Abstract
Background:
Thoracic spinal anesthesia has been used for laparoscopic cholecystectomy and abdominal surgeries, but not in breast surgery. The present study compared this technique with general anesthesia in breast cancer surgeries.
Materials and Methods:
Forty patients were enrolled in this comparative study with inclusion criteria of ASA physical status I-III, primary breast cancer without known extension beyond the breast and axillary nodes, scheduled for unilateral mastectomy with axillary dissection. They were randomly divided into two groups. The thoracic spinal group (S) (n = 20) underwent segmental thoracic spinal anesthesia with bupivacaine and fentanyl at T5-T6 interspace, while the other group (n = 20) underwent general anesthesia (G). Intraoperative hemodynamic parameters, intraoperative complications, postoperative discharge time from post-anesthesia care unit (PACU), postoperative pain and analgesic consumption, postoperative adverse effects, and patient satisfaction with the anesthetic techniques were recorded.
Results:
Intraoperative hypertension (20%) was more frequent in group (G), while hypotension and bradycardia (15%) were more frequent in the segmental thoracic spinal (S) group. Postoperative nausea (30%) and vomiting (40%) during PACU stay were more frequent in the (G) group. Postoperative discharge time from PACU was shorter in the (S) group (124 ± 38 min) than in the (G) group (212 ± 46 min). The quality of postoperative analgesia and analgesic consumption was better in the (S) group. Patient satisfaction was similar in both groups.
Conclusions:
Segmental thoracic spinal anesthesia has some advantages when compared with general anesthesia and can be considered as a sole anesthetic in breast cancer surgery with axillary lymph node clearance.
Keywords: Anesthesia, general, mastectomy, segmental, spinal, thoracic
INTRODUCTION
The incidence of breast cancer, as well as the need of surgical treatment, has increased probably due to prevention campaigns and modern diagnostic tools. Nowadays, surgical intervention is more conservative, but in most cases, partial or total mastectomy associated with axillary exploration to remove lymph nodes for staging or immune-chemical testing is still necessary.[1] General anesthesia is currently the standard technique used for surgical treatment of breast cancer. The drawbacks of general anesthesia include, but not limited to, inadequate pain control due to a lack of residual analgesia, high incidence of nausea and vomiting, and increasing the length of hospitalization.[2] Increasing hospital costs have focused attention on reducing the length of hospital stay for these patients. However, the side-effects and complications of general anesthesia preclude ambulatory surgery for most patients undergoing breast surgery.[3]
The anatomy of the thoracic spinal canal was investigated with magnetic resonance imaging (MRI) in 50 patients.[4] The space between the dura mater and spinal cord in the thoracic region measured with MRI was 5.19 mm at T2, 7.75 mm at T5, and 5.88 mm at T10 [Figure 1]. The angle of entry between T5 and T6 (almost 50°) elongated the distance from the tip of the needle to the posterior surface of the cord. MRI confirms that the spinal cord and the cauda equina are touching the dura mater posteriorly in the lumbar region and anteriorly in the thoracic region. [Figure 1][4] This position increases the distance to a point that allows needle advancement without touching the cord, such as in the case of accidental perforation of the dura mater during the administration of spinal anesthesia. This can be an explanation for the low incidence of neurologic complications during accidental perforation of the dura mater in an attempt to perform a thoracic epidural block.[5,6,7]
Figure 1.
