2.0 mL of aerosolized spray versus 30 undergoing the same procedures without FS [Table 1].[33] Tisseel reduced the total drainage (47 mL (FS study group) versus 98 mL), the time to drain removal (<20 mL per shift in 8 h; 17 h versus 24 h), and reduced the average LOS (1.2 versus 2.1 days (range, 1-5 days)). Within 4 postoperative days, two patients in each group experienced similar frequencies of the following complications; dysphagia, dyspnea, or pneumonia, none of which was attributed to Tisseel.
Use of gelatin sponge or FS/FG to reduce blood loss, LOS, and other benefits
Absorbable gelatin sponge decreases blood loss and LOS following multilevel lumbar spine surgery
Wu et al. utilized an absorbable gelatin sponge to reduce blood loss and shorten the LOS for patients undergoing multilevel posterior lumbar spinal surgery [Table 1].[32] Previously, this technique had decreased drainage and LOS for those undergoing posterior cervical procedures. This lumbar study involved 82 consecutive, prospectively randomized patients undergoing posterior lumbar fusion (PLF) or posterior lumbar interbody fusion (PLIF); they received either absorbable gelatin sponge versus no sponge. Factors monitored included: total drain output, blood transfusion rate, LOS, readmission rate, and postoperative complications. Postoperatively, the gelatin sponge experimental group versus control group demonstrated reduced average drainage (173 mL versus 392 mL), reduced perioperative blood transfusion requirements (34.15% versus 58.5%), and reduced LOS (12.58 versus 14.46 days). Furthermore, none exhibited adverse reactions to the absorbable gelatin sponge.
FS/FG reduces blood loss and other benefits in orthopedic surgery
Thoms and Marwin found that topical FS applied during total joint surgery reduced the time required to achieve intraoperative hemostasis, reduced operative EBL, facilitated wound healing, reduced postoperative infections, and increased postoperative range of motion [Table 1].[28]
Fibrin glue plus hyper-concentrated platelets or platelet gel augments posterolateral fusion
Landi et al. determined the efficacy of utilizing a topical FG (platelet gel) to supplement posterolateral fusions rates in 14-instrumented fusions; one side received this preparation with autograft/allograft, while the other side received autograft/allograft bone alone [Table 1].[15] Hyper-concentrated platelets and FG (fibrinogen, XIII factor, fibronectin) were combined with activated thrombin to produce a “platelet gel” to promote, with autograft, posterolateral one to five-level lumbar fusions. Peripheral blood was mixed with REGEN-THT(®) (Thrombocyte Harvesting Tube, and yielded 8 ml autologous platelet gel in 40-45 min). Patients were assessed with serial X-ray and CT studies performed 3 and 6 months postoperatively. CT fusion criteria included the documentation of incremental bone density (rate of incorporation (ROI) (Hounsfield Units). The authors claimed that more fusion was seen within the first 3 months for the platelet gel group; they observed accelerated bony deposition, tissue healing, and increased bone density at the fusion level. Nevertheless, fusion rates were comparable for both groups at 6 postoperative months.
Postoperative MR appearance of fibrin sealants and their clinical impact
Tarapore et al. evaluated the 3-day postoperative MR findings for 15 patients undergoing intradural surgery supplemented with 3 dural sealants utilized to facilitate dural closure [Table 1].[25] Five patients received FG, five received polyethylene glycol hydrogel (PEGH), and five received bovine serum albumin and gluteraldehyde polymer (BSAG). The incidence of postoperative complications, including pseudomeningoceles and infections, were assessed. MR sequences included; T1, T1 postgadolinium fat saturation (PGFS), and T2 fast spin echo (FSE) studies. Utilizing T1 or T1 PGFS, or T2 FSE, it was not feasible to differentiate CSF from FG or PEGH. However, for BSAG, although no significant differences could be found on T1 sequences, it did differ on the T2 FSE. Notably, none of the patients developed complications within the first postoperative month. The authors concluded that water-based FG and PEGH had similar signals to CSF on T1, T1 PGFS and T2 FSE studies, while BSAG could be differentiated from CSF on T2 FSE examinations.
Injectable calcium phosphate and fibrin sealant/rh-BMP-2 composite for vertebroplasty: An animal study
Qian et al. assessed the feasibility of utilizing injectable calcium phosphate cement (ICPC) with FS impregnated with rh-BMP-2 in New Zealand rabbits to perform vertebroplasties versus utilizing polymethylmethacrylate (PMMA) (e.g., frequent adjacent level fractures due to low degradation rate/high strength) [Table 1].[19] At 8 weeks, parts of the ICPC/FS/rhBMP-2 cement degraded, was increasingly replaced with mature bone tissues and neovascularization, and resulted in stronger vertebral bodies compared with the PMMA construct. They concluded that “bone substitution is synchronous with material degradation” and, therefore, offered ICPC/FS/rhBMP-2 cement as an effective alternative to PMMA.
