Abstract
Background:
Despite proven benefits of upper extremity nerve decompression in diabetics, neurolysis for diabetic patients with lower extremity (LE) nerve compression remains controversial.
Methods:
A search of ClinicalTrials.gov and Cochrane clinical trials registries, CENTRAL (The Cochrane Library), MEDLINE, EMBASE, LILACS, CINAHL, SCOPUS, and Google Scholar from 1962 to 2012, yielded 1956 citations. Any potential randomized or quasi-randomized controlled trials and observational cohort studies of diabetics with neurolysis of the common peroneal nerve, deep peroneal nerve, or tibial nerve were assessed. We included articles in any language that 1) provided information about diabetic patients who had neurolysis for symptomatic nerve compression diagnosed by (+) Tinel sign or electrodiagnostic study, and 2) quantified outcomes for pain, sensibility, or ulcerations/amputations. Case reports, review articles, animal or cadaver studies, and studies with <10 patients were excluded. We assessed pain relief, recovery of sensibility, and postoperative incidence of ulcerations/amputations at follow-up >3 months. A meta-analysis of descriptive statistics was performed.
Results:
Ten clinical series with a mean clinical relevance score of 70% and a mean methodologic quality score of 50% met inclusion criteria. We included 875 diabetic patients and 1053 LEs. Pain relief >3 points on visual analog scale occurred in 91% of patients; sensibility improved in 69%. Postoperative ulceration/amputation incidence was significantly reduced compared to preoperative incidence (odds ratio = 0.066, 95% confidence interval = 0.026–0.164, P < 0.0001).
Conclusions:
Observational data suggest that neurolysis significantly improves outcomes for diabetic patients with compressed nerves of the LE. No randomized controlled trials have been published.
Diabetes mellitus is a hyperglycemic syndrome due to deficient insulin production or increased insulin resistance or both. According to the World Health Organization estimates, the global prevalence of diabetes has increased from 153 [95% confidence interval (CI): 127–182] million people in 1980 to 347 (95% CI: 314–382) million in 2008, and the number continues to rise.1 In 2011, 8.3% of the US population (represented by 25.8 million people) carried a diagnosis of diabetes mellitus.2 Diabetic patients may experience several complications, of which neuropathy is considered to be one of the most common, debilitating, and expensive to treat, affecting up to 60% of people with diabetes.2–5
Diabetic neuropathy has been considered an irreversible and progressive disease6; however, some researchers have suggested that there remains hope for diabetic patients with neuropathy.7–20 Based on the “double crush” hypothesis,21,22 they have proposed that diabetic neuropathy may be due, in part, to compression of the nerves at sites of anatomic narrowing and that surgical decompression of these nerves may be an effective way to alleviate the neuropathic somatosensory symptoms and prevent complications.8–20 On the other hand, other researchers state that there is not enough evidence to support the use of nerve decompression on the diabetic population with neuropathy.23–28
It is within this context of uncertainty that our systematic review and meta-analysis arises. The aim of this study is to systematically review the current literature regarding the effect of neurolysis on pain relief, peripheral sensation recovery, and the incidence of ulcerations/amputations on diabetic patients with superimposed nerve compression of the lower extremities (LEs). In addition, falls, fall-associated fractures, and hospitalizations for foot infections other than surgical site infections (SSIs) were also investigated. A meta-analysis of studies evaluating these selected endpoints was performed.
METHODS
Search Strategy
The authors thoroughly searched the following databases: ClinicalTrials.gov and Cochrane clinical trials registries, CENTRAL (The Cochrane Library), MEDLINE, EMBASE, LILACS, CINAHL, SCOPUS, and Google Scholar from 1962 (first time that neurolysis was applied to progressive peripheral nerve lesions)29 to 2012. The search strategy was adapted to each database using an appropriate combination of subject and text-word terms. (See Appendix, Supplemental Digital Content 1, which describes the neurolysis systematic review search strategy used to explore the electronic databases [ClinicalTrials.gov and Cochrane clinical trials registries, CENTRAL (The Cochrane Library), MEDLINE, EMBASE, LILACS, CINAHL, SCOPUS, and Google Scholar], http://links.lww.com/PRSGO/A2.)
The electronic search retrieved a total of 1956 citations. Using the Endnote X3 software (Thomson Reuters, New York, NY), a total of 570 citations were found to be common among databases and were excluded. This resulted in a pool consisting of 1386 studies.
Twelve additional citations were added by reviewing the references of review articles related to neurolysis on diabetic patients, for a total of 1398 studies. Two of the authors independently reviewed the titles of the 1398 studies and found 70 potentially relevant studies related to neurolysis on the LEs of diabetic patients. Subsequently, 3 authors independently reviewed the abstracts and articles of these 70 studies and consequently included or excluded studies based on the inclusion and exclusion criteria (Table 1). Any discrepancies between the 3 refinements were thoroughly discussed among the corresponding authors, and a decision was made as to whether a study should be included or deselected. The title, abstract, and article-screening phases were supervised by the senior author (G.D.R.). Table 2 shows the reasons for exclusion of the deselected articles. Finally, after refining the list based on predefined criteria, 10 studies published from 1992 to 2012 were included. The search and screening algorithm are shown in Figure 1.
