Abstract
Context:
Medical guidelines advise perioperative continuation many antihypertensives, but discontinuing angiotensin antagonists before surgery.
Aims:
This study is aimed to determine the effect of preoperative discontinuation of angiotensin-converting enzyme inhibitors (ACEI) or angiotensin II receptor antagonists (ARA) on intra-operative blood pressure after induction of general anesthesia.
Settings and Design:
The study was a randomized, prospective and double blinded one done in 60 hypertensive patients, receiving these drugs.
Materials and Methods:
Patients were randomized into two equal groups. In Group A, ACEI or angiotensin II receptor antagonist was stopped the day before surgery, but in Group B it was continued. Anesthetic management was standardized by a study protocol. Systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP) were measured just before induction and after induction at 1 min, 3, 5, 10, 15, 30, 45 and 60 min.
Statistical Analysis:
Difference between means and difference between two proportions was analyzed using Normal test for means and corresponding P values were calculated.
Results:
Pre-induction SBP, DBP and MAP were comparable between groups. However when the pre-induction values were compared with subsequent readings at 3, 5, 10, 15, 30, 45 and 60 min, it was found that there was a significant reduction in SBP, DBP and MAP in Group B up to 60 min.
Conclusions:
Intraoperative hemodynamics can be safely managed when ACEI or ARA are withheld on the day of surgery.
Keywords: Angiotensin II receptor antagonists, angiotensin-converting enzyme inhibitors, general anesthesia, hypotension
INTRODUCTION
Medical guidelines advise perioperative continuation of therapies that have a potential for myocardial protection such as beta blockers, calcium channel blockers, alpha 2 agonists,[1,2,3,4] at the same time discontinuing angiotensin-converting enzyme inhibitors (ACEI) or angiotensin II receptor antagonists (ARA) on the morning of surgery. Hence, the present study was conducted to determine the effect of pre-operative discontinuation of ACEI or ARA therapy on intraoperative blood pressure (BP) in surgical patients after induction of general anesthesia (GA).
MATERIALS AND METHODS
The study was conducted from August 2008 to July 2012, after obtaining approval from the hospital ethical committee and consent from the patients. The type of study was randomized, prospective and double blinded.
A total of 60 patients who were aged between 40 and 60 years, belonging to ASA grade II and III, receiving only ACEI or ARA for control of hypertension for at least 3 months with preoperative BP at the time of admission ≤140/90 mmHg.
Patients were randomized by sealed envelope technique into two equal groups, Group A and Group B. Group A consisted of 30 patients whose ACEI or ARA drug was stopped the day before surgery. Group B consisted of 30 patients whose ACEI or ARA drug was continued on the day of surgery. Patients with valvular and ischemic heart diseases, cardiac failure, carcinoid tumors, pheochromocytoma or thyrotoxicosis were excluded.
Anesthetic management was standardized by a study protocol. The pre medication drugs, induction agents, analgesics, muscle relaxants and volatile anesthetic agents used for maintenance of anesthesia were the same for all patients. In the operation theatre a large bore intravenous (IV) cannula was put under local anesthesia. Midazolam 0.02 mg/kg and fentanyl 2.0 μg/kg were given IV slowly. A crystalloid infusion 10 ml/kg was given to all patients before induction followed by 5 ml/kg/h until the end of surgery.
All patients were induced with propofol 2.0 mg/kg followed by vecuronium 0.1 mg/kg and were ventilated with 60% of oxygen, 40% of nitrous oxide and 1% of isoflurane. At the end of 3 min, a quick and gentle laryngoscopy and tracheal intubation were done. Throughout the surgical procedure anesthesia was maintained with the combination of oxygen, nitrous oxide and isoflurane with controlled ventilation maintaining normocapnia and normoxia with oxygen saturation ≥98%. Intraoperative monitoring included continuous electrocardiogram, noninvasive BP monitoring by an oscillometric device, respiratory gas monitoring and pulseoxymetry.
Systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressures (MAP) were measured just before induction and after induction at 1, 3, 5, 10, 15, 30, 45 and 60 min. Intraoperative hypotension was defined as SBP <85 mmHg and hypertension as SBP >140 mmHg.
Hypotension was treated initially with increasing the infusion rate of IV crystalloids, giving a maximum of up to 1000 ml. Whenever MAP was <60 mmHg, hypotension was treated with IV ephedrine in incremental bolus doses of 6 mg. Those patients who received ephedrine were expelled from the study as further BP readings could be affected by the use of ephedrine.
Data was analyzed using SPSS 11.0 software. Difference between means was analyzed using Normal test for means and corresponding P values were also calculated. Normal test for significant difference between two proportions were also used for analysis and the level of statistical significance P < 0.05.
