Abstract
BACKGROUND:
The treatment of celiac disease is a strict, life-long gluten-free (GF) diet. This diet is complex and can be challenging. Factors affecting adherence to the GF diet are important to identify for improving adherence.
OBJECTIVE:
To identify factors that inhibit or improve adherence to a GF diet in children with celiac disease.
METHODS:
Patients (<18 years of age) with biopsy-confirmed celiac disease followed by the gastroenterology service at a tertiary care paediatric institution were surveyed using a mailed questionnaire. Factors influencing adherence to a GF diet were scored from 1 to 10 based on how often they were problematic (1 = never, 10 = always). Parents of patients <13 years of age were instructed to complete the survey with their child. Adolescents ≥13 years of age were asked to complete the survey themselves.
RESULTS:
Of 253 subjects, 126 completed the survey; the median age was 12 years (range two to 18 years). Forty percent were adolescents. Overall, participants reported good adherence at home and school, but lower adherence at social events. Adolescents reported lower adherence compared with parents. Availability of GF foods and cost were the most significant barriers. Other factors identified to help with a GF diet included education for schools/restaurants and improved government support.
CONCLUSIONS:
Availability, cost and product labelling are major barriers to adherence to a GF diet. Better awareness, improved labelling and income support are needed to help patients.
Keywords: Adherence, Celiac disease, Compliance, Gluten-free diet
Abstract
HISTORIQUE :
Le traitement de la maladie cœliaque consiste à suivre un régime sans gluten (RSG) rigoureux jusqu’à la fin de ses jours. Ce régime est complexe et peut-être difficile à respecter. Il est important de déterminer les facteurs influant sur l’adhérence au RSG pour améliorer cette adhérence.
OBJECTIF :
Déterminer les facteurs qui inhibent ou améliorent l’adhérence au RSG chez les enfants atteints de la maladie cœliaque.
MÉTHODOLOGIE :
À l’aide d’un questionnaire envoyé par la poste, les chercheurs ont sondé les patients (de moins de 18 ans) atteints d’une maladie cœliaque confirmée par biopsie et suivis au service de gastroentérologie d’un établissement pédiatrique de soins tertiaires. Les facteurs influant sur l’adhérence à un RSG ont été classés de un à dix selon la fréquence à laquelle ils causaient problème (1 = jamais, 10 = toujours). Les parents des patients de moins de 13 ans étaient invités à remplir le questionnaire avec l’enfant. Ceux de 13 ans et plus étaient invités à le remplir seuls.
RÉSULTATS :
Sur 253 sujets, 126 ont rempli le sondage. Ils avaient 12 ans d’âge médian (plage de deux à 18 ans). Quarante pour cent étaient des adolescents. Dans l’ensemble, les participants signalaient une bonne adhérence à la maison et à l’école, mais une adhérence plus faible lors d’événements sociaux. Les adolescents déclaraient une adhérence plus faible que les parents. L’offre d’aliments sans gluten et le coût étaient les principaux obstacles. D’autres facteurs ont été signalés pour faciliter un RSG, y compris l’éducation dans les écoles et les restaurants et un meilleur soutien gouvernemental.
CONCLUSIONS :
L’offre, le coût et l’étiquetage des produits sont d’importants obstacles à l’adhérence à un RSG. Une meilleure sensibilisation, un meilleur étiquetage et le soutien du revenu s’imposent pour aider les patients.
Celiac disease is an immune-mediated enteropathy in which ingestion of gluten, a protein found in wheat, barley and rye, leads to small intestinal villous atrophy in genetically susceptible individuals (1). Celiac disease affects approximately 1% of the population, making it one of the most common chronic gastrointestinal disorders (2,3).