Table 1.
Inclusion and Exclusion Criteria
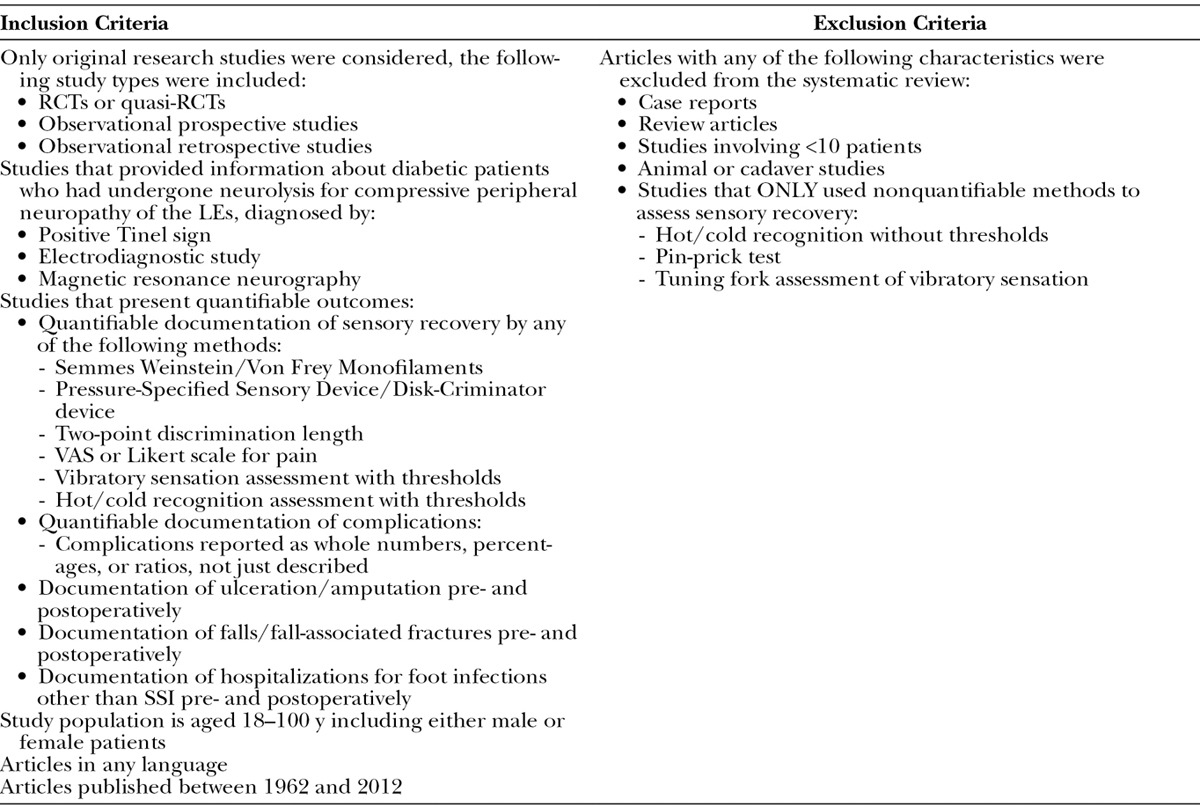
Table 2.
Reasons for Exclusion of Deselected Articles
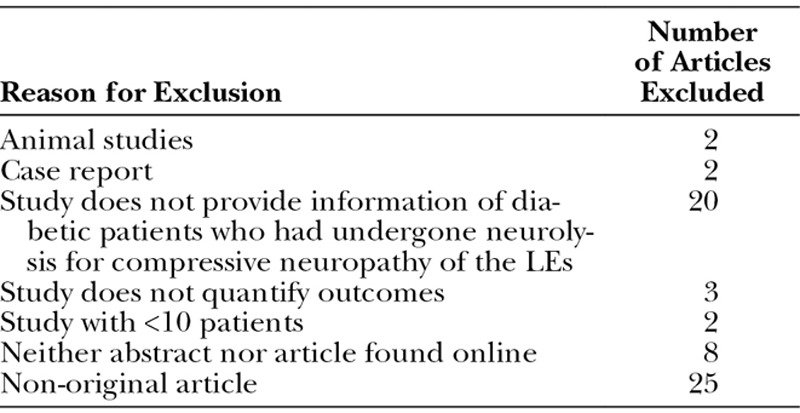
Fig. 1.
Search strategy and systematic assessment of relevant studies. The total pool for detailed analysis of abstracts and articles included 70 studies. Three of the authors independently reviewed all of the abstracts and articles of these 70 studies and consequently included 10 final studies for in-depth appraisal, data extraction, and meta-analysis.
In accordance with Johns Hopkins guidelines (which follow the US Code of Federal Regulations for the Protection of Human Subjects), institutional review board approval was not needed or sought for this systematic review because it only includes data from previously published studies.
