Continuous positive airway pressure (CPAP) is the most common treatment modality for individuals with obstructive sleep apnea. However, for a subset of patients, the efficacy of oronasal CPAP is diminished by posterior displacement of the mandible by oronasal masks. This study investigated whether the use of a mandibular advancement device could enhance the effectiveness of CPAP delivered by oronasal mask. In addition, the authors investigated cephalometric features that may be associated with poor response to oronasal CPAP.
Keywords: Continuous positive airway pressure, CPAP mask, Mandibular advancement device, Obstructive sleep apnea
Abstract
BACKGROUND:
In some individuals with obstructive sleep apnea (OSA), oronasal continuous positive airway pressure (CPAP) leads to poorer OSA correction than nasal CPAP. The authors hypothesized that this results from posterior mandibular displacement caused by the oronasal mask.
OBJECTIVE:
To test this hypothesis using a mandibular advancement device (MAD) for mandibular stabilization.
METHODS:
Subjects whose OSA was not adequately corrected by oronasal CPAP at pressures for which nasal CPAP was effective were identified. These subjects underwent polysomnography (PSG) CPAP titration with each nasal and oronasal mask consecutively, with esophageal pressure and leak monitoring, to obtain the effective pressure (Peff) of CPAP for correcting obstructive events with each mask (maximum 20 cmH2O). PSG titration was repeated using a MAD in the neutral position. Cephalometry was performed.
RESULTS:
Six subjects with mean (± SD) nasal Peff 10.4±3.0 cmH2O were studied. Oronasal Peff was greater than nasal Peff in all subjects, with obstructive events persisting at 20 cmH2O by oronasal mask in four cases. This was not due to excessive leak. With the MAD, oronasal Peff was reduced in three subjects, and Peff <20 cmH2O could be obtained in two of the four subjects with Peff >20 cmH2O by oronasal mask alone. Subjects’ cephalometric variables were similar to published norms.
CONCLUSION:
In subjects with OSA with higher oronasal than nasal Peff, this is partially explained by posterior mandibular displacement caused by the oronasal mask. Combination treatment with oronasal mask and MAD may be useful in some individuals if a nasal mask is not tolerated.
Abstract
HISTORIQUE :
Chez certaines personnes atteintes d’apnée obstructive du sommeil (AOS), la pression positive continue (PPC) oronasale corrige moins bien l’AOS que la PPC nasale. Les auteurs postulent que cette situation est causée par un déplacement de la mandibule postérieure attribuable au masque oronasal.
OBJECTIF :
Vérifier cette hypothèse au moyen d’une orthèse d’avancée mandibulaire (OAM) pour stabiliser les mandibules.
MÉTHODOLOGIE :
Les chercheurs ont déterminé les sujets dont l’AOS n’était pas bien corrigée par PPC oronasale à des pressions auxquelles la PPC nasale était efficace. Trois sujets se sont soumis au titrage de la PPC pendant une polysomnographie (PSG) par le masque nasal et le masque oronasal consécutivement, sous monitorage de la pression œsophagienne et des fuites, afin d’obtenir la pression efficace (Peff) de la PPC pour corriger les événements obstructifs à l’aide de chaque masque (maximum de 20 cm H2O). Le titrage de la PSG a été repris au moyen d’une OAM en position neutre. Une céphalométrie a été effectuée.
RÉSULTATS :
Les chercheurs ont étudié six sujets présentant un Peff nasale moyenne (± ÉT) de 10,4±3,0 cm H2O. La Peff oronasale était plus élevée que la Peff nasale chez tous les sujets, les événements obstructifs se produisait encore par le masque oronasal à 20 cm H2O chez quatre patients. Cette situation n’était pas causée par une fuite excessive. Avec l’OAM, la Peff oronasale diminuait chez trois sujets, et une Peff inférieure à 20 cm H2O a pu être observée chez deux des quatre sujets ayant une Peff supérieure à 20 cm H2O par le seul masque oronasal. Les variables céphalométriques des sujets étaient similaires aux normes publiées.
CONCLUSION :
Chez des sujets atteints d’AOS dont la Peff était plus élevée par voie oronasale que par voie nasale, la situation s’explique partiellement par le déplacement de la mandibule postérieure causé par le masque oronasal. Un traitement combiné par le masque oronasal et l’OAM peut être utile chez certaines personnes qui ne tolèrent pas le masque nasal.