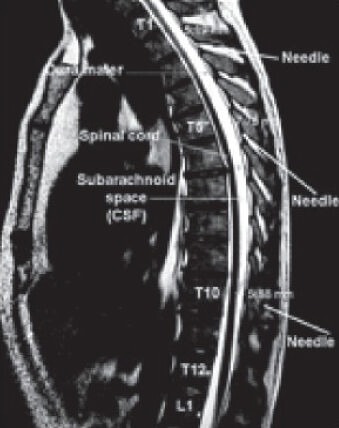
MRI of the thoracic column
There are a number of advantages to deliver the spinal anesthetic directly to the required heights in the body. Firstly, one of the most obvious advantages is that there is no blockade of the lower extremities, i.e. little caudal spread. This means that a significantly larger portion of the body experiences no venal dilation, and may offer a compensatory buffer to adverse changes in blood pressure intra-operatively. This is one of the major risks identified in surgery.[8] Secondly, the dosing of the anesthetic is exceedingly low, given the highly specific block to only certain nerve functions along a section of the cord. Thirdly, the degree of muscle relaxation achievable without central or peripheral respiratory or circulatory depression is superior to that with general anesthesia. In addition, the danger of cardiac arrest is much diminished. Fourthly, the patients have motor control over their legs during the surgery, which in turn means many patients exhibit a high level of satisfaction with the technique and decreased anxiety.[9]
Thomas Jonnesco[10] described the use of spinal anesthesia for surgeries in the skull, head, neck, and the thorax. The punctures were performed between the 1st and the 2nd thoracic vertebrae, which resulted in good analgesia for the head, neck, and upper limbs. Recently, thoracic spinal anesthesia was practiced by van Zundert et al. for laparoscopic cholecystectomy in a patient with severe obstructive lung disease using low thoracic puncture (T10) for combined spinal-epidural block.[11] Then, they performed a feasibility study of segmental spinal anesthesia in healthy patients submitted to laparoscopic cholecystectomy.[12] The aim of the present study was to compare segmental thoracic spinal anesthesia and general anesthesia in female patients undergoing breast cancer surgery with axillary exploration, evaluating intraoperative hemodynamic parameters, discharge time, postoperative analgesia, patient satisfaction and side-effects, such as nausea and vomiting.
MATERIALS AND METHODS
This study was approved by the medical ethical committee at the Medical Research Institute, Alexandria University, and patients were enrolled after signing an informed consent. During the period of January to April 2013, 40 patients, with inclusion criteria of ASA physical status I-III, primary breast cancer without known extension beyond the breast and axillary nodes, scheduled for unilateral mastectomy with axillary dissection. The exclusion criteria included patients aged <20 or > 65 years old, inflammatory breast cancer, previous surgery for breast cancer (except diagnostic lumpectomy), body mass index above 35 Kg/m2, and any condition contra-indicating spinal anesthesia. The patients were randomly divided into two groups; 20 patients each using sealed envelope method. Patients’ preoperative evaluation and preparation were standardized. All patients were informed about thoracic spinal anesthesia in detail, that any anxiety, discomfort or pain during surgery would be dealt with intravenous medications. The patients were also informed about the probability of conversion to general anesthesia, if needed, and written informed consents were obtained. All patients were intramuscularly administered 1-2 mg of midazolam IM hydrochloride half an hour before admission to the operating theater. On patient arrival in the operating room and after establishing non-invasive monitoring (electrocardiogram, non-invasive arterial blood pressure, and pulse oximetry), a 500-1000 mL of Ringer acetate solution was commenced intravenously for every patient. After obtaining baseline vital signs, oxygen at 4 L/min was commenced through a face mask or nasal cannula. Afterwards, patients underwent general anesthesia or segmental thoracic spinal anesthesia, according to the group they were assigned to.
Thoracic spinal group
Before the blockade, patients received intravenously 1 μg.kg−1 of fentanyl. After cleansing the skin with antiseptic preparation, the skin of the puncture site was infiltrated with 1% lidocaine. Patients were placed on the lateral decubitus or sitting position, and the puncture was performed via paramedian approach, at the T5-T6 interspace in all patients, with a 27G cut needle (B. Braun Melsungen AG). After piercing the ligamentum flavum, the needle's stylet was removed and the hub observed for free flow of CSF; once flow of clear CSF began, 1 ml of isobaric bupivacaine 0.5% in addition to 20 μg fentanyl were injected. The patient was then placed in supine position. After testing the quality of anesthesia (adequate sensory block to pin prick from the lower border of the clavicle to the inferior costal margin), the surgery was initiated. If the sensory block was inadequate after 10 minutes, the patient underwent general anesthesia. Hemodynamic parameters, oxygen saturation, and respiratory rate were recorded on admission to the operating theater, then every 5 minutes till end of surgery. Hypotension, defined as fall of mean blood pressure by 30% from baseline reading, or systolic pressure below 90 mm hg, or bradycardia, heart rate below 60 b/minute were treated with ephedrine 8 mg, or atropine 0.01 mg.kg-1, respectively.
