Abstract
Context:
Establishing a near perfect surgical field during functional endoscopic sinus surgery (FESS) is essential and even a minor bleeding can severely compromise an already restricted view. So, if controlled hypotension can be provided without compromising the safety of patient by a relatively effortless method, surgical field can be improved greatly.
Aims:
The aim of this study was to compare the hemodynamic changes and surgical conditions during FESS following oral premedication with clonidine and metoprolol.
Settings and Design:
A total of 40 patients undergoing FESS were included in this prospective, randomized controlled study.
Subjects and Methods:
Patients were divided into two equal groups. Group A patients were premedicated with oral clonidine 300 mcg and Group B with oral metoprolol 50 mg, 2 h before surgery. All patients received fentanyl 2 mcg/kg and induced with propofol 2 mg/kg. Intubation was done following vecuronium 1 mg/kg. Anesthesia was maintained with 66% N2O, 33% O2 and 1% isoflurane. The heart rate (HR) and blood pressure (BP) were measured before induction and thereafter every 15 min up to 2 h. The surgeons were asked to estimate the quality of the operative field using a pre-defined category scale with scores 1-5.
Statistical Analysis:
Difference within the groups was analyzed using analysis of variance and post-hoc test was used to test the difference between individual groups. Chi-square test was used to find out the association between categorical variables.
Results:
Comparison of category scale revealed a lower score in Group A up to 60 min. Group B patients showed a statistically lower HR from pre-induction up to 90 min while systolic BP (SBP), diastolic BP (DBP) and mean arterial pressure did not show a significant difference.
Conclusions:
Oral premedication with 300 mcg of clonidine produced a better operative field than oral metoprolol 50 mg during FESS.
Keywords: Functional endoscopic sinus surgery, oral clonidine, oral metoprolol, surgical field
INTRODUCTION
Establishing a near perfect surgical field during functional endoscopic sinus surgery (FESS) is essential. Minor bleeding can severely compromise an already restricted view obtained through rigid intranasal bronchoscope. As with any other surgical procedure, complications are more likely to result when visualization of local anatomy and vital structures are limited. In addition, in situations of poor visibility more tissue damage is likely to occur and this can affect the development of post-operative adhesions and the success or failure of surgery.
The surgical field can be influenced by a number of factors including physical status of patient, concomitant diseases like bleeding disorders and the pre-existing condition of the vascular network. Local measures like using topical and injected vasoconstrictors are not without side effects. Likewise, induced hypotension also has its own drawbacks. But, if controlled hypotension can be provided without compromising the safety of patient by a relatively effortless method, surgical field can be improved greatly. Hence, we aimed to compare the hemodynamic changes and surgical conditions during FESS following oral premedication with clonidine or metoprolol in this study.
SUBJECTS AND METHODS
This prospective, randomized controlled study was conducted after obtaining approval from hospital Ethical Committee and consent from 40 patients undergoing FESS of age 18-60 years. Because of logistical constraints not every eligible patient was approached for enrollment such that the study population represented a convenient sampling of eligible patients. Patients were divided into two equal groups, A and B, by a closed envelop technique. Group A consisted of patients premedicated with oral clonidine 300 μg and Group B with oral metoprolol 50 mg, both 2 h before surgery.
American Society of Anesthesiologists III (ASA III) or higher, hypertensives, asthmatics and patients already on beta blockers or clonidine were excluded.
Anesthetic management was standardized by a study protocol. The primary Anesthesiologist was not explicitly informed that the patient signed consent for the study. The premedication drugs, induction agents and volatile anesthetic agents used for maintenance of anesthesia were the same for all patients.
All patients received oral premedication of diazepam 10 mg and clonidine or metoprolol on the day of surgery 2 h before operation with sips of water. In the operation, theater a large bore intravenous cannula was put under local anesthesia. Patients then received an analgesic, fentanyl 2 mcg/kg and were induced with sleep dose of propofol, usually 2 mg/kg. Vecuronium 0.1 mg/kg was given to facilitate direct laryngoscopy and orotracheal intubation was done with a cuffed tracheal tube.
