Abstract
Context:
During induction of general anesthesia hypertension and tachycardia caused by tracheal intubation may lead to cardiac ischemia and arrhythmias. Dexmedetomidine attenuates the hemodynamic response to endotracheal intubation and reduces anesthetic requirement.
Aims:
The purpose of this study was to evaluate the effect of a single pre-induction intravenous dose of dexmedetomidine 1 μg/kg on cardiovascular response resulting from laryngoscopy and endotracheal intubation and need for anesthetic agent.
Materials and Methods:
Fifty patients scheduled for elective major surgery were randomized into two groups each having twenty five patients-dexmedetomidine group (Group 1) and control group (Group 2). Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP) and Ramsay sedation score were recorded at 1, 2 and 5 min after completion of administration of study drug. Fentanyl 2 μg/kg was administered to all patients and propofol was given until loss of verbal contact. Intubation was facilitated with vecuronium 0.1 mg/kg i.v. Anesthesia was maintained with oxygen (O2) and nitrous oxide (N2O) 33%: 67% and isoflurane. Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP) was noted at 1 min, 2 min and 5 min after intubation.
Statistical Analysis Used:
For statistical analysis of the clinical data obtained, the analysis of variances (ANOVA) with paired t-test was used.
Results:
Pretreatment with dexmedetomidine 1 ug/kg attenuated, but did not totally abolish the cardiovascular and catecholamine responses to tracheal intubation after induction of anesthesia. In our present study, HR, SBP, DBP all increased after intubation at 1, 2, 3 and 5 min in both the groups, but the rise was significantly less in the dexmedetomidine group. Requirement of propofol was significantly less in the dexmedetomidine group.
Conclusions:
Preoperative administration of a single dose of dexmedetomidine blunted the hemodynamic responses during laryngoscopy, and reduced anesthetic requirements.
Keywords: Anesthetic requirement, dexmedetomidine, intubation reflexes, premedication, sedation, α2 adrenergic
INTRODUCTION
Laryngoscopy and endotracheal intubation are well known to cause tachycardia and hypertension due to rise in plasma concentration of catecholamine and may be associated with myocardial ischemia and arrhythmia.[1,2] Such hemodynamic responses may be attenuated by several methods, including administration of intravenous (I.V) opioids, vasodilators, local anesthetics, β blockers or by deepening anesthesia. α2 adrenergic agonists decrease sympathetic tone and preoperative use of clonidine has been shown to blunt the hemodynamic responses to noxious stimulation and to prevent the overall hemodynamic variability.[3,4] Dexmedetomidine is a highly selective α2 receptor agonist having eight times high affinity and α2 selectivity compared to clonidine and has a shorter duration of action than clonidine.[5,6] It provides anxiolysis, co-operative sedation and analgesia without respiratory depression.[7] The mechanism of action of dexmedetomidine differs from clonidine as it possesses selective alpha2-adrenoceptor agonism, especially for the 2A subtype of this receptor, which causes it to be a much more effective sedative and analgesic agent than clonidine.[5,6]
The hemodynamic effects of dexmedetomidine result from peripheral and central mechanism. Alpha2-adrenoreceptor agonists show a biphasic, dose-dependent, blood pressure effect. At low doses the dominant action of α2-adrenoreceptor agonist activation is a reduction in sympathetic tone, mediated by a reduction of norepinephrine release at the neuroeffector junction, and an inhibition of neurotransmission in sympathetic nerves.[8] The net effect of dexmedetomidine action is a significant reduction in circulating catecholamines with a slight decrease in blood pressure and a modest reduction in heart rate.[9]
Myocardial ischemia might occur during the induction - intubation sequence in patients with coronary artery disease. Intraoperative ischemia has been associated with a high rate of perioperative myocardial infarction.[10] The α2-adrenoreceptor agonists attenuate the stress response and therefore, potentially reduce cardiovascular complications. There are a large number of studies that evaluated dexmedetomidine as an adjunct to cardiac surgery.