General anesthesia group
Anesthesia was induced with propofol (1.5-2.5 mg/kg), fentanyl citrate (2 μg/kg), and atracurium besylate (0.5 mg/kg). Mechanical ventilation was started after intubation of the trachea; anesthesia was maintained with isoflurane in 100% oxygen. Ventilation was controlled with a tidal volume of 6 to 8 mL/kg, and the ventilatory rate was adjusted to maintain a PaCO2 value of 35 to 40 mmHg. Residual neuromuscular block was antagonized with 2.5 mg of neostigmine and 1 mg of atropine sulfate at the end of surgery.
Intra operatively, the adequacy of the block in group S, hemodynamic changes, and other complications, such as the occurrence of paresthesia, nausea, vomiting, and pruritis were recorded as well as the length of the surgery.
All patients were transferred to the PACU. Discharge time was recorded as the time from admission to recovery room until the patient met all discharge criteria from it. These included mental alertness, stable vital signs, absence of nausea or vomiting, control of pain, and (for regional techniques) voiding. Side-effects measured were the incidence of nausea, vomiting, pruritis, urine retention, pain severe enough to require IV rescue analgesics. Postoperatively, all patients were given 75 mg of diclofenac sodium intramuscularly every 12 hours, 500 mg of acetaminophen every 6 hours, and supplementary tramadol 50 mg IV as a rescue analgesic. Postoperative pain was assessed at relaxed conditions by using the visual analog scale (VAS) at the completion of surgery, 4, 8, 12, and 24 hours after the completion of the procedure.
For the statistical analysis, data are shown as mean ± standard deviation in absolute numbers or proportions. Chi-Square test, Monte Carlo test, and Fisher's Exact test were used to test for the qualitative data. Student t test was used to test for quantitative variables. Significant results were detected at P ≤ 0.05.
RESULTS
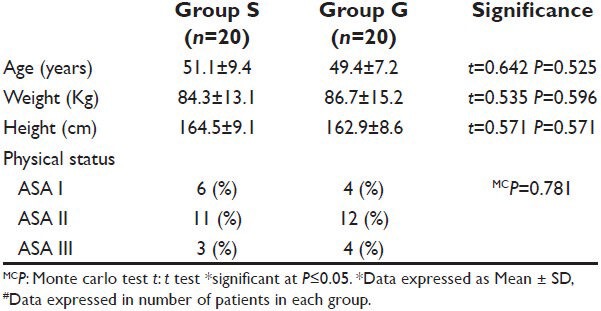
The thoracic spinal anesthesia was successful in all patients of group S without conversion to general anesthesia. The demographic data showed no statistically significant differences between both groups [Table 1].
Table 1.
Demographic data of the studied patients of both groups
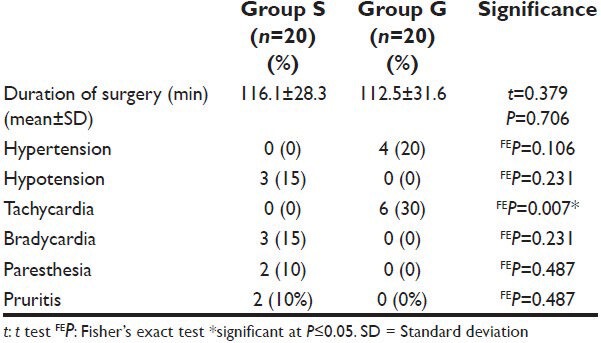
As regards the duration of surgery, there was no difference between the two groups. Regarding the intraoperative hemodynamic changes, hypertension occurred in 4 patients (20%) in group G, while 3 patients (15%) in group S developed hypotension. Tachycardia occurred in 6 patients (30%) in group G, while bradycardia occurred in 3 patients (15%) in group S. Two patients developed paresthesia during spinal puncture in group S, which disappeared after stylet withdrawal and without sequelae. Two patients in group S developed intraoperative pruritis. No intraoperative nausea or vomiting developed in any patient in either group Table 2.
Table 2.