Patients were mechanically ventilated to maintain an end expiratory carbon dioxide tension of 35 ± 2 mmHg. Anesthesia was maintained with 66% N2O, 33% O2 and 1% isoflurane. All patients received lactated Ringer lactate solution at approximately 10 ml/kg/h during 1st h of anesthesia followed by 5 ml/kg/h until the end of surgery. The heart rate (HR) and blood pressure (BP) were measured non-invasively by an oscillometric device before induction and thereafter every 15 min up to 2 h.
Following induction of anesthesia patients in both groups received a topical application of 4 ml of 2% lignocaine with 1:200,000 adrenaline on well wrung out cotton pledgets to the nasal mucous membrane, applied for 10 min. After removal of the pledgets, the surgeon infiltrated 1 ml of 2% lignocaine with adrenaline (1:200,000) submucosally into the medial infundibular wall. The HR and BP were then monitored. If mean arterial pressure (MAP) decreased to less than 50 mm Hg, ephedrine in increments of 3 mg was given and patient was then removed from the study. All patients were placed in 15° reverse trendelenburg position to improve venous drainage.
The surgeons were asked to estimate the quality of the operative field using a pre-defined category scale with scores 1-5.
Category scale score for assessment of intraoperative surgical field:
Slight bleeding: No suctioning of blood required
Slight bleeding: Occasional suctioning of blood required. Surgical field not threatened
Slight bleeding: Frequent suctioning required. Bleeding threatens surgical field a few seconds after suction is removed
Moderate bleeding: Frequent suctioning required. Bleeding threatens surgical field directly after suction is removed
Severe bleeding: Constant suctioning required. Bleeding appears faster than can be removed by suction. Surgical field severely threatened and surgery not possible.
Data was analyzed using Statistical Product and Service solutions version 11.0. Descriptive statistical tools such as mean was used to represent the continuous data and percentage used to represent categorical data. Difference within the groups was analyzed using analysis of variance and post-hoc test was used to test the difference between individual groups. Chi-square test was used to find out the association between categorical variables. In all cases, the level of statistical significance (P < 0.05).
RESULTS
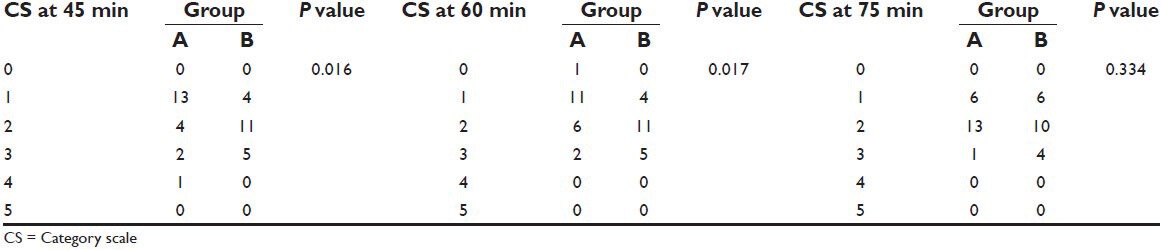
Distribution of patients in both groups was similar with respect to demographics, sex and ASA distribution. Comparison of category scale between groups at pre-induction revealed no difference between groups with a P value of 0.95. While comparing the category scale at 15 min there was a significant difference between groups (P = 0.032) with the majority of Group A patients manifesting a lower category scale. Same observation was made at 30, 45 and 60 min. However, there was a no significant difference between groups thereafter, i.e. at 75, 90, 105 and 120 min [Tables 1–3].
Table 1.
Comparison of category scale at pre-induction, 15 and 30 min
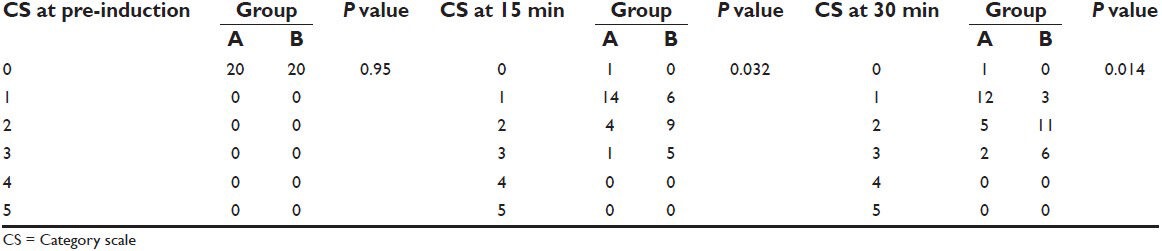
Table 3.