Wijeysundera et al.,[10] investigated the effects of α2 adrenoreceptor agonists, including dexmedetomidine, clonidine, and mivazerol, on perioperative cardiovascular complications and mortality in adults undergoing vascular and cardiac surgery. During cardiac and vascular surgery, α2-adrenoreceptor agonists reduced the number of ischemic episodes and were associated with a reduced risk of myocardial infarction and trend toward decreased mortality.
It simultaneously potentiates the effects of general anesthetic agents, reduces their dose requirements and attenuates sympathoadrenal responses to noxious stimuli encountered during anesthesia and surgery, thus providing improved hemodynamic, metabolic and hormonal stability.[11] In paediatric population, it has been successfully used to reduce emergence agitation and opioid requirement without adverse hemodynamic effect and respiratory depression.[12] Excellent intubating condition with stable hemodynamics has been achieved with dexmedetomidine during awake fibreoptic intubation.[13,14]
This prospective, randomized, double blinded study was planned to investigate the hemodynamic effects of intravenous dexmedetomidine used as anesthetic adjunct during induction of anesthesia. We hypothesized that, in combination with fentanyl 2 μg/kg, I.V dexmedetomidine administered prior to endotracheal intubation may attenuate the hemodynamic response to intubation without causing hemodynamic compromise.
MATERIALS AND METHODS
We studied 50 (ASA grade 1 and 2) patients undergoing major elective surgery [Table 1]. ASA grade 2 patients were selected among the properly treated hypertensive and ischemic heart disease patients controlled by drugs. The study was approved by the Ethics Committee of the Hospital and written informed consent was obtained from all patients. Patients taking any medication, with childbearing potential or with a known allergy were excluded. The patients were allocated randomly into 2 groups of 25 each to receive either dexmedetomidine 1 μg/kg dissolved in 10 ml normal saline (NS) (group 1) over 10 min or placebo- 10 ml NS (group 2) over 10 min before induction of anesthesia. Randomization was done using computer generated random numbers. Allocation concealment was ensured with sealed opaque envelope. The study was conducted in a double-blind fashion by the use of coded syringe. The study was conducted between January 2011 to June 2011.
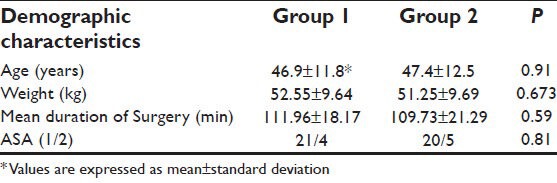
Table 1.
The demographic profile of patients in both the groups
After arrival of the patients to the operating room, multichannel monitor (electrocardiogram, oxygen saturation, non-invasive blood pressure) was attached and monitored continuously. Preoxygenation was started. All the patients received glycopyrrolate 0.2 mg I.V, ondansetron 4 mg I.V and fentanyl 2 μg/kg I.V. Either Dexmedetomidine (Group 1) or NS (Group 2) was administered over 10 min. HR, SBP, DBP and Ramsay sedation score were recorded at 1 min and 2 min after completion of administration of study drug. Ramsay sedation score was studied and level of sedation was assessed after 1 min, 2 min after administration of drug. Then induction was done with propofol 1% and dose requirement for loss of verbal contact was noted. Intubation was facilitated with vecuronium 0.1 mg/kg I.V. All the intubations were done by expert anaesthesiologist within 15 seconds. Anaesthesia was maintained with O2 and N2O 33%: 67% and isoflurane. HR, SBP, DBP were noted at 1 min, 2 min and 5 min after intubation. Isoflurane concentration was adjusted to maintain systolic blood pressure within 20% of preoperative values. After extubation no adverse effects were noted in both the groups.
RESULTS
The demographic data in both groups was comparable, the mean age being 46.9 ± 11.8 years in Group 1, 47.4 ± 12.5 years in Group 2. The mean weights in both the groups were 52.55 ± 9.64 kg and 51.25 ± 9.69 kg, respectively. ASA grade were similar and mean duration of surgery was also comparable in both the groups 111.96 ± 18.17 min and 109.73 ± 21.29 min in Group 1 and Group 2 respectively and found to be statistically non significant. (P > 0.05) [Table 1].
