Abstract
Pain control is an important part of dentistry, particularly in the management of children. Behavior guidance, and dose and technique of administration of the local anesthetic are important considerations in the successful treatment of a pediatric patient. The purpose of the present review is to discuss the relevant data on topics involved, and on the current methods available in the administration of local anesthesia used for pediatric dental patients.
Keywords: Local anesthesia, pain control, pedodontics
INTRODUCTION
Fear-related behaviors have long been recognized as the most difficult aspect of patient management and can be a barrier to good care.[1] Administering local anesthesia by injection is still the most common method used in dentistry. However, there is a constant search for ways to avoid the invasive and often painful nature of the injection, and find a more comfortable and pleasant means of achieving local anesthesia before dental procedures.[2,3]
Chemically, the local anesthetic agents in common clinical use today may be divided into two broad groups: (A) agents containing an ester linking and (B) agents containing an amide. The most commonly used local anesthetics for pediatric dentistry are the amide type agents. Lidocaine hydrochloride (HCl) 2% with 1:100,000 epinephrine is preferred because of their low allergenic characteristics and their greater potency at lower concentrations.[4] Table 1 shows the dosage per 1.8 mL cartridge of lidocaine.
Table 1.
Dosage per dental cartridge
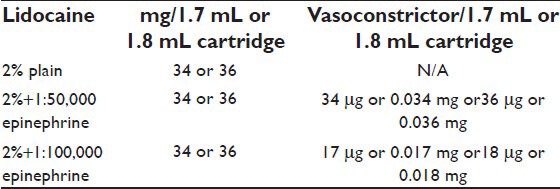
Local anesthetic carpules also contain organic salts and may contain vasoconstrictors. Vasoconstrictors are used to constrict blood vessels, counteract the vasodilatory effects of the local anesthetic, prolong its duration, reduce systemic absorption and toxicity, and provide a bloodless field for surgical procedures.[4,5] The use of the vasoconstrictor will allow the maximum total dose of the anesthetic agent to be increased by nearly 40%.[6,7] Many agents have been employed as vasoconstrictors with local anesthetics. But none has proved to be as clinically effective as epinephrine.[6]
The maximum dose of lidocaine and mepivacaine, without vasoconstrictors, recommended for children is 4.4 mg/kg body weight, and 7 mg/kg body weight for lidocaine with vasoconstrictors.[8]
The average duration of pulpal anesthesia is 60 minutes for 20% lidocaine with 1:100,000 epinephrine, 50 minutes for 2% mepivacaine with 1:20,000 levonordefrin, and 25 minutes for 3% mepivacaine without vasoconstrictor. In the present local anesthetic agents used, the soft tissue anesthesia is more than that of pulpal anesthesia.[5] Attempts have been made to find agents that reduce the duration of soft tissue anesthesia. However, no such reduction has been observed; thus, the authors recommend that 2% lidocaine with 1:100,000 epinephrine be used when administering local anesthesia in young children.
If a local anesthetic is injected into an area of infection, its onset will be delayed or even prevented.[3] The inflammatory process in an area of infection lowers the pH of the extracellular tissue from its normal value (7.4) to 5-6 or lower. This low pH inhibits anesthetic action because little of the free base form of the anesthetic is allowed to cross into the nerve sheath to prevent conduction of nerve impulses. Inserting a needle into an active site of infection could also lead to a possible spread of the infection.[3,4,6,8,9]
Safety of local anesthetic agents and adverse reaction
The inherent use of local anesthetic injections allows practitioners to use them frequently with the confidence that adverse events are rare.[10,11] The most common reaction associated with local anesthetics is a toxic reaction, resulting usually from an inadvertent intravenous injection of the anesthetic solution.[8] Table 2 shows the adverse reaction to commonly used local anesthetics.
Table 2.
