Abstract
Background
Many programmes to detect and prevent cardiovascular disease (CVD) have been performed, but the optimal strategy is not yet clear.
Aim
To present a systematic review of cardiometabolic screening programmes performed among apparently healthy people (not yet known to have CVD, diabetes, or cardiometabolic risk factors) and mixed populations (apparently healthy people and people diagnosed with risk factor or disease) to define the optimal screening strategy.
Design and setting
Systematic review of studies performed in primary care in Western countries.
Method
MEDLINE, Embase, and CINAHL databases were searched for studies screening for increased cardiometabolic risk. Exclusion criteria were studies designed to assess prevalence of risk factors without follow-up or treatment; without involving a GP; when fewer than two risk factors were considered as the primary outcome; and studies constrained to ethnic minorities.
Results
The search strategy yielded 11 445 hits; 26 met the inclusion criteria. Five studies (1995–2012) were conducted in apparently healthy populations: three used a stepwise method. Response rates varied from 24% to 79%. Twenty-one studies (1967–2012) were performed in mixed populations; one used a stepwise method. Response rates varied from 50% to 75%. Prevalence rates could not be compared because of heterogeneity of used thresholds and eligible populations. Observed time trends were a shift from mixed to apparently healthy populations, increasing use of risk scores, and increasing use of stepwise screening methods.
Conclusion
The optimal screening strategy in primary care is likely stepwise, in apparently healthy people, with the use of risk scores. Increasing public awareness and actively involving GPs might facilitate screening efficiency and uptake.
Keywords: cardiometabolic risk factors, primary health care, screening
INTRODUCTION
Cardiovascular diseases (CVD) are the leading causes of death and disability worldwide.1 Early detection and treatment of cardiometabolic risk factors can prevent development of CVD. GPs could play a central role in primary prevention as they are easily accessible to patients. Performing screening in a familiar setting — inside the general practice — is likely to enhance participation.2 In addition, counselling and treatment could easily follow screening, as these are already part of usual care.
Screening programmes can be performed among apparently healthy individuals (not yet known to have CVD, diabetes, or cardiometabolic risk factors) and in mixed populations (including apparently healthy people and people already diagnosed with a risk factor or established disease). Screening entire populations could lead to considerable unnecessary testing, with a fairly low yield, as most people screened will be healthy. Other ways of screening have been advocated, for example, targeted or stepwise screening methods.3 In targeted screening, a presumed high-risk group is considered, for example, people with central (abdominal) obesity. Stepwise methods can be used to identify high-risk groups, thereby limiting the number of people qualifying for further examinations.
Even though many screening programmes have been conducted in primary care over recent decades, no attempt had been made to compare the various approaches and define lessons. In the authors’ opinion, the optimal screening strategy should identify all people with an increased cardiometabolic risk, with a minimum effort to detect these people. Therefore, this study was a systematic review of cardiometabolic screening programmes in a primary care setting. The aim was to define the optimal screening strategy, by focusing on the population in which the screening was performed, the approach taken with patients, the different screening steps, the uptake, and the yield of screening.
METHOD
Criteria for considering studies for this review
In this study, the focus was on screening studies that were aimed at detecting an increased cardiometabolic risk, performed in primary care. Studies were excluded when they assessed only the prevalence of risk factors without further follow-up or treatment; those without involving a GP in the screening process; when fewer than two cardiometabolic risk factors (hypertension, dyslipidaemia, impaired glucose tolerance, diabetes, overweight/obesity) were considered as the primary outcome; and those with study populations constrained to an ethnic minority.
It was assumed that people with established disease or risk factors already receive extensive care through existing pathways, although this probably only applies to countries with a well-established primary care system. Therefore, only studies performed in Western countries were included: European countries, Australia, New Zealand, Canada, and the US.
How this fits in
Screening programmes can identify cardiometabolic risk factors that, when treated, can prevent development of cardiovascular disease. Several strategies, settings, and populations can be eligible. This study defines that the optimal screening strategy in primary care could be a stepwise approach, using, for example, risk scores to select people qualifying for further screening examinations. Increasing public awareness and actively involving GPs may facilitate screening efficiency and uptake.
Search methods
The MEDLINE, Embase, and CINAHL databases were searched for synonyms for primary care, screening, and cardiometabolic risk factors, on 27 January 2013. For the detailed search strategy see Appendix 1 (available from the authors on request). Language was restricted to English.
Data collection and analysis
Two reviewers independently checked all titles and abstracts. Potentially relevant articles were retrieved full-text, and subsequently assessed for inclusion by two reviewers independently. When a full-text article was not available, the author and/or editor was contacted. In cases of disagreement between two reviewers, these were discussed and resolved by the third reviewer.
For included studies, relevant data were extracted using a standardised template. Data were extracted on the screened population, screening method, patient approach, response rates, and yield of screening in terms of detected cardiometabolic risk factors. When more than one article reported on the same study population, the article with the most information on the method was included.