Mean heart rate [Table 2] increased in group 1compared to Group 2 up to 1 and 2 min after administration of dexmedetomidine but it was not statistically significant (85.1 ± 16.12 in Group 1 vs. 89.9 ± 9.96 in Group 2 after 1 min and 82.4 ± 14.57 in Group 1 vs. 88.7 ± 9.9 in Group 2 after 2 min). But after 1, 2, 3 and 5 min of intubation the increase of mean heart rate was significantly less (P < 0.05) in Group 1 (110 ± 16.75 in Group 1 vs. 122.8 ± 11.4 in Group 2, 101 ± 13.96 in Group 1 vs. 114 ± 7.9 in Group 2, 97.6 ± 14.75 in Group 1 vs. 106.6 ± 10.03 in Group 2, 88.6 ± 10.76 in Group 1 vs. 98.6 ± 14.07 in Group 2 at 1, 2, 3, 5 min respectively after intubation) [Figure 1].
Table 2.
Heart rate (beats per minute) in two groups at different point of time and its statistical significance
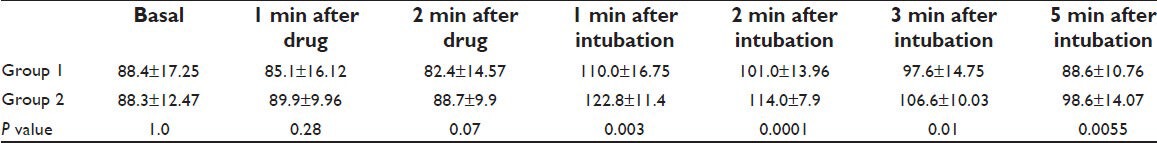
Figure 1.
Comparison of mean heart rate (beats per minute)
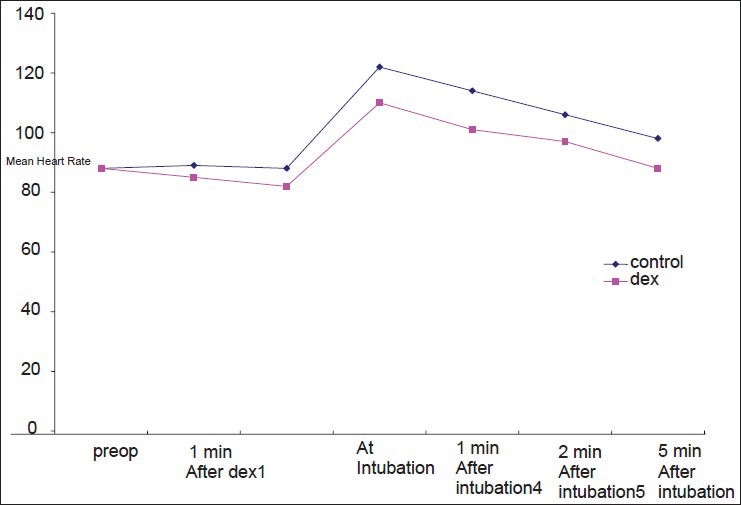
Mean systolic blood pressure [Table 3] was 136.4 ± 17.68 mm Hg in Group 1 and 127.7 ± 5.68 mm Hg in Group 2 after 1 min and 130.3 ± 18.44 mm Hg in Group 1 and 127.8 ± 9.71 mm Hg in Group 2 after 2 min of administration of dexmedetomidine. Mean diastolic blood pressure [Table 4] was 87.9 ± 11.74 mm Hg in Group 1 and 80.06 ± 3.06 mm Hg in Group 2 after 1 min and 83.0 ± 11.91 mm Hg in Group 1 and 82.2 ± 4.11 mm Hg in Group 2 after 2 min of administration of dexmedetomidine.
Table 3.
