Abstract
Objective
Evaluate golimumab in patients with active rheumatoid arthritis (RA) and previous tumour necrosis factor-α (TNF) inhibitor use.
Methods
Patients (n=461) previously receiving ≥1 TNF inhibitor were randomised to subcutaneous injections of placebo, golimumab 50 mg or golimumab 100 mg q4 weeks. Primary endpoint (≥20% improvement in American College of Rheumatology (ACR20) criteria at week 14) findings have been reported for all patients in the trial. Reported herein are further assessments of efficacy/safety among patients receiving golimumab+methotrexate (MTX).
Results
Among efficacy-evaluable patients who received MTX at baseline, more receiving golimumab+MTX (n=201) than placebo+MTX (n=103) achieved ACR20 (40.8% vs 14.6%), ACR50 (20.9% vs 3.9%), and ACR70 (11.4% vs 2.9%) responses at week 24. Among the 137 patients who had received only one prior TNF inhibitor (adalimumab, n=33; etanercept, n=47; and infliximab, n=57), week 24 ACR20 rates were 30.3%, 46.8% and 50.9%, respectively, and thus lowest among those who previously used adalimumab. ACR20 response rates were 44.5% (61/137), 36.2% (17/47) and 23.5% (4/17) among patients who had received one, two or three TNF inhibitors, respectively. Adverse event (AE) rates were comparable across type/number of prior anti-TNF agents, but appeared somewhat higher among patients who discontinued previous TNF inhibitor(s) due to intolerance (37/49, 75.5%) versus lack of efficacy (LOE, 113/191, 59.2%).
Conclusions
Patients with active RA previously treated with ≥1 TNF inhibitor had clinically relevant improvement with golimumab+MTX, which appeared somewhat enhanced among those who received only etanercept or infliximab as their prior TNF inhibitor. Golimumab+MTX safety appeared similar across patients, regardless of TNF inhibitor(s) previously used, with fewer AEs occurring among patients who discontinued prior therapy for LOE.
Keywords: Anti-TNF, Rheumatoid Arthritis, DAS28
More than a decade has passed since the initial introduction of tumour necrosis factor-α (TNF) inhibitors, which have greatly expanded treatment options for patients with rheumatoid arthritis (RA).1 Given that patients may not always respond to the first TNF inhibitor prescribed and that there is long-term experience with using other TNF inhibitors, it is reasonable to assume that, in line with recent disease management recommendations,2 3 clinicians will be treating increasing numbers of patients exposed previously to one or more TNF inhibitor(s).
Results of several small case series, open-label studies and registries have indicated that patients who switched from one TNF inhibitor to another resulting from lack of efficacy or intolerance may respond to a second or even third TNF inhibitor.4–9 Benefits of switching from etanercept to infliximab, and vice versa, have been investigated.10–14 Additionally, the strategy of switching patients with RA who are inadequately responsive to a TNF inhibitor to a biological agent with a different mode of action has been compared with that of switching to another TNF inhibitor in non-randomised observational studies of data from registries.6 15
To date, the results of several randomised controlled trials (RCTs) investigating therapies targeted against molecules other than TNF in patients with RA who failed TNF-blockade have been published.16–19 However, the GO-AFTER trial evaluated the efficacy of TNF inhibitor therapy after prior TNF inhibitor use in an RCT.20 In the GO-AFTER trial, not all patients were receiving concomitant methotrexate (MTX), and the primary clinical endpoint was evaluated at 14 weeks because of ethical considerations, although secondary clinical and co-primary functional endpoints were assessed at 6 months in all patients.20 Some RCTs of biological therapies for patients with RA with prior TNF inhibitor use have typically studied the biological agent in combination with MTX and assessed primary endpoints at 6 months.16–20 Some,21 22 but not all,23 systematic reviews may not have considered differences in trial design when evaluating studies. Because some authors have suggested that switching to another monoclonal antibody rather than to an anti-TNF receptor construct agent may be more efficacious after anti-TNF failure,15 especially if the prior TNF inhibitor was discontinued due to lack of efficacy,24 more detailed information on response rates to golimumab in patients who had previously received different TNF inhibitors would inform the selection of candidates for golimumab therapy.
To assess and compare the efficacy and safety of golimumab following discontinuation of one or more other TNF inhibitors in a subgroup of patients and at a time point comparable to those of most other RCTs of biological RA therapies, we examined GO-AFTER trial data from a novel perspective. We present the findings of post-hoc analyses of data obtained from patients with active RA previously treated with one or more TNF inhibitor and also receiving MTX after 6 months of study drug treatment in that trial, as well as hypotheses for assessment in future studies.
Methods
Patients
As detailed previously,20 eligible patients had RA for ≥3 months prior to screening and active disease with ≥4 swollen and ≥4 tender joints (mean values: 16.6/66 and 29.8/68, respectively). Patients had received one or more doses of etanercept, adalimumab or infliximab ≥8 (adalimumab, etanercept) or ≥12 (infliximab) weeks prior to receiving the first dose of study agent. Patients must not have had a clinically serious adverse reaction to any of the prior anti-TNF agents. Previous anti-TNF treatment could have been discontinued for any reason, and the reason(s) for discontinuation were documented by the investigator as either lack of efficacy, intolerance or ‘other’.
Procedures
Patients were randomised (1:1:1) to receive subcutaneous placebo, golimumab 50 mg or golimumab 100 mg every 4 weeks. Randomisation was stratified by investigational site and baseline MTX use (yes/no). Patients and investigators were masked to study treatment assignment; golimumab and placebo were supplied in identical single-use vials. Concomitant MTX use was permitted, but not required, if continued at a stable dose.
Patients in the placebo and golimumab 50-mg groups with <20% improvement in both tender and swollen joint counts at week 16 escaped early to receive golimumab 50 mg and 100 mg, respectively, at week 16 and week 20. Study medication was not altered in the 100-mg group. Week 24 was the efficacy time point of interest in these post-hoc analyses.
