| ABSTRACTS/RÉSUMÉS | |
| Neonatal-Perinatal Medicine (Platform Presentations) / Présentations plateformes en médecine néonatale et périnatale | e36 |
| Abstract presentation A (Platform) / Présentation d’affiches A (plateforme) | e39 |
| Abstract presentation B (Platform) / Présentation d’affiches B (plateforme) | e40 |
| Abstract presentation C (Platform) / Présentation d’affiches C (plateforme) | e41 |
| Abstract presentation D (Platform) / Présentation d’affiches D (plateforme) | e43 |
| Abstract presentation E (Platform) / Présentation d’affiches E (plateforme) | e44 |
| Abstract presentation F (Platform) / Présentation d’affiches F (plateforme) | e46 |
| Abstract presentation G (Platform) / Présentation d’affiches G (plateforme) | e47 |
| Abstract presentation H (Platform) / Présentation d’affiches H (plateforme) | e48 |
| Poster Session 1 / Séance de résumés par affiches 1 | e50 |
| Poster Session 2 / Séance de résumés par affiches 2 | e78 |
| DEPARTMENTS / RUBRIQUES | |
| Author Index to Abstracts / Index des auteurs des résumés | e108 |
| Index to Abstracts / Index des résumés | e112 |
Abstract
BACKGROUND:
Very preterm infants are predisposed to postnatal infections and necrotizing enterocolitis (NEC) that are associated with poor outcome and increased risk of brain injury.
OBJECTIVES:
To assess brain metabolic development in infants exposed to neonatal infections and NEC using indices of neuronal integrity (N-acetyl aspartate [NAA]/choline), measured with magnetic resonance spectroscopy (MRS). Hypothesis: NEC with concurrent sepsis is associated with impaired brain development, as reflected by NAA/choline ratios.
DESIGN/METHODS:
A total of 213 preterm born neonates (gestational age 24 to 32 weeks) recruited from two hospitals underwent MRS in the first weeks of life (32 weeks) and term-equivalent age (41 weeks). Ratios of NAA to choline were calculated from the basal ganglia. Data were categorized into six groups: preterm controls with and without brain injury, clinical infection, culture positive infection, NEC diagnosis with and without sepsis. A generalized linear model was used to assess the change in NAA/choline from scan 1 to scan 2 across groups (divided by the difference between ages at scan), adjusted for gestational age at birth and site. Post-hoc between-group comparisons were Bonferroni corrected (P<0.05).
RESULTS:
The groups were composed of the following number of infants: 51 with brain injury, 31 without brain injury, 28 had clinical infection, 61 had sepsis, 17 had NEC without sepsis and 25 had NEC with sepsis. The change in NAA/choline from scan 1 to 2 was significantly different between groups (P=0.04). Post-hoc comparisons revealed the rate of NAA/choline change was significantly lower in infants with NEC and concurrent sepsis in comparison to controls without injury (P=0.01).
CONCLUSIONS:
Infants with NEC and additional sepsis are at high risk for adverse metabolic brain development. This work highlights the importance of the prevention of NEC and sepsis.
Abstract
BACKGROUND:
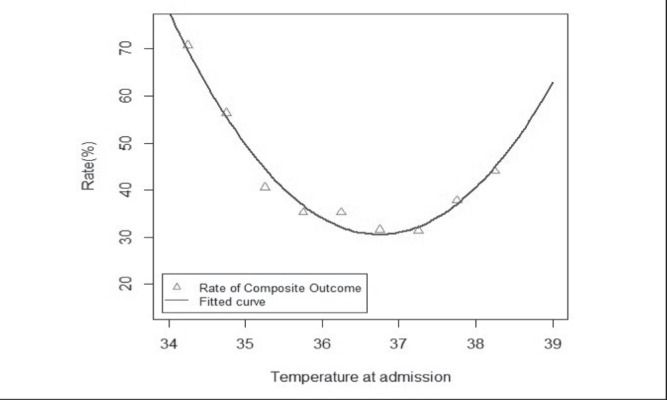
There have been limited investigations of the influence of admission body temperature on neonatal outcomes. Optimal ranges of admission temperature associated with mortality and morbidity are still unclear.
OBJECTIVES:
To examine the impact of admission temperature on adverse neonatal outcomes and to identify optimal ranges of temperature in very preterm infants.
DESIGN/METHODS:
Inborn neonates with gestational age <33 weeks admitted to Neonatal Intensive Care Units (NICUs) in Canadian Neonatal Network between 2010 and 2012 were included. Neonates with major congenital anomalies were excluded. The admission temperature measured within 5 h after admission to NICU was classified into nine groups starting from <34.5°C to ≥38°C with 0.5°C increment. The composite outcome was defined as mortality or any major morbidity including bronchopulmonary dysplasia(BPD), necrotizing enterocolitis(NEC), nosocomial infection(NI), severe intraventricular haemorrhage or periventricular leukomalacia and severe retinopathy of prematurity (ROP). The relationship between admission temperature and composite outcome and individual components of composite outcome identified in univariate analyses were further examined and used to determine the optimal temperature range using multivariable analyses.
RESULTS:
Of all 9833 neonates, 12%, 24%, 38%, 19%, 5%, and 2% of neonates had admission temperature <36°C, 36°C to 36.4°C, 36.5°C to 36.9°C, 37°C to 37.4°C, 37.5°C to 37.9°C, ≥38°C respectively. After adjustment for related maternal and infants characteristics, admission temperature was inversely related to mortality (19.5% increase per 0.5°C decrease) and a significant ‘U’ shaped relationship between admission temperature and composite outcome, NEC, ROP, BPD, and NI was observed, respectively .The rates of composite outcome, NEC, ROP, BPD, NI were lowest when the admission temperature was between 36.5°C and 37.4°C.
CONCLUSIONS:
Admission temperature in very preterm infants is associated with mortality and major morbidities. The optimal admission temperature in preterm infants ranged between 36.5°C and 37.4°C. This is the first outcome-based and population-based study in our knowledge with findings of optimal range of temperatures in very preterm infants consistent with WHO’s recommendations.
Figure 1).
Abstract
BACKGROUND:
Nasal intermittent positive pressure ventilation (NIPPV) is increasingly used in newborns in an effort to prevent/treat respiratory failure while minimizing ventilator-induced lung injury. Limited data are available in regards to whether NIPPV effectively supports CO2 elimination, what fraction of set ventilator pressures are delivered to the lungs and the resulting tidal volumes (Tv).
OBJECTIVES:
To evaluate NIPPV-dependent CO2 clearance and measure delivered pressures and Tv using two commonly employed interfaces.
DESIGN/METHODS:
An anatomically appropriate neonatal lung model, with either short bi-nasal prongs (FP; Fisher-Paykel, Quebec, Canada) or a small caliber nasal cannula (RAM; Neotech, California, USA), was tested over a range of clinically relevant NIPPV settings. To evaluate CO2 elimination, a fixed amount of CO2 was infused and the fraction remaining in the lung 100 s post-infusion was measured using a CO2 analyzer. Pressure transmission to the lung and Tv were measured via a pressure transducer and a Pneumotach respectively, at the level of the trachea.
RESULTS:
Lung CO2 elimination did not occur under continuous positive airway pressure (CPAP) and was directly proportional to the inspiratory pressure during NIPPV. At peak pressures of 22 to 34 cm H2O, CO2 clearance was greater (**P<0.001) with FP as compared with RAM (Figure panel A). Relative to the set ventilator pressure, a substantial dampening effect was documented at the lung level, which was significantly lower with RAM vs. FP (mean [± SD]) 2.8±0.2% vs. 11.9±1.5%; P<0.0001]. As shown in Figure panel B, CO2 elimination was dependent on Tv and effective despite amounting to only a small fraction of physiological Tv [maximum delivered % Tv: FP 15.5% (0.7) vs. RAM 6.1% (1.4), P<0.0001].
CONCLUSIONS:
NIPPV is capable of CO2 elimination despite substantial reduction in delivered lung pressure but less effective with RAM cannula as compared with FP. CO2 elimination occurs at such small Tv that these data suggest that NIPPV may depend on non-conventional mechanisms of ventilation.
Figure 1).
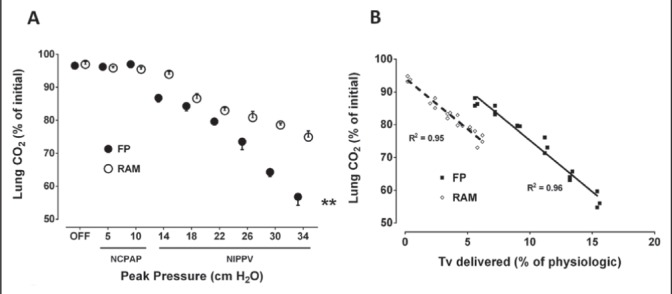
A and B
Figure 2).
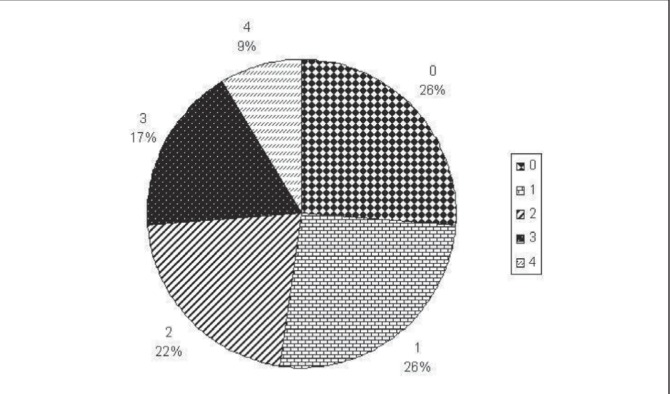
Number of significant impairments
Abstract
BACKGROUND:
Data on survival and morbidities of babies weighing <500 g at birth is needed for antenatal counseling and decision making regarding resuscitation.
OBJECTIVES:
To describe survival of babies <500 g birth weight (BW) born 1985–2012 and long term outcomes of babies born 1985–2008.
DESIGN/METHODS:
Institutional survival rates were calculated for all births and live births for epochs: 1985–87, 1988–92, 1993–97, 1998–2002, 2003–07 and 2008–12. Pregnancy terminations were excluded. All survivors with BW <500 g were invited to the Neonatal Follow-Up Program (NFUP). Birth characteristics and neurodevelopmental outcomes at 18 months (m) corrected age (CA) and at 4.5 years (yr) were evaluated and analyzed descriptively. Definitions: Cerebral palsy (CP) – abnormalities of tone and reflexes according to Bax; bilateral visual impairment; hearing impairment – hearing aid or cochlear implant prescribed. Motor impairment was defined at 18 m CA as <70 on the Bayley I, II or III; and at 4.5 yr as <70 on a motor quotient of the Peabody PDMS 1 or 2 and/or Developmental Coordination Disorder (DCD) as less than or equal to 5%le on Movement ABC I or II. Cognitive impairment was defined at 18 m CA as <70 on the BSID-I or II and adjusted Bayley-III score (Moore et al, 2012) and at 4.5 yr as <70 on Wechsler testing (WPPSI-R and WPPSI III).
RESULTS:
Survival rates were 2.7% for all births (according to epochs: 0.9%, 0%, 1.2%, 2.0%, 10.5% and 3.6%) and 6.6% for live births (according to epochs: 1.9%, 0%, 3.4%, 4.1%, 24% and 11.1%). Of 25 neonatal survivors, one died at 9 m CA (BW 492 g) and one refused follow-up. Data were extracted for 23 children. The earliest survivor was born in 1987 (male, BW 480 g). Babies had a median BW 465 g (range 380 g to 495 g), and gestation 26 1/7 weeks (range 22 4/7 to 30 2/7 weeks); 21 (84%) were inborn and 12 (48%) were male; 20% were of multiple pregnancy; 19 babies (76%) were small for gestational age (BW <3rd percentile). Median Apgar at 5 min was 7 (range 1 to 10).
Table 1).
Follow-up data
| Significant Impairments | n (%) |
| Motor at 18m | 10/21 (48) |
| Motor at 4.5 yr | 15/22 (68) |
| CP | 4/23 (17) |
| DCD | 6/22 (27) |
| Cognitive at 18 m | 8/22 (36) |
| Bayley Cognitive score (Mean. SD) | 74.8 (22.7) |
| Cognitive at 4.5 yr | 11/23 (48) |
| IQ 3–5 yr (Mean, SD) | 76.7 (19.6) |
| Visual | 6/22 (27) |
| Hearing | 3/22 (14) |
Abstract
BACKGROUND:
Our aim was to reduce bronchopulmonary dysplasia (BPD) at Foothills Medical Center (FMC), which had one of the highest rates among Canadian NICUs. We developed evidence-based practice guidelines called Open Lung Strategy (OLS), to help maintain functional residual capacity with distending pressures.
OBJECTIVES:
To examine the impact of ‘open lung strategy’ on short term neonatal outcomes among preterm infants with gestational age <33 weeks.
DESIGN/METHODS:
This is retrospective cohort study. In October 2011, OLS was implemented through multidisciplinary meeting, use of checklist and quarterly feedback to the neonatal group. We included all infants with gestational age <33 weeks. The pre-OLS group included infants admitted between July 2010 and Sept 2011 and the post-OLS group were those admitted between Oct 2011 to Dec 2012. Neonatal outcomes between the two groups were analyzed using univariate and multivariate analysis. The primary outcome was bronchopulmonary dysplasia (BPD) at 36 weeks postmenstrual age. Secondary outcomes included intraventricular hemorrhage (IVH), retinopathy of prematurity (ROP) and necrotizing enterocolitis (NEC).
RESULTS:
Of the 792 eligible infants, 396 were admitted in post OLS study period. No significant differences were observed in the baseline characteristics between the two groups. On univariate analysis, BPD and ROP ≥ stage3 was significantly reduced in post OLS group. However, IVH was significantly increased in the Post OLS group.
CONCLUSIONS:
The implementation of a practice change targeting a respiratory management strategy resulted in reduced rates of BPD. There was an associated decrease in ROP and increase in IVH the secondary outcomes. A longer period of study will determine if the improvement in BPD and ROP is sustained and if the change in IVH is a true increase. When quality improvement strategies are implemented comprehensive disease free survival should be studied.
Table 1).
| Pre OLS N=396 | Post OLS N=396 | Unadjusted OR | Adjusted OR* | |
|---|---|---|---|---|
| BPD | 113/378(29.8) | 81/375(21.6) | 0.64 (0.46–0.89) | 0.69 (0.46–1.03) |
| ROP ≥ stage3 | 33/241 (13.6) | 18/239 (7.5) | 0.50 (0.27–0.92) | 0.44 (0.20–0.94) |
| IVH ≥ grade3 | 15/386(3.9) | 38/387(9.8) | 2.69 (1.45–4.98) | 4.17 (2.02–8.59) |
| NEC ≥ stage2 | 14(3.5) | 11 (2.78) | 0.77 (0.34–1.73) | 0.66 (0.27–1.57) |
| Mortality | 18(4.5) | 23 (5.8) | 1.29 (0.68–2.43) | 0.99 (0.44–2.22) |
Abstract
BACKGROUND:
Adult studies have shown that outbreaks in nosocomial infections are associated with understaffing and overcrowding.
However, no study has assessed the impact of nurse overtime and patient volume in the neonatal intensive care unit (NICU) on neonatal nosocomial bacteremia.
OBJECTIVES:
The objective of this study was to assess the impact of patient volume and nurse overtime on neonatal nosocomial bacteremia in all infants hospitalised in the NICU.
DESIGN/METHODS:
We conducted a retrospective study on all infants (n=7473) admitted in the CHU de Québec NICU (capacity of 51 beds) from April 1, 2008 to March 31, 2013. Administrative data (nursing overtime hours per day, patient census per day) were obtained from the database Logibec, patient information was obtained from Med-Echo and information on neonatal nosocomial bacteremia was obtained from the local infectious disease database TDR. We assessed the association between administrative data and patient outcomes by using logit and probit models.
RESULTS:
The average patient volume as percentage of capacity during the study period was 98.7±6.5%. The average overtime as percentage of total daily hours of work was 4.0±3.4%. Overtime is positively related to occupancy levels. For every increase of occupation by one patient, there was an increase of 1.65 h of overtime per day (P<0.001). There were a total of 306 events of nosocomial bacteremia during the study period. Coagulase-negative staphylococcus caused 82% of infections. The overall risk of nosocomial bacteremia was 4.2%. The total number of regular worked hours was not associated with a higher risk of infection. Higher overtime (expressed as percentage of total worked hours) was significantly associated with an increased risk of nosocomial bacteremia (P=0.02). Also, days when overtime was >8% of total worked hours, are significantly associated with an increase risk of nosocomial bacteremia (OR 1.51 [95% CI 1.10 to 2.08]; P=0.01). There was a trend between higher patient volume (100% occupancy compared to 90% capacity) and higher risk of nosocomial bacteremia (OR=1.60; P=0.08).
CONCLUSIONS:
In our study, high patient volume and nursing overtime was directly associated with a higher risk of nosocomial bacteremia in the NICU. This suggests that re-organising the medical workforce to better adapt to periods of high activity in the NICU should become an integral part of nosocomial infection prevention.
Abstract
BACKGROUND:
Preterm birth conveys an increased risk of medical and development problems,which may translate into higher health resource utilization. Resource use has not been described among preterm born infants in Canada.
OBJECTIVES:
To describe health resource use including health technology aides, medication and community referrals in infants born prematurely and examine factors associated with use.
DESIGN/METHODS:
A total of 818 preterm infants born <29 weeks gestation between January 1 to December 31, 2010, and seen at a Canadian Neonatal Follow-Up site at 18 to 22 months’ corrected age (CA) were studied. Data was collected through chart review and parental interview using standardized forms. The associations between health resource use child/family characteristics were assessed by Pearson χ2 analyses or Fisher’s exact test and by ANOVA F-test for continuous variables.
RESULTS:
Between NICU discharge home and the 18-month CA visit, 181 infants (22%) utilized various aides in the home: supplemental oxygen (n=112), pulse oximeter (n=37), CPAP (n=8), tracheostomy (n=7), tube feeding (n=60), braces (n=42) and walker (n=10). Aid use decreased from 68.8% for infants born ≤23 weeks’ gestational age (GA) to 37.5% at 24 weeks’ GA and 17.5% at 28 weeks’ GA.
More than one-half (56.2%) received regular medication in the three months preceding the 18-month visit, including 20% on inhalers, 32% on vitamins, 17.5% on antibiotics, 5% on anti-reflux treatment and 2% on anti-convulsants.
Longer time to neonatal discharge was associated with health resource use. Children with technology dependence were also more likely to be neurologically abnormal at 18 months’ CA (30% vs. 6%; P<0.01) and to have foster parents (4.6% vs. 1.3%; P=0.01) and slightly more were on social welfare (12% vs. 8%).
Most infants (78.6%) were referred to an allied health professional (Table 1)
CONCLUSIONS:
A substantial number of extremely preterm infants require various health care resources. The association between health technology dependence and social disadvantage warrants further investigation as this may indicate that families of medically fragile children need more support.
Table 1).
| Dietician | 24.5% |
| Early intervention program | 32% |
| Occupational therapist | 33% |
| Physical therapist | 40% |
| Speech - language pathologist | 33% |
Abstract
BACKGROUND:
Low birth weight neonates in the neonatal intensive care unit (NICU) are commonly managed with early and prolonged continuous positive airway pressure (CPAP). CPAP therapy is used to maintain functional residual capacity and allow the lungs to grow at optimized inflation. Historically, CPAP has been considered a contraindication for initiation of oral feeding. Delayed introduction of oral feeding is associated with delayed progression of oral feeding skills. Although prolonged CPAP has lessened the burden of bronchopulmonary dysplasia (BPD), oral feeding delay has resulted in longer NICU stays and increased the potential for long term feeding problems.
OBJECTIVES:
To study the clinical feasibility of initiating early oral feeding for neonates who are CPAP dependent. Physiological stability and infant cues guide the nursing assessment for oral readiness. Breastfeeding is encouraged and preferred method of feeding. Emerging evidence suggests such a technique encourages the neonate to associate food and eating with safety and pleasure.
DESIGN/METHODS:
We report a quality improvement project designed as an observational study. An original algorithm called “Eating “in SINC” (Safe Individualized Nipple-feeding Competence) was introduced for all neonates <32 weeks’ corrected gestational age who have been on CPAP. The SINC algorithm encourages frequent oral feeding practice opportunities, specifies maximum oral feeding volumes and limits oral feeding times with a goal of building skill and stamina in fragile feeders. Breastfeeding is encouraged at every stage of the algorithm. Progression in the SINC algorithm is allowed only if the neonate displays competency over a number of days. The intervention group eating with the SINC algorithm (collected over a six month period) is compared to a historical cohort of neonates from a similar time period during which time the neonates were maintained on prolonged CPAP for lung optimization but did not receive any oral feeding while on CPAP therapy.
RESULTS:
Early project results support our SINC algorithm. Neonates can be maintained on CPAP to prevent BPD and oral feeding can be safely initiated at the same time. Overall length of stay has been reduced between the two comparative groups. Breast feeding rates and oral feeding difficulties following discharge from the NICU are being tracked.
CONCLUSIONS:
It is possible to maintain prolonged CPAP for lung optimization in very low birth weight neonates and initiate safe early oral feeding.
Abstract
BACKGROUND:
With barely 3% of health care workers (HCW) and over 25% of the global health burden, Sub-Sahara African nations saw an urgent need to build capacity in community focused research in 2008 (WHO Bamako ‘Call for Action’). Borrowing from principles of microfinance, MicroResearch (MR) provides training, coaching and small grants for community focused interdisciplinary research (CFIR) and knowledge translation.
OBJECTIVES:
To assess if MicroResearch addresses the local need for CFIR in East Africa (EA).
DESIGN/METHODS:
We used targeted on-line surveys to assess health challenges and barriers for EA HCW researchers. In phase 1, questionnaires to assess health care challenges were sent to senior researchers (deans, department heads) and junior HCW engaged in CFIR. In phase 2, we assessed an on-line focus group of community researchers from five academic sites in EA using qualitative analyse of responses to prompted questions.
RESULTS:
In phase 1, 68 questionnaires were distributed, and 40 (59%) responded, 17 from senior and 23 junior HCW researchers. The two groups were pooled since response differences were <3% to most questions. Access to healthcare (36%), social determinants (33%) and health service infrastructure (21%) were the most common healthcare needs identified. Lack of research skills (design, analytic methods, training programs), capacity (coaching, mentoring), and funding were identified, as common research capacity needs. Both groups recommended research funding be directed to community (33%), health system (25%) or epidemiologic research. In phase 2, a focus group of 10 multidisciplinary participants (five female, five male) was formed. There were 16 valid comments with 21 points raised for saturation to be reached. Thematic content analysis and summaries were made at stages of the analysis. The four main thematic areas identified as barriers to health research, listed in order of frequency, were; Knowledge, Finance, Mentorship/Coaching, and Ethical Regulation/clearance, Incentives.
CONCLUSIONS:
Healthcare needs and barriers to research for CFIR in EA were identified in surveys of senior and junior East African HCW. Strategies, like MR, are addressing these capacity building issues.
Abstract
BACKGROUND:
Sub-Saharan African countries have urged grassroots input to improve research capacity (WHO 2008) including in community directed research. In Uganda, Tanzania and Kenya, MR is building capacity to find local, sustainable, community solutions for local health problems.
OBJECTIVES:
After five years of MR in EA, we report outcomes.
DESIGN/METHODS:
MR training occurred during intensive two-week workshops (WS) where 20 to 30 health workers (HW) were introduced to principles of research, community engagement, knowledge translation, health policy. In small interdisciplinary teams (six to eight HW) self-identified community directed research outlines were created. Post WS, each team developed a full proposal supported by MR coaches (one EA, one NA) and submitted for international MR peer review. Following local ethics approval, successful projects were funded (up to $2,000). Projects were implemented, results reported and knowledge translated, including written report and extended abstract published in peer-reviewed PubMed journal. MR evaluation at five years consisted of review of WS participant and proposal data, standardized questions post each WS, input from attendees at two EA MR Forums held in March and November 2013.
RESULTS:
Between 2008 and mid-November 2013, 14 workshops were conducted at five EA training sites with 366 participants (43% female); 32% MD, 18% RN or Midwife, 50% other HW. By 2012, 27 projects approved for funding (74% in Uganda): seven completed, four published or accepted, 20 ongoing. Three projects helped change health policy/practice and four lead to career advancement. 37% focused on child health, 37% maternal health, 26% both. MR fostered gender equity in team PIs, funding success, EA coaches, MR local teachers. MR principles now in HW undergrad curriculum at two EA sites. Post WS, 90% participants rated WS positively; 20% noted MR changed culture of inquiry at work. Post MR 2013 Forums, an online MR network, MR alumni network and an EA MR site leaders consortium formed to grow MR.
CONCLUSIONS:
MR builds capacity for EA community directed interdisciplinary team research at modest cost. MR projects lead to local health care changes, enhance culture of inquiry. EA MR successes, with EA MR leadership will support growth beyond the five EA sites if resources become available.
Footnotes
Supported by International Development Research Council, Canada, Canadian Child Health Clinician Scientist Program, Dalhousie Medical Research Foundation, Canadian Paediatric Society and private donors.
Abstract
BACKGROUND:
In Canada asylum seekers may be detained in prison-like institutions. This includes children. The official statistics of the CBSA suggest that between 2005 and 2010, >650 children were detained each year. While international studies acknowledge the negative health consequences of detention on children, until now there has been no research on the detention of children in Canada.
OBJECTIVES:
This study aimed to generate an understanding of the well-being, health and experiences of migrant children who have been detained in Canada by documenting their perspectives during or after detention.
DESIGN/METHODS:
This was a qualitative study anchored in an ethnographic methodology. Data was collected using two methods: 1) in-depth interviews with 18 families, who had been detained or were detained at the time of interview; and 2) participatory observation in the field (at the detention centres in Montreal and Toronto). Detention impacts on children mental health, wellbeing and sense of identity was documented.
RESULTS:
Results suggest that even very brief periods of detention are distressing for children, with potentially longstanding sequelae. During detention, children are often separated from one or both parents, which appears to compound suffering. Children’s narratives show that detention may negatively impact their sense of self and safety in Canada.
CONCLUSIONS:
Children experience detention as highly stressful, frightening and even, in some cases, traumatizing. Our findings suggest that detention may be significant determinant of health for this subgroup of children and that future policy and advocacy efforts should address this.
Abstract
BACKGROUND:
The neighbourhood environment provides both a social and physical context that is thought to have an effect on behaviours that may influence weight gain. There is limited research in this area on pre-school children.
OBJECTIVES:
The objective of this study is to examine the association between the built environment and body mass index (BMI) among pre-school-age children while adjusting for known individual level factors associated with pre-school obesity.
DESIGN/METHODS:
A cross sectional study of children one to five years of age was conducted using individual level data from the TARGet Kids! cohort in Toronto, Canada which includes prospectively collected data from 3928 children between September 2008 and June 2012. We characterized a child’s neighbourhood using a validated neighbourhood walkability index based on 1) car ownership; 2) population per square kilometer of residential area; 3) all services per 10,000 population; 4) average distance from residential points to nearest five retail locations; 5) crime per 100,000).The main outcome was child’s zBMI.
RESULTS:
The mean age of participants at baseline was 33.5 months. The proportion of children included in TARGetKids! with zBMI >1 (overweight) was 20.5% and zBMI >2 (obese) was 4.8%. The outcome, zBMI, was adjusted for: gender, ethnicity, age of child, birth weight, parental BMI, mother’s education, free play outdoors, immigration status and neighbourhood level income. The mean zBMI decreased as the walkability of the neighbourhood increased. Compared to the most walkable neighbourhood, the average zBMI of the least walkable was 0.269 vs 0.063 in the most walkable neighbourhood in Toronto. This relationship was maintained after adjustment for individual level factors.
CONCLUSIONS:
Living in a walkable neighbourhood was associated with lower zBMI among preschool-age children after adjustment for individual level factors known to be associated with obesity in young children. Identifying modifiable built environment features that could mitigate the epidemic of childhood obesity could have population wide impact on the health of our children and the adults that they subsequently become.
Abstract
BACKGROUND:
Uretral catheterization (UC) is widely performed to diagnose urinary tract infection (UTI) in febrile young children presenting to the emergency department (ED). However, potential complications related to this procedure have not been well studied.
OBJECTIVES:
The purpose of this study was to assess adverse events in the week following diagnostic uretral catheterization in the ED in young children and to determine the impact of these adverse events on the patient and his parent.
DESIGN/METHODS:
This was a prospective cohort study conducted over a period of nine months in a tertiary care pediatric emergency department. Recruitment mainly occurred during week days from 9:00 AM until 7:00 PM. All children three to 24 months of age with fever ≥38°C (≥100,4°F) and who had a UC procedure were invited to participate. Parents were contacted by phone seven to 10 days following the ED visit to answer a standardized questionnaire about adverse events potentially related to the UC. The primary outcome was the occurrence of an unfavourable event in the seven days following the UC. This was prospectively defined as painful urination, genital pain, urinary retention, hematuria and UTI occurring secondary to the UC. Secondary outcome included the impact of these complications, defined as the need for further medical care or intervention and school/work missed days. It was estimated that the evaluation of 200 participants would provide a 95% CI smaller than 4%.
RESULTS:
240 patients were invited to participate. Among them, 219 patients accepted and were included in the study with 20 (9%) missed to follow-up. Of the 199 patients who completed the study, 110 were females (55%) and the median age was 10 months. Overall, 41 (21%) patients experienced at least one adverse event and a total of 56 complications were noted: painful urination in 19 children (10%), genital pain in 16 (8%), urinary retention in 11 (6%), hematuria in nine (5%) and UTI in one (0.5%). Three parents reported the need for further medical care with their child and three missed work.
CONCLUSIONS:
Uretral catheterization is associated to adverse events in the following week in 21% of young children even though parents rarely seek medical care for them. Accordingly, it should be used parsimoniously in children considering its potential for unfavourable events.
Abstract
BACKGROUND:
Previously healthy children often present to the emergency room with fever. When complete blood count shows isolated neutropenia, these patients are often hospitalised and treated with broad-spectrum antibiotics. This approach for patients with febrile neutropenia (FN) is a clear standard of care recommended by various guidelines. However, such recommendations are based upon studies on chemotherapy and cancer-related neutropenia. Whether these recommendations are applicable to children with non-oncological neutropenia, including viral-induced or benign neutropenia, remains poorly studied.
OBJECTIVES:
Our objective was to describe the outcomes of children with fever and de-novo neutropenia.
DESIGN/METHODS:
Through a six-year (April 1, 2005 to March 31, 2011) retrospective cohort study at a tertiary pediatric hospital, we reviewed the outcomes of patients who presented to the emergency room with non-oncological, isolated severe FN (absolute neutrophil count (ANC) ≤0.5×109/L, and temperature >38.5°C). All patients with prior history of cancer, chemotherapy, bone marrow transplant, known neutropenia and children <3 months of age were excluded from this study.
RESULTS:
Forty-seven children, median age of 1.1 years (range 0.3 to 6.1), were included in this study. Median ANC on admission was 0.2×109/L. Seasonal variation with higher incidence in fall and spring was observed. Broad-spectrum antibiotics were given in 91.4% of cases. Six patients had suspected bacterial infections: three (6.4%) had a urinary tract infection, one (2.1%) had pneumonia, and one (2.1%) had a peritonsillar abscess. Only one patient had a severe presentation with a rapidly controlled compensated shock and the outcome was favourable. Although an external ear canal culture revealed pseudomonas aeruginosa, blood, CSF and urine cultures remained negative for this patient. The vast majority of patients, 37 children (78.7%), received a final diagnosis of probable viral infection and four patients (8.5%) had a discharge diagnosis of FN (unspecified cause). All patients had favourable outcomes with a median hospital stay of three days. None had positive blood cultures.
CONCLUSIONS:
In this study, the rate of severe bacterial infections in children with non-oncological FN is low, contrasting with a rate of 10% to 20% of documented bacteremia, and a up to 45% of invasive infections in oncology patients. Well-appearing children with non-oncological FN may not require intravenous antibiotics or hospitalisation, but should be closely followed. Physicians could therefore rely on the presence of other clinical findings such as patient appearance and possible source for bacterial infection in order to make such a decision. The safety of such an approach warrants further prospective studies.
Abstract
BACKGROUND:
Approximately 1/100 children are born with congenital heart disease (CHD) yearly. Delayed diagnosis of a critical subset of CHD that are cyanotic or require surgery within the first weeks of life increases morbidity and mortality. Pulse oximetry screening has improved detection of critical CHD otherwise undiagnosed by prenatal ultrasound and newborn examination. The AAP endorsed a screening protocol that requires oxygen saturation checks in all neonates prior to discharge and a saturation of <95% triggers further evaluation.
OBJECTIVES:
We sought to quantify the number of neonates that would have benefited from pulse oximetry screening in our region, to support the need for a screening protocol.
DESIGN/METHODS:
Medical records of all neonates with critical CHD who required surgery within six months of life were reviewed from April 2008 to April 2013, with REB approval.
RESULTS:
A total of 115 neonates from four regions required surgery for critical CHD, of whom 70 (61%) had surgery within the first two weeks of life. Fifty-six (49%) were not identified prenatally, with notable differences in detection rates between regions. Fifteen of 56 (27%) were not diagnosed prior to newborn discharge (eight coarctations, two total anomalous pulmonary venous connections, two transpositions, one interrupted arch, one pulmonary atresia, and one double inlet left ventricle). Twelve of 15 (80%) of these late diagnoses had saturations <95% at re-presentation with CHD (this increases to 100% excluding the coarctation group, who are not necessarily cyanotic at birth). Among the 15 late diagnoses, the most common findings in addition to cyanosis were murmurs (80%), tachypnea (47%), weak femoral pulses (47%) and increased work of breathing (33%). Forty-one of 56 (73%) without prenatal diagnosis were detected prior to discharge (11 transpositions, 11 coarctations, six hypoplastic left hearts, five total anomalous pulmonary venous connections, three pulmonary atresias, two truncus arteriosus, one tetralogy of Fallot, one double inlet left ventricle, one interrupted arch). The most common signs in this group were cyanosis (69%), murmurs (55%), weak femoral pulses (33%), and tachypnea (31%). Seven of 41 (17%) showed only cyanosis. Among these 41, 25 (61%) were detected within 24 h, four (10%) between 24 h and 48 h, and 12 (29%) >48 h of age.
CONCLUSIONS:
This study reaffirms the limitations to prenatal ultrasound and newborn examination in detecting critical CHD. It is likely that the 15 late diagnoses we identified could have been detected with pulse oximetry screening prior to discharge, equating to two to three patients each year that screening may help to detect in our region.
Abstract
BACKGROUND:
Oral sweet solutions have been accepted as effective analgesics for procedures in the neonatal population. While the evidence of effect has been established in neonates, there have been a limited number of published clinical trials in older infants for the painful procedures commonly performed in any setting and these few studies have shown conflicting results.
OBJECTIVES:
To compare the efficacy of an oral sucrose solution versus placebo in reducing pain in children one to three months of age during venipuncture in the Emergency Department (ED).
DESIGN/METHODS:
A single-center, randomized, double-blind, placebo controlled clinical trial was conducted in an urban tertiary care pediatric university-affiliated hospital ED. The study population was all infants from one to three months of age requiring venipuncture as part of their planned ED management. Study participants were randomly allocated to receive 2 mL of 88% sucrose solution or 2 mL of a placebo solution orally, 2 min before the procedure. The primary outcome measure was the difference in pain levels during venipuncture as assessed by the Face, Legs, Activity, Cry and Consolability Pain Scale (FLACC) 1 min post venipuncture. Secondary outcome measures were the difference in pain levels using the Neonatal Infant Pain Scale (NIPS) 1 min post venipuncture, crying time and variations in heart rate following the procedure.
RESULTS:
Eighty-seven participants were recruited, 45 in the sucrose group and 42 in the placebo group. Overall, both groups had similar baseline demographic and clinical characteristics, including administration of pacifier and other analgesia. The mean difference in FLACC pain scores compared to baseline was 2.07±0.77 in the placebo group vs. 1.36±0.59 in the sucrose group (P=0.49). For the NIPS pain score, it was 1.73±0.62 in the placebo group vs. 0.75±0.58 in the sucrose group (P=0.36). The difference in the mean crying time following venipuncture was statistically significant between both groups (69±13 s in the placebo group vs. 49±13 in the sucrose group; P=0.04). No significant difference was found in the difference of participants’ heart rates one minute post venipuncture compared to baseline (18±4 beats/min for placebo vs. 16±4 for sucrose; P=0.74). No significant adverse effects were reported. The overall blinding was successful.
CONCLUSIONS:
In children one to three months of age undergoing venipuncture in the ED, administration of an oral sweet solution did not statistically decrease pain scores as measured by the FLACC and NIPS scales or participants’ heart rates. However, crying time was significantly decreased by providing sucrose instead of a placebo.
Abstract
BACKGROUND:
Return of menses (ROM) is a well known objective determinant of health in adolescents with eating disorders (EDs), and is helpful in predicting a target weight treatment goal to which the patient should be working towards. Although weight gain is a well known prerequisite for re-establishing a normal menstrual cycle, the degree of weight gain required, the predictors and the temporal association between weight and menstrual resumption have not been well established.
OBJECTIVES:
The primary aim of this study was to examine the relationships between hormone levels (estradiol, LH, FSH), body mass index (BMI), percent body fat and menstrual status in patients with a restrictive ED to ascertain whether these indicators were helpful predictors of ROM. The secondary goal was to compare hormone levels in patients who achieved ROM with those who remained amenorrheic with the aim of better understanding the role of hormones in ROM.
DESIGN/METHODS:
A retrospective chart review was completed on a random sample of 100 patients diagnosed with a restrictive ED (anorexia nervosa, eating disorder not otherwise specified) between November 2001 and December 2011. Demographic information, BMI, hormone levels, bone density scores, percent body fat and menstrual history were examined.
RESULTS:
Patients with restrictive EDs who have menses at assessment differed from those with secondary amenorrhea in that they had higher BMI (19 kg/m2 vs 16.4 kg/m2); higher percentage of their healthy body weight goal (89% vs 79%); longer chronicity of symptoms (20.3 vs 16.4 months); higher estradiol levels (196 vs 86) and higher body fat percentage (25% vs 14%). Preliminary analyses reveal largely variant hormone levels existed across the groups, although themselves were not found to be predictive of ROM.
CONCLUSIONS:
Patients with restrictive EDs with and without menses differed at assessment with regard to their hormone and weight profiles, although these indicators were not found to be predictors of ROM. These findings agree with current literature that serum sex hormones are not sufficiently precise for prediction of ROM at an individual level. More research is required to delineate predictors of ROM in amenorrheic adolescents with EDs in order to help inform accurate healthy body weight predictions.
Abstract
BACKGROUND:
Les intoxications, accidentelles (Ia) ou intentionnelles (Ii), sont un problème fréquent en pédiatrie. Une minorité nécessitera une hospitalisation aux soins intensifs (SI), qui représente les cas d’intoxications les plus graves. Aucune étude canadienne récente n’a décrit cette population précise et la morbidité associée.
OBJECTIVES:
Décrire une cohorte de patients souffrant d’intoxication nécessitant une hospitalisation aux SI pédiatriques. Définir ce qui différencie les deux sous-groupes (Ia et Ii), ainsi que leur évolution aux SI.
DESIGN/METHODS:
Étude rétrospective des cas admis aux SI de 2003 à 2009, dans trois centres universitaires pédiatriques. Les données ont été recueillies par une revue de dossiers : caractéristiques du patient et de l’intoxication, évaluation initiale, évolution aux SI, traitements nécessaires et durée de séjour. Une analyse descriptive de tous les patients est rapportée, suivie d’une analyse comparative (Ia versus Ii).
RESULTS:
Deux cent soixante-et-un cas ont été identifiés : 123 (47.1%) de nature accidentelle et 138 (52.9%) de nature intentionnelle. Les médicaments représentaient les substances le plus souvent impliquées (76.9%), suivi des intoxications éthyliques (16.3%). Parmi les médicaments, l’intoxication à l’acétaminophène prédominait (25%). Les poly-intoxications étaient fréquentes (42.5%). L’âge moyen des enfants suivait une distribution bimodale avec un pic (Ia) à 3 ans (3.6±3.3, 2.6) et un pic (Ii) à 15 ans (15±2.2, 15.4). À l’admission, 39.7% des patients présentaient un score <15 à l’échelle de Glasgow, 20.8% une agitation motrice et 6.3% des convulsions. La majorité des patients présentaient une évolution favorable : 6.1% ont développé une insuffisance hépatique, 1.5% une insuffisance rénale et quatre (1.5%) patients sont décédés. Soixante-seize (29.1%) patients ont reçu un antidote et soixante-trois (24.1%) ont été intubés. La durée moyenne de séjour aux SI était courte (1.6 jours±6.1, 1). Les intoxications à l’acétaminophène (40.7% vs 6.6%, P<0.001) et éthyliques (28.9% vs 2.4%, P<0.001) prédominaient dans le groupe Ii. On y retrou-vait aussi plus d’insuffisance hépatique (10.1% vs 1.6%, P=0.004), un séjour hospitalier plus long (5±7 vs 3.3±9.6, P<0.001) et l’administration d’un antidote plus fréquemment (37.5% vs 19.5%, P=0.002). Dans le groupe Ia, on retrouvait plus de garçons (52.4% vs 37.6%, P=0.017) et ils étaient plus susceptibles d’avoir reçu du charbon activé (35.8% vs 23.9%, P=0.036).
CONCLUSIONS:
Les intoxications aux SI pédiatriques sont surtout de nature médicamenteuse, parmi lesquelles l’intoxication à l’acétaminophène prédomine. La majorité des patients présentent une évolution favorable; les décès sont rares et la durée de séjour aux SI est courte. Des différences significatives existent entre les deux groupes.
Abstract
BACKGROUND:
Hospitalization is the treatment of choice for medically unstable adolescents with anorexia nervosa (AN).
OBJECTIVES:
The aim of this study was to determine the cost of inpatient treatment for adolescents with AN from both a hospital and societal perspective and to identify determinants of such costs.
DESIGN/METHODS:
Micro-costing methods were used for this retrospective cohort study of all adolescents (12 to 18 years) admitted for the first time with AN at a tertiary care child and adolescent eating disorder program in Toronto, Canada between September 1, 2011 and March 31, 2013. Demographic data and clinical variables were collected. Hospital administrative cost data and Canadian census data were used to calculate hospital and societal costs. Multivariate linear regression analyses were performed to identify significant predictors of hospital costs.