Comparison of category scale at 90, 105 and 120 min
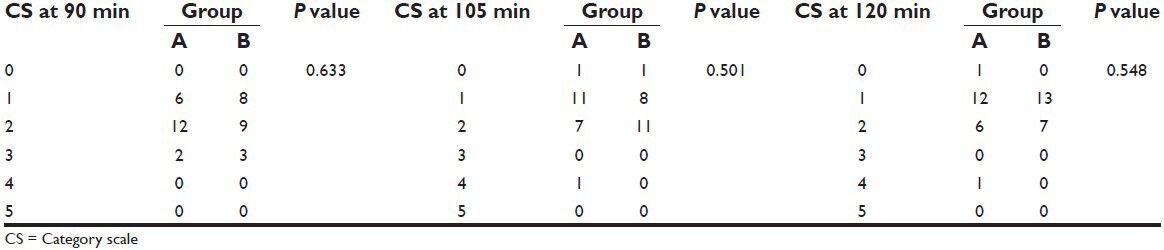
Table 2.
Comparison of category scale at 45, 60 and 75 min
While comparing HRs among groups, there was a significant difference between groups at pre-induction, 15, 30, 45, 60, 75 and 90 min (P < 0.05) with Group B patients showing a statistically lower HR. There was no significant difference between groups at 105 and 120 min (P > 0.05) [Table 4, Figure 1].
Table 4.
Comparison of mean HR
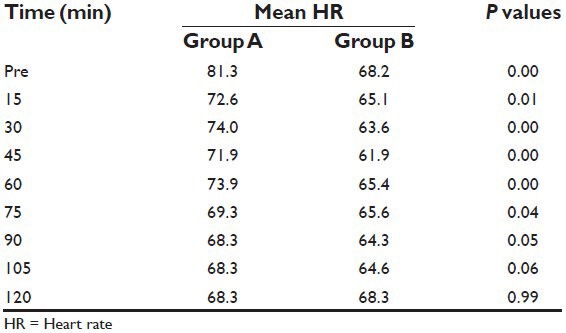
Figure 1.
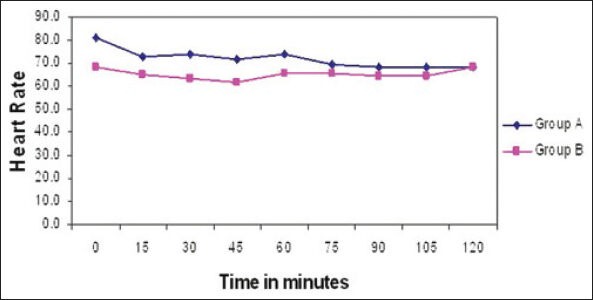
Changes in mean heart rates among groups
When SBP was compared between groups, there was a significant difference between groups at pre-induction and at 120 min (P = 0.01) with Group B patients showing a statistically higher SBP. There was no significant difference between groups at 15, 30, 45, 60, 75, 90 and 105 min (P > 0.05) [Table 5, Figure 2].
Table 5.
Comparison of mean systolic BP
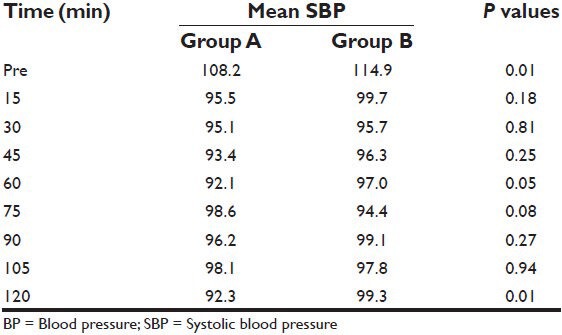
Figure 2.