Clinical response was assessed using the American College of Rheumatology (ACR) criteria indicating ≥20%, 50% and/or 70% (ACR20,25 ACR50 and ACR70) improvement, as well as by achievement of a good or moderate response according to the 28-joint Disease Activity Score (DAS28) and/or DAS28 <2.6.26 27 DAS28 was determined using C reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Physical function was assessed using the Health Assessment Questionnaire Disability Index (HAQ-DI),28 and a functional response was defined as ≥0.25-unit improvement29 from baseline to week 24. Safety was evaluated by reviewing documentation of reported adverse events (AEs).
Data analysis
Prior anti-TNF therapy was summarised using descriptive statistics by reason for discontinuation and by duration of prior TNF inhibitor for patients who had taken only one prior TNF inhibitor. Since patients could have received more than one TNF inhibitor, the numbers of patients who had discontinued their prior TNF inhibitor were also summarised by reason for discontinuation using non-mutually exclusive prior TNF inhibitor cessation categories.
Efficacy analyses were performed using patients randomised to receive golimumab who reported concomitant MTX use at baseline (n=205). Efficacy data from one North American site were excluded from these analyses because of protocol violations identified during the Sponsor's standard audit processes, yielding 201 efficacy-evaluable patients. Clinical outcomes by prior anti-TNF treatment were summarised using descriptive statistics for randomised patients. The proportions of patients achieving ACR20 and ACR50 responses, DAS28-CRP and DAS28-ESR responses, DAS28-CRP and DAS28-ESR each <2.6, and HAQ–DI response at week 24 were determined among patients who previously had received only one anti-TNF agent and discontinued the treatment for any reason. Clinical response was similarly assessed among patients who had discontinued prior anti-TNF therapy as a result of lack of efficacy, because of intolerance, or for ‘other’ reasons, as well as among patients based on the number of previous TNF inhibitors received. For patients who escaped early, efficacy data from week 16 were carried forward for analysis at week 24 to ensure that the results were not biased by the increased dose of golimumab that the patient received at week 16 or week 24.20
Summaries of AEs include only treated patients (n=204). Data from patients who were treated at the site that was excluded from efficacy analyses are included in these safety summaries. The overall incidences of AEs are summarised by prior anti-TNF agent, as well as by the number of anti-TNF agents received previously and by the reason(s) for discontinuation of prior anti-TNF therapy.
Results
Disposition of prior anti-TNF therapy
In the GO-AFTER trial, 461 patients were randomly assigned to receive placebo (n=155), golimumab 50 mg (n=153) or golimumab 100 mg (n=153) every 4 weeks.20 Baseline characteristics for the MTX-treated subgroup of randomised patients (table 1) were generally consistent with those of the overall study population,20 although fewer MTX-treated patients tested positive for rheumatoid factor at baseline than did patients with no MTX use at baseline (table 1).
Table 1.
Summary of baseline characteristics* in randomised patients and previous TNF inhibitor use† among patients receiving MTX at baseline
| MTX use at baseline | No MTX use at baseline | |||
|---|---|---|---|---|
| Placebo | Golimumab | Placebo | Golimumab | |
| Randomised patients*, n | 107 | 205 | 48 | 101 |
| Women | 89 (83.2%) | 160 (78.0%) | 43 (89.6%) | 75 (74.3%) |
| Age—years | 54.8±12.94 | 53.5±12.23 | 54.8±13.50 | 54.4±11.07 |
| Disease duration—years | 12.4±8.94 | 11.2±8.34 | 12.3±10.96 | 12.0±9.19 |
| Swollen joint count (0–66) | 17.0±11.90 | 16.0±10.02 | 18.6±11.47 | 17.8±12.12 |
| Tender joint count (0–68) | 29.8±18.09 | 29.1±16.20 | 30.3±16.50 | 31.4±17.85 |
| Rheumatoid factor positive | 69 (67.0%) | 137 (69.5%) | 41 (85.4%) | 76 (77.6%) |
| HAQ-DI (0–3) | 1.6±0.58 | 1.4±0.63 | 1.6±0.71 | 1.7±0.68 |
| CRP (mg/L) | 20.8±31.70 | 19.4±30.62 | 20.2±31.59 | 24.6±33.94 |
| ESR (mm h) | 38.9±24.94 | 34.6±28.10 | 37.3±29.26 | 40.4±28.97 |
| DAS28-CRP score | 5.7±1.01 | 5.7±1.04 | 5.7±1.16 | 6.0±1.05 |
| DAS28-ESR score | 6.3±1.10 | 6.1±1.24 | 6.2±1.37 | 6.5±1.24 |
| Number of Prior TNF inhibitors | ||||
| 1 TNF inhibitor | 2 TNF inhibitors | 3 TNF inhibitors | ||
| Golimumab-randomised MTX-treated patients†, n | 137 | 47 | 17 | |
| Prior TNF inhibitor | ||||
| Adalimumab only | Etanercept only | Infliximab only | ||
| Golimumab-randomised patients who received only one prior TNF inhibitor†, n | 33 | 47 | 57 | |
| Reason for discontinuation of prior TNF inhibitor | ||||
| Lack of efficacy | 22 (66.7%) | 23 (48.9%) | 22 (38.6%) | |
| Intolerance | 5 (15.2%) | 2 (4.3%) | 8 (14.0%) | |
| ‘Other’ reason‡ | 6 (18.2%) | 22 (46.8%) | 27 (47.4%) | |
| Distribution by duration of prior treatment, n | ||||
| <4 weeks | 2 | 5 | 2 | |
| ≥4 to <12 weeks | 8 | 12 | 4 | |
| ≥12 to <24 weeks | 7 | 3 | 4 | |
| ≥24 to <36 weeks | 5 | 5 | 3 | |
| ≥36 to <48 weeks | 1 | 2 | 8 | |
| ≥48 weeks | 10 | 20 | 36 | |
| % patients receiving therapy for ≥24 weeks | 48.5% | 57.4% | 82.5% | |
Data presented are number (%) of patients or mean±SD unless otherwise noted.