RESULTS:
Seventy-three adolescents were identified and included in this cost-analysis. Mean total hospital cost was $51,349±26,598 and mean total societal cost was $54,932±27,864 per admission, based on a mean length of stay of 37.9±19.7 days. Body mass index (BMI) was found to be a significant predictor of hospital costs (P=0.0002). For every unit increase in BMI there was a 15.7% decrease in hospital costs after controlling for time spent on the waiting list. Higher BMI (P<0.0001) and younger age (P=0.0480) at admission were both found to be significant negative predictors of caregiver costs after controlling for time spent on the waiting list.
CONCLUSIONS:
The economic burden of AN among adolescents is substantial. Younger age and lower BMIs were associated with increased hospitalization costs.
Abstract
BACKGROUND:
Substance use is a prevalent behaviour in adolescents and is associated with acute and long-term health risks. The 2011 Ontario Student Drug Use and Health Survey found that 54.9% of high school students reported using alcohol in the 12 months prior to the survey while 37.4% reported using a drug other than alcohol or tobacco. The current study is part of a multi-centre project examining emergency department (ED) visits relating to alcohol or other drug use
OBJECTIVES:
To determine the prevalence of adolescents presenting to a tertiary care pediatric ED with substance-use associated conditions, and to identify associated patient variables, including chronic health conditions.
DESIGN/METHODS:
A retrospective chart review was performed of visits to the ED between September 1, 2010 and August 31, 2011. Inclusion criteria were: patients 12 to 18 years, visits coded with ‘alcohol/substance use/abuse’, ‘overdose/accidental’, ‘overdose/intentional’, and ‘overdose/undetermined’. Data was collected and reviewed by two independent researchers. Simple descriptive statistics were used to summarize the findings.
RESULTS:
A total of 149 patient encounters were identified that met inclusion criteria. Of these, 41 involved no evidence of substance use on history or toxicology screen, and were excluded. Of the 108 remaining, substance use was identified by history and toxicology screen in 88 and on history alone in the remaining 20 visits. The mean patient age was 15 years (range 12 to 17) with 66% identified as female. A pre-existing mental health condition was identified in 27 cases (25%). Twenty-three patients (21%) were followed in the past 12 months for a chronic health condition other than substance use (eg, T1DM, asthma). The most commonly used substance was alcohol (n=68 [63%]). The second most common substance was cannabis (n=26 [24%]), followed by MDMA (n=16 [15%]) and OTC cough/cold medication components (n=6 [5%]). Other substances identified included ketamine, methamphetamine, cocaine, and opioids. Polysubstance use was identified in 30 encounters (28%).
CONCLUSIONS:
Consistent with provincial data, alcohol was the most commonly used substance among adolescents presenting to a pediatric ED with substance-use related conditions. One quarter of patients had a pre-existing mental health condition, while 21% of patients were already connected with the institution for treatment of a chronic disease. These findings have implications for both the assessment and management of adolescents across a variety of health care settings. Future research should explore additional ways of identifying those adolescents at increased risk for morbidity relating to the use of alcohol and other substances.
Abstract
BACKGROUND:
Headaches are the most frequently reported persistent symptoms following a pediatric mild traumatic brain injury (MTBI), may be challenging to treat and can transform into debilitating chronic headaches. The beneficial use of peripheral nerve blocks of the scalp has been reported for adults with post-traumatic headaches.
OBJECTIVES:
Characterize the therapeutic effect of peripheral nerve blocks of the scalp for children and adolescents with post-traumatic headaches.
DESIGN/METHODS:
Retrospective case series on all patients <18 years of age treated between January 2012 and June 2013 in the MTBI clinic with a nerve block. The main outcome measure was the proportion of patients with a good therapeutic effect, defined by the duration of the block being >24 h and/or repeat blocks requested. A data extractor blinded to main outcome measures performed the chart review. A patient satisfaction survey also assessed the perceived benefit of the procedure and whether the patients would recommend this treatment to their family and friends.
RESULTS:
A total of 62 nerve blocks were performed on 28 patients for 30 injuries that led to post-traumatic headaches. The mean age was 14.6 (1.7) years, 80% female, with 77% resulting from a sport-related concussion. The first nerve blocks were performed 70 (54.2) days post-injury; 47% had a single nerve block encounter with a mean number of nerve blocks of 2.1 (1.4) with a range of 1 to 6. A greater occipital nerve block was done on all patients with 73% having other nerves of the scalp blocked as well (supra-orbital and/or lesser occipital). The therapeutic effect was good in 93% of patients with 71% reporting immediate complete relief of their headaches; the mean percent headache reduction was 94%. The satisfaction survey (response rate 82%) revealed a similar trend: 83% recalled immediate relief of their headaches, 83% and 61% indicated that it improved or resolved their headaches in the days to weeks following the injection(s), respectively and 91% would recommend a nerve block for post-traumatic headaches.
CONCLUSIONS:
The ease with which peripheral nerve blocks of the scalp can be performed combined with the immediate relief experienced by patients makes them a potential addition to the armamentarium of headache management strategies for children and adolescent with post-traumatic headaches.
Abstract
BACKGROUND:
Reduction of forearm fractures in children is frequently performed with the aid of fluoroscopy. Point-of-care ultrasound has emerged as a tool clinicians can use to diagnose and treat fractures; advantages include no radiation, real-time high quality images, availability in most emergency departments and no need for specialized personnel.
OBJECTIVES:
The objective of this study is to determine how ultrasound compares to fluoroscopy in assessing the adequacy of reduction of single-bone distal forearm fractures in pediatrics.
DESIGN/METHODS:
We completed a prospective observational study in a tertiary-care pediatric emergency department. Eligible patients were <18 years of age with acute (<72 h) single-bone fractures of the mid or distal forearm that required reduction. Exclusion criteria included fractures with displacement of the radius and ulna, intra-articular fractures, open fractures or any neurovascular compromise. A one-hour simulation-based session was given to novice-ultrasound emergency physicians who then performed the reduction under ultrasound guidance (high frequency linear probe) until they felt they had the best possible reduction and saved images in at least two-planes. Based on the saved images, the physician recorded whether the reduction was adequate or if further reduction was necessary. Fluoroscopy was then performed and the physician assessed the fluoroscopic images to decide whether the fracture had been adequately reduced; management continued based on the fluoroscopic images. Results were defined dichotomously as “adequately” or “inadequately” reduced for all images.
RESULTS:
To date, 96 patients were enrolled. The mean age was 10.8±3.3 years and 74.2% were male. The radius was fractured in 99% of cases: distal radius 88.7% of which 26.8% involved the growth plate. Physicians performed a mean number of six (range one to 29) reductions with the aid of ultrasound and ranked its ease of use at a mean of 1.9±0.9 on a 5-point Likert scale (1 extremely easy, 5 extremely difficult); 77.3% reported that ultrasound helped with the reductions. Ultrasound revealed 83 adequate, 11 inadequate, two false negative (ie, ultrasound inadequate but fluoroscopy adequate) and no false positives yielding a sensitivity and specificity (95% CI) of 97.6% (94.4 to 100.9) and 100% for adequacy of reduction, respectively. The overall diagnostic accuracy was of 97.9%; only one of 16 physician had discordant fluoroscopy and ultrasound interpretations that occurred during their first 2/5 cases.
CONCLUSIONS:
Point-of-care ultrasound can be used reliably by most physicians to guide and determine adequacy of fracture reductions of distal radius fractures in children. Optimal training strategies need to be determined in order to ensure accurate interpretations.
Abstract
BACKGROUND:
Purposes of the study: 1) to determine if youth under 16 years of age are at a greater risk of severe injuries related to all terrain vehicle (ATV) use and 2) to determine if legislation for a minimum drivers age of 16 years reduces the risk of ATV-related injuries in youth.
OBJECTIVES:
Outcomes: 1) Moderate to severe injury (concussions, injuries requiring admission to hospital, fractures, intracranial injuries, amputations and fatal injuries) versus mild injury; 2) rate of ATV injuries.
DESIGN/METHODS:
Study Designs: Cross sectional surveillance study and an interrupted time series analysis. Setting. Nine pediatric and four adult emergency departments across Canada participating in the Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP) between 1990 and 2009. Population: Children and adults who presented to a CHIRPP emergency department with ATV-related injuries. Exposures: (1) Less than 16 years of age at the time of injury; (2) injured in a province with legislation for a minimum drivers age for ATVs.
RESULTS:
Of the 5005 analysed presentations, 58% were <16 years of age and 35% were admitted to hospital. Among those <16 years of age (n=2883), the most common ATV-related injuries were fractures (39%) and superficial wounds (18%). There was no significant difference in the odds of a moderate to severe injury versus minor injury among ATV users <16 years of age compared with ≥16 years of age (OR 0.94 [95% CI 0.84 to 1.06]). After adjusting for confounding, children <16 years were more likely to present with a head injury (OR 1.45 [95% CI 1.19 to 1.77]) and fractures (OR 1.6 [95% CI 1.43 to 1.81]), compared to those ≥16 years. Helmets significantly reduced the odds of an isolated severe head injury compared with a non-head injury (OR 0.35 [95% CI 0.22 to 0.55]). Compared with provinces without legislation, rates of ATV-related injuries, in particular moderate to severe injuries, decreased in children <16 years of age in provinces following the enactment of legislation for a minimum drivers age for ATV use.
CONCLUSIONS:
There was no difference in the odds of a moderate to severe injury compared with mild injury for younger or older ATV users, however youth <16 years of age are at an increased risk of head injuries and fractures compared to individuals ≥16 years of age. ATV-related injuries decreased in children <16 years of age after provincial legislation for a minimum drivers age. These data support calls for a minimum drivers age as a strategy to protect children from ATV-related injuries.
Abstract
BACKGROUND:
Subarachnoid hemorrhage (SAH) is an independent prognostic indicator of outcome in adult patients who have suffered a severe traumatic brain injury (sTBI). There is a paucity of investigations on SAH in pediatric sTBI.
OBJECTIVES:
The goal of this study was to determine SAH incidence, associated factors and its relationship to outcome in pediatric sTBI patients.
DESIGN/METHODS:
Included were 171 sTBI patients (pre-sedation GCS ≤8 and head MAIS ≥4) who underwent CT head imaging within the first 24 h of hospital admission
RESULTS:
We found that 42% of sTBI patients had SAH (n=71 of 171), and that SAH was more frequently associated with cerebral edema, diffuse axonal injury, contusion and intraventricular hemorrhage (P<0.05). Patients with SAH had higher injury severity scores (P=0.032) and a greater frequency of fixed pupil(s) on admission (P=0.001). There were no significant differences in etiologies between sTBI patients with and without SAH. Worse disposition occurred in sTBI patients with SAH, including increased mortality (P=0.009), increased episodes of central diabetes insipidus (P=0.002), greater infection rates (P=0.002) and fewer ventilator-free days (P=0.001). In sTBI survivors, SAH was associated with increased lengths of stay (P<0.001) and a higher level of care required on discharge (P=0.004). Despite a strong relationship between SAH and sTBI outcome on univariate analysis, multivariate analysis failed to demonstrate that SAH had an independent association with mortality (P=0.969).
CONCLUSIONS:
In conclusion, SAH was a frequent head imaging abnormality in almost half of pediatric sTBI patients and it appeared to be indicative of more severe TBI. As opposed to adult sTBI, SAH in pediatric patients was not independently associated with increased risk of mortality.
Abstract
BACKGROUND:
Hyperbilirubinemia is the most common cause of neonatal readmissions to hospital in Canada. The majority of neurological sequelae associated with severe neonatal hyperbilirubinemia can be avoided through early detection and proper treatment. Our previous surveillance study through the Canadian Pediatric Society (CPS) estimated the incidence of severe neonatal hyperbilirubinemia to be one in 2480 live births from 2002 to 2004. These and other studies influenced the 2007 CPS position statement “Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants (35 or more weeks gestation)”, which recommended routine bilirubin screening on all infants in the first 72 h of life.
OBJECTIVES:
To compare rates of severe hyperbilirubinemia pre- and post- introduction of the Canadian guidelines and comment on their effectiveness.
DESIGN/METHODS:
Data on infants (60 days of age or less) were collected prospectively through the Canadian Paediatric Surveillance Program. Infants born between March 2011 and February 2013 were included if they either had a peak serum total bilirubin >425 μmol/L or underwent neonatal exchange transfusion. Infants who have had exchange transfusion for well-documented Rh isoimmunization disease or who were born at less than 35 weeks’ gestational age were excluded.
RESULTS:
A total of 141 cases were reported, of which 88 were confirmed to be severe neonatal hyperbilirubinemia. The cause of hyperbilirubinemia was identified in 54 cases and included ABO incompatibility (n=33), glucose-6-phosphate dehydrogenase deficiency (n=10), other antibody incompatibility (n=5) and sepsis (n=3). Mean (± SD) reported peak bilirubin was 482±92 μmol/L (range 181 μmol/L to 788 μmol/L). Twenty infants (37%) underwent an exchange transfusion. A total of 67 infants (76.1%) were readmitted to hospital, 35 (39.8%) of them within five days of age. Comparisons with our previous surveillance data (2002 to 2004) showed that an infant was 3.48 times more likely to be diagnosed with severe hyperbilirubinemia prior to the guidelines.
CONCLUSIONS:
Severe neonatal hyperbilirubinemia continues to occur in Canada with an estimated incidence of 1.2 per 10,000; our previous surveillance data had estimated the 2002 to 2004 incidence rate to be 4 per 10,000. This significant reduction (P<0.001) is likely the result of the new Canadian Paediatric Society guidelines combined with increased physician awareness of severe neonatal hyperbilirubinemia though numerous publications in the last 10 years.
Abstract
BACKGROUND:
There is emerging evidence that non-anemic iron deficiency (NAID) in early childhood may be association with poor health and developmental outcomes. Some guidelines recommend screening for iron deficiency anemia; however, the role of screening for NAID is unknown.
OBJECTIVES:
Our overall objective was to evaluate outcomes following screening for NAID. Our specific objectives were: to determine the prevalence and risk factors associated with NAID in pre-school children; describe the practice patterns associated with the management of NAID in primary care settings; and describe the hematological outcomes of NAID with or without treatment.
DESIGN/METHODS:
A cohort study of healthy children, aged one to five years, seen for primary health care between July 2008 and June 2012 was conducted through the TARGet Kids! practice based research network. Descriptive statistics were used to describe the prevalence, risk factors, practice patterns and the hematological outcomes of children identified with NAID (defined as serum ferritin level ≤12 μg/L and a hemoglobin level ≥110 g/L). The association between NAID and potential risk factors were examined using a multivariate logistic regression analysis.
RESULTS:
Of 2276 children undergoing screening, 155 had NAID, for a prevalence of 7% (95% CI 5.95 to 8.05%). Risk factors significantly associated with NAID included younger age and those with higher zBMI. An assessment of practice patterns revealed that for 57 of 155 children (37%) an intervention for NAID was recommended (diet, oral iron or both); and for 14 of 155 children (9%) a follow-up blood test was completed to reevaluate their iron status. An assessment of the hematological outcomes of NAID with treatment (n=57) revealed that of the 14 children with a follow-up blood test, 11 children resolved their NAID and in three cases NAID did not resolve. An assessment of the hematological outcomes of NAID without treatment (n=98), revealed that of the 26 children with a follow-up blood test, NAID resolved in 17, did not resolve in eight, and in one child progressed to iron deficiency anemia.
CONCLUSIONS:
This study shows that NAID is a prevalent condition in young Canadian children; that there is substantial practice variation in management of NAID following screening. Further research is necessary to understand the benefits of screening for NAID and evidence-based practice guidelines are needed to manage NAID in early childhood.
Abstract
BACKGROUND:
Ontario uses school-based vaccination delivery for three adolescent programs: hepatitis B (HB) (since 1994/5), meningococcal conjugate (serogroup C from 2005/6, serogroups A,C,Y,W-135 since 2009/10), and human papillomavirus (HPV) (since 2007/8). HB (two doses) and quadrivalent meningococcal (one dose) vaccination is offered to grade 7 students and HPV vaccine (three doses) to grade 8 girls. Until 2012/13, all 36 Public Health Units (PHUs) assessed vaccine coverage and recorded immunization exemptions using the Immunization Records Information System (IRIS). Under Ontario legislation, for six designated diseases (measles, mumps, rubella, diphtheria, tetanus and polio), students with incomplete immunizations must be vaccinated or provide a statement of exemption, otherwise risk school suspension.
OBJECTIVES:
1) To present coverage for Ontario’s three school-based vaccination programs for the 2012/13 school year, and to relate these to recent temporal trends and national coverage targets; 2) To describe temporal trends in immunization exemptions to measles-containing vaccines (MCV) among Ontario students between 2002/3 and 2012/13.
DESIGN/METHODS:
In June 2013, IRIS immunization coverage data were requested from all PHUs for select publicly-funded vaccine antigens. Data reflected immunizations delivered as of June 30, 2013. PHU-specific data were compiled to derive provincial estimates following a validation step. Historical data from IRIS were reviewed to present historical trends in coverage and information on MCV exemptions. Trends in exemptions were expressed for seven- and 17-year-olds by classification (medical, religious/conscientious belief, total) at a provincial and regional level, and by school year and birth cohort. Poisson distribution was used to examine temporal trends.
RESULTS:
Coverage and exemptions data for 2012/13 will be presented but are currently being validated. Ontario coverage for the 2011/12 school year was 86.6% for HB, 84.4% for the meningococcal program, and 70.2% for HPV, representing notable increases in coverage for HPV (11.8%) and HB (10.0%), as compared to the 2010/11 school year. For both seven- and 17-year-old students, religious/conscientious exemptions for measles-containing vaccines significantly increased over the period of study (both P<0.001). However, the proportion of Ontario students with any exemption classification (total exemptions) remained low (<2%) and relatively stable over the period of analysis. Considerable geographic variation in coverage and exemptions was noted.
CONCLUSIONS:
School-based delivery of adolescent vaccination programs is an effective strategy for achieving high provincial coverage. Ontario data suggest that non-medical exemptions have increased over the last ten years, consistent with trends found elsewhere, although the proportion remains low at <2%.
Abstract
BACKGROUND:
Autism Spectrum Disorder (ASD) is associated with significant lifetime costs. The Early Start Denver Model (ESDM) has shown efficacy in children with ASD as young as 18 months. New service delivery models propose providing ASD-targeted treatment to young children who show signs of ASD before a diagnosis. There are no studies examining the cost-effectiveness of this model.
OBJECTIVES:
We performed a cost-effectiveness analysis comparing the costs and dependency-free life years (DFLYs) generated by pre-diagnosis intensive ESDM (ESDM-I), pre-diagnosis parent-delivered ESDM (ESDM-PD) and the Ontario Status Quo (SQ).
DESIGN/METHODS:
We took a government perspective and a time horizon to age 65. We constructed a decision-analytic model delineating three treatment pathways. We assumed 37% of children received Early Intensive Behavioural Intervention (EIBI). The ESDM-I and ESDM-PD contributed gains of 17.6 and 4.94 IQ points, respectively. These were added to expected mean IQs for children who enter EIBI before and after age four, and those who do not receive EIBI. IQ outcomes were stratified into >70 and <70. Each IQ stratum was assigned a probability of achieving an Independent (60 DFLYs), Semi-Dependent (30 DFLYs) or Dependent (0 DFLYs) outcome. Costs for each pathway were determined using the budget of an ESDM pilot project and government publications. An incremental cost-effectiveness ratio (ICER) was calculated. Discount rates of 0%, 3% and 5% were applied and a probabilistic sensitivity analysis was conducted to account for variability in costs and effects.
RESULTS:
With no discount rate applied, the SQ program cost an average of $380,000 per child over the lifetime and generated an average of 4.23 DFLYs. The ESDM-PD had an average cost of $386,000 and generated 6.86 DFLYs. The ESDM-I cost $410,000 for 7.36 DFLYs. The ICER for ESDM-PD compared to SQ was $2400 per DFLY gained, and the ICER for ESDM-I compared to SQ was $9,500 per DFLY gained. The ICER for the ESDM-I compared to the ESDM-PD was $47,500 per DFLY gained. The pattern of increasing costs and increasing effectiveness remained for both the ESDM-PD and ESDM-I when 3% and 5% discount rates were applied.
CONCLUSIONS:
From a government payer perspective, parent-delivered, pre-diagnosis ASD interventions may offer an efficient model for service delivery. Our model did not produce the savings seen in previous economic evaluations due to use of poorer prognostic expectations in our analysis. More prognostic evidence is needed for adults with ASD, particularly those who have received EIBI.
Figure 1).
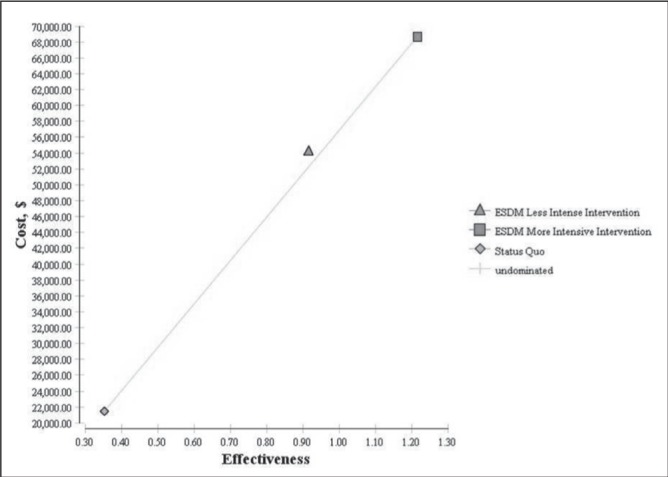
Cost-effectiveness analysis
Abstract
BACKGROUND:
The Complex Care Program (CCP) evolved from the acknowledgement that the health care system for technology dependent medically complex, fragile children and youth across the region was fragmented, with multiple organizations working in silos in order to provide care for these complex patients. To improve upon this reality, a partnership was developed between the hospital and community partner organizations working together to better serve the needs of these complex patients.
OBJECTIVES:
The goals of the CCP are to provide care coordination in a family-centered approach; to facilitate communication and collaboration among care providers; to maximize the days out of hospital and improve healthcare system utilization; with the overall objective of improving the health status of those impacted.
DESIGN/METHODS:
An outcome evaluation based on participatory evaluation and hospital utilization data was performed. The evaluation framework focused on implementation and effectiveness of the CCP since its inception in 2010 and specifically evaluated four domains: accessibility of the program, health service utilization, health outcomes and impact, and acceptability of the program.
RESULTS:
The findings of the evaluation confirmed that patients (n=33) enrolled in CCP met criteria for medical complexity, fragility and technology dependency, while it also demonstrated favorable trends and good family and stakeholder satisfaction with the program. To investigate health service utilization changes, a series of paired-sample t tests of 12 months pre versus 12 months post program initiation were performed for 19 patients. Table 1 summarizes the analysis and demonstrates a statistically significant decrease (P value 0.049) in hospital days, from 20 to seven days over one year. This resulted in over ¾ of a million in savings based on a case-costing analysis.
CONCLUSIONS:
The CCP was successful in increasing efficiency in healthcare utilization, improving health care costs, while providing service coordination that is satisfactory to the families and the stakeholders involved. These trends also show a move towards providing care in the most appropriate setting from expensive inpatient treatment to more outpatient-based treatment.
Table 1).
Differences in medical services 12 months before entry to CCP compared to 12 months after CCP Entry (n=19)
| Number of: | 12 months PRE Mean(SD) | 12 months POST Mean(SD) | t | df | p-value |
|---|---|---|---|---|---|
| ED visits | 2.58 (2.71) | 2.11 (1.73) | .791 | 18 | .439 |
| Hospitalizations | 1.89 (2.36) | 1.32 (.95) | 1.09 | 18 | .290 |
| Days in hospital | 20.95 (31.03) | 7.38 (11.87) | 2.113 | 18 | .049 |
| School visits(nursing) | 48.73 (39.43) | 92.93 (192.89) | −1.05 | 14 | .311 |
| Respite hours provided by community agency | 843.15(1344.50) | 1416.85 (1970.41) | −1.996 | 12 | .069 |
Abstract
BACKGROUND:
Resources available to manage children’s pain in the pediatric emergency department (PED) may be sub-optimal.
OBJECTIVES:
a) To evaluate currently available resources for pediatric pain management in Canadian PEDs and b) to evaluate which currently unavailable resources were felt to be most amenable to rapid implementation.
DESIGN/METHODS:
This cross sectional survey evaluated pain and anxiety management policies and procedures used in PEDs across Canada. All attendees of the 2012 Pediatric Emergency Research Canada (PERC) annual conference (>50 pediatric emergency physicians) were asked to provide a comprehensive list of pain and anxiety management interventions available at their institution. This information was then used as the basis for creation for this survey, along with expert opinion and literature review. The study tool was pilot tested for face and content validity, and data were collected via an electronic survey. The PERC site representative for each pediatric hospital across Canada was contacted to identify the most appropriate administrator to complete the survey.
RESULTS:
We had an 80% (12 of 15) response rate. Most settings (58%) did not have access to a child life specialist; 17% thought it could be easily implemented in their centre. The most frequently used distraction method was TV/video recordings (83%). Fifty-eight percent of the centre offered the parental lap/sitting position for IV insertion; another 33% felt that this could be easily implemented in their center. Local anesthetic use before IV insertion was employed by 83%; all remaining centres reported that this could be easily organised in their ED. Most settings used nurse-initiated protocols for local anesthetic (67%), acetaminophen (100%), ibuprofen (100%) and opioids (39%). Intranasal fentanyl was used in 58% of the centres; another 33% of centres felt it could be easily implemented. Only 36% of centres used nitrous oxide; all remaining centres felt it would be difficult to use. Biers blocks were minimally used (20%), and were perceived as difficult to implement by 50%.
CONCLUSIONS:
There is a wide variability in resources available at the different PEDs across Canada. We have identified some known, effective techniques for pain management (parental lap/sitting, local anesthetic for IV insertion, intranasal fentanyl) that were felt to be easy to implement. By implementing these changes first, clinicians and administrators may find greater success in addressing current deficits in children’s pain management in the PED.
Abstract
BACKGROUND:
Peripheral IV (PIV) line placement is painful, stressful and is the most common procedure performed in the pediatric emergency department (PED). First attempt cannulation success rates are variable and practitioner dependent.
OBJECTIVES:
The primary objective of this study was to investigate whether the use of either ultrasound or VeinViewer could improve the rate of success of the initial attempt at PIV placement in comparison to the current standard approach. Secondary objectives were to investigate, when compared to standard approach, whether the use of ultrasound or VeinViewer 1) reduced the number of IV punctures required to achieve successful PIV placement, 2) reduced the time taken to achieve successful PIV placement, 3) improved nursing satisfaction with PIV placement in children.
DESIGN/METHODS:
Prospective, randomized controlled trial, stratified by age, comparing three PIV placement approaches: 1) ultrasound 2) VeinViewer 3) standard traditional approach. All children aged 0 to 16, requiring PIV for routine care in the PED, were approached for enrollment.
RESULTS:
Four hundred patients were enrolled. Overall success of IV placement on first attempt was similar across study arms: Standard (109 of 146 [74.7%]); Ultrasound (97 of 137 [70.8%]); VeinViewer (89 of 135 [65.9%]); P=0.28. When stratified, differences were also non-significant. For age three and under: Standard (31 of 50 [62.0%]); Ultrasound (22 of 42 (52.4%)); Vein Viewer: (18 of 43 [41.9%]); P=0.15. For age four and above: Standard (78 of 96 [81.3%]); Ultrasound (75 of 95 [79.0%]); Vein Viewer (71 of 92 [77.2%]), P=0.77. Overall mean number of attempts did not differ significantly between groups: Standard (1.43); Ultrasound (1.40); VeinViewer (1.58). Overall time variables across groups were not significantly different. Mean times from verbalization of study arm to successful PIV were: Standard (14.8 min); Ultrasound (17.6 min), VeinViewer (16.1 min); P=0.44. Mean times from tourniquet to time of successful PIV were: Standard (6.5 min); Ultrasound (8.3 min); VeinViewer (7.8 min); P=0.50. Nurse satisfaction was not improved by use of either technology.
CONCLUSIONS:
We found no evidence that either Ultrasound or VeinViewer improves the first-attempt success rate, number of cannulation attempts, speed of cannulation for children or nursing satisfaction in the pediatric emergency department.
Abstract
BACKGROUND:
Glucocorticoid (GC) therapy is effective for the treatment of many paediatric disorders. Hypothalamic-pituitary-adrenal axis suppression (‘adrenal suppression’ (AS)) is a proven but under-recognized side effect of GC use. The incidence of AS has not been established. AS may go undetected until a physiologic stress precipitates an adrenal crisis.
OBJECTIVES:
To estimate the national incidence of paediatric adrenal crisis and symptomatic adrenal insufficiency due to AS in association with GC treatment, diagnosed by Canadian Paediatricians.
To describe the clinical features of AS at diagnosis and to document burden of illness.
To identify characteristics of children with symptomatic AS.
To generate awareness among paediatricians of the frequency of AS and associated morbidity in children on GC therapy.
DESIGN/METHODS:
Through the established methodology of the CPSP, >2500 paediatricians and paediatric subspecialists were actively surveyed monthly for two years to report new cases of symptomatic AS.
RESULTS:
Forty-four cases of symptomatic AS were confirmed. The estimated minimal annual incidence of symptomatic AS is 0.34 per 100,000 children aged 0 to 18 years (95% CI 0.25 to 0.45). Adrenal crisis occurred in six cases (14%). The most common presentations were growth failure (36%), non-specific symptoms (25%) and both growth failure and non-specific symptoms (14%). The predominant form of GC treatment in most cases was inhaled corticosteroids (ICS). Thirty-six children (82%) received ICS alone or in combination with other GC forms. The most commonly reported ICS was fluticasone (11 of 12 of those who received ICS only; 20 of 24 of those who received ICS in combination with other GC forms). Of the 11 children who received fluticasone only, doses were 500 mcg/day (n=7) or greater (n=4). Eight children (18%) received primarily systemic GCs.
CONCLUSIONS:
The minimal estimated incidence reported in our study is for the entire paediatric population and would be much higher in the at-risk group (ie, children treated with GCs). The lack of consistent, specific signs and symptoms for AS indicates that many cases may not be recognized without proactive screening. The high frequency of growth failure and/or non-specific symptoms at presentation underlines the importance of close monitoring of growth and potential symptoms associated with AS. The six cases of adrenal crisis demonstrate the potential morbidity associated with this condition. Many children received high but commonly prescribed doses of ICS. To reduce the risk of AS, physicians must be aware of the risk of AS, revisit GC doses frequently to ensure that patients are being treated with the lowest effective dose, and consider the cumulative GC dose. Further studies are needed to assess screening methods and to further evaluate risk factors and duration of suppression.
Abstract
BACKGROUND:
Adult studies have shown that increased fatigue in workers is associated with a higher risk of error. Medical incidents are preventable causes of adverse events in the hospital setting. To our knowledge, no study has assessed the impact of nurse overtime on the risk of medical incidents in the neonatal intensive care unit (NICU).
OBJECTIVES:
The objective of this study was to assess the impact of nurse overtime on the risk of medical incidents on all infants hospitalised in the NICU.
DESIGN/METHODS:
We conducted a retrospective study on all infants (n=7473) admitted in the CHU de Québec NICU (capacity of 51 beds) from April 1, 2008 to March 31, 2013. Administrative data (overtime hours per day) was obtained from the database Logibec, patient information was obtained from Med-Echo and information on medical incidents was obtained from the local incident reporting database Gesrisk. We assessed the association between administrative data and patient outcomes by using logit and probit models. Two-sample test of proportions and t test were used to assess risk factors.
RESULTS:
The mean total of worked overtime was 22.7±20.7 h. The average overtime as percentage of total daily hours of work was 4.0±3.4%. There were a total of 601 medical incidents that were reported during the study period. The most common categories of incidents were related to medication (78.9%), feeding (7.7%) and treatment (7.1%). On average, incidents happened on day of life 9.5±1.1. A total of 428 (5.7%) patients had at least one medical incident. Patients who had a medical incident had significantly smaller gestational age (32.6±0.25 weeks compared to 36.3±0.1 weeks; P<0.001)) and had a smaller birth weight (2022.2±55.3 g compared to 2786.7±10.7 g; P<0.001). Days of higher overtime (expressed as percentage of total worked hours) were significantly associated with an increased risk of medical incidents (P=0.02). Adjusted risk of suffering from a medical incident was significantly higher on days of high overtime (>8% of all hours worked) (OR=1.34; P=0.03). On days of very high overtime (>12% of all hours worked), the risk of medical incidents was greatest (OR= 1.62; P=0.045).
CONCLUSIONS:
In our study, periods of high overtime were significantly associated with an increased risk of medical incidents in the NICU. Preterm infants had the highest risk of having a medical incident. This suggests that re-organising the medical workforce to reduce nursing overtime should become an integral part in improving patient care and reducing risk of medical errors in the NICU.
Abstract
BACKGROUND:
Sleep is essential for healthy development. However, school-aged children are not getting the recommended number of hours of sleep each night. Research suggests that electronic media use is associated with shorter sleep duration and poorer sleep quality in pediatric populations. Few studies have examined this connection in school-aged children and none have employed objective measurements of sleep.
OBJECTIVES:
The aim of the current study is to examine the association between electronic media use and sleep timing and quality in school age children using objective sleep measures.
DESIGN/METHODS:
Participants included 48 school-aged children (mean [± SD] age 8.5±1.6 years). Sleep was assessed objectively using actigraphy, a wrist-watch used to examine sleep-wake patterns by assessing movement. Variables of interest included sleep duration, sleep latency, and sleep continuity. Electronic media use was assessed via parental reports of media availability and the Children’s Leisure Activities Study Survey. Electronic media variables included screen time exposure (ie, time spent watching TV/videos, playing videogames, and using the computer), and availability of electronic media (ie, TV, DVD and MP3 players, computer, radio, video game console, and cell phone) in the bedroom.
RESULTS:
More screen time was associated with significantly shorter sleep duration sleep, poor sleep efficiency, and increased sleep fragmentation (r=−0.40, P<0.01; r=−0.34, P<0.05; r=0.45, P<0.01, respectively). More time spent playing video games was associated with shorter sleep duration, poor sleep continuity (r=−0.54, P<0.01; r=−0.29, P<0.05; r=0.46, P<0.01, respectively). 12% of children had a computer in their bedroom, which was found to be strongly associated with longer sleep latency, later sleep onset, and later sleep end time (r=0.50, P<0.01; r=0.49, P<0.01; r=0.42, P<0.01, respectively).
CONCLUSIONS:
This study shows that there are significant associations between use and availability of electronic media and poorer sleep as measured by actigraphy in school-aged children. These findings support previous research utilizing subjective measures of sleep in adolescents and help shed light on the potential factors at play in the context of sleep deprivation in younger age groups.
Abstract
BACKGROUND:
Handoffs of care are a leading source of medical errors and preventable adverse events. Large scale multi-site studies assessing the impact of handoff improvement programs are lacking.
OBJECTIVES:
To determine the impact of an educational and systems-based handoff intervention, the I-PASS Handoff Bundle, on medical error rates, preventable adverse events, verbal and written miscommunications, and resident workflow.
DESIGN/METHODS:
We measured medical errors, verbal and written miscommunications, and conducted a time motion study of resident work-flow for six months before and after implementation of the I-PASS Handoff Bundle in staggered waves of implementation at nine pediatric residency training programs from January 2011 to May 2013. The I-PASS Handoff Bundle consists of communication and handoff skills training, a novel verbal mnemonic (I-PASS: illness severity, patient summary, action list, situation awareness, synthesis by receiver), a computerized handoff tool, faculty development, simulation and role play exercises, and a campaign to ensure sustainability. Error rates were measured using an established surveillance methodology including daily chart review, debriefing of post-call residents, and review of formal hospital reports. Printed handoff documents and audio recordings of verbal handoffs were reviewed for completeness. Time motion data were captured using a validated list of physician activities.
RESULTS:
We reviewed 11,087 patient admissions for errors. Following implementation of the I-PASS Handoff Bundle, rates of errors and preventable adverse events significantly decreased; there was no change in rates of non-preventable adverse events (Table 1). There were significantly fewer omissions of key patient data elements for both verbal and written handoffs. There were no significant changes in the length of handoff per patient (2.4 min vs 2.5 min per patient; P=0.55).
CONCLUSIONS:
I-PASS Handoff Bundle implementation was associated with a significant reduction in medical errors and improvements in verbal and written communication patterns without a negative impact on resident workflow.
Table 1).
Number of errors (rate per 100 admissions)
| Pre- | Post- | P-value | |
|---|---|---|---|
| Total Overall Errors | 24.5 | 17.6 | <0.001 |
| Preventable Adverse Events | 4.7 | 3.1 | <0.001 |
| Near Misses / Non Harmful Medical Errors | 19.7 | 14.5 | <0.001 |
| Non-Preventable Adverse Events | 3.0 | 2.6 | 0.48 |
Abstract
BACKGROUND:
Genetic testing for developmental problems is routine. Because of increased performance, microarray-based Comparative Genomic Hybridization (CGH) has replaced karyotyping. Up to 30% of children with developmental problems have an abnormal CGH. Using CGH results to establish diagnosis and prognosis may be complex.
OBJECTIVES:
Examine the impacts of a CGH on families of children with developmental problems.
DESIGN/METHODS:
Ongoing pilot study. Interview with families of children with developmental delay who had CGH testing.
RESULTS:
Preliminary results; n=21 parents of children zero to six years of age with developmental delay. Families identify both positive and negative impacts of CGH. The following themes were identified:
– LIMITED UNDERSTANDING of CGH and its implications by parents and families (recall, indications, benefits, limitations, implications).
– COMPLEX DIVULGATION of results: to child, siblings and family: “this is a diagnosis for the whole family”.
– GENETIC DETERMINISM: “This is why hours and hours of doing his homework with him barely worked. We now know there is little we can do” (abnormal CGH); “We will work hard because there is some hope” (normal CGH).
– GUILT: could be increased or decreased. “Deep down, I felt it was something I had done during my pregnancy. Now I know his genes are fine and I am relieved it is not”; “I also have the weird band, so does our last child. It comes from me and it is very hard to live with that” (abnormal CGH).
– ANXIETY: may be increased or decreased with both normal and abnormal tests.
– EFFECT ON HEALTHCARE SERVICES were diverse but mainly unchanged because services are based on child’s functioning. Some parents reported increased anxiety because their child was not eligible for services despite the fact that the CGH suggested that long-term disability was likely.
CONCLUSIONS:
Using CGH in the context of developmental delay can have both positive and negative impacts on families and children; both need to be discussed during pre-test counseling and when returning results. Negative impacts have been overlooked and CGH has replaced the karyotype. Increasingly detailed (and expensive) genetic testing technologies, such as whole exome sequencing, are beginning to be used in clinical settings. Before such technologies can be routinely used in practice, it is essential to appropriately assess the impacts these new genetic tests can have on children and families. Parents cannot provide informed consent without prior understanding of these impacts.
Abstract
BACKGROUND:
There is limited Canadian data on blood lead, cadmium and mercury levels in early childhood, a population that is highly vulnerable to the effects of these metals. Mercury and lead exposures have been linked to neurological effects and cadmium exposures have been linked to kidney and bone damage. Identifying subpopulations with higher levels and the assoicated risk factors is important for directing future clinical and public health intiatives in this age group of Ontario chidren.
OBJECTIVES:
To build capacity within the public health and primary healthcare sectors, collaboration between Public Health and a primary care research network for children was formed to study blood lead, cadmium and mercury levels in children <6 years of age receiving routine primary healthcare.
DESIGN/METHODS:
Children younger than five years of age receiving routine primary healthcare were recruited through this primary-care research network of family physicians, pediatricians, researchers and policy makers. Risk factors for heavy metal exposure were collected through a series of standardized questionnaires administered to the participant’s parents. In addition, a small blood sample was obtained from each child and tested for lead, mercury and cadmium.
RESULTS:
Preliminary heavy metal data was available for 205 children. Mean age was 42 months and 52% of participants were male. 70% of children were Caucasian and 30% were visible minorities. Eighty-five percent of the participants had a household income >$60,000. Geometric mean concentrations of lead, mercury and cadmium were 0.67 μg/dL (95% CI 0.63 μg/dL to 0.73 μg/dL), 0.59 μg/L (95% CI 0.45 μg/L to 0.55 μg/L) and 0.11 μg/L (95% CI 0.11 μg/L to 0.12 μg/L), respectively. Two children had mercury levels above the Health Canada methylmercury guidance of 8 μg/L. No child had abnormal lead or cadmium levels.
CONCLUSIONS:
Through a multidisciplinary collaboration, we have demonstrated that heavy metal exposure can be measured in early childhood during routine primary healthcare. In this preliminary study, two children were identified with elevated mercury blood levels. These findings should be interpreted with caution until a larger, more diverse, population of children is studied.
Abstract
BACKGROUND:
In the spring of 2008, Newborn Screening Ontario (NSO) expanded their panel to include cystic fibrosis (CF), using an immunoreactive trypsinogen (IRT)/DNA protocol. Those that are positive are referred for a sweat test, which is still considered the gold standard for diagnosis. The goal is to detect a population at risk for CF and upon diagnosis, initiate therapy, minimizing adverse outcomes. We have chosen to perform confirmatory molecular testing on each screen-positive individual, differing from some other centres in Ontario, because our hospital laboratory uses a larger mutation panel (70+6 polymorphisms) compared to that used by NSO (39 +3 polymorphisms). This aligns with the provincial recommendations set out by NSO as part of the diagnostic work up.
OBJECTIVES:
To examine whether confirmatory molecular testing using our expanded panel on all screen-positive newborns is justified.
DESIGN/METHODS:
We performed a retrospective descriptive analysis of the results of our program recorded from April 2008 to 2013 using an internal database. Particular note was made of individuals found to have a second mutation with our confirmatory panel, and of the sweat chloride obtained.
RESULTS:
337 patients have screened positive and been referred to our centre for sweat chloride testing. Of these, 25 (7.4%) have been referred with two mutations identified and 258 (76.5%) have one known mutation found. In addition, 47 (13.9%) have no known mutations, but are offered a sweat chloride as their IRT level exceeds the 99th percentile. Using our expanded panel, we uncovered a second mutation in 14 children, eight of whom would have been discharged as unaffected as they had normal initial sweat tests. Thirteen infants had a sweat chloride that fell within the ‘borderline’ range of 30 mmol/L to 60 mmol/L, of whom seven infants had two known mutations already identified by NSO, four infants had an additional mutation identified on our panel, and two infants required sequencing to identify a second mutation.