Intraoperative complications of the two study groups
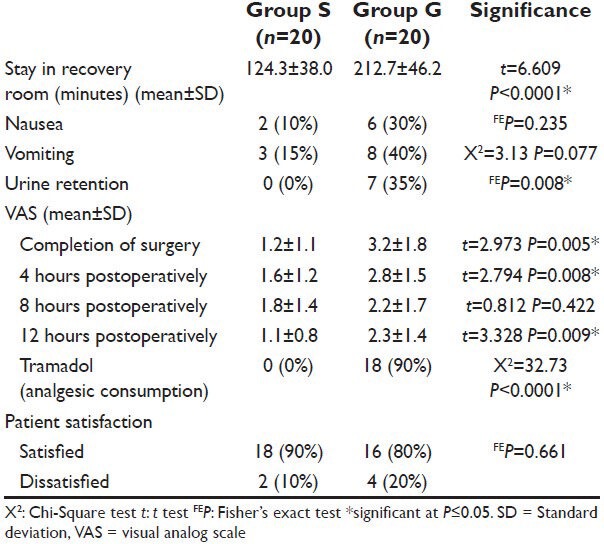
Postoperatively, the length of stay in PACU, nausea, and vomiting was significantly lower in group S. No pruritis developed in any patient of any group. Urine retention occurred in 7 patients in group G, while none in group S with significant difference. VAS was significantly less in group S than in group G at completion of surgery, 4, 8, and 12 hours postoperatively. The intensity of pain and consumption of supplementary analgesics were lower in group S. Supplementation with tramadol was used only for patients in group G, while pain was easily controlled with non-steroidal anti-inflammatory drugs in group S. Satisfaction with the anesthesia was similar in both groups Table 3.
Table 3.
Postoperative complications of the two study groups
DISCUSSION
Neuraxial anesthesia can inhibit the neuroendocrine stress response, and patients who receive regional analgesia have lower opioid requirements.[5] Paravertebral analgesia can reduce opioid requirements after breast surgery.[13] Opioids may themselves inhibit cell-mediated immunity and host anti-tumor defenses.[14,15,16,17,18,19,20] Because it negatively affects patients’ daily lives, methods to prevent and reduce chronic pain and its severity should be developed.[21] In our study, the segmental thoracic spinal showed some advantages over general anesthesia for the treatment of breast cancer. There were no recorded neurological complications.
The amount of CSF at thoracic levels is diminished compared to lumbar and cervical levels,[22] and the thoracic nerve roots are very slight compared to segments above and below.[23] Thus, there is less anesthetic dilution per segmental unit of distance from the site of injection, and the roots are easily blocked due to their small size, both factors predicting efficient blockade of these segments.
The thoracic spinal block was practiced at the mid-thoracic level without any great difficulty. Two patients experienced some paresthesia during initial insertion of the spinal needle; these symptoms responded to needle withdrawal and not leading to any postoperative sequelae or neurological deficits. Paresthesia can occur with any technique of spinal anesthesia, but are of potentially greater significance when the needle is inserted above the termination of the spinal cord. The low potential for cord damage with this technique was given in the earlier case report by Zundert and colleagues,[12] where it was noted that the thoracic segment of the cord lies anteriorly. Imbelloni et al. showed in their study that the incidence of paresthesia in a study with 300 patients subjected to thoracic spinal puncture at T10-11 was 4.67% in the cut needle and 8.67% in the pencil point needle group, and without sequelae,[24] similar to the incidence reported by other investigators in lumbar spinal anesthesia.[25,26]
During the intra-operative period, the quality of anesthesia was adequate in all patients of group S. No patient in group S developed any respiratory abnormalities like apnea or hypopnea or hypoxemia (SpO2 <90%). In agreement with us, Van Zundert et al. published a case-report in which a patient with severely abnormal respiratory function (chronic obstructive pulmonary disease with severe emphysema attributed to homozygote α-1-anti-trypsine deficiency), requiring continuous oxygen therapy, had frequent respiratory infections and severe functional impairment.[11] Even with minimal activity, the patient developed hypoxemia. Using the thoracic CSE technique, with a minute dose of local anesthetic, cholecystectomy could be performed successfully, with no problems preoperatively. The patient was discharged from the hospital on day 4 with no further deterioration of his pulmonary function.