The only treatment for celiac disease is strict, life-long adherence to a gluten-free (GF) diet. A GF diet is not only complex and costly, but can also be restrictive in social situations such as dining out, birthdays, camping, etc (4). Cross contamination with gluten is a major issue because wheat is ubiquitous in the Western diet. Poorly treated celiac disease can lead to complications including nutritional deficiencies such as anemia and osteoporosis, growth failure, infertility, development of other autoimmune disorders and malignancy (5).
As the number of patients diagnosed with celiac disease increases, the challenges of a GF diet will become more common. There is limited information on barriers to adhering to a GF diet, especially the effects of patient age or geographical location (ie, smaller versus larger communities). The identification of factors that affect adherence would aid in the development of strategies to improve a patient’s ability to maintain a strict GF diet. This will not only help symptoms but will also reduce the risk of complications.
The aim of the present study was to investigate adherence to a GF diet among children with celiac disease, and to identify factors that inhibit or improve adherence.
METHODS
All patients <18 years of age with biopsy-confirmed celiac disease followed by the gastroenterology service at a tertiary care, university-affiliated paediatric institution were surveyed using a mailed questionnaire. As standard clinical care, all patients had received counselling about a GF diet from a registered dietitian. The patients were from the three Canadian Maritime provinces (Nova Scotia, New Brunswick and Prince Edward Island). All potential cases of celiac disease from these provinces are referred for biopsy confirmation to the only paediatric tertiary care centre in the Maritimes, located in Nova Scotia. This ensured the capture of essentially all paediatric cases of celiac disease in the region.
The survey questionnaire was developed following a review of the literature identifying areas of daily living that may be impacted by a GF diet. The process also included consultation with paediatric gastroenterologists and dietitians who provide counselling regarding a GF diet. The survey included items to assess demographic characteristics, time since diagnosis, comorbid conditions such as type I diabetes, geographical location, family size, affected family members and number of family members on a GF diet. Factors affecting eating in social situations, such as restaurants, school/daycare, travel and social life, over the past year were investigated. The factors were scored from 1 to 10 based on how often they were problematic (1 = never, 10 = always). For the study, adherence was defined as not knowingly ingesting gluten-containing products. Participants were also asked if they were aware of the tax benefit available and if they had ever applied for it. The survey concluded with open-ended questions, for which patients and their families could comment on any other barriers to adherence to a GF diet and provide suggestions for improving their quality of life. The questionnaire was pretested on a sample of patients for feasibility.
Parents of patients <13 years of age were instructed to complete the survey with their child. Adolescents ≥13 years of age were asked to complete the survey themselves. A question was included in the survey to confirm who completed the form. Forms received were not coded or identified, thus maintaining complete anonymity of the participants. Only one mailing was performed.
The study was approved by the Research Ethics Board at Dalhousie University (Halifax, Nova Scotia).
Statistical analysis
Questionnaire items regarding compliance and factors that may contribute to difficulty maintaining a GF diet were analyzed using independent t tests for two-group comparisons of responses that were normally distributed (eg, comparison of the overall difficulty of maintaining a GF diet between male and female sexes) and ANOVAs for comparisons of normally distributed data among >2 groups (eg, comparison of overall difficulty among different age groups). When the variables were not normally distributed, non-parametric measures (eg, Mann-Whitney U test for two groups and Kruskal-Wallis test for >2 groups) were used. Wilcoxon rank sum tests were used to examine responses to questions about difficulty with adherence in different settings (eg, home versus school). The relationships between years since diagnosis and both the degree of difficulty with adherence and the degree to which areas of functioning are affected by a GF diet were examined using bivariate correlations (Pearson’s r).
RESULTS
A total of 253 subjects with celiac disease were contacted for the study. The survey was completed by 50% of subjects (126 of 253). Forty percent (n=51) of questionnaires were completed by adolescent patients (13 to 18 years of age) themselves and the remainder were completed by parents or other primary caregivers for younger children. The demographic characteristics of the participants are presented in Table 1. Approximately 8% of responders also had type 1 diabetes. Most families (63%) included only one individual on a GF diet, while 8% included the entire family on the diet.