*Baseline characteristics are summarised for all randomised patients with available data.
†Efficacy-related patient subgroups exclude patients from a single site due to violations at the study site identified during the Sponsor's standard audit processes.
‡In the vast majority of patients, the ‘other’ reason for discontinuation of previous anti-TNF agent(s) was related to cost/insurance coverage.
CRP, C reactive protein; DAS28, 28-joint Disease Activity Score; ESR, erythrocyte sedimentation rate; HAQ-DI, Health Assessment Questionnaire Disability Index; MTX, methotrexate; TNF, tumour necrosis factor.
With the exception of shorter disease duration (8.5 vs 11.6 years, respectively; p=0.023) and more women patients (90.9% (30/33) vs 70.2% (40/57), respectively; p=0.023) among adalimumab-only versus infliximab-only-treated patients, no consistent baseline differences were observed across prior TNF inhibitors (data not shown).
Without the 16 patients treated at the excluded site, 445 randomised patients were available for efficacy analyses, 304 of whom were also receiving MTX at baseline. Two hundred and one of them were randomised to golimumab and were also receiving MTX (table 2); much smaller proportions of patients were receiving sulfasalazine (4.9%) and/or hydrochloroquine (7.4%) in addition to MTX. Among the efficacy-evaluable golimumab-randomised patients who were also receiving MTX, 137 had previously received only one TNF inhibitor (adalimumab, n=33; etanercept, n=47; and infliximab, n=57). For each prior TNF inhibitor, the proportion of patients who discontinued that agent because of lack of efficacy was 2.5-fold to 11-fold greater than those who discontinued because of intolerance (table 1). Overall, most patients received prior anti-TNF therapy for ≥24 weeks (table 1).
Table 2.
Summary of clinical efficacy at week 24* among efficacy-evaluable randomised patients receiving MTX at baseline†
| Golimumab | ||||
|---|---|---|---|---|
| Placebo | 50 mg | 100 mg | Combined | |
| Efficacy-evaluable randomised patients receiving study agent+MTX, n | 103 | 101 | 100 | 201 |
| ACR20 response | 15 (14.6%) | 36 (35.6%) | 46 (46.0%) | 82 (40.8%) |
| ACR50 response | 4 (3.9%) | 20 (19.8%) | 22 (22.0%) | 42 (20.9%) |
| ACR70 response | 3 (2.9%) | 12 (11.9%) | 11 (11.0%) | 23 (11.4%) |
| DAS28-CRP response‡ | 24 (23.3%) | 49 (48.5%) | 65 (65.0%) | 114 (56.7%) |
| DAS28-CRP score <2.6 | 2 (1.9%) | 12 (11.9%) | 14 (14.0%) | 26 (12.9%) |
| DAS28-ESR response‡ | 27 (26.2%) | 49 (48.5%) | 67 (67.0%) | 116 (57.7%) |
| DAS28-ESR score <2.6 | 1 (1.0%) | 11 (10.9%) | 16 (16.0%) | 27 (13.4%) |
| HAQ-DI ≥0.25-unit improvement | 35 (34.0%) | 48 (47.5%) | 54 (54.0%) | 102 (50.7%) |
Data presented are number (%) of patients unless otherwise noted.
*For patients who early escaped, efficacy data from week 16 were carried forward for analysis at week 24.
†Excludes patients from a single site due to violations at the study site identified during the Sponsor's standard audit processes. These violations were not confirmed until after the initial publication of trial results, thus resulting in minor numerical differences in response rates between the initial report20 and the current paper regarding patients treated with golimumab+MTX.
‡DAS28-CRP/ESR score indicating a ‘good’ or ‘moderate’ response.
ACR20, ACR 50, ACR70, at least 20%, 50%, or 70% improvement according to the American College of Rheumatology response criteria; CRP, C reactive protein; DAS28, 28-joint Disease Activity Score; ESR, erythrocyte sedimentation rate; HAQ-DI, Health Assessment Questionnaire Disability Index; MTX, methotrexate.
Clinical improvement
All golimumab-randomised patients who were receiving MTX at baseline
Among patients with active RA who were previously treated with a TNF inhibitor, 40.8% of golimumab+MTX-treated patients and 14.6% of placebo+MTX-treated patients achieved an ACR20 response at week 24. The ACR50 and ACR70 response rates were also higher among patients who received golimumab+MTX (20.9% and 11.4%, respectively) than among those who received placebo+MTX (3.9% and 2.9%, respectively). Similar patterns of improvement were observed when disease activity was assessed using the DAS28-CRP or the DAS28-ESR and also when using achievement of a ≥0.25-unit reduction in the HAQ-DI score to assess improvement in physical function (table 2).