Adverse reactions of commonly used local anesthetics
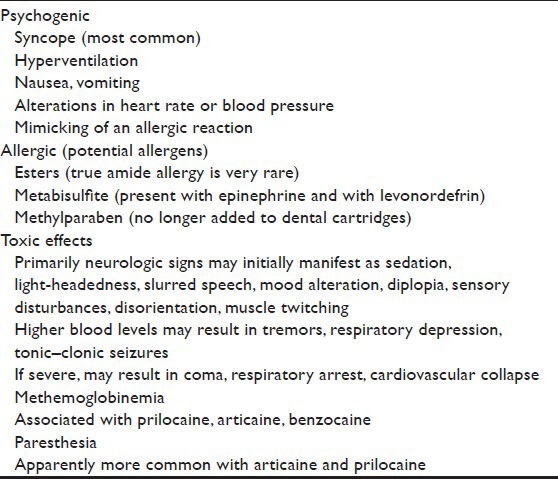
Overdose reactions are a particular risk in treating children.[5,6] The dosage of the local anesthetic depends on the physical status of patient, area to be anesthetized, vascularity of oral tissues, and the technique of administration. It is difficult to recommend a maximum dose for children because dose varies with functions of age and weight. For pediatric patients less than 10 years who have lean body mass and normal body development, the maximum dose may be determined by application of one of the standard formulas (Clarks rule). In any case, the maximum dose should not exceed 7 mg/kg body weight for lidocaine with epinephrine and 4.4 mg/kg for plain adrenaline. Toxicity occurs primarily in the cardiovascular and central nervous system; this toxic reaction could stimulate or depress the central nervous system. Stimulation of the central nervous system can cause a toxic vasoconstrictor reaction, and the signs and symptoms are tachycardia, apprehension, sweating, and hyperactivity. Depression of the central nervous system may follow, leading to bradycardia, hypoxia, and respiratory arrest.[3,8,10,11,12]
Epinephrine is contraindicated in patients with hyperthyroidism.[5] Its dose should be kept to a minimum in patients receiving tricylic antidepressants since dysrhythmias may occur. Levonordefrin and norepinephrine are absolutely contraindicated in these patients. Patients with significant cardiovascular disease, thyroid dysfunction, diabetes, or sulfite sensitivity, and those receiving monoamine oxidase inhibitors, tricyclic antidepressants, or phenothiazines may require a medical consultation to determine the need for a local anesthetic without a vasoconstrictor[5,10,11]
Local anesthetic toxicity can be prevented by careful injection technique, watchful observation of the patient, and knowledge of the maximum dosage based on weight. Practitioners should aspirate before every injection and inject slowly.[11] Early recognition of a toxic response is critical for effective management. When signs or symptoms of toxicity are noted, administration of the local anesthetic agent should be discontinued. Additional emergency management is based on the severity of the reaction.
Allergic reactions to local anesthesia are rare. The local anesthetic agent with the highest incidence of allergic reactions is procaine. Its antigenic component appears to be para-aminobenzoic acid (PABA). Cross-reactivity had been reported between lidocaine and procaine. Allergies can manifest in a variety of ways, some of which include urticaria, dermatitis, angioedema, fever, photosensitivity, or anaphylaxis.[8,11,12] Emergency management is dependent on the rate and severity of the reaction.[13]
Patients, with a history of allergy to a local anesthetic, who cannot identify the specific agent used, present a problem. The patient should be referred for evaluation and testing, which will usually include both skin testing and provocative dose testing (PVT). For patients having an allergy to bisulfates, use of a local anesthetic without a vasoconstrictor is indicated.[8,13] Local anesthetics without vasoconstrictors should be used with caution due to rapid systemic absorption which may result in overdose.[13,14]
A long-acting local anesthetic (i.e., bupivacaine) is not recommended for the child or the physically or mentally disabled patient due to its prolonged effect, which increases the risk of soft tissue injury.[14]
Paresthesia is persistent anesthesia beyond the expected duration; injuries to the inferior alveolar nerve (IAN) and lingual nerve (LN) can be caused by local analgesic block injections. The nerve injury may be physical from the needle or chemical from the local anesthetic solution. The patient may experience an ‘electric shock’ in the involved nerve distribution area. Paresthesia also can be caused by hemorrhage in or around the nerve. Reports of paresthesia are more common with articaine and prilocaine than expected, from their frequency of use. Most cases resolve in eight weeks.[8,15]
Patient management while administering local anesthetic injections
In children, behavior management is critical to the success of dental procedures. A relaxed and calm child during the administration of local anesthesia is important for the success of the clinical process as well.[2,3,4] Many techniques have been described for managing child behavior in the dental office, including both pharmacological and nonpharmacological methods.[5]
Techniques for administering the local anesthetic
There is no perfect technique that guarantees success in anesthetizing all children. However, there are a few key procedures that are mutual to all administrations that may be valuable to the success of all techniques.