TABLE 1.
Demographic characteristics of study participants (n=126)
| Characteristic | |
|---|---|
| Age, years, median (range) | 12 (2–18) |
| Sex | |
| Male | 38 (32) |
| Female | 81 (68) |
| Years since diagnosis, median (range) | 3 (0.5–15) |
| Family members with celiac disease | |
| 1 | 85 (68) |
| 2 | 26 (21) |
| >2 | 14 (11) |
| Family members on a gluten-free diet | |
| 0 | 2 (2) |
| 1 | 79 (63) |
| 2 | 27 (21) |
| >2 | 18 (14) |
| Province of residence | |
| Nova Scotia | 81 (65) |
| New Brunswick | 27 (21) |
| Prince Edward Island | 17 (14) |
| Community size (population) | |
| <10,000 | 36 (29) |
| 10,000 to <50,000 | 26 (22) |
| 50,000 to 100,000 | 10 (8) |
| >100,000 | 36 (29) |
| Not known | 15 (12) |
Data presented as n (%) unless otherwise indicated
Knowledge about the Canada Revenue Agency’s tax benefit was reported by 82.5% of respondents and 41% had applied for it previously.
Adherence to a GF diet
The cumulative rates of adherence in various situations of everyday living are shown in Figure 1.
Figure 1).
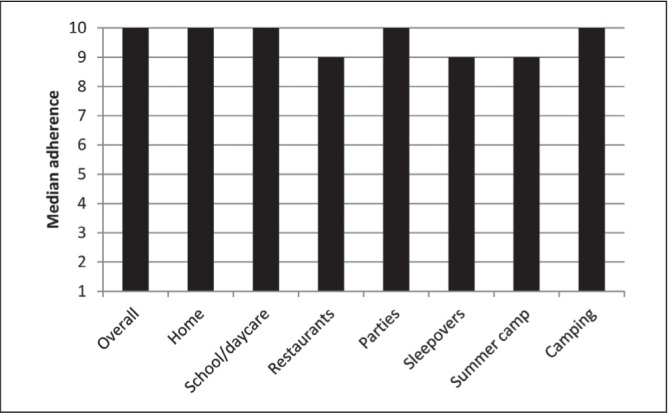
Median adherence to a gluten-free diet according to location (1 = never, 10 = always)
Overall adherence to a GF diet was good, with a median score of 10 (1 = never, 10 = always). The interquartile range (IQR) was 5 to 10. Adherence was best at home and school, and somewhat lower during certain social events including sleepovers and summer camps.
Figure 2 presents a comparison of responses provided by adolescents themselves and parents of younger patients. There was a significantly lower overall adherence reported by adolescents (P<0.01). Adolescents had a median overall adherence of 9 (IQR 3 to 10) compared with 10 (IQR 9 to 10) in younger children according to parents (Mann Whitney P=0.009). Adherence was also comparatively lower among adolescents while dining in restaurants (P=0.02)
Figure 2).
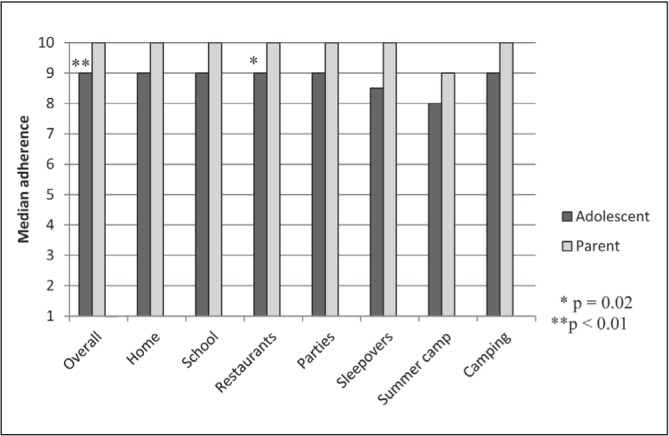
Overall median adherence and median adherence according to location to a gluten-free diet reported by parents (n=76) and adolescent patients (n=50) (1 = never, 10 = always)
There was no significant correlation between years since diagnosis and ratings of adherence to a GF diet or overall difficulty with GF foods.