All golimumab-randomised patients who were receiving MTX at baseline and who had discontinued only one prior TNF inhibitor
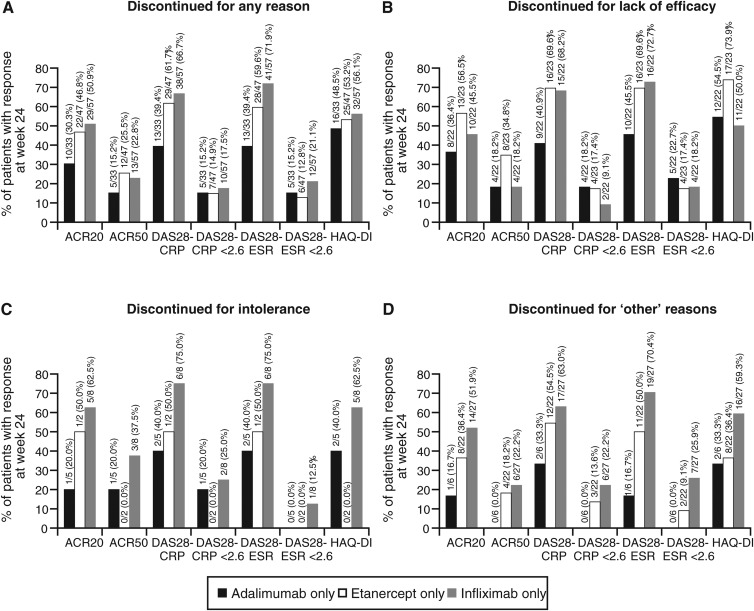
Among efficacy-evaluable, golimumab-randomised patients receiving MTX at baseline, 137 had previously received only one prior TNF inhibitor (adalimumab, n=33; etanercept, n=47; infliximab, n=57). The proportion of patients who achieved an ACR20 response at week 24 was 30.3% among those who previously had been treated only with adalimumab, 46.8% among those who previously had been treated only with etanercept and 50.9% among those who previously had been treated only with infliximab. A similar pattern of clinical response was observed when ACR50 response criteria were applied (figure 1).
Figure 1.
Improvement in rheumatoid arthritis signs and symptoms and physical function in golimumab-randomised patients with baseline methotrexate use by reason for discontinuations of prior TNF inhibitor use, including any reason (A), lack of efficacy (B), intolerance (C) and ‘other’ reasons (D). ACR20, ACR50, at least 20% or 50% improvement according to the American College of Rheumatology response criteria; CRP, C reactive protein; DAS28, 28-joint Disease Activity Score; ESR, erythrocyte sedimentation rate; HAQ-DI, Health Assessment Questionnaire Disability Index response (≥ 0.25-unit improvement); TNF, tumour necrosis factor.
Also at week 24, the proportions of patients achieving DAS28-CRP response (good/moderate) and DAS28-CRP <2.6 were 39.4% and 15.2%, respectively, among those who previously had been treated only with adalimumab, 61.7% and 14.9%, respectively, among those who previously had been treated only with etanercept and 66.7% and 17.5%, respectively, among those who previously had been treated only with infliximab. Similar patterns were observed for DAS28-ESR response (good/moderate) and DAS28-ESR<2.6 (figure 1). Improvement in physical function, as assessed by achievement of a ≥0.25-unit reduction in the HAQ-DI score from baseline to week 24, was fairly consistent across the three TNF inhibitors used previously and was achieved by 48.5%, 53.2% and 56.1% of patients who had received only adalimumab, etanercept or infliximab, respectively (figure 1).
Among patients who discontinued prior TNF inhibitor treatment because of lack of efficacy, ACR20 response rates at week 24 were 36.4% for those who previously had been treated only with adalimumab, 56.5% for those who previously had been treated only with etanercept and 45.5% for those who previously had been treated only with infliximab. Among patients who discontinued previous TNF inhibitor treatment because of intolerance, ACR20 response rates at week 24 were 20.0%, 50.0% and 62.5% for adalimumab, etanercept and infliximab, respectively, but sample sizes were small. Similarly, among those who discontinued previous TNF inhibitor treatment for ‘other’ reasons, respective ACR20 response rates at week 24 were 16.7%, 36.4% and 51.9% for adalimumab, etanercept and infliximab, respectively (figure 1).
In table 3, clinical responses at week 24 are compared by the number of TNF inhibitors that patients had received prior to study entry. By most measures, improvement in clinical signs and symptoms and in physical function appeared to be more robust among patients who previously had received fewer TNF inhibitors. However, the numbers of patients who had received two (n=47) and three (n=17) prior TNF inhibitors were limited.
Table 3.
Clinical response at week 24* among golimumab+ MTX-treated patients† by number of previous TNF inhibitor(s)
| Number of previous TNF inhibitor(s) | |||
|---|---|---|---|
| 1 TNF inhibitor | 2 TNF inhibitors | 3 TNF inhibitors | |
| Patients who discontinued one or more previous TNF-inhibitor for any reason, n | 137 | 47 | 17 |
| ACR20 response | 61 (44.5%) | 17 (36.2%) | 4 (23.5%) |
| ACR50 response | 30 (21.9%) | 11 (23.4%) | 1 (5.9%) |
| DAS28 response (good/moderate) | |||
| DAS28-CRP | 80 (58.4%) | 24 (51.1%) | 10 (58.8%) |
| DAS28-ESR | 82 (59.9%) | 24 (51.1%) | 10 (58.8%) |
| DAS28 score <2.6 | |||
| DAS28-CRP | 22 (16.1%) | 3 (6.4%) | 1 (5.9%) |
| DAS28-ESR | 23 (16.8%) | 3 (6.4%) | 1 (5.9%) |
| HAQ-DI ≥0.25-unit improvement | 73 (53.3%) | 22 (46.8%) | 7 (41.2%) |
Data presented are number (%) of patients unless otherwise noted.
*For patients who escaped early, efficacy data from week 16 were carried forward for analysis at week 24.
†Excludes patients from a single site due to violations at the study site identified during the Sponsor's standard audit processes.
ACR20, ACR50, at least 20% or 50% improvement according to the American College of Rheumatology response criteria; CRP, C reactive protein; DAS28, 28-joint Disease Activity Score; ESR, erythrocyte sedimentation rate; HAQ-DI, Health Assessment Questionnaire Disability Index; MTX, methotrexate; TNF, tumour necrosis factor.
Adverse events
Safety findings for all patients enrolled in the GO-AFTER study have been reported through week 2420 and also through up to 3 years of golimumab therapy.30 AEs were reported by 64.3% of all MTX-treated patients. Among these, 75.5% of patients who had been intolerant of prior therapy and 59.2% of those who had an inadequate response to treatment with the prior TNF inhibitor(s) reported AEs. The overall proportions of patients developing AEs were similar among those treated with either golimumab or placebo, when grouped by number of prior TNF inhibitors received, specific prior TNF inhibitor received or reason for discontinuation of that previous agent (table 4).