Systolic blood pressure (mm hg) in two groups at different point of time and its statistical significance
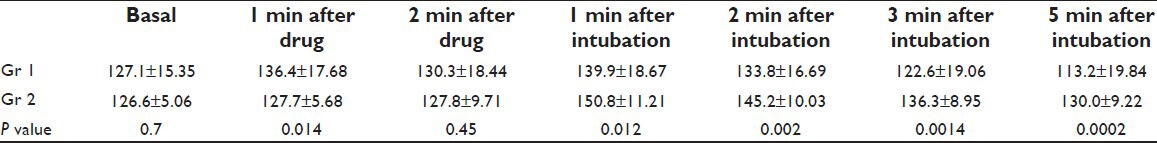
Table 4.
Diastolic blood pressure (mm hg) in two groups at different point of time and its statistical significance
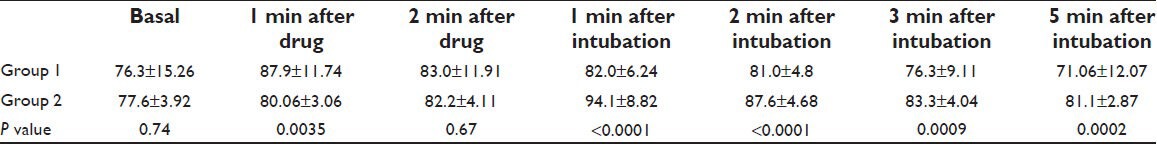
Differences of both, mean systolic and diastolic blood pressure at 2 min after administration of dexmedetomidine was not statistically significant (P > 0.05) as opposed to 1 min which was statistically significant (P value 0.01 for systolic and 0.003 for diastolic blood pressure).
Mean systolic blood pressure after 1, 2, 3, 5 min after intubation were 139.9 ± 18.67 mm Hg in Group 1 vs. 150.8 ± 11.21 mm Hg in Group 2, 133.8 ± 16.69 mm Hg in Group 1 vs. 145.2 ± 10.03 mm Hg in Group 2, 122.6 ± 19.06 mm Hg in Group 1 vs. 136.3 ± 8.95 mm Hg in Group 2, 113.2 ± 19.84 mm Hg in Group 1 vs. 130.0 ± 9.22 mm Hg in Group 2, respectively. Mean diastolic blood pressure after 1, 2, 3, 5 min after intubation were 82.0 ± 6.24 mm Hg in Group 1 vs. 94.1 ± 8.82 mm Hg in Group 2, 81.0 ± 4.8 mm Hg in Group 1 vs. 87.6 ± 4.68 mm Hg in Group 2, 76.3 ± 9.11 mm Hg in Group 1 vs. 83.3 ± 4.04 mm Hg in Group 2, 71.06 ± 12.07 mm Hg in Group 1 vs. 81.1 ± 2.87 mm Hg in Group 2, respectively.
So after 1 min, 2 min, 3 min and 5 min of intubation the rise of both mean SBP and DBP was significantly less in Group 1 (P < 0.05) [Figures 2 and 3].
Figure 2.
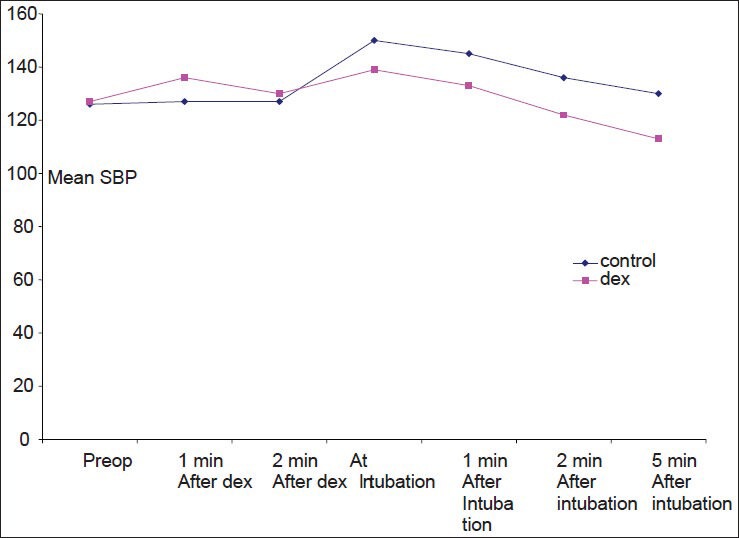
Comparison of mean systolic blood pressure (mm Hg)
Figure 3.
