Abstract
We present a rare case of osseous metaplasia in a poorly healing breast abscess. An 87-year-old woman was referred to the breast surgery clinic with a painful lump in her right breast. Initial imaging and core biopsy suggested a breast abscess. Despite several courses of antibiotics and repeated attempts at aspiration the painful lesion persisted. It was eventually surgically excised in its entirety and final histopathology showed the presence of bone formation within the abscess. The patient's symptoms subsequently resolved. To the best of our knowledge, this is the first case in the literature, of osseous metaplasia within a breast abscess in the absence of malignancy.
Background
In the presence of an abnormal stimulus or pathological stress such as chronic inflammation, cells may change into a different subtype. This process is described as metaplasia. Osseous metaplasia can be defined as the presence of heterotrophic bony tissue within a soft tissue and can be clinically difficult to distinguish from carcinoma1 2 It has been noted to follow soft-tissue tumours, trauma and post-traumatic haematoma.2 However it has not been known to be present within a poorly healing breast abscess. To the best of our knowledge this is the first such case, to be reported in the published literature.
Case presentation
An 87-year-old woman was referred to the breast surgery clinic with a painful lump in her right breast which she had noticed a few weeks prior. She was systemically well and denied feeling unwell or having had a fever.
Her medical history was significant for angina, hypertension, depression and chronic obstructive pulmonary disease (for which she was on home oxygen therapy). Ten years previously she was diagnosed with carcinoma of the right bronchus and was treated with radiotherapy.
She had two children, both of whom she breastfed. She underwent menarche at the age of 12 and menopause at 48 years of age. She has never taken any hormonal contraceptive or replacement therapy. She was a nursing home resident and she had never smoked, but she occasionally drank alcohol.
On examination there were no overlying skin changes of abnormalities on inspection. There were no palpable lesions in the left breast, however there was a tender palpable mass in the superior-medial aspect of her right breast. The rest of the examination was normal.
Investigations
A mammogram and ultrasound was arranged in the clinic. Mammogram did not show any suspicious microcalcification, mass or architectural distortion in either breast. Benign microcalcification was noted bilaterally and was concluded as M2 (benign findings) bilaterally.
Ultrasound investigation confirmed the presence of this lump and described it as a 14 mm hypoechoic nodule with oedema in the surrounding tissues. This was concluded as U4 (suspicious abnormality) and possibly an abscess or carcinoma. Ultrasound scan (USS)-guided aspiration did not yield any fluid, so a core biopsy of the lesion was conducted and the core sample was sent for histopathological analysis.
The patient was seen 1 week later with the result of the core biopsy which showed a partly organising abscess. No malignancy was seen and this was concluded as B2 (benign findings).
Differential diagnosis
The most important diagnosis to bear in mind is breast carcinoma. In light of the reassuring radiological and pathological findings a simple breast abscess is an appropriate diagnosis to secure at this stage.
Treatment
The results were discussed at a multidisciplinary team meeting and it was decided to treat her with antibiotic therapy and to monitor her response. She was seen in the clinic and the lesion was now erythematous and slightly more tender. She was treated with flucloxacillin and penicillin orally with local hygiene for 2 weeks. She was seen in the clinic following this regimen and it was noted that the abscess had responded to antibiotics and was improving. She was prescribed a further course of antibiotics and seen 2 weeks later where the patient explained that the breast lump was now much smaller in size but that she was still have some associated discomfort.
On examination the mass was still palpable in the right breast and the central part of it seemed quite fluctuant. An aspiration was attempted again but this was unsuccessful. In light of the patients history of radiotherapy for lung cancer, the abscess was not deroofed but a further appointment in 1 weeks’ time was arranged to reconsider aspiration repeat USS was performed at this appointment which showed that the appearances had improved and a USS-guided aspiration yielded only two drops of serosanguineous fluid.
When she was seen 2 weeks later it was noted that the skin now appeared normal but the lump had not decreased in size any further and the decision was made to excise it. This was planned to be carried out under local anaesthetic in light of her respiratory problems and due to the lesions close proximity to the overlying skin.
The excision of the right breast infected mass was performed using 20 mL 0.25% bupivacaine and 10 mL 1% lignocaine local anaesthetic. An elliptical incision was used and the specimen was excised and orientated with silk specimens before the wound closed primarily with 3/0 Vicryl subcutaneous and 4/0 Monocryl subcuticular sutures. Antibiotics were continued for a further 10 days at which point she was seen in the outpatient clinic with the results of the histology specimen.
Outcome and follow-up
The sections of the excised breast lesion showed ulcerated skin with an underlying abscess cavity exhibiting acute inflammation surrounded by fibrosis and some scattered multinucleate giant cells. Occasional foci of osseous metaplasia were seen (figure 1). There was no in situ or invasive malignancy. Stains for fungal hyphae or acid-fast bacilli were negative. The features were benign and of active inflammation within which there was bone, likely to be metaplastic. This did not appear to be a metaplastic carcinoma or sarcoma. Although the possibility of dystrophic calcification was considered, the clinical and pathological findings were consistent with the interesting finding of abscess with focal osseous metaplasia. Although an alternative diagnosis would be displacement of bone following an injury, this is unlikely since there was no history of localised trauma. The wound had healed well postoperatively. There was an area of hypergranuation tissue which was treated with silver nitrate and her symptoms had now completely resolved.