Obstructive sleep apnea (OSA) is a highly prevalent condition (1) that is associated with obesity and specific craniofacial features such as retrognathia, primarily in nonobese patients (2–4). OSA is best treated using continuous positive airway pressure (CPAP) (5). Mandibular advancement devices (MADs) are an alternative treatment in patients with mild-to-moderate OSA (6). A variety of interfaces are available for CPAP (7). Although nasal masks are most frequently used, oronasal masks, covering the nose and mouth, may be chosen due to patient preference, nasal obstruction or air leak through the mouth. In practice, nasal and oronasal masks are often used interchangeably, and are generally believed to be equally effective (7–9). There is, however, growing evidence suggesting that CPAP by oronasal mask is less effective at establishing airway patency in some individuals (10–13).
We hypothesized that, in individuals in whom oronasal CPAP is less effective than nasal CPAP at correcting upper airway obstruction, this results from posterior displacement of the mandible by the oronasal mask, exacerbating upper airway obstruction. The primary objective of the present study was to determine whether mandibular stabilization in a neutral position using a MAD can reduce the oronasal CPAP level required for effective OSA correction in such individuals. The secondary objective was to evaluate whether any anatomical features are associated with poor response to oronasal CPAP by analyzing cephalometric characteristics.
METHODS
Subjects
Subjects were recruited from the sleep clinic of a tertiary care academic hospital. OSA was diagnosed based on clinical findings and sleep testing (American Academy of Sleep Medicine level 1 or 3 study). Based on clinical or polysomnography (PSG) records, individuals whose OSA was not adequately corrected by oronasal CPAP at pressures for which nasal CPAP was effective, or in whom high CPAP pressures were reached using an oronasal mask without achieving correction of obstructive events, were identified. The present study was approved by the institutional ethics review board. Patients provided written informed consent.
Procedures
All subjects underwent overnight PSG twice. Each time, CPAP was titrated twice successively, once with a nasal mask and once with an oronasal mask. The order in which the masks were used was determined randomly for the first subject, alternating for subsequent subjects. The order of the first night was maintained for the second night. During the second PSG, CPAP titration was repeated using the MAD in the neutral position. All subjects also underwent cephalometry.
PSG and CPAP titration
Recording included standard electroencephalogram and electrooculogram leads, chin electromyography, electrocardiogram, snoring and body position (Sandman system, Covidien, USA). Oxygen saturation was measured using pulse oximetry (Oximax, Nellcor Puritan Bennett Ltd, USA). Respiratory efforts were measured via thoracic and abdominal piezoelectric belts. Respiratory flow was measured using a pneumotachograph (Hans Rudolph Inc, USA) directly connected to the mask. Pressure at the mask was measured via a pressure transducer (Validyne Engineering Corp, USA) connected through a catheter inserted into a tight opening in the mask shell. With the nasal mask, a thermistor was used to detect any airflow through the mouth. Intrathoracic pressure was recorded using an esophageal balloon (Cardinal Heath, USA) connected to a pressure transducer (Validyne, USA). Sleep scoring was performed according to Rechtschaffen and Kales (14).
For CPAP titration, the best-fitting size of nasal (Profile Lite, Philips-Respironics, USA) and oronasal (Disposable Non-vented Full Face Mask, ResMed, USA) masks were chosen for each subject by the same experienced respiratory therapist attending the PSG. Masks themselves were devoid of intentional leaks. The exhaust was distal to the pneumotachograph through a fenestrated connector piece. A BiPAP Synchrony connected to an Omnilab system (Philips-Respironics, USA) was used for titration. Titration was performed only during supine stage 2 sleep, by increasing the pressure by 1 cmH2O every 5 min until the effective pressure (Peff) was achieved for each type of mask or a maximal pressure of 20 cmH2O was reached. Peff was defined by achievement of stable tidal breathing with absence of snoring and inspiratory esophageal pressure stability. Total air leak was continuously measured by the Omnilab system. Higher-than-expected leak led to mask readjustment before any further titration.
MAD
Subjects had a set of upper and lower dental impressions made in alginate (Plastalgin ortho, Septodont, USA) with a bite (Imprint Bite, 3M ESPE, USA) taken in maximum intercuspidation. A MAD (orthèse O.R.M, Laboratoires Narval, Res Med, USA) was fabricated in a neutral position (without any advancement of the mandible). The MAD was adjusted in the clinic by the same orthodontist for proper fit and comfort with and without the CPAP masks in place.