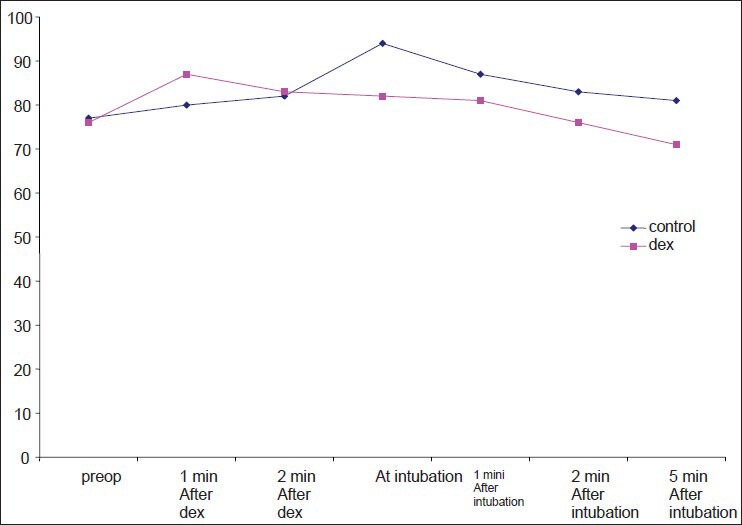
Comparison of mean diastolic blood pressure (mm Hg)
Mean induction dose of propofol [Table 5] was much less in group 1 (55 ± 7.31 mg in Group 1 vs. 95 ± 7.43 mg in Group 2) which was statistically highly significant (P < 0.001) following pre-medication with dexmedetomidine as compared to control group [Figure 4].
Table 5.
Propofol requirement and its statistical significance

Figure 4.
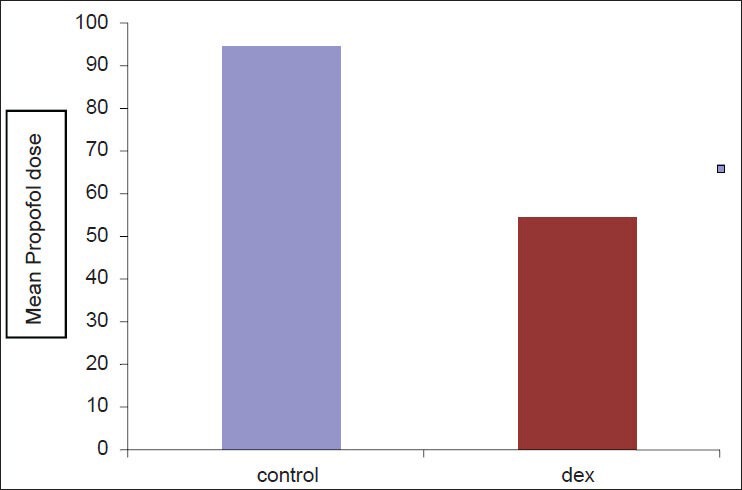
Comparison of required propofol dose (mg)
Ramsay sedation score [Table 6] was applied and sedation level was studied in both the groups [Table 7]. In Group 1 mean sedation score (2.8 ± 0.41 after 1 min, 2.73 ± 0.45 after 2 min of drug) was more as compared to Group 2 (1.5 ± 0.51 after 1 min, 1.125 ± 0.34 after 2 min of drug) and which was statistically significant (P < 0.05) [Figure 5].
Table 6.
Ramsay sedation score
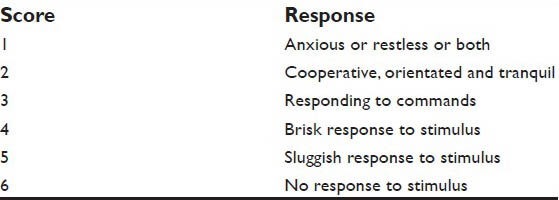
Table 7.
Sedation score and its statistical significance
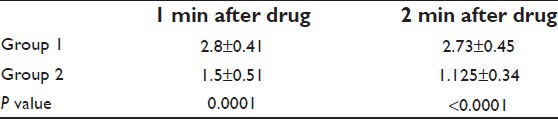
Figure 5.