Barriers to adherence
Availability of GF foods was, by far, the most significant barrier to overall adherence, especially at school (median 9) and in restaurants (median 8). Respondents also believed that restaurants had limited choices and knowledge of a GF diet. Cost (median 7) and labelling (median 6) were also substantial obstacles. Taste was of moderate importance (median 5) across locations. Social pressure was not a substantial barrier, although it did vary according to location, being lowest at home (median 1) and highest at school (median 3).
The majority of respondents were female (68%), but there were no significant differences in responses according to sex (P>0.05 for all barriers). A subanalysis was performed to determine the effect of age by dividing the respondents into three age groups: <5 years of age (n=6); five to 13 years of age (n=68); and >13 years of age (n=49). All barriers were similar across age groups (P>0.05).
Adherence to a GF diet according to province showed an overall median adherence of 10 (IQR 5 to 10) for Nova Scotia, 10 (IQR 3 to 10) for New Brunswick and 9 (IQR 3.25 to 10) for Prince Edward Island. There was no significant difference between provinces (P=0.47).
Data from all provinces were combined and the effect of community size was examined. The size of the community did not significantly affect adherence to a GF diet. However, there was a suggestion of lower adherence in smaller communities. The median adherence was 9 (IQR 3 to 10) in communities of <10,000, 10 (IQR 3.5 to 10) in communities of 10,000 to <50,000, 10 (IQR 9 to 10) in communities of 50,000 to 100,000 and 10 (IQR 9 to 10) in communities of >100,000. Barriers to adherence, including availability and cost, did not vary significantly according to community size (P>0.05 for all).
Impact of a GF diet
Effects of a GF diet on areas of functioning are presented in Figure 3. Most participants (70%) reported that the GF diet positively affected their health. A sample of participants’ comments about the impact of diet is presented in Table 2.
Figure 3).
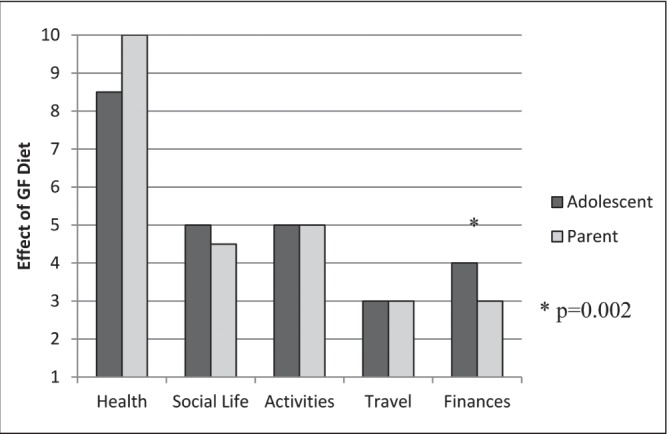
Effects of a gluten-free (GF) diet on areas of functioning reported by parents (n=76) and adolescent patients (n=50). The effect was considered neutral if it was equal to 5, positive if >5 and negative if <5
TABLE 2.
A sample of quotations from the respondents regarding positive and negative effects of a gluten-free diet
| Positive effects of a GF diet | Negative effects of a gluten-free diet |
|---|---|
| “He feels so much better and is growing and looking well.” | “We will not eat at restaurants because we do not want to put our child’s health in the hands of a stranger.” |
| “Our son seems to be much healthier than other kids. Sick less often. Also seems to be stronger and bigger and faster than other kids.” | “Not very many items on gluten-free menus cater to children. Most often they are geared for adults.” |
| “Kids bully those who are different.” | |
| “I get embarrassed because I have to eat different food at hockey tournaments and parties.” | |
| “Religion – I am Catholic and allergic to the host.” (bread or wafer consecrated in the Eucharist) |
The GF diet negatively affected family finances for 70% (n=87) of participants. Travel was negatively affected for 62% (n=78) and 47% (n=59) reported that their social life was also negatively affected. When impact was compared between adolescent respondents and parents of younger children (Figure 3), results were similar except for effect on finances, which were more negatively affected according to parents of younger children than adolescents (P=0.002).