RESULTS
Included studies
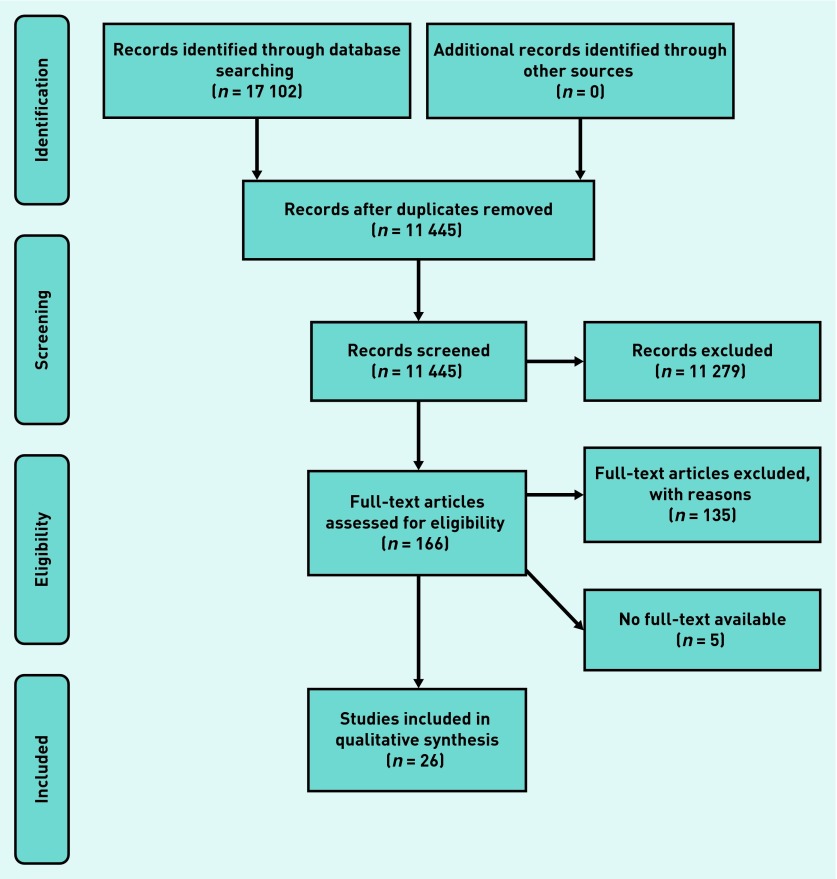
Figure 1 represents the study flow diagram. The search strategy yielded 11 445 hits, of which 26 met the study inclusion criteria. Data on population characteristics, screening method, patient approach, and response rates are listed in Tables 1 (apparently healthy populations) and 2 (mixed populations).
Figure 1.
Review flow diagram.
Table 1.
Overview of included screening initiatives, performed in an apparently healthy population
| Study name | Country | Age, years | Screening method | Approach | Number eligible | Response rate | |
|---|---|---|---|---|---|---|---|
| McMenamin, 199512 | NA | New Zealand | 30–69 | Eligible males were invited by the doctor when attending the surgery to return for a preventive health check | Opportunistic | 361 malesa | 79% |
| Marshall et al, 200811 b | The Sandwell Project | England | 35–74 | For all patients without known CVD and not currently receiving antihypertensive medication, a Framingham risk score calculation was made with data from medical records. Default risk factor values were used for all missing risk factor data. Those with a risk >20% were mailed an appointment to attend a CVD assessment in their practice | Actively invited, stepwise | 11 901; 598 invited for second step | 62% of those invited for risk assessment |
| Van den Donk et al, 200913 | IJSCO | Netherlands | 20–70 | Patients not known to have a diagnosis of CVD, DM, hypertension, or dyslipidaemia received a tape measure mailed to their home and were asked to measure their own WC. Those with an increased WC were invited for further risk assessment | Actively invited, stepwise | 11 862; 2004 invited for second step | 50% measured their own WC; 86% of those with an increased WC underwent all screening examinations |
| Godefrooij et al, 20129 | NA | Netherlands | 40–75 | Patients without a diagnosis of CVD, cerebrovascular disease, DM, hypertension, or dyslipidaemia, were asked to return a questionnaire. Based on this questionnaire a risk score was calculated and patients at risk were invited for further risk assessment | Actively invited, stepwise | 1704 | 75% returned questionnaire; 72% of those invited for further risk assessment attended screening |
| Lambert et al, 201210 | The Deadly Trio Programme | England | ≥40 | Males who were not registered in a disease register for CHD, hypertension, DM, CKD, heart failure, or atrial fibrillation were invited for cardiovascular assessment either by their own GP or an alternative provider | Actively invited | 24 166 males | 24% |
CHD = chronic heart disease. CKD = chronic kidney disease. CVD = cardiovascular disease. DM = diabetes mellitus. NA = not applicable. WC = waist circumference.
In case of an opportunistic approach: the number of eligible people refers to the number of people who attended screening.
Results only represent the intervention group.
The first four studies concerning screening for cardiovascular risk were published between 1967 and 1972.4–7 These were all so-called multiple screening studies: besides cardiovascular risk factors the screening programmes also screened for other diseases like glaucoma, anaemia, or cervical cancer. The first study that focused solely on screening for an increased cardiovascular risk was published in 1978.8
Screening population
Apparently healthy populations
Five studies focused on apparently healthy patients only (Table 1),9–13 including the four most recently published. The number of people eligible for screening ranged from 361 to 24 166. Four studies defined a specific age-category, the lower threshold varying between 20 and 40 years and the upper threshold varying between 69 and 75 years. Only the study by Lambert et al set a minimum age, excluding males <40 years.10
Mixed populations
Twenty-one screening programmes were performed in mixed populations (Table 2).4–7,14–27 The British Family Heart Study reported which part of their study population was not previously diagnosed with coronary heart disease, high blood pressure, high cholesterol, or diabetes. None of the other studies provided any information about the composition of their study population. Most studies included males and females. The number of people eligible for screening ranged from 120 to 40 000. Sixteen studies defined a specific age-category, with lower thresholds from 15 to 45 years and upper thresholds from 50 to 65 years. The remaining studies excluded school children,4,7 or specifically considered older patients.5,26,28
Table 2.