CONCLUSIONS:
To our knowledge, since the inception of this program, there have been no children with classical CF that were not identified on newborn screen. Though our approach may identify otherwise ‘healthy’ infants with a second mutation of unknown clinical relevance, given the uncertainty of the long-term prognosis associated with some mutations, we feel it continues to be warranted until more information is known.
Abstract
BACKGROUND:
Global, pediatric advisory committee guidelines recommend palivizumab prophylaxis for -infants at high risk for respiratory syncytial virus (RSV) infection and hospitalization. CARESS is a prospective registry that documents utilization, compliance and health outcomes of all Canadian infants who received ≥1 dose of palivizumab for RSV prophylaxis across 32 sites during the 20052013 RSV seasons.
OBJECTIVES:
Compare respiratory illness hospitalizations (RIH), RSV-positive hospitalizations (RSVH) and serious adverse events (SAE) among infants who received palivizumab for various indications.
DESIGN/METHODS:
Demographic data were collected at enrollment and respiratory illness-related hospitalization events were recorded monthly. Standard risk indications that qualified for RSV prophylaxis were categorized as prematurity (≤35 completed weeks gestational age), chronic lung disease (CLD) and hemodynamically significant congenital heart disease (CHD). Infants with other underlying medical illnesses such as cystic fibrosis, neuromuscular impairments, Down syndrome and immune-compromise (MI) also received prophylaxis. SAEs were recorded during each RSV season. Cox proportional hazards analyses were conducted to examine hospitalization rate differences across indications adjusting for group differences.
RESULTS:
Of the 16,290 infants enrolled, 10,576 were premature, 1290 had CLD, 1758 had CHD, and 2666 qualified with MIs. Of 211 SAE reports (excluding RIH related events), only nine were possibly related to palivizumab. After adjusting for risk factors (living with siblings, residing with ≥1 smoker in the household, family history of atopy, and multiple birth status), the hazard (hazard ratio [95% CI]; P value) for RIH was significantly higher in infants with CLD (2.49 [95% CI 2.05 to 3.01]; P<0.0005), CHD (2.20 [95% CI 1.84 to 2.64]; P<0.0005), and MI (2.02 [95% CI 1.71 to 2.38]; P<0.0005) compared to those with prematurity only. CHD infants, unlike CLD and MI, had a significantly higher hazard ratio for RSVH compared to the premature group (1.63 [95% CI 1.09 to 2.439]; P=0.018).
CONCLUSIONS:
Hazard for RIH was dissimilar across indications for prophylaxis, with CLD, CHD, and MI at greater risk for RIH than prematurity. However, only CHD infants had an increased hazard for RSVH. Palivizumab was well-tolerated across groups without any directly related SAEs.
Abstract
BACKGROUND:
The Canadian Neonatal Follow-Up Network (CNFUN) has followed the developmental outcomes of all survivors of preterm birth <29 weeks gestation in 26 centres across Canada. The variation in the incidence of CP in Canadian NICUs is not known.
OBJECTIVES:
To determine the incidence, severity and type of cerebral palsy in preterm infants admitted to CNFUN NICUs in Canada.
DESIGN/METHODS:
Preterm infants born <29 weeks of gestational age (GA) in CNFUN between April 1, 2009 and July 1, 2011 were evaluated between 18 and 24 months corrected age (CA) using standardized criteria. Demographic and neurodevelopmental outcomes, specifically incidence, severity and type of CP were compared according to GA and birth weight (BW) categories by using Pearson χ2 or Fisher exact test for categorical variables and ANOVA F-test for continuous variables.
RESULTS:
Of 2528 infants, 419 were not followed up and CP status was missing in 45. The number of infants evaluated as confirmed CP, suspect CP and no CP were 140 (6.8%), 72 (3.5%) and 1852 (89.7%) respectively. In CP, suspect CP and no CP groups, the mean BW was 908 g (223), 929 g (205) and 943 g (224) (P=0.18) and median GA was 26 weeks (25 to 27 weeks), 27 weeks (25 to 27 weeks) and 27 weeks (25 to 28 weeks) (P<0.01) respectively. The incidence, severity and type of CP by GA and BW are shown in Table 1 and Figure 1 respectively. Variation in incidence of cerebral palsy was observed in preterm infants born in Canada’s NICUs.
CONCLUSIONS:
This study provides population-based information about incidence of cerebral palsy in preterm infants admitted to Level 3 NICUs in Canada over a two-year period. The incidence of CP is greatest in the extremely preterm infants born <26 weeks of GA. The incidence of CP varies among CNFUN centers and in various centres in Canada will be explored further.
Figure 1).
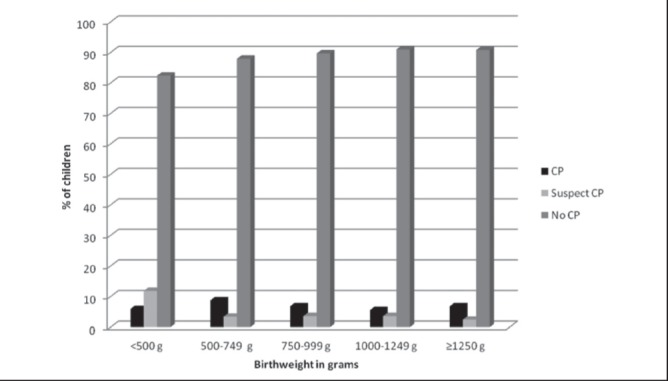
Table 1).
Incidence, severity and type of CP by gestational age
| Gestational Age (Weeks) no. (%) | |||||||
| 23 | 24 | 25 | 26 | 27 | 28 | All | |
| CP | 6(15.4) | 20(11.6) | 37(10.9) | 24(6) | 25(5) | 28(5) | 140(6.8) |
| Suspect CP | 1(2.6) | 13(7.5) | 5(1.5) | 15(3.6) | 22(4.2) | 16(3) | 72(3.5) |
| GMFCS level in CP | |||||||
| 1 and 2 | 3(50) | 12(60) | 22(59.4) | 6(25) | 8(32) | 10(35.7) | 61(43,6) |
| 3 and 4 | 1(16.6) | 5(25) | 5(13.5) | 9(37.5) | 7(28) | 7(25) | 34(24.3) |
| 5 | 1(16.6) | 2(10) | 6(16.2) | 1(4.1) | 3(12) | 5(18) | 18(13) |
| Type of CP | |||||||
| Spastic | 2(5.1) | 16(9.3) | 32(9.4) | 20(5) | 22(4.2) | 26(4.5) | 118(6) |
| Hemiplegia | 1(2.6) | 5(3) | 11(3.2) | 7(1.7) | 7(1.3) | 4(0.7) | 35(0.7) |
| Diplegia | 1(2.6) | 5(3) | 10(3) | 7(1.7) | 9(1.7) | 10(1.7) | 42(2) |
| Other | 0(0) | 5(3) | 9(2.6) | 6(1.5) | 6(1.2) | 12(2.1) | 38(2) |
| Non-spastic | 2(5.1) | 3(1.7) | 2(0.6) | 2(0.5) | 1(0.2) | 1(0.2) | 11(0.5) |
| Ataxic | 1(2.6) | 0(0) | 0(0) | 1(0.2) | 0(0) | 0(0) | 2(0.1) |
| Dyskinetic | 1(2.6) | 0(0) | 0(0) | 1(0.2) | 0(0) | 1(0.2) | 3(0.2 |
| Hypotonic | 0(0) | 3(1.7) | 2(0.6) | 0(0) | 1(0.2) | 0(0) | 6(0.3) |
Abstract
BACKGROUND:
For pediatric trainees, acquiring the skill of neonatal endotracheal intubation (ETI) is difficult because of particularities in the neonate’s airway. The videolaryngoscope (VL) technique has been used for adult and pediatric airways, and could be a method of choice in teaching neonatal ETI. On the neonatal mannequin model, VL improves success rate of ETI. However, only preliminary clinical experience has been described in newborns.
OBJECTIVES:
Assess if the VL is superior to the classic laryngoscope (CL) in acquiring neonatal ETI skill in the Neonatal Intensive Care Unit (NICU).
DESIGN/METHODS:
A randomized controlled trial was held in the NICU at CHU Ste-Justine (July 2011 to June 2013). Primary outcome: Success rate and learning curve (Generalized estimating equations). Secondary outcomes: a) Time to successful intubation (Mann-Whitney Test); b) Recognition of problems related to ETI by the supervisor and residents’ level of confidence (Independent t-test).
RESULTS:
We randomized 34 pediatric residents to perform 213 ETI using either the VL or the CL. In both groups, prior training, experience in the NICU and with neonatal ETI were similar. Patient characteristics, success rate and time to successful intubation are presented in the table. The learning curve seems better with the CL for the first two intubations, however the initial success rate in this group is lower. After the second intubation, the learning curve is similar for both laryngoscopes. Supervisors recognized problems related to visualization of glottis (P=0.02) and insertion of endotracheal tube (P=0.05) more easily with the VL. Residents’ level of confidence regarding their technical competence was higher with the CL (P=0.01).
CONCLUSIONS:
In the NICU, while learning ETI, success rate is improved with the VL. Although time to successful intubation with the VL is longer, this difference is not clinically significant. Residents have a higher level of confidence in their technical competence when using the CL, however supervisors recognize more easily problems in the ETI procedure with the VL.
Table 1).
| VL group n=101 | CL group n= 112 | P | |
|---|---|---|---|
| Patient characteristics Median gestational age - weeks Median birth weight - g Median age at ETI - weeks Median weight at ETI - g Male - n (%) |
28 6/7 1080 31 1500 65(64) |
29 1/7 1315 31 5/7 1602 68 (62) |
0,16 0,05 0,32 0,24 0,75 |
| Success Rate - n (%) | 76 (75.2) | 71 (63.4) | 0.03 |
| Median time to successful intubation - sec | 57.4 | 45.0 | 0.008 |
Abstract
BACKGROUND:
NEC remains a major cause of morbidity and mortality in very low birth weight infants. Surgery is required in a third of cases, however randomised trials have shown no difference in early mortality of NEC managed with laparotomy versus peritoneal drain.
OBJECTIVES:
To compare short term outcomes and neurological morbidities of infants with NEC treated by laparotomy or peritoneal drain.
DESIGN/METHODS:
Retrospective multicenter study on infants <33 weeks’ gestation born between January 2010 and December 2012 with NEC Stage II or greater, using Canadian Neonatal Network data. Infants were stratified by medical and surgical treatments. Significant difference between group outcomes was assessed using the Pearson χ2 test for categorical variables and Student’s t test for continuous variables. Odds ratios with 95% CIs) were calculated using standard methods.
RESULTS:
A total of 11,974 infants were admitted to 30 CNN NICUs during the study period and 214 of NEC cases (39%) required surgery. Seventy infants were treated with drain or drain and laparotomy; they had significantly lower birth weights and gestational ages, P<0.0001 and higher mortality P<0.001 than the laparotomy group. Both medical and surgical NEC infants had significantly greater rates of IVH and PVL (P<0.0001) compared to no NEC infants with decreased head growth at 36 weeks, (P<0.05). However, there was no difference in adjusted head growth at 36 weeks between those treated with drain or laparotomy at 36 weeks (−0.82 [95% CI −2.40 to 0.77], P=0.30).
CONCLUSIONS:
In contrast to previous studies, we show mortality in the peritoneal drain group is higher. Longer-term neurodevelopmental outcomes will be important to determine best practice.
Table 1).
| Variable | No NEC | NEC medical treatment | NEC drain | NEC laparotomy | NEC drain and laparatomy |
|---|---|---|---|---|---|
| Patient number | 11426 | 334 | 41 | 144 | 29 |
| Birth weight mean, g (SD) | 1137 (455) | 1113(446) | 844 (249) | 1088 (387) | 941(435) |
| Gestational age at birth, wk mean (SD) | 29.1 (2.5) | 27.5 (2.6) | 25.4 (2.0) | 27.3 (2.5) | 26.4 (2.2) |
| IVH Grade III or higher, n (%) | 1059 (11%) | 56 (18%) | 14 (35%) | 36 (26%) | 9(31%) |
| PVL, n (%) | 410 (4%) | 22 (7%) | 2(5%) | 22(16%) | 5(17%) |
| Week 36 head circumference, cm mean (SD) | 31.6 (1.8) | 30.7(2.1) | 30.2 (1.2) | 30.6 (2.4) | 30.1 (2.4) |
| Mortality, n (%) | 670 (6%) | 63(19%) | 29 (71%) | 55 (38%) | 14 (48%) |
Abstract
BACKGROUND:
Meconium aspiration syndrome (MAS) is a common cause of respiratory distress in neonatal period. Antibiotic treatment is one of medical therapy which widely used in newborns with MAS but the efficacy of routine antibiotic administration is doubtful.
OBJECTIVES:
To conduct a systematic review of the clinical trials evaluating the role of antibiotics in MAS.
DESIGN/METHODS:
We searched Medline, EMBASE, CENTRAL AND CINAHL, SCOPUS, International Pharmaceutical Abstracts, Proquest Dissertations and Theses and EBM Reviews (until August 2013). Studies were included if they satisfied the following criteria: randomized or quasi-randomized trials comparing the use of antibiotics to no antibiotics for treatment or prevention of MAS and reporting on any of the following outcomes: development of infection, need for ventilation or oxygen support, duration of hospital stay, air leaks syndrome, PPHN, need for ECMO or inhaled nitric oxide (iNO), and mortality. We calculated relative risks (RR) for the dichotomous outcomes and mean differences (MD) for the continuous outcomes, along with the 95% CIs.
RESULTS:
Four RCTs were identified; three studies enrolled subjects for treatment of MAS and one study evaluated prophylactic use of antibiotics in infants exposed to meconium stained amniotic fluid (MSAF). These trials enrolled 693 infants in total and the duration of antibiotics used was three to seven days. All studies excluded subjects considered to be at higher risk for neonatal sepsis at onset due to antenatal risk factors and/or positive septic screen. There were no difference in development of infection (RR 0.67 [95% CI 0.28 to 1.59] for clinical sepsis and 0.93 [95% CI 0.36 to 2.40] for culture-proven sepsis), mortality (RR 1.25 [95% CI 0.36 to 4.39]), need for ventilation (RR 1.16 [95% CI 0.50 to 2.66] for mechanical ventilation and 1.09 [95% CI 0.71 to 1.69] for CPAP), duration of oxygen (MD −0.64 [95% CI −1.49 to 0.21]), air leaks syndrome (RR 1.56 [95% CI 0.62 to 3.91]) and hospital stay (MD 0.16 days [95% CI −1.16 to 1.48]) between the two groups.
CONCLUSIONS:
In neonates who are otherwise at low-risk for neonatal sepsis, there is insufficient evidence to support the routine use of antibiotics for treatment of MAS or for prophylaxis in infants exposed to MSAF.
Abstract
BACKGROUND:
The MAI and AIMS have been widely used to assess infant neuromotor status. Their predictive validity with the first editions of the Bayley has been modest.
OBJECTIVES:
To examine the predictive validity of the MAI and AIMS at four months corrected age (CA) in determining neurodevelopmental outcome at 18 months (CA) using the Bayley Scales of Infant and Toddler Development 3rd edition (BSITD-3).
DESIGN/METHODS:
This retrospective cohort study included all surviving infants <29 weeks gestation born at or admitted at a tertiary care university center in 2009 to 2011 and followed until 18 months. All were assessed at four months with the MAI and AIMS by a physiotherapist and at 18 months with the BSITD-3 by a psychologist, blinded to previous test scores, and for cerebral palsy (CP) by a physician. Abnormal results were: MAI ≥14, AIMS ≤5th percentile, Bayley score ≤85 or CP. Severe outcome was: Bayley ≤70, severe CP, bilateral blindness, severe bilateral neurosensory hearing loss.
RESULTS:
Characteristics for the 133 children were: mean (± SD) gestational age 26.2±1.4 weeks, birth weight 891±202 g, 55% boys, 25% multiples, 91% prenatal steroids, 95% inborn, 94% appropriate weight for age, 65% cesarean section; and for the mothers: 30.7±5.0 years; 68% caucasian, 62% college or university education. Risk factors were: 38% bronchopulmonary dysplasia with home oxygen, 11% severe retinopathy, 7% severe cerebral anomaly, 35% sepsis, 20% patent ductus with intervention, 10% necrotizing enterocolitis.
Infants with normal MAI (≤13), compared to those with abnormal MAI (≥14), had higher cognitive, language and motor Bayley scores (all Anovas <.005); less cognitive or language score ≤85 and less severe global impairments (all χ2 <0.05). Motor score ≤85 and CP were not different. Classification according to AIMS normal or abnormal, to both tests normal, one test out of two abnormal or both tests abnormal did not improve prediction. In predicting severe outcomes the MAI had: 95% sensitivity, 47% specificity, 98% negative predictive value and 23% positive predictive value.
CONCLUSIONS:
Preterms with MAI scores ≤13 at four months have better outcomes than those with higher scores. However, both the MAI and AIMS do not strongly predict neurodevelopment status at 18 months.
Table 1).
| MAI≤13 | MAI≥14 | AIMS>5thp | AIMS≤5thp | 2 tests N | 1/2testAbN | 2 testsAbN | |
|---|---|---|---|---|---|---|---|
| n=55 | n=78 | n=36 | 11=97 | n=33 | n=25 | n=75 | |
| Cognitive | 100,1 (9,7) | 93,0 (13,5) | 100,7 (9,7) | 94,2 (13,0) | 101,8 (9,2) | 96,4 (10,3) | 93,2 (13,6) |
| Language | 94,1 (11,8) | 84,2 (14,1) | 94,1 (16,2) | 86.1 (12.6) | 97,0 (13,6) | 86.6 (12.3) | 85,1 (13,6) |
| Motor | 91,0 (10,0) | 84,3 (13,1) | 91,8 (10,0) | 85,3 (12,7) | 93,0 (9,5) | 87,0(10,1) | 84,5 (13,3) |
| Cognit≤85 | 3 (5%) | 21 (27%) | 1 (3%) | 23 (24%) | 0 | 4 (16%) | 20 (27%) |
| Langua≤85 | 12 (22%) | 33 (42%) | 10 (29%) | 35 (36%) | 7 (22%) | 8 (32%) | 30 (40%) |
| Motor≤85 | 17 (31%) | 30 (38%) | 12 (33%) | 35 (36%) | 9 (27%) | 11 (44%) | 27 (36%) |
| C Palsy | 2 (4%) | 6 (8%) | 1 (3%) | 7 (7%) | 1 (3%) | 1 (4%) | 6 (8%) |
| Severe imp | 1 (2%) | 18 (23%) | 2 (6%) | 17 (18%) | 0 | 3 (12%) | 16 (21%) |
Abstract
BACKGROUND:
The Canadian Paediatric Society (CPS) published guidelines for detection, management and prevention of hyperbilirubinemia. Proposed benefits of screening are earlier diagnosis, treatment and lower peak total serum bilirubin (TSB), including prevention of severe hyperbilirubinemia. Prior to institutional implementation of universal screening in June 2012, CPS treatment guidelines were presented at nursing education days and maternal newborn operations committee.
OBJECTIVES:
1) To determine if CPS guidelines are applied in practice; 2) To determine if peak bilirubin levels for readmitted children with jaundice are lower when guidelines followed.
DESIGN/METHODS:
Ethics board review determined this project was exempt. This retrospective chart review included 25 birth admissions and 26 infants readmitted for neonatal jaundice between June 2012 and May 2013. Cases were randomly selected. In-patient and community charts were reviewed. A data collection template was developed and CPS guidelines were applied retrospectively to determine if guidelines were followed (GF) or guidelines not followed (GNF). Data was coded into an Excel spreadsheet for descriptive and non-parametric analysis with SPSSX.
RESULTS:
No significant differences were found between GF and GNF groups, regarding maternal, delivery, baby characteristics or duration of birth admission. Peak bilirubin trends lower when GF. Among birth admissions, 63% had GF and peak bilirubin was lower when GF than when GNF (median peak bilirubin 89 μmol/L, 198 μmol/L, P=0.003). Among infants readmitted for newborn jaundice, 15% had GF at birth and median peak bilirubin trended lower when GF than when GNF (median peak 284 μmol/L, 300 μmol/L, P=0.91). The most common reasons for GNF among both admission groups (n=51) are: DAT indicated but not done (n=24), follow up as required not recommended (n=25), phototherapy not initiated when indicated (n=6), TSB not obtained within 72 h (n=2). Odds ratio for readmission is 11 when newborns do not have guidelines followed at birth admission but subgroup analysis of infants requiring DAT reveals an OR of 2.
CONCLUSIONS:
Guideline adherence does not appear to prolong birth admission and peak bilirubin trends lower. Odds ratio for readmission is higher when GNF at birth admission. A larger sample size would facilitate subgroup analysis of infants with DAT indicated (clinical jaundice within 24 h of birth, TSB in high-intermediate or high zone, TSB in phototherapy range, infant of group 0 mom and clinically jaundiced). Education and policy must ensure DAT is done when indicated, early follow-up is advised when appropriate and treatment is initiated when indicated. A standard order set is advised to promote guideline adherence.
Abstract
BACKGROUND:
Recommendations about prenatal counseling for preterm labor are based on expert opinions, while mothers’ perspectives are lacking.
OBJECTIVES:
To evaluate mother’s expectations from the prenatal consultation for preterm labor.
DESIGN/METHODS:
This was a prospective survey of hospitalized women at risk of preterm delivery 26 to 32 weeks’ GA, who had met the neonatologist for prenatal consultation in the previous 72 h. The tool was developed using data from a qualitative exploratory study; construct and content validity were accounted for through several validation phases. A single-center study was conducted in 2008, leading to a multicenter trial in three tertiary care university hospitals (April 2012 to September 2013). Variables were analyzed using χ2 tests; qualitative data was transcribed and categorized to identify emerging themes.
RESULTS:
A total of 229 of 334 surveys were returned (67.2%). It was important for almost all respondents to discuss complications of prematurity, but several other topics were also essential (Table 1). 56.6% of women wanted prematurity’s complications explained in both general terms and percentages. Most wanted written information about services offered by the NICU (91.7%), prematurity’s complications (87.3%) and how the NICU functions (86.9%). 56.4% wished to see the neonatologist again to obtain more information (evolution of prematurity over time and maternal roles for their baby), to visit the NICU or for their spouse to be present. 53.0% preferred meeting several times: they reported feeling initially too stressed and unprepared to ask questions important to them or to remember all the information. Women who did not want another meeting reported feeling well informed, but would ask to meet again if need be. Those who were offered a NICU visit or who had discussed their roles as decision makers for their baby were less likely to want to meet again (P<0.05).
CONCLUSIONS:
Women at risk of preterm labor want to address many issues important to them, including the risks of prematurity, their role as mother of a premature baby and the care they can provide for their baby. Consultations could be improved by ensuring spouses are present, by offering NICU visits or a second meeting, in which women could prepare questions important to them.
Table 1).
*4 or 5, on 5-point Likert scale
| Mothers’ perspectives | %* |
|---|---|
| Important to discuss : - Prematurity complications - Feeding strategies - Care they can provide their baby - Role as mother of premature baby - How to feel close to baby |
96% 91.4% 83.4% 82.2% 81.7% |
| Wanted to visit NICU | 68.5% |
| Wanted spouse present | 71.4% |
Abstract
BACKGROUND:
The role of chorioamnionitis (CA) in the development of retinopathy of prematurity (ROP) has not been well established.
OBJECTIVES:
To conduct a systematic review and meta-analysis of the association between CA and ROP in preterm infants.
DESIGN/METHODS:
Data Sources: The authors searched Medline, Embase, CINAHL, Cochrane Central Register of Controlled Trials and PubMed, reviewed reference lists of relevant articles, abstracts and conference proceedings (Society for Pediatric Research, European Society for Paediatric Research 1990 to 2012) and seeking results of unpublished trials, and contacted the primary authors of relevant studies.
STUDY SELECTION:
Studies were included if they had a comparison group, examined preterm infants, and reported primary data that could be used to measure the association between exposure to CA and the development of ROP.
DATA EXTRACTION:
Two reviewers independently screened the search results, applied inclusion criteria and assessed methodological quality using the Newcastle-Ottawa scale. One reviewer extracted data and a second reviewer checked data extraction. Summary relative risks (RRs) were calculated using a random effects model.
RESULTS:
We identified 1249 potentially relevant studies from the electronic databases. Twenty seven studies involving 10,590 preterm neonates with 2562 cases of ROP were included. Taking into account all included studies without adjusting for gestational age (GA), CA was significantly associated with ROP (any stage) (summary RR 1.33 [95% CI 1.14 to 1.55], I2=77%, pheterogeneity <0.0001)] and a borderline significant association was observed for severe ROP (stage >3) (summary RR 1.27 [95% CI 0.99 to 1.63], I2=74%, pheterogeneity<0.0001). There was no publication bias with Begg’s test. However, subgroup analysis of studies adjusting for GA shows no significant association on CA with ROP (summary RR 0.98 [95% CI 0.77 to 1.26], I2=0%, pheterogeneity=0.89).
CONCLUSIONS:
Unadjusted analyses showed that CA was significantly associated with ROP(any stage) as well as with severe ROP (> stage 3). However the association disappeared on analysis of studies adjusting for GA. Hence CA cannot be definitively considered as a risk factor for ROP and further studies should adjust for potential confounding factors to clarify the association with severe ROP. This study underlies the importance of taking into account all possible sources of heterogeneity across studies while interpreting the results of a meta-analysis.
Forest plot for 27 studies examining the effect of CA (any type) on ROP (any stage). RR>1 indicates increased risk of ROP in infants born to mothers with CA
Forest plot for stratified analysis of eight studies (adjusted for GA) examining the effect of CA on ROP. RR>1 indicates increased risk of ROP in infants born to mothers with CA
Figure 1).
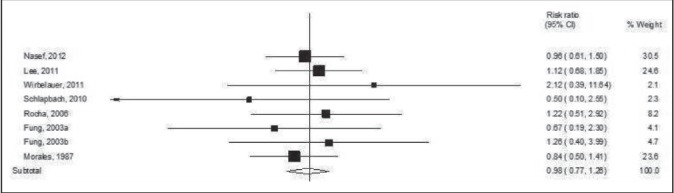
Forest plot for stratified analysis of eight studies (adjusted for GA) examining the effect of CA on ROP. RR>1 indicates increased risk of ROP in infants born to mothers with CA
Figure 2).
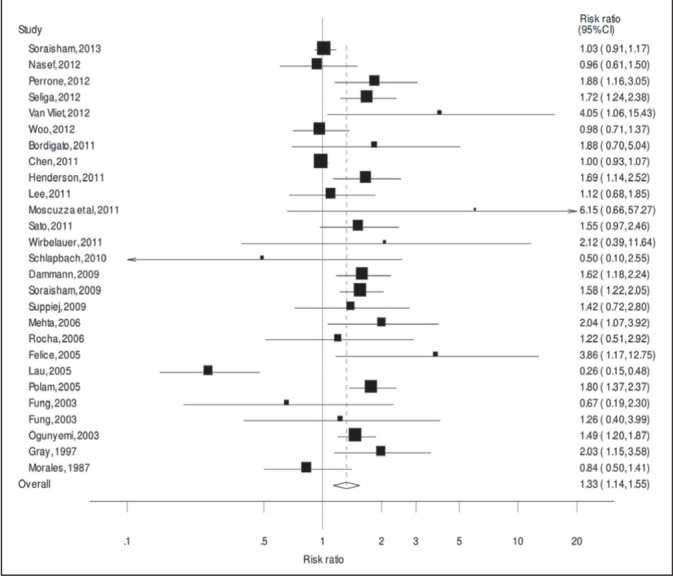
Forest plot for 27 studies examining the effect of CA (any type) on ROP (any stage). RR>1 indicates increased risk of ROP in infants born to mothers with CA
Abstract
BACKGROUND:
Instituto de Promoção da Nutrição e do Desenvolvimento Humano (IPREDE), established in 1987 in Fortaleza, Brazil, is an organization committed to providing nutrition, promoting early childhood development and women’s empowerment, as well as the social inclusion of families that live in or close to poverty. The program has no formal monitoring framework, and its long-term impact on the families it serves has never been evaluated.
OBJECTIVES:
Create a monitoring system that will enable IPREDE to monitor and evaluate the progress and quality of its interventions.
Design a prospective cohort study that uses cases and controls to evaluate the impact of IPREDE’s work.
Suggest general recommendations to improve the impact of IPREDE.
DESIGN/METHODS:
We performed open-ended key informant interviews with stakeholders from the field of Maternal and Child Health (MCH), as well as IPREDE employees. This study was conducted in January 2013 as part of a study session focusing on child and maternal health by the Harvard School of Public Health.
RESULTS:
Our evaluation and monitoring study of IPREDE first aimed to identify areas within the centre that could be improved to help optimize their impact on the community. These measures included a comprehensive monitoring system which should include the following: entry and exit interviews and data collection forms; a survey administered each visit (15 days); a survey administered every six months; a follow-up survey conducted each year after discharge from the program until the child is 17 years of age. Moreover, in order to quantitatively evaluate the causal impact of IPREDE’s work, we also proposed a prospective cohort study that uses cases and controls with surveys comparing various measures: height, weight, age, development chart until age six years, school attendance, community involvement, family income, and maternal occupation.The treatment group will consist of a cohort of children entering IPREDE during a one-year period (estimated at 1200 children) while the control group will consist of a cohort of children that share similar socioeconomic characteristics. Additional recommendations for the centre included the use of electronic records, a discharge checklist, and developing a more efficient ID system to track the mother and child.
CONCLUSIONS:
In addition to providing insight on the growth and development of children and the mothers’ capacity, the results of the evaluation can be used by IPREDE in order to obtain further funding for future programs, to increase program visibility both nationally and internationally in the field of maternal/child health and child development, and to gain insight into the potential for further improvements in IPREDE’s work.
Abstract
BACKGROUND:
Persons with disabilities were not mentioned in the eight MDGs. The Interprofessional Project on Disability – Focus on Maternal and Child Health is a bilateral Canadian/Bangladesh Canadian Government funded training/advocacy/policy project, that explicitly includes disability in maternal and child health programming.
OBJECTIVES:
To contribute to the achievement of MDG 4 (reduce child mortality) and 5 (improve maternal health) with a rights based focus.
DESIGN/METHODS:
From the baseline study regarding maternal/child health and disability (MCHD) in five Bangladesh project districts, a total of 77 women and men in two annual cohorts were selected by 10 MCH and six disability/rehabilitation organizations to participate in ‘Train the Trainer’ workshops at a rehabilitation center that works for inclusion of people with disabilities into mainstream society. Interdisciplinary participants included Physicians, Physio/Occupational/Speech Therapists, Midwives, Nurses, Family Health Visitors, Administrators. The bilingual Bangla/English curriculum module was also produced in Braille for blind participants. Interactive programmes included presentations and videos highlighting evidence based activities to prevent/reduce disability and maternal,/neonatal/child morbidity/mortality. Team activities developed knowledge translation skills to prepare them to share knowledge and learn from experiences of families with a disabled member, and also with advocates, policy makers to identify, provide appropriate health, education, social services for disability prevention and rehabilitation in large and remote communities. Canadian Faculty presented workshops at the Training Institutes for Physio/Occupational/Speech Therapists, Nurses, Midwives and the National Institute of Population and Research Training. A Distance Education Disability Certificate was also offered.
RESULTS:
In teams, participants implemented highly evaluated workshops for over 2000 MCHD providers/participants in Dhaka and in the regions. Workshops/activities for the 2013–2014 cohort were modified based on initial feedback. After the second cohort MCHD Train the Trainers program in September, 2013, the Bangladesh participants and disability advocates developed/presented an excellent interdisciplinary District Workshop. They included the practical hands on core curriculum to demonstrate birth management, basic neonatal care. They also used Bangla videos related to Child Survival and Development. Representatives from ten governmental and non-governmental organizations participated.
CONCLUSIONS:
This innovative, inclusive, rights based interprofessional collaborative project addressing disability issues within MCH programs at service, education and policy levels can contribute to achieving MDG 4 and 5.
Abstract
BACKGROUND:
Inhaled corticosteroids (ICS) are used to treat BPD despite limited evidence of efficacy and safety. Systemic corticosteroids (SCS) yield significant morbidity, but have not been recently examined in a large population-based study.
OBJECTIVES:
To examine variation in ICS and SCS use and neonatal outcomes across Canadian NICUs.
DESIGN/METHODS:
A retrospective cohort study of neonates 22≤ GA <29 weeks, receiving steroids for BPD, and admitted between 2010 and 2012 was conducted using data from the Canadian Neonatal Network (CNN) database. Demographics, ventilation status, and rates of mortality, BPD, nosocomial infection (NI), ROP, and NEC were compared between those who received ICS, SCS, and both ICS+SCS, and those who did not. ICS and SCS use were compared across sites.
RESULTS:
A total of 4087 infants met inclusion criteria; 368 (9%) received SCS, 234 (6%) ICS, and 137 (3%) both. Baseline comparison revealed a significantly lower GA (P<0.0001), birth weight (P<0.0001) and higher SNAP II score (P<0.0001) among those who received ICS and/or SCS. Antenatal steroid use was not associated with ICS and/or SCS use (P=0.05). Mortality was more common among those who received SCS after exclusion of neonates that died prior to median SCS initiation (AOR 4.98 [95% CI 3.15 to 7.88]). Severe ROP was more common in infants who received SCS (AOR 2.95 [95% CI 2.16 to 4.05]). NEC and NI preceded steroid use. Site-specific BPD rates did not correlate with SCS or ICS use. SCS use varied significantly between units (AOR range 0.0 [95% CI 0.0 to 0.0) to 4.2 (95% CI 1.1 to 16]). ICS use ranged from 0% to 39.8% (median 1.2% [IQR 0% to 8.3%]); nine sites did not use ICS.
CONCLUSIONS:
ICS and SCS are commonly used medications in Canadian NICUs, although considerable site variation exists. Further study of efficacy and safety is required to develop guidelines for neonatal steroid use.
Figure 1).
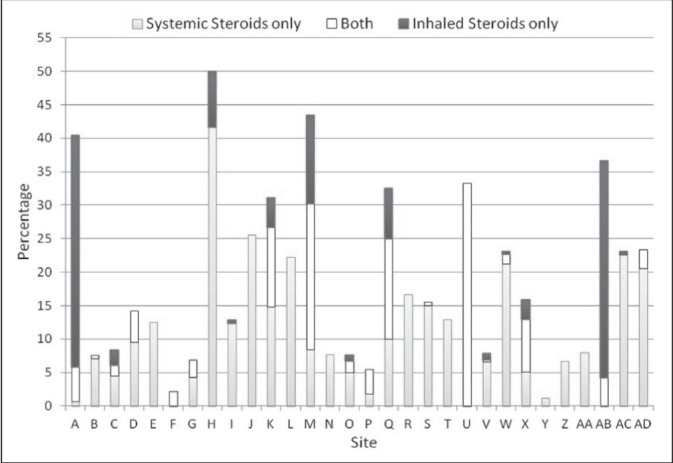
Variability in corticosteroid use across CNN sites. Y axis represents the percentage of neonates at each site.
Abstract
BACKGROUND:
Bicycle-related head injuries are an important cause of death and disability, despite the availability of helmets. It has long been recognized that individual education aimed at changing behavior is not enough to effectively prevent injury. Programs need to address environmental factors that are some of the largest determinants of health status. Actively involving the community in the planning and implementation of activities fosters enduring change and program.
OBJECTIVES:
To determine the association between bicycle helmet legislation, wide-scale community promotional effort and the use of bicycle helmets by children.
DESIGN/METHODS:
Design: Over two years, a Safe Community committee coordinated a range of activities including municipal helmet legislation, school based intervention, parent information, social media campaign, peer educators, free helmet distribution and police enforcement to promote helmet use.
SETTING: Cyclists were observed by two independent observers in July 2011 (postcampaign) in Sherbrooke, Canada. The data were compared with a similar survey completed at the same locations and days in July 2006, 2008 (precampaign). Data were collected for 319 cyclists in 2006, 212 in 2008 and 183 cyclists in 2011.
RESULTS:
Helmet use increased from 57% in 2006, to 43% on 2008 to 88% in 2011 for children cyclist (estimated five to nine years old). The greatest increase was observed among older children and young teens (10 to 15 years of age) (38% in 2006 and 32% in 2008 to 92% in 2011). Helmet used also increased in older teens and young adults (estimated 16 to 24 years of age) also increased (12% in 2006, 28% in 2008, 57% in 2011).
CONCLUSIONS:
Wide-scale, long-term community promotion appears to be effective in increasing the use of bicycle helmets
Abstract
BACKGROUND:
Attention-Deficit/Hyperactivity Disorder (ADHD) is characterized by impulsivity, hyperactivity, and inattention, which affects 5% to 10% of school-age children. The first-line treatments for ADHD are stimulant medications, such as methylphenidate and amphetamine. These medications are highly effective, but not always tolerated. Sleep side effects, such as insomnia, can lead to treatment discontinuation. They are reported for both methylphenidate and amphetamine stimulants and are usually, but not always, mild and transitory. Poor tolerability may limit efficacy by compromising the ability to prescribe optimal doses. Few studies have directly compared dose response effects of long-acting methylphenidate and amphetamine formulations in youth with ADHD, and it is unclear if there are differential effects of drug and/or dose on sleep. MAS increase norepinephrine (NE) and dopamine (DA) levels release as well as reuptake, in contrast to d-MPH, and hence could affect sleep differently.
OBJECTIVES:
We sought to determine if there are significant differences in the dose-response effects of ER D-MPH and ER MAS on objective measures of sleep.
DESIGN/METHODS:
Children, aged 10 to 17 (n=37), participated in a double-blind crossover study comparing two stimulants (extended release D-MPH, MAS) at three doses (10 mg, 20 mg, 30 mg) and placebo. Each treatment session lasted one week, for a total protocol duration of eight weeks. Sleep was assessed in all conditions using actigraphy and sleep questionnaires.
RESULTS:
Sleep duration revealed a significant dose effect on actual sleep duration (F[1, 36]=8.112, P<0.05), with significantly shorter actual sleep duration for subjects receiving 30mg compared to those on placebo (P<0.05). Sleep schedule measures showed a significant effect for dosage on sleep start time (F[1, 36]=6.284; P<0.05), with a significantly later sleep start time when children were on 20mg or 30mg dosages, compared to placebo (P<0.05). No significant differences were found between medications.
CONCLUSIONS:
Increased dosages of stimulants lead to shorter sleep duration and later sleep start times for both ER-MAS and ER D-MPH.
Abstract
BACKGROUND:
Psychosocial interventions often aim to alleviate negative emotional states. There is a growing interest in cultivating positive emotional states and qualities. Few studies have been done in a pediatric population, but results were inconclusive. We now know that the relation that children have with others, especially with their families, makes them happy.
OBJECTIVES:
To test the effect of a family-centered positive psychology intervention on subjective well-being of children.
DESIGN/METHODS:
A randomized controlled trial of a community sample of children and their family. Participants were assigned to a one-week family-centered positive psychology intervention (PPI), a control literacy intervention (CPS Read, speak, sing program) or a wait list control. The PPI consisted of a ‘Gratitude visit’ (children were given one week to write and then deliver a letter of gratitude in person to someone who had been especially kind to them but had never been properly thanked) and ‘Three good things in life’ (participants were asked to write down three things that went well each day and their causes every night for one week. In addition they were asked to provide a causal explanation for each good thing and discuss it with their family). Participants completed self-reported inventories that measured happiness (Subjective Happiness Scale [SHL] and Student’s Life Satisfaction Scale [SLSS]) and gratitude (Gratitude Adjectives Checklist(GAC)) pre-intervention, post-intervention and one month.
RESULTS:
A total of 24 children (14 girls [52%]; mean (± SD) age 10±2 years) and their family were randomly assigned to PPI (n=7), literacy intervention (n=10) or wait list control (n=7). Well-being increased significantly for the PPI group at post- and follow-up assessment on the SHL and the SLSS compared to the control or wait list group. Parents happiness (SHL) and life satisfaction increased significantly in the the PPI compared to the literacy or wait list group. No significant changes were detected on the GAC but the PPI group showed more positive emotions (optimism and enthousiasm). The perception that parents had of their child’s happiness was increased in the PPI and the literacy groups at post-assessment, and at the one-month follow-up in the PPI group.
CONCLUSIONS:
A family-centered intervention based on promoting positive emotions and well-being was effective not only in increasing psychological well-being of children but also their parents. These findings may have important implications for mental health and well-being.
Abstract
BACKGROUND:
Since 2009, a Nordic and Quebec Working Group has been working on an adaptation of the Baby-Friendly Hospital Initiative for neonatal units (Neo-BFHI). The program will be disseminated globally as a package that will include a core document with adapted standards and criteria for each of the BFHI Ten Steps to Successful Breastfeeding, as well as self-appraisal, monitoring and external assessment tools to be used by units/institutions considering or seeking Neo-BFHI certification.
OBJECTIVES:
In order to evaluate the newly-adapted tools, a pilot study was conducted to measure compliance with Baby-Friendly practices in three neonatal units with intensive or intermediate care beds in the province of Quebec that were not seeking certification at the time of the assessment.
DESIGN/METHODS:
Compliance with each Neo-BFHI criterion was measured following the same process used for Baby-Friendly certification in regular maternity units (ie, based on three sources of information – mothers; managers/staff; an external observer). A total of 32 managers/staff members (10 to 11 per hospital) have participated in the assessment interviews and to date, 71 mothers of premature or ill infants requiring neonatal care (22 to 25 per hospital) have completed the interviews.
RESULTS:
Compliance with each of the Neo-BHFI criteria was measured by the percentage of respondents giving ‘correct’ answers. For example, the assessments showed that only 6% of clinical staff confirm that transport of a stable infant from the birthing ward to the neonatal ward is performed in skin-to-skin contact/kangaroo position on a parent’s chest (Step 4), and 31% described infant stability as the only criterion for early initiation of breastfeeding (Step 5). Data collected from mothers and observations will also be presented and compared to those provided by staff.
CONCLUSIONS:
The pilot-test revealed the many challenges of measuring Baby-Friendly practices in neonatal settings, given the complexity and variability of care needs among this vulnerable pediatric population. Study findings will be used to fine-tune the adaptation and to finalize assessment tools that can be used to support the implementation and evaluation of Baby-Friendly practices in neonatal units.