Cephalometry
Each subject underwent a lateral cephalometric radiograph (Orthophos CD orthopantomograph, Siemens, Canada) taken in natural head position to perform measurements using the landmarks shown in Appendix 1. The tracings and measurements (15) were performed manually from the radiograph by the same orthodontist on two different occasions for all subjects to ensure reproducibility of measurements (Appendix 2).
RESULTS
Six subjects were identified between July 2008 and February 2009. Subject characteristics are presented in Table 1. None of the subjects had undergone any oropharyngeal surgery.
TABLE 1.
Subject characteristics and study results
| Subject | Sex | Age, years | Body mass index, kg/m2 | RDI | RDI supine | Peff without MAD, cmH2O | Peff with MAD, cmH2O | Mask used in first half of each night* | ||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Nasal | Oronasal | Nasal | Oronasal | |||||||
| 1 | Female | 64 | 20.9 | 27 | 41 | 10 | >20 | 11 | >20 | Nasal |
| 2 | Male | 52 | 25.7 | 20 | 26 | 11 | >20 | 12 | 18† | Oronasal |
| 3 | Male | 49 | 31.2 | 127 | 127 | 15 | >20 | 16 | >20 | Oronasal |
| 4 | Male | 65 | 32.9 | 83 | 72 | 12 | >20 | 12 | 19† | Oronasal |
| 5 | Male | 58 | 25.5 | 36 | 76 | 8 | 13 | 10 | 15 | Nasal |
| 6 | Male | 33 | 32.7 | 48 | 68 | 10 | 18 | 9 | 10† | Nasal |
| Mean ± SD | 53.5±11.9 | 28.1±4.9 | 56.8±40.1 | 68.3±34.8 | 10.4±3.0 | 16.3±5.4 | 11.1±2.6 | 15.9±4.7 | ||
The maximal available continuous positive airway pressure was 20 cmH2O;
Clinically significant improvement in oronasal effective pressure (Peff) for correction of obstructive respiratory events in supine stage 2 sleep with versus without the mandibular advancement device (MAD). RDI Respiratory disturbance index
Nasal Peff significantly correlated with the respiratory disturbance index (r=0.843; P=0.04). Using the oronasal mask, Peff was not attained in four patients, with obstructive events persisting at the maximal CPAP of 20 cmH2O (Figure 1). In the other two patients, oronasal Peff was higher than nasal Peff. Total air leak was similar with the two types of mask (Figure 2).
Figure 1).
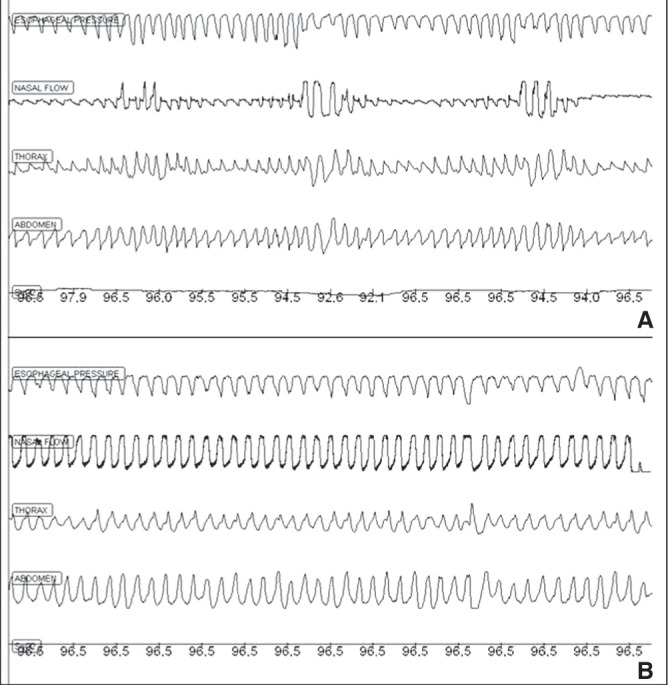
Example of polysomnographic recordings for subject 3 – oronasal versus nasal mask. Recordings with an oronasal mask at continuous positive airway pressure (CPAP) 20 cmH2O (A), and with a nasal mask at CPAP 15 cmH2O (B), both in supine stage 2 sleep. The epoch depicted is 180 s. Inspiration on the nasal flow signal is an upward deflection
Figure 2).