Clinical Relevance and Methodological Quality Assessment
An adapted version of the clinical and methodological quality scales developed by Cho and Bero30,31 were considered appropriate for assessing the studies included in this systematic review. Both the clinical relevance and the methodological quality assessments were done independently by 4 of the authors. The mean scores were calculated per article and finally the overall clinical relevance and methodological quality mean scores were calculated as well. In this scale, a score of 100% represents the highest level of clinical relevance and methodological quality.
Meta-analysis
We summarized the data of the effects of neurolysis on patient outcomes using pooled means and odds ratios with 95% CIs calculated using inverse-variance weighting, adjusted for baseline characteristics. Patient outcomes of interest included pain relief, peripheral sensation recovery, and the incidence of ulcerations/amputations, falls, fall-associated fractures, and hospitalizations for foot infections other than SSI. Heterogeneity among studies reporting the outcomes of interest was assessed using forest plots and was found to be negligible; hence a fixed-effects meta-analytic model was employed. The meta-analysis was performed in R-2.15.2 with package Meta (R Foundation for Statistical Computing, Vienna, Austria).
Ethical Approval
This systematic review only includes de-identified patient information obtained from previously published studies. Thus, no institutional review board approval was needed or sought. This study conforms to the Declaration of Helsinki ethical principles for medical research.
RESULTS
Characteristics of Included Studies
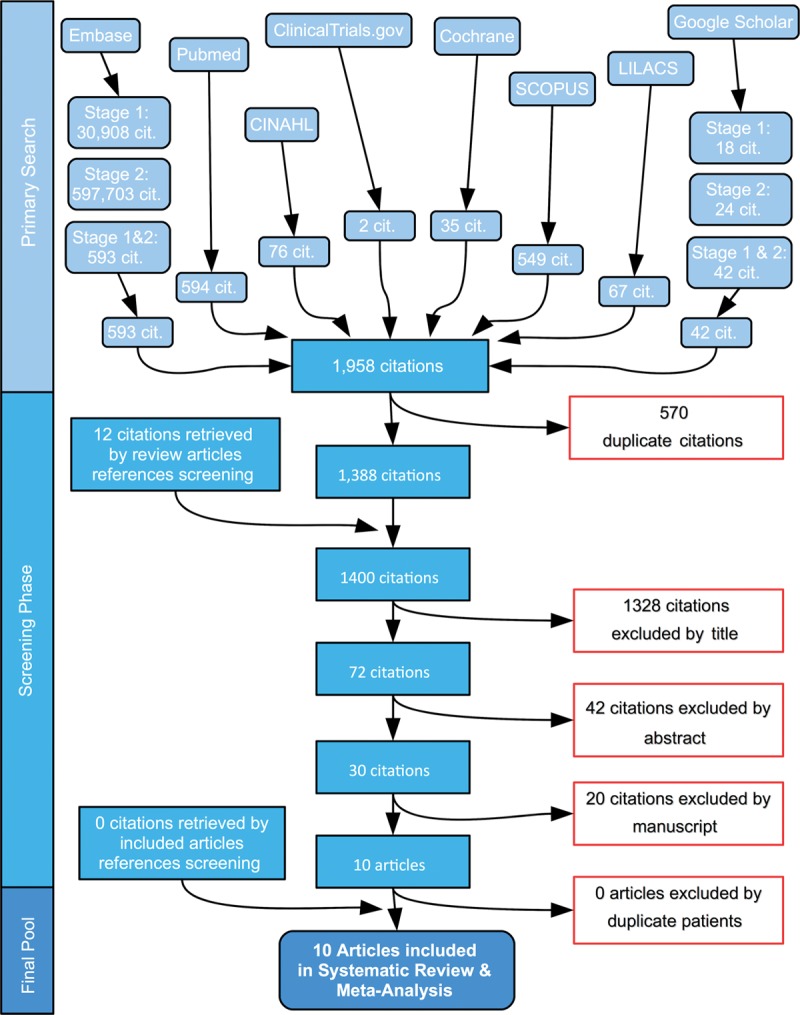
Our search strategy identified a total of 1956 citations. After a systematic assessment, 10 of these 1956 citations were considered relevant and were included for meta-analysis.8,10,13–20 Table 3 presents a summary of the included studies and their results. Although not a single randomized controlled trial (RCT) or quasi-RCT has been published, 2 currently ongoing RCTs were identified (ClinicalTrials.gov Identifier: NCT00703209 and NCT01006915). Both RCTs are currently recruiting participants and are expected to be completed by mid-2013. Of the 10 relevant observational studies, 4 were listed as prospective8,15,18,19 and 6 as retrospective.10,13,14,16,17,20 These 10 clinical series were found to have a mean clinical relevance score of 70% and a mean methodological quality score of 50% (Table 4). The overall study period extended from 1982 to 2012, and the pooled mean follow-up period was 16.8 ± 12.5 months.
Table 3.
Summary of the Included Studies and Their Results
Table 4.