Abstract
BACKGROUND:
The incidence of ‘early-onset neonatal sepsis’ (EONS) has significantly declined in North America following the implementation of guidelines for intrapartum antibiotic prophylaxis for Group B streptococcus, but the Canadian rates of EONS are not well defined. Each year, approximately 600 newborns are admitted to our Level II Intermediate Nursery (IN), of whom many receive antibiotics for ‘rule out sepsis’. However the incidence of culture-proven EONS and the distribution of pathogenic bacteria in this population is presently not well defined.
OBJECTIVES:
The primary purpose of this study is to determine the incidence of culture-positive blood infections in infants admitted to the Level II Intermediate Nursery (IN). Secondary aims will be to characterize patterns of bacterial susceptibility, specifically to the antibiotics that are currently used to treat neonatal sepsis in the IN.
DESIGN/METHODS:
In this study, blood cultures from neonates admitted to the Level II nursery over a three-year period from 2007 to 2009 were retrospectively reviewed. Ethical approval was obtained prior to data collection. Admission criteria were: >33 weeks gestation, birth weight >1500 g, mild to moderate respiratory distress, infants requiring IV fluid, infants at risk for abnormal transition, cord pH <7.0, and infants with congenital anomalies requiring observation. We excluded infants admitted from other hospitals and infants transferred to the Intermediate Nursery from the Level III NICU. Charts for infants with positive blood cultures were evaluated for clinical signs and symptoms of sepsis using our centres established sepsis protocol. The incidence of EONS was determined, and the offending bacterial pathogens were characterized.
RESULTS:
A total of 733 blood cultures were reviewed during the three-year period, of which 12 were positive for bacterial growth. Six were identified as contaminants based on species and clinical manifestation. The overall incidence of EONS was found to be between 0.4% to 1.3% of cultured patients, with the most common organisms being coagulase-negative Staphylococci, followed by Streptococcus agalactiae. All clinically significant isolates were sensitive to ampicillin and gentamycin.
CONCLUSIONS:
The incidence of culture positive EONS in a cohort of neonates >33 weeks’ gestation at a major Canadian level II nursery is extremely low. In light of these findings future work will focus on further characterizing risk factors for true EONS, with a view to reducing the number of infants, at potential risk, who receive empiric antibiotics in the first days of life. This would have positive implications for the burden of care of IV antibiotic administration, as well as financial savings and benefits for the gut microbiome.
Abstract
BACKGROUND:
TH use within 6 h of birth in newborns with HIE reduces the risk of death and neurologic impairment. The Northern Alberta Neonatal program provides a regionalized service covering a catchment area of 440,000 square kilometers. TH became a standard of care in Edmonton since July 2006.
OBJECTIVES:
Audit the implementation of TH for HIE in a regionalized setting including initiation in referral centres from July 2006 to September 2013.
DESIGN/METHODS:
This is a prospective review of newborns ≥35 weeks with HIE and <6 h old on initiation of TH . A stepwise protocol of a qualifying perinatal event (one of acidosis [pH <7.0 or BE ≥−16 by arterial cord or gas ≤1 h of age], Apgar score [≤5 at 10’] or continued resuscitation at 10’) followed by an abnormal neurological exam of moderate or severe encephalopathy. Amplitude integrated electroencephalogram was used as an adjunct to clinical decision making. From July 2006 to April 2007 TH was initiated only at level 3 centers and thereafter passive cooling was started at the referring centre and continued actively by the neonatal transport team, using gel packs, en-route to level 3 centers. TH was continued for 72 h.
RESULTS:
Of 169 eligible newborns, 123 (73%) were cooled, only one of
15 (7%) prior to 2007 vs 122 of 154 (79%) after. Ninety-three of 123 (76%) were outborn and 77 of 93 (83%) were cooled on transport. 116 of 123 (94%) had at least one perinatal event (70% had acidosis, 68% had Apgar ≤5 at 10’, and 81% required resuscitation at 10’). All had abnormal neurologic exam and 20 of 123 (16%) died. All surviving newborns are being followed for neurodevelopmental outcomes.
CONCLUSIONS:
Despite the vast catchment area and transport time, sometimes >6 h, the initiation of TH for newborns with HIE prior and during transport could be achieved in a timely manner in >80% of cases. Recognition and timely referral is crucial in reducing risk of mortality and morbidity in these newborns.
Table 1).
Eligible and cooled newborns and age to target temp. *Mean ± SD
| Yr | 2006/2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|
| Eligible n | 26 | 21 | 27 | 24 | 25 | 27 | 19 |
| Cooled n(%) | 6(23) | 10(48) | 22(81) | 22(92) | 22(88) | 24(89) | 17(89) |
| Initiation age (hrs)* | 5.4±0.6 | 4.4±1.1 | 3.8±1.6 | 3.3±1.6 | 2.7±1.5 | 2.5±1.6 | 3.2±1.5 |
| Age target temp (hrs)* | 6.8±1.2 | 5.5±1.6 | 5.6±1.7 | 5.1±2.7 | 4±1.9 | 4.4±2.2 | 5.7±2.6 |
Abstract
BACKGROUND:
The World Health Organization defines paediatric palliative care as holistic care for mind, body and spirit of the child with life threatening/life limiting conditions and his/her family. Neonatal palliative care is increasingly recognized as an important aspect of the care of critically ill neonates, especially with increasing survival of extremely premature infants with complex medical issues. However, neonatal palliative care is not being implemented in a comprehensive manner in many neonatal units across North America.
OBJECTIVES:
The aim of the study is to explore the concept of ‘neonatal palliative care’ as understood by parents and health care professionals in the neonatal intensive care unit (NICU) setting in Edmonton, Alberta. The secondary aim is to identify the factors that either enable or impede delivery of palliative care to these infants and their families.
DESIGN/METHODS:
Four focus groups composed of NICU nurses/nurse practitioners, neonatologists and parents whose critically ill infants had received care in the NICU were conducted. Data from the focus groups were analysed using qualitative content analysis.
RESULTS:
Anticipated death of a critically ill infant is a tragic, traumatic and paradoxical event, primarily for the families, but also for the health care professionals involved in providing treatment and care. The parents, while acknowledging the high quality of care delivered, expressed a need for consistent care and support as well as respect for the role of parents in the decision-making process. The nurses emphasized the need for better communication, support to families and nurses and early identification of the need for palliative care. The physicians acknowledged the lack of specific training they had in effective delivery of palliative care, and ambiguity as to how this should be delivered. Most saw this as part of their own role. Lack of suitable private space for palliative care, absence of a written policy and limited resources were expressed as obstacles, while the quality of care and a family-focused approach were acknowledged as facilitators in the process of delivering palliative care. The need for an on-going education in palliative care and creating a multi-disciplinary team support was emphasized by health care professionals.
CONCLUSIONS:
Delivering Neonatal palliative care is a complex multidisciplinary process that is resource intensive requiring specialised skill sets. Various factors that would enable or impede effective palliative care delivery were identified. The need for developing a broader, integrated and flexible model of palliative care that includes prenatal and post bereavement care was underlined.
Abstract
BACKGROUND:
The use of peripherally inserted central catheter (PICC) via a peripheral vein has become routine for providing nutrition, fluids and medicaments to premature and ill newborns. PICCs are usually placed in the upper and lower extremities.
OBJECTIVES:
To review our experience with scalp vein placed PICCs.
DESIGN/METHODS:
A retrospective review of neonates who had PICC inserted from January 2010 to June 2013 was conducted. Data retrieved and analyzed were: birth weight (BW), gestational age (GA), gender, site of insertion, duration in place and complications, including: central line associated blood stream infection (CLABSI), extravasation of fluid, mechanical (occlusion, phlebitis and leakage) and migration to non-central positions on follow-up.
RESULTS:
We identified 691 PICCs, with 64 inserted via scalp veins, 142 in the lower limb and 485 in the upper limbs. All but two neonates survived to discharge from hospital (97%). Median BW and GA were 2757 g (IQR 2308 g to 3153 g) and 37 weeks (IQR 35 to 39 weeks), respectively. Scalp PICCs were inserted via left temporal veins in 33 (52%) neonates and via right temporal veins in 31 (48%) neonates. There was a slight predominance of male gender 38 (60%). Median age at insertion was eight days (IQR five to 15 days). Median duration of placement was 12.5 days (IQR eight to 22 days). PICC tip location was central (tip at T3–T7 or within brachiocephalic vein or medial to clavicle) in 54 (84%). The incidence of CLABSI was 2.4 per 1000 catheter-days. Two infants (3%) had infiltration complications (one pleural effusion and one extravasation of TPN fluid into soft tissues) and two (3%) had occlusion. No leakage or phlebitis was reported. Among 19 neonates with chest x-ray done within two weeks after PICC insertion, three (16%) had migration of PICC tip to a non-central positions. PICCs with non-central tip position, at the time of insertion, were associated with shorter catheter days (13.5 vs. 7.0; P=0.032) and a trend towards higher mechanical or infiltration complications (20.0% vs. 3.7%; P=0.112) compared with those having a centrally placed PICC tip.
CONCLUSIONS:
PICC placement via scalp veins offers a safe and useful alternative for providing central venous access in neonates. Non-central tip position can be associated with a shorter duration of catheter use and higher rate of mechanical or infiltrative complications.
Abstract
BACKGROUND:
Recommendations about prenatal counseling for pre-term labor, based on expert opinions, emphasize informing parents. Mothers’ perspectives are lacking.
OBJECTIVES:
To evaluate mother’s experiences of prenatal consultations for preterm labor.
DESIGN/METHODS:
This was a prospective survey of hospitalized women at risk of preterm delivery 26 to 32 weeks GA, who had met the neonatologist for prenatal consultation within the last 72 h.The tool was developed using data from a qualitative exploratory study; construct and content validity were accounted for through several validation phases. A single-center pilot study was conducted in 2008, leading to a multicenter trial in three tertiary care university hospitals (April 2012 to September 2013). Variables were analyzed using Chi2 and Student T-tests.
RESULTS:
A total of 229 of 334 surveys were returned (67.2%). Sixty-five percent of consultations were performed by one healthcare provider, with neonatologists providing most explanations (77.9%). Participants’ overall experiences were positive (89.9%). Consultations lasted 10 min to 20 min (68.1%); length of meeting was associated with women feeling informed about prematurity, prepared for their role as mother, and reassured (P<0.001). Complications of prematurity were explained adequately for 53.9% of women and in too much detail for 39.3%. Sixteen percent of women did not receive data on prematurity’s complications; of those who did, most obtained it in general terms (72.0%). After the meeting, women felt very well informed about prematurity (mean 4.4 on a 5-point Likert scale), but they felt less well prepared as the mother of a premature baby (mean 3.65; P<0.001). More highlights and potential improvements are presented in the table.
CONCLUSIONS:
Prenatal consultations with a neonatologist are strongly appreciated. Information about prematurity predominates the physicians’ discourses. This study informs clinicians about potential improvements, especially in light of mothers’ priorities..
Table 1).
*4 or 5 on a 5-point Likert scale
| Highlight: Meeting neonatologists | Good bond with neonatologist* | 87.3% |
| Good bond with neonatologist* | 96.0% | |
| At ease to discuss issues important to them* | 87.7% | |
| Information relevant to their situation* | 88.5% | |
| Spouse absent | 51.1% | |
| Improvements possible | Not warned about meeting | 19.2% |
| Clinicians’ roles not explained | 18.9% | |
| Offered NICU visit | 34.4% | |
| Received explanations on decision-making processes for baby | 24.8% |
Abstract
BACKGROUND:
Although Peripherally Inserted Central Catheters (PICC) provide vascular access to newborns who require parenteral nutrition (PN) and medications, they can be associated with complications that lead to significant morbidity and mortality.
OBJECTIVES:
To describe the characteristics of major complications other than sepsis associated with PICC use in a large level 3 NICU.
DESIGN/METHODS:
A retrospective review of major PICC related complications (PICC-RC) in newborns was conducted for the five year period, 2008 to 2012. Approximately 1,000 PICCs were inserted and provided 74,000 catheter-days. The following complications were audited: pleural effusion (PLE), pericardial effusion, ascites, retroperitoneal collection, significant extravasations in soft tissues requiring surgical intervention, and cardiac arrhythmia.
RESULTS:
Major PICC-RC were identified in 10 infants during the study period. Newborns were of a median gestational age 32 weeks [IQR 26 to 37 weeks] and birth weight 1373 g [IQR 590 g to 2979 g]. PICCs were inserted at a median age of five days [IQR three to nine days]. Median time from catheter insertion to development of PICC-RC was 16 days [IQR 13 to 28 days]. The incidence of the commonest PICC-RC, PLE (seven of 10), was 0.09 per 1000 catheter days. No PICC related pericardial effusion was identified. All except one PICC catheter tip was located in a central position at time of insertion (catheter tip T3–T7 inserted from upper limb [UL]/scalp or tip T9 to L1–L2/L3–L5 from lower limb [LL]). In all cases of PLE, catheter tips were centrally located at insertion but migrated to subclavian veins or tributaries at the time of events. Two newborns born at 24 weeks deteriorated and succumbed after major PICC-RC.
CONCLUSIONS:
Major complications of PICCs are rare but can be life threatening and occasionally associated with death in extremely low birth weight infants. PN-related PLE is the most common major PICC-RC and can be associated with migration of PICC tips to non-central locations despite positioning the catheter tip optimally at the time of insertion.
Table 1).
Characteristics of major PICC-RC
| Major Complication | Pleural effusion (median; range) | Intra-abdominal collection | Extravasation Into soft tissue requiring incision | Ataril flutter |
|---|---|---|---|---|
| Total number of patients | 7 | 1 | 1 | 1 |
| Gestation age, weeks | 28 (24–38) | 24 | 37 | 37 |
| Site of insertion | UL - 6; Scalp - 1 | LL | Scalp | UL |
| Day of developing complication post insertion | 16(7–75) | 35 | 15 | 4 |
| Outcome | 6 Alive; 1 Dead | Dead | Alive | Alive |
Abstract
BACKGROUND:
Endotracheal intubation (EI) is recommended in neonatal resuscitation whenever chest compressions (CC) are indicated. Laryngeal mask airway (LMA) is used effectively to provide positive pressure ventilation (PPV) to newborns after delivery but the efficacy of LMA during PPV with CC is not well studied.
OBJECTIVES:
To determine if LMA or EI deliver comparable tidal volumes, inspiratory (VTi) and expiratory (VTe), during PPV and CC in neonatal piglets.
DESIGN/METHODS:
Twenty four- to six-day-old piglets (with weight 1.8 kg to 2.8 kg) were randomized to either EI (size 3.5 cuffed [n=9]) or LMA (size 1.5 [n=11]); mechanically ventilated; anesthetized with ketamine/propofol; and paralyzed with rocuronium. Arterial and venous lines were placed. Respiratory flow and airway pressure were measured continuously using a pneumotach, pressure transducer, and WinDaq acquisition system. Two-minute samples were recorded, and blood gases analyzed during baseline ventilation (BL), PPV with T-piece resuscitator (TP), and PPV with CC (TPCC) at 3:1 ratio.
RESULTS:
LMA insertion failed in one animal mandating EI. Ten animals were analyzed in each group. At BL there was no significant difference between EI and LMA in VTi, VTe, VT leak, Positive end expiratory pressure (PEEP), ventilator rate, FiO2, PaCO2, or PaO2. Peak inspiratory pressure (PIP) was significantly higher with LMA; mean difference was 1.6 cm H2O, and 95% CI (0.12 to 3.1). Respiratory data during TP and TPCC are presented in Table 1. Comparing TP to TPCC showed that adding CC resulted in higher leak (P<0.05), lower PEEP (P<0.001) and lower PaO2 (P<0.001). Abdominal distension was observed with LMA but not EI, with postmortem gastric air aspirates of 22 to 80 mL.
CONCLUSIONS:
LMA provided comparable VT to EI during PPV and PPV with CC with slightly higher PIP. EI resulted in lower PaCO2 levels, which was within acceptable limits with both devices. Newer LMAs which allow decompression of the stomach as well as the efficacy of LMA in restoring spontaneous circulation after asphyxia should be investigated.
Table 1).
Respiratory data and blood gases during TP and TPCC. Values are presented as mean ± SD, except leak is presented as median (IQR). *P<0.05 when comparing EI and LMA
| TP | TPCC | |||
|---|---|---|---|---|
| EI | LMA | EI | LMA | |
| VTe (ml) | 30.1 ± 3.8 | 25.8 ± 9.7 | 29.9 ± 6.5 | 29.7 ± 3.4 |
| Leak (%) | 10 (3,20) | 14 (8,55) | 28 (23,40) | 34 (25,39) |
| PIP (cm H20) | 18.4 ± 2 | 20 ± 1.7 | 18.4 ± 2.2 | 20.9 ± 2.9 * |
| PEEP (cm H20) | 6 ± 1.1 | 6.1 ± 0.9 | 4.3 ± 1.1 | 4 ± 0.8 |
| PaC02 (torr) | 38.1 ± 6.1 | 44.1 ± 6.1 * | 37.5 ± 4.2 | 43.7 ± 4.6 * |
| Pa02 (torr) | 73.9 ± 11.1 | 68.5 ± 6.9 | 55.1 ± 10.6 | 53 ± 5.7 |
Abstract
BACKGROUND:
Blood product transfusions are common in NICU, but transfusion practices are not well described.
OBJECTIVES:
To describe the incidence and determinants of red blood cells (RBC), plasma and platelets transfusions in our NICU.
DESIGN/METHODS:
Single-center prospective observational cohort study. All neonates admitted to the NICU of CHU Sainte-Justine Hospital (level 3B) from May 30 to August 6 2013 were included. Daily data were extracted from medical charts using a validated case report form up to 44 weeks post conception or discharge. Clinician’s justifications for transfusion were assessed using a questionnaire.
RESULTS:
All 152 patients admitted in the NICU during the study period were included. Mean (± SD) birth weight (BW) and gestational age (GA) were 2.41±1 kg and 34.4±4.3 weeks. At least one RBC, plasma or/and platelets transfusion was given in 19 (12.5%) patients. RBC, plasma and platelets were transfused to 16 (10.5%), seven (4.6%) and seven (4.6%) patients respectively. Six (37.5%) of the RBC, three (43%) of the plasma and four (57%) of the platelets transfused patients received single transfusion. Donor exposure was restricted to only one in 14 (87%) of RBC, in four (57%) of plasma and in five (71%) of platelets recipients. Compared to non transfused patients, those who received at least one blood product transfusion had a significantly lower platelets level on the cord sample (172×109/L vs 236×109/L; P=0.01). Sex, GA, BW, cord hemoglobin (Hb) were comparable among both groups. Transfused patients were more frequently admitted for suspected bacterial infection (P=0.01) and hypoxic-ischemic encephalopathy (HIE) (P<0.001). At admission, neonates with higher SNAPPE-II score (P<0.001), on high frequency ventilation (HFV) (P<0.001) and with lower Hb (138 g/L vs 175 g/L; P<0.001) were more likely to receive transfusion during their NICU stay.
Most frequently quoted justifications for RBC transfusions were repectively 1 – low Hb level, 2 – intent to improve oxygen delivery and 3 – severity of the illness.
CONCLUSIONS:
In this study, transfusions were not as frequent as expected. Lower platelets count on the cord sample and admission for bacterial infection or HIE are associated with transfusions in NICU patients. A higher SNAPPE-II score, HFV and lower Hb at admission in NICU are significant determinants for later RBC, plasma and/or platelets transfusions.
Abstract
BACKGROUND:
Advances in perinatal-neonatal care over the last 30 years have significantly reduced mortality rates of extremely premature neonates. As the gestational age (GA) at birth increases, morbidity rates at discharge decrease. The distribution of morbidity free survival (MFS) for neonates born extremely premature in Canada is presently unknown.
OBJECTIVES:
Estimate MFS by GA among extremely premature neonates.
Identify the lowest GA at which survival without moderate or severe morbidities (MFS) at discharge is possible and the associated maternal and neonatal characteristics at this GA.
Compare MFS rates between genders.
DESIGN/METHODS:
This retrospective observational study examined data collected prospectively by the Canadian Neonatal Network™ (CNN) on neonates born at 22+0 to 29+6 weeks GA and admitted to neonatal intensive care units participating in the CNN from 2003 to 2012. Neonates who were moribund on admission, had major congenital anomalies or missing information were excluded. Survival and MFS (survival free of all five major short term morbidities, ie, lung injury, brain injury, necrotizing enterocolitis, retinopathy of prematurity and nosocomial infection) rates were calculated for each GA. At the lowest GA with MFS, maternal and neonatal characteristics were assessed for association with MFS by Chi-square or Fisher exact test for categorical variables and t-test for continuous measures. Similar analyses compared MFS between genders at each GA.
RESULTS:
Study subjects included 16,312 neonates. The lowest GA at which MFS is possible was 23 weeks (4.6% [95% CI 2.7% to 6.5%]). The largest, 2.3-fold relative increase in MFS rates occurred between 24 and 25 weeks GA. Subsequently, MFS increased linearly each week up to 29 weeks GA (Figure 1). Factors predictive of MFS at 23 weeks GA included cesarean section delivery, maternal antibiotics and maternal hypertension (P=0.03). Antenatal steroids (P=0.07) and female gender (P=0.08) may also impact MFS. Females had higher MFS rates at 25, 27, 28 (P<0.01) and 29 (P<0.001) weeks GA.
CONCLUSIONS:
The lowest GA at which MFS is possible in Canada is 23 weeks. In addition to antenatal steroids and maternal antibiotics, maternal hypertension was also associated with MFS at this GA. Females had higher MFS rates after 24 weeks GA. Future studies are needed to explore the long term neurodevelopmental outcomes of morbidity free survivors on a national scale. This may help to guide clinicians and parents in critical care decision making.
Figure 1).
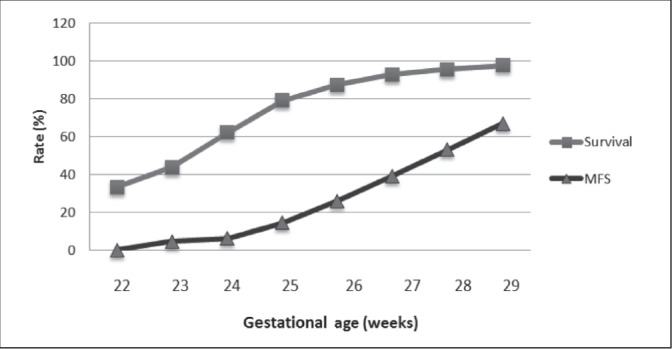
Survival and morbidity free survival (MFS) by GA
Abstract
BACKGROUND:
As effective treatment for infants born very preterm has decreased mortality, the NI risk in that population has increased. The impact of NI on mortality and morbidity is unclear and the trends in NI rates in Canadian NICUs has not been well documented.
OBJECTIVES:
To characterize recent trends of NI among preterm infants admitted to Canadian Level 3 NICUs during 2008–2012, and assess the impact of NI trends on trends in neonatal mortality and severe morbidities.
DESIGN/METHODS:
A retrospective observational cohort study was performed on infants born <33 weeks gestational age and admitted to 24 NICU sites participating in the Canadian Neonatal NetworkTM during 2008–2012. NICU sites were classified into three groups according to baseline NI rates in 2008 using Cochrane-Armitage trend test (14% or less, 15% to 19%, more than 19%). Data was extracted from health records after discharge using standardized definitions and manual of operations. Association of NI trends and trends in the composite mortality/morbidity were tested using multivariable logistic regression after adjustment for potential confounders and important risk factors.
RESULTS:
Sites with high baseline NI rates showed significantly decreasing trends in the following years however no significant NI trends were detected for sites with low or medium baseline NI rates. The trend in composite mortality/morbidity was significantly decreased for sites with decreased NI trends (OR 0.89 [95% CI 0.85 to 0.93]), but no significant trend in mortality/morbidity was detected for sites with increased NI rates. However a decreasing trend in mortality/morbidity was also observed in sites with constant NI rates.
CONCLUSIONS:
NI trends decreased only for sites with high baseline NI rates, which indicates that future reporting of NI rates must account for baseline NI rates. NI trends may affect NICU mortality/morbidity but further research must be done to determine the exact relationship between these variables.
Abstract
BACKGROUND:
A delay in cord clamping improves outcomes of pre-term babies and is currently recommended by professional societies (SOGC and ACOG). However, guidelines for managing umbilical cord clamping after preterm birth do not clarify specific indications, contraindications and procedural steps. Clinical trials select healthier babies and defer to immediate clamping in the presence of certain criteria, including fetal compromise, placental abruption, need for resuscitation, and when the resuscitation team is not present. Thus many high risk babies have immediate cord clamping by design.
OBJECTIVES:
To audit outcomes of babies born at <33 weeks gestational age (GA) who receive immediate vs later cord clamping.
DESIGN/METHODS:
The Royal Alexandra Hospital is a tertiary perinatal centre with a delayed cord clamping protocol of 45 s to 60 s for preterm babies. Charts were reviewed of babies with the above indications for immediate clamping (IC), and from those in whom later clamping (LC) occurred. Data fields included patient demographics, early neonatal outcomes, and outcomes at the time of discharge
RESULTS:
Between May 2008 and Dec 2009, the LC was provided in 236 babies. IC was indicated and occurred in 131 babies. The IC group was significantly smaller, more preterm and more likely to be born by C-section than the LC group (Table 1). The IC babies had lower 5 min Apgars; were more likely to be ventilated in the delivery room; had lower initial hemoglobin levels; were three times more likely to require blood pressure support with volume expansion or inotropes; received twice as many blood transfusions; and trended to higher mortality.
CONCLUSIONS:
Indications for IC select for smaller, sicker babies who have worse outcomes than those who are eligible for later clamping. Resuscitation with the cord attached or alternative placental transfusion strategies, such as cord milking or stripping, should be investigated in the IC population.
Table 1).
t test for continuous variables. χ2 (or Fisher exact) for proportions. Percentages or SDs in brackets
| Later clamping (n=236) | Immediate clamping (n=131) | p-value | |
|---|---|---|---|
| Gestation (weeks) | 29.6 (2.0) | 29.1 (2.2) | 0.030 |
| Birthweight (g) | 1454 (402) | 1362 (375) | 0.033 |
| Cesarean section (%) | 115/236 (48.7%) | 91/131 (70%) | 0.000 |
| Death (%) | 4/236 (1.7%) | 7/131 (5%) | 0.060 |
| 5-minute Apgar | 7.6 (1.6) | 6.8(1.8) | 0.000 |
| 5-minute Apgar <7 (%) | 50/236 (21.2%) | 58/131 (44%) | 0.000 |
| Delivery room ventilation (%) | 62/235 (26.4%) | 70/131 (53%) | 0.000 |
| Initial Hb (g/1) | 166 (20) | 156 (26) | 0.000 |
| BP support (%) | 19/235 (8.1%) | 32/131 (24%) | 0.000 |
| Max bilirubin (micromol/l) | 180 (44) | 170 (47) | 0.039 |
| Any RBC transfusion | 34/236 (14%) | 38/129 (29%) | 0.001 |
| Nosocomial infection (%) | 16/235 (6.8%) | 8/130 (6.2%) | 0.106 |
| Preterm brain injury (%) | 12/233 (5.2%) | 7/129 (5.4%) | 0.920 |
| Necrotizing enterocolitis (%) | 3/236 (1.3%) | 3/129 (2.3%) | 0.670 |
Abstract
BACKGROUND:
Despite specific benefits for infants and mothers, breastfeeding initiation at birth remains problematic in the subgroup of obese women.
OBJECTIVES:
To evaluate the incidence of breastfeeding initiation at hospital, according to maternal pre-pregnancy body mass index (BMI) in “Grossesse en Santé”, a large prospective birth cohort in Quebec City.
DESIGN/METHODS:
Data (2005 to 2010) includes pregnant women with a singleton, with delivery expected in a second or third line hospital. Sociodemographic and prenatal factors including women’s weight and height were self-reported by questionnaire within 12 weeks of gestation. Initiation of breastfeeding at hospital as well as intra- and postpartum data were collected from the mother’s and infant’s obstetrical chart. Log-binomial analyses were performed to assess relative risk between maternal BMI and breastfeeding initiation in a model including pre- and post-natal determinants.
RESULTS:
Among participants (n=6592), 13% were obese, 48% were primiparous, 97% were Caucasian, 10% were smoker and 40% had a university degree. Average maternal age was 30±4.3 years, gestational age at birth was 39.4±1.5 weeks and 21.21% of mothers gave birth by C-section. Compared with normal weight, obese women (BMI ≥30 kg/m2) initiated less often breastfeeding before discharge home (RRunadj 1.69 [95% CI 1.44 to 1.98]) even after adjustment for multiple prenatal factors including education, smoking, maternal age and parity (RRadj 1.25 [95% CI 1.08 to 1.46]). After introduction in the previous model of the per- and post-natal perinatal factors (eg, type of delivery, gestational diabetes, type of anesthesia, gestational age, baby’s weight, neonatal unit transfer), the association was decreased indicating that these factors determined breastfeeding initiation after birth (RR 1.18 [95% CI 1.005 to 1.19]). However, it still remained statistically significant highlighting a potential role of other behavioural factors such as mother’s motivation. Indeed, documented in a subgroup of the cohort (year 2009 to 2010, n=1174), prenatal intention of breastfeeding was decreased in the obese population, with an increased risk of bottle-feeding intention compared with normal weight women (RRunadj 1.72 [95% CI 1.10 to 2.68]).
CONCLUSIONS:
Maternal obesity is associated with poor breastfeeding issues. Both pre and post natal factors should be targeted by interventions in this population, considering the specific breastfeeding benefits and the increasing rates of obesity. Perinatal professionals should be aware of this reality.
Abstract
BACKGROUND:
The Canadian Neonatal Follow-up Network (CNFUN) monitors the outcomes of infants born <29 weeks gestational age (GA) at 26 neonatal follow-up centres across Canada. The use of a standardized assessment tool, the Bayley Scales of Infant and Toddler Development – Third Edition (Bayley-III), at a common age allows for systematic evaluation of cognitive, language and motor development across sites.
OBJECTIVES:
To describe the cognitive, language and motor development at 18 to 21 months corrected age (CA) for the cohort of CNFUN preterm infants born April 1 2009 to July 1 2011.
DESIGN/METHODS:
Trained and qualified Bayley-III testers administered the assessment of cognitive, language and motor abilities to preterm infants at 18 to 21 months CA. Bayley-III composite scores are normally distributed and have a mean of 100, SD 15. Scores <85 are considered below the normal range and are defined here as indicating impairment.
Results are presented by gestational age at birth (GA) and by birthweight (BW) category.
RESULTS:
Of 2528 infants born <29 weeks GA, 2109 (83.4%) were seen in follow-up at 18 to 21 months CA. Cognitive composite scores were obtained for 1958 (92.8%) infants, language composite scores for 1899 (90.0%), and motor composite scores for 1887 (89.5%). The table shows outcomes by GA and by BW category.
CONCLUSIONS:
A high rate of below normal scores was evident for infants born at younger gestational ages and lower birthweights, indicating impairments at 18 to 21 months corrected age, especially with respect to language and motor development. Gestational age specific data on outcomes at 18 to 21 months will be helpful for counseling.
Table 1).
Bayley-III outcomes by gestational age and by birthweight category. *Caution in interpreting values at lower extreme of GA and BW due to small numbers
| GA | 23 wks* | 24 wks | 25 wks | 26 wks | 27 wks | 28 wks |
|---|---|---|---|---|---|---|
| Cognitive Composite <85, n (%) | 11 (31.4) | 42 (25.6) | 60 (18.4) | 64 (16.1) | 68 (13.7) | 45 (8.4) |
| Language Composite <85, n (%) | 19 (55.9) | 83 (51.6) | 128 (39.9) | 132 (33.8) | 167 (34.7) | 133 (26.0) |
| Motor Composite <85, n (%) | 16 (47.1 | 60 (37.3) | 85 (26.9) | 94 (24.4) | 85 (18.1) | 83 (16.0) |
| BW | <500g* | 500–749 g | 750–999 g | 1000–1249 g | ≥21250 g | |
| Cognitive Composite <85, n (%) | 5 (31.3) | 86 (21.9) | 120 (15.2) | 64 (11.4) | 15 (7.9) | |
| Language Composite <85, n (%) | 7 (46.7) | 175 (45.3) | 277 (35.9) | 160 (29.9) | 41 (22.2) | |
| Motor Composite <85, n (%) | 7 (46.7) | 127 (33.1) | 161 (21.1) | 101 (18.8) | 25 (13.8) |
Footnotes
FUNDING: CIHR Team in Maternal Infant Care.
Abstract
BACKGROUND:
Ureaplasma species infection has been associated with the development of bronchopulmonary dysplasia (BPD) in preterm infants. Macrolides have been used for the treatment of Ureaplasma infection. It is not clear whether use of macrolides has a role in the prevention of BPD.
OBJECTIVES:
To evaluate the effects of macrolides in the prevention of BPD.
DESIGN/METHODS:
We searched MEDLINE, EMBASE, and Cochrane Central Register of Controlled trial, abstracts of the major pediatric society meetings and bibliographies of retrieved articles. We included randomized controlled trials assessing the effects of macrolides therapy on BPD in pre-term infants. A random/fixed effect model was used to synthesize predefined outcomes.
RESULTS:
Of 6746 references, six studies involving 469 preterm infants were eligible for the analysis. Macrolides when used prophylactically (four studies) did not show significant reduction either in the risk of BPD (RR 0.88 [95% CI 0.75 to 1.03]), or in the combined outcome of BPD or death (RR 0.89 [95% CI 0.79 to 1.01]). Similarly, there was no significant reduction in the risk of BPD (RR 0.64 [95% CI 0.31 to 1.31]) or the combined outcome of BPD or death (RR 0.41 [95% CI 0.05 to 3.13]) when macrolides are used in Ureaplasma positive infants. There was no significant difference in any of the secondary outcomes (duration of ventilation, length of hospital stay, and sepsis).
CONCLUSIONS:
This meta-analysis did not support sufficient evidence for use of macrolides either prophylactically in preterm infants or therapeutically in Ureaplasma positive preterm infants for prevention of BPD.
Figure 1).
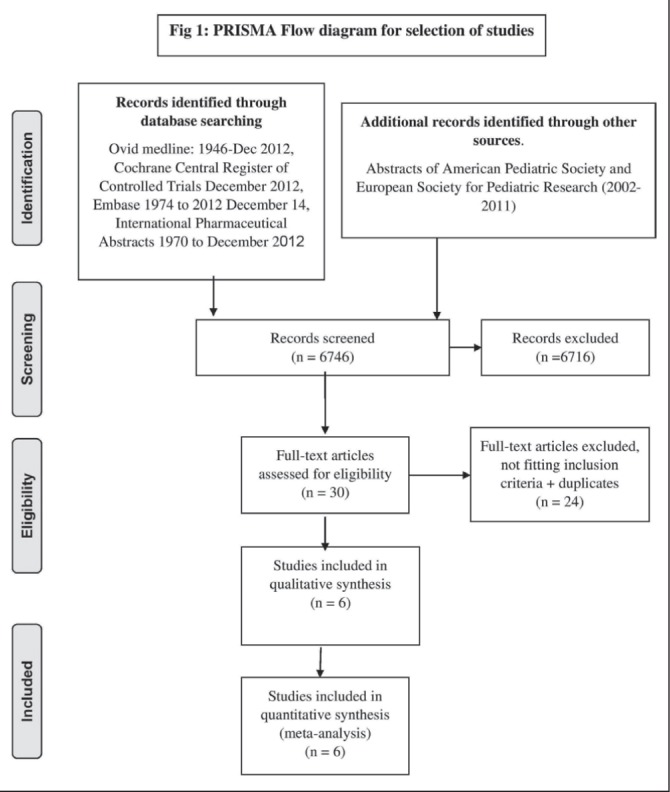
PRISMA Flow diagram for selection of studies
Figure 2).
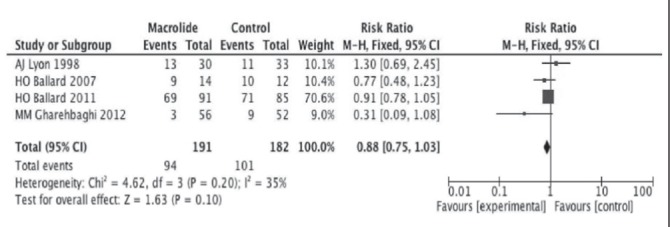
Effect of macrolides on BPD when used as prophylaxis
Figure 3).
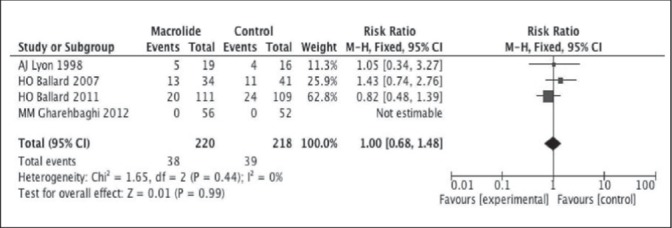
Effect of macrolides on death when used as prophylaxis
Abstract
BACKGROUND:
The multivariate risk model proposed by Puopolo et al (Pediatrics 2011;128(5):e11655–1163) has been shown to identify 35% fewer asymptomatic infants born at ≥ 36 weeks in a single maternity center as high risk for early onset neonatal sepsis (EOS) when compared with standard algorithms. (Mukhopadhyay et al E-PAS2013:3355.6)
OBJECTIVES:
To retrospectively examine the number of infants assessed and treated for EOS using local guidelines in a Canadian neonatal unit in comparison with the numbers that would have been assessed by using the quantitative multivariate risk model of Puopolo et al.
DESIGN/METHODS:
Retrospective cohort study of infants born at ≥34 weeks gestational age (GA) admitted to a Canadian NICU, between July 2012 and June 2013. The cohort, which includes infants admitted to the NICU for a variety of clinical and child welfare reasons, was first stratified into high- and low-risk groups according to the risk calculated by the model of Puopolo et al. This model uses GA highest maternal intrapartum temperature, duration of rupture of membranes, maternal group B Strep status as well as timing and type of intrapartum antibiotics to calculate a risk. A value of ≥0.5 per 1000 live births was used to define high risk and therefore the threshold for assessment and treatment. The numbers who were investigated (CBC, blood culture, or CSF culture) and/or treated for EOS within each group were then identified.
RESULTS:
89.5% (239 of 267) of infants were calculated as being low risk while 10.5% (28 of 267) were high risk, with the mean risk scores being 0.12±0.01 (95% CI 0.0 to 0.47) and 1.68±0.91 (95% CI 0.52 to 13.19), respectively. Within the low risk group, 130 of 239 (54%) were investigated for EOS, while 31 of 239 (13%) received antibiotics. Within the high risk group, 18 of 28 (64%) were investigated with only two of 28 (7%) also being treated for EOS. There were no differences in the mean risk scores in the high risk group between those who were investigated and those who were not. The scores of the two patients in the high risk group who received antibiotics were 13.19 and 0.94, and the mean score of those who did not was 1.26±0.39 (95% CI 0.52 to 4.47). In total, 148 of 267 (55.4%) of infants were investigated for EOS in this cohort based on clinical judgement. No cases of EOS as defined by a positive blood or CSF culture were identified during this period.
CONCLUSIONS:
Use of the Puopolo et al. neonatal sepsis predictive model for evaluation of EOS would have resulted in 81% fewer infants investigated. Costs associated with the investigations and treatment and potential cost savings of using this model are currently being evaluated. Prospective study is needed to further evaluate the practical impact of this predictive instrument on EOS identification and associated cost savings in Canadian NICUs.
Abstract
BACKGROUND:
Screening total serum (TSB) or transcutaneous (TcB) bilirubin in all infants is recommended. The JM-103 Drager Jaundice meter is approved for TcB screening in Canada.
OBJECTIVES:
The accuracy of six TcB meters was determined by comparing meter results with the clinical laboratory TSB results.
DESIGN/METHODS:
Ethical approval was obtained for this prospective observational study. Participants received the institutional standard (TSB) for bilirubin screening. Infants under 14 days of age, over 35 weeks gestation, with no history of phototherapy or transfusion were eligible. Prior to TSB collection, skin tone and sternal TcB readings were obtained. Enrolment continued until there were at least five participants, for each of six meters in each TSB range (TSB <150 μmol/L, 151 μmol/L to 250 μmol/L, and >251 μmol/L). Up to five TcB meter readings were obtained per participant. Data was analyzed using Deming regression to determine the relationship between TcB and TSB for each meter. Regression slopes for each meter were compared for statistical significance (P<0.05).
RESULTS:
Two hundred and four participants were enrolled in this study and 909 TcB meter results were obtained. The regression line for each meter is the following, Meter 1: y = 1.05x − 6.8; Meter 2: y = 0.94x − 11.4; Meter 3: y = 0.96x − 14.3; Meter 4: y = 0.88x − 10.5; Meter 5: y = 0.97x − 20.6; Meter 6: y = 0.89x − 4.3. The regression slope for Meter 1 was significantly different from meters 2–6. The regression slopes for meters 2–6 were not significantly different. At TSB = 100 umol/L, Meters 2–6 results ranged from 76 μmol/L to 81 μmol/L while Meter 1 reported 94 μmol/L. At TSB = 200 μmol/L, Meters 2–6 results ranged from 167 μmol/L to 178 μmol/L and Meter 1 reported 200 μmol/L. At TSB = μmol/L, Meters 2–6 results ranged from 304 μmol/L to 326 μmol/L while Meter 1 reported 359 μmol/L. Significantly different TcB results were obtained with meter 1 when compared with meters 2–6 results. Results obtained with meters 2–6 were not significantly different. No mathematical adjustment to an intervention nomogram can accommodate TcB readings from both Meter 1 and Meters 2–6.
CONCLUSIONS:
Correlation of new meters with the clinical laboratory TSB method is required to determine specific action thresholds before integration of meters into community screening protocols. Our study demonstrates that TcB meters may report clinically significant variant results. Furthermore, between-meter accuracy must be determined before different TcB meters are used for longitudinal clinical surveillance (trending).
Abstract
BACKGROUND:
Critical decisions regarding infants at risk of being born at the limits of viability are primarily discussed during the antenatal consultation with a Neonatologist. These decisions are emotionally unthinkable; choosing between intensive care to support survival or palliative care. One the one hand, we don’t know whether the baby will survive, and if it survives, will the baby be significantly handicapped; on the other hand, certain death. Each participant of the antenatal consultation, the parents and the neonatologist, carry their own values to define the best interest of the infant that will support the final decision. Even though shared decision-making is promoted by professional societies, the parents might not participate as they expect. Moreover, the neonatologist might inaccurately estimate the parents desire to participate or limit the parents’ authority to make decision. In those circumstances, open communication between the parents and the neonatologist is essential. However, the most effective strategies for communication and encouragement of parent participation are unknown.