Overview of included screening initiatives, performed in a mixed population: screening methods, patient approach, and response rate
| Study name | Country | Age, years | Screening method | Approach | No. eligible | Response rate | |
|---|---|---|---|---|---|---|---|
| Cope et al, 19674 | NA | England | >15 | All people responding to posters, talks, and other advertising literature that was distributed throughout the practice were screened | Opportunistic | 1711a | 39% |
| Scott et al, 19687 | NA | England | ≥15 | All eligible females in one practice were invited for an examination | Actively invited | 1800 females | 43% |
| Pike, 19695 | NA | England | >68 | All eligible patients were sent a letter to invite them for a series of tests | Actively invited | 671 | 43% |
| Pike, 19726 | NA | England | 45–55 | Eligible males were sent a letter inviting them to attend a morning for examinations and interviews | Actively invited | 309 males | 45% |
| Brown, 19788 | NA | England | 37–43 | All eligible males were sent a letter inviting them to attend for a screening test in the morning | Actively invited | 120 males | 64% |
| Anggard et al, 198616 | NA | England | 20–59 | Patients could attend screening at their own request or were invited during a regular consultation | Opportunistic | 40 000a | Unknown |
| Jones et al, 198823 | NA | England, Wales | 25–55 | All patients were invited for screening and those with any of the risk factors were referred for treatment | Actively invited | 3800 | 62% |
| Mann et al, 198825 | NA | England | 25–59 | Two approaches in different centres: 1. All eligible patients invited; 2. Patients visiting clinic offered a health check consultation | Invited/opportunistic | 12 092a | 73% |
| Bennett et al, 198917 | South Birmingham Coronary Prevention Project | England | 35–65 | People attending the GPs surgery were invited to participate, alternatively invitations were sent by post | Invited/opportunistic | 2261a | Unknown |
| Björkelund et al, 199118 | NA | Sweden | 45–64 | Eligible women were invited for a free health survey | Actively invited | 1084 | 86% |
| OXCHECK Study Group, 199114 | OXCHECK | England | 35–64 | Eligible people were invited for a health check and randomised for participation in the first, second, third, or fourth study year | Actively invited | 11 090 responded to initial questionnaire; 2674 were randomised for participation in the first year | 73% responded to questionnaire, 82% of those invited for first-year screening accepted |
| Hellénius et al, 199322 | NA | Sweden | 15–60 | All eligible people visiting the health centre were offered the opportunity to fill in a short questionnaire. Those with ≥ 1 risk factor (known hypertension, hyperlipidaemia, DM, smoking, overweight, physical inactivity, family history of early CVD or symptoms of angina pectoris or intermittent claudication) were offered a free check-up | Opportunistic, stepwise | 1904 filled in risk questionnaire, 94% were eligible for the second stepb | 6% |
| Family Heart Study Group, 199415 | British Family Heart Study | England, Wales, Scotland | 40–59 | Eligible patients were identified by household through the male partner; families were screened | Actively invited | 4158 males and their families were invited | 57% of the families were represented by one or more member |
| Persson et al, 199432 | Sweden | 33–42 | All eligible males received a postal invitation to a health examination | Actively invited | 757 | 86% | |
| Gran et al,199521 | NA | Sweden | 30–59 | All people living in one primary healthcare centre’s catchment area were invited to participate in a population-based screening programme | Actively invited | 3884 | 68% |
| Lauritzen et al, 199524 | Ebeltoft project | Denmark | 30–50 | Random sample of all inhabitants of Ebeltoft who were registered with one of the study practices received an invitation. Those willing to participate received a questionnaire and were randomised in three groups: one control group and two intervention groups (health check and written feedback with or without consultation of GP) | Actively invited | 2000 were invited; 1370 were willing to participate (control: 465; intervention: 449 and 456) | 69% |
| van den Berg et al, 199926 | NA | Netherlands | ≥60 | All persons registered with one general practice received a letter from their GP offering a cardiovascular health check | Actively invited | 1002 | 80% |
| Weinehall et al, 199927 | Västerbotten Intervention Programme | Sweden | 30–60 | All people aged 30, 40, 50, and 60 years of age were invited annually to a health provider survey focusing on the traditional risk factors for CVD | Actively invited | 2046b | 93% |
| Devroey et al, 200420 | NA | Belgium | 45–64 | All inhabitants of three Belgian towns were invited. An information campaign in the local press had been set up to augment the recruitment | Actively invited | 12 756 | 7% |
| Bunescu et al, 200819 | NA | Romania | 25–65 | Eligible patients were invited for assessment of CVD risk | Actively invited | 1012 | 79% |
| Tiessen et al, 201228 | NA | Netherlands | >50 | Males >50 and females >55 years, without registered DM and not under second-line follow-up by a cardiologist or internist, were invited for assessment of CVD risk by their GP | Actively invited | 521 | 82% responded; 68% participated |
CVD = cardiovascular disease. DM = diabetes mellitus. NA = not applicable.