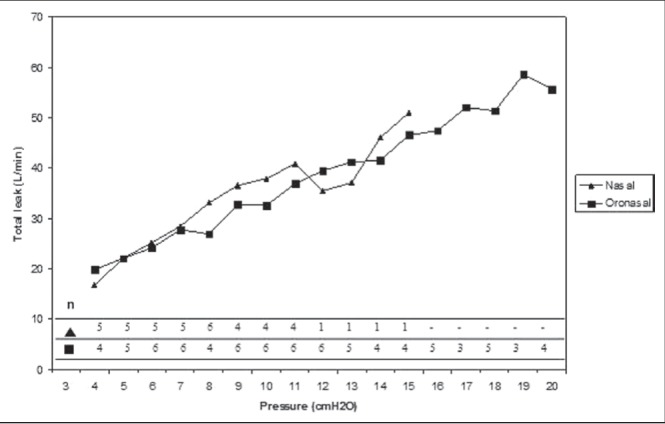
Total air leak during continuous positive airway pressure titration via nasal and oronasal mask (without mandibular advancement device). While leak was continuously available during polysomnography (PSG) titration on the Omnilab (Philips-Respironics, USA) system, it was not recorded as part of the PSG. Rather, it was documented intermittently as a comment; hence, it is not available for all subjects for all pressure levels
With mandibular stabilization, Peff by nasal mask remained within 1 cmH2O of the nasal Peff without MAD for five of the six subjects, suggesting no direct effect of the MAD on airway obstruction. In the other subject (subject 5), nasal Peff increased by 2 cmH2O (Table 1). Oronasal Peff decreased in three subjects, remained >20 cmH2O in two and increased in one (subject 5). Two individuals, who could not be treated by oronasal mask alone (Peff > 20 cmH2O), achieved oronasal Peff 19 cmH2O and 18 cmH2O, respectively, with the MAD (Figure 3).
Figure 3).
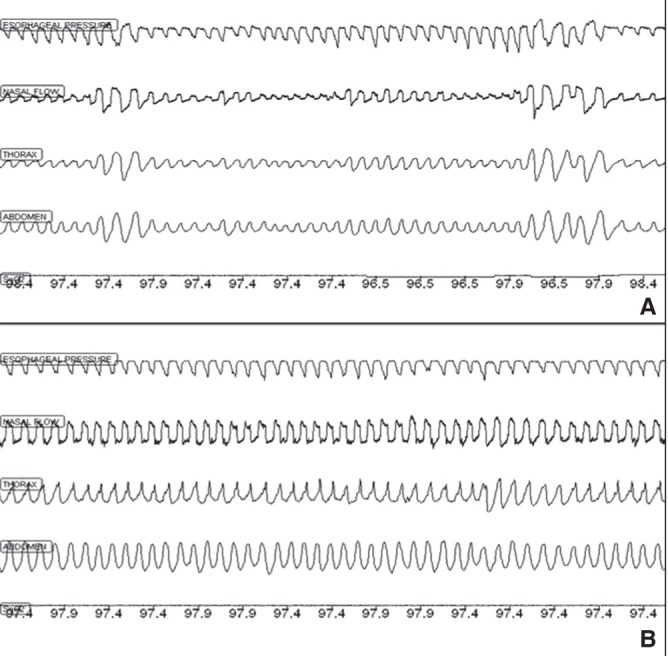
Example of polysomnographic recordings for subject 2 – oronasal mask with and without mandibular retention. Recordings with an oronasal mask alone at continuous positive airway pressure (CPAP) 20 cmH2O (A), and with an oronasal mask AND mandibular advancement device at CPAP 18 cmH2O (B), both in supine stage 2 sleep. The epoch depicted is 180 s. Inspiration on the nasal flow signal is an upward deflection
Cephalometric measurements were compared with published norms (16,17) by calculating Z scores. The group mean Z score for each measurement was >−1.65, suggesting no significant differences compared with the general population.