OBJECTIVES:
The goals of this study are to explore the communication between the parents and the neonatologist and to describe the factors that promote parent satisfaction in their participation in the decision-making process.
DESIGN/METHODS:
We conducted a qualitative study based on ethno-methodology to analyze videotapes of the interactions between parents and neonatologists during the antenatal consultation. Post-antenatal consultation interviews were used to define parent satisfaction scores for their participation during interaction.
RESULTS:
Five system – infant at risk including 10 parents and six neonatologists participated in the study. Results highlight key factors such as sharing ‘weighted’ information, offering choices, allowing time to think and building trustworthy parent-doctor relationships through communication promote the opportunity for parents to participate. Important communication behaviours including empathy, support and listening, taking turns as “expert” facilitate parent participation in the decision making process.
CONCLUSIONS:
The key factors were integrated in a model to facilitate parents’ participation in the decision making to their satisfaction (Figure). From this model we identified specific communication strategies examples useful to the neonatologist that will support parents in their participation in a true shared decision-making process
Abstract
BACKGROUND:
Placement of umbilical arterial and/or venous (UA or UV) lines is a common practice in the care of preterm babies in Canada. It is not, however, clear whether they improve neonatal outcomes
OBJECTIVES:
To explore the effect of umbilical lines on mortality and morbidities in very preterm babies
DESIGN/METHODS:
Data were abstracted from the Canadian Neonatal Network database for babies born at <29 weeks gestational age (GA) from January 2010 to December 2012 (excluding babies who were moribund on admission or with major congenital anomalies). Four groups were identified: Gp0 with no umbilical lines; Gp1 with umbilical venous (UV) lines only; Gp2 with umbilical artery (UA) lines only; and Gp3 with both UA and UV lines. Data fields included demographics, peripartum factors, major inpatient morbidities (nosocomial infection (NI), necrotizing enterocolitis (NEC), bronchopulmonary dysplasia (BPD), brain injury (BI) and retinopathy of prematurity (ROP)), and mortality. Univariable and multivariable regression analyses were performed to compare the four groups.
RESULTS:
Of 4623 babies 820 (17.7%) were in Gp0, 1032 (22.3%) in Gp1, 120 (2.6%) in Gp2, and 2651 (57.3%) in Gp3. With increasing number of lines babies were smaller, had lower Apgar scores, were more likely to have high SNAPII scores, and were more likely to be born by Cesarean Section. Univariate analysis showed that babies with no umbilical lines (Gp0) had the lowest mortality and lowest rates of NI, NEC, BPD, BI, and ROP. Increasing from one to two lines also increased rates. After adjustment for risk factors (see table and footnote) babies with no lines had significantly lower rates of a composite outcome of death or major inpatient morbidity - there was no difference in mortality between groups. Similar results were obtained when the model was adjusted for SNAPII instead of Apgar score.
CONCLUSIONS:
Most very preterm babies in Canada get UA and/or UV lines (usually both). Umbilical lines are more likely to be inserted into smaller, sicker babies. However, after adjustment for risk factors and acuity, babies with no umbilical lines are more likely to survive without major morbidity. Adding a second umbilical line appears to increase risk further. Clinical strategies should take into account the inherent risks of UA and/or UV lines. Alternative practices, such as early placement of peripherally inserted central catheters, require further evaluation.
Table 1).
Adjusted odds ratios (AOR) (95% CIs) – AORs were based on a multiple logistic regression model adjusted for gender, GA, small for gestational age, Apgar score, outborn status, maternal hypertension, Cesarean and antenatal steroid use
| GpO vs Gpl | GpO vs Gp2 | GpO vs Gp3 | |
|---|---|---|---|
| Mortality | 0.85(0.59,1.22) | 0.77(0.40,1.49) | 0.76(0.56,1.04) |
| Composite outcome | 0.75(0.62.0.92) | 0.56(0.37,0.87) | 0.52(0.43,0.63) |
Abstract
BACKGROUND:
American Academy of Pediatrics (AAP) recommends the use of TcB devices for the diagnosis of significant hyperbilirubinemia in infants >35 weeks of gestational age and for making decisions for initiation of phototherapy. However, the accuracy of TcB devices in infants receiving phototherapy is unclear.
OBJECTIVES:
To conduct systematic review of diagnostic accuracy studies comparing TcB devices with total serum bilirubin (TSB) estimation in near-term and term neonates receiving phototherapy or post-phototherapy phase
DESIGN/METHODS:
Search Strategy MEDLINE, EMBASE, Cochrane library, CINAHL, Scopus databases (all from the date of inception to August 2013) were searched. Additional citations were identified from the bibliography of selected articles and from abstracts of the conference proceedings.
Study Selection and Data Extraction
The studies were included if they compared TcB results with TSB in term and near-term infants during phototherapy or after discontinuation of phototherapy in neonatal period. Two reviewers independently assessed studies for inclusion and discrepancies were resolved with consensus. Data were extracted by one reviewer and checked for accuracy by the second reviewer. Quality assessment of included studies was performed using QUADAS-2 tool.
RESULTS:
Seventy-three studies were selected for full text review of which 12 were eligible for inclusion (seven studies awaiting decision). Studies varied in terms of site of TcB estimation (forehead [12], sternum [6], back [2]); TcB devices used (Bilicheck [2], Minolta air shields [4], JM101 [6]); method of estimation of TSB (Direct Spectrophotometry [5], Diazo method [8], both [2], not specified [1]). All studies provided results of comparison of TcB with TSB as co-relation coefficients (r=0.67 [95% CI 0.61 to 0.72]), with five studies providing data separately for TcB measurements from a covered area (r=0.71 [95% CI 0.65 to 0.77]) and two studies providing results for post phototherapy phase (r=0.75 [95% CI 0.66 to 0.82]) data One study provided data for Bland-Altman difference plots and showed TcB underestimated TSB by a mean difference of29.2 mmol/L.
CONCLUSIONS:
Our results show that TcB devices were not as reliable for estimation of serum bilirubin in infants receiving phototherapy as compared to pre-phototherapy phase. However, majority of studies were conducted using older TcB devices that are currently not in practice. Also, there is insufficient data for recommending the use of TcB devices in post phototherapy phase.
Footnotes
Authors report no conflict of interest.
Abstract
BACKGROUND:
Premature infants frequently develop anemia and often require transfusions. Packed red blood cells transfusions can be associated with complications, some potentially life-threatening. Best evidence of strategies to reduce blood loss and red blood cells transfusions has not previously been summarized in a single review and knowledge gaps in this area are unclear.
OBJECTIVES:
To perform a scoping review of the evidence on blood saving practices and strategies to reduce red blood cells transfusions in premature neonates.
DESIGN/METHODS:
Standard methodology for scoping reviews was followed. MEDLINE (1946 to April 15, 2013), Embase (1947 to April 15, 2013), and Cochrane Central Register of Controlled Trials (CENTRAL, Issue 1, March 2013) were searched using the Ovid interface. The target population included premature infants (<1500g or <37 weeks) during initial hospital admission. Interventions included recombinant human erythropoietin, the use of defined thresholds for transfusion, delayed cord clamping or cord milking, iron supplementation, techniques to obtain blood samples (capillary, venous or arterial), point of care testing and non-invasive monitoring techniques. Titles, abstract and full publications to include were independently reviewed by two of the authors.
RESULTS:
A total of 1353 records were identified; 138 abstracts were selected and 37 full publications were reviewed and included in this review (Table 1). High quality evidence such as systematic reviews and randomized controlled trials have been performed for some interventions (erythropoietin, transfusion thresholds, delayed cord clamping and iron supplementation). Early erythropoietin and delayed cord clamping have been shown to reduce the need for blood transfusions. For blood sampling techniques and non-invasive monitoring, evidence is limited to prospective cohort studies and case series. Non invasive monitoring has shown variable reliability when compared to standard methods and point of care testing can reduce blood volume losses and the need for transfusions.
CONCLUSIONS:
Sufficient high quality evidence exists demonstrating that erythropoietin, transfusion thresholds, the use of delayed cord clamping reduce the need for transfusions. A gap has been identified in good quality research for strategies such as methods of point of care testing and non-invasive monitoring.
Table 1).
| Study Type | Erythropoietin | Thresholds | Delayed cord clamping | Iron Suppl. | Blood Sampling and point of care testing | Noninvasive monitoring | Other |
| Systematic Review (# of RCT included) | 3 (57) | 1 (4) | 1 (15) | 2 (51) | |||
| RCT | 3 | 2 | 1 | 2 | 2 | ||
| Prospective Cohort | 1 | 1 | 2 | 3 | |||
| Prospective Case series | 10 | ||||||
| Retrospective Cohort or Chart Review | 2 | 1 |
Abstract
BACKGROUND:
Sound levels in neonatal intensive care units (NICU) often exceed recommendations. An adverse sound environment may have harmful effects on newborns. Previous studies have explored strategies to reduce sound levels in the NICU but few have focused on direct audit and feedback methods.
OBJECTIVES:
To determine if the use of noise alarms, providing direct audit and feedback, reduces sound levels in a level 3 NICU.
DESIGN/METHODS:
SoundEar® noise alarms were installed in each of three patient care areas (blue, yellow and green pod) and at a central desk area in a level 3 NICU. The alarms continuous measured sound levels and provided direct audit and feedback. Above a set threshold the alarm displayed red, within 5 dB the alarm displayed yellow and at more than five dB below threshold the alarms displayed green. Sound levels were measured for two months with the noise alarms visible but not providing any direct audit and feedback (i.e. always displaying red). The threshold was then set to 50 dB, a level which (based on previous data) could discriminate quiet from noisy periods in our NICU. Sound data was collected for another two months. Data was adjusted for measures of unit activity. The adjusted sound levels pre and post direct audit and feedback were compared.
RESULTS:
The percent of measured sound levels below 45 dB, 50 dB and 55 dB post intervention and the difference from pre-intervention are shown below in Table 1. The largest effect was a statistically significant increase in the percentage of sound levels below 50 dB in all three patient care areas. The desk area did not show a change. The percentage of time where sound levels were below 45 dB and 55 dB was also not significantly altered by direct audit and feedback.
CONCLUSIONS:
Noise alarms providing direct audit and feedback seem effective in reducing sound levels in patient care areas. Conversations may have moved to non-patient care areas, preventing a similar change there. The time below 45 dB did not change likely due to non-modifiable background noise levels. The lack of effect for 55 dB is possibly due to the unit being below this threshold the majority of the time pre-intervention.
Table 1).
| NICU Area | |||||
|---|---|---|---|---|---|
| Blue Pod | Yellow Pod | Green Pod | Desk | ||
| 45dB | % at or Below | 5.5 | 1.9 | 8.6 | 3.0 |
| Change in % (Post - Pre) | 4 | 1.3 | 1.5 | 0.3 | |
| p - value | >0.001 | 0.16 | 0.7 | 0.98 | |
| 50dB | % at or Below | 33.9 | 33.3 | 46.2 | 26.7 |
| Change in % (Post - Pre) | 9.9 | 8.9 | 7.3 | 2.0 | |
| p - value | >0.001 | 0.02 | 0.02 | 0.97 | |
| 55dB | % at or Below | 91.4 | 90.4 | 84.8 | 77.9 |
| Change in % (Post - Pre) | −0.3 | −1.0 | 1.2 | −0.03 | |
| p - value | 0.98 | 0.92 | 0.91 | 1.0 | |
Abstract
BACKGROUND:
Clinical practice guidelines and consensus statements recommend car seat testing of preterm infants prior to discharge from hospital with the goal of detecting those who experience hypoxic events while in sitting devices.
OBJECTIVES:
To determine the rate of car seat testing failure in LPI (34 0/7 to 36 6/7 weeks GA) in a tertiary level Canadian institution. A secondary objective was to identify factors predicting failure.
DESIGN/METHODS:
Retrospective chart review of all inborn LPI admitted to our level I, II or NICU between July 1, 2012 and June 30, 2013 was conducted. Infants with genetic disorders or congenital malformations and those transferred to another hospital before discharge were excluded. Data were collected on standardized forms and included maternal demographics, labour and delivery history, clinical course and length of stay. Infants were placed in their car seat, connected to SaO2 monitoring and tested according to hospital protocol. “Failure” criteria were symptomatic bradycardia <80 beats/min (> one desaturation <88% for >10 s, or any desaturation <80%). Data were analyzed by backward logistic regression.
RESULTS:
A total of 511 charts were reviewed; 364 infants were eligible. Testing was requested but not performed in 35 infants and not requested for 18 infants who met criteria. Of the 311 infants tested (GA mean [± SD] 36.0 weeks ±5 days, birth weight 2615±405 g) 80 did not pass (26%). 69 went on to have a 2-hour flat bed test; 41 did not pass (59%). Sixty also had a second car seat test, either alone or after a 2-hour flat test; 21 did not pass (35%). Forty-one infants were admitted to NICU for further investigation or monitoring. Factors predictive of car seat failure were (adjusted odds ratio); multiple gestation (2.3, P=0.004), primaparity (0.76, P=0.10) and post-natal age at testing (0.99, P=0.06). Infants failing car seat testing had lower post-natal ages than those who passed (mean difference −32.5 h [95% CI −57.6 h to −7.5 h]).
CONCLUSIONS:
A high number of LPI do not pass car seat probe test. In this population, it may be possible to target testing multiple gestations and primigravidas. Ideally infants should be tested after an appropriate transitional period. Future research should evaluate resource utilization, economic burden and clinical significance of car seat testing and failure.
Abstract
BACKGROUND:
Monitoring protocols are used for early detection of hypoglycemia in at-risk term newborns such as infants of diabetic mothers, those with growth restriction or macrosomia and infants with acute neonatal illness. Universal glucose monitoring is not recommended since benign transient hypoglycemia occurs in up to 14% of healthy term newborns. Clinically significant hypoglycemia is felt to be uncommon in newborns with no known risk factors. However, unmonitored newborns who do become hypoglycemic often have a delay in diagnosis and treatment as onset of symptoms may be the indication to measure blood glucose.
OBJECTIVES:
To determine the prevalence of significant hypoglycemia amongst full term newborns with no pre-identified risk factors in a regional centre.
DESIGN/METHODS:
We reviewed the charts of newborns born at 37 to 42 weeks, birthweight 2500 g to 3999 g with documented hypoglycemia at a regional centre over a three year period. We focussed on those with a glucose level of <2.0 mmol/L and requiring IV dextrose. Infants of mothers with gestational and pre-gestational diabetes were excluded as were infants with birth depression, transient respiratory distress and those with acute illness.
RESULTS:
From a population of 6272 term newborns we identified eight hypoglycemic infants who met the criteria. Four of the newborns were less than the10th centile for weight and one baby had Down Syndrome. Of the remaining three hypoglycemic infants the first presented at 26 h of life with jitteriness. Blood glucose was 1.3 mmmol/L. Hypoglycemia resolved three days later. Polycythemia was noted. Mother was obese and hypertensive. The second case presented with jitteriness at 60 h of life with blood glucose 1.5 mmol/L. Hypoglycemia resolved a day later. No diagnosis was made. Mother was obese. The third case presented at 13 h with jitteriness and blood glucose 0.3 mml/L. He subsequently had three seizures. Hypoglycemia resolved six days later. The diagnosis was transient hyperinsulinism. Mother was hypertensive.
CONCLUSIONS:
Use of <10th centile weight parameter, as recommended by the CPS, is superior to an arbitrary weight cut-off in identifying growth-restricted term newborns who may be at risk of hypoglycemia. A small number of normal birth weight newborns fall outside current monitoring recommendations yet have clinically significant hypoglycemia. Many of these infants do not have a chronic underlying metabolic or endocrine disorder. We recently launched a Canadian Pediatric Survellance Program project to determine incidence of hypoglycemia in term newborns without pre-identified risk factors, to document presentation and early morbidity and to obtain clues about unrecognized or underappreciated risk factors.
Abstract
BACKGROUND:
Sildenafil citrate, a phosphodiesterase-5-inhibitor, is a controversial treatment option for pulmonary arterial hypertension (PHT), a significant complication of bronchopulmonary dysplasia (BPD).There is scarce data in premature infants.
OBJECTIVES:
Evaluate the use of sildenafil citrate in infants with BPD complicated by PHT.
DESIGN/METHODS:
Retrospective cohort study in a level 3 NICU. All medical records of premature infants with PHT secondary to BPD treated with sildenafil citrate between January 2009 and May 2013 were reviewed. Primary outcomes were:
Clinical response with 20% decrease in: respiratory support score or FiO2 requirements
Echocardiographic response with decrease in tricuspid regurgitation gradient (at least 20%) or septal flattening (at least one degree)
RESULTS:
Twenty three infants (61% male) with a median (IQR) gestational age of 26 weeks (23 to 30weeks) and birth weight of 710 g (480 g to 1170 g) were included. Antenatal data is marked by presence of chorioamnionitis (17%), oligohydramnios (22%), intrauterine growth retardation (39%) and premature rupture of membranes (39%). Neonatal course included: confirmed sepsis (48%), grade 2 or more necrotizing enterocolitis (32%), stage 3 retinopathy of prematurity (ROP) (56%) and patent ductus arteriosus (78%). Pharmacologic data, benefits and side effects are represented in the table.
CONCLUSIONS:
Sildenafil citrate treatment for patients with PHT
Table 1).
| Pharmacologic data (Median [IQR]) | |
|---|---|
| Corrected age (weeks) at introduction of treatment | 40 [28–54] |
| Dose (mg/kg/day) | 4,4 [1–81] |
| Length (days) of sildenafil treatment | 68 [2–857] |
| Time (days) to reach maximum dose | 9 [2–39] |
| Benefits (n (%) or median [IQR])) | |
| Clinical response | 8(35) |
| Clinical response in first 48 hours | 6(26) |
| Clinical response in first 7 days | 2(9) |
| Echocardiographic response | 16(73) |
| Time (days) to echocardiograhic response | 19 [2–312] |
| Side effects (n (%)) | |
| Significant hypotension related to sildenafil | 10(44) |
| Other side effects (priapism and progression of ROP) | 0(0) |
| Other data (n(%)) | |
| Survival | 15(65) |
| Death during treatment | 5(23) |
Abstract
BACKGROUND:
Epidural analgesia is the commonest mode of providing analgesia during labor, with a combination of bupivacaine and fentanyl most often used in practice. Pharmacokinetic studies have shown that opioids diffuse freely from the epidural space into maternal blood and across the placenta.
OBJECTIVES:
To test whether late-preterm infants exposed to opioids from maternal epidural analgesia in labor are more likely to develop respiratory distress in the immediate neonatal period.
DESIGN/METHODS:
Singleton babies of 33 to 36 weeks gestation, born between the dates of January 1, 2006 to December 31, 2011 at two hospital sites in Edmonton were eligible for recruitment. Subjects with major congenital malformations, culture proven sepsis, or birth by elective caesarean section without onset of labor were excluded. The outcomes of babies exposed to epidural analgesia (Exposed group) were compared with babies without epidural exposure (Unexposed group) adjusting for the following variables, ie, gestational age at birth, infant’s sex, site of birth, antenatal steroids, maternal diabetes and hypertension, oligohydramnios, route of delivery and other modes of analgesia used in labor. The outcomes of interest were Apgar scores at 1 min and 5 min, need for resuscitation (defined as need for any one of the following in the delivery room – bag and mask ventilation, intubation, chest compression or resuscitation drugs) and development of respiratory distress within 24 h of birth.
RESULTS:
We recruited 1045 infants; 12.5% needed resuscitation in the delivery room and 15.6% developed respiratory distress following admission to the NICU. 58.6% subjects were exposed to epidural analgesia in labor. The exposure to epidural analgesia was associated with lower 1 min (P=0.009) and 5 min (P<0.001) Apgar scores but not with greater need for resuscitation (P=0.43) or the development of respiratory distress (OR 1.30 [95% CI 0.86 to 1.96]; P=0.220). In subgroup analysis, we noted a trend towards higher incidence of respiratory distress in infants at 33 to 34 weeks gestation (OR 1.45 [95% CI 0.91 to 2.30]; P=0.11) exposed to epidural analgesia.
CONCLUSIONS:
Exposure to maternal epidural analgesia was associated with lower Apgar scores in late preterm infants with a trend towards higher risk of development of respiratory distress in more immature infants.
Abstract
BACKGROUND:
Developmental interventions for parents of preterm infants have been shown to improve parental outcomes. We developed a family-focused educational program of developmentally-supportive care using a multimodal approach that integrates web-based technologies.
OBJECTIVES:
To assess the effect of our program on parental outcomes at four months corrected age (CA) among parents of extremely preterm infants.
DESIGN/METHODS:
Preliminary clinical trial with a historical comparison group. Families with preterm infants born <29 weeks and admitted at Ste-Justine Hospital NICU were recruited, with a total of 55 in each comparison and intervention groups. At four months CA, parents completed the Parental Cognitions and Conduct Toward the Infant scale, the Parenting Stress Index, and the Bates Parental Perception of Infant Temperament scale. Comparisons were made using T-test and chi square analyses.
RESULTS:
Mean gestational age was 27±3 weeks and birth weight 1010±236 g. The table shows parental outcomes by intervention group (table1). Analyses with the current available data (comparison: n=48, intervention: n=38), demonstrated no significant difference between the two groups regarding mean scores and proportion of parents scoring in the abnormal range.
CONCLUSIONS:
The program in the present format did not show benefits on short-term parental outcomes. Using a more interactive and individualized web-based approach may be an option for improving our program and outcomes.
Table 1).
| Intervention | Comparison | |
|---|---|---|
| PACOTIS | ||
| Parental self-efficacy, mean (SD) | 8.5±1.3 | 8.7±0.8 |
| -low self- efficacy | 21% | 23% |
| Perceived parental impact, mean (SD) | 8.0±1.9 | 8.3±1.7 |
| -low parental impact | 16% | 12% |
| Parental coercive behavior, mean (SD) | 1.6±1.4 | 1.1±1.6 |
| -high coercive parenting | 26% | 17% |
| Parental affection, mean (SD) | 9.4±1.0 | 9.6±0.6 |
| Parental overprotection, mean (SD) | 4.7±2.5 | 4.9±2.4 |
| -high parental overprotection | 21% | 19% |
| Perception of infant qualities, mean (SD) | 7.8±l.7 | 7.7±1.4 |
| Parenting Stress Index | ||
| Total stress score, mean (SD) | 65.5±17.6 | 62.4±11.9 |
| -abnormal score | 11% | 0 |
| Parental distress, mean (SD) | 26.3±9.3 | 24.1±6.2 |
| -abnormal score | 16% | 3% |
| Parent-Child Dysfunction Interaction, mean (SD) | 17.5±4.8 | 17.6±4.3 |
| -abnormal score | 11% | 8% |
| Difficult child, mean (SD) | 21.6±8.8 | 20.7±6.0 |
| -abnormal score | 3% | 0 |
| Bates | ||
| Total score, mean (SD) | 22.8±7.6 | 23.2±6.1 |
| -fussy child | 71% | 83% |
Abstract
BACKGROUND:
It is unclear if infants with gastroschsis develop metabolic acidosis as a result of prolonged intrauterine gut compromise or dehydration secondary to increased fluid loss. There is little literature regarding postnatal preoperative management of these infants.
OBJECTIVES:
To assess the frequency of preoperative metabolic acidosis in infants with gastroschisis and to investigate whether this acidosis reflects the severity of gut compromise as assessed by time to feeding tolerance.
DESIGN/METHODS:
All infants with gastroschisis born between May 2005 and April 2013 in a single tertiary care centre were reviewed. Metabolic acidosis was defined by the presence of pH <7.26 and serum bicarbonate (HCO3) <18.5 or base excess (BE)< −8.5 mmol/L. Infants with birth depression were excluded. Maternal and neonatal data were collected. Frequency of preoperative metabolic acidosis and its correlation with time to first feeding, time to reach full feeds and GPS (Gastroschisis Prognostic Score, Cowan et al 2012) were investigated.
RESULTS:
Sixty infants were identified, 11 were excluded (birth depression or lack of preoperative blood gases). Twenty infants (41%) had pH <7.26, eight (16%) had serum HCO3 <18.5 mmol/L, and 10 (20%) had BE <−8.5 mmol/L at a median age of 1.2 h. Median preoperative total fluid intake was 130 ml/kg/d and median age at repair was 4 h (Figure). No correlation was found between metabolic acidosis or serum lactate and age at first feed, age at full feeds or Gastroschisis Prognostic Score (Table). By logistic regression analysis, only lower fluid intake (<120 mL/kg/day) was predictive of early first feeding (OR 3.43 [95% CI 1.05 to 11.2]).
CONCLUSIONS:
Preoperative metabolic acidosis was identified in a significant proportion of patients with gastroschisis despite high fluid intake. However, it does not appear to be related to the degree of gut compromise. The practice of providing high fluid to these infants needs more investigation.
Table 1).
| Late First Feed (>12 d) N=14 | Late Full Feeds (>19 d) N=10 | High GPS (≥2) N=7 | |
|---|---|---|---|
| Unadjusted metabolic acidosis, OR(95%CI) | 1.5(0.3–8.3) | 2.4(0.3–21.8) | 2(0.4–9.1) |
| Adjusted metabolic acidosis. OR(95%CI) | 1.3(0.2–7.4) | 2(0.2–19.2) | 2.2(0.3–14.5) |
Table 2).
| Median (Interquartile Range) | |
|---|---|
| GA (weeks) | 36.9 (35.9–37.5) |
| Birth weight (g) | 2412 (2004–2785) |
| Apgar score at 1 min | 7 (5–9) |
| Apgar score at 5 min | 9(8–9) |
| Cord arterial pH | 7.28 (7.25–7.34) |
| Total fluid intake (ml/kg) | 130(120–150) |
| Age at gastroschisis repair (hrs) | 4 (2.7–6.3) |
| Age at first feed (days) | 16(11.3–23) |
| Age at full feed (days) | 24(18.5–36.5) |
| Gastroschisis Prognostic Score | 1 (0–1) |
Abstract
BACKGROUND:
Clinically suspected chorioamnionitis (CSC) is a commonly diagnosed complication of pregnancy. The burden of this diagnosis continues to impact maternal and neonatal care.
OBJECTIVES:
To determine the usefulness of a single C-reactive protein (CRP) measurement in identifying when antibiotic treatment can be discontinued in asymptomatic neonates ≥35 weeks, investigated for early onset neonatal sepsis (EONS) secondary to CSC.
DESIGN/METHODS:
As part of a quality improvement (QI) project to keep asymptomatic babies with their mothers, a clinical care map was developed focusing on reducing the intensity and duration of monitoring, investigating and treating those born to mothers with CSC. These at-risk newborns had routine diagnostic testing at birth and were monitored at their mothers’ bedside where they received empiric intravenous antibiotic therapy. Antibiotic duration was reassessed based on the 24 h clinical exam and a CRP measurement obtained between 15 h and 22 h of age. Infants who remained well with CRP values less than 10 mg/L could have their antibiotics discontinued prior to the 48 h culture results and potentially be discharged home with parental counseling. A retrospective chart review was conducted between November 1, 2011 and November 1, 2012, on infants’ ≥35 weeks gestation who were evaluated for EONS secondary to CSC. Data were abstracted for both maternal and infant diagnostic evaluations and clinical signs and symptoms.
RESULTS:
Of 5886 babies delivered during this period, 162 initially asymptomatic infants were investigated after birth for EONS secondary to CSC. Although none of the neonates had positive blood cultures, 10 went onto develop symptoms consistent with EONS. Despite three of the symptomatic infants having low CRP levels, all 10 received antibiotics in NICU for between 48 h to seven days. Of the remaining 152 asymptomatic infants, 125 had CRP values <10 mg/L and 113 (90%) of those neonates had <48 h of antibiotics. Forty-nine infants were discharged home before two days. The 27 asymptomatic infants with high CRP measurements remained in postpartum and were treated until the 48 h blood culture results were reported as negative.
CONCLUSIONS:
For asymptomatic at-risk neonates, a CRP measurement <10 mg/L between 15 h and 22 h of age supported clinical assessment and reduce both antibiotic exposure and length of hospital stay. The clinical care map optimizes the allocation of neonatal resources, supports a family centered approach to practice and is clinically safe.
Abstract
BACKGROUND:
Although adverse events are pervasive in NICUs, many events are preventable. Most healthcare organizations rely on traditional methods of detecting adverse events, focusing on voluntary reporting by healthcare personnel. It is estimated that only five to ten percent of errors are reported using these methods, and of those, 90% to 95% cause no harm. The use of a Trigger Tool helps identify and target harmful events.
OBJECTIVES:
In an effort to improve safe care for neonatal patients, a program-specific tool for identifying adverse events with associated harm was developed. The trigger tool will help prioritize focused quality improvement (QI) initiatives to reduce adverse events.
DESIGN/METHODS:
The Neonatal trigger tool utilizes an approach where a “triggered event” prompts a detailed review of the account in an effort to determine the occurrence of adverse events and associated harm. Every month, 20 charts are randomly selected from discharges where babies have had a minimum NICU stay of 48 h. Two research nurses review all medical records looking for the presence of program-specific triggers. Once triggers are identified, the chart is independently analyzed on two further occasions by trained team members. These reviews are time sensitive, taking 20 min per chart, and focus on determining the associated adverse events and rating preventability. Quarterly meetings are held to discuss adverse events and any discrepancies in reporting. Data is cumulated biannually based on categories of events. Neonatal QI initiatives are prioritized, focusing on reducing the most harmful and frequently observed adverse events.
RESULTS:
Data is presented as types of events and graphed into pie charts. In comparison to conventional hospital reporting systems, where 35% of identified errors are medication related, the 2010 trigger tool report indicated medication errors causing harm accounted for 4% of the program’s adverse events whereas; airway management, including unplanned extubations and unsuccessful intubations, accounted for 26% of harmful errors. Focused QI initiatives reduced the incidence of airway associated adverse events by 25%, which was sustained over an 18-month period. Focused strategies consisted of purchasing a video laryngoscope, limiting intubations in VLBW infants to skilled intubators, safety learning videos and focused nursing education.
CONCLUSIONS:
The Neonatal trigger tool provides an effective method of identifying harmful adverse events. QI initiatives aimed at reducing patient harm can be implemented and tested.
Abstract
BACKGROUND:
Pediatricians are daily confronted with monitoring and safe discharge issues concerning late preterm infants (34 0/7 to 36 6/7 weeks postmenstrual age (PMA)) considering the risk of apnea of prematurity (AOP). Late preterms are 15 times more at risk of AOP when compared with term newborns. Since AOP peak arises beyond the very first days of life, timing and duration of monitoring arouse debate. Current recommandations regarding late preterms hospital discharge do not systematically mandate cardiorespiratory monitoring.
OBJECTIVES:
The objective of this study was to describe a late preterms population affected by Respiratory Distress Syndrome (RDS) in order to documented AOP prevalence during neonatal intensive care unit (NICU) hospitalization.
DESIGN/METHODS:
A descriptive and retrospective study including late preterms with RDS diagnosis, admitted to a tertiary NICU, from January 2009 to December 2011, was conducted.
RESULTS:
Eighty five late preterms with RDS diagnosis were included and underwent cardiorespiratory monitoring. There was an increase in AOP prevalence with younger PMA; 34.8%, 70.4% and 88.6% for 36, 35 and 34 weeks PMA, respectively (P<0.0001). Caffeine treatment was used in 8.7%, 11.1% and 25,7% of 36, 35 and 34 weeks PMA late preterms, respectively. Late preterms with AOP diagnosis, whether treated or not with caffeine had a longer hospitalization (10.40 vs. 8.18 days, P=0.0019, without caffeine) (13.8 vs. 9.69 days, P=0.047, with caffeine). Patients treated with caffeine presented an extended duration of ventilatory support (5.05 vs. 4.18 days, P=0.027).
CONCLUSIONS:
The unexpected discovery of AOP high prevalence and its association with caffeine treatment in monitored late preterms admitted for RDS highlights that current recommendations about safe discharge in late preterms are not optimal when addressing this specific population. RDS occurrence in near term infants reflects their immaturity and consequently, their susceptibility to AOP. Therefore, late preterms should be considered for an extended period of monitoring after RDS resolution. Further studies are necessary to determine if recommandations should be made requiring a normal respirogram record or a seven-day period without apnea before safe discharge in late preterms.
Abstract
BACKGROUND:
To date, no recommendation guides the management of respiratory distress syndrome (RDS) in late preterm infants (34 0/7 to 36 6/7 weeks postmenstrual age (PMA)).
OBJECTIVES:
The objective of this study was to describe a late preterms population affected by RDS and their respiratory management during neonatal intensive care unit (NICU) hospitalization in order to identify potential prognostic factors.
DESIGN/METHODS:
A descriptive and retrospective study including late preterms with RDS diagnosis, admitted in a tertiary NICU, from January 2009 to December 2011 was conducted.
RESULTS:
RDS prevalence in late preterms was 13.6% during the studied period and 85 late preterms were included in the study. Median length of hospitalization was 8.9 (IQR 7.2 to 12.7) days and was significantly longer in late preterms with caffeine treatment for apnea of prematurity (13.8 vs. 9.7, days; P=0.047). Oxygen requirements lasted a median time of 2.2 (IQR 0.5 to 3.2) days. Median duration of respiratory support was 4.5 (IQR 2.9 to 6.1) days and was significantly longer when associated with younger PMA (P=0.023), female sex (P=0.003) and caffeine treatment (P=0.027). Five different modes of non invasive ventilation (NIV) were used. At some moment, 96% of the 85 patients were supported with nasal continuous positive airway pressure. Intubation was considered as NIV failure and occurred in 25% of patients who subsequently received surfactant. Intubated patients were younger at oxygen introduction (1.1 h vs 2.3 h; P=0.029) and had higher PCO2 at NIV initiation (66.0 mmHg vs 59.5 mmHg; P=0.049). Pneumothorax occurred on NIV support for 10 of 11 patients. Six patients had their pneumothorax drained and there was a trend for longer duration of oxygen requirements (P=0.142), ventilatory support (P=0.039) and hospitalization (P=0.059) in those patients. Nasal sigh intermittent positive pressure ventilation (NSIPPV) was more frequently used in patients who presented a pneumothorax (P=0.013).
CONCLUSIONS:
In this study, NIV management of RDS failed in 25% of patients. Early oxygen introduction seems to be a predictive factor of NIV failure. Due to great variability in respiratory management, no specific conduct arises to show advantages. However, almost all pneumothorax occurred while on NIV support and NSIPPV was more frequently used in those patients. Nonetheless, more studies addressing prognostic factors are needed to make recommandations regarding surfactant administration in RDS management in late preterms to prevent complications and avoid prolonged mechanical ventilation.
Abstract
BACKGROUND:
Extended interval dosing (EID) of gentamicin results in higher peak and lower trough levels with greater efficacy and reduced toxicity. The clearance, serum half-life and volume of distribution changes during the neonatal period. There is abundant data on EID of gentamicin in neonates <7 days but data on optimal gentamicin dosing in preterm neonates >7 days is lacking.
OBJECTIVES:
To determine if EID of gentamicin achieves therapeutic serum trough (<2 μg/mL) and peak (5 μg/mL to 12 μg/mL) levels in premature neonates <32 weeks gestational age (GA) and >7 days of age.
DESIGN/METHODS:
Premature neonates <32 weeks GA and >7 days of age who received gentamicin for >5 days for suspected/confirmed sepsis were included. The dosing interval was based on 22 h level after first dose of 5 mg/kg. Trough and peak levels were drawn with the second dose if infant was receiving gentamicin 36 h or 48 h and with the third dose if gentamicin was 24 h. Exclusion criteria included major congenital anomalies or renal anomalies and renal dysfunction.
RESULTS:
There were 39 infants with median GA of 27 weeks and mean birth weight of 902 g. At start of gentamicin, median postnatal age (PNA) was 27 days and mean birth weight 1338 g. Based on 22 h level, the dosing interval was 24 h in 30, 36 h in six and 48 h in three neonates. All infants had trough levels <2 μg/mL (median 0.9 μg/mL, range 0.4 μg/mL to 1.5 μg/mL) and peak levels >5 μg/mL (median 9.0 μg/mL, range 5.4 μg/mL to 15.1 μg/mL) with two infants having levels of 13.1 μg/mL and 15.1 μg/mL. There was no effect on urine output or serum creatinine levels after starting gentamicin. Of the available hearing screen results, one infant, the recipient twin of twin to twin transfusion, had sensorineural hearing loss. Using quantile regression to correct for confounders including GA, PNA correlated negatively with random, peak and trough levels (all P<0.01).
CONCLUSIONS:
In premature neonates <32 weeks GA and >7 days of age, EID of gentamicin using single 22 h level after the first dose for dosing interval achieves therapeutic serum peak and trough levels.
Figure 1).
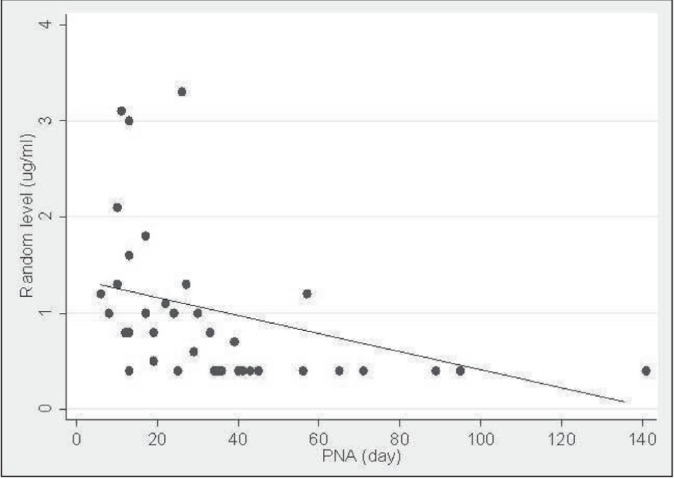
Quantile regression analysis showing negative correlation between PNA and random gentamicin levels.
Figure 2).
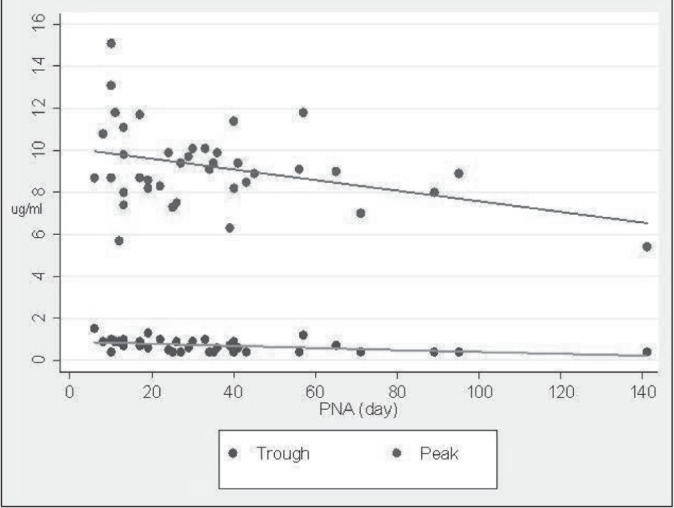
Quantile regression analysis showing negative correlation between PNA and peak/trough levels.
Abstract
BACKGROUND:
In preterm infants, the antioxidant defenses are still poorly developed. The two major sources of oxidants during intensive care stay are oxygen and parenteral nutrition (PN) which is contaminated with peroxides. We hypothesize that early O2 supplementation and longer PN duration increase the risk for oxidative stress associated diseases such as bronchopulmonary dysplasia (BPD), retinopathy of prematurity (ROP) and necrotizing enterocolitis (NEC).
OBJECTIVES:
To assess the effect of early oxygen (on day 7 and 28) and the PN duration on oxidative stress markers at 36 weeks corrected age and on oxidative stress related diseases.
DESIGN/METHODS:
A prospective observational study including all infants <29 weeks GA without major congenital anomalies admitted to our NICU during one year period (116 infants). During the first week of life, in fifty-one out of 116 infants, consent for blood sample at 36 corrected age (CA) was obtained. GSH and GSSG (nmol/mg protein) were measured by capillary electrophoresis and were used for redox potential (mV) calculation using Nernst equation -expressed as mean (sem).
BPD was defined as the need of O2 supplement at 36 weeks CA. Significant ROP was defined as any ROP stage 3 or higher or that required laser or anti-VEGF treatment. Cases of NEC grade 2 or higher according to Bell’s criteria were included. Student’s t test or χ2 were used, as appropriate, *=P<0.05, **=P<0.01.
RESULTS:
Basline chracteristics was similar in the consent group and the whole cohort. FiO2 ≥25 on day 7 and 28 of life and PN duration >14 days resulted in higher GSSG concentration and more oxidized redox potential at 36 weeks CA indicating prolonged oxidative stress. FiO2 ≥25 early on life and PN duration >14 days increased the incidence of BPD, significant ROP and NEC (Table 1).
CONCLUSIONS:
Early life exposure to oxidants is associated with prolonged oxidative stress and higher incidence of oxidative stress-related diseases. These results suggest that strategies targeting judicious O2 use and either decreasing the duration or using safer formulation PN will help decreasing the incidence of BPD, ROP and NEC.
Table 1).
| GSH | GSSG | Redox potenial | BPD or Death | ROP | NEC | |
|---|---|---|---|---|---|---|
| Fi02 <25% day 7 | 7.6 (0.5) | 0.18(0.02) | −198 (2) | 26/54 | 2/56 | 7/56 |
| Fi02 ≥25% day 7 | 7.4 (0.6) | 0.29 (0.04) | −191 (2) | 46/50 | 6/50 | 17/50 |
| P | * | * | ** | ** | ||
| Fi02 <25% day 28 | 8.3 (0.8) | 0.17(0.02) | −201 (4) | 9/36 | 0/37 | 4/37 |
| Fi02 ≥25% day 28 | 7.3 (0.5) | 0.26 (0.03) | −193 (2) | 55/60 | 8/60 | 17/60 |
| P | * | ** | * | |||
| PN ≤14 days | 7.5(1.2) | 0.13(0.02) | −203 (5) | 16/42 | 0/44 | 2/44 |
| PN >14days | 7.5 (0.4) | 0.26 (0.03) | −193 (2) | 58/64 | 8/65 | 22/65 |
| P | * | * | ** | * | ** |
Abstract
BACKGROUND:
Aqueous and alcohol based chlorhexidine solutions are commonly used for skin antisepsis in neonates but their relative efficacy is unknown.