Clinical Relevance and Methodological Quality Evaluation

Population Characteristics
A pooled number of 935 patients were included in the selected studies. Of these, 875 patients had diabetes and 1053 LEs underwent neurolysis for compressed nerves and were included in our meta-analysis.8,10,13–20 Four studies8,10,13,15 for a total of 130 patients reported the number of males (47 patients) and females (83 patients) in their study population. Four studies,8,10,15,17 for a total of 164 patients, reported the number of type 1 (73 patients) and type 2 (91 patients) diabetics in their study population.
Additionally, 4 studies8,13,15,17 for a total of 130 diabetic patients reported the mean duration of diabetes in their population, with a pooled mean of 13.87 ± 1.96 years. Six studies8,13,15–17,20 for a total of 214 patients reported the mean age of their population, the pooled mean age being 56.01 ± 7.07 years.
Diagnostic Methods
Regarding the method to diagnose nerve compression, 7 studies13,15–20 for a total of 762 patients relied on a positive Tinel sign to diagnose nerve compression. On the other hand, 3 studies8,10,14 for a total of 113 patients based the diagnosis of nerve compression on electrodiagnostic studies. None of the included studies based their diagnosis of nerve compression on magnetic resonance neurography findings. Five studies14,15,17–19 for a total of 745 patients used the Pressure-Specified Sensory Device, whereas 1 study13 for a total of 26 patients used the Disk-Criminator device to assess the degree of sensory impairment. One study16 including 12 patients assessed sensory impairment with both devices.
Location of Nerve Decompression
All the 1053 (100%) operated LEs had decompression of the tibial nerve at the tarsal tunnel and 1011 (96%) operated LEs had decompression of the common peroneal nerve at the fibular head and the deep peroneal nerve at the dorsum of the foot.8,10,13–20
Effect of Neurolysis on Pain
Three studies14,15,20 assessed improvement on the visual analog scale (VAS) for pain. A pooled analysis of postoperative vs preoperative VAS for pain for these 3 studies including a total of 69 LEs showed significant pain relief by >4 points on the VAS (95% CI: 4.04–6.77) after neurolysis (Fig. 2).
Fig. 2.
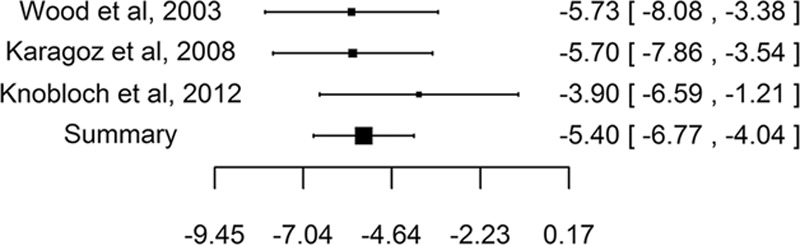
Forest plot of postoperative to preoperative VAS score difference. Outcome of interest: improvement on the VAS for pain. Pooled analysis of postoperative vs preoperative VAS for pain for these 3 studies including a total of 69 LEs showed significant pain relief by >4 points on the VAS (95% CI: 4.04–6.77) after neurolysis.
Four studies10,13,14,16 reported the percentage of postoperative pain relief. Pooled analysis of the 102 LEs included in these 4 studies showed that significant pain relief after neurolysis occurred in 91%, worsening of symptoms occurred in 5%, and no improvement in 4% of the LEs. The degree of improvement that constituted “significant pain relief” was not always defined in these 4 studies.
Effect of Neurolysis on Sensibility
Two studies13,14 assessed improvement on 2-point discrimination. A pooled analysis of postoperative vs preoperative 2-point discrimination for these 2 studies including a total of 59 LEs showed an improvement of 3.90 mm (95% CI: 0.13–7.67 mm) after neurolysis, from a mean of 16.16 ± 3.51 mm to a mean of 12.26 ± 3.92 mm (Fig. 3).
Fig. 3.
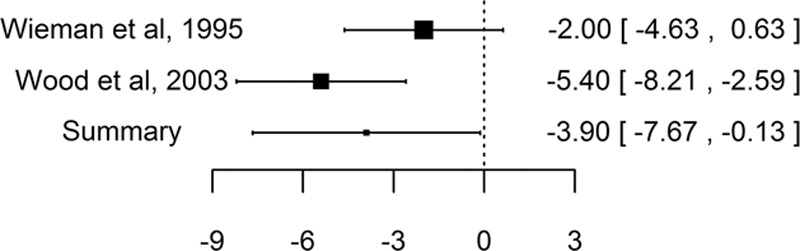
Postoperative to preoperative 2-point discrimination score difference. Outcome: improvement on 2-point discrimination. Pooled analysis of postoperative vs preoperative 2-point discrimination for these 2 studies including a total of 59 LEs showed an improvement of 3.90 mm (95% CI: 0.13–7.67 mm) after neurolysis, from a mean of 16.16 ± 3.51 mm to a mean of 12.26 ± 3.92 mm.