Minimal hypotension and bradycardia occurred in 25% of patients in group S, and they were easily controlled with increments of ephedrine and atropine, respectively. Imbelloni et al. used a spinal anesthesia with similarly reduced dose of hyperbaric bupivacaine (7.5 mg) given in combination with 20 μg fentanyl in T10-11 in patients undergoing laparoscopic cholecystectomy affords better hemodynamic stability and fewer adverse events, as reflected in the minimal need for vasopressor support in a study comparing laparoscopic cholecystectomy under thoracic spinal anesthesia with low-dose hyperbaric bupivacaine.[27] The occurrence of hypertension (20%) and tachycardia (30%) in group G may be explained by surgical stress response.
Patients undergoing breast surgery are normally associated with a high incidence of postoperative nausea and vomiting (PONV). Troublesome pain and PONV can prolong recovery and hospitalization, and are some of the most common causes of hospital admission following ambulatory surgery.[28] Regional block has a lower incidence of nausea and vomiting, when compared with general anesthesia, which has been demonstrated in several procedures and studies.[29] In our study, we reported an incidence of 70% of POVN among patients of general anesthesia, compared with significantly lower incidence of 25% in segmental thoracic anesthesia group. These results are consistent with those of Bansal et al., who mentioned that the incidence of PONV during the 24-hour interval after breast cancer surgery was higher in general anesthesia group, and that 75% of patients in that group required antiemetic.[30]
Postoperative pain varied significantly between groups; in group S, patients did not complain of very strong or strong pain and the request for supplementary analgesic was lower. Tramadol was not used postoperatively in patients in the spinal group. Adequate control of pain in this situation is important since it makes for a better postoperative period and early hospital discharge, and can have a long-term effect, decreasing complications such as chronic pain.[31,32] The length of stay in the recovery room and in the hospital was less in the thoracic spinal group compared with the general anesthesia one. Yousef et al., who studied the effect of thoracic spinal anesthesia (TSA) in laparoscopic cholecystecomy, showed that pain assessed throughout any time in the postoperative period at 2, 4, 6, 8, and 12 hours was significantly lesser in the TSA group compared to GA group, and attributed that to the residual analgesic effect of local anesthetic and fentanyl in subarachnoid space.[33]
No pruritis developed in any patient of any group. Urine retention occurred in 7 patients in group G, while none in group S. This may be explained by the ability of thoracic spinal anesthesia to preserve the motor power in both lower limbs. Satisfaction with the anesthesia was similar in both groups.
To conclude, single-dose thoracic spinal block associated with local anesthetic and opioid was an adequate option for mastectomy. Among its advantages are the quality of postoperative analgesia, lower incidence of nausea and vomiting, and shorter recovery time, with the consequent early hospital discharge.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Belzarena SD. Comparative Study between thoracic epidural block and general anesthesia for oncologic mastectomy. Rev Bras Anestesiol. 2008;58:561–8. doi: 10.1590/s0034-70942008000600001. [DOI] [PubMed] [Google Scholar]
- 2.Oddby-Muhrbeck E, Jakobsson J, Andersson L, Askergren J. Postoperative nausea and vomiting. A comparison between intravenous and inhalation anaesthesia in breast surgery. Acta Anaesthesiol Scand. 1994;38:52–6. doi: 10.1111/j.1399-6576.1994.tb03837.x. [DOI] [PubMed] [Google Scholar]