OBJECTIVES:
To compare the efficacy of 2% aqueous chlorhexidine solution (AQC) vs. 2% chlorhexidine in 70% isopropyl alcohol (ALC) for skin antisepsis prior to venepuncture in very low birth weight (VLBW) infants.
DESIGN/METHODS:
A total of 199 VLBW neonates (birth weight <1500 g) between two and 28 days of age were randomized to receive skin antisepsis (single application) with either AQC or ALC prior to a venepuncture. Skin swabs were collected pre- and post-antisepsis and processed by ‘swab-wash’ method. Colony forming units (CFU) were quantified up to a maximum of 150 CFU. Primary outcome was the proportion of ‘negative’ post-cleansing skin swabs defined as the presence of ≤15 CFU. Secondary outcomes included reduction in CFU and clearance proportion stratified by type of organism. After cleansing, the site was monitored for adverse reactions for 24 h.
RESULTS:
Results: There was no difference in the baseline characteristics or any measured outcome between groups (Table 1). The odds ratio for skin clearance using AQC vs. ALC was 1.36 (0.55 to 3.40). Results did not change after excluding infants with ‘negative’ pre-swabs or after adjustment for pre-cleansing CFU. No adverse reactions were noted.
CONCLUSIONS:
The majority of VLBW infants had skin colonization with bacteria in the pre-cleansing swab, with CONS being the most common organism. When used in a standardized manner, both AQC and ALC provided high skin clearance rates and were not significantly different in antisepsis properties.
Table 1).
Baseline characteristics and outcomes. Results presented as mean (SD), median (IQR), n (%), point estimate (95% CI)
| Variables | ALC(IOO) | AQC (99) | p value |
| GA (wks) | 27.5 (2.8) | 27.3 (2.3) | 0.55 |
| BW(g) | 956 (287) | 954 (265) | 0.97 |
| Male sex | 55 (55%) | 54 (55%) | 0.95 |
| C-section | 56 (56%) | 45 (46%) | 0.13 |
| Intrapartum antibiotics | 62 (62%) | 65 (66%) | 0.71 |
| Apgar score at 5 minutes | 7 (5,9) | 8 (6,9) | 0.37 |
| Age at the time of procedure (days) | 10 (6,15) | 9(7,13) | 0.93 |
| Antibiotic therapy at the time of procedure | 48 (48%) | 60(61%) | 0.07 |
| ‘Negative’pre-antisepsis swabs | 11 (11%) | 19(19%) | 0.16 |
| Baseline bacterial count (CFU) | 100(26- 150) | 75 (24,−123) | 0.95 |
| Types of bacteria CONS Other |
72(81%) 17(19%) |
65(81%) 15(19%) |
|
| Proportion of negative post-antisepsis (95% CI) | 88 (82, 94) | 90(85,97) | 0.66 |
| Reduction in CFU Absolute Proportion |
63(18, 100) 100(99.7, 100) |
61 (16, 110) 100(97.1, 100) |
0.65 0.20 |
Abstract
BACKGROUND:
The Canadian Neonatal Follow-Up Network (CNFUN), a collaboration between all 26 Neonatal and Perinatal Follow-up Programs in Canada, was developed in liaison with the Canadian Neonatal Network (CNN) to facilitate collaboration in research, integrated data collection, knowledge translation and to improve the quality of care and long term outcomes of children seen in their programs. CNFUN implemented a standardized assessment at 18 months corrected age (CA) and a three year CA questionnaire for all survivors <29 weeks gestational age starting with births April 1, 2009 onwards.
OBJECTIVES:
Describe the cohort of CNFUN preterm subjects born April 1, 2009 to July 1, 2011 and major adverse outcomes.
DESIGN/METHODS:
NICUs notified local follow-up programs of eligible subjects. Patients were evaluated according to a standardized protocol and data manual. Bayley -III assessors completed online training specific for this study. Deidentified data was uploaded. Data was extracted from the CNFUN database to calculate cerebral palsy, hearing and visual impairment rates and outcomes on the Bayley -III cognitive, motor and language scores. Linkage with the Canadian Neonatal Network is planned.
RESULTS:
Of 2528 infants, 2109 were seen at 18 months CA. Subjects with missing information: CP status 45, Bayley III-cognitive 151, Bayley III language 210, Bayley III motor 222, hearing 139 and vision 59.
CONCLUSIONS:
Neurodevelopmental outcomes confirm a relatively low incidence of severe adverse outcomes but a significant percentage with scores <85 on the Bayley-III. This large CNFUN cohort of preterm survivors is a promising source of data for further analyses.
Table 1).
| CP definitive n (%) | 140(6.8%) |
| CP suspect n (%) | 72 (3.5%) |
| Cognitive composite median (IQR) | 95(90–105) |
| Cognitive <70 n (%) | 71 (3.6%) |
| Cognitive <85 n (%) | 290(14.8%) |
| Language composite median (IQR) | 91 (79–100) |
| Language <70 n (%) | 208(11%) |
| Language <85 n (%) | 662 (34.9%) |
| Motor composite median (IQR) | 94(85–100) |
| Motor <70 n (%) | 130(6.9%) |
| Motor <85 n (%) | 423 (22.4%) |
| Sensorineural hearing loss n (%) | 35(1.8%) |
| Bilateral visual loss n (%) | 37(1.8%) |
Footnotes
FUNDING: CIHR Team in Maternal Infant Care
Abstract
BACKGROUND:
Recommendations encourage informing mothers at risk of preterm labor.
OBJECTIVES:
To evaluate whether prenatal consultations for preterm labor worry or reassure women at risk of preterm delivery.
DESIGN/METHODS:
This was a prospective survey of hospitalized women at risk of preterm delivery 26 to 32 weeks GA, who had met the neonatologist for prenatal consultation in the last 72 h. The tool was developed using data from a qualitative exploratory study; construct and content validity were accounted for through several validation phases. A single-center study was conducted in 2008, leading to a multicenter trial in three tertiary care university hospitals (Apr. 2012–Sept. 2013). Variables were analyzed using Chi2 tests; qualitative data was transcribed and categorized to identify emerging themes.
RESULTS:
A total of 229 of 334 surveys were returned (67.2%). Participants’ experiences were positive (89.9%). 23.3% were worried by the consultation, while 87.2% were reassured by it – reasons provided in table. Longer consultations were associated with reassurance (P<0.001). 66.1% of women’s perception of prematurity changed after the consultation. Of these, 51.3% changed for the better: the facts that the complications of prematurity and survival rates were better than anticipated, that feeling informed was a reassurance, and that a sense of competence and trust were instilled by neonatologists all contributed to this improvement. 6.3% changed for the worse due to prematurity’s complications being greater than expected. 33.9% of women’s perceptions – mostly negative or worried – remained unchanged; many reported already knowing about prematurity, but felt better informed by the meeting. GA (below vs. over 30 wks GA) was associated with a change in perception on prematurity (P<0.05), but not with worrisome or reassuring consultations.
CONCLUSIONS:
To be reassuring, neonatologists should strive to establish a trusting relationship with mothers, in which realistic, clear, but optimistic, information is offered. Most women’s outlooks on prematurity can improve through such a process, especially at an earlier GA.
Table 1).
*Similar answers
| Worried by consultation (n=52) | Reassured/not worried* by consultation (n=209) |
Worrisome consultation process:
|
Neonatologist:
|
Information:
|
Information:
|
Abstract
BACKGROUND:
Many clinicians refer to published or local guidelines when counseling expectant parents about perinatal care decisions. The number of guidelines created and currently in use in Canada and the quality of those guidelines is unknown.
OBJECTIVES:
To assess the quality of guidelines created and used in Canada regarding the perinatal care of 22 to 25 week GA infants.
DESIGN/METHODS:
We contacted the 32 Canadian Neonatal Network centres to determine: 1) if they had created their own guideline; and, 2) what Canadian guideline(s) they used. Any guideline(s) used were retrieved for assessment with the validated Appraisal of Guidelines for Research & Evaluation (AGREE II) Instrument. This six-domain, 23-item instrument assesses guideline quality (eg, scope, stakeholder involvement, rigour and transparency of development, clarity of presentation, applicability, and editorial independence). Three reviewers independently assessed each guideline. Items with a score difference of >3 were reviewed to reach consensus on a revised score.
RESULTS:
Twenty-nine of the 32 centres responded (91%). Twenty-seven of the 29 centres used the national Canadian Pediatric Society (CPS) statement as a guideline. One centre used their regional guideline. An outborn centre reported the CPS statement did not apply to them. Two centres used local guidelines in addition to the CPS statement; only one provided their guideline. Therefore, one national, one regional and one local guideline were obtained and assessed with the AGREE-II instrument. Major deficits were found within all AGREE II domains for the three guidelines. The domains with the lowest scores were generally ‘rigour of development’ and ‘applicability’. The overall quality score was 44%, 39%, and 33% for the national, regional and local guidelines, respectively. No guideline was deemed suitable for clinical use given the identified flaws. The national guideline was considered useable with many modifications.
CONCLUSIONS:
Several guidelines on the perinatal care of 22 to 25 week GA infants exist in Canada. Many deficits were identified in the quality of their development. The benefits of guidelines are dependent on their quality; therefore, the use of a poorly developed guideline may be detrimental to decision-making processes and patient care. Canada urgently needs a guideline with recommendations established through a rigorous and transparent development process.
Abstract
BACKGROUND:
Quality of care during decision-making and at end-of-life influences how parents cope with neonatal death. Associated moral distress affects individuals and an organization’s ethical climate.
OBJECTIVES:
To explore the challenges of meeting parents’ and infants’ needs in end-of-life care and decision-making in the NICU.
DESIGN/METHODS:
Thirty-six semi-structured interviews were undertaken with 43 health care workers (HCW) from one tertiary Canadian NICU: 23 nurses, five neonatologists, five residents, three social workers, two fellows, two nurse practitioners, two chaplains, and one dietician. Questions (developed by a multidisciplinary research team including parents) probed for HCW’s experiences, perception of parent needs, and challenges to providing quality end-of-life care. Recorded interviews were transcribed, thematic analysis performed with triangulation of themes across investigators, and an organizational ethics model of end-of-life care evolved.
RESULTS:
Figure 1 depicts an organizational model of roles, challenges, and quality indicators of end-of-life care based on HCW themes. The ability to meet parents’ and infants’ needs were influenced by intrinsic and extrinsic factors related to HCW’s roles and perception of team function. These were influenced by prior experiences and training, personal and societal values, and situational context. Similarly, indicators of quality care were both intrinsic (self-satisfaction) and extrinsic (parent feedback). Consequences of poor quality of care resulted in ‘harm’ to both families and HCWs. Finally, lack of institutional supports and resources were barriers to care (Figure 1).
CONCLUSIONS:
An organizational model identifying HCW roles and challenges in providing quality end-of-life care was developed through stakeholder interviews. This model may guide institutional identification of quality indicators and inform the development of policies and programs aimed toward improving end-of life care practices.
Figure 1).
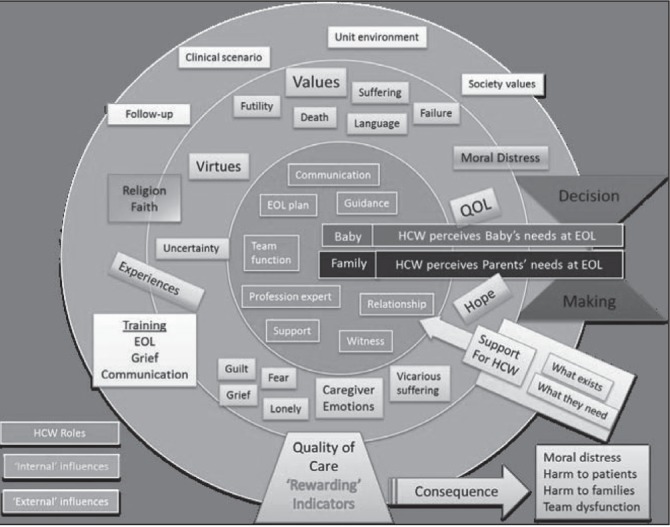
Abstract
BACKGROUND:
Maternal hypertension and cigarette smoking during pregnancy are associated with adverse neonatal outcomes. Paradoxically, smoking during pregnancy is associated with a reduced incidence of gestational hypertension. However, mothers who smoke during pregnancy and develop hypertension have worse pregnancy outcomes as compared to mothers who only have hypertension or non-smoking normotensive mothers. There is little data on neonatal outcomes of infants born to mothers with hypertension who also smoke.
OBJECTIVES:
To study the outcomes of infants of mothers with hypertension who smoke.
DESIGN/METHODS:
Using the Canadian Neonatal Network Database, we analyzed the outcomes of infants <29 weeks GA admitted to Canadian NICUs from 2003–2012. Infants were divided into four groups. Group 0 comprised infants of hypertensive mothers who smoked, group 1 infants of non-smoking hypertensive mothers, group 2 infants of normotensive mothers who smoked and group 3 infants of normotensive non-smoking mothers. Composite outcome of neonatal mortality or any of the major morbidities {grade 3/4 intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), retinopathy of prematurity (ROP) > stage 2, late onset sepsis (LOS) or bronchopulmonary dysplasia (BPD) was assessed using a multivariable model.
RESULTS:
Of the 12,307 eligible infants, 172 were in group 0, 1689 in group 1, 1535 in group 2 and 8911 in group 3. Adjusted ORs with 95% CIs with reference to group 3 (normotensive, non-smokers) are reported in Table 1.
CONCLUSIONS:
Infants of hypertensive mothers, whether smokers or non-smokers, were associated with higher rates of BPD. Smoking cessation campaigns during pregnancy are needed for both maternal and neonatal benefits.
Table 1).
Adjusted for GA, gender, small for gestational age, SNAPII score, maternal age, antenatal steroid use and multiple births.
| Characteristics | Group 0 | Group 1 | Group 2 |
|---|---|---|---|
| N | 172 | 1689 | 1535 |
| Composite outcome | 1.43(0.90,2.1) | 1.21(1.06,1.39) | 1.06(0.92,1.22) |
| Mortality | 1.09(0.63,1.87) | 1.03(0.84,1.27) | 1.02(0.85,1.23) |
| BPD | 1.54(1.06,2.22) | 1.43(1.24,1.64) | 1.05(0.92,1.21) |
| ROP>stage 2 | 1.40(0.80,2.45) | 1.19(0.95,1.48) | 1.10(0.89,1.37) |
| IVH grade 3/4 or PVL | 0.73(0.44,1.21) | 0.72(0.61,0.86) | 0.99(0.85,1.16) |
| Necrotizing Enterocolitis | 1.08(0.59,1.96) | 1.34(1.09,1.64) | 0.99(0.80,1.23) |
| LOS | 1.23(0.85,1.77) | 1.18(1.03,1.36) | 1.06(0.92,1.21) |
Abstract
BACKGROUND:
Cigarette smoking during pregnancy is associated with adverse pregnancy outcomes. Paradoxically, women who smoke during pregnancy have a reduced risk of preeclampsia (PE). Placentas of women with PE show higher levels of trophoblast apoptosis. Both Fas and Fas ligand belong to the tumor necrosis factor family of proteins and the Fas-Fas ligand system, also known as the death factor system, is one of the main pathways for apoptosis. Higher levels of soluble Fas (sFas) have been reported in PE.
OBJECTIVES:
To determine levels of sFas and soluble Fas Ligand (sFasL) in pregnant women who smoke.
DESIGN/METHODS:
Using enzyme linked immunosorbent assay (ELISA), we prospectively analyzed serum levels of sFas and sFasL in normotensive mothers who smoke and normotensive non-smoking mothers. Exclusion criteria include chronic hypertension, autoimmune disorders, rupture of membranes, evidence of labour and history of drug use. Statistical analysis was performed using a two-way non-paired Student t test or the Mann-Whitney U test as appropriate.Using enzyme linked immunosorbent assay (ELISA), we prospectively analyzed serum levels of sFas and sFasL in normotensive mothers who smoke and normotensive non-smoking mothers. Exclusion criteria include chronic hypertension, autoimmune disorders, rupture of membranes, evidence of labour and history of drug use. Statistical analysis was performed using a two-way non-paired Student t test or the Mann-Whitney U test as appropriate.
RESULTS:
The median maternal age in smoking mothers was lower as compared to normotensive nonsmoking mothers. The median gestational age was 31 weeks in both the groups. Levels of sFasL were significantly higher in smoking group compared to normotensive non-smoking group (37 pg/mL* vs. 12.14 pg/mL; P<0.0001). sFas did not differ between the two groups.
CONCLUSIONS:
We found higher levels of sFasL in normtensive smoking mothers. We speculate that higher sFasL may explain the reduced incidence of PE in pregnant mothers who smoke by binding to the elevated sFas levels in pregnant mothers who may otherwise go on to develop PE.
Table 1).
| Variables | Smoking mothers (n=49) | Non-smoking mothers (n=60) | ‘P’ Value |
|---|---|---|---|
| Maternal age in years (median /IQR) | 25(22–31) | 30(27–33) | 0.007 |
| Body Mass Index (median /IQR) | 22.4(19.9–26) | 23.1(21.2–26.75) | 0.32 |
| Gestational age in weeks (median /IQR) | 31(28–35) | 31 (27–35) | 0.85 |
| Primiparous (%) | 15(31) | 22(33) | 0.72 |
| sFas (pg/ml) [median/IQR] | 9479 (8447–11072) | 10368.56 (8820–11973) | 0.08 |
| sFas Ligand (pg/ml) [median/IQR] | 37* (23–56) | 12.14(5–33) | <0.0001 |
Abstract
BACKGROUND:
Survivors of preterm birth are at higher risk of re-hospitalisation during infancy, especially for respiratory-related conditions. Determinants of hospital re-admission have not been studied comprehensively in Canadian preterm-born infants.
OBJECTIVES:
To examine whether health-related, sociodemographic and geographical factors are associated with hospital re-admission among extremely preterm infants in Canada.
DESIGN/METHODS:
A total of 818 preterm infants born at <29 weeks gestation between January 1st and December 31st 2010 and followed at 18 to 24 months corrected age (CA) in 26 Canadian Neonatal Follow-Up Network centers were studied. Data was collected through chart review and parental interview using standardised forms. All infants underwent a neurological examination. The association between hospital re-admission and child/family characteristics was assessed by Pearson χ2 analyses for categorical variables and by ANOVA F-test for continuous variables.
RESULTS:
From neonatal discharge to 18 months CA, 271 infants (33%) were re-admitted 377 times. Re-hospitalization rates ranged from 50% for infants born at ≤23 weeks to 29% for those born at 28 weeks. Most common reasons were respiratory issues (50%), surgery (23%), infections (8%) and growth-related problems (5%). Comparisons between children re-hospitalized vs. not re-hospitalized revealed longer neonatal stay (88 vs. 73 days; P<0.01), greater proportion of infants neurologically abnormal at 18 months (20% vs. 8%; P<0.01), fewer primary caregivers subsequently employed (53% vs. 63%; P=0.02) and more on social welfare (16% vs. 8%; P=0.02) at 18 months, as well as more infants from the First Nation (8% vs. 3%, P=0.04). Marked variations across the country were observed with re-hospitalization rates between 19% and 50% for various provinces.
CONCLUSIONS:
Re-hospitalization of extremely preterm infants is related to neonatal, socio-demographic and regional factors. Whether geographical variations are explained by population characteristics or hospital-related practices remains to be explored.
Abstract
BACKGROUND:
Unintentional injury is the leading cause of death in youth ages one to 19, and suicide is the second leading cause of death in those ages 15 to 19. Asphyxiation injuries, including choking, drowning, and hanging, account for a great proportion of these injuries, with the latter two accounting for up to 18% of all suicides. There are few reports on the imaging and neurologic consequences of such injuries in contrast to extensive research on hypoxic insults in the perinatal period.
OBJECTIVES:
We report on the presentation, imaging findings, and sequelae of asphyxiation injuries outside the perinatal period.
DESIGN/METHODS:
A retrospective chart review was conducted of nine paediatric patients referred to a tertiary paediatric care hospital between 1990 and 2012. These children were all admitted to the Intensive Care Unit with severe asphyxiation injuries and were all assessed by a Paediatric Neurologist. The ages of the patients ranged from 14 months to 17 years, mean age of eight years.
RESULTS:
Asphyxiation resulted from aspiration (33% of cases), near-hanging (44% of cases), and near-drowning (11% of cases). In one case, the mechanism of injury was unclear, aspiration or near-drowning. All patients had evidence of hypoxic insult on neuroimaging. In the majority of patients, imaging demonstrated diffuse cortical and basal ganglia involvement, little white matter abnormality and minimal cerebral edema. 89% of the patients had an EEG performed. The background activity was abnormal, suggestive of diffuse and severe depression of cortical activity and graded IV–V on the dysrhythmia scale in 75% of the patients. Medical support was withdrawn within one week in 56% of patients and after four months in 11%, with 22% of patients going on to cadaveric donation. Forty-four percent of patients survived to one year post-injury, 100% of which developed severe spasticity and feeding problems. Therefore, at one year the mortality rate was 67% with severe morbidity in 100% of survivors.
CONCLUSIONS:
We describe nine children with severe acute hypoxic insult. The majority of patients exhibited severe neurological dysfunction on EEG. All patients had significant abnormalities on neuroimaging. Brain MRIs of these patients showed a unique pattern of cortical and basal ganglia involvement, which has not been previously described in the literature. The outcomes from these injuries can be devastating, with significant morbidity and mortality. Injury prevention strategies and resuscitation skills should be included in publically funded programs for parents and caregivers of children.
Abstract
BACKGROUND:
Overweight and obesity are a major health threat in middle and low-income countries and mark a new evolution in the nutritional situation of impoverished populations. Indigenous populations face additional risk factors for malnutrition such as food insecurity and low food diversity. It is estimated that in Ecuador, the rate of stunting in children <5 years of age is 23%, and 6% are overweight. In our study we present stunting and overweight data in an indigenous population in Ecuador and identify risk factors in this population.
OBJECTIVES:
To examine anthropomorphic measures in children 0 to 12 years old, household food security, dietary diversity, and demographic variables in a rural community in the Andean mountains of Ecuador.
DESIGN/METHODS:
Child nutritional status of children in a single isolated indigenous community were assessed according World Health Organization (WHO) criteria for stunting (low height-for-age), wasting (low weight-for-age) and overweight (BMI >25) and obesity (BMI >30). Escala Latina Americana de Seguridad Alimentaria (ELCSA) survey was used to assess household food security, locally designed dietary diversity score questionnaire measuring the number of food categories consumed by household.
RESULTS:
Sixty households (63% indigenous) and 88 children were included in our study. Overall, 40 (46%) of children were stunted, 25 (28%) were overweight, and three (3%) were obese. The concurrent prevalence of stunting and overweight or obesity was 17%. Nine (10%) children were wasted or severely wasted. Only two (2%) of households were food secure, with 28 (43%), 34 (39%) and 14(16%) being mild, moderately, and severely food insecure respectively. Indigenous children were more likely to be stunted than non-indigenous (P=0.01), and increasing number of children per household, and absence of primary education correlated with worsening food security (P=0.02, P=0.01). Regression analysis revealed dietary diversity scores correlated with education (P<0.001).
CONCLUSIONS:
We document that concurrent childhood stunting and overweight or obesity is an important health issue for indigenous children in Ecuador. Furthermore, we identify low education and having more than two children per family as risk factors for food insecurity.
Abstract
BACKGROUND:
Vitamin D fortification of cow’s milk is the main dietary source of vitamin D in early childhood. The consumption of non-dairy milk, such as plant-based milk beverages and goat’s milk is increasing. Vitamin D fortification of non-dairy milk is voluntary in North America. We hypothesize that the consumption of non-dairy milk may be associated with lower 25-hydroxyvitamin D in early childhood.
OBJECTIVES:
For our primary objective, we aimed to determine if there is an association between daily volume of non-dairy milk consumption and serum 25-hydroxyvitamin D in healthy young Canadian children. For our secondary objective we aimed to explore whether cow’s milk consumption modifies this relationship.
DESIGN/METHODS:
Children attending one of seven pediatric or family medicine primary care practices were recruited during routine primary healthcare. For our primary analysis, a multiple linear regression model was developed to test the association between daily volume of non-dairy milk consumption and 25-hydroxyvitamin D, adjusted for age, gender, z-BMI, season, vitamin D supplementation, skin pigmentation, and daily outdoor play time. To explore whether cow’s milk modifies this relationship, the interaction between non-dairy milk and cow’s milk consumption was included in this model.
RESULTS:
A total of 2831 children were included in the analysis. Mean age was 2.9 years, 53% were male, 53% were taking a vitamin D containing supplement, 87% of children were consuming cow’s milk and 13% of children consumed non-dairy milk daily. In the univariate analysis, each cup of non-dairy milk consumed per day was associated with a 2.3 nmol/L (P=0.005, 95% CI 1.0, 4.9) lower mean 25-hydroxyvitamin D concentration. Multiple linear regression, adjusted for clinically relevant covariates, revealed that each additional 250 ml cup of non-dairy milk was associated with a 3.8 nmol/L (95% CI 1.0 to 8.6; P=0.01) lower 25-hydroxyitmian D among children who drink cow’s milk, and a non-significant increase in 25-hydroxyvitmain D of 0.3 nmol/L (95% CI −3.0 to 3.1; P=0.6) among children who do not drink cow’s milk.
CONCLUSIONS:
Non-dairy milk consumption is associated with a lower 25-hydroxyvitamin D level in early childhood. This relationship appears to be modified by cow’s milk consumption, suggesting that consumption of lower vitamin D containing non-dairy milk may be replacing consumption of higher vitamin D containing cow’s milk.
Abstract
BACKGROUND:
Iron is an essential micronutrient for normal growth and cognitive development in early childhood. After the first six months of life, iron requirements rise rapidly and infants exclusively fed breast milk beyond six months are at risk for developing iron deficiency. In 2005, Health Canada recommended that iron-rich foods be introduced at six months of age, emphasizing that naturally iron-rich foods such as meat or meat alternatives be infant’s first complementary foods, rather than iron-fortified infant cereal. In 2012, Health Canada advised that infants be offered iron-rich foods two or more times per day. Little is known about the meat consumption patterns among infants and young children in Canada.
OBJECTIVES:
To describe the meat consumption patterns in healthy Canadian children and examine the association between meat consumption and sociodemographic factors.
DESIGN/METHODS:
A cross-sectional study of healthy children, aged six months to five years, seen for routine primary health care between December 2008 and December 2012 was conducted through a practice-based research network. Meat consumption and sociodemographic factors were measured using standardized parent-completed survey instruments. Adjusted logistic regression was used to determine the independent variables associated with meat consumption.
RESULTS:
A total of 4614 healthy children (median age 25 months) were included. Most children (94%) consumed meat over a three-day period. Adjusted logistic regression analysis identified the odds of eating meat increased by 6.5% (95% CI 4.9 to 8.2) with each additional month of age. Children of African, Caribbean, Indian-Caribbean ethnicity (OR 0.4 [95% CI 0.2 to 0.8]; P=0.007), South Asian ethnicity (OR 0.4 [95% CI 0.2 to 0.7]; P=0.005), Latin American ethnicity (OR=0.4, 95% CI 0.2 to 0.8, P=0.009) and North American Aboriginal or Oceania ethnicity (OR 0.5 [95% CI 0.3 to 0.9]; P=0.03) were less likely to eat meat. Only 71% consumed at least two servings of meat or other iron-rich foods daily as per Health Canada recommendations. Children from lower income families were less likely to eat meat according to Health Canada recommendations (OR 0.6 [95% CI 0.4 to 0.7]; P<0.001). Poultry was the meat most frequently consumed (83% poultry, 65% red meat, 62% eggs, 41% fish and 6% shellfish).
CONCLUSIONS:
Most infants and young children eat meat, however almost one third do not eat meat according to the Health Canada recommendations. Eating meat or meat alternatives less than two times per day was associated with a lower family income. The association between poor meat consumption and iron deficiency in this cohort is a focus of future investigation.
Abstract
BACKGROUND:
Vitamin D dietary intake is an important predictor of vitamin D status in young children; however, measuring vitamin D intake in early childhood is challenging in the pediatric office setting.
OBJECTIVES:
To determine how well a simple, 1 min parent completed, dietary screening questionnaire (DSQ) completed in the pediatric office setting correlates with a detailed prospective three-day estimated food record (EFR) in measuring daily dietary vitamin D intake in children one to five years of age and to examine the correlation between the DSQ and EFR for assessing milk and vitamin D supplement intake.
DESIGN/METHODS:
The mean vitamin D dietary intake values derived from the DSQ and EFR were compared using a paired two-tailed Student’s t test and Spearman correlation coefficient.
RESULTS:
Seventy-four children consented to participate in this study and were included in the analysis. Mean age was 34 months, 60% were male, 55% were European, and median zBMI was 0.12. The mean calorie intake according to the EFR was 1257 calories. The mean vitamin D dietary intake according to the DSQ was 493 (SD 399) IU and EFR was 443 (SD 389) IU. Paired student t-test revealed a P value of 0.37. The Spearman correlation was 0.47 for total vitamin D intake, 0.56 for vitamin D supplement intake and 0.69 for cow’s milk intake.
CONCLUSIONS:
A 1 min DSQ completed in the pediatric office setting, including cow’s milk and supplement use correlates well with a detailed EFR. Future studies include determining whether the DSQ predicts 25-hydroxyvitmain D.
Abstract
BACKGROUND:
The association between adiposity and milk and alternative (milk and alt.) intakes in prepubescent children is unclear.
OBJECTIVES:
This study assessed the impact of a family-based lifestyle intervention on changes in adiposity in overweight (n=14) and obese (n=64) children (age 7.5±0.78 years).
DESIGN/METHODS:
Children were randomized to control (CTRL) (no intervention), standard (SInt) (two milk and alt./d) or intensive (IInt) (four milk and alt./d) interventions focused on meeting Canada’s food guide for healthy eating and the Canadian physical activity recommendations. Measurements for height (Ht; m) and weight (Wt; kg) to compute body mass index for-age- z-scores (BAZ) using WHOAntroPlus Software (WHO 2007), waist circumference (WC; cm) and percentage body fat (%BF) assessed using dual-energy X-ray absorptiometry, were done at baseline and six-month follow up visits. Proc mixed model ANOVAs were computed using SAS (Version 9.3, SAS Inc., Cary, NC).
RESULTS:
No differences were seen at baseline among groups for BAZ or %BF. At six months, Ht increased compared to baseline (P=0.898) and was not different among groups. Compared to baseline, %BF (−2.4±0.92%; P=0.0015) and BAZ (−0.5±0.08; P<0.001) was reduced only in IInt whereas WC increased only in CTRL (+2.5±1.61 cm; P=0.007).
CONCLUSIONS:
These preliminary results demonstrate the possible benefits of participating in a lifestyle intervention focused on increased milk and alt and activity guidelines in the context of the family environment. Study funded by the Dairy Research Cluster (Agriculture and Agri-Food Canada, Dairy Farmers of Canada and the Canadian Dairy Commission).
Abstract
BACKGROUND:
Vitamin D status is lower in Canadian children who are overweight or obese than in healthy weight children.
OBJECTIVES:
This study explored the association between regional adiposity and vitamin D status in overweight and obese children.
DESIGN/METHODS:
Baseline data was collected from participants enrolled in the McGill Youth and Lifestyle Intervention with Food and Exercise (MYLIFE) study; healthy children six to 12 years of age with BMI-for-age >85th percentile were included. Vitamin D status was assessed using plasma 25-hydroxyvitamin D (25(OH)D) concentration (chemiluminescence immunoassay). Standard measurements of weight, height and waist circumference (WC) were taken; BMI and BMI-z scores were calculated. Body composition was measured using dual-energy X-ray absorptiometry. Constitutive and facultative skin pigmentation was measured using a hand-held spectrophotometer in order to determine Fitzpatrick skin types. Children were categorized according to cutaneous UVB synthesis period. Ethnicity was self-disclosed and pubertal status was reported and categorized according to Tanner stages. Differences among categories were tested using a mixed model ANOVA.
RESULTS:
One hundred and twelve children (50 boys and 62 girls) took part in this study. The mean 25(OH)D concentration was 65.2±20.9 nmol/L, with no significant difference between sexes (P=0.723). Boys had lower percent body fat (%BF) (boys, 36.4±5.0%; girls, 38.4±4.8%; P=0.022) and greater BMI z-scores (boys, 3.4±1.1; girls, 2.8±0.7; P=0.004) than girls; no other differences were found between sexes for body composition. Plasma 25(OH)D concentrations were lower in fair-skinned compared to olive-skinned children (50.2±1.1 nmol/L vs. 67.5±1.1 nmol/L; P=0.025). Children of Caucasian mothers had greater 25(OH)D concentrations than those of African American mothers (74.0±1.1 nmol/L vs. 41.2±0.2 nmol/L, P=0.040); plasma 25(OH)D was not different according to paternal ethnicity nor child’s sex, UVB period, age or pubertal status. There were no correlations between adiposity indicators (weight, fat mass (FM), %BF, android or gynoid FM, trunkal or appendicular FM, WC, BMI or BMI z-score) and 25(OH)D concentration, while accounting for sex, age, puberty, UVB period and skin colour.
CONCLUSIONS:
The vitamin D status of the children in this study was similar to that of national surveillance studies, although many fair-skinned children had low status (<50 nmol/L). Future longitudinal research is required to examine if a reduction in fat mass would lead to a concomitant increase in vitamin D status.
Abstract
BACKGROUND:
Electronic medical record (EMR) use is increasing with 57% of physicians using an EMR in 2013. Successful adoption of an EMR is dependent on many factors including the type, practice setting, interface design and usability. Many providers express discomfort and concern in adapting from a paper-based documentation system to an EMR. At our institution we completed an assessment of our readiness to implement an ambulatory care EMR.
OBJECTIVES:
To understand provider concerns In preparation for the EMR implementation and to respond to their needs to increase implementation success.
DESIGN/METHODS:
An EMR Readiness Assessment (RA) and Technical Adoption questionnaire was distributed electronically to end users through Electronic Data Capture software (Version 5.6.1 – © 2013 Vanderbilt University). The questions were derived from three sources previously validated in a physician based healthcare setting; a questionnaire used by Morton (2008) to determine factors that contribute to physician EMR acceptance; an Organizational RA questionnaire for targeted follow-up; and a Benefits Evaluation and Technology Acceptance Model (Davis, 1989; Chutter, 2009). All three sources were compared to eliminate duplication. The final questionnaire was pilot tested for face-validity.
Participation was voluntary. The questionnaire was administered for three consecutive weeks prior to the EMR go-live; two separate email reminders were sent.
RESULTS:
A total of 167 (48%) providers completed the RA questionnaire; 21% were <30 years and 60% 30 to 50 years of age; 57% had worked in health care for >10 years. 99% used a computer as part of their daily work with 59% stating general and 37% advanced proficiency. Overall attitude regarding the EMR is given in the table.
CONCLUSIONS:
We have seen provider anticipation, engagement and acceptance of the EMR implementation. Providers are aware of the need for an EMR and the benefits for patient care. The majority of providers use computers in their daily work and are proficient in its use. We plan to perform a post go-live RA questionnaire to ensure ongoing provider engagement.
Table 1).
| Will encourage EMR use by colleague | The EMR will help me provide effective patient care | I am not satisfied using a paper-based patient record | All providers should learn to use the EMR effectively | Overall, my attitude about EMR use is positive | |
|---|---|---|---|---|---|
| Disagree / Strongly Disagree (%) | 2(1.2) | 19(11.9) | 24(16.9) | 0(0) | 10 (6.3) |
| Neither Agree or Disagree (%) | 28 (17.4) | 43 (27.0) | 28(17.5) | 17 (10.7) | 19(11,.9) |
| Agree / Strongly Agree (%) | 121 (75.2) | 84 (52.8) | 79 (49.4) | 136 (85.5) | 124(77.5) |
| Don’t Know (%) | 10(6.2) | 13(8.2) | 7 (4.4) | 8 (5.0) | 7 (4.4) |
| Total | 161 | 159 | 160 | 159 | 160 |
Abstract
BACKGROUND:
Wait time reduction for outpatient appointments has been connected to reduced healthcare costs and improved patient outcomes. At the pediatric hospital where this study was performed, one key goal of the administration was to reduce wait times for pediatric sub-specialists, particularly appointments for new referrals (also known as “Wait One”). However, attempts to measure and improve these entry-level wait times were hampered by an incomplete understanding of how referrals were handled by the sub-specialist divisions.
OBJECTIVES:
The purpose of this ethnographic study was to describe the steps by which a new referral to each of ten of the pediatric sub-specialist divisions was processed, triaged, and booked.
DESIGN/METHODS:
A qualitative study using standardized open-ended interview questions was carried out with each divisional administrator involved in referrals. They were asked to describe the process they followed from ‘when the new referral hits the fax machine’ to when the machine outpatient appointment was booked. Sub-specialist physicians in charge of triaging the referrals were also interviewed to gain greater insight into the process. In addition, employees in the central booking department, which most of the sub-specialist divisions use, were interviewed. Rough time estimates for the different steps were requested, if available. The data collected were arranged into flowcharts.
RESULTS:
The managements of referrals to sub-specialists had some similarities: all 10 had successful mechanisms for funneling urgent appointments into timely appointments if necessary. However, there was variation between divisions for less urgent new referrals: 60% of divisions utilized many triage categories based on three or more priority levels, and 20% booked based on ‘see by’ time frames, in contrast to others using only urgent and non-urgent categories; 30% had new referral declination/redirection measures to reduce backlog, while others accepted virtually all referrals; 30% pooled all referrals to be distributed to any specialist in the division, while others assigned a referral to a specific physician based on the preliminary diagnosis.
CONCLUSIONS:
These flowcharts we created highlight differences and similarities between divisions for dealing with new referrals. This information is useful in guiding future data collection on Wait One times in our hospital, and this in turn will help in the design and institution of effective and feasible measures for reducing such Wait One times.
Abstract
BACKGROUND:
Residents play a key role in the care of children in the pediatric emergency department (PED). However, the knowledge and preferences parents/guardians (parents) have regarding residents is not established.
OBJECTIVES:
Assess parental knowledge of the definition, level of training, and roles of residents in the PED.
Assess parental preferences with respect to the involvement of residents in the care of their children and how residents introduce themselves and address the parents.
DESIGN/METHODS:
A quality improvement project was undertaken in the PED of a large urban tertiary care children’s hospital. Two surveys were administered to parents, with the first survey containing questions assessing parental knowledge of the definition, level of training, and roles of residents. The second survey provided parents with a definition of a resident and assessed parental preferences. Responses were reported on Likert scales where appropriate.
RESULTS:
A total of 99 parents were surveyed (77% female). Thirty-nine percent (95% CI 30% to 49%) of parents did not know that a resident is a doctor and 32% (95% CI 24% to 42%) did not know that residents require supervision. Eighty-two percent (95% CI 73% to 88%) of parents felt it was important to know the level of training of their doctor in the PED and 73% (95% CI 64% to 81%) felt it was ok for supervised trainees to care for their children. Eighty-seven percent (95% CI 80% to 94%) of parents preferred residents to introduce themselves with a ‘Dr’ prefix and 90% (95% CI 83% to 95%) wanted the doctor to state their level of training. 41% (95% CI 32% to 51%) of parents preferred to be addressed as ‘Mom/Dad’ and 31% (95% CI 23% to 41%) by their first name, but 71% (95% CI 61% to 79%) of parents did not perceive this to be important.
CONCLUSIONS:
A large proportion of surveyed parents did not have a strong understanding of the definition, level of training, and roles of residents but expressed a desire to be informed of the level of training of doctors involved in the care. Parents preferred residents to introduce themselves with a ‘Dr’ prefix. This project underscores the importance of communication with, and empowerment of, parents of children brought to PEDs and may provide guidance for interactions between residents and families in the future.
Table 1).
| Statement (N=99) | True (N) | False (N) | Do not know (N) |
|---|---|---|---|
| An attending doctor needs supervision by a resident | 16 | 59 | 24 |
| A resident is a doctor | 60 | 23 | 16 |
| A resident has finished medical school | 67 | 18 | 14 |
| A resident is the most highly trained doctor in the Paediatric Emergency Department | 12 | 69 | 18 |
| A resident does not need any supervision when caring for patients | 18 | 66 | 14 |
| A resident needs several years of training to become an attending doctor | 73 | 10 | 16 |
| A resident is the boss of the Paediatric Emergency Department | 5 | 79 | 15 |
| Residents and medical students are at different levels of training | 75 | 11 | 13 |
Abstract
BACKGROUND:
To improve health outcomes and enhance patients’ health care experiences, research-based evidence is necessary for the decisions of health care professionals. Undertaking clinical research in the paediatric population, however, presents many unique legal and ethical issues. Children are considered a vulnerable population and as such, numerous methodological challenges arise in relation to their participation in research. Predictably, these difficulties may deter researchers and funding bodies, and have contributed to a dearth of high quality paediatric research. Indeed, <40% of medical decisions have the support of the required level of evidence and <50% of medicines administered during childhood have been formally studied in children. Subject recruitment is essential for conducting clinical research, yet is often perceived as the primary barrier to conducting research in the paediatric population. However, there are very few studies evaluating research uptake in a paediatric setting.
OBJECTIVES:
The primary objective of this study was to determine how frequently paediatric patients and their families receiving care at a tertiary paediatric hospital participate in research. The secondary objectives were to explore factors that influence patient families’ decisions to participate in research and how they perceived their experiences.
DESIGN/METHODS:
We conducted a cross sectional study surveying families of children receiving care in a sample of clinical areas at a tertiary care paediatric hospital in the province of British Columbia, Canada. We used a self-administered questionnaire facilitated by trained interviewers. We used descriptive statistics to report the proportion of patient families that have previously been invited to participate in research, and among these, the proportion that had agreed to participate. We also report how patient families perceive research and their past experiences therein.
RESULTS:
We approached 657 families, of which 543 were enrolled (uptake rate of 82.6%). We found that 26% [95% CI 0.22 to 0.30] had previously been invited to participate in research, and 86.8% (95% CI 0.79 to 0.92) of those respondents had agreed to participate. Only a single family (1.1% [95% CI 0.00 to 0.06]) had a negative experience while previously participating in research, and 80.5% (95% CI 0.77 to 0.84) of all families were at least somewhat likely to participate in research again in the future.
CONCLUSIONS:
Despite the majority of patient families having never been invited previously to participate in research, there is a high rate of participation and willingness to partake again among those who are invited in a paediatric setting.