Furthermore, the improvement in sensibility was assessed by 4 studies.8,10,13,14 Pooled analysis of the 106 LEs included in these studies showed that sensibility improved significantly in 69% of the LEs. Similar to the pain scales, the precise degree of improvement that constitutes “significant improvement” was not always defined.
Effect of Neurolysis on Ulceration/Amputation
Two studies13,18 assessed the incidence of postoperative ulcerations. Pooled analysis of the 865 LEs included in these studies showed that the postoperative ulceration incidence was significantly reduced compared to preoperative incidence (odds ratio = 0.066, 95% CI = 0.026–0.164, P < 0.0001). With a pooled follow-up period of 27.7 ± 20.2 months, the pooled incidence of postoperative ulcerations for the 865 LEs included in these studies was 0.6%.
Furthermore, 4 studies assessed the postoperative incidence of LE amputations.13,17,18,20 After a pooled follow-up period of 19.9 ± 14.8 months, the pooled incidence of postoperative amputations for the 937 LEs included in these studies was determined to be 0.2%.
Effect of Neurolysis on Falls and Fall-associated Fractures
None of the included studies reported outcomes regarding neuropathy-associated falls and fall-associated fractures.
Effect of Neurolysis on Hospitalizations for Foot Infections
Only 1 study18 assessed the postoperative incidence of hospitalizations for foot infections (not SSI). Of 628 total patients, 4 patients (0.6%) were hospitalized postoperatively for foot infections other than SSI.
Neurolysis-related Complications
Complications were reported by 6 studies (Table 5).10,13–16,20 The overall complication rate for the 138 LEs included in these studies was 22%. Specifically, the incidence of wound dehiscence was assessed by 5 studies.10,14–16,20 The pooled incidence of wound dehiscence for the 112 LEs included in these studies was 15%. Additionally, the incidence of SSI was assessed by 4 studies.10,13,14,16 The pooled incidence of SSI after neurolysis for the 112 LEs included in these studies was 6%.
Table 5.
Neurolysis-related Reported Complications
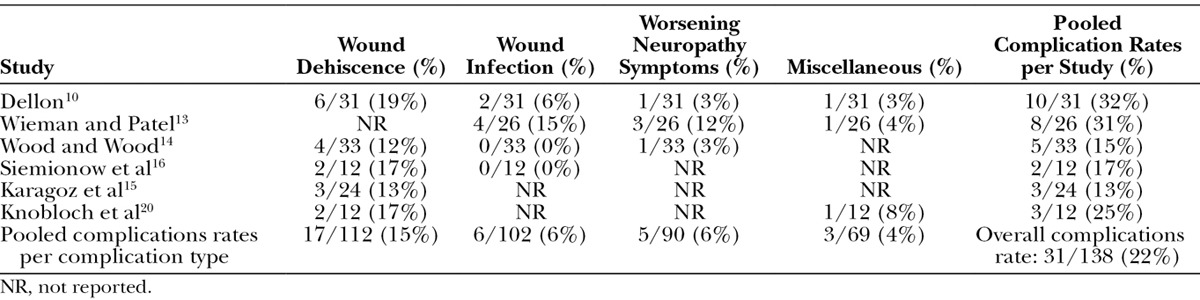
Finally, the occurrence of miscellaneous complications was reported by 3 studies.10,13,20 Dellon10 reported 1 patient having loss of superficial peroneal nerve requiring foot brace. Wieman and Patel13 reported 1 patient requiring dialysis and treatment for congestive heart failure, and Knobloch et al20 reported 1 episode of venous thromboembolism. The overall incidence of the aforementioned postoperative miscellaneous complications for the 69 patients included in these studies was 4%.
DISCUSSION
The lack of published RCTs or quasi-RCTs restricts the physician caring for diabetic patients with neuropathy to rely solely on the existing observational cohort studies when considering the possibility of neurolysis for this population. We have identified 2 currently ongoing RCTs that when published will help clarify the controversy regarding this intervention. In the meantime, the meta-analytic assessment of data from nonrandomized observational studies constitutes the highest level evidence available to the clinician dealing with diabetic patients with neuropathy.
A previous systematic review performed by Chaudhry et al23 assessed the effect of neurolysis on patients with diabetic symmetric distal polyneuropathy, including diabetic patients with and without superimposed compression. They found no evidence to support the use of neurolysis in the overall diabetic population with neuropathy. However, that study has a significant limitation, which is the inclusion of patients without evidence of superimposed nerve compression. The approach first described by Dellon10 was proposed for diabetic patients with neuropathy and associated superimposed compressed nerves. Thus, the present study aimed to address this specific issue by limiting the population to diabetic patients with evidence (positive Tinel sign or electrodiagnostic studies) of superimposed nerve compression of the LEs. We believe that the pooled diabetic population (875 diabetic patients and 1053 operated LEs) along with the pooled study (1982 to 2012) and follow-up (16.8 ± 12.5 mo) periods are adequate to analyze the predefined endpoints of interest of this systematic review.