In case of an opportunistic approach: the number of eligible people refers to the number of people who attended screening.
This is the total number of people invited over 8 consecutive screening years.
Screening method
Apparently healthy populations
Three of the five studies performed in an apparently healthy population used a stepwise approach.9,11,13 Calculation of a risk score based on a questionnaire completed by patients,9 data available in electronic medical records,11 or self-measuring waist circumference,13 were used as first screening steps; subsequently people with scores above a threshold were invited for additional examinations.
Mixed populations
Hellénius et al were the only group to use a stepwise approach in a mixed population. People were asked to fill in a questionnaire about the presence of cardiometabolic and lifestyle risk factors. Those with at least one risk factor were invited for further examinations.22
Patient approach
Apparently healthy populations
Four studies in apparently healthy populations actively invited people to participate in the screening, by a written invitation from their GP,9,11,13 or by either their own GP or an alternative provider.10 One study used an opportunistic approach: eligible males were asked during a regular GP visit to participate in screening.12
Mixed populations
Most studies performed in mixed populations actively invited people. Five studies used a different approach. Two studies asked people to participate in screening during a regular GP visit;22 in one of them people could also attend on their own request.16 Cope et al informed people about the screening through public advertising inside and outside the general practice.4 Two studies combined the active and opportunistic approaches.17,25
Response rate
Apparently healthy populations
Four studies performed among apparently healthy people had response rates between 50% and 79%; if necessary, one or more reminders were sent. One study had a lower response rate of 24%; sending reminders was not reported.10 The age group eligible for screening did not seem to influence the response rate. The study with the highest rate was the only one with an opportunistic approach and lasted for 3 years.12
Mixed populations
Response rates in mixed populations ranged from 6% to 93%. The age group eligible for screening did not seem to influence the response rate. The lowest response rate (6%) was observed by Hellénius et al using a stepwise method and an opportunistic approach.22 Devroey et al reported a rate of 7%; in this study the local authorities invited all inhabitants of three Belgian towns to visit their GP for a health check.20 The highest response rate was found in the Swedish Västerbotten Intervention Programme, in which all people of a specific age were annually invited.27
Yield in terms of cardiometabolic risk
Apparently healthy populations
An overview of the yield of the studies in apparently healthy populations is given in Table 3. Four studies calculated a CVD risk score for participants. The results varied from a 10-year cardiovascular mortality risk ≥10% in 6% of the study population,9 to a 10-year cardiovascular mortality and morbidity risk ≥20% in 20% of the study population.10
Table 3.
Overview of included screening initiatives, performed in an apparently healthy population: yield of screening
|
Risk factors
|
Risk score | ||||
|---|---|---|---|---|---|
| Obesity | Hypertension | Diabetes | Dyslipidaemia | ||
| McMenamin, 199512 | DBP >90: 9% | TC >7.5 mmol/l: 8% | High CHD-risk: 10% Moderate risk: 14% |
||
| Marshall et al, 200811 a | 28% eligible for antihypertensive treatment | 49% eligible for statin | Framingham risk score >20% in first screening step: 9% | ||
| van den Donk et al, 200913 | WC >88/102 cm (females/males): 34% | Metabolic syndrome: 28% of those people with a self-measured WC >88/102 cm | |||
| Godefrooij et al, 20119 | BMI ≥25: 51% | SBP ≥180: 2% | FBG ≥7: 2% | TC ≥8.0 mmol/l: 0.4% LDL ≥5.0 mmol/l: 1% |
SCORE risk function ≥10%: 6% |
| Lambert et al, 201210 | 6% was added to hypertension register; an additional 20% had BP >140 | 3% was added to diabetes register | TC >5 mmol/l: 45% | Framingham risk score ≥20%: 20% | |
BMI = body mass index in kg/m2. BP = blood pressure in mmHg. CHD = coronary heart disease. DBP = diastolic blood pressure in mmHg. FBG = fasting blood glucose in mmol/l. HbA1c = haemoglobin A1c in mmol/l. LDL = Low-density lipoprotein cholesterol. RBG = random blood glucose in mmol/l. SBP = systolic blood pressure in mmHg. TC = total cholesterol. WC = waist circumference.
Results only represent those of the intervention group.
Mixed populations
The yield of the studies performed in mixed populations is presented in Table 4. All but one of the studies measuring obesity (BMI ≥30 kg/m2) report prevalence rates between 10% and 21%. This percentage does not clearly increase in the more recent studies. The yield of diabetes ranged from 1% to 3%. Prevalence of hypercholesterolaemia (total cholesterol ≥6.5 mmol/l) ranged between 24% and 48% for females, and 26% and 46% for males.14,17,21,22,25–27 Seven studies calculated a cardiovascular risk score for participants:15,16,19–21,24,28 five studies reported results.15,19,20,24,28
Table 4.