Table 4.
MTX-treated patients with adverse events by number, type, and reason for discontinuation of previous TNF inhibitor(s) during the placebo-controlled study period (weeks 0–16)
| Placebo+MTX | Golimumab+MTX | All patients | |
|---|---|---|---|
| All Adverse Events (AEs) | 67/107 (62.6%) | 133/204 (65.2%) | 200/311 (64.3%) |
| All AEs by number of prior agents | |||
| 1 TNF inhibitor | 38/60 (63.3%) | 93/140 (66.4%) | 131/200 (65.5%) |
| 2 TNF inhibitors | 20/33 (60.6%) | 28/46 (60.9%) | 48/79 (60.8%) |
| 3 TNF inhibitors | 9/14 (64.3%) | 12/18 (66.7%) | 21/32 (65.6%) |
| All AEs by prior agent* | |||
| Adalimumab only | 10/14 (71.4%) | 21/34 (61.8%) | 31/48 (64.6%) |
| Etanercept only | 9/17 (52.9%) | 31/49 (63.3%) | 40/66 (60.6%) |
| Infliximab only | 19/29 (65.5%) | 41/57 (71.9%) | 60/86 (69.8%) |
| All AEs by reason for d/c of agent† | |||
| Lack of efficacy | 40/70 (57.1%) | 73/121 (60.3%) | 113/191 (59.2%) |
| Intolerance | 13/16 (81.3%) | 24/33 (72.7%) | 37/49 (75.5%) |
| ‘Other’ reason | 24/40 (60.0%) | 52/75 (69.3%) | 76/115 (66.1%) |
| Serious Adverse Events (SAEs) | 8/107 (7.5%) | 6/204 (2.9%) | 14/311 (4.5%) |
| SAEs by number of prior agents | |||
| 1 TNF inhibitor | 3/60 (5.0%) | 2/140 (1.4%) | 5/200 (2.5%) |
| 2 TNF inhibitors | 2/33 (6.1%) | 1/46 (2.2%) | 3/79 (3.8%) |
| 3 TNF inhibitors | 3/14 (21.4%) | 3/18 (16.7%) | 6/32 (18.8%) |
| SAEs by prior agent* | |||
| Adalimumab only | 0/14 (0.0%) | 2/34 (5.9%) | 2/48 (4.2%) |
| Etanercept only | 0/17 (0.0%) | 0/49 (0.0%) | 0/66 (0.0%) |
| Infliximab only | 3/29 (10.3%) | 0/57 (0.0%) | 3/86 (3.5%) |
| SAEs by reason for d/c of agent† | |||
| Lack of efficacy | 7/70 (10.0%) | 4/121 (3.3%) | 11/191 (5.8%) |
| Intolerance | 1/16 (6.3%) | 2/33 (6.1%) | 3/49 (6.1%) |
| ‘Other’ reason | 1/40 (2.5%) | 1/75 (1.3%) | 2/115 (1.7%) |
| Serious Infections (SIs) | 3/107 (2.8%) | 2/204 (1.0%) | 5/311 (1.6%) |
| SIs by number of prior agents | |||
| 1 TNF inhibitor | 2/60 (3.3%) | 1/140 (0.7%) | 3/200 (1.5%) |
| 2 TNF inhibitors | 1/33 (3.0%) | 0/46 (0.0%) | 1/79 (1.3%) |
| 3 TNF inhibitors | 0/14 (0.0%) | 1/18 (5.6%) | 1/32 (3.1%) |
| SIs by prior agent* | |||
| Adalimumab only | 0/14 (0.0%) | 1/34 (2.9%) | 1/48 (2.1%) |
| Etanercept only | 0/17 (0.0%) | 0/49 (0.0%) | 0/66 (0.0%) |
| Infliximab only | 2/29 (6.9%) | 0/57 (0.0%) | 2/86 (2.3%) |
| SIs by reason for d/c of prior agent† | |||
| Lack of efficacy | 2/70 (2.9%) | 1/121 (0.8%) | 3/191 (1.6%) |
| Intolerance | 0/16 (0.0%) | 1/33 (3.0%) | 1/49 (2.0%) |
| ‘Other’ reason | 1/40 (2.5%) | 1/75 (1.3%) | 2/115 (1.7%) |
Data presented are number (%) of treated patients.
*Among patients who received only one prior TNF inhibitor.
†Some patients had received more than one TNF inhibitor and could have discontinued each one for a different reason. In the vast majority of patients, the ‘other’ reason for discontinuation of previous anti-TNF agent(s) was related to cost/insurance coverage.
d/c, discontinuation; MTX, methotrexate; TNF, tumour necrosis factor.
The incidences of serious AEs and serious infections appeared to be comparable across the subgroups of patients evaluated, with the exception of a higher incidence of serious AEs among patients who had received three (18.8%) prior TNF inhibitors, compared with those who previously had received one (2.5%) or two (3.8%) TNF inhibitors. However, interpretation of these findings is limited by the small numbers of patients who experienced serious AEs or serious infections (table 4).
Discussion
Although data derived from several small case series, open-label studies and registries have suggested that patients with RA switched from one to another TNF inhibitor because of lack of efficacy or intolerance may respond to the second or even third agent,4–9 such response patterns have not previously been examined in a randomised, controlled study. Using data from the GO-AFTER trial,20 we evaluated the efficacy and safety of golimumab when switching from another TNF inhibitor among more than 200 patients with active RA who previously received adalimumab, etanercept and/or infliximab and reported MTX use at baseline. Our post-hoc data analyses indicate that among patients taking MTX at baseline, the response rates at week 24 are somewhat higher than those reported previously for all patients at the primary endpoint of week 14.20 This is consistent with the generally accepted principle that concomitant use of MTX with a TNF inhibitor results in better clinical and functional outcomes.31–33 Moreover, patients who switch from adalimumab, etanercept or infliximab to golimumab demonstrate clinically relevant responses at week 24, regardless of whether the prior TNF inhibitor was a monoclonal antibody or a soluble receptor fusion protein.