DISCUSSION
We identified and studied individuals with OSA whose Peff by oronasal mask was considerably higher compared with nasal Peff. In four patients, airway patency could not be established by oronasal mask even with CPAP 20 cmH2O, but CPAP by nasal mask resulted in stable breathing at ≤15 cmH2O. We used esophageal manometry to confirm the obstructive nature of the persistent respiratory events. Excessive air leak was not responsible for the difference between masks. Mandibular stabilization resulted in partial reduction of the higher oronasal Peff.
While oronasal masks were previously found to be effective for OSA treatment (8,9,11,18), several reports suggest they may not be equivalent, at least in some patients, to nasal masks. In one study, oronasal Peff was at least 2 cmH2O greater than nasal Peff in 46% of patients. In other studies, patient satisfaction and average nightly compliance were lower (18), and sleep was slightly more perturbed (8) with oronasal compared with nasal masks. It has been suggested that the higher Peff by oronasal mask is primarily due to excessive air leak (12). Our results suggest otherwise: any excessive leak led to immediate mask readjustment and leak was equivalent for both types of masks (Figure 2). Interestingly, in a physiological study, Smith et al (19) were unable to obtain airway patency by oronasal mask in their group of subjects. The discrepancy between the results from the study by Smith et al (19) and the prevalent use of oronasal CPAP has not been explained. A recent case report (10) described a patient in whom nasal CPAP was effective at a relatively low pressure whereas oronasal CPAP resulted in persistent airway obstruction with elevated pressures; endoscopy confirmed oropharyngeal airway obstruction.
Oronasal masks may cause or exacerbate upper airway obstruction directly by displacing the mandible posteriorly. We used a MAD in the neutral position in conjunction with oronasal CPAP to verify this hypothesis. MADs are a treatment option for mild-to-moderate OSA, particularly in nonobese patients with positional OSA (6). A response (significant partial or complete OSA correction) has been associated with an increase in the size of the pharyngeal lumen (20). We expected the MAD in neutral position to lower oronasal Peff to close to nasal Peff by preventing any posterior manibular displacement caused by the oronasal mask. Nasal Peff showed no or minimal change, confirming that there was no significant direct effect of the MAD on upper airway obstruction. With the oronasal mask, the MAD appeared to show partial benefit in three of the six patients. Hence, it appears that mandibular displacement accounted in part for the unfavourable effect of the oronasal mask, and that the mechanisms underlying poor oronasal mask effectiveness may differ among individuals. This may be related to different sites of obstruction. In the single case described by Schorr et al (10), endoscopy demonstrated posterior displacement of the base of the tongue with the oronasal mask. However, the level of obstruction may differ among individuals. Also, the MAD may not achieve the same effect in all cases. The literature suggests that patients with oropharyngeal collapse at baseline (21) or a smaller oropharynx (22) are more likely to respond to a MAD. However, a magnetic resonance imaging study showed that response to the MAD was primarily explained by expansion of the velopharyngeal volume in its lateral dimension (20). It should also be noted that the MAD itself may create a change in the position of the mandible by opening the occlusion, as well as crowding in the mouth with posterior displacement of the tongue. Both of these factors may exacerbate airway obstruction. These effects may explain the small increase in both nasal and oronasal Peff in one of our cases. However, because nasal Peff did not change significantly with the MAD for the remaining subjects, this effect is unlikely to be relevant in most cases.
With an oronasal mask, patients may mouth breathe and mouth opening may be responsible for mandibular position change, which can in turn affect upper airway patency because the position of the mandible (23) and tongue (24) are significant elements in OSA pathogenesis. Additionally, CPAP, when applied at the nose and mouth simultaneously, may fail to achieve a sufficient airway transmural pressure difference to establish airway patency (19). Mouth breathing can also increase upper airway surface tension, in turn worsening OSA (25). The MAD may then work by promoting mouth closure and tongue apposition to the palate. We did not ascertain mouth opening with the oronasal mask in our study. However, Sanders et al (9) showed that even with a mouthpiece in place to maintain the mouth open, oronasal CPAP remained effective at a level comparable with the nasal mask in their group of subjects, suggesting that mouth opening does not explain oronasal CPAP ineffectiveness, although the effect, once again, may vary among individuals and the mouthpiece itself may alter the physiology.
Concomitant use of the MAD in neutral position with CPAP was well tolerated in our subjects, although more long-term data will be needed to confirm our single-night findings. Nevertheless, concomitant use of CPAP with a MAD is feasible and could be a treatment option in patients who do not tolerate nasal CPAP but have very high or unattainable oronasal Peff.