RESULTS
The group comparison demonstrated no significant difference in distribution among two groups with regard to distribution of age, sex, ASA physical status, antihypertensive drugs (ACEI and ARA) and operative procedures.
When pre-induction SBP, DBP and MAP were compared between groups at 1 min there was no significant change in both groups. However when pre-induction SBP, DBP and MAP were compared with subsequent readings at 3, 5, 10, 15, 30, 45 and 60 min it was found that Group A and Group B were significantly different. There was a significant reduction in SBP, DBP and MAP in Group B at 3, 5, 10, 15, 30, 45 and 60 min (P < 0.01, P < 0.05, P < 0.01 respectively) [Tables 1-3 and Figures 1-3].
Table 1.
Comparison of mean and SD of difference between pre-induction SBP and SBP values at various time intervals
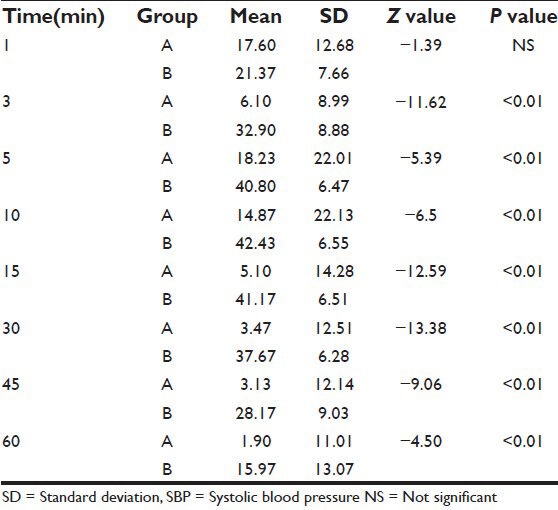
Table 3.
Comparison of mean and SD of difference between pre-induction MAP and MAP values at various time intervals
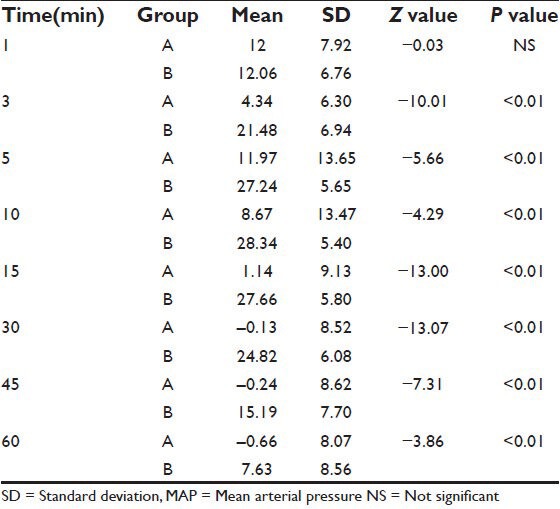
Figure 1.
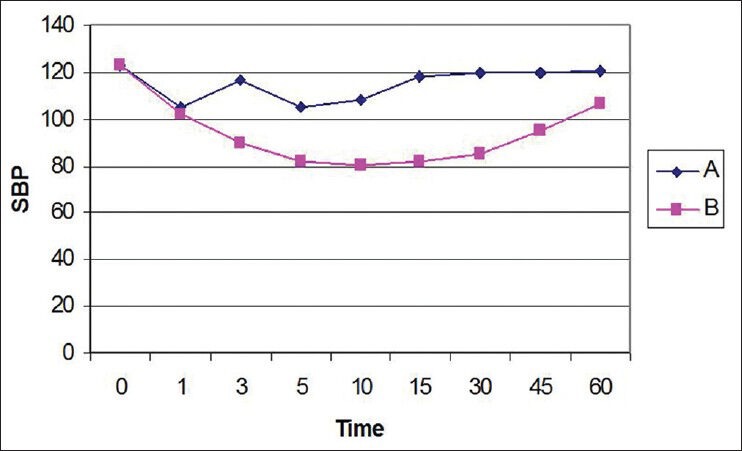
Changes in systolic blood pressure in both groups
Figure 3.
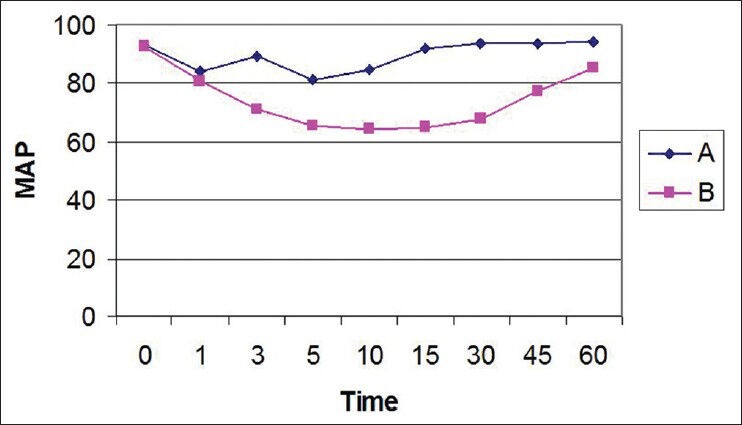
Changes in mean arterial pressure in both groups
Table 2.