Of note and consistent with results of a comparative meta-analysis,23 although it is difficult to compare outcomes across clinical trials due to differences in trial design, week 24 ACR response rates among patients who had discontinued prior anti-TNF therapy and received golimumab+MTX in GO-AFTER are comparable to those observed at the same week 24 time point for other biological agents with different mechanisms of action in combination with MTX. For example, week 24 ACR50 response rates for study agent versus placebo, both with concomitant disease-modifying antirheumatic drugs, were 27% and 5% for rituximab16; 29% (8 mg/kg), 17% (4 mg/kg) and 4% for tocilizumab34; and 20% and 4% for abatacept.18
The most straightforward approach to assess effects of switching agents is to analyse data derived from patients previously treated with only one prior TNF inhibitor. Despite our previously reported observations of clinically relevant responses to golimumab in the overall trial population,20 patients previously exposed to more than two TNF inhibitors appear to be less likely to demonstrate marked improvement in clinical and functional outcomes. ACR50 response rates were similar among patients who had been treated with one or two prior TNF inhibitors, but were much lower when golimumab was initiated as the fourth TNF inhibitor. Although these findings suggest that such patients might respond better to a biological agent with a different mechanism of action, it should be considered that the rates of response to each of rituximab and abatacept also decrease with previous exposure to increasing numbers of TNF inhibitors.35 36 Future studies employing biomarkers may help to predict which patients are more likely to respond to the different agents, following initial exposure to a TNF inhibitor.
Because patients were not stratified by prior TNF inhibitor use when randomised to treatment arms, the size of some of the subgroups that were evaluated was small, and our subgroup analyses were performed post-hoc, no formal statistical testing was performed. Despite these limitations, the data reveal numerical trends. For example, ACR20 response rates at week 24 for patients treated with golimumab 50 or 100 mg and MTX were numerically higher among those who switched from etanercept (46.8%) or infliximab (50.9%) compared with those who had previously received adalimumab (30.3%), the agent most similar in structure to golimumab.37 Conversely, the proportion of patients who were previously treated with adalimumab for more than 24 weeks was much lower than that of patients who had previously received treatment with etanercept or infliximab for more than 24 weeks, which could have been due to a larger number of patients with refractory disease among those receiving adalimumab treatment. It is possible that patients previously treated with agents structurally more dissimilar to golimumab developed antibodies to the prior TNF inhibitor that precluded continued response to the previous agent38; these antibodies might have been less likely to cross-react with the human golimumab molecule, allowing a better subsequent response to golimumab. The presence of antibodies to prior TNF inhibitor(s) was not assessed in GO-AFTER. However, future studies of switching among TNF inhibitors should include such assessments to better characterise the mechanisms underlying differential responses to subsequent treatment.
The safety profile of golimumab+MTX was similar to that of placebo+MTX and was consistent among patients who previously received adalimumab, etanercept or infliximab, and among those who had received one, two or three prior TNF inhibitors. When assessed by reason for discontinuation of previous anti-TNF agent(s), however, AEs appeared to be more common among patients who had discontinued prior anti-TNF therapy because of intolerance than because of lack of efficacy or ‘other’ reasons. The incidences of serious AEs and serious infections were low, but appeared comparable across patient subgroups evaluated, except for a somewhat higher incidence of serious AEs among patients who had received three (18.8%) prior TNF inhibitors, compared with those who previously had received one (2.5%) or two (3.8%) inhibitors. Overall, the safety findings are not unexpected given that TNF inhibitors as a class, regardless of the specific molecular construct, share similar potential safety risks.37 39–41
This post-hoc subgroup analysis has several limitations. As mentioned above, patient randomisation was not stratified by the specific TNF inhibitor or by the number of TNF inhibitors used previously. Subgroup sample size was small in some of these comparisons. Also, patients enrolled into the GO-AFTER trial could have discontinued their prior TNF inhibitor(s) for any reason; reasons for discontinuation were categorised at the discretion of the study investigator, as no formal definitions were provided.
In conclusion, patients with active RA who previously received TNF inhibitor therapy and were treated with golimumab and concomitant MTX in the GO-AFTER trial demonstrated clinically relevant improvement in disease activity and physical function after switching to golimumab, regardless of which TNF inhibitor had been taken previously. Of particular note, patients who switched from either etanercept or infliximab appeared to exhibit better subsequent responses to golimumab than those that were observed among patients who previously had received adalimumab which, of the three prior TNF inhibitors, is most structurally similar to golimumab. However, further study is required to confirm the current findings.
Acknowledgments
We thank Kirsten Schuck, Michelle Perate, MS, and Mary Whitman, PhD, of Janssen Services, LLC, for their assistance in the development and submission of this manuscript.
Footnotes
Funding: This study was supported by Janssen Research & Development, LLC and Merck/Schering-Plough.
Competing interests: JSS, JK, ELM and RL are research investigators for the GO-AFTER golimumab clinical trial. JSS has received research grant support from Abbott, BMS, MSD, Pfizer, Roche and UCB and consultation and/or speaking honoraria from Abbott, Astra-Zeneca, BMS, Celgene, Glaxo, Janssen, MSD, Novo-Nordisk, Pfizer, Roche, Sanofi-Aventis and UCB. JK has received research funding paid to the University of Massachusetts Medical School from Bristol Myers Squibb Co., F. Hoffmann-La Roche Ltd. and Sanofi-Aventis and consulting income from Bristol Myers Squibb Co., Crescendo BioScience Inc., Eisai Co. Ltd., Janssen, Johnson & Johnson, Mallinckrodt Inc., NovoNordisk Inc., Pfizer Inc. and UCB S.A. ELM has received research grant support and consultation honoraria from Janssen. RL has received research grant support from Abbott, Pfizer, Roche and UCB and consultation and/or speaking honoraria from Abbott, Astra-Zeneca, BMS, Glaxo, Janssen, MSD, Pfizer, Roche and UCB. EC Hsia, S Xu, and Y Zhou are employees of Janssen Research & Development, LLC; MKD was employed by Janssen at the time this manuscript was initially drafted and is now employed by Alexion Pharmaceuticals.