While not assessed in the present study, the MAD with mandibular advancement may further reduce oronasal Peff, and likely also nasal Peff. This may be useful for treatment of severe OSA. It is conceivable that both a MAD and CPAP, used concomitantly, could be titrated for optimal OSA correction while minimizing the discomfort and adverse effects of excessive mandibular advancement and high pressure, respectively. This may lead to improved overall tolerance and, hence, adherence to OSA treatment.
A limitation of our study was that two titrations (one with each mask) were performed consecutively during a single night, once without and once with the MAD. To avoid any potential effect of differences in OSA from early to late night, we have alternated the type of mask used first (Table 1), and standardized our analyses to supine stage 2 sleep only. Additionally, while the technologist was aware of the results of the first titration while performing the second titration of each night, bias was minimized by using esophageal pressure monitoring to reduce the risk of overtitration.
We did not find any cephalometric variables in our subjects that could predict ineffectiveness of oronasal CPAP or its improvement with the MAD. Changes in airway dimensions may occur in the supine position (26), which we did not assess. Cephalometric data should be interpreted with caution given our limited sample size.
SUMMARY
Although the prevalence of the difference in nasal versus oronasal CPAP effectiveness and impact on CPAP adherence are unknown, it is important to be aware of this potential source of CPAP failure. Given the increasingly recognized adverse consequences of OSA, optimizing treatment effectiveness and adherence is an important goal for each patient. Our data suggest that it may be feasible to combine therapy using a MAD with oronasal CPAP in individuals intolerant to CPAP by nasal mask.
Acknowledgments
The authors acknowledge Dr Francois Bellemare for his help in setting up the study protocol. They extend their thanks to Magalie Valières who performed the titration studies, and to Anne-Marie Laurin, Chief Technician of the Sleep Laboratory of the Centre-Hospitalier Universitaire de Montreal.
APPENDIX 1. Lateral cephalometric landmarks
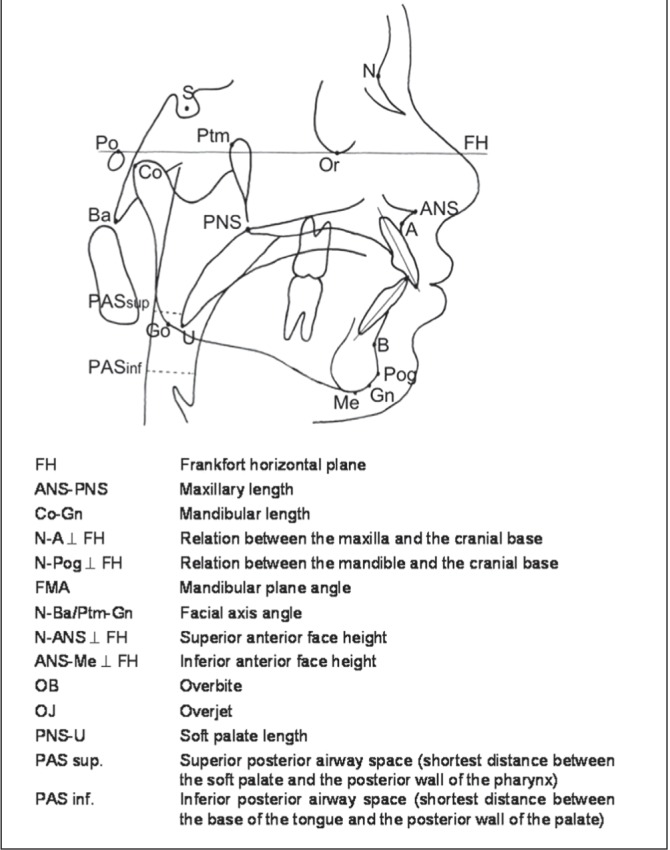
APPENDIX 2. Cephalometric variables (see Appendix 1 for landmarks)
| FH | Frankfort horizontal plane | Plane built from the line joining porion (Po) and orbital (Or) points |
| Co-A | Maxillary length | Distance in mm between condylion (Co) and subspinal (A) points |
| ANS-PNS | Maxillary length | Distance in mm between the anterior nasal spine (ANS) and the posterior nasal spine (PNS) points |
| Co-Gn | Mandibular length | Distance in mm between condylion (Co) and gnation (Gn) points. |
| SNA | Antero-posterior position of the maxilla | Angle formed by nasion (N), sella (S) and subspinal (A) points |
| SNB | Antero-posterior position of the mandible | Angle formed by nasion (N), sella (S) and supramental (B) points |
| ANB | Antero-posterior relation between the maxilla and the mandible | Angle formed by subspinal (A), nasion (N) and supramental (B) points |
| N-A ┴ FH | Antero-posterior position of the maxilla | Distance in mm between a line perpendicular to FH plane at nasion (N) point and subspinal (A) point. |
| N-Pog ┴ FH | Antero-posterior relation of the mandible | Distance in mm between a line perpendicular to FH plane at nasion (N) point and pogonion (Pog) point |
| FMA | Mandibular plane angle | Angle formed between the mandibular plane and FH plane Mandibular plane: Line joining gnation (Gn) and menton (Me) points |