- 3.Coveney E, Weltz CR, Greengrass R, Iglehart JD, Leight GS, Steele SM, et al. Use of Paravertebral Block Anesthesia in the Surgical Management of Breast Cancer Experience in 156 Cases. Ann Surg. 1998;227:496–501. doi: 10.1097/00000658-199804000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Imbelloni LE, Quirici MB, Ferraz Filho JR, Cordeiro JA, Ganem EM. The anatomy of the thoracic spinal canal investigated with magnetic resonance imaging. Anesth Analg. 2010;110:1494–5. doi: 10.1213/ANE.0b013e3181d5aca6. [DOI] [PubMed] [Google Scholar]
- 5.Scherer R, Schmutzler M, Giebler R, Erhald J, Stöcker L, Kox WJ. Complications related to thoracic epidural analgesia: A prospective study in 1071 surgical patients. Acta Anaesthesiol Scand. 1993;37:370–4. doi: 10.1111/j.1399-6576.1993.tb03731.x. [DOI] [PubMed] [Google Scholar]
- 6.Giebler RM, Scherer RU, Peters J. Incidence of neurologic complications related to thoracic epidural catheterization. Anesthesiology. 1997;86:55–63. doi: 10.1097/00000542-199701000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Leão DG. Thoracic epidural anesthesia: Analysis of 1240 cases. Rev Bras Anestesiol. 1997;47:138–47. [Google Scholar]
- 8.Monk TG, Saini V, Weldon BC, Sigl JC. Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analg. 2005;100:4–10. doi: 10.1213/01.ANE.0000147519.82841.5E. [DOI] [PubMed] [Google Scholar]
- 9.Lee RA, Van Zundert AA, Visser WA, Lataster LM, Wieringa PA. Thoracic Combined Spinal-Epidural (CSE) Anaesthesia. Southern African J Anaesth and Analg. 2008;14:63–9. [Google Scholar]
- 10.Jonnesco T. Remarks on general spinal anesthesia. Br Med J. 1909;2:1396–401. doi: 10.1136/bmj.2.2550.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Zundert AA, Stultiens G, Jakimowicz JJ, van den Borne, van der Ham WG, Wildsmith JA. Segmental spinal anaesthesia for cholecystectomy in a patient with severe lung disease. Br J Anaesth. 2006;96:464–6. doi: 10.1093/bja/ael036. [DOI] [PubMed] [Google Scholar]
- 12.van Zundert AA, Stultiens G, Jakimowicz JJ, Peek D, van der Ham WG, Korsten HH, et al. Laparoscopic cholecystectomy under segmental thoracic spinal anaesthesia: A feasibility study. Br J Anaesth. 2007;98:682–6. doi: 10.1093/bja/aem058. [DOI] [PubMed] [Google Scholar]
- 13.Moller JF, Nikolajsen L, Rodt SA, Ronning H, Carlsson PS. Thoracic paravertebral block for breast cancer surgery: A randomized double-blind study. Anesth Analg. 2007;105:1848–51. doi: 10.1213/01.ane.0000286135.21333.fd. [DOI] [PubMed] [Google Scholar]
- 14.Beilin B, Martin FC, Shavit Y, Gale RP, Liebeskind JC. Suppression of natural killer cell activity by high-dose narcotic anesthesia in rats. Brain Behav Immun. 1989;3:129–37. doi: 10.1016/0889-1591(89)90013-5. [DOI] [PubMed] [Google Scholar]
- 15.Gupta K, Kshirsagar S, Chang L, Schwartz R, Law PY, Yee D, et al. Morphine stimulates angiogenesis by activating proangiogenic and survival-promoting signaling and promotes breast tumor growth. Cancer Res. 2002;62:4491–8. [PubMed] [Google Scholar]
- 16.Farooqui M, Li Y, Rogers T, Poonawala T, Griffin RJ, Song CW, et al. COX-2 inhibitor celecoxib prevents chronic morphine-induced promotion of angiogenesis, tumour growth, metastasis and mortality, without compromising analgesia. Br J Cancer. 2007;97:1523–31. doi: 10.1038/sj.bjc.6604057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beilin B, Shavit Y, Hart J, Mordashov B, Cohn S, Notti I, et al. Effects of anesthesia based on large versus small doses of fentanyl on natural killer cell cytotoxicity in the perioperative period. Anesth Analg. 1996;82:492–7. doi: 10.1097/00000539-199603000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Yeager MP, Colacchio TA, Yu CT, Hildebrandt L, Howell AL, Weiss J, et al. Morphine inhibits spontaneous and cytokine-enhanced natural killer cell cytotoxicity in volunteers. Anesthesiology. 1995;83:500–8. doi: 10.1097/00000542-199509000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Page GG, McDonald JS, Ben-Eliyahu S. Pre-operative versus postoperative administration of morphine: Impact on the neuroendocrine, behavioural, and metastatic-enhancing effects of surgery. Br J Anaesth. 1998;81:216–23. doi: 10.1093/bja/81.2.216. [DOI] [PubMed] [Google Scholar]