Ethics approval: The GO-AFTER study (ClinicalTrials.gov: NCT00299546) was conducted according to principles of the Declaration of Helsinki. All patients provided written informed consent, and the protocol was approved by a central and individual institutional review boards.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hetland ML, Christensen IJ, Tarp U, et al. ; on behalf of All Departments of Rheumatology in Denmark. Direct comparison of treatment responses, remission rates, and drug adherence in patients with rheumatoid arthritis treated with adalimumab, etanercept, or infliximab: results from eight years of surveillance of clinical practice in nationwide Danish DANBIO registry. Arthritis Rheum 2010;62:22–32 [DOI] [PubMed] [Google Scholar]
- 2.Smolen JS, Landewé R, Breedveld FC, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs. Ann Rheum Dis 2010;69:964–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh JA, Furst D, Bharat A. 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 2012;64:625–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alivernini S, Laria A, Gremese E, et al. ACR70-disease activity score remission achievement from switches between all the available biological agents in rheumatoid arthritis: a systematic review of the literature. Arthritis Res Ther 2009;11:R163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erickson AR, Mikuls TR. Switching anti-TNF-alpha agents: what is the evidence? Curr Rheumatol Rep 2007;9:416–20 [DOI] [PubMed] [Google Scholar]
- 6.Gomez-Reino JJ, Carmona L; and the BIOBADASER Group. Switching TNF antagonists in patients with chronic arthritis: an observational study of 488 patients over a four-year period. Arthritis Res Ther 2006;8:R29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hyrich KL, Lunt M, Watson KD, et al. for the British Society for Rheumatology Biologics Register. Outcomes after switching from one anti–tumor necrosis factor α agent to a second anti–tumor necrosis factor α agent in patients with rheumatoid arthritis: results from a large UK national cohort study. Arthritis Rheum 2007;56:13–20 [DOI] [PubMed] [Google Scholar]
- 8.Scrivo R, Conti F, Spinelli FR, et al. Switching between TNFα antagonists in rheumatoid arthritis: personal experience and review of the literature. Reumatismo 2009;61:107–17 [DOI] [PubMed] [Google Scholar]
- 9.van Vollenhoven RF. Switching between biological agents. Clin Exp Rheumatol 2004;22(Suppl 35):S115–21 [PubMed] [Google Scholar]
- 10.Cohen G, Courvoisier N, Cohen JD, et al. The efficiency of switching from infliximab to etanercept and vice-versa in patients with rheumatoid arthritis. Clin Exp Rheumatol 2005;23:795–800 [PubMed] [Google Scholar]
- 11.Furst DE, Gaylis N, Bray V, et al. Open-label, pilot protocol of patients with rheumatoid arthritis who switch to infliximab after an incomplete response to etanercept: the opposite study. Ann Rheum Dis 2007;66:893–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hansen KE, Hildebrand JP, Genovese MC, et al. The efficacy of switching from etanercept to infliximab in patients with rheumatoid arthritis. J Rheumatol 2004;31:1098–102 [PubMed] [Google Scholar]
- 13.Laas K, Peltomaa R, Kautiainen H, et al. Clinical impact of switching from infliximab to etanercept in patients with rheumatoid arthritis. Clin Rheumatol 2008;27:927–32 [DOI] [PubMed] [Google Scholar]
- 14.van Vollenhoven R, Harju A, Brannemark S, et al. Treatment with infliximab (Remicade) when etanercept (Enbrel) has failed or vice versa: data from the STURE registry showing that switching tumour necrosis factor α blockers can make sense. Ann Rheum Dis 2003;62:1195–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Finckh A, Ciurea A, Brulhart L, et al. ; on behalf of the physicians of the Swiss Clinical Quality Management Program for Rheumatoid Arthritis. B cell depletion may be more effective than switching to an alternative anti–tumor necrosis factor agent in rheumatoid arthritis patients with inadequate response to anti–tumor necrosis factor agents. Arthritis Rheum 2007;56:1417–23 [DOI] [PubMed] [Google Scholar]
- 16.Cohen SB, Emery P, Greenwald MW, et al. for the REFLEX Trial Group. Rituximab for rheumatoid arthritis refractory to anti–tumor necrosis factor therapy: results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial evaluating primary efficacy and safety at twenty-four weeks. Arthritis Rheum 2006;54:2793–806 [DOI] [PubMed] [Google Scholar]
- 17.Emery P, Keystone E, Tony HP, et al. IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to anti-tumour necrosis factor biologicals: results from a 24-week multicentre randomised placebo-controlled trial. Ann Rheum Dis 2008;67:1516–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Genovese MC, Becker J-C, Schiff M, et al. Abatacept for rheumatoid arthritis refractory to tumor necrosis factor α inhibition. N Engl J Med 2005;353:1114–23 [DOI] [PubMed] [Google Scholar]
- 19.Genovese MC, Schiff M, Luggen M, et al. Efficacy and safety of the selective co-stimulation modulator abatacept following 2 years of treatment in patients with rheumatoid arthritis and an inadequate response to anti-tumour necrosis factor therapy. Ann Rheum Dis 2008;67:547–54 [DOI] [PubMed] [Google Scholar]
- 20.Smolen JS, Kay J, Doyle MK, et al. , for the GO-AFTER study investigators. Golimumab in patients with active rheumatoid arthritis after treatment with tumour necrosis factor α inhibitors (GO-AFTER study): a multicentre, randomised, double-blind, placebo-controlled, phase III trial. Lancet 2009;374:210–21 [DOI] [PubMed] [Google Scholar]