| N-Ba/Ptm-Gn | Facial axis angle | Angle formed between the line joining basion (Ba) and nasion (N) points and the line joining sella (S) and gnation (Gn) points |
| N-ANS ┴ FH | Upper anterior face height | Distance in mm between nasion (N) and anterior nasal spine (ANS) points measured perpendicular to the FH plane |
| ANS-Me ┴ FH | Lower anterior face height | Distance in mm between anterior nasal spine (ANS) point and menton (Me) point measured perpendicular to the FH plane |
| I/SN | Upper incisor angulation | Angle between the long axis of the most anterior upper incisor and the line joining sella (S) and nasion (N) points |
| OB | Overbite | Vertical distance in mm from the tip of the lower incisor to the tip of the upper incisor |
| OJ | Overjet | Horizontal distance in mm from the labial of the lower incisor to the labial of the upper incisor |
| PNS-U | Soft palate length | Distance in mm between posterior nasal spine (PNS) and uvula (U) points |
| PAS mid. | Posterior airway space at oropharynx level | Shortest distance in mm between the soft palate and the posterior wall of the pharynx |
| PAS inf. | Posterior airway space at laryngopharynx level | Shortest distance in mm between the base of the tongue and the posterior wall of the pharynx |
Footnotes
FUNDING: This study was funded by the Foundation of the Centre Hospitalier Universitaire de Montreal.
DISCLOSURES: The authors have no financial disclosures or conflicts of interest to declare.
REFERENCES
- 1.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 2.Chi L, Comyn FL, Mitra N, et al. Identification of craniofacial risk factors for obstructive sleep apnoea using three-dimensional MRI. Eur Respir J. 2011;38:348–58. doi: 10.1183/09031936.00119210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mayer P, Pepin JL, Bettega G, et al. Relationship between body mass index, age and upper airway measurements in snorers and sleep apnoea patients. Eur Respir J. 1996;9:1801–9. doi: 10.1183/09031936.96.09091801. [DOI] [PubMed] [Google Scholar]
- 4.Sakakibara H, Tong M, Matsushita K, Hirata M, Konishi Y, Suetsugu S. Cephalometric abnormalities in non-obese and obese patients with obstructive sleep apnoea. Eur Respir J. 1999;13:403–10. doi: 10.1183/09031936.99.13240399. [DOI] [PubMed] [Google Scholar]
- 5.Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29:375–80. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 6.Kushida CA, Morgenthaler TI, Littner MR, et al. Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances: An update for 2005. Sleep. 2006;29:240–3. doi: 10.1093/sleep/29.2.240. [DOI] [PubMed] [Google Scholar]
- 7.Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006:CD005308. doi: 10.1002/14651858.CD005308.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prosise GL, Berry RB. Oral-nasal continuous positive airway pressure as a treatment for obstructive sleep apnea. Chest. 1994;106:180–6. doi: 10.1378/chest.106.1.180. [DOI] [PubMed] [Google Scholar]
- 9.Sanders MH, Kern NB, Stiller RA, Strollo PJ, Jr, Martin TJ, Atwood CW., Jr CPAP therapy via oronasal mask for obstructive sleep apnea. Chest. 1994;106:774–9. doi: 10.1378/chest.106.3.774. [DOI] [PubMed] [Google Scholar]
- 10.Schorr F, Genta PR, Gregorio MG, Danzi-Soares NJ, Lorenzi-Filho G. Continuous positive airway pressure delivered by oronasal mask may not be effective for obstructive sleep apnoea. Eur Respir J. 2012;40:503–5. doi: 10.1183/09031936.00145111. [DOI] [PubMed] [Google Scholar]