Comparison of mean and SD of difference between pre-induction DBP and DBP values at various time intervals
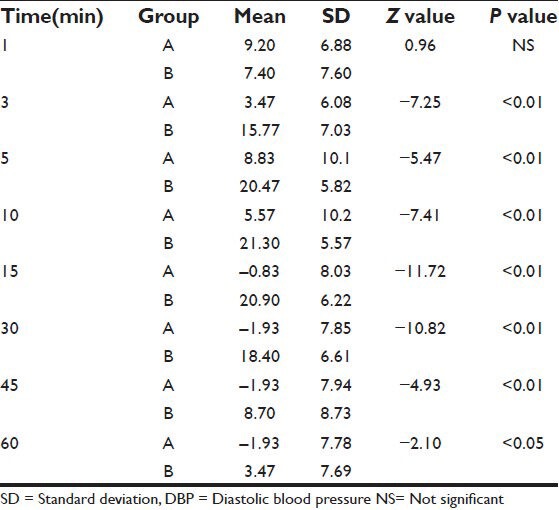
Figure 2.
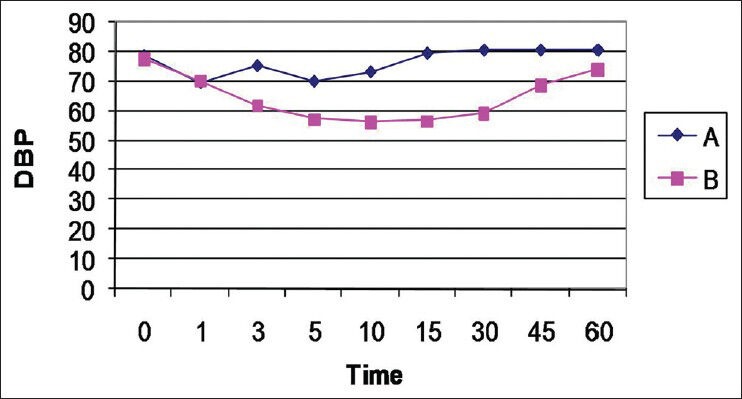
Changes in diastolic blood pressure in both groups
DISCUSSION
The present study was in agreement with several studies in the past, which all had reported intraoperative hypotension with the use of ACEI and ARA in the surgical setting.[5,6,7,8,9,10,11] In the present study, we defined hypotension as SBP ≤85 mmHg, based on the previous study by Comfere et al.[6] However, the patient safety was not compromised as hypotension lasting for >1 min and/or MAP <60 mmHg was promptly treated.
In the study by Comfere et al.,[6] it was reported that hypotension occurred in about 60% of patients who had last ACEI or ARA therapy less than 10 h prior to anesthetic induction. But in the present study, hypotension occurred much more frequently with almost all patients developing hypotension who had ACEI or ARA on the day of surgery. The difference could be due to the fact that in the study by Comfere et al.,[6] various induction agents were used like thiopentone and propofol. In the present study only propofol was used as an induction agent, which could have caused more frequent hypotensive episodes. Malgorzata et al.[12] who also found more profound hypotension with propofol induction when compared with etomidate induction in patients who had received ACEI.
In the study by Bertrand et al.[9] statistically significant reduction in SBP was seen during the initial 5-23 min time interval only. But we found that significant hypotension persisted even at the end of 60 min in Group B, though clinically BP had returned to normal levels by that time. This could be because in the study by Bertrand et al.,[9] hypotension was corrected by vasopressors, which might have influenced further BP readings so that significant hypotension was observed only initially. In the present study to correct a fall in MAP up to 60 mmHg only IV fluids was used and those who needed vasopressors were expelled from the study. However it could be said that in the present study, there was no influence of vasopressors on subsequent BP readings after their use. Omeed et al.[7] had also observed significant hypotension not only during the induction of anesthesia, but throughout the entire anesthetic period.
We were able to maintain MAP above 60 mm of Hg with IV fluids in most of the patients who received ACEI or ARA on the day of surgery, which was in agreement with observations made by Tohmo and Karanko.[13] They stated that intraoperative hypotension in these patients was related to improper fluid balance due to pre-operative fasting and had recommended that proper IV volume status should be ensured. Similarly Colson et al.[14] attained rapid restoration of arterial BP with the IV lactated ringer solution in these patients. Toraman et al.[15] also reported an association between ACEI and an increased need for volume replacement.