Control of the child's head
Once a child has grabbed the syringe or bumped the operator's hand and driven the needle into the tissue of the bone, it may be too late to respond, and a lasting impression has been made in the child's mind relative to pain associated with the local anesthetic injection.[4] Therefore, some authors recommend that the practitioner should have a control of the child's head and a good finger rest, to control the syringe in case the child moves or resists. The dental assistant should be prepared to restrain the child's hand, gently but firmly.[16]
Topical anesthesia
The primary goal in using topical anesthesia is to minimize the painful sensation of needle penetration into the soft tissue. The topical anesthetic agent must be placed on dried mucosa and left in place for at least one minute to achieve maximum effect. The onset duration of lidocaine is 3-5 minutes. A recent study which compared the efficacy of commonly used topical anesthetics demonstrated the superiority of 5% EMLA cream (eutectic mixture of local anesthesia containing lidocaine and prilocaine) over all other topical anesthetic agents. The topical anesthetic benzocaine is manufactured in concentrations up to 20%; lidocaine is available as a solution or ointment up to 5% and as a spray up to 10% concentration. Localized allergic reactions, however, may occur after prolonged or repeated use. Topical lidocaine has an exceptionally low incidence of allergic reactions but is absorbed systemically and can combine with an injected amide.[17]
Needle size and length
A short (20 mm) or long (32 mm) 27- or 30-gauge needle may be used for most intraoral injections in children. An extrashort (10 mm) 30-gauge needle has been suggested for maxillary anterior injections. Long needles are frequently recommended for inferior dental nerve block anesthesia. However, the clinical experience of many dentists has shown that shorter needles are adequate and safe especially for the young difficult-to-manage dental patients.[3,12]
Duration of injection
Injection of local anesthetics should always be made slowly, preceded by aspiration to avoid intravascular injection and systemic reactions to the local anesthetic agent or the vasoconstrictor.[8,16]
Postoperative soft tissue injury
Self-induced soft tissue trauma is an unfortunate clinical complication of local anesthetic use in the oral cavity. Most lip- and cheek-biting lesions of this nature are self-limiting and heal without complications, although bleeding and infection may possibly result.[18]
Caregivers responsible for postoperative supervision should be given a realistic time for duration of numbness and be informed of the possibility of soft tissue trauma.
Failure in local anesthesia
A number of factors contribute to the failure of local anesthesia. These may be related either to the patient or the operator. Operator-dependent factors are (a) bad choice of local anesthetic solution and (b) poor technique.