Abstract
BACKGROUND:
Up to 59 percent of children with bilateral vocal cord paralysis require a tracheostomy for airway management. While the recurrent laryngeal nerve is usually compromised, the cricothyroid muscle, a tensor of the vocal cords has a separate innervation.
OBJECTIVES:
We report an innovative approach whereby a tracheostomy is averted by injecting Onabotulinum Toxin into the cricothyroid muscles in patients with bilateral vocal cord paralysis. The goal is to denervate the cricothyroid muscles thereby decreasing vocal fold tension and a subsequent increase in the glottic space.
DESIGN/METHODS:
We review pediatric cases of bilateral vocal paralysis managed with Onabotulinum Toxin A injections by the senior author. Medical charts were retrospectively reviewed; the clinical manifestation, injection dosage and outcomes are reported.
RESULTS:
Six patients were included. Five were female and one male infants, ranging from three weeks old to four years old. The clinical presentations included stridor and respiratory distress. We used Onabotulinum toxin to paralyze the cricothyroid muscles of five patients who would have undergone a tracheostomy for airway obstruction secondary bilateral vocal cord paralysis. We had a successful decanulation of an additional patient with a long-term tracheostomy for the same pathology. No complications were reported.
CONCLUSIONS:
Onabotulinum toxin injection in the cricothyroid muscles provides a safe, fast, effective and successful option for patients suffering with vocal cord paralysis.
Abstract
BACKGROUND:
Vocal cord paralysis is known to be associated with Arnold Chiari malformation (ACM). Bilateral vocal cord (VC) paralysis has been reported to account for 30% to 60% of pediatric VC paralyses. Surgical management of ACM often leads to resolution of the VC paralysis.
OBJECTIVES:
The aim of this review was to evaluate the effect of primary surgical management of ACM on VC paralysis.
DESIGN/METHODS:
A comprehensive search was carried out on electronic databases of Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid MEDLINE Daily and Ovid OLDMEDLINE, Embase, and Cochrane Library. Articles published between 1946 and July 2013 were retrieved. Search terms included medical subject subheadings and free text words with Arnold Chiari, ac, Chiari malformation, vocal cord paralysis, and vocal folds. Eligibility criteria included studies in the pediatric population where patients had clinical and radiological diagnosis of ACM; clinical diagnosis of VC paralysis had to be confirmed with laryngoscopy. Eligible articles also had to include the surgical management carried out and the VC outcome after the management.
RESULTS:
Eighteen articles fulfilled inclusion criteria, for a total of 31 patients. Fifty-eight percent of patients were males. All patients received surgical interventions, which included surgical decompression, shunt operation or a combination of shunt operation and decompression. 67.7% showed full recovery of their VC paralysis. Partial resolution occurred in 22.6% of patients, while 9.7% showed no improvement at all. Complete recovery of VC function occurred either immediately postoperatively or up to several weeks after surgery and was sustained long-term.
CONCLUSIONS:
Vocal cord paralysis associated with ACM resolved fully or partially in over 90% of patients following neurosurgical decompression without a need for further laryngeal surgery. This was noticed long-term.
Abstract
BACKGROUND:
Peu décrite dans la littérature, la voie transmuqueuse buccale (TMB) pour l’administration de médication de confort chez les nourrissons en fin de vie est depuis longtemps privilégiée par notre équipe de soins palliatifs pédiatrique (SPP). Son utilisation demeurait cependant jusqu’à présent basée sur une évaluation non standardisée des enfants.
OBJECTIVES:
Établir la faisabilité d’implanter un protocole de soins de confort standardisé par voie TMB chez les nourrissons en fin de vie.
DESIGN/METHODS:
Cette étude prospective a été réalisée dans une population d’enfants en fin de vie à l’unité néonatale de notre centre hospitalier universitaire pédiatrique de mars 2011 à 2013. D’abord, un protocole de confort prescrivant la médication par voie TMB (opiacés, benzodiazépines, anticholinergiques) et son évaluation standardisée ont été établis. Ensuite, chaque nourrisson souffrant d’une pathologie à issue potentiellement fatale avec orientation vers des soins de confort exclusifs s’est vu offrir notre protocole. Chaque enfant était évalué avec l’échelle N-PASS aux 4 heures, lors de l’administration d’une médication (0, 30 et 60 minutes post dose) et lorsque jugé pertinent par les soignants. La satisfaction des intervenants a été évaluée à l’aide d’un questionnaire. La faisabilité d’implanter le protocole a été déterminée par 3 paramètres: la proportion d’évaluations faites lorsque requises, le taux de cessation du protocole et les commentaires des infirmières l’ayant utilisé.
RESULTS:
Douze patients ont été inclus dans l’étude. L’âge médian des nourrissons à l’introduction du protocole était de 8 jours (3–39) et la durée médiane de celui-ci, de 2 jours (0–22). Les évaluations régulières ont été réalisées dans 85% du temps. Lors d’une médication au besoin, 71% des cas ont été évalués préalablement, contre 63% pour les doses régulières. Les doses au besoin étaient suivies d’une évaluation à 30 minutes dans 49% des cas et à 60 minutes pour 41%, pour un total de 64% dans l’heure suivant l’administration de la médication. Outre deux patients exclus de l’étude car transférés à domicile, aucun protocole n’a été cessé. Finalement, 17/18 infirmières ont affirmé qu’elles recommanderaient ce protocole à d’autres institutions, mais que le nombre d’évaluations devrait être diminué.
CONCLUSIONS:
Dans un contexte de SPP néonataux, l’implantation d’un protocole standardisé d’administration de médicaments par voie TMB est réalisable. Son utilisation et l’analyse qu’en a faite le personnel infirmier incitent à sa diffusion. Par contre, l’adhérence limitée aux fréquentes évaluations oriente vers un nombre moindre afin de faciliter son implantation.
Abstract
BACKGROUND:
Paediatric palliative care (PPC) focuses on achieving the best possible quality of life for children with life-threatening conditions and their families. To achieve this goal, paediatricians have to identify the needs of children with life-threatening conditions and provide care that responds adequately to suffering.
OBJECTIVES:
This study investigates how paediatricians define PPC and their perception of the needs of children with life-limiting diseases.
DESIGN/METHODS:
Cross-sectional survey of a sample of 2485 Canadian paediatric specialists and subspecialists. The Canadian Paediatric Surveillance Program (CPSP) provided the sampling frame and survey management. The survey was distributed electronically and in hard copy formats.
RESULTS:
Of 420 respondents (17% response rate), 219 (52%) cared for patient with PPC needs in the month prior to the survey distribution. Most paediatricians (78%) offered a definition that included, but was not limited to end-of-life, 17% defined it as end-of-life only, and 5% did not know. A majority (58%) agreed with the four broad groups of children who would benefit from PPC (progressive conditions in which treatment is exclusively palliative after diagnosis, conditions for which curative treatment is possible but may fail, conditions requiring intensive long-term treatment aimed at maintaining quality of life, and conditions involving severe, non-progressive disability, causing extreme vulnerability to health complications). Of a total of 1127 children with PPC needs, paediatricians cared directly for 861 (76%) without referral to a PPC team. Most frequent PPC needs in these children were: support for family (94%); coordination of services in the community (88%); physical symptom management (84%); respite care (81%); support for child (80%); and care at the time of death (78%). Only 48% felt that their patients were receiving all the services needed. Although paediatricians overwhelmingly cited the need for many types of PPC services, only 35% had referred their patients to PPC and 18% did not have access to PPC team.
CONCLUSIONS:
Canadian paediatricians care for a large number of children with PPC needs. Despite recommendations to refer children to palliative care early in the course of illness, many paediatricians define palliative care as similar to hospice care. Paediatricians need to become familiar and comfortable with the provision of palliative care to children. Residency training and continuing education programs should include topics such as palliative medicine, communication skills, grief and loss, managing prognostic uncertainty, and decisions to forgo life-sustaining medical treatment, spiritual dimensions of life and illness.
Abstract
BACKGROUND:
Mild traumatic brain injury (mTBI), often called concussion, is a common injury sustained by children participating in sports and recreational activities. There is evidence to suggest that children who has sustained a concussion is at increased risk for subsequent head injuries, and that such injuries may be cumulative and lead to prolonged or persistent symptoms. Prevention strategies for mTBI should aim at age-specific mechanism of injury.
OBJECTIVES:
The aim of this study was to determine the mechanisms of minor traumatic brain injury (mTBI) among children presenting to the emergency room.
DESIGN/METHODS:
A retrospective study of all emergency room visits for minor traumatic brain injury suffered by children between zero and 18 years of age between November 2010 and November 2011. Children with loss of consciousness, post-traumatic amnesia and/or short-lived impairment of neurological function were considered to suffer from mTBI.
RESULTS:
A total of 518 cases of mTBI were reported, 87 were not considered for this study due to missing information required for diagnosis of mTBI. A total of 431 confirmed case of mTBI were identified with an estimated incidence of 12.7 per 1000 children per year (95% CI 11.6 to 13.9 per 1000). Of these, 191 (44%) were children between 0 and 4 years of age, 70 (16%) five to nine years old, 96 (22%) 10 to 14 years old and 74 (17%) 15 to 17 years old. The two most frequent mechanisms leading to mTBI were falls from height (38%) and sports related injury (27%). The latter was responsible for 61% of mTBI suffered by children between 10 and 17 years of age, when, on the other hand, falls from height represented 69% of the zero to four years old cases.
CONCLUSIONS:
mTBI is very prevalent in the pediatric population and is caused by a variety of mechanisms. This study reveals that mTBIs affect preschoolers at home resulting from a fall from a height in proportion comparable to sports related mTBI among older children.
Abstract
BACKGROUND:
Soft tissue neck radiographs (STNRs) have always been recognized as a helpful tool to differentiate benign causes of acute upper airway obstructions (AUAO) from epiglottitis, retropharyngeal abscess or foreign body aspiration among children.
OBJECTIVES:
Based on the frequency at which some of those life-threatening pathologies now occur, are STNRs still widely used, at which intent and what is the impact of their clinical use?
DESIGN/METHODS:
A retrospective, observational study was conduct to examine STNR use and usefulness in the pediatric population. All the medical files from children zero to 17 years of age who had a STNR between January 1, 2010 and December 31, 2011 in a mid-size Canadian university pediatric hospital were reviewed. STNRs were identified using the hospital electronic radiologic studies database. From all STNRs, those performed in an AUAO context were analyzed. Patient’s characteristics, symptomatology, likely diagnosis before STNRs, and final interpretations by radiologists were collected. To evaluate the value of STNR regarding AUAO, patients were divided in two groups according to the conditions clinicians first suspected (benign vs. life-threatening: retropharyngeal abscess/epiglottitis/bacterial tracheitis/foreign body aspiration) and compared the STNRs’ interpretations with Fisher exact test. In addition, based on discharge diagnosis from hospitalisation charts, cases of epiglottitis and retropharyngeal abscess for the same period were reviewed.
RESULTS:
Among 520 STNRs identified, 88% intended to evaluate AUAO among children (2010, n=231; 2011, n=226). Nearly all (99%) took place at the emergency room, with 73% of patients presenting with triage score 3 and above, and 49% necessitating admission. Most STNR were performed among males (67%) younger than five years of age (66%; mode one year of age). A life-threatening cause of AUAO was first suspected by clinicians among 40% of reviewed charts. However, convincing radiologic signs of life-threatening pathologies were only found in 40 children (9%), with no significant statistical difference based on clinicians’ suspicions (11% for life-threatening vs. 7% for benign conditions suspected; P=0.128). Overall, two cases of epiglottitis and eight retropharyngeal abscesses were diagnosed during the study period, among which four of five STNR were positive.
CONCLUSIONS:
STNR is a radiologic study that is frequently used among children, mostly in the context of moderate to severe AUAO. The current value of STNRs appears uncertain as few showed solid evidences that may modify how clinicians currently manage pediatric AUAO.
Abstract
BACKGROUND:
CARESS is a prospective registry that documents utilization, compliance and health outcomes of all Canadian infants who received ≥1 dose of palivizumab for respiratory syncytial virus (RSV) prophylaxis across 32 sites during the 2005–2013 RSV seasons.
OBJECTIVES:
To determine factors associated with palivizumab compliance among recruited infants.
DESIGN/METHODS:
Neonatal and demographic data were collected at enrolment. Hospitalizations related to respiratory illness (RIH) and RSV-related infection (RSVH) were collected monthly. Compliance was defined as receipt of all expected injections at 25 to 35 day intervals during the season. Logistic regression was used to assess independent predictors of compliance.
RESULTS:
16,290 infants received an average of 90.5±18.2% of expected injections and 73.3% were within appropriate time intervals. Compliance differed between indications for prophylaxis (χ2=22.717, P<0.0005). Premature infants ≤35 weeks gestational age had the highest compliance (7864 of 10,576 [74.4%]), followed by infants with chronic lung disease (949 of 1290 [73.6%]), those with other pre-existing medical disorders (1915 of 2666 [71.8%]), and infants with hemodynamically significant congenital heart disease (1220 of 1758 [69.4%]). Factors independently associated with compliance (OR [95% CI]; P value) were: household crowding (1.13 [1.04 to 1.23]; P=0.005), siblings (1.11 [1.03 to 1.21]; P=0.006), maternal smoking (0.81 [0.74 to 0.90]; P<0.0005) and Aboriginal status (0.74 [0.62 to 0.89]; P=0.002). After adjusting for risk factors, compliance was significantly associated with lower hazard rates of RIH (0.85 [0.74 to 0.96]; P=0.012), but not RSVH (0.97 [0.95 to 1.70]; P=0.83).
CONCLUSIONS:
In the CARESS registry, compliance with RSV prophylaxis across eight RSV seasons is associated with several, known demographic and environmental risk factors including Aboriginal status. Better compliance resulted in lower RIH hazard rates though the effect on RSVH was insignificant.
Abstract
BACKGROUND:
While written action plans are standard in the treatment and management of asthma, variability exists in the content and format amongst plans. This variability results in inconsistent educational messages that lend themselves to patient confusion and decreased health outcomes.
OBJECTIVES:
We aimed to assess the content of Canadian pediatric written action plans for consistency in format, layout, zone-defining symptoms, suggested treatment options, and adherence to current Canadian asthma care guidelines.
DESIGN/METHODS:
Written action plans were sought from Canadian pediatric hospitals, teaching hospitals associated with academic centres, and from three national organizations, for a total of 17 plans. An analysis was carried out to assess the similarities and differences amongst the written action plans in relation to the study’s objectives.
RESULTS:
Of all the Canadian pediatric written action plans, 76% were found to consist of three zones and 82% incorporated a traffic light-style design. The plans were divided between symptom-based (59%) and combined symptom- and peak-flow approaches (41%). The most common symptom descriptor in the green zone was “normal life/regular activities” (76%), in the yellow zone it was “cold/cold symptoms” (94%), and in the red zone it was “reliever medication does not work as usual” (53%). Considerable variability existed amongst written action plans and the symptom descriptors that define each zone. This variability was exemplified in the red zone where a total of twenty-four different symptom descriptors existed across the plans, but on average an individual plan contained only five symptom descriptors. Only 53% of asthma action plans mentioned asthma triggers within the plan. Greater consistency existed amongst the treatment strategies. However, the suggested treatment was often left to prescriber discretion as some plans included a blank text box to be filled by the health-care provider. In relation to the 2012 Canadian Thoracic Society guidelines, it was found that 59% of plans specified that inhaled corticosteroids should be taken daily, 47% of plans included a framework for an inhaled corticosteroid escalation strategy, and 41% of plans included oral corticosteroids as a treatment option.
CONCLUSIONS:
Canadian pediatric written action plans would be improved by nationally clarifying the symptom descriptors for each zone, the addition of asthma trigger information, increased emphasis on the common cold as a potential harbinger of worsening asthma symptoms, and further adoption of Canadian Thoracic Society guideline recommendations.
Abstract
BACKGROUND:
FeNO is a known marker of airway inflammation, and is a topic of recent investigation for asthma control in children.
OBJECTIVES:
To investigate the relationship between FeNO and known parameters of asthma control in a regional paediatric asthma center. A secondary objective was to investigate the correlation between different types of inhaled corticosteroids (ICS) and FeNO concentration.
DESIGN/METHODS:
We conducted a retrospective chart review of children tested with both spirometry and FeNO over a one-year period. Collected data included age, anthropometrics, ICS type, equivalent dose, and duration of use, recent oral steroid use, asthma severity score, season, smoking status of family, and the presence or absence of; eczema, allergic rhinitis and respiratory tract infection. Data was analyzed by descriptive statistics and stepwise linear regression. A univariate generalized linear model was built to evaluate FeNO by ICS type, while correcting for statistically significant covariates.
RESULTS:
A total of 183 children were included. Mean (± SD) age was 12.8±2.8 years. Fluticasone was used most commonly (n=66, 36.1%) followed by ciclesonide (n=50 [27.3%]). Most children had moderate-persistent asthma (n=73 [39.9%]). FeNO level was associated with percent-change in FEV1 while adjusting for allergic rhinitis, parental smoking and ICS type (B=0.08 [95% CI 0.04 to 0.12]; P<0.001). Likewise, FeNO was associated with percent-change in FEF 25–75 while adjusting for parental smoking and ICS type (B=0.13 [95% CI 0.01 to 0.24]; P=0.03). However, FeNO accounted for only 16% and 9% of the variability in FEV1 and FEF 25–75, respectively. FeNO level differed by ICS type, while adjusting for equivalent dosing, allergic rhinitis and weight. Mean adjusted FeNO was lowest in fluticasone users compared to no ICS (mean difference ppb = 18.3 (95% CI 4.5 to 32.1]) and there was no difference in adjusted FeNO level between ciclesonide and no ICS (6.1 [95% CI −5.9 to 18.2]).
CONCLUSIONS:
FeNO levels correlate with known parameters of asthma control in a regional pediatric asthma center. However, FeNO accounts for only 16% and 9% of the variability in FEV1 and FeF 25–75. Mean adjusted FeNO varied by ICS type suggesting there is a difference in relative efficacy between inhaled corticosteroids beyond their dose equivalents.
Abstract
BACKGROUND:
Parents seek child health information for dealing with acute illnesses, guidance on parenting, and to improve knowledge of child development. There are many comprehensive child health information sources available; however, no centralized access point exists making navigation a challenge for many parents. Well-defined barriers include access, language, appraisal of information sources, and health literacy.
OBJECTIVES:
This study aimed to determine the health knowledge needs, information resources, and barriers to access among families with well children aged zero to 12 years who are seeking preventative or proactive health knowledge information.
DESIGN/METHODS:
Ethics approval was obtained from our institutional Quality Improvement Projects review board. Six focus groups were conducted with parents of children aged zero to 12 years from various racial and socioeconomic backgrounds. Focus groups were recorded and transcribed using a professional transcription service. Data analysis involved thematic coding of transcripts. Data triangulation was achieved by having multiple investigators code the first focus group to develop, through a consensus-building approach, a series of general themes that were explored across data sets. This model was refined using the subsequent focus group data. Major themes and sub-themes were determined by analyzing trends and patterns.
RESULTS:
Analysis yielded four major themes: sources for health information, information autonomy, insecurity, and barriers. Major sources of health information included the internet, physicians, and help lines. Information autonomy referred to parents’ ability to make decisions and obtain information without health care assistance. Insecurity referred to acute or chronic stress associated with child health and wellness issues. Barriers referred to social and health care related difficulties in accessing information. A central theme, empowerment, was found to link all major themes. Empowerment referred to parents’ ability to be successfully involved in the care of their child in terms of information seeking, investigation and maintaining general well-being. A subgroup of parents were unempowered and described a lack of information autonomy, a higher level of insecurity and more varied and severe barriers in caring for their children. Parents expressed a desire for a resource that is broadly accessible, interactive, personalizable, credible, up to date, and intuitive.
CONCLUSIONS:
In a subgroup of unempowered parents, it may not be adequate to give specific information for discrete issues as this may perpetuate reliance. The goal of child health information resource development should be to produce a system that will empower all parents and provide the tools and resources for parents to search for information autonomously and effectively.
Abstract
BACKGROUND:
Sleep problems occur in up to 25% of children and are more prevalent in children who have symptoms of inattention/hyperactivity as well as those who are insecurely attached to their caregivers. Studies show that foster children display sleep problems, but limited research exists on the prevalence and etiology of specific sleep disorders in adopted children.
OBJECTIVES:
To investigate the relationships between psychosocial factors and the incidence of sleep disorders in adopted children.
DESIGN/METHODS:
Participants were recruited through a notice sent to parents on an adoption council listserv and through discussion with families attending a social service meeting. Families were eligible to participate if their child was between two and seven years of age. Thirty parent questionnaires, measuring demographics, behavior, parent/child relationships, and sleep problems, were sent to families. Responses were analyzed using descriptive statistics and correlations. T-tests were used comparing children reported to be good vs. poor-sleepers.
RESULTS:
A total of 67% responded (n=20). Twelve children (60%) had sleep problems based on the Children’s Sleep Habits Questionnaire. As compared to good-sleepers, those reporting sleep problems experienced more parasomnias (P<0.002) and trends to issues with sleep onset delay and sleep duration. Children with sleep disorders also had more attention problems (P<0.025), which correlated significantly with parental attachment scores (r=−0.69, P=0.01).
CONCLUSIONS:
Sleep disorders (especially parasomnias) were frequently reported in adopted children. Those reporting sleep disorders showed more attention problems, which were associated with lower levels of parental attachment. Further research in this area will help to develop targeted interventions to prevent sleep disorders in adopted children.
Abstract
BACKGROUND:
Cleft lip is a common facial defect with an incidence of 1:750 to 1:1000 and can be unilateral or bilateral. It can occur as an isolated defect or in association with cleft palate. Feeding difficulties are well documented in babies with cleft lip and management requires multidisciplinary approach. There are many controversies regarding the timing of surgery and the post-operative care with specific emphasis on feeding mode.
OBJECTIVES:
This study was designed to determine that early-unrestricted breast and bottle-feeding has no detrimental effect on the repaired cleft lip.
DESIGN/METHODS:
Single institution, randomized controlled trial was conducted between January 2013 to November 2013 and data of 40 patients with isolated cleft lip were analysed. Guidelines regarding surgical technique and the timing of surgery (three to 15 months) were identical in both groups. Postoperatively, two different feeding protocols were set, Group 1; included patients who were fed with spoon for 14 days; whereas, in Group 2; breast or bottle feeding was started immediately. Patients were assessed for wound dehiscence on follow up for one month.
RESULTS:
Of 40 patients, five lost follow-up. The remaining 35 patients were analysed and their age ranged between three to 15 months. On follow up, presence of early wound complication of wound dehiscence was observed. Partial wound dehiscence occurred in two patients of group 1 and only in one patient of group 2. Other 32 patients had a good primary wound healing. We believe this reason to be due to poor compliance of postoperative wound care and not due to mode of feeding.
CONCLUSIONS:
Cleft lip is a common facial defect with multiple controversies in various aspects of its management. In this study we highlight the controversies regarding the postoperative feeding protocols. Several postoperative feeding protocols had been reported in the literature. Conservative approach and restrain from feeding is still the approach of choice by majority of surgeons. In this cohort, we observed that in patients for whom feeding was started immediately after repair, there was no early wound complication like dehiscence as compared to those who were only fed through spoon or glass. On basis of which we concluded that breast and bottle-feeding is safe and has no detrimental effect on wound healing. We recommend that unrestrained breast or bottle-feeding should be included in the postoperative protocols for all babies undergoing cleft lip repair.
Abstract
BACKGROUND:
Children experiencing sexual abuse (SA) are found to display significant internalizing and externalizing behaviour problems compared to non-abused children, In addition, victims of sexual abuse also appear at greater risk of dissociative symptoms than non-maltreated children. Adult studies have shown a link between dissociation and sleep disturbances. Yet, few studies have been conducted with young children although retrospective studies on adult survivors have shown that the pre-school period may be crucial in the development of dissociation.
OBJECTIVES:
The aim of this study was to document the contribution of sleep problems to the prediction of dissociation in sexually abused preschoolers.
DESIGN/METHODS:
The sample consisted of 224 children and the non-offending mother who were referred to the Child Protection Clinic of a tertiary care hospital following alleged SA. Abuse-related variables were abstracted from medical records. The child’s level of dissociative symptoms was assessed with the Child Dissociative Checklist and the seven-item Sleep Problems subscale of the Child’s Behavior Checklist (Achenbach & Rescorla, 2000) was used as an index of sleep disturbance. Maternal psychological distress was evaluated by the Psychiatric Symptom Index. Factors contributing to the prediction of dissociative symptoms were evaluated with a hierarchical multiple regression analysis.
RESULTS:
The mean (± SD) age of the participants was 4.6±0.7 years, and there were 33 boys and 191 girls. Approximately 36% of SA children reported a single episode of abuse, 40% reported more than two episodes and 24% abuse lasting for more than six months. SA was described as complete or attempted penetration in 46% of cases. An immediate family member was identified as the perpetrator in 60% of cases. Entering age and sex of the child and maternal psychological distress in the multiple regression analysis to predict dissociative symptoms gets an R2=0.14, F (2, 138)=7.31; P<0.001. Adding other traumas experienced resulted in a significant increment in R2=0.20, F(1, 137)=10.97; P<0.01. With the addition of sleep disturbance, prediction of dissociation symptoms reached R2=0.37, F(1, 136)=36.07; P<0.001. After controlling for socio-demographic and maternal variables, and other traumatic experiences, sleep disturbance significantly added to the prediction of dissociative symptoms.
CONCLUSIONS:
Sleep disturbances appear to contribute to the frequency of dissociative symptoms. This regulation deficit should be addressed promptly, in order to help decrease long-term detrimental effects of sexual victimization, such as the development of dissociation.
Abstract
BACKGROUND:
Abdominal trauma is an uncommon and poorly recognized form of child abuse associated with a high risk of mortality. Abuse is considered as a possible cause when the mechanism of the injury is poorly explained and/or there are other indicators of physical abuse. Physicians may also screen for occult abdominal injuries in the context of other signs of physical abuse, however currently no recognized guideline exists for the identification of occult inflicted abdominal injuries
OBJECTIVES:
The goal of this study was to describe the current practices of Canadian experts in Child Maltreatment in the assessment of abdominal injury. This information will help inform the future development of national guidelines on this topic.
DESIGN/METHODS:
A 21- item survey was developed and reviewed for content. The anonymous electronic survey was sent to participants in the 4th Canadian Symposium on Advanced Practices in Child Abuse Pediatrics and to the Canadian Pediatric Society (CPS) Child Maltreatment section members. The survey contained questions on demographics, experience and current practices with cases of abdominal trauma and approach to clinical scenarios.
RESULTS:
The survey was completed by 46 of 162 individuals (54 Symposium participants and 108 Section members) for a response rate 28.4%. Respondents were primarily pediatricians (88.1%). Cases of abdominal trauma had been assessed by 65.9% of respondents, with 76.9% of these having seen one to five cases. Cases most commonly involved injuries to the liver (n=16 [61.5%]), intestine (n=13 [50%]), spleen (n=9 [34.6%]) and pancreas (n=8 [30.8%]). Occult solid organ and intestinal injuries were identified through screening bloodwork, however mesentery/vascular injuries were not. Most physicians (97%) sometimes or always ordered screening tests for abdominal injury in cases of suspected physical abuse. The most frequently ordered tests were AST (n=38 [97.4%]), ALT (n=37 [94.9%]), amylase (n=26 [66.7%]), lipase (n=26 [66.7%]) and urinalysis (n=26 [66.7%]). Respondents were most likely (65.8%) to recommend a CT scan if suspecting a possible visceral injury, however 26.3% recommended an ultrasound. Most respondents (81.6%) favoured a national guideline on this topic, with 50% indicating that there were areas of controversy/uncertainty that created difficulty in formulating a child maltreatment opinion on cases.
CONCLUSIONS:
This study provides a description of the current experiences and practices in cases of abdominal injury of Canadian child maltreatment physicians. There is substantial variability in number of cases assessed, organs involved, and medical testing used in assessments. Child maltreatment pediatricians support the need for a clinical guideline on this topic.
Abstract
BACKGROUND:
Adolescent sleep deprivation is common and has a significant negative impact on health and well-being. Pediatric health care professionals must measure sleep timing accurately in order to identify and then treat sleep deprivation in this age group. Currently, parents often respond on behalf of their child and are inaccurate in reporting their child’s sleep timing. It is possible that asking the adolescent directly about their sleep patterns may yield more accurate sleep information. However, there is a lack of research evaluating how well adolescents are able to estimate their sleep timing.
OBJECTIVES:
The current study seeks to compare adolescent self-reported and objective actigraphy estimates of bedtime and wake time in order to assess how valid adolescents are in reporting their sleep timing on the weekdays and weekends.
DESIGN/METHODS:
Adolescents were recruited from a high school in Montreal and survey completion took place in classrooms during school hours. Thirty-five participants answered a four-item questionnaire pertaining to when they typically went to bed and woke up on weekdays and weekends. Sleep duration was then calculated as a function of bedtime and wake time. All participants underwent actigraphy and completed sleep logs for five consecutive weekdays. Twenty-seven of the 35 participants also underwent actigraphy and completed sleep logs on the weekend.
RESULTS:
There were significant positive correlations between actigraphy and survey data for sleep variables including weekday sleep start time (r=0.71), end time (r=0.77) and sleep duration (r=0.63), and weekend sleep start time (r=0.68) and end time (r=0.82) but not sleep duration (r=0.22). While adolescents reported sleeping for an average of 10 h on weekend nights, actiwatch data indicated that they were sleeping for only 8.8 h.
CONCLUSIONS:
Adolescents can accurately report their sleep timing on weekdays. One explanation for the non-significant correlation between actigraphy and survey weekend sleep duration data is that actigraphy sometimes interprets movement during sleep as a state of wake, thus causing a decrease in the estimation of actual sleep. In addition to asking parents about their child’s sleep habits and assessing sleep objectively, health care professionals should consider asking adolescents directly about their sleep timing.
Table 1).
Pearson correlations between actigraphy and survey sleep variables. **Correlation is significant at the 0.01 level
| Sleep Variable | Correlation (r) |
|---|---|
| Weekday Start Time | .71** |
| Weekday End Time | .77** |
| Weekend Start Time | .68** |
| Weekend End Time | .82** |
| Weekday Sleep Duration | .63** |
| Weekend Sleep Duration | .22 |
Abstract
BACKGROUND:
The media has long been established as a powerful socializing agent for youth. Recently, there has been an upsurge in media portraying teen pregnancy and parenting, such as ‘Teen Mom’. While this type of programming is tailored to teens, research has not yet examined ways in which pregnant and parenting adolescents deconstruct these media messages. Moreover, it remains unknown whether media depictions of teenage motherhood shape the meanings pregnant teens and young parents construct about health and well being, and whether these perceptions influence their health behaviours.
OBJECTIVES:
This study explored pregnant and parenting teens’ experiences with and perceptions of media messages portraying teen pregnancy, as well as how media messages influenced their social and health interactions.
DESIGN/METHODS:
Five focus groups were conducted at two urban community centres that service pregnant youth and young parents. A convenience sample of 26 participants was recruited across both sites. Focus groups were audio recorded and transcribed verbatim, then analyzed thematically. To establish trustworthiness in the findings, the researchers triangulated focus group data, maintained an audit trail and engaged in peer debriefing.
RESULTS:
Participants were a mean age of 18.7 years, and accessed broadcast media, print media and film containing teen pregnancy and parenting content. Participants were acutely aware of the negative impact of media messages on public perception, noting that the storylines in television reality programming were highly incongruent with their lived experiences. They felt these representations glamorized teenage pregnancy while failing to capture other realities of teenage parenting, such as the financial struggles and necessary role transitions. Moreover, that these representations reinforce damaging stereotypes, render maternal judgement and criticism socially acceptable, and create a double standard for teen parents. They felt that healthcare providers were not immune to media messaging; some participants reported withdrawing socially and delayed accessing health services because of the media-fuelled public views.
CONCLUSIONS:
This study highlights the need for heightened awareness of the influence of popular media on the construction of notions of teen pregnancy and parenting. Acknowledging and challenging stereotypes of teen pregnancy, as well as initiating dialogue with youth about the impact media has in their lives, could act as a protective factor to empower pregnant and parenting teens to engage with healthcare. To enhance the quality of care provided, healthcare providers should elicit the stories of pregnant youth and young parents, and consider their own biases when servicing this vulnerable group.
Abstract
BACKGROUND:
The prevalence of autism spectrum disorders (ASD) is estimated at 62 per 10 000 children based on systematic review of epidemiological surveys worldwide. In many cases, ASDs can be accurately diagnosed in children two to three years old and high risk children can be identified earlier than 24 months, but Canadian data shows a median age at diagnosis of 39 to 55 months. Despite advances in diagnosis of ASD, data on general paediatric practice regarding ASD screening in Canada is lacking.
OBJECTIVES:
The objectives of this study were to examine general paediatricians’ current practices regarding ASD screening and identify the factors that influence paediatricians’ decisions for including ASD screening tools in their clinical practice. The aim was to obtain broad opinions and perspectives to support future research.
DESIGN/METHODS:
Twelve paediatricians from four practice groups participated in four focus groups and one interview. Each focus group took 40 min to 60 min and was conducted using a semi-structured interview with targeted open ended questions, digitally recorded, and transcribed verbatim. A qualitative interpretive description approach was chosen since the aim was to present the participants’ point of view by staying close to the data. All meaningful texts from the transcripts were coded, categorized and reviewed with the co-investigators and final themes were obtained with care taken to describe the participants’ experiences in their own language.
RESULTS:
Five main categories were identified: 1) benefits, 2) limitations, 3) elements that limit utility, 4) elements that foster utility, and 5) process of application in ASD screening. Participants identified factors that influence their current practice such as availability of time, comfort and experience, and knowledge of specific tools. They also identified important barriers and facilitators to ASD screening including screening tool characteristics that influence their decisions to use a formal tool. Furthermore, the participants commented on the current infrastructure for ASD screening and possible changes, such as the participation of allied health professionals and implementation of guidelines that could affect accessibility for both diagnosis and ASD resources.
CONCLUSIONS:
This study identified factors that play into a paediatrician’s role in formal ASD screening as well as obstacles and facilitators to implementing an ASD screening program. While the feasibility and effectiveness of a nationwide autism screening program remains controversial, this study provides grounds for future research questions with implications on policy and practice.
Figure 1).
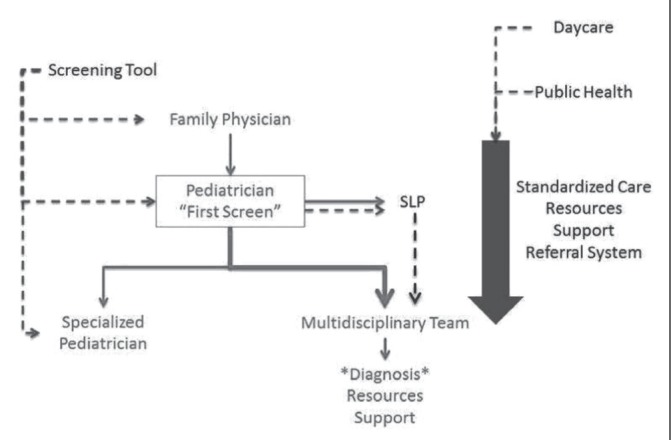
The solid lines show the current process and the dotted lines show suggestions for possible future changes or points for implementation of standardized ASD screening
Abstract
BACKGROUND:
Academic success plays an important role in improving future lifetime opportunities and accumulating evidence indicates that sleep has beneficial effects on academic success. Although a myriad of factors have been identified as being relevant to academic achievement, the role played by sleep in this process has been largely ignored. A considerable proportion of elementary school-aged children sleep for less than the recommended hours per night and 25% to 40% of youth are affected by asleep disorder during infancy, childhood and/or or adolescence. This is a major concern given that restricted sleep can negatively impact the academic performance of children.
Measures used to assess school achievement include report cards marks. Previous studies examining the associations between sleep and marks on report cards used subjective measures of sleep. Thus, we do not know what aspects of sleep are related to performance in specific academic subjects. It is also not known which aspects of sleep are most relevant to academic performance. Determining which aspects of academic performance are specifically affected by poor sleep is important because this can inform the development of sleep interventions to improve these domains
OBJECTIVES:
To examine the association between objectively measured aspects of sleep (sleep duration and sleep efficiency) and report card marks in healthy school-age children
DESIGN/METHODS:
Nighttime sleep was monitored by actigraphy, which uses a wristwatch-like device (AW-64 series, Mini-Mitter) to evaluate sleep through the measurement of ambulatory movement, and parents provided their child’s most recent report card. The study sample consisted of 72 participants between seven and 11 years of age (mean [± SD] 8.85±1.6 years).
RESULTS:
The amount of sleep that children obtained gradually decreased with age. Children in Cycle 1 obtained an average of 608.21±24.65 min, while those in Cycle 2 received 565.7±26.15 min and those in Cycle 3 received 547.43±34.5 min (F[2, 69]=24.65; P<0.0001). Using multiple linear regression analyses it was found that higher sleep efficiency showed a statistically significant association with better marks in Math, English Language, and French as a Second Language above and beyond the contributions of age, gender, and socioeconomic status.
CONCLUSIONS:
Our findings suggest that higher sleep efficiency in healthy school-age children is positively associated with better marks in Math, English Language and French as a Second Language.
Abstract
BACKGROUND:
It is important to identify early predictors of functional limitations in children after congenital heart surgery in order to optimize their independence as they prepare for school.
OBJECTIVES:
The purpose of this study is to determine potentially modifiable predictor variables of functional outcomes in children at 4.5 years of age with congenital heart disease who underwent complex cardiac surgery at six weeks of age or earlier.
DESIGN/METHODS:
This prospective inception cohort study comprised a sample of 165 survivors (63% boys) who had complex cardiac surgery (75% biventricular repairs). We excluded children with chromosomal abnormalities. When children were 4.5 years of age, the parents completed the Adaptive Behavioral Assessment System II questionnaire (ABAS). Regression analysis was used to assess the association between multiple risk factors and each of the four continuous outcomes.
RESULTS:
The mean scores for the practical domain and general adaptive composite (GAC) score of the ABAS were lower than the conceptual and social domains, with 13.3% of the children having a delay (score >2 SD below the population mean) in the practical domain and 14% of the children having a delay on the GAC. There was a significant association between the GAC (P=0.003; P=0.012), conceptual (P=0.0004; P=0.042), social (P=0.0007; P=0.028) and the practical (P=0.046; P=0.003) domain composite scores and mother’s education and highest pre-operative plasma lactate respectively.
CONCLUSIONS:
Maternal education may be a marker for the social context of children, and warrants societal attention to improve functional outcomes. Pre-operative lactate is a potentially modifiable variable that predicts adverse functional outcome. Much effort is already being made to optimize hemodynamics pre-operatively, focusing on the measured lactate; however, continued advances in peri-operative management may yield yet more improvement in this regard, and result in improved outcomes.
Abstract
BACKGROUND:
In Canada the incidence of Fetal Alcohol Spectrum Disorder (FASD) is estimated to be one in 100 live births. FASD is the leading cause of developmental and cognitive disabilities in Canada. In 2007, we examined the cost of FASD in Canada. In that study we did not include prospective data of the cost of diagnosis, the cost of integrating homeless youth into the community, and the cost beyond 53 years of age.
OBJECTIVES:
To calculate a revised estimate of direct and indirect costs associated with FASD at the patient level.
DESIGN/METHODS:
Cross-sectional study design was used. Three-hundred and five (305) participants completed the study tool. Participants included caregivers of children, youth and adults, with FASD, from day of birth to 65 years, living in urban and rural communities throughout Canada. Participants completed the Health Services Utilization Inventory (HSUI). Key cost components were elicited: direct costs: medical, education, social services, out-of-pocket costs; and indirect costs: productivity losses. Total average costs per individual with FASD were calculated by summing the costs for each in each cost component, and dividing by the sample size. Costs were extrapolated to one year. A stepwise multiple regression analysis was used to identify significant determinants of costs and to calculate the adjusted annual costs associated with FASD.
RESULTS:
Total adjusted annual costs associated with FASD at the individual level was $32,840 (95% CI $26,452 to $40,092), compared to $21,642 (95% CI $19,842 to $24,041) in the last study. Severity of the individual’s condition, intellectual level, age, and relationship of the individual to the caregiver (biological, adoptive, foster) were significant determinants of costs (P<0.001). Cost of FASD annually to Canada of those from day of birth to 65 years old, was $6.8 billion (95% CI $5.2 billion to $7.4 billion).
CONCLUSIONS:
Study results demonstrated the cost burden of FASD in Canada was profound. Inclusion of the cost of diagnosis, adults beyond the age of 53 years, and the costs of integrating homeless youth into the community provided a more accurate estimate of the costs of FASD. Implications for practice, policy, and research are discussed.
Abstract
BACKGROUND:
Fetal Alcohol Spectrum Disorder (FASD) has no specific diagnostic marker, and the facial features and growth restriction found in the full Fetal Alcohol Syndrome are found only in a small percentage of children diagnosed within the Fetal Alcohol Spectrum. The presentation of FASD often overlaps with genetic syndromes. Thus, a genetic opinion is frequently requested in the assessment of a child with suspected FASD.
OBJECTIVES:
To study the outcome of genetic assessments of 220 children and youth referred to a FASD clinic between 2009 and 2013.
DESIGN/METHODS:
DESIGN:
Prospective study design.
PARTICIPANTS:
220 children and youth, aged 18 months to 23 years.
SETTING:
FASD clinic in a large teaching hospital in Ontario.
METHODS:
Data from the medical records were abstracted, entered onto a standard study pro forma, recorded in an Excel spreadsheet, and analyzed using simple frequency analysis.
RESULTS:
Sixty-eight percent of children and youth assessed in the clinic were diagnosed with Fetal Alcohol Spectrum Disorder. Twenty-eight percent had at least one facial feature of the full Fetal Alcohol Syndrome including thin upper lip, smooth philtrum, or short palpebral fissures. Only 4% had all of the three facial features. The most common alternative diagnosis was a chromosome disorder including Fragile X, 22q11.2 deletion, Williams Syndrome and others, representing 11.2% of the FASD referrals.
CONCLUSIONS:
Genetic assessment was of particular value in excluding other diagnoses and providing information to caregivers. Structural malformations were not common in the group overall, and some previously reported diagnostic signs were not found to be reliable markers of FASD. Chromosome disorders showed phenotypic overlap with FASD, and are an important differential diagnosis. The study findings support a large multi-centre project.
Abstract
BACKGROUND:
Evidence suggests that parents use the Internet to find information and resources for their children’s health condition, yet web presence differs and some health conditions sell their information and resources more effectively than others.