In our study, four patients in Group B required ephedrine to maintain MAP above 60 mmHg and were subsequently expelled from the study as per protocol. This was done so as further BP readings could be affected by the use of ephedrine. Four new patients were recruited in Group B in place of the patients who were removed from the study.
One of the main drawbacks of our study was that we did not analyze heart rate. Another drawback was that hypotension was treated with ephedrine as terlipressin, the most effective drug for treating hypotension in ACEI or ARA treated patients, was not available in our institution.
CONCLUSION
As the continuation of ACEI or ARA into the perioperative setting produces undesirable hypotension after induction of GA, it can be concluded that intraoperative hemodynamics can be more safely managed when these agents are withheld on the day of surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mangano DT, Layug EL, Wallace A, Tateo I. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. multicenter study of perioperative ischemia research group. N Engl J Med. 1996;335:1713–20. doi: 10.1056/NEJM199612053352301. [DOI] [PubMed] [Google Scholar]
- 2.Wallace A, Mangano DT. Use of beta-blockade to prevent death after noncardiac surgery. West J Med. 1997;166:203–4. [PMC free article] [PubMed] [Google Scholar]
- 3.Wallace A, Layug B, Tateo I, Li J, Hollenberg M, Browner W, et al. McSPI Research Group. Prophylactic atenolol reduces postoperative myocardial ischemia. Anesthesiology. 1998;88:7–17. doi: 10.1097/00000542-199801000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Stevens RD, Burri H, Tramèr MR. Pharmacologic myocardial protection in patients undergoing noncardiac surgery: A quantitative systematic review. Anesth Analg. 2003;97:623–33. doi: 10.1213/01.ANE.0000074795.68061.16. [DOI] [PubMed] [Google Scholar]
- 5.Coriat P, Richer C, Douraki T, Gomez C, Hendricks K, Giudicelli JF, et al. Influence of chronic angiotensin-converting enzyme inhibition on anesthetic induction. Anesthesiology. 1994;81:299–307. doi: 10.1097/00000542-199408000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Comfere T, Sprung J, Kumar MM, Draper M, Wilson DP, Williams BA, et al. Angiotensin system inhibitors in a general surgical population. Anesth Analg. 2005;100:636–44. doi: 10.1213/01.ANE.0000146521.68059.A1. [DOI] [PubMed] [Google Scholar]
- 7.Khodaparast O, Kheterpal S, Shanks A, Tremper KK. Chronic treatment with ACE inhibitors or ARAs and intra-operative hypotension. Anesthesiology. 2006;105:A44. [Google Scholar]
- 8.Schirmer U, Schürmann W. Preoperative administration of angiotensin-converting enzyme inhibitors. Anaesthesist. 2007;56:557–61. doi: 10.1007/s00101-007-1177-x. [DOI] [PubMed] [Google Scholar]
- 9.Bertrand M, Godet G, Meersschaert K, Brun L, Salcedo E, Coriat P. Should the angiotensin II antagonists be discontinued before surgery? Anesth Analg. 2001;92:26–30. doi: 10.1097/00000539-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Park KW. New therapeutic targets and modalities in cardiovascular medicine. Int Anesthesiol Clin. 2005;43:23–37. [Google Scholar]
- 11.Brabant SM, Bertrand M, Eyraud D, Darmon PL, Coriat P. The hemodynamic effects of anesthetic induction in vascular surgical patients chronically treated with angiotensin II receptor antagonists. Anesth Analg. 1999;89:1388–92. doi: 10.1097/00000539-199912000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Malinowska-Zaprzałka M, Wojewódzka M, Dryl D, Grabowska SZ, Chabielska E. Hemodynamic effect of propofol in enalapril-treated hypertensive patients during induction of general anesthesia. Pharmacol Rep. 2005;57:675–8. [PubMed] [Google Scholar]
- 13.Tohmo H, Karanko M. Angiotensin-converting enzyme inhibitors and anaesthesia. Acta Anaesthesiol Scand. 1996;40:132–3. doi: 10.1111/j.1399-6576.1996.tb04401.x. [DOI] [PubMed] [Google Scholar]
- 14.Colson P, Saussine M, Séguin JR, Cuchet D, Chaptal PA, Roquefeuil B. Hemodynamic effects of anesthesia in patients chronically treated with angiotensin-converting enzyme inhibitors. Anesth Analg. 1992;74:805–8. doi: 10.1213/00000539-199206000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Toraman F, Evrenkaya S, Yuce M, Turek O, Aksoy N, Karabulut H, et al. Highly positive intraoperative fluid balance during cardiac surgery is associated with adverse outcome. Perfusion. 2004;19:85–91. doi: 10.1191/0267659104pf723oa. [DOI] [PubMed] [Google Scholar]