Figure 1.
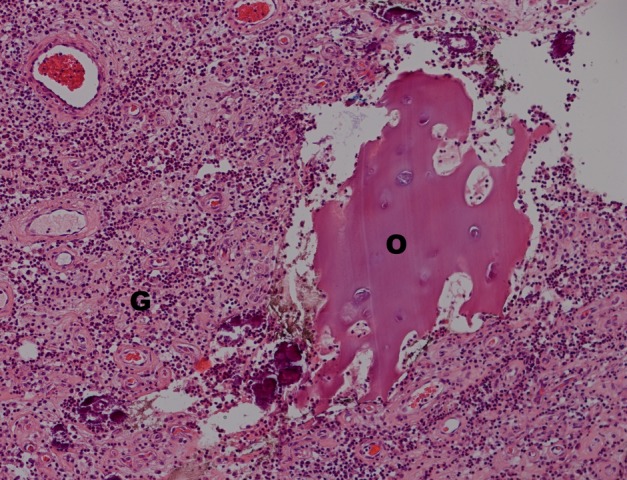
The excised breast abscess, magnification ×10. Granulation tissue (G) with osseous metaplasia (O).
Discussion
The presence of bone within soft tissue has been described since as early as the 18th century.2 3 However, it continues to be a unusual finding, particularly in breast tumours.4 Gal-Gombos et al2 reviewed approximately 200 reported cases in the literature of osseous metaplasia in the presence of breast tumours and noted this to be a rare finding. Spagnolo and Shilkin reviewed 307 cases and reported osseous metaplasia in only four cases. They described the appearance of osseous metaplasia in the context of fibroadenoma, carcinoma, benign mesenchymoma and benign mixed tumour. However, the case presented in this report of the appearance of osseous metaplasia within a breast abscess does not appear in these categories.5
Smith and Taylor also aimed to differentiate the bone containing tumours of the breast into categories, however these again do not include abscess-related osseous metaplasia.6 To our knowledge this is the first case where osseous metaplasia has been reported within a benign breast abscess in the absence of metaplastic changes.
The condition has traditionally been difficult to determine radiologically. Mammogram and ultrasound findings classically show oval, well demarcated lesions with or without dense microcalcifications.7 In malignant tumours, speculated appearances may be apparent.8 However, in this case the lesion was not distinguishable radiologically from the breast abscess. The underlying aetiology of bone formation within this breast abscess is likely to be multifactorial involving several intracellular and inflammatory processes but remains poorly understood.
Learning points.
A breast abscess which is failing to heal with antibiotics and conservative measures should prompt the clinician to consider surgical biopsy for definitive histology and treatment.
Chronic inflammation is a stimulus for metaplastic change which in turn can detrimentally affect the prospects of healing in the absence of intervention.
A low threshold for carcinoma should be held in cases of persistent breast lumps and until excluded by definitive histopathology.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Pontikides N, Botsios D, Kariki E, et al. Extramedullary hemopoiesis in a thyroid nodule with extensive bone metaplasia and mature bone formation. Thyroid 2003;13:877–80 [DOI] [PubMed] [Google Scholar]
- 2.Gal-Gombos EC, Esserman LE, Poniecka AW, et al. Osseous metaplasia of the breast: diagnosis with stereotactic core biopsy. Breast J 2002;8:50–2 [DOI] [PubMed] [Google Scholar]
- 3.Boneti T . De ventris tumore: mammae osseae in virgine cum pectoris hydrope: Lugduno: yons: Cramer et Perachin; 1700.
- 4.Joshi M, Remoundos DD, Ahmed F, et al. An unusual breast lump: osseous metaplasia. BMJ Case Rep 2013;2013:pii:bcr2012008239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spagnolo DV, Shilkin KB. Breast neoplasms containing bone and cartilage. Virchows Arch A Pathol Anat Histopathol 1983;400:287–95 [DOI] [PubMed] [Google Scholar]
- 6.Smith BH, Taylor HB. The occurrence of bone and cartilage in mammary tumors. Am J Clin Pathol 1969;51:610–18 [DOI] [PubMed] [Google Scholar]
- 7.Mertens HH, Langnickel D, Staedtler F. Primary osteogenic sarcoma of the breast. Acta Cytol 1982;26:512–16 [PubMed] [Google Scholar]
- 8.Watt AC, Haggar AM, Krasicky GA. Extraosseous osteogenic sarcoma of the breast: mammographic and pathologic findings. Radiology 1984;150:34. [DOI] [PubMed] [Google Scholar]