Overview of included screening initiatives, performed in a mixed population: yield of screening
|
Risk factors
|
Risk score | ||||
|---|---|---|---|---|---|
| Obesity | Hypertension | Diabetes | Dyslipidaemia | ||
| Cope et al, 19674 | DBP >100 or SBP >150: 3% | 0.3% | |||
| Scott et al, 19687 | >10% above ideal weight: 30% | DBP >90: 16% | IFG: 4%; 2 people had DM | TC >260 mg/100 ml: 19% | |
| Pike, 19695 | 6% females and 7% males required advice to reduce their weight | 8 females and 9 males had symptoms that could be associated with hypertension; more had SBP >200, or DBP >120 | Glycosuria: 2% females, 3% males (apart from the known diabetics); one male had DM | ||
| Pike, 19726 | Obesity (estimated by skin-fold calliper and height/weight tables): 31% | DBP >105: 5% | Glycosuria: 0.7% | TC >250 mg/100 ml: 12% | |
| Brown, 19788 | 7% were considered overweight | 0% | TC>6.5 mmol/l or TG>1.7 mmol/l: 20% | ||
| Anggard et al, 198616 | SBP >160: 6% DBP >95: 10% |
TC >7.0 mmol/l: 15% | A risk score was calculated, results not reported | ||
| Jones et al, 198823 | BP >150/90 (<40 years) or >155/95 (≥40 years): 3% | Glycosuria: 2% Proteinuria: 2% |
TC >6.0/6.5 mmol/l (female/male, <30 years) or >6.5/7.1 mmol/l (female/male, ≥30 years):7%; >8.0 mmol/l: 2% | ||
| Mann et al, 198825 | BMI >25: 46% male, 37% female | BP >160/90: 15% male, 10% female | 1% male, 1% female | TC > 5.5 mmol/l: 58% male, 53% female; TC > 6.5 mmol/l: 26% male, 24% female; TC >8.0 mmol/l: 4% male, 4% female | |
| Bennett et al, 198917 | >10% above ideal BMI: 42% | DBP >90 on 3 readings: 18% | TC > 6.5 mmol/l: 27% | ||
| Björkelund et al, 199118 | BMI ≥30: 13% | BP >160/95 (<60 years) or >170/105 (≥ 60 years) or antihypertensive medication: 22% | FBG ≥5.5 or previously diagnosed DM: 2%. Newly detected DM: 0.2% | TC ≥ 9.0 mmol/l (<50 years) or ≥10 mmol/l (≥50 years): 3% | |
| OXCHECK Study Group, 199114 | BMI 25–29: 45% male, 32% female BMI ≥30: 10% male, 16% female |
DBP >90: 14% male, 9% female | TC 6.5–7.9 mmol/l: 30% male, 29% female; TC ≥ 8.0 mmol/l: 8% for male and female | ||
| Hellénius et al, 199322 | BMI ≥30: 17% male, 14% female | DBP ≥90: 33% male, 22% female | Blood glucose ≥6.7: 12% male; 6% female | TC ≥5.2 mmol/l: 68% male, 62% female; TC ≥6.5 mmol/l: 29% male, 27% female; TG ≥2.3 mmol/l: 22% male, 10% female | |
| Family Heart Study Group, 199415 | Total population: BMI 25–29: 49% male, 31% female BMI ≥30: 13% male, 13% female. Apparently healthy population: BMI 25–29: 49% male, 31% female BMI ≥30: 11%, male, 11% female |
Total population: DBP ≥90: 38% male, 23% female. Apparently healthy population: DBP ≥90: 33% male, 18% female |
Total population: RBG ≥7: 12% male, 6% female. Apparently healthy population: RBG ≥7.0: 10% male, 5% female |
Total population: TC ≥6.5 mmol/l: 22% male, 18% female. Apparently healthy population: TC ≥6.5 mmol/l: 19% male, 16% female |
A coronary risk score was calculated; 16% of males and 15% of females without previously diagnosed coronary heart disease or self-reported chest pain on exercise were in the high-risk quintile |
| Persson et al, 199432 | TC 6.5–7.8 mmol/l: 14%TC ≥7.9 mmol/l: 2% | A risk profile was worked out with ‘risk points’ for different risk factors | |||
| Gran et al, 199521 | DBP >90: 33% male, 22% female | TC >6.5 mmol/l: 44% in male, 37% in female | A risk score was calculated but the results cannot be extracted | ||
| Lauritzen et al, 199524 | BMI >30 or BMI 25–29 plus WHR >0.8: 16% | SBP >160 or DBP >90: 10% | FBG >7: 2% | TC >7 mmol/l: 10% | Increased or very high myocardial infarction risk: 11% |
| Van den Berg et al, 199926 | BMI ≥30: 11% | SBP ≥160 or DBP ≥95: 30% Newly: detected 5% hypertension and 10% isolated systolic hypertension | 7%; Newly detected: 2% | TC ≥6.5 mmol/l: 26%; newly detected: 8% | |
| Weinehall et al, 199927 b | SBP ≥160: 30% male, 29% female | TC >6.5 mmol/l: 46% male, 48% female | |||
| Devroey et al, 200420 a | BMI ≥30: 54% male; 39% female | BP >140/90: 75% of those untreated for hypertension | FBG 6.1–6.9: 8%; FBG ≥ 7.0 or previously diagnosed DM: 2% | TC ≥6.5 mmol/l: 20% of those untreated for hypercholesterolaemia | Framingham risk score; ≥10%: 55% male, 44% female |
| Bunescu et al, 200819 | BMI 25–30: 35% BMI ≥30: 21% | BP >140/90 in patients without comorbidity; >130/80 in patients with DM, congestive heart failure or renal insufficiency; >125/75 in patients with proteinuria >1 g/24 hours; or those taking antihypertensive medication: totally 24% | DM: 3% | TC ≥190 mg%: 47%; TC ≥240 mg%: 12% | SCORE risk function <5% without CVD or DM: 60% SCORE risk function ≥ 5% without CHD or DM: 30% SCORE risk function in patients with CHD or DM: 9% |
| Tiessen et al, 201228 | Low risk (SCORE <5%): 60%; aged <65: 78%; aged 50–55 (only males): 92% Intermediate risk (SCORE 5–10% without additional risk factors): 14%. Increased risk (SCORE 5–10% with additional risk factors or ≥10%): 26% | ||||
BMI = body mass index in kg/m2. BP = blood pressure in mmHg. CHD = coronary heart disease. DBP = diastolic blood pressure in mmHg. DM = diabetes mellitus. FBG = fasting blood glucose in mmol/l. IFG = impaired fasting glucose. RBG = random blood glucose in mmol/l. SBP = systolic blood pressure in mmHg. TC = total cholesterol. TG = triclycerides. WHR = waist to hip ratio; years: years.