What would improve living with a GF diet?
When asked what would support better adherence to a GF diet, participants listed improving the variety and taste of GF products as the most important. The support of family members and the Canadian Celiac Association (a national patient support/advocacy organization) were also identified as being helpful. Many respondents commented that although the taste of GF products has improved, it remains an issue. Parents expressed their concern that GF products often contain more fat and/or sugar and, hence, may be inappropriate for children.
When asked what would make it easier to eat GF food, increased availability (n=40), lower cost (n=48) and education for schools/restaurants (n=39) were noted. In addition, participants suggested certification for restaurants and vendors to prove knowledge of GF dietary requirements. More flexible financial support from government agencies and insurance companies was also suggested. Many participants also expressed the wish that alternative treatments, such as pills or a vaccine, that could ‘cure’ the condition were available.
DISCUSSION
The fact that a GF diet is protective against adverse outcomes and can alleviate symptoms should be sufficient to motivate individuals to maintain adherence (6). However, this is not always the case. Our study adds to the growing body of literature documenting the difficulty patients experience in adhering to a GF diet (6–10). While much research has focused on rates of adherence and methods of its assessment, including laboratory blood tests, questionnaires, etc, little information is available on the reasons for nonadherence, especially in children. To our knowledge, no study to date has quantified the barriers to adherence or attempted to determine whether they vary among age groups or community size (ie, small versus large). Our goal was to gain insight into the barriers to adherence and the impact of a GF diet on patients and their families in the hope of improving adherence through targeted support programs.
Adherence
The overall adherence rates to a GF diet, both by young children according to parents and by adolescent patients, were reasonably high (70%) in our study. Rates in the literature vary from 30% to 95% (7,10–13) depending on many factors (eg, self-report, laboratory testing, prediagnosis symptomatology, etc). The high adherence rates reported in our study may be due, in part, to a responder bias. We cannot discount the possibility that participants who were strictly adherent to a GF diet were more motivated and likely to complete the survey. Therefore, based on this potential bias, one should be cautious in generalizing the results to all individuals with celiac disease. There has been improved availability of GF foods over the past few years, which may also have positively influenced the adherence results. Similar to previous studies, there were no significant differences in adherence according to age or sex (12,13).
Interestingly, adherence to a GF diet and barriers to adherence, including availability and cost, did not vary significantly according to community size. One would expect the difficulties to be greater in smaller communities in which GF products would be less readily available. It is possible that the availability of GF products has, in fact, improved in smaller communities, or patients may be buying these products on the Internet. The study design did not permit us to investigate this issue.
Adolescents reported significantly lower adherence compared with caregivers reporting for children <13 years of age. It is difficult to ascertain whether this represents true lower adherence in teenagers compared with younger children or a difference due to substitute report compared with self report. Olsson et al (6) studied teenagers on a GF diet in Sweden and found that most found it easier to adhere at home than when out in social situations. They also found that teenagers were greatly influenced by the attitudes and knowledge of individuals in their environments (eg, peers, family, teachers, food providers). In our study, adolescents’ adherence to a GF diet while dining at restaurants was particularly lower. This may be due to lack of easy availability of GF foods outside the home or peer pressure when dining out. Similarly, Errichiello et al (12) reported that adherence often decreased in adolescence, and school integration and self-esteem were significantly impacted by celiac disease. Previous research has also shown that diagnosis by screening of asymptomatic adolescents can lead to poor adherence in this group (13,14). Further research to evaluate the changing influences on adolescent adherence is needed. Teenagers may represent a target group most in need of support to maintain optimal adherence.