Changes in mean systolic BP among groups
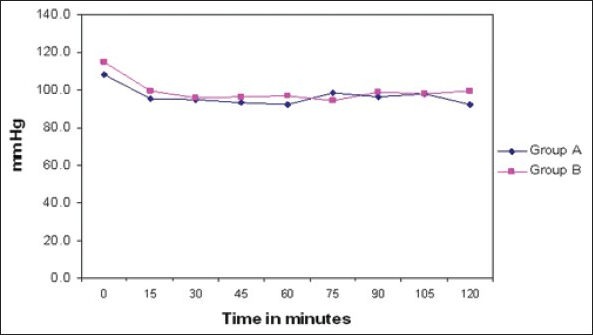
When DBP was compared between groups, there was a significant difference between groups at 30 and at 60 min (P value 0.00 and 0.01 respectively) with Group B patients showing a statistically lower DBP. There was no significant difference between groups at pre-induction, 15, 45, 75, 90, 105 and 120 min (P values more than 0.05) [Table 6, Figure 3]. When MAP was compared between the groups, there was a significant difference between groups at 30 min (P = 0.01) and at 75 min (P = 0.04) with Group B patients showing a statistically lower MAP [Table 7, Figure 4].
Table 6.
Comparison of mean diastolic BP
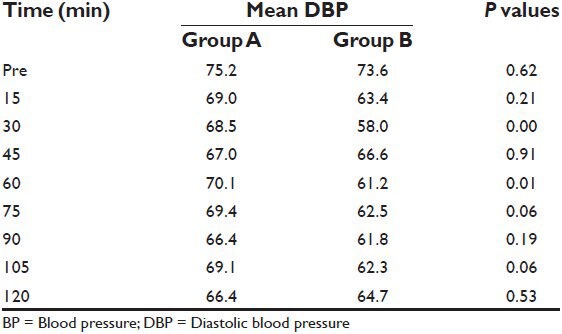
Figure 3.
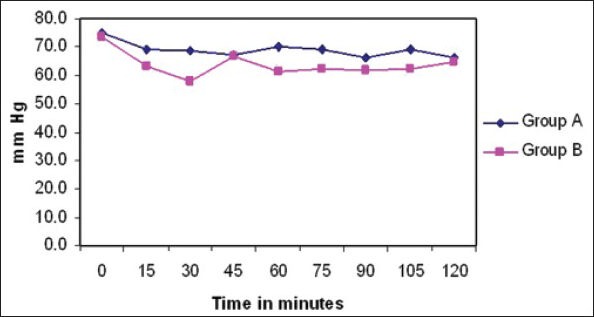
Changes in mean diastolic BP among groups
Table 7.
Comparison of mean MAP
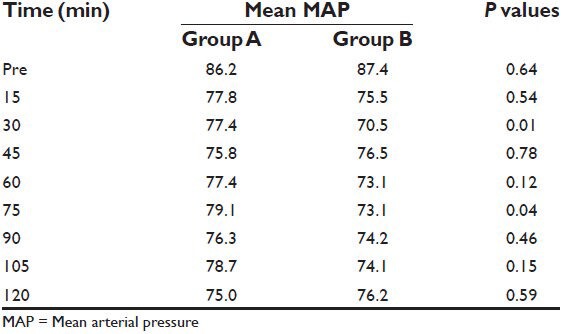
Figure 4.
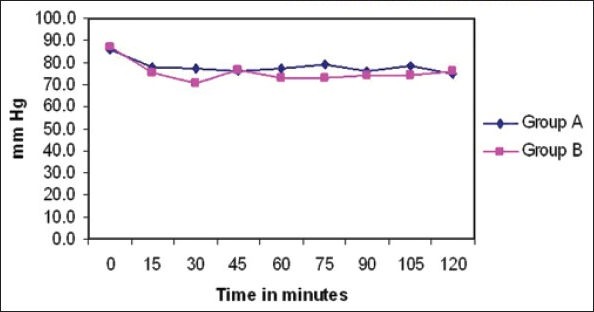
Changes in mean arterial pressures among groups
DISCUSSION
There were many previous studies comparing effects of various hypotensive agents on the surgical field during endoscopic sinus surgery,[1,2,3] but there is no direct comparison between the effects of clonidine and metoprolol as hypotensive agents in FESS. So in this study, we compared the effects of these two drugs. The effect of clonidine given as an oral pre-anesthetic medication in producing a bloodless surgical field in patients undergoing middle ear surgery was examined by Marchal et al.[4] and the patients received clonidine (300 mcg/oral) 90 min prior to surgery. So, in the present study also we decided to use the same dose of clonidine orally.
