Abstract
Subarachnoid block with local anaesthetic agent and opiod as an adjuvant is a well-known technique with a good record of safety. However, some rare neurological complications like aphonia, dysphagia and tingling sensation have been reported following their administration in pregnant females posted for labour analgesia or caesarean section. We report a case of transient aphonia, aphagia and facial tingling following intrathecal administration of bupivacaine along with fentanyl for lower limb wound debridement in a male patient.
Keywords: Aphagia, facial tingling, intrathecal fentanyl, transient aphonia
INTRODUCTION
Intrathecal opiods like fentanyl are increasingly being used as a safe adjuvant in spinal anesthesia. However some rare neurological complications such as aphonia, aphagia and abnormal facial sensations have been reported following their administration and can alarm the anesthesiologist and the patient.[1,2,3] Herein, we report a case of aphonia, aphagia and tingling sensation of face after intrathecal administration of fentanyl with bupivacaine for lower limb wound debridement. Although transient in nature, this rare complication can alarm the anesthesiologist and the patient.
CASE REPORT
This was a case report of a 35-year-old, 168 cm, 54 kg male patient who was admitted to the emergency department with a history of motor vehicle accident leading to degloving injury of his left lower limb. He did not have a past history of any drug allergy or prior exposure to anesthesia. He was taken to the operating room (OR) for debridement of his lower limb wound under spinal anesthesia. Surgery lasted for 1 h; the course was uneventful and he was shifted to ward. Two days later, he was again posted for wound debridement and flap cover.
On arrival in the OR, standard monitoring was initiated and oxygen @ 4l/min was administered by mask. His blood pressure (BP) was 129/84 mmHg, pulse 82/min and respiratory rate (RR) 14/min. Ringer lactate (1000 ml) was infused intravenously before administration of block. Subarachnoid block was given in sitting position with midline approach at L3-4 interspace in the first attempt. After establishing free flow of cerebro-spinal fluid (CSF), bupivacaine 12.5 mg (2.5 ml of 0.5% hyperbaric bupivacaine) with fentanyl 25 mcg was injected into the subarachnoid space. Immediately after spinal anesthesia, his pulse rate was 88/min, BP 134/90 mmHg, RR 18/min and oxygen saturation (SpO2) was 99%. However, 3 min after the subarachnoid block it was noticed that the patient was unable to talk and swallow. The patient was anxious and was complaining of breathlessness. Bag and mask ventilation with 100% oxygen was initiated. At 5 min, his vital parameters remained stable and sensory block to pin prick was at the level of T10. Oxygen was administered with simple oxygen mask @ 6l/min and the surgeons were allowed to proceed with surgery. There were no signs of motor blockade in upper extremities and the patient was able to move his upper limbs completely with a firm hand grip. Although anxious, he was completely awake, alert and was able to follow commands. The patient was reassured and did not require any treatment. He regained the ability to talk and swallow in 10-15 min after the onset of symptoms. On further enquiry, the patient complained that he also had a tingling sensation over the face which got relieved along with the return of speech. Level of sensory block was reassessed and found to be fixed at T10. Rest of the surgery was uneventful.
Post-operatively, the patient was monitored in the recovery room until complete reversal of motor blockade. 12 lead electrocardiography (ECG) was done which was normal. Neurological examination did not reveal any abnormality. After shifting the patient to ward magnetic resonance imaging (MRI), ultrasound Doppler of the lower leg veins, carotid artery Doppler, transthoracic echocardiography and electroencephalography (EEG) were done which revealed normal findings.
DISCUSSION
Transient neurologic symptoms after spinal anesthesia have been described in the literature. However, transient aphonia and aphagia are rare complications after intrathecal administration of fentanyl with bupivacaine. The possible differential diagnosis of these clinical symptoms could be: (1) High spinal anesthesia (2) Transient ischemic attack (TIA) (3) Conversion disorder and (4) Absence seizures. High spinal anesthesia could easily be ruled out in our patient as he was completely awake, hemodynamically stable and maintaining normal oxygen saturation throughout the episode with sensory level of block fixed at T10. As per 2009 guidelines from the American Heart Association and American Stroke Association, TIA is defined as “a transient episode of neurologic dysfunction caused by focal brain, spinal cord or retinal ischemia, without acute infarction”.[4] It may lead to temporary loss of vision, aphasia, hemiparesis and paresthesia usually on one side of the body. Our patient did not have any features of TIA and ultrasound Doppler of the lower leg veins for deep vein thrombosis and carotid artery Doppler for arterial embolus were normal ruling out the possibility of any thrombo-embolic episode. Furthermore, trans-thoracic echocardiography and ECG of the patient were also normal, which ruled out atrial fibrillation. MRI of the patient was normal suggesting against any acute ischemic lesion. Conversion disorder can present with symptoms such as aphonia, numbness, blindness, paralysis, difficulty swallowing or fits, but was unlikely in our patient as there was no such past history.[5] Absence seizures could also be ruled out in view of no similar past history and normal EEG.[6]
Review of literature to explain such phenomenon revealed some unusual findings following intrathecal administration of fentanyl and have been summarized in Table 1.