Barriers
Despite high adherence to a GF diet, the responses demonstrated that there are many obstacles to this diet, which has a significant impact on everyday living and quality of life. The main barriers include availability, labelling and cost.
Similar to our results, several studies have found that patients had particular difficulty adhering to a GF diet when dining out and while travelling (4,7,8). This is likely due to variability in the availability of GF foods or cross contamination with gluten. Many respondents found ingredient labelling to be inadequate. This has been observed in previous studies in adults (7). Canada’s new food allergen labelling regulations came into effect in 2012 and will hopefully help by mandating the manufacturers to declare gluten sources on the package (15).
Several studies from North America and Europe have demonstrated that the cost of GF food products is significantly higher than gluten-containing ones (9,16,17). In a study from Canada (9), GF products were, on average, 2.5 times more expensive than their regular counterparts. Cost becomes an even more significant factor if multiple individuals in the household have celiac disease or other gluten-related disorders. Also, because the GF diet is lifelong, the overall economic impact can be substantial. The cost may decrease as the number of consumers increase and more manufacturers start producing GF products. Barratt et al (8) found that better adherence was associated with more affluent backgrounds. The authors speculate that higher levels of education and income may help to facilitate social mobility and problem solving to overcome challenges of the diet (eg, cost, availability, need for planning).
While most respondents in the study were aware of the Canada Revenue Agency’s tax benefit, only one-half actually applied for it. The study did not inquire about the reasons for not applying. This tax benefit consists of claiming the incremental costs associated with the purchase of GF products, which is the price difference between a GF product and its gluten-containing counterpart (18). Claiming this benefit is cumbersome because the difference must be calculated each time a GF product is purchased and all receipts kept.
Based on the study results, some recommendations can be made to the government, health profession and food industry. A GF diet needs to be viewed as a prescribed therapy. Despite the increasing number of patients affected by celiac disease, there is still a lack of easily accessible financial support. Appropriate financial support by government and medical insurers should be considered. There is a lack of knowledge regarding GF diets by grocery store and restaurant workers. Standardized training for staff at schools, camps and restaurants is essential to protect children from inadvertent gluten exposure. This will, in turn, help their integration with peers and improve their quality of life.
CONCLUSIONS
Availability, cost and labelling of food products are major barriers to adherence to a GF diet for children with celiac disease and their families. A GF diet can adversely affect certain aspects of social life such as the ability to travel. Better awareness, improved labelling of packaged food products and income support are required to improve the lives of children with celiac disease.
Acknowledgments
The authors thank Colleen M O’Connell PhD for her help with statistical analysis.
Footnotes
DISCLOSURES: Dr Rashid is a member of the Professional Advisory Board of the Canadian Celiac Association.