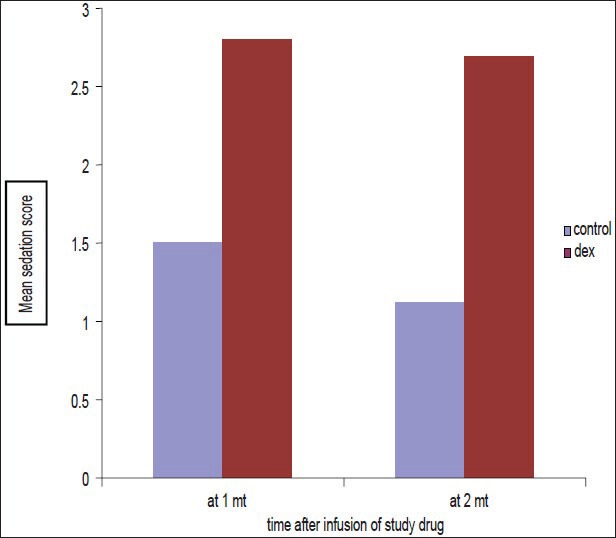
Comparison of mean sedation score
DISCUSSION
Tracheal intubation is associated with increase in arterial pressure, heart rate and plasma catecholamine concentrations. Opioids, adrenergic blocking agents, vasodilating agents and local anesthetics have been used to attenuate the hemodynamic effects of endotracheal intubation. In the present study, pretreatment with α2-adrenergic agonist dexmedetomidine 1ug/kg attenuated, but did not totally abolish the cardiovascular and catecholamine surge responses to tracheal intubation after induction of anesthesia. After administration of dexmedetomidine before intubation there was a fall in mean heart rate compared to control group, which was not statistically significant (P value 0.28 and 0.07 after 1 and 2 min respectively). Varshali M Kenya et al.,[15] also observed bradycardia in their study with dexmedetomidine and no fall in blood pressure. In our study, both systolic and diastolic blood pressure increased after 1 and 2 min of administration of dexmedetomidine compared to control group and the increase was statistically significant at 1 min (P value 0.01 for systolic and 0.003 for diastolic blood pressure). Similar increase in blood pressure was observed by Bloor et al.[8]
In our present study, the rise in mean heart rate, systolic blood pressure and diastolic blood pressure after intubation at 1, 2, 3 and 5 min was significantly less in dexmedetomidine group compared to control group. In both the groups, the systolic and diastolic blood pressure increased after intubation compared to baseline but in the dexmedetomidine group (Group 1) pressure came to baseline or below baseline after 3 min of intubation. Mean heart rate also increased in both the groups compared to baseline but in Group 1 it came to baseline at 5 min.
Scheinin et al.,[16] also observed that dexmedetomidine attenuated the cardiovascular responses to laryngoscopy and tracheal intubation. In their study, they measured catecholamine concentration and found that the concentration of noradrenaline in mixed venous plasma was smaller in the dexmedetomidine group during all phases of induction. Ferdi Menda et al.,[17] concluded that dexmedetomidine effectively blunts the hemodynamic response to endotracheal intubation in patients undergoing myocardial re-vascularization and can be safely used at induction of general anesthesia in combination with fentanyl even among patients receiving beta blockers.
Sağıroğlu et al.,[18] conducted a study with different doses of dexmedetomidine and found that to control hemodynamic responses to tracheal intubation, dexmedetomidine 1 μg/kg is more effective than dexmedetomidine 0.5 μg/kg without any side effect.
So we conducted the study with dose of 1 μg/.kg of dexmedetomidine.