Antibiotic impregnated FS/FG to fight surgical site instrumented spinal infections
In vivo rat model utilizing antibiotic impregnated fibrin sealant (vitagel) to prevent instrumented spinal infection
Cashman et al. utilized an in vivo rat animal model to assess whether a FS could effectively be utilized to administer antibiotics to an infected instrumented spinal fusion [Table 1].[3] The study mixed cefazolin, fusidic acid, or 5-fluorouracil with Vitagel (Orthovita, Malvern, Pennsylvania), another tissue sealant. The dose release/bioactivity of the antibiotics when mixed with Vitagel were measured when exposed to Staphylococcus aureus in vitro (e.g., utilizing zone of inhibition), and in vivo (e.g., a rat instrumented spinal fusion model that employed a titanium clip on the spine directly inoculated with the organism). Over 2- to 4 -day periods, Vitagel/FS effectively delivered antibacterial activity; no animals developed symptoms of systemic illness. Histological evaluation of the titanium clips from animals not receiving antibiotics/Vitagel/FS revealed encapsulated abscesses, while those receiving this treatment demonstrated reduced infection/swelling/bacterial counts/abscesses, and infection-related mortality.
In vitro and clinical model utilizing antibiotic impregnated FS to treat instrumented surgical site infection
Utilizing an in vitro model and a clinical series, Tofuku et al. found that antibiotic-impregnated FS (AFS) helped prevent instrumented surgical site infections (SSIs) [Table 1].[29] Out of 10 nuts placed, 5 were infected and exposed to vancomycin-impregnated FS versus 5 infected nuts that remained untreated; antimicrobial efficacy was documented in the former utilizing agar diffusion testing. In a secondary in vivo clinical setting, 188 patients had instrumented spinal fusions performed without AFS, while 196 had the same procedures performed with AFS; 11 (5.8%) of 188 patients without AFS developed deep SSI versus 0% of 196 patients treated with AFS.
Impregnating FS/FG with medications to inhibit epidural fibrosis in different animal models
Topical application of methylprednisolone acetate and/or fibrin glue failed to prevent epidural fibrosis in rats
Cekinmez et al. developed a rat model to compare the efficacy of different steroid-doses versus steroids combined with FG versus FG alone for limiting epidural fibrosis following spinal procedures [Table 1].[4] One hundred L4-L5 laminectomies were performed in 100 Sprague-Dawley rats; they topically applied 0.05 ml/kg FG, 0.05 ml/kg methyl prednisolone acetate, 0.05 ml/kg FG + methyl prednisolone acetate, and 0.10 ml/kg FG + methyl prednisolone acetate versus normal saline controls. Interestingly, histological evaluations performed 1, 2, 4 and 6, weeks later showed comparable frequencies of “epidural fibrosis, acute inflammation, necrosis and abscess formation”; and, therefore, no treatment arm proved beneficial.
Reduced postlaminectomy epidural adhesions in a sheep model utilizing fibrin sealant with Adcon-Gel
Richards et al. utilized FS with Adcon-Gel (Tributyrin: Gliatech, Cleveland, OH, USA; carbohydrate polymer gel shown clinically to inhibit postsurgical adhesions), as a Medicated Adhesion Barrier (MAB) to reduce posterior spinal epidural adhesions following laminectomies performed in a sheep model [Table 1].[20] Laminectomy defects were treated with FS alone, Adcon-L Gel, or no treatment. Twelve weeks later, epidural fibrosis/adhesions were assessed with MR, peel-off testing, and histology. They concluded that the Adcon-L Gel preparation effectively reduced epidural adhesions in this sheep model.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2014/5/8/304/139615
REFERENCES
- 1.Bou Monsef J, Buckup J, Waldstein W, Cornell C, Boettner F. Fibrin sealants or cell saver eliminate the need for autologous blood donation in anemic patients undergoing primary total knee arthroplasty. Arch Orthop Trauma Surg. 2014;134:53–8. doi: 10.1007/s00402-013-1876-5. [DOI] [PubMed] [Google Scholar]
- 2.Cammisa FP, Jr, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2000;25:2663–7. doi: 10.1097/00007632-200010150-00019. [DOI] [PubMed] [Google Scholar]