- 20.Sasamura T, Nakamura S, Iida Y, Fujii H, Murata J, Saiki I, et al. Morphine analgesia suppresses tumor growth and metastasis in a mouse model of cancer pain produced by orthotopic tumor inoculation. Eur J Pharmacol. 2002;441:185–91. doi: 10.1016/s0014-2999(02)01450-4. [DOI] [PubMed] [Google Scholar]
- 21.Cho AR, Kwon JY, Kim KH, Lee HJ, Kim HK, Kim ES, et al. The effects of anesthetics on chronic pain after breast cancer surgery. Anesth Analg. 1013;116:685–93. doi: 10.1213/ANE.0b013e31827ee372. [DOI] [PubMed] [Google Scholar]
- 22.Hogan QH, Prost R, Kulier A, Taylor ML, Liu S, Mark L. Magnetic resonance imaging of cerebrospinal fluid volume and the influence of body habitus and abdominal pressure. Anesthesiology. 1996;84:1341–9. doi: 10.1097/00000542-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Hogan Q. Size of human lower thoracic and lumbosacral nerve roots. Anesthesiology. 1996;85:37–42. doi: 10.1097/00000542-199607000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Imbelloni LE, Pitombo PF, Ganem EM. The incidence of paresthesia and neurologic complications after lower spinal thoracic puncture with cut needle compared to pencil point needle. Study in 300 patients. J Anesth Clin Res. 2010;1:106. [Google Scholar]
- 25.Moen V, Dahlgren N, Irestedt L. Severe neurological complications after central neuraxial blockades in Sweden 1990-1999. Anesthesiology. 2004;101:950–9. doi: 10.1097/00000542-200410000-00021. [DOI] [PubMed] [Google Scholar]
- 26.Hopkinson JM, Samaan AK, Russel IF, Birks RJ, Patrick MR. A comparative multicentre trial of spinal needles for caesarean section. Anaesthesia. 1997;52:1005–11. doi: 10.1111/j.1365-2044.1997.191-az0324.x. [DOI] [PubMed] [Google Scholar]
- 27.Imbelloni LE, Santanna R, Fornasari M, Fialho JC. Laparoscopic cholecystectomy under spinal anesthesia: Comparative study between conventional-dose and low-dose hyperbaric bupivacaine. Local Reg Anesth. 2011;4:41–6. doi: 10.2147/LRA.S19979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pavlin DJ, Rapp SE, Polissar NL, Malmgren JA, Koerschgen M, Keyes H. Factors affecting discharge time in adult outpatients. Anesth Analg. 1998;87:816–26. doi: 10.1097/00000539-199810000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Borgeat A, Ekatodramis G, Schenker C. Postoperative nausea and vomiting in regional anesthesia: A review. Anesthesiology. 2003;98:530–47. doi: 10.1097/00000542-200302000-00036. [DOI] [PubMed] [Google Scholar]
- 30.Bansal P, Saxena KN, Taneja B, Sareen B. A comparative randomized study of paravertebral block versus wound infiltration of bupivacaine in modified radical mastectomy. J Anaesthesiol Clin Pharmacol. 2012;28:76–80. doi: 10.4103/0970-9185.92449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lynch EP, Welch KJ, Carabuena TM, Eberlein TJ. Thoracic epidural anesthesia improves outcome after breast surgery. Ann Surg. 1995;222:663–9. doi: 10.1097/00000658-199511000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kroner K, Knudsen UB, Lundby L, Hvid H. Long-term phantom breast syndrome after mastectomy. Clin J Pain. 1992;8:346–50. doi: 10.1097/00002508-199212000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Yousef GT, Lasheen AE. General anesthesia versus segmental thoracic or conventional lumbar spinal anesthesia for patients undergoing laparoscopic cholecystectomy. Anesth Essays Res. 2012;6:167–73. doi: 10.4103/0259-1162.108302. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]