Our meta-analysis of nonrandomized observational studies shows that neurolysis significantly improves pain, sensibility, and renders a low incidence of postoperative ulcerations/amputations. Assuming a placebo effect of 30%, a change of >1.5 VAS units represents a true difference between the postoperative scores and the preoperative scores. Additionally, a true difference between scores of 4.1 to 2.6 would be clinically significant because it would bring a patient from the “moderate” down into the “mild” pain category. Thus, the observed meta-analytic pooled improvement in pain by >4 points (95% CI: 4.04–6.77) on VAS is considered clinically and statistically significant. Furthermore, the fact that pooled analysis showed significant pain relief after neurolysis occurring in 91% of the operated LEs, with worsening of symptoms in 5% and no improvement in 4%, suggests that with regard to pain, this intervention has acceptable effectiveness. Improvement on sensibility was less dramatic with a pooled significant improvement on 2-point discrimination of 3.90 mm (95% CI: 0.13–7.67 mm), occurring on 69% of the operated LEs.
Importantly, the present meta-analysis of observational studies suggests that neurolysis significantly reduces (P < 0.0001) the incidence of postoperative ulcerations when compared to the preoperative period. This statistically significant reduction on postoperative ulcerations is more evident when the pooled incidence of postoperative ulcerations for the 865 operated LEs included in these studies (0.6%) after a pooled follow-up period of 27.7 ± 20.2 months is compared to the expected lifetime occurrence of ulceration in this population (15–25%).32–34 The most likely explanations for the reduction in postoperative ulcerations are the gain of protective sensation and trophic innervation of the skin, although these were not studied directly.
Furthermore, pooled data analysis showed that the postoperative incidence of amputations (0.2%) after a pooled follow-up period of 19.9 ± 14.8 months was significantly reduced compared to the expected incidence of postoperative amputations (10–15%).35 In the diabetic population, amputation of the LEs is the result of 2 phenomena that may exist independently or coexist: ischemia due to peripheral vascular disease vs loss of protective sensation (which exposes the patient to inadvertent trauma with the subsequent development of ulcerations, soft-tissue infection, and necrosis). All the patients in our study population had an ankle-brachial index >0.7, making ischemia an unlikely cause of amputation. Hence, the reduced postoperative incidence of amputations is likely due to the gain of protective sensation with a subsequent lower incidence of ulceration, infection, and soft-tissue necrosis. Alternatively, some sort of surgical selection bias might explain the reduction on the postoperative incidence of ulcerations because only patients without significant peripheral vascular disease were deemed candidates for neurolysis.
Unfortunately, none of the included studies assessed the effect of neurolysis on prevention of neuropathy-associated falls and fall-induced fractures, whereas only one assessed its effect on postoperative incidence of hospitalizations for foot infections other than SSI. This study found this incidence to be 0.6%, a significant decrease when compared to the 3.7% incidence at 2 years reported by previous studies on diabetics undergoing the best available, intensive primary foot care.36 This can be explained by the same mechanism that decreases the incidence of postoperative ulceration/amputation in this population.
Finally, but equally important, neurolysis for diabetic patients with compressed nerves of the LEs is associated with a 22% overall complication rate. Wound dehiscence (15%) is the most common complication after neurolysis, followed by SSI (6%) and miscellaneous complications (4%). All but one of the patients included in this systematic review and meta-analysis healed appropriately and did not progress to amputation of the extremities affected by delayed wound healing.
Although the present study includes the ideal patient population, the subjectivity inherent to some of the endpoints assessed (pain and sensibility) along with some methodological flaws of the included observational studies lower the strength of data interpretation and the conclusions reached. The overall clinical relevance score of the included articles (70%) clearly demonstrates the importance of the population and intervention. Nevertheless, the methodological quality score (50%) reflects how poor our attempts have been toward elucidating the real impact of this clinically relevant intervention. Furthermore, in these 10 included studies, the side of surgery (generally more symptomatic), the number of nerves operated upon, the endpoints, and the follow-up differed. Nine of the 10 included studies were not blinded,10,13–20 and 1 study was blinded only to the technician recording sensation measurements.8
All of the above justify the need for RCTs to further assess the effect of neurolysis on diabetic patients with compressed nerves of the LEs. To date, there are several ongoing RCTs worldwide; however, there is no consensus as to the ideal RCT design to determine the effect of neurolysis on this population. The following RCT designs could be considered:
Patients are randomized to receive either actual decompression surgery or sham operation; experimental group = unilateral neurolysis; control group = unilateral sham surgery; all patients will have unilateral surgery.
Patients are randomized to receive either actual decompression surgery or no operation; experimental group = unilateral neurolysis; control group = no surgery, optimized medical and podiatric care; half the patients will have unilateral surgery, and the half will receive no surgery.
Limbs are randomized to receive either actual decompression surgery or sham operation; experimental group = unilateral neurolysis; control group = contralateral sham surgery; all patients will have bilateral surgery.
Limbs are randomized to receive either actual decompression surgery or no operation; experimental group = unilateral neurolysis; control group = contralateral limb receives no surgery, but receives optimized medical and podiatric care; all patients will have unilateral decompression surgery, without contralateral surgery.