Table 1.
Comparison with the findings of other authors
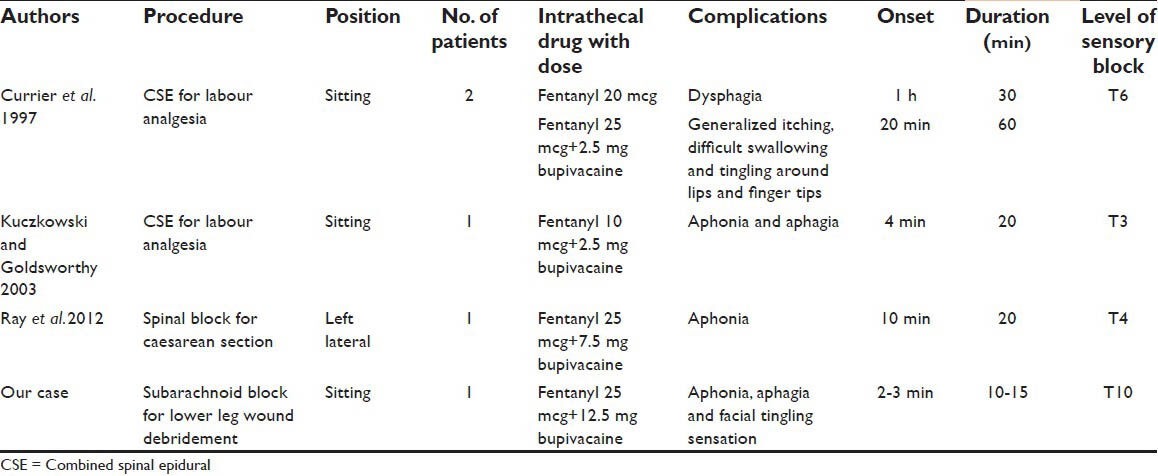
In an article in 1997, Currier et al.[1] reported their experience with two cases who received intrathecal fentanyl as a part of combined spinal epidural (CSE) technique for labor analgesia in a sitting position. The first patient experienced dysphagia 1 h after receiving 20 mcg of fentanyl intrathecally, which got resolved in 30 min. The second patient experienced generalized itching, difficulty in swallowing and tingling sensation around lips and finger tips 20 min after receiving 25 mcg of intrathecal fentanyl combined with 2.5 mg bupivacaine which got resolved in 60 min. In 2003, Kuczkowski and Goldsworthy[2] reported a case of a previously healthy parturient who received 10 mcg of fentanyl combined with 2.5 mg of bupivacaine intrathecally at L2-3 interspace as a part of CSE technique for labor analgesia in a sitting position. At 4 min after intrathecal injection she suddenly developed transient aphonia and aphagia. The pinprick sensory level of analgesia was found to be at T3 and her symptoms got resolved in 20 min.
In 2012, Ray et al.[3] reported a case of a pregnant female posted for caesarean section under subarachnoid block. She received 25 mcg of fentanyl combined with 7.5 mg of bupivacaine intrathecally at L2-3 interspace in left lateral position. At 10 min after block the patient complained of weakness of voice and tingling sensation of face followed by complete aphonia. Level of sensory block was found to be fixed at T4. Her symptoms got resolved in 20 min.