Only participants without CHD, peripheral arterial disease, and stroke were analysed.
Results were extracted from another publication presenting the prevalence rates of cardiometabolic risk factors for the first 6 years of the Västerbotten Intervention Programme.33
Apparently healthy people versus a mixed population
The British Family Heart Study Group is the only study performed in a mixed population that separately reports results for their apparently healthy subpopulation.15 Of the 2246 males, 1716 were apparently healthy, and of the 1604 females, 1321 were apparently healthy. The prevalence rates were comparable or slightly lower in the apparently healthy population. A diastolic blood pressure ≥90 mmHg was present in 38% and 23% of all males and females, and in 33% and 18% of the apparently healthy males and females, respectively. For a total cholesterol level ≥6.5 mmol/l, the prevalence rates were 22% and 18% for all males and females, and 19% and 16% for the apparently healthy males and females.
DISCUSSION
Summary
To the best of the authors’ knowledge, this is the first systematic review, having systematically searched and assessed the literature, of screening programmes to identify individuals with an increased cardiometabolic risk in primary care. The screening studies were published between 1967 and 2012. Over the past 50 years the attitude towards screening for an increased cardiometabolic risk has changed. Earlier studies focus on the benefits of screening, whereas later publications search for the best way to screen. With increasing knowledge of benefits of treating cardiometabolic risk factors, the cut-off values for the separate risk factors have become stricter.
A time trend in eligible populations was also observed. Not until 1995 was the first study focusing on an apparently healthy population published.12 In the last 8 years, four of the five existing studies on apparently healthy populations were performed and only two studies in mixed populations were published.19,20 This finding supports the authors’ assumption that people with established CVD, diabetes, hypertension, or dyslipidaemia already receive further risk assessment and treatment through existing pathways; therefore screening among them should not be necessary.
Most published screening programmes were performed in England; no studies were found performed in the US. This might be because of the requirement for actively involving GPs, as the GP has a less strong gatekeeper function in the US.
The first stepwise screening was published in 1993;22 the other three studies using a stepwise method were published in or after 2008.9,11,13 The latter studies all concerned apparently healthy populations. Particularly in these populations a stepwise method can be useful, as a substantial part of them will be healthy. A stepwise method will limit the number of people qualifying for elaborate examinations. A first step that requires action from the invited participants does not seem to influence the response rate compared with being invited for a total risk assessment at once. As only one study also invited a sample of people who did not qualify for further examinations after the first step, it was not possible to compare the discriminative ability of the different stepwise methods.
Sending reminders resulted in a higher screening uptake in apparently healthy populations. As expected, with an opportunistic approach the highest response rate was found with the longest study period.
Public awareness seems to be an important determinant of screening uptake. The highest response rate (93%) was found by Weinehall et al who describe the results of the first 8 years of the Västerbotten Intervention Programme in Sweden.27 The individual screening strategy was combined with a population strategy by creating a local health promotion collaboration to raise public awareness. The opportunistic screening by Cope et al lasted 1 week, but the screening uptake was 39%.4 The investigators advertised their health week in advance, within the general practice and by giving talks.
Devroey et al had an active approach but also the lowest response rate; people were invited by the local authorities to visit their GP for a health check.20 In most studies, people were invited by their GP; in no other study were the authorities responsible for inviting people. Six of the seven studies published in or after 2004 calculated a risk score; this reflects the increased use of risk scores in clinical practice. One might expect lower prevalence rates in an apparently healthy population than in a population with participants already diagnosed with risk factors. When comparing prevalence rates of hypertension, diabetes, or dyslipidaemia between healthy and mixed populations, no substantial differences were observed. From this, it can be concluded that a substantial part of the apparently healthy people have an increased cardiometabolic risk, which makes screening among this population worthwhile.
Strengths and limitations
Before discussing the yield of the screening programmes, some limitations of this systematic literature review need to be considered. As mentioned above, the cut-off values for risk factors have become stricter over the years, hindering the comparison of the yield over time. As a result of heterogeneity of used thresholds and risk scores, it was not possible to compare prevalence rates of cardiometabolic risk factors, nor relate the yield of the different studies to programme characteristics. Because most of the studies performed in mixed populations did not provide information about the composition of their study population, it was not possible to compare the yield of screening between healthy and mixed populations.