Patient-dependent factors are (a) anatomical variations, (b) the presence of infection, that is, the acidic environment prevents the local anesthetic agent from reaching and penetrating the nerve, and (c) psychogenic factors, that is, severe anxiety may influence pain perception.[10,19,20]
When a local anesthetic fails, generally, it is best to repeat the injection; this will often lead to success. In the case of repeat block injections, it is easier to palpate bony landmarks at the second attempt as the needle can be maneuvered in the tissues painfully.[19]
Conventional methods of obtaining local anesthesia
Infiltration is the choice to anaesthetize maxillary teeth successfully. In this case, the needle should penetrate the mucobuccal fold and be inserted to the depth of the apices of the buccal roots of the teeth. The solution is deposited supraperiosteally and infiltrates through the alveolar bone to reach the root apex, as the alveolar bone in children is more permeable than it is in adults. A little local anesthetic may be sufficient to produce anesthesia of teeth.[21]
Stretching the mucosa of the injection site and gently pulling onto the obliquely placed bevel of the needle is recommended for buccal infiltrations. In so doing, the initial needle penetration is shallow. A small amount of solution has to be injected into the superficial mucosa. After a few seconds, the needle can be slowly advanced 1-2 mm and after a negative aspiration, another small amount of solution can be deposited. This should be repeated until the remaining anesthetic solution is completely injected.[21]
Anesthesia of the mandibular primary molars may usually be achieved by infiltration in children up to the age of five years. A few studies have evaluated the effectiveness of mandibular infiltration as a possible alternative to mandibular block for the restoration of primary molars. No significant differences between infiltration and block were found. In addition, the quality of anesthesia was not significantly related to tooth location, age, or type of anesthetic agent.[22]
Mandibular block is the local anesthesia technique of choice when treating mandibular primary or permanent molars. Depth of anesthesia has been the primary advantage of this technique. Anesthesia of all the molars, premolars, and canines on the same side of injection allows for treating multiple teeth of the same quadrant at one appointment. For the inferior alveolar block, the child is requested to open his mouth as wide as possible while the operator positions the ball of the thumb on the coronoid notch of the anterior border of the ramus. The needle is inserted between the internal oblique ridge and the pterygomandibular raphe.[23] The position of the foramen changes with the child's age: In a young child (4 years old and younger) the foramen is sometimes located below the plane of occlusion. In a young child, the foramen is located on the occlusal plane. As the child matures, it moves to a higher position.[5,24]
The barrel of the syringe overlies the two primary mandibular molars on the opposite side of the arch and parallel to the occlusal plane. In this case, a small amount of solution should be injected and, after a negative aspirate, the needle should advance until bony contact is made, very gently and slowly. When the inferior alveolar nerve block may not adequately anesthetize the teeth, long buccal anesthesia is required. This is achieved by infiltrating a few drops of the anesthetic into the buccal sulcus just posterior to the molars.[5,22]
The intraligamentary injection is given into the periodontal ligament using a syringe specially designed for the purpose. Intraligamentary injections also can be given with a conventional needle and syringe. In this technique, the needle is inserted at the mesiobuccal aspect of the root and advanced in for maximum penetration. The needle does not penetrate deeply onto the periodontal ligament but is wedged at the crest of the alveolar ridge. A 12 mm 30-gauge needle is recommended, and the bevel should face the bone, although effectiveness is not impaired with different orientation. Intraligamentary anesthesia has limitations as a principal method of anesthesia, due to the variable duration, but has been used to overcome failed conventional methods or as an adjunct.[24] Intraligmentary injections produce significant bacteremia and therefore should not be given to a patient at the risk of infective endocarditis unless appropriate antibiotic prophylaxis has been provided.[25]
The intrapulpal method achieves anesthesia as a result of pressure. Saline has been reported to be as effective as an anesthetic solution when injected intrapulpally. When a small access cavity is available into the pulp, a needle which fits snugly into the pulp is used and a small amount (about 0.1 mL) of solution is injected under pressure. There will be an initial feeling of discomfort during this injection; however, this is transient and anesthetic onset is rapid. When the exposure is too large to allow a snug needle to fit, the exposed pulp should be bathed in a little local anesthetic for about a minute before introducing the needle as far apically as possible into the pulp chamber and injecting under pressure.[26]
Intraligamentary anesthesia has a role to play in local anesthesia in modern dentistry but it does not fulfil all the requirements for a primary technique. As with traditional methods of obtaining oral local anesthesia, the alternative methods generally are safe if the practitioner understands the principles for their use. Alternative techniques for the delivery of local anesthesia may be considered to minimize the dose of anesthetic used, improve patient comfort, and/or improve successful dental anesthesia. Some of these techniques are desirable, especially in infants, children, adolescents, and patients with special health-care needs, since specific teeth may be anesthetized with less residual anesthesia (i.e., avoid discomfort and potential self-mutilation of block anaesthesia). The mandibular bone of a child usually is less dense than that of an adult, permitting more rapid and complete diffusion of the anesthetic. Mandibular buccal infiltration anesthesia is as effective as inferior nerve block anesthesia for some operative procedures. In patients with bleeding disorders, the PDL injection minimizes the potential for postoperative bleeding of soft tissue vessels. Intraosseous techniques may be contraindicated with primary teeth due to the potential for damage to developing permanent teeth. Also, the use of the periodontal ligament injection or intraosseous methods is contraindicated in the presence of inflammation or infection in the injection site.[5,10,16,21,27]
New techniques for obtaining local anesthesia
Computerized local anesthesia
The Wand system consists of a disposable handpiece component and a computer control unit. The handpiece is an ultralight pen-like handle which is linked to a conventional anesthetic cartridge with plastic micro tubing.