Sham surgery in the control group can be used to blind the patients and account for the placebo effect; study designs without sham surgery will not have blinding. Additionally, in study designs with a sham surgery, someone other than the surgeon should do the follow-up, such that both the patient and the evaluator would be blinded. The control and experimental groups should receive optimized medical and podiatric care during the preoperative and postoperative periods. Additional evaluations of the economic implications of this intervention are also warranted.
CONCLUSION
Meta-analytic assessment of observational (prospective and retrospective) studies shows that neurolysis significantly improves symptoms and natural history of diabetic patients with superimposed compressed nerves on the LE. RCTs and subsequent meta-analysis of RCTs have not yet been published and will further enlighten the use of neurolysis on diabetic patients with superimposed nerve compression.
Supplemental Digital Content
Footnotes
Poster presented at the 92nd Annual Meeting of the American Association of Plastic Surgeons, April 20–23, 2013, New Orleans, LA.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the Open Access Promotion Fund of the Johns Hopkins University Libraries
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Danaei G, Finucane MM, Lu Y, et al. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Pre-diabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 3.Caro JJ, Ward AJ, O’Brien JA. Lifetime costs of complications resulting from type 2 diabetes in the U.S. Diabetes Care. 2002;25:476–481. doi: 10.2337/diacare.25.3.476. [DOI] [PubMed] [Google Scholar]
- 4.Polydefkis M, Griffin JW, McArthur J. New insights into diabetic polyneuropathy. JAMA. 2003;290:1371–1376. doi: 10.1001/jama.290.10.1371. [DOI] [PubMed] [Google Scholar]
- 5.Dyck PJ, Kratz KM, Karnes JL, et al. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: the Rochester Diabetic Neuropathy Study. Neurology. 1993;43:817–824. doi: 10.1212/wnl.43.4.817. [DOI] [PubMed] [Google Scholar]
- 6.Coppini DV, Spruce MC, Thomas P, et al. Established diabetic neuropathy seems irreversible despite improvements in metabolic and vascular risk markers—a retrospective case-control study in a hospital patient cohort. Diabet Med. 2006;23:1016–1020. doi: 10.1111/j.1464-5491.2006.01934.x. [DOI] [PubMed] [Google Scholar]
- 7.Aszmann O, Tassler PL, Dellon AL. Changing the natural history of diabetic neuropathy: incidence of ulcer/amputation in the contralateral limb of patients with a unilateral nerve decompression procedure. Ann Plast Surg. 2004;53:517–522. doi: 10.1097/01.sap.0000143605.60384.4e. [DOI] [PubMed] [Google Scholar]
- 8.Aszmann OC, Kress KM, Dellon AL. Results of decompression of peripheral nerves in diabetics: a prospective, blinded study. Plast Reconstr Surg. 2000;106:816–822. doi: 10.1097/00006534-200009040-00010. [DOI] [PubMed] [Google Scholar]
- 9.Biddinger KR, Amend KJ. The role of surgical decompression for diabetic neuropathy. Foot Ankle Clin. 2004;9:239–254. doi: 10.1016/j.fcl.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 10.Dellon AL. Treatment of symptomatic diabetic neuropathy by surgical decompression of multiple peripheral nerves. Plast Reconstr Surg. 1992;89:689–697; discussion 698–699. [PubMed] [Google Scholar]
- 11.Hollis C. Treatment of diabetic neuropathy by decompression of the posterior tibial nerve. Plast Reconstr Surg. 2000;106:813–815. doi: 10.1097/00006534-200009020-00009. [DOI] [PubMed] [Google Scholar]
- 12.Tambwekar DS. Extended neurolysis of the posterior tibial nerve to improve sensation in diabetic neuropathic feet. Plast Reconstr Surg. 2001;108:1452–1453. doi: 10.1097/00006534-200110000-00072. [DOI] [PubMed] [Google Scholar]
- 13.Wieman TJ, Patel VG. Treatment of hyperesthetic neuropathic pain in diabetics. Decompression of the tarsal tunnel. Ann Surg. 1995;221:660–664; discussion 664–665. doi: 10.1097/00000658-199506000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wood WA, Wood MA. Decompression of peripheral nerves for diabetic neuropathy in the lower extremity. J Foot Ankle Surg. 2003;42:268–275. doi: 10.1016/s1067-2516(03)00313-2. [DOI] [PubMed] [Google Scholar]
- 15.Karagoz H, Yuksel F, Ulkur E, et al. Early and late results of nerve decompression procedures in diabetic neuropathy: a series from Turkiye. J Reconstr Microsurg. 2008;24:95–101. doi: 10.1055/s-2008-1064923. [DOI] [PubMed] [Google Scholar]