- 11.Teo M, Amis T, Lee S, Falland K, Lambert S, Wheatley J. Equivalence of nasal and oronasal masks during initial CPAP titration for obstructive sleep apnea syndrome. Sleep. 2011;34:951–5. doi: 10.5665/SLEEP.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bakker JP, Neill AM, Campbell AJ. Nasal versus oronasal continuous positive airway pressure masks for obstructive sleep apnea: A pilot investigation of pressure requirement, residual disease, and leak. Sleep Breath. 2012;16:709–16. doi: 10.1007/s11325-011-0564-3. [DOI] [PubMed] [Google Scholar]
- 13.Ebben MR, Oyegbile T, Pollak CP. The efficacy of three different mask styles on a PAP titration night. Sleep Med. 2012;13:645–9. doi: 10.1016/j.sleep.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Rechtschaffen A, Kales A, editors. Brain Research Institute, University of California. Los Angeles: 1968. A manual of standardized terminology, techniques and scoring system of sleep stages in human subjects. [Google Scholar]
- 15.McNamara JA., Jr A method of cephalometric evaluation. Am J Orthod. 1984;86:449–69. doi: 10.1016/s0002-9416(84)90352-x. [DOI] [PubMed] [Google Scholar]
- 16.Mostafiz W, Dalci O, Sutherland K, et al. Influence of oral and craniofacial dimensions on mandibular advancement splint treatment outcome in patients with obstructive sleep apnea. Chest. 2011;139:1331–9. doi: 10.1378/chest.10-2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ng AT, Darendeliler MA, Petocz P, Cistulli PA. Cephalometry and prediction of oral appliance treatment outcome. Sleep Breath. 2012;16:47–58. doi: 10.1007/s11325-011-0484-2. [DOI] [PubMed] [Google Scholar]
- 18.Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53:290–2. doi: 10.1136/thx.53.4.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith PL, Wise RA, Gold AR, Schwartz AR, Permutt S. Upper airway pressure-flow relationships in obstructive sleep apnea. J Appl Physiol. 1988;64:789–95. doi: 10.1152/jappl.1988.64.2.789. [DOI] [PubMed] [Google Scholar]
- 20.Chan AS, Sutherland K, Schwab RJ, et al. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 2010;65:726–32. doi: 10.1136/thx.2009.131094. [DOI] [PubMed] [Google Scholar]
- 21.Ng AT, Qian J, Cistulli PA. Oropharyngeal collapse predicts treatment response with oral appliance therapy in obstructive sleep apnea. Sleep. 2006;29:666–71. [PubMed] [Google Scholar]
- 22.Liu Y, Lowe AA, Fleetham JA, Park YC. Cephalometric and physiologic predictors of the efficacy of an adjustable oral appliance for treating obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2001;120:639–47. doi: 10.1067/mod.2001.118782. [DOI] [PubMed] [Google Scholar]
- 23.Meurice JC, Marc I, Carrier G, Series F. Effects of mouth opening on upper airway collapsibility in normal sleeping subjects. Am J Respir Crit Care Med. 1996;153:255–9. doi: 10.1164/ajrccm.153.1.8542125. [DOI] [PubMed] [Google Scholar]
- 24.Cartwright RD, Samelson CF. The effects of a nonsurgical treatment for obstructive sleep apnea. The tongue-retaining device. JAMA. 1982;248:705–9. [PubMed] [Google Scholar]
- 25.Verma M, Seto-Poon M, Wheatley JR, Amis TC, Kirkness JP. Influence of breathing route on upper airway lining liquid surface tension in humans. J Physiol. 2006;574:859–66. doi: 10.1113/jphysiol.2005.102129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pae EK, Lowe AA, Sasaki K, Price C, Tsuchiya M, Fleetham JA. A cephalometric and electromyographic study of upper airway structures in the upright and supine positions. Am J Orthod Dentofacial Orthop. 1994;106:52–9. doi: 10.1016/S0889-5406(94)70021-4. [DOI] [PubMed] [Google Scholar]