The core technology is an automatic delivery of local anesthetic solution at a fixed pressure; volume ratio is regardless of variations in tissue resistance. This results in a controlled, highly effective, and comfortable injection even in resilient tissues such as the palate and periodontal ligament. While ‘the Wand’ has been shown to reduce the pain associated with the delivery of the anesthetic solution, the time involved in the procedure appears to negate the effectiveness of the device; a review of computer-controlled delivery devices as well as other alternative anesthesia delivery methods found that they each present adverse side effects and generally are more expensive than conventional methods.[28,29]
Electronic dental anesthesia
The concept of electronic dental anesthesia (EDA) involves the application of electric current that loads the nerve stimulation pathway to the extent that pain stimulus is blocked. A review of the literature shows a significant reduction in pain observed during all the dental procedures conducted under TENS (TENS: Transcutaneous electrical nerve stimulator). Thus, TENS should be considered as a useful adjunct in the treatment of pediatric patients during various minor dental procedures.[29,30]
There are medical contraindications to the use of EDA: Patients with a pacemaker or cochlear implant, heart disease, seizure disorders, or cerebrovascular disease, head tumor, neurological disorders involving the head and neck (e.g., Bell's palsy, trigeminal and postherpetic neuralgia, multiple sclerosis, or Tourette's syndrome), skin lesions or abrasions on the face, and patients with abnormal bruising or bleeding disorder.[31]
Intraoral lidocaine patch
These are anesthetic patches containing a lidocaine base that is dispended through a bioadhesive matrix and applied directly to the oral mucosa. These patches are available in 10 and 20% concentrations, each containing approximately 23 and 416 mg of lidocaine and can reduce the pain of insertion of needle.[29,32]
Jet injection
This instrument was developed to achieve local anesthesia for dental procedures without the use of a needle. This is accomplished by delivering the anesthetic solution under high compressive forces. A number of uncontrolled studies of needleless devices have examined adult and child patients, typically focusing on the anesthetic properties of the device used. In these studies, the percentage of patients who obtained sufficient anesthesia with the devices ranged from about 50 to about 90%.[33] Traditional infiltration was more effective, acceptable, and preferred, compared with the needleless injection.[34]
CONCLUSION
Local anesthesia forms the backbone of pain control techniques in dentistry and has a major role in dentistry for children. There is a constant search for ways to avoid the invasive and often painful nature of the injection, and to find a more comfortable and pleasant means of achieving local anesthesia before dental procedures. Despite the recent innovations, the injection remains the method of choice in providing local anesthesia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Milgrom P, Coldwell SE, Getz T, Weinstein P, Ramsay DS. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128:756–66. doi: 10.14219/jada.archive.1997.0301. [DOI] [PubMed] [Google Scholar]