- 3.Cashman JD, Jackson JK, Mugabe C, Gilchrist S, Ball K, Tredwell S, et al. The use of tissue sealants to deliver antibiotics to an orthopaedic surgical site with a titanium implant. J Orthop Sci. 2013;18:165–74. doi: 10.1007/s00776-012-0325-6. [DOI] [PubMed] [Google Scholar]
- 4.Cekinmez M, Sen O, Atalay B, Erdogan B, Bavbek M, Caner H, et al. Effects of glue and combination of methyl prednisolone acetate and fibrin glue in prevention of epidural fibrosis in a rat model. Neurol Res. 2010;32:700–5. doi: 10.1179/016164110X12556180206239. [DOI] [PubMed] [Google Scholar]
- 5.Dafford EE, Anderson PA. Comparison of dural repair techniques. Spine J. 2013;(13):S1529–9430. doi: 10.1016/j.spinee.2013.06.044. 00719-5. [DOI] [PubMed] [Google Scholar]
- 6.Dhillon S. Fibrin sealant (evicel® [quixil®/crosseal™]): A review of its use as supportive treatment for haemostasis in surgery. Drugs. 2011;71:1893–915. doi: 10.2165/11207700-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Epstein NE. Wound-peritoneal shunts: Part of the complex management of anterior dural lacerations in patients with ossification of the posterior longitudinal ligament. Surg Neurol. 2009;72:630–4. doi: 10.1016/j.surneu.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Epstein NE. Dural repair with four spinal sealants: Focused review of the manufacturers’ inserts and the current literature. Spine J. 2010;10:1065–8. doi: 10.1016/j.spinee.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 9.Hannalah D, Lee J, Khan M, Donaldson WF, Kang JD. Cerebrospinal fluid leaks following cervical spine surgery. J Bone Joint Surg Am. 2008;90:1101–5. doi: 10.2106/JBJS.F.01114. [DOI] [PubMed] [Google Scholar]
- 10.Hutchinson RW, Mendenhall V, Abutin RM, Muench T, Hart J. Evaluation of fibrin sealants for central nervous system sealing in the mongrel dog durotomy model. Neurosurgery. 2011;69:921–8. doi: 10.1227/NEU.0b013e318222ad63. [DOI] [PubMed] [Google Scholar]
- 11.Jankowitz BT, Atteberry DS, Gerszten PC, Karausky P, Cheng BC, Faught R, et al. Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J. 2009;18:1169–74. doi: 10.1007/s00586-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim KD, Wright NM. Polyethylene glycol hydrogel spinal sealant (DuraSeal Spinal Sealant) as an adjunct to sutured dural repair in the spine: Results of a prospective, multicenter, randomized controlled study. Spine (Phila Pa 1976) 2011;36:1906–12. doi: 10.1097/BRS.0b013e3181fdb4db. [DOI] [PubMed] [Google Scholar]
- 13.Kumar A, Maartens NF, Kaye AH. Reconstruction of the sellar floor using Bioglue following transsphenoidal procedures. J Clin Neurosci. 2003;10:92–5. doi: 10.1016/s0967-5868(02)00262-x. [DOI] [PubMed] [Google Scholar]
- 14.Kumar A, Maartens NF, Kaye AH. Evaluation of the use of BioGlue in neurosurgical procedures. J Clin Neurosci. 2003;10:661–4. doi: 10.1016/s0967-5868(03)00163-2. [DOI] [PubMed] [Google Scholar]
- 15.Landi A, Tarantino R, Marotta N, Ruggeri AG, Domenicucci M, Giudice L, et al. The use of platelet gel in postero-lateral fusion: Preliminary results in a series of 14 cases. Eur Spine J. 2011;(20 Suppl 1):S61–717. doi: 10.1007/s00586-011-1760-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miscusi M, Polli FM, Forcato S, Coman MA, Ricciardi L, Ramieri A, et al. The use of surgical sealants in the repair of dural tears during non-instrumented spinal surgery. Eur Spine J. 2014 doi: 10.1007/s00586-013-3138-1. [In Press] [DOI] [PubMed] [Google Scholar]
- 17.Mulder M, Crosier J, Dunn R. Cauda equina compression by hydrogel dural sealant after a laminotomy and discectomy: Case report. Spine (Phila Pa 1976) 2009;34:E144–8. doi: 10.1097/BRS.0b013e31818d5427. [DOI] [PubMed] [Google Scholar]
- 18.Patel VV, Zhao L, Wong P, Pradhan BB, Bae HW, Kanim L, et al. An in vitro and in vivo analysis of fibrin glue use to control bone morphogenetic protein diffusion and bone morphogenetic protein-stimulated bone growth. Spine J. 2006;6:397–403. doi: 10.1016/j.spinee.2005.11.006. discussion 404. [DOI] [PubMed] [Google Scholar]