In the previous reported cases, all the patients were pregnant females whereas our patient was a male with degloving injury of lower limb posted for debridement. In all cases the authors believe extensive cephalad spread of fentanyl through the CSF as the cause for neurological symptoms.[1,2,3] The study by Gourlay et al.[7] have noted rapid cephalad spread of fentanyl in the cervical CSF after lumbar administration. Sudden onset, life-threatening respiratory depression have been reported following administration of intrathecal fentanyl for labor analgesia.[8] These findings suggest that lipophilic opioids may move rapidly from lumbar cistern to brainstem level via CSF.[9] Rapid clearance of fentanyl from the CSF might explain the transient nature of symptoms.[1] Baricity of drug and position of the patient at the time of block plays a major role in determining the extent of cephalad spread of drug.[10] Administration of a hyperbaric solution in a patient in sitting position results in a more restricted block.[10] However, higher level of sensory block was found when bupivacaine and fentanyl were administered intrathecally in a sitting position when compared to lateral position.[11] In an in vitro study by Parlow et al.[12] a decrease in the baricity of the mixture was found by the addition of fentanyl to isobaric bupivacaine, but the effect on baricity by the addition of fentanyl to hyperbaric bupivacaine has not been studied until now to the best of our knowledge. On sharing our experience with other anesthetists it was interesting to know that although only few cases have been reported in the literature; there were many more such incidents but were diagnosed as hysterical event! Multicentric trials should be conducted to know the actual incidence of this rare complication.
To summarize, transient neurological complications such as aphonia, aphagia and facial tingling have been reported following intrathecal administration of fentanyl in pregnant females. Our case report adds to the fact that this complication is not limited to pregnant females only but can also occur in males. Hence, one should be vigilant for these findings while administering intrathecal fentanyl in every patient irrespective of their gender and physiological condition. Though the possibility of high spinal anesthesia or any thrombo-embolic episode should always be ruled out, but one should not panic and should reassure the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Currier DS, Levin KR, Campbell C. Dysphagia with intrathecal fentanyl. Anesthesiology. 1997;87:1570–1. doi: 10.1097/00000542-199712000-00037. [DOI] [PubMed] [Google Scholar]
- 2.Kuczkowski KM, Goldsworthy M. Transient aphonia and aphagia in a parturient after induction of combined spinal-epidural labor analgesia with subarachnoid fentanyl and bupivacaine. Acta Anaesthesiol Belg. 2003;54:165–6. [PubMed] [Google Scholar]
- 3.Ray BR, Baidya DK, Gregory DM, Sunder R. Intraoperative neurological event during cesarean section under spinal anesthesia with fentanyl and bupivacaine: Case report and review of literature. J Anaesthesiol Clin Pharmacol. 2012;28:374–7. doi: 10.4103/0970-9185.98349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, et al. Definition and evaluation of transient ischemic attack: A scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276–93. doi: 10.1161/STROKEAHA.108.192218. [DOI] [PubMed] [Google Scholar]
- 5.Ng KO, Lee JF, Mui WC. Aphonia induced by conversion disorder during a Cesarean section. Acta Anaesthesiol Taiwan. 2012;50:138–41. doi: 10.1016/j.aat.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Hughes JR. Absence seizures: A review of recent reports with new concepts. Epilepsy Behav. 2009;15:404–12. doi: 10.1016/j.yebeh.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Gourlay GK, Murphy TM, Plummer JL, Kowalski SR, Cherry DA, Cousins MJ. Pharmacokinetics of fentanyl in lumbar and cervical CSF following lumbar epidural and intravenous administration. Pain. 1989;38:253–9. doi: 10.1016/0304-3959(89)90210-8. [DOI] [PubMed] [Google Scholar]
- 8.Kuczkowski KM. Respiratory arrest in a parturient following intrathecal administration of fentanyl and bupivacaine as part of a combined spinal-epidural analgesia for labour. Anaesthesia. 2002;57:939–40. doi: 10.1046/j.1365-2044.2002.279317.x. [DOI] [PubMed] [Google Scholar]
- 9.Saxena AK, Arava SK. Current concepts in neuraxial administration of opioids and non-opioids: An overview and future perspectives. Indian J Anaesth. 2004;48:13–24. [Google Scholar]
- 10.Hocking G, Wildsmith JA. Intrathecal drug spread. Br J Anaesth. 2004;93:568–78. doi: 10.1093/bja/aeh204. [DOI] [PubMed] [Google Scholar]
- 11.Richardson MG, Thakur R, Abramowicz JS, Wissler RN. Maternal posture influences the extent of sensory block produced by intrathecal dextrose-free bupivacaine with fentanyl for labor analgesia. Anesth Analg. 1996;83:1229–33. doi: 10.1097/00000539-199612000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Parlow JL, Money P, Chan PS, Raymond J, Milne B. Addition of opioids alters the density and spread of intrathecal local anesthetics? An in vitrostudy. Can J Anaesth. 1999;46:66–70. doi: 10.1007/BF03012518. [DOI] [PubMed] [Google Scholar]