- 21.Nam JL, Winthrop KL, van Vollenhoven RF, et al. Current evidence for the management of rheumatoid arthritis with biological disease-modifying antirheumatic drugs: a systematic literature review informing the EULAR recommendations for the management of RA. Ann Rheum Dis 2010;69:976–86 [DOI] [PubMed] [Google Scholar]
- 22.Singh JA, Christensen R, Wells GA, et al. Biologics for rheumatoid arthritis: an overview of Cochrane reviews. Cochrane Database of Systematic Reviews 2009;(4):CD007848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schoels M, Aletaha D, Smolen JS, et al. Comparative effectiveness and safety of biological treatment options after tumour necrosis factor α inhibitor failure in rheumatoid arthritis: systematic review and indirect pairwise meta-analysis. Ann Rheum Dis 2012;71:1303–8 [DOI] [PubMed] [Google Scholar]
- 24.Finckh A, Ciurea A, Brulhart L, et al. , on behalf of the doctors of the Swiss Clinical Quality Management Programme for Rheumatoid Arthritis. Which subgroup of patients with rheumatoid arthritis benefits from switching to rituximab versus alternative anti-tumour necrosis factor (TNF) agents after previous failure of an anti-TNF agent? Ann Rheum Dis 2010;69:387–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Felson DT, Anderson JJ, Boers M, et al. American College of Rheumatology preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum 1995;38:727–35 [DOI] [PubMed] [Google Scholar]
- 26.Prevoo MLL, van't Hof MA, Kuper HH, et al. Modified disease activity scores that include twenty-eight-joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 1995;38:44–8 [DOI] [PubMed] [Google Scholar]
- 27.van Riel PLCM, van Gestel AM, Scott DL; on behalf of The EULAR Standing Committee for International Clinical Studies including Therapeutic Trials—ESCISIT. EULAR Handbook of Clinical Assessments in Rheumatoid Arthritis. Alphen Aan Den Rijn, The Netherlands: Van Zuiden Communications B.V., 2000:40 [Google Scholar]
- 28.Fries JF, Spitz P, Kraines RG, et al. Measurement of patient outcome in arthritis. Arthritis Rheum 1980;23:137–45 [DOI] [PubMed] [Google Scholar]
- 29.Wells GA, Tugwell P, Kraag GR, et al. Minimum important difference between patients with rheumatoid arthritis: the patient's perspective. J Rheumatol 1993;20:557–60 [PubMed] [Google Scholar]
- 30.Smolen JS, Kay J, Landewé RBM, et al. Golimumab in patients with active rheumatoid arthritis who have previous experience with tumour necrosis factor inhibitors: results of a long-term extension of the randomised, double-blind, placebo-controlled GO-AFTER study through week 160. Ann Rheum Dis 2012;71:1671–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Breedveld FC, Weisman MH, Kavanaugh AF, et al. for the PREMIER Investigators. the PREMIER study: a multicenter, randomized, double-blind clinical trial of combination therapy with adalimumab plus methotrexate versus methotrexate alone or adalimumab alone in patients with early, aggressive rheumatoid arthritis who had not had previous methotrexate treatment. Arthritis Rheum 2006;54:26–37 [DOI] [PubMed] [Google Scholar]
- 32.Klareskog L, van der Heijde D, de Jager JP, et al. for the TEMPO (Trial of Etanercept and Methotrexate with Radiographic Patient Outcomes) study investigators. Therapeutic effect of the combination of etanercept and methotrexate compared with each treatment alone in patients with rheumatoid arthritis: double-blind randomised controlled trial. Lancet 2004;363:675–81 [DOI] [PubMed] [Google Scholar]
- 33.Maini RN, Breedveld FC, Kalden JR, et al. Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor α monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum 1998;41:1552–63 [DOI] [PubMed] [Google Scholar]
- 34.Emery P. Optimizing outcomes in patients with rheumatoid arthritis and an inadequate response to anti-TNF treatment. Rheumatology (Oxford) 2012;51(Suppl 5):v22–30 [DOI] [PubMed] [Google Scholar]
- 35.Kremer JM, Tony H, Tak PP, et al. Efficacy of rituximab in active RA patients with an inadequate response to one or more TNF inhibitors. Ann Rheum Dis 2006;65(Suppl II):326 (Abstract FRI0133). Poster session FRI0133 presented at the 7th Annual European Congress of Rheumatology (EULAR 2006), Amsterdam, 21–24 June 2006 [Google Scholar]
- 36.Schiff M, Pritchard C, Huffstutter JE, et al. The 6-month safety and efficacy of abatacept in patients with rheumatoid arthritis who underwent a washout after anti-tumour necrosis factor therapy or were directly switched to abatacept: the ARRIVE trial. Ann Rheum Dis 2009;68:1708–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tracey D, Klareskog L, Sasso EH, et al. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther 2008;117: 244–79 [DOI] [PubMed] [Google Scholar]
- 38.Wolbink GJ, Vis M, Lems W, et al. Development of antiinfliximab antibodies and relationship to clinical response in patients with rheumatoid arthritis. Arthritis Rheum 2006;54:711–5 [DOI] [PubMed] [Google Scholar]
- 39.Enbrel (Etanercept) Summary of Product Characteristics. European Medicines Agency. http://www.medicines.org.uk/emc/medicine/3343/SPC/ (accessed Jan 2013)
- 40.Humira (Adalimumab) Summary of Product Characteristics. European Medicines Agency. http://www.medicines.org.uk/emc/medicine/21201/SPC/ (accessed Jan 2013)
- 41.Remicade (Infliximab) Summary of Product Characteristics. European Medicines Agency. http://www.medicines.org.uk/emc/medicine/3236/SPC/ (accessed Jan 2013)