- 19.Qian G, Dong Y, Yang W, Wang M. Injectable calcium phosphate cement and fibrin sealant recombined human bone morphogenetic protein-2 composite in vertebroplasty: An animal study. Bosn J Basic Med Sci. 2012;12:231–5. doi: 10.17305/bjbms.2012.2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richards PJ, Turner AS, Gisler SM, Kraft S, Nuss K, Mark S, et al. Reduction in postlaminectomy epidural adhesions in sheep using a fibrin sealant-based medicated adhesion barrier. J Biomed Mater Res B Appl Biomater. 2010;92:439–46. doi: 10.1002/jbm.b.31533. [DOI] [PubMed] [Google Scholar]
- 21.Rihn JA, Patel R, Makda J, Hong J, Anderson DG, Vaccaro AR, et al. Complications associated with single-level transforaminal lumbar interbody fusion. Spine J. 2009;9:623–9. doi: 10.1016/j.spinee.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Ruban D, O’Toole JE. Management of incidental durotomy in minimally invasive spine surgery. Neurosurg Focus. 2011;31:E15. doi: 10.3171/2011.7.FOCUS11122. [DOI] [PubMed] [Google Scholar]
- 23.Sekhar LN, Natarajan SK, Manning T, Bhagawati D. The use of fibrin glue to stop venous bleeding in the epidural space, vertebral venous plexus, and anterior cavernous sinus: Technical note. Neurosurgery. 2007;(61 Suppl 3):E51. doi: 10.1227/01.neu.0000289711.95426.50. [DOI] [PubMed] [Google Scholar]
- 24.Sun X, Sun C, Liu X, Liu Z, Qi Q, Guo Z, et al. The frequency and treatment of dural tears and cerebrospinal fluid leakage in 266 patients with thoracic myelopathy caused by ossification of the ligamentum flavum. Spine (Phila Pa 1976) 2012;37:E702–7. doi: 10.1097/BRS.0b013e31824586a8. [DOI] [PubMed] [Google Scholar]
- 25.Tarapore PE, Mukherjee P, Mummaneni PV, Ames CP. The appearance of dural sealants under MR imaging. AJNR Am J Neuroradiol. 2012;33:1530–3. doi: 10.3174/ajnr.A3078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Than KD, Baird CJ, Olivi A. Polyethylene glycol hydrogel dural sealant may reduce incisional cerebrospinal fluid leak after posterior fossa surgery. Neurosurgery. 2008;(63 Suppl 1):ONS182–6. doi: 10.1227/01.neu.0000335034.08274.d2. [DOI] [PubMed] [Google Scholar]
- 27.Thavarajah D, De Lacy P, Hussain R, Redfern RM. Postoperative cervical cord compression induced by hydrogel (DuraSeal): A possible complication. Spine (Phila Pa 1976) 2010;35:E25–6. doi: 10.1097/BRS.0b013e3181b9fc45. [DOI] [PubMed] [Google Scholar]
- 28.Thoms RJ, Marwin SE. The role of fibrin sealants in orthopaedic surgery. J Am Acad Orthop Surg. 2009;17:727–36. doi: 10.5435/00124635-200912000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Tofuku K, Koga H, Yanase M, Komiya S. The use of antibiotic-impregnated fibrin sealant for the prevention of surgical site infection associated with spinal instrumentation. Eur Spine J. 2012;21:2027–33. doi: 10.1007/s00586-012-2435-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Turgut M, Erkuş M, Tavus N. The effect of fibrin adhesive (Tisseel) on interbody allograft fusion: an experimental study with cats. Acta Neurochir (Wien) 1999;141:273–8. doi: 10.1007/s007010050298. [DOI] [PubMed] [Google Scholar]
- 31.Wang HR, Cao SS, Jiang YQ, Li JN, Li XL, Fu YG, et al. A comparison between “sandwich” and conventional methods of repairing spinal dura rupture. Orthop Surg. 2012;4:233–40. doi: 10.1111/os.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu J, Jin Y, Zhang J, Shao H, Yang D, Chen J. Hemostatic techniques following multilevel posteriorlumbar spine surgery: A randomized control trial. J Spinal Disord Tech. 2013 doi: 10.1097/BSD.0000000000000063. [In Press] [DOI] [PubMed] [Google Scholar]
- 33.Yeom JS, Buchowski JM, Shen HX, Liu G, Bunmaprasert T, Riew KD. Effect of fibrin sealant on drain output and duration of hospitalization after multilevel anterior cervical fusion: A retrospective matched pair analysis. Spine (Phila Pa 1976) 2008;33:E543–7. doi: 10.1097/BRS.0b013e31817c6c9b. [DOI] [PubMed] [Google Scholar]
- 34.Yuen T, Kaye AH. Persistence of Bioglue in spinal dural repair. J Clin Neurosci. 2005;12:100–1. doi: 10.1016/j.jocn.2004.06.006. [DOI] [PubMed] [Google Scholar]