In our study, we observed that requirement of propofol was significantly (P < 0.0001) less in dexmedetomidine group than in control group as was found by Scheinin and co-workers regarding requirement of thiopentone.[16]
Many other authors have used single dose dexmedetomidine prior to induction and have achieved suppression of hemodynamic responses during laryngoscopy and intubation and also have noticed reduction of anesthetic requirement.[16,18] Stress response to extubation is equally suppressed by dexmedetomidine given prior to reversal.[19,20]
Even with other routes of administration e.g., intranasal dexmedetomidine has produced good sedation, anxiolysis and stable hemodynamics.[21]
Sedation was significantly more in dexmedetomidine group at 1 min and 2 min after infusion of the drug but SpO2 was not affected. Sağıroğlu A et al.,[18] also found no respiratory depression or decrease in SpO2 with similar dose of dexmedetomidine. In another study, in which the infusion of opioid and α2 adrenergic agonists were compared, it was concluded that dexmedetomidine doesn’t cause significant respiratory depression and it decreases the risk of apnea.[22]
The major limitations of our study being a single center study was that it was not feasible to validate our conclusion as the sample size was small (n = 25). Though we found that propofol requirement was much less in the dexmedetomidine group but depth of anaesthesia was not substantiated by bispectral index monitoring.[23] Hemodynamic stability offered by dexmedetomidine would have been better established by measuring plasma catecholamine level which was not practically feasible in our institute. Future study on larger number of patients could strongly prove the hypothesis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Shibman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth. 1987;59:295–9. doi: 10.1093/bja/59.3.295. [DOI] [PubMed] [Google Scholar]
- 2.Longnecker DE. Alpine anesthesia: Can pretreatment with clonidine decrease the peaks and valleys? Anesthesiology. 1987;67:1–2. [PubMed] [Google Scholar]
- 3.Aantaa R, Scheinin M. α-2-adrenergic agents in anesthesiology. Acta Anaesthesiol Scand. 1993;37:433–48. doi: 10.1111/j.1399-6576.1993.tb03743.x. [DOI] [PubMed] [Google Scholar]
- 4.Quintin L, Bonnet F, Macquin I. Aortic surgery: Effect of clonidine on intraoperative catecholaminergic and circulatory stability. Acta Anaesthesiol Scand. 1990;34:132–7. doi: 10.1111/j.1399-6576.1990.tb03057.x. [DOI] [PubMed] [Google Scholar]
- 5.Virtanen R, Savola J, Nyman L. Characterization of the selectivity, specifity and potency of medetomidine as an α-2 adrenoceptor agonist. Eur J Pharmacol. 1988:9–14. doi: 10.1016/0014-2999(88)90744-3. [DOI] [PubMed] [Google Scholar]
- 6.Scheinin H, Virtanen R, MacDonald E, Lammintausta R. Medetomidine-a novel α-2-adrenoceptor agonist: A review of its pharmacological effects. Prog Neuro-Psychopharmacol Biol Psychiatry. 1989;13:635–51. doi: 10.1016/0278-5846(89)90051-1. [DOI] [PubMed] [Google Scholar]
- 7.Keith A, Sergio D, Paula M, Marc A, Wisemandle W, Alex Y. Monitored anesthesia care with dexmedetomidine: A prospective, randomized, double-blind, multicenter trial. Anesth Analg. 2010;110:47–56. doi: 10.1213/ane.0b013e3181ae0856. [DOI] [PubMed] [Google Scholar]
- 8.Bloor BC, Ward DS, Belleville JP, Maze M. Effects of intravenous dexmedetomidine in humans. II. Hemodynamic changes. Anesthesiology. 1992;77:1134–42. doi: 10.1097/00000542-199212000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Khan ZP, Ferguson CN, Jones RM. Alpha-2 and imidazoline receptor agonists. Their pharmacology and therapeutic role. Anaesthesia. 1999;54:146–65. doi: 10.1046/j.1365-2044.1999.00659.x. [DOI] [PubMed] [Google Scholar]