A systematic review often includes a risk of bias assessment of quality items like randomisation, selection bias, blinding, and loss-to-follow-up. The main interest in this study were cross-sectional aspects of screening; the focus was on the eligible population, screening method used, patient approach, response rate, and yield of screening. Because the focus was on ‘how’ rather than ‘how well’, no critical appraisal was performed on the above-mentioned items.
Another limitation of this study is that five articles were missed in the analyses as it was not possible to retrieve them full-text.
Comparison with existing literature
Ultimately, it is not the yield of the screening that makes sense, but the reduction of cardiovascular morbidity and mortality by early treatment of risk factors. Si et al examined the effect of screening versus no screening in general practice on surrogate endpoints, and found significant improvement in several cardiovascular risk factors, especially in high-risk populations.29 A Cochrane review, however, found no effect of health checks on total and cardiovascular mortality.30 The studies included in these reviews all started in the 20th century. As shown here, much has changed over the years, not only with regard to the characteristics of the screening programmes, but also with regard to new treatment insights.
Before implementing a screening programme it is first necessary to identify optimal programme efficiency, with regard to method and targeted population. This may influence the effects of screening on morbidity and mortality. In the authors’ opinion, the optimal screening strategy should identify all people with an increased cardiometabolic risk, with a minimum effort to detect these people. Defining ‘optimal’ in such a way, the authors realise that not all the Wilson and Jungner criteria are taken into account,31 such as cost-effectiveness, or psychological harm. Screening might reduce the costs for treating diseases, but screening programmes are also expensive. Therefore, it is important to use the available resources as efficiently as possible. A stepwise approach is likely to be the best way to reduce these costs through selection of a high-risk population, reducing the number of further examinations. Future research will have to prove whether stepwise screening methods are indeed more cost-effective.
Implications for research and practice
As people with established disease or risk factors are likely to receive extensive care through existing chronic care pathways, screening programmes should focus on apparently healthy people.
Stepwise methods can limit the number of people qualifying for further examinations; a stepwise method, in which the first step requires action from the invited participants, does not seem to influence response rate.
An invitation, and if necessary reminders, sent by the GP, appears to increase screening uptake.
Increased public awareness of the opportunity and relevance of screening seem to lead to a higher screening uptake.
In this review, 26 screening programmes are described for detecting people with an increased cardiometabolic risk, performed in primary care. Observed time trends were the shift in focus from a mixed population to an apparently healthy population, an increased use of risk scores, and an increasing use of stepwise methods, especially in apparently healthy populations.
In apparently healthy populations a substantial number of people were detected with an increased cardiometabolic risk, stressing the need for ongoing detection. Stepwise methods, increasing public awareness, and actively involving GPs could improve screening efficiency and uptake.
Funding
Not applicable.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org.uk/letters
REFERENCES
- 1.World Health Organization . The Global Burden of Disease: 2004 Update. Geneva, Switzerland: WHO; 2008. [Google Scholar]
- 2.Gidman W, Ward P, McGregor L. Understanding public trust in services provided by community pharmacists relative to those provided by general practitioners: a qualitative study. BMJ Open. 2012;2:e000939. doi: 10.1136/bmjopen-2012-000939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chamnan P, Simmons RK, Khaw KT, et al. Estimating the population impact of screening strategies for identifying and treating people at high risk of cardiovascular disease: modelling study. BMJ. 2010;340:c1693. doi: 10.1136/bmj.c1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cope JT, Smith DH. A health week in rural general practice. BMJ. 1967;2(5554):756–758. doi: 10.1136/bmj.2.5554.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pike LA. A screening programme for the elderly in a general practice. Practitioner. 1969;203(218):805–812. [PubMed] [Google Scholar]
- 6.Pike LA. Screening middle-aged men in a general practice. Practitioner. 1972;209(253):690–695. [PubMed] [Google Scholar]
- 7.Scott R, Robertson PD. Multiple screening in general practice. BMJ. 1968;2(5606):643–647. doi: 10.1136/bmj.2.5606.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown JS. A coronary screening programme in general practice. J R Coll Gen Pract. 1978;28(197):735–742. [PMC free article] [PubMed] [Google Scholar]
- 9.Godefrooij MB, van de Kerkhof RM, Wouda PJ, et al. Development, implementation and yield of a cardiometabolic health check. Fam Pract. 2012;29(2):174–181. doi: 10.1093/fampra/cmr068. [DOI] [PubMed] [Google Scholar]
- 10.Lambert AM, Burden AC, Chambers J, Marshall T. Cardiovascular screening for men at high risk in Heart of Birmingham Teaching Primary Care Trust: the ‘Deadly Trio’ programme. J Public Health (Oxf) 2012;34(1):73–82. doi: 10.1093/pubmed/fdr052. [DOI] [PubMed] [Google Scholar]