- 16.Siemionow M, Alghoul M, Molski M, et al. Clinical outcome of peripheral nerve decompression in diabetic and nondiabetic peripheral neuropathy. Ann Plast Surg. 2006;57:385–390. doi: 10.1097/01.sap.0000221979.13847.30. [DOI] [PubMed] [Google Scholar]
- 17.Valdivia JM, Dellon AL, Weinand ME, et al. Surgical treatment of peripheral neuropathy: outcomes from 100 consecutive decompressions. J Am Podiatr Med Assoc. 2005;95:451–454. doi: 10.7547/0950451. [DOI] [PubMed] [Google Scholar]
- 18.Dellon AL, Muse VL, Nickerson DS, et al. Prevention of ulceration, amputation, and reduction of hospitalization: outcomes of a prospective multicenter trial of tibial neurolysis in patients with diabetic neuropathy. J Reconstr Microsurg. 2012;28:241–246. doi: 10.1055/s-0032-1306372. [DOI] [PubMed] [Google Scholar]
- 19.Dellon AL, Muse VL, Scott ND, et al. A positive Tinel sign as predictor of pain relief or sensory recovery after decompression of chronic tibial nerve compression in patients with diabetic neuropathy. J Reconstr Microsurg. 2012;28:235–240. doi: 10.1055/s-0032-1306371. [DOI] [PubMed] [Google Scholar]
- 20.Knobloch K, Gohritz G, Vogt PM. [Surgical decompression of the lower leg in painful diabetic polyneuropathy]. Oper Orthop Traumatol. 2012;24:74–79. doi: 10.1007/s00064-011-0096-9. [DOI] [PubMed] [Google Scholar]
- 21.Upton AR, McComas AJ. The double crush in nerve entrapment syndromes. Lancet. 1973;2:359–362. doi: 10.1016/s0140-6736(73)93196-6. [DOI] [PubMed] [Google Scholar]
- 22.Dellon AL, Mackinnon SE. Chronic nerve compression model for the double crush hypothesis. Ann Plast Surg. 1991;26:259–264. doi: 10.1097/00000637-199103000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Chaudhry V, Russell J, Belzberg A. Decompressive surgery of lower limbs for symmetrical diabetic peripheral neuropathy. Cochrane Database Syst Rev. 2008;3:CD006152. doi: 10.1002/14651858.CD006152.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dyck PJ, Engelstad JK, Giannini C, et al. Resistance to axonal degeneration after nerve compression in experimental diabetes. Proc Natl Acad Sci U S A. 1989;86:2103–2106. doi: 10.1073/pnas.86.6.2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jaramillo J, Simard-Duquesne N, Dvornik D. Resistance of the diabetic rat nerve to ischemic inactivation. Can J Physiol Pharmacol. 1985;63:773–777. doi: 10.1139/y85-128. [DOI] [PubMed] [Google Scholar]
- 26.Seneviratne KN, Peiris OA. The effects of hypoxia on the excitability of the isolated peripheral nerves of alloxan-diabetic rats. J Neurol Neurosurg Psychiatry. 1969;32:462–469. doi: 10.1136/jnnp.32.5.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steiness I. Vibratory perception in diabetics during arrested blood flow to the limb. Acta Med Scand. 1959;163:195–205. doi: 10.1111/j.0954-6820.1959.tb10400.x. [DOI] [PubMed] [Google Scholar]
- 28.Steiness I. Influence of diabetic status on vibratory perception during ischaemia. Acta Med Scand. 1961;170:319–338. doi: 10.1111/j.0954-6820.1961.tb00245.x. [DOI] [PubMed] [Google Scholar]
- 29.Carayon A. [Fascicular neurolysis. Application to progressive peripheral nerve lesions. (Trauma, leprosy, tumors)]. J Chronic Dis. 1962;83:435–472. [PubMed] [Google Scholar]
- 30.Sanderson S, Tatt ID, Higgins JP. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol. 2007;36:666–676. doi: 10.1093/ije/dym018. [DOI] [PubMed] [Google Scholar]
- 31.Cho MK, Bero LA. Instruments for assessing the quality of drug studies published in the medical literature. JAMA. 1994;272:101–104. [PubMed] [Google Scholar]
- 32.Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293:217–228. doi: 10.1001/jama.293.2.217. [DOI] [PubMed] [Google Scholar]
- 33.Crawford F, Inkster M, Kleijnen J, et al. Predicting foot ulcers in patients with diabetes: a systematic review and meta-analysis. QJM. 2007;100:65–86. doi: 10.1093/qjmed/hcl140. [DOI] [PubMed] [Google Scholar]
- 34.Crawford F, McCowan C, Dimitrov BD, et al. The risk of foot ulceration in people with diabetes screened in community settings: findings from a cohort study. QJM. 2011;104:403–410. doi: 10.1093/qjmed/hcq227. [DOI] [PubMed] [Google Scholar]
- 35.Bartus CL, Margolis DJ. Reducing the incidence of foot ulceration and amputation in diabetes. Curr Diab Rep. 2004;4:413–418. doi: 10.1007/s11892-004-0049-x. [DOI] [PubMed] [Google Scholar]
- 36.Lavery LA, Armstrong DG, Wunderlich RP, et al. Risk factors for foot infections in individuals with diabetes. Diabetes Care. 2006;29:1288–1293. doi: 10.2337/dc05-2425. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