- 10.Wijeysundera DN, Naik JS, Beattie WS. Alpha-2 adrenergic agonists to prevent perioperative cardiovascular complications: A meta-analysis. Am J Med. 2003;114:742–52. doi: 10.1016/s0002-9343(03)00165-7. [DOI] [PubMed] [Google Scholar]
- 11.Taittonen MT, Kirvela OA, Aantaa R, Kanto JH. Effect of clonidine and dexmedetomidine premedication on perioperative oxygen consumption and hemodynamic state. Br J Anaesth. 1997;78:400–6. doi: 10.1093/bja/78.4.400. [DOI] [PubMed] [Google Scholar]
- 12.Patel A, Davidson M, Tran MC, Quraishi H. Dexmedetomidine infusion for analgesia and prevention of emergence agitation in children with obstructive sleep apnea syndrome undergoing tonsillectomy and adenoidectomy. Anesth Analg. 2010;111:1004–10. doi: 10.1213/ANE.0b013e3181ee82fa. [DOI] [PubMed] [Google Scholar]
- 13.Avitsian R, Manlapaz M, Doyle J. Dexmedetomidine as a sedative for awake fiberoptic intubation. In Trauma Care. 2007;17:1. [Google Scholar]
- 14.Kunisawa T, Nagashima M, Hanada S, Suzuki A, Takahata O, Iwasaki H. Awake intubation under sedation using target-controlled infusion of dexmedetomidine: Five case reports. J Anesth. 2007;24:789–92. doi: 10.1007/s00540-010-0980-8. [DOI] [PubMed] [Google Scholar]
- 15.Keniya VM, Ladi S, Naphade R. Dexmedetomidine attenuates sympathoadrenal response to tracheal intubation and reduces perioperative anaesthetic requirement. Indian J Anaesth. 2011;55:352–7. doi: 10.4103/0019-5049.84846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scheinin B, Lindgren L, Randell T, Scheinin H, Scheinin M. Dexmedetomidine attenuates sympathoadrenal responses to tracheal intubation and reduces the need for thiopentone and peroperative fentanyl. Br J Anaesth. 1992;68:126–31. doi: 10.1093/bja/68.2.126. [DOI] [PubMed] [Google Scholar]
- 17.Menda F, Koner O, Sayin M, Ture H, Imer P, Aykac B. Dexmedetomidine as an adjunct to anesthetic induction to attenuate hemodynamic response to endotracheal intubation in patients undergoing fast-track CABG. Ann Card Anaesth. 2010;13:16–21. doi: 10.4103/0971-9784.58829. [DOI] [PubMed] [Google Scholar]
- 18.Sağıroğlu AE, Celik M, Orhon Z, Yüzer S, Sen B. Dıfferent doses of dexmedetomidine on controlling haemodynamic responses to tracheal intubation. Internet J Anesthesiol. 2010;27:2. [Google Scholar]
- 19.Yildiz M, Tavlan A, Tuncer S, Reisli R, Yosunkaya A, Otelcioglu S. Effect of dexmedetomidine on haemodynamic responses to laryngoscopy and intubation: Perioperative haemodynamics and anaesthetic requirements. Drugs R D. 2006;7:43–52. doi: 10.2165/00126839-200607010-00004. [DOI] [PubMed] [Google Scholar]
- 20.Lee YY, Wong SM, Hung CT. Dexmedetomidine infusion as a supplement to Isoflurane anaesthesia for vitreoretinal surgery. Br J Anaesth. 2007;98:477–83. doi: 10.1093/bja/aem040. [DOI] [PubMed] [Google Scholar]
- 21.Jain D, Khan RM, Maroof M. Effect of dexmedetomidine on stress response to extubation. The Internet J Anesthesiol. 2009;21:1. [Google Scholar]
- 22.Yuen VM, Irwin MG, Hui TW, Yuen MK, Lee LH. A double-blind, crossover assessment of the sedative and analgesic effects of intranasal dexmedetomidine. Anesth Analg. 2007;105:374–8. doi: 10.1213/01.ane.0000269488.06546.7c. [DOI] [PubMed] [Google Scholar]
- 23.Hsu YW, Cortinez LI, Robertson KM, Keifer JC, Sum-Ping ST, Moretti EW, et al. Dexmedetomidine pharmacodynamics: Part I: Crossover comparison of the respiratory effects of dexmedetomidine and remifentanil in healthy volunteers. Anesthesiology. 2004;101:1066–76. doi: 10.1097/00000542-200411000-00005. [DOI] [PubMed] [Google Scholar]