REFERENCES
- 1.National Institutes of Health Consensus Development Conference Statement on Celiac Disease, June 28 to 30, 2004. Gastroenterology. 2005;128(4 Suppl 1):S1–9. doi: 10.1053/j.gastro.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Fasano A, Berti I, Gerarduzzi T, et al. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: A large multicenter study. Arch Intern Med. 2003;163:286–92. doi: 10.1001/archinte.163.3.286. [DOI] [PubMed] [Google Scholar]
- 3.Hoffenberg EJ, MacKenzie T, Barriga KJ, et al. A prospective study of the incidence of childhood celiac disease. J Pediatr. 2003;143:308–14. doi: 10.1067/s0022-3476(03)00282-8. [DOI] [PubMed] [Google Scholar]
- 4.Rashid M, Cranney A, Zarkadas M, et al. Celiac disease: Evaluation of the diagnosis and dietary compliance in Canadian children. Pediatrics. 2005;116:e754–9. doi: 10.1542/peds.2005-0904. [DOI] [PubMed] [Google Scholar]
- 5.Hill ID, Dirks MH, Liptak GS, et al. Guideline for the diagnosis and treatment of celiac disease in children: Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2005;40:1–19. doi: 10.1097/00005176-200501000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Olsson C, Hornell A, Ivarsson A, Sydner YM. The everyday life of adolescent coeliacs: Issues of importance for compliance with the gluten-free diet. J Hum Nutr Diet. 2008;21:359–67. doi: 10.1111/j.1365-277x.2008.00867.x. [DOI] [PubMed] [Google Scholar]
- 7.Ukkola A, Maki M, Kurppa K, et al. Patients’ experiences and perceptions of living with coeliac disease – implications for optimizing care. J Gastrointerstin Liver Dis. 2012;21:17–22. [PubMed] [Google Scholar]
- 8.Barratt S, Leeds J, Sanders D. Quality of life in coeliac disease is determined by perceived degree of difficulty adhering to a gluten-free diet, not the level of dietary adherence ultimately achieved. J Gastrointestin Liver Dis. 2011;20:241–5. [PubMed] [Google Scholar]
- 9.Stevens L, Rashid M. Gluten-free and regular foods: A cost comparison. Can J Diet Pract Res. 2008;69:147–50. doi: 10.3148/69.3.2008.147. [DOI] [PubMed] [Google Scholar]
- 10.Hogberg L, Grodzinsky E, Stenhammar L. Better dietary compliance in patients with coeliac disease diagnosed in early childhood. Scand J Gastroenterol. 2003;38:751–4. doi: 10.1080/00365520310003318. [DOI] [PubMed] [Google Scholar]
- 11.Hommel KA, Mackner LM, Denson LA, Crandall WV. Treatment regimen adherence in pediatric gastroenterology. J Pediatr Gastroenterol Nutr. 2008;47:526–43. doi: 10.1097/MPG.0b013e318175dda1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Errichiello S, Esposito O, Di Mase R, et al. Celiac disease: Predictors of compliance with a gluten-free diet in adolescents and young adults. J Pediatr Gastroenterol Nutr. 2010;50:54–60. doi: 10.1097/MPG.0b013e31819de82a. [DOI] [PubMed] [Google Scholar]
- 13.Fabiani E, Taccari LM, Ratsch IM, Di Giuseppe S, Coppa GV, Catassi C. Compliance with gluten-free diet in adolescents with screening-detected celiac disease: A 5-year follow-up study. J Pediatr. 2000;136:841–3. [PubMed] [Google Scholar]
- 14.Jadresin O, Misak Z, Sanja K, Sonicki Z, Zizic V. Compliance with gluten-free diet in children with coeliac disease. J Pediatr Gastroenterol Nutr. 2008;47:344–8. doi: 10.1097/MPG.0b013e31816f856b. [DOI] [PubMed] [Google Scholar]
- 15.Food Allergen Labeling – Health Canada < www.hc-sc.gc.ca/fn-an/label-etiquet/allergen/index-eng.php> (Accessed February 27, 2014).
- 16.Lee AR, NG DL, Zivin J, Green PH. Economic burden of a gluten-free diet. J Hum Nutr Diet. 2007;20:423–30. doi: 10.1111/j.1365-277X.2007.00763.x. [DOI] [PubMed] [Google Scholar]
- 17.Singh J, Whelan K. Limited availability and higher cost of gluten-free foods. J Hum Nutr Diet. 2011;24:479–86. doi: 10.1111/j.1365-277X.2011.01160.x. [DOI] [PubMed] [Google Scholar]
- 18.Gluten-free products – Canada Revenue Agency < www.cra-arc.gc.ca/tx/ndvdls/tpcs/ncm-tx/rtrn/cmpltng/ddctns/lns300-350/330/clc-eng.html> (Accessed February 27, 2014).