It has been postulated that reduction of MAP during general anesthesia (GA) can minimize intraoperative bleeding.[5,6] But regarding hemodynamic variables, not only MAP, but also venous pressure and capillary blood flow account for the extent of surgical bleeding. Of these variables, only arterial pressure is easily and readily measured. However studies[7] have demonstrated that MAP and total blood loss are not necessarily correlated. Improved surgical field during FESS with a beta blocker has been attributed to vasoconstriction of the mucous membrane arterioles and pre-capillary sphincters resulting from unopposed alpha adrenergic effects of endogenous catecholamines[8] and solely on the effect of MAP.
In the study by Nair et al.[7] they found a correlation with HR and surgical field grade as there was a better surgical field with a reduction in HR. The metoprolol group had a significantly lower HR than the placebo group.
In our study, there was a statistically different HR in the beta blocker group, but it did not correspond to an improved category scale. None of the patients in either group had significant hypotension. Mild degrees of hypotension occurred in two patients, which responded to intravenous fluid administration. None of the patients in both groups had blood loss necessitating blood transfusion intraoperatively or post-operatively.
Limitations of the study
The grading system employed in our study was on broad guidelines that might have been insensitive to finer surgical field qualities. Operator differences existed as many surgeons were involved in these cases. Interobserver variability was also a limitation as a number of operators were involved.
CONCLUSION
Oral premedication with 300 mcg of clonidine 2 h before surgery produced a better operative field than oral metoprolol 50 mg given at the same time prior to surgery for FESS.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Shams T, El Bahnasawe NS, Abu-Samra M, El-Masry R. Induced hypotension for functional endoscopic sinus surgery: A comparative study of dexmedetomidine versus esmolol. Saudi J Anaesth. 2013;7:175–18. doi: 10.4103/1658-354X.114073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmed HM, Mohamed AA, Abo-Zaid EH. Efficacy of controlled hypotension during microsurgery of the middle ear: Comparative study between esmolol and prostaglandin-E1. Egypt J of Anesth. 2003;19:25–31. [Google Scholar]
- 3.Mengistu AM, Wolf MW, Boldt J, Röhm KD, Suttner SW, Piper SN. Influence of controlled hypotension using esmolol and sodium nitroprusside on natriuretic peptides in patients undergoing endonasal sinus surgery. European Journal of Anaesthesiology. 2007;24:529–34. doi: 10.1017/S0265021506002286. 3. [DOI] [PubMed] [Google Scholar]
- 4.Marchal JM, Gómez-Luque A, Martos-Crespo F, De La Cuesta Sánchez F, Martínez-López MC, Delgado-Martinez AD. Clonidine decreases intraoperative bleeding in middle ear microsurgery. Acta Anaesthesiol Scand. 2001;45:627–33. doi: 10.1034/j.1399-6576.2001.045005627.x. [DOI] [PubMed] [Google Scholar]
- 5.Jabalameli M, Hashemi SM, Soltani HA, Hashemi SJ. Oral clonidine premedication decreases intra operative bleeding in patients undergoing endoscopic sinus surgery. J Res Med Sci. 2005;10:25–30. [Google Scholar]
- 6.Blau WS, Kafer ER, Anderson JA. Esmolol is more effective than sodium nitroprusside in reducing blood loss during orthognathic surgery. Anesth Analg. 1992;75:172–8. doi: 10.1213/00000539-199208000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Nair S, Collins M, Hung P, Rees G, Close D, Wormald PJ. The effect of beta-blocker premedication on the surgical field during endoscopic sinus surgery. Laryngoscope. 2004;114:1042–6. doi: 10.1097/00005537-200406000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Boezaart AP, van der Merwe J, Coetzee A. Comparison of sodium nitroprusside- and esmolol-induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth. 1995;42:373–6. doi: 10.1007/BF03015479. [DOI] [PubMed] [Google Scholar]