- 11.Marshall T, Westerby P, Chen J, et al. The Sandwell Project: a controlled evaluation of a programme of targeted screening for prevention of cardiovascular disease in primary care. BMC Public Health. 2008;8:73. doi: 10.1186/1471-2458-8-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McMenamin JP. Screening for coronary heart disease risk among men in a general practice. N Z Med J. 1995;108(999):167–168. [PubMed] [Google Scholar]
- 13.van den Donk M, Bobbink IWG, Gorter KJ, et al. Identifying people with metabolic syndrome in primary care by screening with a mailed tape measure. A survey of 14,000 people in the Netherlands. Prev Med. 2009;48(4):345–350. doi: 10.1016/j.ypmed.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Prevalence of risk factors for heart disease in OXCHECK trial: implications for screening in primary care. Imperial Cancer Research Fund OXCHECK Study Group. BMJ. 1991;302(6784):1057–1060. doi: 10.1136/bmj.302.6784.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.British family heart study: its design and method, and prevalence of cardiovascular risk factors. Family Heart Study Group. Br J Gen Pract. 1994;44(379):62–67. [PMC free article] [PubMed] [Google Scholar]
- 16.Anggard EE, Land JM, Lenihan CJ, et al. Prevention of cardiovascular disease in general practice: a proposed model. Br Med J (Clin Res Ed) 1986;293(6540):177–180. doi: 10.1136/bmj.293.6540.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bennett P, Blackall M, Clapham M, et al. South Birmingham Coronary Prevention Project: a district approach to the prevention of heart disease. Community Med. 1989;11(2):90–96. doi: 10.1093/oxfordjournals.pubmed.a042464. [DOI] [PubMed] [Google Scholar]
- 18.Björkelund C, Bengtsson C. Risk factor pattern for cardiovascular and cerebrovascular disease as observed in the female population of a Swedish community, Stromstad. Scand J Prim Health Care. 1991;9(1):11–15. doi: 10.3109/02813439109026575. [DOI] [PubMed] [Google Scholar]
- 19.Bunescu DM, Stoffers HE, van den Akker M, Dinant GJ. Coronary heart disease and cardiovascular risk factors among people aged 25–65 years, as seen in Romanian primary healthcare. Eur J Gen Pract. 2008;14(2):56–64. doi: 10.1080/13814780802343141. [DOI] [PubMed] [Google Scholar]
- 20.Devroey D, Kartounian J, Vandevoorde J, et al. Primary prevention of coronary heart disease in general practice: a cross sectional population study. Int J Clin Pract. 2004;58(2):130–138. doi: 10.1111/j.1368-5031.2004.0104.x. [DOI] [PubMed] [Google Scholar]
- 21.Gran B. Major differences in cardiovascular risk indicators by educational status. Results from a population based screening program. Scand J Soc Med. 1995;23(1):9–16. doi: 10.1177/140349489502300103. [DOI] [PubMed] [Google Scholar]
- 22.Hellénius ML, de Faire U, Krakau I, Berglund B. Prevention of cardiovascular disease within the primary health care system — feasibility of a prevention programme within the Sollentuna primary health care catchment area. Scand J Prim Health Care. 1993;11(1):68–73. doi: 10.3109/02813439308994905. [DOI] [PubMed] [Google Scholar]
- 23.Jones A, Davies DH, Dove JR, et al. Identification and treatment of risk factors for coronary heart disease in general practice: a possible screening model. Br Med J (Clin Res Ed) 1988;296(6638):1711–1714. doi: 10.1136/bmj.296.6638.1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lauritzen T, Leboeuf-Yde C, Lunde IM, Nielsen KD. Ebeltoft project: baseline data from a five-year randomized, controlled, prospective health promotion study in a Danish population. Br J Gen Pract. 1995;45(399):542–547. [PMC free article] [PubMed] [Google Scholar]
- 25.Mann JI, Lewis B, Shepherd J, et al. Blood lipid concentrations and other cardiovascular risk factors: distribution, prevalence, and detection in Britain. BMJ (Clin Res Ed) 1988;296(6638):1702–1706. doi: 10.1136/bmj.296.6638.1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van den Berg PJ, van Dalsen CL, de Rooij RA, et al. Cardiovascular health check in the elderly in one general practice: does it offer new information and lead to interventions? Fam Pract. 1999;16(4):389–394. doi: 10.1093/fampra/16.4.389. [DOI] [PubMed] [Google Scholar]
- 27.Weinehall L, Westman G, Hellsten G, et al. Shifting the distribution of risk: results of a community intervention in a Swedish programme for the prevention of cardiovascular disease. J Epidemiol Community Health. 1999;53(4):243–250. doi: 10.1136/jech.53.4.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tiessen AH, Smit AJ, Zevenhuizen S, et al. Cardiovascular screening in general practice in a low SES area. BMC Fam Pract. 2012;13:117. doi: 10.1186/1471-2296-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Si S, Moss JR, Sullivan TR, et al. Effectiveness of general practice-based health checks: a systematic review and meta-analysis. Br J Gen Pract. 2014 doi: 10.3399/bjgp14X676456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krogsboll LT, Jorgensen KJ, Gronhoj LC, Gotzsche PC. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ. 2012;345:e7191. doi: 10.1136/bmj.e7191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilson JMG, Jungner G. Principles and practice of screening for disease. Public Health Papers nr 34. Geneva: WHO; 1968. [Google Scholar]
- 32.Persson LG, Lindstrom K, Lingfors H, Bengtsson C. A study of men aged 33–42 in Habo, Sweden with special reference to cardiovascular risk factors. Design, health profile and characteristics of participants and non-participants. Scand J Soc Med. 1994;22(4):264–272. doi: 10.1177/140349489402200405. [DOI] [PubMed] [Google Scholar]
- 33.Brannstrom I, Persson LA, Wall S. Gender and social patterning of health: the Norsjo cardiovascular preventive programme in northern Sweden 1985–1990. Scand J Prim Health Care. 1994;12(3):155–161. doi: 10.3109/02813439409003692. [DOI] [PubMed] [Google Scholar]