- 2.Dower JS, Jr, Simon JF, Peltier B, Chambers D. Patients who make a dential most anxious about giving injections. J Californian Dent Assoc. 1995;23:34–40. [PubMed] [Google Scholar]
- 3.Simon JF, Peltier B, Chanbers D, Dower J. Dentists troubled by the administration of anesthetic injections: Long-term stress and effects. Quint Int. 1994;25:641–6. [PubMed] [Google Scholar]
- 4.Troutman KC. Pharmacologic Management of pain and anziety for pediatric patients. In: Wei SH, editor. Pediatric Dentistry Total Patient Care. Philadelphia, PA: Lea and Febbiger; 1985. pp. 156–62. [Google Scholar]
- 5.Wilson SW, Dilley DC, Vann WF, Jr, Anderson JA. Pain and anxiety control (Partl: Pain perception control) In: Pickham J, Casmassinno PS, Field HW, Mctigue DJ, Nowak A, editors. Pediatric Dentistry, Infancy Through Adolescesce. 3rd ed. Philadelphia, PA: WB Saunders; 1999. pp. 108–15. [Google Scholar]
- 6.Scott DB, Jebson PJ, Braid DP, Prtengren B, Frish P. Factors affecting plasma levels of lignocaine and prilocaine. Br J Anaesth. 1972;44:1040–9. doi: 10.1093/bja/44.10.1040. [DOI] [PubMed] [Google Scholar]
- 7.Cannell H, Walters H, Beckett AH, Saunders A. Circulating levels of lignocaine after peri-oral injections. Br Dent J. 1975;138:87–93. doi: 10.1038/sj.bdj.4803383. [DOI] [PubMed] [Google Scholar]
- 8.Malamed SF. Handbook of Local Anesthesia. 5th ed. St. Louis, Mo: Mosby; 2004. Local complications; pp. 285–7. [Google Scholar]
- 9.Hersh EV, Hermann DG, Lamp CI. Assessing the duration of mandibular soft tissue anesthesia. J Am Dent Assoc. 1995;126:1531–6. doi: 10.14219/jada.archive.1995.0082. [DOI] [PubMed] [Google Scholar]
- 10.Malamed SF. Hand-book of Local Anesthesia. 5th ed. St. Louis, Mo: Mosby; 2004. Pharmacology of vasoconstrictors; pp. 41–54. [Google Scholar]
- 11.Jeske AH, Blanton PL. Misconceptions involving dental local anesthesia. Part 2: Pharmacology. Tex Dent J. 2002;119:310–4. [PubMed] [Google Scholar]
- 12.Haas DA. An update on local anesthetics in dentistry. J Can Dent Assoc. 2002;68:546–51. [PubMed] [Google Scholar]
- 13.Scott DB. Toxicity caused by local anesthetic drugs. Br J Anaesth. 1981;53:553–4. doi: 10.1093/bja/53.6.553. [DOI] [PubMed] [Google Scholar]
- 14.Yagiela JA. Adverse drug interactions in dental practice: Interactions associated with vasoconstrictors. J Am Dent Assoc. 1999;130:701–9. doi: 10.14219/jada.archive.1999.0280. [DOI] [PubMed] [Google Scholar]
- 15.Haas DA, Lennon D. A 21 year retrospective study of reports of paresthesia following local anesthetic administration. J Can Dent Assoc. 1995;61:319. [PubMed] [Google Scholar]
- 16.American Academy of Pediatric Dentistry (www.aapd.org) Guideline on Use of Local Anesthesia for Pediatric Dental Patients. Clinical Guidelines, reference manual. 2009. available from www.aapd.org/media/policies_guidelines/g_localanesthesia.pdf .
- 17.Kravitz ND. The use of compound topical anesthetics: A review. J Am Dent Assoc. 2007;138:1333–9. doi: 10.14219/jada.archive.2007.0048. [DOI] [PubMed] [Google Scholar]
- 18.Chi D, Kanellis M, Himadi E, Asselin ME. Lip biting in a pediatric dental patient after dental local anesthesia: A case report. J Pediatr Nurs. 2008;23:490–3. doi: 10.1016/j.pedn.2008.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boronat-López A, Peñarrocha-Diago M. Failure of locoregional anesthesia in dental practice. Review of the literature. Med Oral Pathol Oral Circ Bucal. 2006;11:E510–3. [PubMed] [Google Scholar]
- 20.Wong MK, Jacobsen PL. Reasons for local anesthesia failures. J Am Dent Assoc. 1992;123:69–73. doi: 10.14219/jada.archive.1992.0004. [DOI] [PubMed] [Google Scholar]
- 21.Ogle OE, Mahjoubi G. Local Anesthesia: Agents, Techniques, and Complications. Dent Clin North Am. 2012;56:133–48. doi: 10.1016/j.cden.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Wright GZ, Weinberger SJ, Marti R, Plotzke O. The effectiveness of infiltration anesthesia in the mandibular primary molar region. Pediatr Dent. 1991;13:278–83. [PubMed] [Google Scholar]
- 23.Oulis C, Vadiakas G, Vasilopoulou A. The effectiveness of mandibular infiltration compared to mandibular block anesthesia in treating primary molars in children. Pediatr Dent. 1996;18:301–5. [PubMed] [Google Scholar]
- 24.Malamed SF. Handbook of Local Anesthesia. 5th ed. St. Louis, Mo: Mosby; 2004. Anatomical considerations; pp. 173–4. [Google Scholar]
- 25.Roberts GJ, Holzel HS, Sury MR, Simmons Dental bacteremia in children. Ped Cardiol. 1997;18:24–7. doi: 10.1007/s002469900103. [DOI] [PubMed] [Google Scholar]
- 26.Van Gheluwe MS, Walton R. Intrapulpal injection. Factors related to effectiveness. Oral Surg. 1997;83:38–40. doi: 10.1016/s1079-2104(97)90088-3. [DOI] [PubMed] [Google Scholar]
- 27.Meechan JG. How to overcome failed local anaesthesia. Br Dent J. 1999;186:15–20. doi: 10.1038/sj.bdj.4800006. [DOI] [PubMed] [Google Scholar]
- 28.Koyuturk AE, Avsar A, Sumer M. Efficacy of dental practitioners in injection techniques: Computerized device and traditional syringe. Quintessence Int. 2009;40:73–7. [PubMed] [Google Scholar]
- 29.Blanton PL, Jeske AH. Dental local anesthetics: Alternative delivery methods. J Am Dent Assoc. 2003;134:228–34. doi: 10.14219/jada.archive.2003.0140. [DOI] [PubMed] [Google Scholar]
- 30.Harvey M, Elliott M. Transcutaneous electrical nerve stimulation for pain management during cavity preparations in pediatric patient. ASDC J Dent child. 1995;62:49–51. [PubMed] [Google Scholar]
- 31.Dhindsa A, Pandit IK, Srivastava N, Gugnani N. Comparative evaluation of the effectiveness of electronic dental anesthesia with 2% lignocaine in various minor pediatric dental procedures: A clinical study. Contemp Clin Dent. 2011;2:27–30. doi: 10.4103/0976-237X.79305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hersh EV, Houpt MI, Cooper SA, Feldman RS, Wolff MS, Levin LM. Analgesic efficacy and safety of an intra-oral lidocaine patch. J Am Dent Assoc. 1996;127:1626–34. doi: 10.14219/jada.archive.1996.0098. [DOI] [PubMed] [Google Scholar]
- 33.Ram D, Peretz B. Administering local anaesthesia to paediatric dental patientscurrent status and prospects for the future. Int J Paediatr Dent. 2002;12:80–9. doi: 10.1046/j.1365-263x.2002.00343.x. [DOI] [PubMed] [Google Scholar]
- 34.Dabarakis NN, Alexander V, Tsirlis AT, Parissis NA, Nikolaos M. Needle-less local anesthesia: Clinical evaluation of the effectiveness of jet anesthesia Injex in local anesthesia in dentistry. Quintessence Int. 2007;38:572–6. [PubMed] [Google Scholar]