OBJECTIVES:
The purpose of this study was to compare the web content available in the google domain for five pediatric developmental disorders and to determine the characteristics and implications of these differences for health information and health service access.
DESIGN/METHODS:
Research was conducted on five pediatric developmental disorders: CF, FXS, Down Syndrome (DS), Duchenne Muscular Dystrophy (DMD), and Spina Bifida (SB). These disorders were chosen because they each are: lifelong, incurable, multi-systemic and genetically-based. Content analysis was conducted using a coding sheet that allowed for consistent evaluation of the Google domain content retrieved via standardized search queries. Content analysis was conducted on pre-set dates and times, with the top 30 links being ranked and evaluated.
RESULTS:
Significant differences were seen between the disorders with respect to total number of hits, website category and website content. Averaged over two research sessions, DS and CF accumulated more hits overall (101,300,000 and 23,500,000 respectively) with the other disorders totaling to less than 5,100,000 hits each. For website category, CF and SB were found to have a higher proportion of National Organizations ranking in the top 30 hits; DS had the greatest proportion of local organizations, while DMD and FXS had the majority of their top 30 hits dedicated to health informational databases. A subjective analysis of tone was performed on the top 30 hits; >65% of the websites for both CF and DS depicted an overarching positive tone, while at least 50% of each of SB, DMD and FXS’s hits were neutral. Of note, websites targeted the public as their audience as opposed to those affected by the condition.
CONCLUSIONS:
Although these disorders share many attributes, they present vast differences in both their web presence and web content. CF and DS present a more well-rounded and positive approach to the disease, while FXS, SB and DMD focus more on dissemination of disorder- related information. These disparities in resources and access to information among disorders hold many implications for practicing physicans as well as the health care system at large. Physicians should be mindful that more activist disorders may receive inequitable attention from the health care system. Improvements to tools and information are necessary to provide reliable and useful online resources to families for FXS, SB and DMD.
Abstract
BACKGROUND:
The Multiattribute Health Status Classification System (MHSCS) is a parent/proxy administered tool including a series of health-specific domains that give levels of functioning between 1 (normal health) to 4 or 5 (most severe). Previous studies have used the MHSCS to document chronic health impairment and child morbidity (Gemke et al., 1995; 1996; Feeny et al., 1992; 1993; Saigal et al., 1994). There is a high inter-rater reliability exceeding 70% between caregivers and physiatrists with sensitivity and specificity from acute injury predictors at 75% and 70% (Robertson et al., 2001). The MHSCS is a useful parent-report surveillance tool to audit outcome after severe Traumatic Brain Injury (TBI).
OBJECTIVES:
To assess the post-injury health outcomes of young children sustaining a severe TBI using the MHSCS.
DESIGN/METHODS:
This is a retrospective chart review of children who sustained severe TBI before 12 years of age & were followed in the Brain Injury program. Severe TBI was defined as Glasgow Coma Scale =<8/15. Ethics approval was granted. Demographic variables were collected and expressed as mean (± SD) (range). A multivariate analysis of variance was conducted to compare scores on the MHSCS.
RESULTS:
A total of 18 children (10 male, eight female) mean age 6.84±3.4 years, (range 1.5 to 11.8 years) were reviewed at three years (n=8) or ≥5 years (n=10) post-injury. An independent t test indicated no significant difference between the Total scores at three and ≥5 years (P=0.23) (Chart 1). The overall difference across subscales was not significantly different (Chart 2). The Cognition Subscale scores increased significantly between three and ≥5 years (P=0.038) and the Emotional Subscale scores increased marginally (P=0.073).
CONCLUSIONS:
Outcomes of severe TBI persist beyond the acute recovery stages. Children experience significantly more difficulties with cognition and emotion at ≥5 years post injury than at three years. This may reflect emerging deficits as they face more complex material at school. Children also experience marginally more emotional difficulties at ≥5 years than at three years. This may reflect developmental maturity making them more aware of their TBI-related limitations. Although it was not significantly different, there was a trend towards lower scores for Mobility and Self-Care Subscales. The MHSCS was a useful parent-report surveillance tool to audit outcome after severe TBI.
Abstract
BACKGROUND:
Idiopathic Hypercalcemia of Infancy (IIH) has been associated with mutations in the vitamin D degrading enzyme CYP24A1. The classic phenotype involves infants who present with hypercalcemia although individuals without an apparent infantile hypercalcemic phase have presented later in life. Typically, at least one vitamin D metabolite is elevated at the time of presentation, and usually CYP24A1 mutations described to date have completely abrogated enzyme activity. The frequency of CYP24A1 mutations and their phenotype is still poorly documented.
OBJECTIVES:
To recruit children from across Canada with presumed IIH to examine their vitamin D metabolite profile using sensitive LC-MS/MS profiling and mutational analyses.
DESIGN/METHODS:
Endocrinologists and nephrologists across Canada were contacted to identify potential cases of hypercalcemia or hypercalciuria without another identifiable etiology. LC-MS/MS was used to determine the ratio of 25(OH)D: 24,25(OH)2D, a marker of CYP24A1 activity. A ratio greater than 80 (ng/mL/ng/mL) is suggestive of CYP24A1 mutations. Mutational analyses were then carried out in all children.
RESULTS:
To date, five children have been recruited and 25 other cases are pending analyses. Three were infants with serum total calcium >2.90 mM and urine calcium: creatinine ratio >95th CI for age, and two were adolescents presenting with nephrocalcinosis or nephrolithiasis. Almost all had elevated 1,25(OH)2D concentrations and suppressed PTH. All vitamin D metabolite ratios were normal except in one girl who presented at nine years of age with an incidental finding of nephrocalcinosis on ultrasound performed for urinary tract infection. Her labs demonstrated intermittent hypercalciuria (peak 6.2 mmol/d), sporadically suppressed PTH, normal serum calcium, and normal vitamin D metabolites in the clinical laboratory. Family history was positive on both sides for nephrolithiasis. Her vitamin D metabolite ratio was 121; the mutational analysis demonstrated a known homozygous mutation E143del.
CONCLUSIONS:
The full phenotype of CYP24A1 mutations is not yet fully described. Likely other gene mutations are associated with IIH. Clinicians need to consider CYP24A1 mutations in the presence of suppressed PTH concentrations and incidental hypercalciuria or nephrocalcionosis.
Abstract
BACKGROUND:
It is well-documented that participation in mock codes improves resident confidence and knowledge in pediatric acute care. While real-life critical pediatric events are extremely rare, mismanagement bears serious consequences, rendering a mock code curriculum an essential part of pediatric residency training. Traditional mock codes, however, involve only a small number of learners within a limited time-frame due to competing clinical and academic demands.
OBJECTIVES:
To determine the impact of an online mock code curriculum on acute care exposure during pediatric residency. In addition, we aim to assess the curriculum’s impact on resident perception of acute care knowledge, awareness of crisis resource management principles, confidence in managing critical events, and competency in relevant RCPSC Objectives of Training.
DESIGN/METHODS:
A tiered longitudinal curriculum was designed. Mock code scenarios were authored by pediatric residents with PICU mentorship. Content was based on applicable RCPSC Objectives of Training addressed in that month’s academic half-day curriculum. Four residents participated in a monthly PICU staff-facilitated interdisciplinary mock code. The authoring resident assisted with the scenario and debrief, thereafter distributing a computer-based module to all residents, comprising a) the scenario in stepwise form, b) targeted RCPSC objectives, and c) key learning points and resources.
RESULTS:
Over a nine-month period, nine modules have been designed and disseminated to all 50 residents. Thirty-six residents have participated in one or more simulated scenarios which, as surrogates of clinical encounters, represents a five-fold increase in pediatric acute care exposure. A total of 92 RCPSC Medical Expert and 38 intrinsic competency objectives encompassing all CanMeds domains have been met to date. Results of a confidence and satisfaction survey are pending.
CONCLUSIONS:
Given that critical events are relatively infrequent in pediatric patients, computer-based modules that are widely disseminated and easily accessible to pediatric residents can increase exposure to acute care issues in a way that is patient-safe. This innovative mock code curriculum effectively targets multiple RCPSC objectives encompassing all CanMeds roles, and may easily be adapted for other areas of medical expertise and residency programs.
Abstract
BACKGROUND:
Breastfeeding provides the ideal nourishment for the infant, yet prevalence rates are low. Understanding the effect of maternal health behaviours on enhancing breastfeeding practice may allow health care practitioners to better provide health behaviour counselling and effectively target vulnerable populations.
OBJECTIVES:
We examined the relationship of maternal diet and breastfeeding practice
DESIGN/METHODS:
We used cross-sectional data on 2594 mothers from the 2009–2010 Ohio CDC Pregnancy Risk Assessment Monitoring System. Multivariable logistic regression was conducted to examine the relationships of maternal diet (fruit, vegetable, and multivitamin intake) with breastfeeding practice (breastfeeding intention, breastfeeding initiation, any breastfeeding at four weeks postpartum, and any breastfeeding at eight weeks postpartum).
RESULTS:
Mothers who ate a diet low in fruits and vegetables were less likely to intend to breastfeed, initiate, or continue breastfeeding to eight weeks after birth, compared with mothers who ate a diet adequate in fruits and vegetables. A diet low in fruits and vegetables (adjusted OR [aOR] 0.22 [95% CI 0.08 to 0.66]) and multivitamin intake (AOR 1.55 [95% CI 1.24 to 1.93]) were independent predictors of any breastfeeding at eight weeks postpartum.
CONCLUSIONS:
Eating a diet low in fruits and vegetables during pregnancy negatively predicts breastfeeding practice, whereas taking multivitamins positively predicts breastfeeding practice.
Abstract
BACKGROUND:
Massive hemorrhages (MH) are life-threatening complications of trauma and obstetrical cases. Expertise and effective communication is key among all team members involved. Collaboration with blood bank technologists (BBT) and hematologists assisting teams with prompt preparation and delivery of blood products further contributes to optimizing care.
OBJECTIVES:
To evaluate communication and expertise when preparing and delivering blood products during MH cases using in situ simulation.
DESIGN/METHODS:
Prospective observational study held at a blood bank (BB) and simlab of a tertiary care facility. Participants were BBTs and hematologists and pediatric emergency/critical care and obstetrical/anesthesia teams submitted to high fidelity (HF) simulated pediatric trauma and post-partum MH scenarios, respectively. BBT were videotaped at the BB and conversations with teams at the simlab were recorded. If hematologists were consulted, the chief BBT questioned them on issues relevant to MH.BBT were evaluated by a blinded trained independent rater using a checklist rating expertise and key communication skills necessary when preparing and delivering blood products to teams involved in MH. Hematologists were rated using a questionnaire exploring their ability to assist and communicate with BBTs and clinicians dealing with choosing blood products or compatibility issues. Means and SDs of scores on checklists and questionnaires were calculated.
RESULTS:
Participants were eight BBT, eight hematologists and 62 healthcare professionals involved in eight interdisciplinary teams (four obstetrics/anaesthesia and four pediatric emergency/critical care). BBT scored on average 78% (61% to 92%) and 76%(62% to 100%) in expertise and communication checklists (trauma and post-partum simulations, respectively). Hematologists rightly refused blood specimens to determine blood type in 57% (four of seven) (discrepant ABO/Rh blood group with previous ABO group results).Their ability to choose or substitute blood products was observed in 71% (five of seven).When challenged by the fact that an incompatible blood product was delivered to the patient, 37.5% (three of eight) asked for phenotype analysis of products already transfused and those being prepared and no one advised teams or of the possibility of a hemolytic transfusion reaction.
CONCLUSIONS:
BBT were considered relatively ready and possess necessary expertise and communication skills to prepare and deliver blood products to teams dealing with MH. For hematologists, knowledge gaps were identified and additional training is mandatory to ensure proficiency when assisting teams with such emergencies. Using in situ simulation at the BB and hematologists in addition to HF interdisciplinary team simulations at a simlab can further add to improving performances of all professionals actively involved in MH crisis situations.
Abstract
BACKGROUND:
It is important for residents to communicate effectively with attending physicians, especially in critical on call situations. In recent years, handover mnemonics have gained attention as a way to improve communication. Although one of the best studied is SBAR (situation, background, assessment and recommendations), few publications have examined the effect of formal SBAR training and usage on resident to staff communication.
OBJECTIVES:
To determine if a structured SBAR teaching session and an SBAR based communication checklist improves resident self-assessment of their ability to communicate in critical situations.
DESIGN/METHODS:
A convenience sample of 22 paediatric residents at the Children’s Hospital of Eastern Ontario was recruited to participate in the study. Participants watched a video of a mock-code scenario and dictated an audio summary of the case, as though they were presenting to an attending physician. After baseline recordings, participants were randomly divided into three groups (stratified by year of training): SBAR teaching and checklist (group 1), SBAR teaching only (group 2), and no teaching or checklist (control group). Teaching consisted of a one-hour didactic session on SBAR. Participants then watched another mock-code scenario and recorded a second summary. After each recording, participants completed self-assessments using Likert-scales.
RESULTS:
Ultimately, there were nine residents in group 1, four residents in group 2 and nine residents in the control group. The year of training was evenly distributed within each group (ranging from year 1 to 3). Of the 13 residents who received SBAR teaching, 92% agreed that it was helpful. All nine residents who used the checklist felt that it was helpful. Residents in group 1 assessed themselves as being more organized in their presentation compared to baseline (P=0.03) which is also significant when compared to the change in the control group (P=0.02). Additionally there was a perceived improvement in their ability to handover all necessary information (P<0.01) but this was not significant when compared to the change in the control group (P=0.7). There was no significant difference in the change from baseline for either category of self-assessment when group 2 and the control group were compared.
CONCLUSIONS:
Formal SBAR teaching and use of an SBAR checklist were helpful in improving resident communication, as indicated by improved resident self-assessment of presentation organization from baseline compared to those with no teaching and no checklist. The effect of teaching alone was difficult to interpret due to a small sample size. Subsequent analyses will include blinded-staff evaluation of the recorded communications for content and organization.
Abstract
BACKGROUND:
Palivizumab is recommended by national and international pediatric advisory committees for the prevention of respiratory syncytial virus (RSV) infection and subsequent related hospitalization in high-risk infants. The CARESS registry tracks palivizumab use and respiratory outcomes in such infants, including those with congenital airway anomalies (CAA).
OBJECTIVES:
The primary objective of this study is to compare hazards for hospitalization for respiratory illness (RIH) and RSV positive infection (RSVH) in CAA infants versus those prophylaxed for other pre-existing medical illnesses (MI) and standard indications (SI).
DESIGN/METHODS:
Infants who received ≥1 dose of palivizumab during the 2005–2013 RSV seasons were recruited from 32 Canadian sites and followed prospectively. The MI group included a spectrum of infants with underlying disorders such as cystic fibrosis, neuromuscular impairments, Down syndrome and immune-compromised individuals. The SI group comprised preterm infants (≤35 weeks gestational age who were <6 months at the start of the RSV season) and those aged <2 years with either chronic lung disease (bronchopulmonary dysplasia) or infants with hemodynamically significant congenital heart disease. Palivizumab utilization and hospitalization outcomes were collected monthly throughout respective seasons. A Cox proportional hazard analysis adjusting for risk factors compared hazard ratios (HR) across prophylaxis indications.
RESULTS:
16,290 infants were enrolled (447 CAA; 2120 MI; 13,723 SI). Infants received an average of 90.5±18.2% of their expected injections, and no significant differences (P<0.05) were seen across groups (F[2, 16268]=2.66; P=0.07). Adjusting for significant (P<0.05) group differences (enrolment age, having siblings, aboriginal origin and multiple birth status) showed CAA infants had a significantly higher hazard of RIH (HR [95% CI]; P value) compared to MI (1.59 [95% C1.03 to 2.44]; P=0.03) and SI (95% C1.85 [95% C1.27 to 2.69]; P=0.001). However, the CAA group had a similar HR for RSVH compared to MI (2.15 [95% C0.75 to 6.21]; P=0.16) and SI (2.28 [95% C0.92 to 5.659]; P=0.08), but other risk factors remained significant (P<0.05).
CONCLUSIONS:
This is the largest report of CAA infants who have received palivizumab world-wide. CAA infants have an increased hazard for RIH compared to MI and SI but appear to have a similar RSVH hazard despite differences in risk factors.
Abstract
BACKGROUND:
Physicians’ attitudes and recommendations directly impact breastfeeding duration. Yet, studies in other parts of the world have shown that physicians lack the skills to offer proper guidance to breastfeeding mothers.
OBJECTIVES:
This study aims to identify gaps in breastfeeding knowledge, confidence, beliefs and attitudes of Canadian physicians, and factors associated with breastfeeding knowledge.
DESIGN/METHODS:
A breastfeeding questionnaire was developed and piloted for validity. These questionnaires were sent to 1429 pediatricians (PED) and 1329 family physicians (FP), for a target sample size of 385 per group, and to final-year pediatric and family medicine residents (PR and FMR). Multiple linear regression was used to identify factors independently associated with knowledge score.
RESULTS:
The analysis included 397 PED, 322 FP, 17 PR and 44 FMR who completed the questionnaire. Mean overall correct knowledge score was 67.8% for PED, 64.3% for FP, 72.7% for PR and 66.8% for FMR. 285 PED (74.2%), 228 FP (73.1%), seven PR (41.2%) and 21 FMR (53.8%) felt confident with their breastfeeding counseling skills, but few PED and FP (5.1% and 11.3%) routinely observed breastfeeding in mother-infant pairs. Most participants (72.1%) felt that residency had prepared them poorly or somewhat poorly to support breastfeeding mothers. Independent predictors of breastfeeding knowledge included female gender, >50% of one’s practice under one year of age, breastfeeding one’s own child, self-directed learning and confidence teaching mothers about breastfeeding.
CONCLUSIONS:
Breastfeeding knowledge, confidence, beliefs and attitudes are suboptimal among Canadian physicians. Confidence and knowledge are closely intertwined, and currently develop through learning methods other than residency training. This study identified specific areas of concerns in physicians’ breastfeeding knowledge, confidence, beliefs and attitudes, allowing for the development of targeted educational tools that will help physicians better support breastfeeding.
Abstract
BACKGROUND:
Physicians’ attitudes and recommendations directly impact breastfeeding duration. Yet, Canadian primary care physicians are ill-equipped to support breastfeeding mothers as their confidence, attitudes and knowledge are known to be suboptimal.
OBJECTIVES:
This study aimed to develop, deliver, evaluate and refine a combination of continuing professional development (CPD) activities targeting specific gaps uncovered on a recent breastfeeding needs assessment of Canadian physicians, with the ultimate goal of encouraging study participants to integrate new skills and knowledge in their clinical practice.
DESIGN/METHODS:
We developed and delivered an interactive 90-minute workshop to facilitate physicians’ ability to support patients’ breastfeeding practices. The workshops were held at the Canadian Pediatric Society Annual Meeting in June 2012 in London, Ontario, at a continuing medical education event at the Children’s Hospital of Eastern Ontario in November 2012, and at the Montfort Hospital in February 2013. Communication tools were distributed to improve information retention. Phone outreach was performed four to eight weeks post workshop to reinforce take-home messages from the workshop, gather information on the obstacles and challenges to implementing the various breastfeeding support practices provided at the workshop and to gather information regarding physicians’ current perceptions and practices. Participation, participants’ satisfaction with each element of the CPD activities and participants’ learning were also tracked through the use of questionnaires and the follow-up phone outreach. We aimed to recruit 30 to 40 physicians.
RESULTS:
In total, seven physicians agreed to participate in the study. Workshop participation increased these participants’ confidence levels in breastfeeding counseling skills (ie, latch evaluation, sore nipple complaints, milk transfer evaluation), improved their knowledge, and was associated with a desire to change their clinical practice. The workshop was overall rated as relevant, interesting, effective, and helpful.
CONCLUSIONS:
Physician recruitment was found to be much more difficult than anticipated, and a large selection bias was inevitable as only physicians with a keen interest in learning about breastfeeding participated in the study. However, our participants rated the intervention very positively. Given the difficulty in recruitment, a more feasible approach needs to be adapted and evaluated. In future, the intervention will be targeted at residency level.
Abstract
BACKGROUND:
Procedural competence is defined as “the ability to perform a procedure independently, without supervision, with a high likelihood of successful completion” (Gaies MG et al. Pediatrics. 2007;120(4):715–22). The Royal College of Physicians and Surgeons of Canada has outlined 19 procedural skills for Neonatal-Perinatal Medicine (NPM) trainees to demonstrate competence by the end of a two-year program. It is unclear how Canadian NPM training programs prepare their residents to acquire these procedural skills. There is no formal way to evaluate which competencies require increased training or exposure.
OBJECTIVES:
To examine the self-reported attitudes and procedural skill competencies of Neonatal Perinatal Medicine trainees across Canada for 19 procedural skills listed by the Royal College for NPM training.
DESIGN/METHODS:
A cross-sectional confidential electronic survey was sent to first and second year NPM trainees in 13 Canadian NPM programs (2012–2013). A five-point Likert scale was used to rate perceived importance (1 = not important to 5 = very important) and competence (1 = not competent to 5 = neonatologist) of each skill before and during their NPM training. Demographic and training data was collected. Two-tailed paired t tests (P<0.05) were used to analyze pre versus current training “competence” for each skill. Only anonymous aggregate data was reported.
RESULTS:
A total of 47 trainees (68%) completed the survey of which 36 consenting respondents with >6 months Canadian NPM training were analyzed. Only 25% of trainees were FRCPC exam eligible (CMG) (25%), with majority of respondents 12 to 24 months (47.3%) into their training. There were larger changes in pre versus current training perceived competencies in CMG compared to international medical graduates. Most CMG’s procedural skills reached competence and improved by >1 during training, with the exception of suprapubic (mean difference 0.55), urinary catheterization (0.67), pericardiocentesis (0.45), and paracentesis (1.00). Pericardiocentesis did not meet competence (1.9/5) despite type and duration of training. Skills performed frequently in NICU (compared to pediatric residencies): umbilical lines (1.3), intubation (1.2), chest tubes (1.7), PICC lines (1.7), and arterial lines (1.5) had a high level of change and competence. Despite training, some NICU procedures rated poorly (x/5) in self-rated competence including paracentesis (2.4), PICC line insertion (3.1), suprapubic tap (2.2) and exchange transfusion (3.1).
CONCLUSIONS:
Observed skills most frequently done by trainees have the greatest change in competence during training for CMG in NPM. Some necessary procedural skills may require changes to instruction methods and these results could help guide curricular improvement.
Abstract
BACKGROUND:
Intravenous Immunogloblin (IVIG) is frequently used in the treatment of immune-mediated disorders such as immune thrombocytopenia, inflammatory diseases, and as replacement therapy in immune deficiencies. It is prepared from plasma pooled from thousands of healthy donors and has been used since 1952. It is generally considered safe and secure with acceptable adverse events including headaches, fever, myalgia, urticaria, and nausea. However, rare serious adverse events (SAE) can occur. Over the last decade, IVIG use has dramatically increased across the world.
OBJECTIVES:
Following one case of IVIG-SAE, we reviewed incidence of such SAE through reports of Quebec Hemovigilance System (QHS).
DESIGN/METHODS:
A 16-year-old female presented for severe thrombocytopenia. Given her age and menorrhagia, we choose to give platelet-enhancing agents. She had recurrent episodes of severe thrombocytopenia. First IVIG infusion was followed by severe aseptic meningitis. Given new episode of thrombocytopenia, she received fractionated IVIG infusion which again resulted in normalisation of platelet count, but was complicated within 10 days by hemiparesis and seizures, associated with sinus vein thrombosis. She eventually had a good outcome without minimal sequelae.
RESULTS:
Through QHS, we found four other reports of thrombotic events possibly related to IVIG therapy, all being adults. Based upon most recent estimates, this corresponded to 0.6% to 1.6% of all reported IVIG-related SAE in QHS. Over a five year period (2005 to 2010), there have been 112 CNS-related events including headaches or aseptic meningitis. The incidence of all reported events further ranged between 1:6683 and 1:9580 events per gram of IVIG given. Since the first report of IVIG-associated thrombosis in 1986, more than one hundred cases have been reported, with only six paediatric cases. Patient’s predispositions, such as advanced age, previous thrombotic events, and hypercoagulable state were found to be associated with higher risk of thrombosis. Rapid infusion, high dosage and concentration, have also been implicated. The thrombotic effects of IVIG may be due to contamination with activated coagulation factor XI, arterial vasospasm or increased blood viscosity. ITP has itself been paradoxically recognized as a possible prothrombotic condition. The presence of large platelets with enhanced endothelial adherence, as well as complement activation may partly explain such enhanced thrombotic propensity.
CONCLUSIONS:
Clinicians should have a high suspicion for intracranial complications, including thrombosis, in patients receiving IVIG and history of recurrent headache. IVIG related complications should be thoroughly investigated and properly reported, in order to improve hemovigilance system and study of such rare serious adverse events.
Abstract
BACKGROUND:
In recent years there has been increasing emphasis on critical appraisal skills in medical training. This is reflected in both the requirements of the Royal College of Physicians and Surgeons of Canada (RCPSC) and the Accreditation Council for Graduate Medical Education (ACGME). However, little information exists to guide educators on developing relevant competencies. Research has shown that the majority of residents lack sufficient knowledge to understand data analysis in much of the published literature.
OBJECTIVES:
We sought to determine which statistical concepts are most frequently reported in pediatric journals, in order to inform resident education in critical appraisal.
DESIGN/METHODS:
We conducted a review of articles in seven pediatric journals previously reported to contain best evidence for clinical practice: (1) Archives of Diseases in Childhood, (2) British Medical Journal (BMJ), (3) Journal of the American Medical Association (JAMA), (4) Journal of Pediatrics, (5) Lancet, (6) New England Journal of Medicine, and (7) Pediatrics. For each of these publications, a single monthly issue was included (June 2009). Review of two additional months of publication is in progress. Original research articles enrolling at least one patient <18 years of age were considered eligible. Two independent reviewers abstracted relevant statistical tests and terms; disagreements were resolved by consensus. Descriptive statistics were used in determining the most common statistical tests in the relevant pediatric literature. We then determined the proportion of literature accessible to readers who understand the three most commonly reported statistical tests/procedures.
RESULTS:
A total of 102 articles met inclusion criteria. Of these, the majority were observational in design (n=88 [86%]). Fourteen studies (14%) did not use any inferential statistics, while the remainder employed at least one statistical test. The most commonly reported were the chi square test (n=37 [36%]), logistic regression (n=37 [36%]) and the t test (n=27 [26%]). A reader familiar with these three commonly reported tests would be able to understand 30% of the literature. ANOVA, Fisher’s exact test, tests of correlation and linear regression were also used in more than 10% of articles.
CONCLUSIONS:
These results identify which statistical tests are most commonly used in the pediatric medical literature and therefore which tests are the most important for residents to understand. Such information could be used to 1) promote competency in critical appraisal, and 2) meet RCPSC and ACGME education guidelines.
Abstract
BACKGROUND:
The diagnosis and management of immune thrombocytopoenia (ITP) of childhood is controversial amongst paediatricians. ITP is the most common bleeding disorder of childhood and is characterized by an isolated low platelet count (<100×109/L). The disorder is usually self-limiting – nearly 80% of childhood ITP spontaneously resolve within a year. However, many patients receive therapy to avoid the rare incidence of clinically significant bleeding. Published guidelines have differed in recommendations for diagnosis and management.
OBJECTIVES:
This study aimed to explore approaches in managing acute ITP at the IWK Health Centre and across the Maritimes Provinces.
DESIGN/METHODS:
A literature review, retrospective chart review of ITP patients followed at the IWK since January 1, 1990, and an online survey of paediatricians’ practices were conducted.
RESULTS:
Published guidelines are converging and encourage paediatricians to treat based on symptoms not absolute platelet counts. Chart review showed that 99 of 144 patients received at least one course of treatment – 60 of 99 with IVIg and 37 of 99 with corticosteroids. The decision to treat 66 of 99 was on platelet count alone. Bone marrow examinations, recommended in an atypical presentation or prolonged course of disease, were performed in 54 patients. IWK paediatricians relied on clinical experience in 135 cases and consultation with colleagues in 36 cases. Twenty-four Maritime paediatricians who responded to our online questionnaire manage ITP. 17completed the survey. Nineteen of 24 were uncertain of recommended diagnostic platelet counts for ITP. Two of 24 reported using published resources to complete the survey. Thirteen of 21 paediatricians reported they would use published guidelines to guide management in provided case scenarios and 17 of 21 would consult colleagues.
CONCLUSIONS:
Actual management of acute ITP differs from published guidelines: patients are treated more for platelet counts and may be over-investigated and over-treated. Lack of adequate documentation may bias results. Maritime paediatricians prefer managing patients collaboratively, suggesting that further education would benefit practice. A prospective pan-Canada survey would explore this further.
Abstract
BACKGROUND:
Neuroblastoma (NBL) is the most common extracranial solid tumour in children, and is responsible for more deaths than any other type of pediatric cancer. Approximately 50% NBL are metastatic at diagnosis and 25% to 35% of all patients will relapse, for which there are generally no curative therapies. Surveillance to detect recurrent disease in NBL patients includes clinical assessment, measurement of urinary catecholamines (UCats), cross-sectional imaging, and I123-meta-idodobenzylguanidine scans (MIBG). Surveillance is costly and results in high cumulative doses of radiation. We hypothesize that relapses may be readily detected with investigations that result in lower doses of cumulative radiation.
OBJECTIVES:
We sought to determine 1) how relapses were detected (symptoms, physical exam, UCats, MIBG, chest film (CXR), ultrasound (US), CT, and/or MRI) and 2) whether surveillance investigations can identify relapses without using routine CT or MRIs.
DESIGN/METHODS:
We reviewed all cases of relapsed NBL at our hospital, a tertiary paediatric centre, between January 2000 and December 2011.
RESULTS:
183 children with NBL were treated during the study period. 27% (50 of 183) relapsed, of which 84% (42 of 50) had metastatic disease at diagnosis. Median time from diagnosis to relapse was 1.2 years. 64% (32 of 50) of relapses were detected by surveillance investigations and 36% (18 of 50) due to new symptoms. A median number of nine CTs, four MIBGs, and one MRI were completed between time of diagnosis and relapse. The median effective radiation dose was 99.7 mSv, 84% of which was from CTs and 14.4% from MIBGs. This effective radiation dose was estimated to carry an overall excess cancer risk of >2%. 74% (37 of 50) had new lesions visible by MIBG scan at relapse. Of the remaining 13 relapses, five were detected by elevated UCats, two by bone scan, one by US, and another by CXR. Only four relapses were solely detected by CT and none by MRI: two by routine CT and had no concurrent MIBG, and two by CT ordered due to new symptomatology.
CONCLUSIONS:
Relapsed disease was detected in almost all patients by MIBG scan, UCats, CXR, or US alone. Our results support reduced use of CT imaging in post-therapy surveillance, thereby reducing cumulative radiation doses as the radiation exposure from an MIBG scan is approximately 50% of a CT scan. The intensity of post-therapy surveillance may also be guided by initial disease risk group.
Abstract
BACKGROUND:
Family centered rounds (FCR) are the most common rounding format in North American pediatric hospitals. If conducted with a clear understanding of the settings, goals, and teaching strategies, FCR permit explicit teaching of CanMEDS competencies. If not done effectively, learners and teachers run the risk of being led room to room with suboptimal participation, minimal educational value and very poor efficiency.
OBJECTIVES:
The purpose of this study was to describe the dimensions of FCR within the Canadian CanMEDS context in order to develop recommendations for effective teaching and learning earning in thi this e environment.
DESIGN/METHODS:
Data were collected from focus group meetings of pediatric residents and attending paediatricians on the clinical teaching unit at a tertiary care academic children’s hospital. Data were analyzed using grounded theory methodology.
RESULTS:
Rounds were described along a spectrum from successful and highly educational to unsuccessful and of low educational value. Three dimensions impacted the rounds experience; the environment, education, and competing priorities. The physical aspects of the hospital learning environment and the fact that the environment was both family centred and team based impacted educational success. Both the content and the process (or how teaching was done) affected the experience. Last, preceptors and senior residents faced competing priorities between patient care, learners (and the range of learners) and the need to maximize efficiency and patient numbers. Attending paediatrician and resident perceptions of educational effectiveness were influenced by how well these dimensions were managed. The ability to manage the rounds was the core variable for successful rounds being led by individuals who were able to maximize predictability in the environment and minimize learner vulnerability. Specific strategies for leading educationally effective FCR were also discussed.
CONCLUSIONS:
The CanMEDS Manager Role was central to creating an educationally effective FCR experience and this is an ideal environment for the teaching and evaluation of this core competency. A framework and tool for leading successful FCR based on the CanMEDS Manager role was developed based on study findings. The importance of the Manager Role needs to be made explicit for trainees and attending staff.
Abstract
BACKGROUND:
Training in ambulatory care and continuity of care has become an integral part of residency programs. Continuity clinics attempt to address these challenging aspects of medical education. Our centre has a long-standing paediatric residents’ continuity clinic (PRCC) that had never been formally evaluated.
OBJECTIVES:
To assess resident satisfaction of their continuity clinic experience, before and after evidence-based improvements were made.
DESIGN/METHODS:
Cross-sectional surveys were conducted at a single paediatric training site in the academic years of 2012–2013 and 2013–2014 using online questionnaires. Our ethics committee approved this study.
RESULTS:
Most eligible residents participated in both questionnaires, of which around 60% had a high probability of becoming a general paediatrician. Residents had one monthly clinic; half the residents would increase this frequency. The majority had a mean of three to four appointments per session and in general they thought this was just enough. Before the study, 37% of residents were using standardised general follow-up tools, and 7% were using developmental screening tools. These figures only slightly improved at the time of the second questionnaire (48% and 8%). This is in the process of being formally addressed. Complex patients were perceived as being a difficult population to attend to within the settings of the PRCC, yet more than half the residents (55%) wished to see a greater number of complex patients. To attempt to facilitate this, PRCC patients became eligible to care coordination in our medical home program. Perception of teaching seemed to greatly improve during the study, becoming more consistent amongst preceptors. Teachers were generally perceived as being more enthusiastic and better acquainted with the resident following changes in the clinic’s schedule. Evaluation was drastically improved; at the beginning of the study, one resident out of two had never been evaluated and 80% had never experienced direct observation of their ambulatory performance. In 2013–2014, the majority of residents had been evaluated (84%) and directly observed (56%). General resident satisfaction was also significantly enhanced; no resident said to be unsatisfied with the experience in the second questionnaire as opposed to 26% in the first. The overwhelming majority of residents agree that the continuity clinic is important in their training and for their future career.
CONCLUSIONS:
Residents highly value the continuity clinic educational experience; satisfaction markedly increased after improvements were made. These findings reiterate the importance of the continuity clinic model and the need for constant appraisal of this fundamental teaching opportunity.
Abstract
BACKGROUND:
The adolescent interview is a challenging task that requires strong communication skills developed through practice and training
OBJECTIVES:
To explore whether receiving structured feedback from an adolescent and mother Standardized Patient (SP) pair improves medical students’ confidence regarding interviewing adolescents. Secondly, to identify self-perceived learning needs in the adolescent interview.
DESIGN/METHODS:
Participants were medical students undergoing their core Pediatric Clerkship Rotation. Students were randomized into two groups and asked to rate their confidence levels involving basic communication components of adolescent interviewing on a 13-item structured questionnaire. Following an interview with an adolescent SP and mother pair, one group received structured feedback (F1) on their performance and a second group received no structured feedback (F0). After the SP pair encounter, students were asked to rate their confidence levels a second time using the 13-item questionnaire. Students also ranked self-perceived learning needs in six components of adolescent medicine.
RESULTS:
Students who received structured feedback (n=25) on their adolescent interviewing skills from an SP pair showed an increase in mean confidence scores on all the 13-item structured questions. Mann-Whitney analysis comparing post-intervention confidence scores between the feedback, (F1) and no feedback (F0) groups showed that the F1 group (Mdn=27.58) had a significantly higher mean confidence score on Question 3 ‘Physical Exam’ than did the F0 group (Mdn=17.28), U=135.50, z=−2.97, P=0.001. The F1 group (Mdn=26.14) also had a significantly higher mean confidence score on Question 6 ‘Sexual Issues’ than the F0 group (Mdn=19.08), U=171.50, z=−1.93; P=0.023. The F1 group demonstrated a trend towards increased mean confidence scores post-intervention on questions that were directly referenced by the structured feedback tool used by the SP pair. The six ranked self-perceived learning needs indicated students felt least prepared for ‘Sexuality Questioning’ and most prepared for ‘Physical Examination’.
CONCLUSIONS:
An SP interview followed by structured feedback from the SP pair improved medical students’ confidence level in their adolescent interviewing skills. This study also highlighted important areas of the adolescent interview that required further training, which have since been incorporated into the undergraduate medical training at our institute. Lastly, structured feedback was shown to be a useful tool in the adolescent interview and was further incorporated into our curriculum.
Abstract
BACKGROUND:
There is emerging evidence that child temperament is associated with sedentary behaviours and obesity in young children, but physical activity (PA) has not been evaluated. Parent-reported outdoor free play correlates with directly measured PA in young children.
OBJECTIVES:
The primary objective is to determine if Negative Affectivity, a construct of child temperament, is associated with outdoor free play in young children. Secondary objectives are to determine if the constructs of Surgency and Effortful Control are each associated with outdoor free play.
DESIGN/METHODS:
Subjects were children <6 years old (n=3784) recruited through TARGet Kids! primary care-based research network. Child temperament was measured by the Children’s Behaviour Questionnaire. The primary exposure was Negative Affectivity. The outcome was parent-reported daily outdoor free play (minutes). A linear regression model was performed, adjusting for covariates of age, sex, ethnicity, income, maternal employment, daycare use, presence of siblings, and presence of family rules. Age, sex and family rules were identified a priori as potential interactions, and stratified analysis was planned. Analysis was repeated with Effortful Control and Surgency as exposures.
RESULTS:
On average, children participated in outdoor free play for 58 min/day. Outdoor free play was significantly associated with Negative Affectivity (P<0.01) and Surgency (P=0.01), but not Effortful Control (P=0.23). Multivariate analysis including interactions revealed that sex had a significant moderating effect; adjusting for covariates, boys, but not girls, with higher Negative Affectivity had reduced outdoor free play. For boys at the lowest and highest quartile of outdoor free play time, with each one-point increase in Negative Affectivity, free play was reduced by 3.5 min/day (95% CI 1.8 to 5.2 min/day), and 6.2 min/day (95% CI 3.1 to 9.4 min/day), respectively. For Surgency, age had a significant moderating effect. Adjusting for covariates, children older than two years with higher Surgency had increased outdoor free play; for the lowest and highest quartile of free play, with each 1-point increase in Surgency, free play increased by 3.1 min/day (95% CI 0.9 to 5.3 min/day), and 4.5 min/day (95% CI 1.3 to 7.8 min/day), respectively. There was no association found for children less than two years old.
CONCLUSIONS:
Negative Affectivity and Surgency are temperaments shown to be associated with outdoor free play in young children. This information may help in the development of effective interventions to promote PA in this age group.
Abstract
BACKGROUND:
Literature on high reliability organizations suggests that structured communication can reduce errors. The I-PASS Handoff Bundle aims to improve resident handoff and consists of teamwork training, structured verbal communication using a mnemonic, and an electronic written handoff tool. The program was implemented as part of a nine-site study. This qualitative study examines the implementation of structured handoff in the context of residency training programmes.
OBJECTIVES:
This study examined to what extent I-PASS was adopted amongst residents, what factors facilitate and impede adoption, and in particular the impact of social factors.
DESIGN/METHODS:
Focus groups were conducted with residents (n=54) at eight of nine IPASS sites. The data were analysed using grounded theory techniques to generate insight into how adoption of structured communication could be facilitated in health care.
RESULTS:
The results were very consistent across sites, and resident perspectives fell into four main themes.
Residents expect communication to be efficient. Time is universally regarded as a scarce resource and it is expected that communication should cover only the information necessary for on-going quality patient care. The perception that the I-PASS mnemonic requires that the same information be covered regardless of the professional’s level or knowledge of the patient and for all patients regardless of complexity was seen as violating this norm.
Residents expect communication to respect professional competence. The standardized nature of the information communicated to colleagues can be seen as insensitive to the requirements of residents at different stages of professional competence. Junior residents were more receptive to comprehensive information while the same information was felt redundant by senior residents.
Residents expect allowance for professional judgment and autonomy. The standardized format of IPASS communication, particularly the Synthesis by Receiver step (read back) was seen as limiting professionals’ right to exercise judgment in communication.
Residents expect informal communication among peers: The standardized format of IPASS was seen as more suited to demonstrating skill to a superior rather than for use among colleagues of the same hierarchical level.
CONCLUSIONS:
These data must be interpreted in the context of residency training. Residents who have varying levels of professional identity formation may vary in their ability to adopt new structured communication practices. Acknowledgement of these norms in the training and ongoing reinforcement phases could lead to more positive attitudes and greater receptivity to ongoing efforts to improve communication, which will be required to bring about transformative change.
Abstract
BACKGROUND:
Rotavirus (RV) is the most common vaccine-preventable cause of gastroenteritis (GE) in children. Currently, RV vaccination of infants in the NICU is not recommended. Infants in the NICU are however at very high risk of complications related to RVGE and a proportion will exceed age-eligibility for the first vaccine dose while admitted. RV vaccination was implemented in 2011 at a tertiary care NICU in response to this problem.
OBJECTIVES:
We aimed to describe the safety and feasibility of a NICU-based vaccination program against RV.
DESIGN/METHODS:
The RV vaccination program was implemented in July 2011. Hospitalized infants in a tertiary care NICU who received ≥1 dose of the RV5 vaccine were included. Of 62 infants vaccinated, 36 charts have been reviewed so far. Healthcare-associated (HA) RV cases from April 2009 to March 2013 have been identified through prospective HA infections surveillance and reviewed.
RESULTS:
Our NICU has an annual average of 393 admissions per year and 7229 patient-days during the study period. Since July 2011, 8.5% of NICU admissions were vaccinated against rotavirus. Twenty-two infants (61%) were males, the vaccinated population had a median gestation age of 33 weeks (IQR 28 6/7 to 38 3/7), a median birth weight of 1740 g (IQR 980 g to 2989 g) and a median length of stay of 79 days (IQR 55 to 110 days). The three main primary diagnostic categories of vaccinated infants were gastrointestinal (n=12), respiratory tract (n=7), and genetic (n=6). Thirty-six first doses, 11 second doses and eight third doses were administered at a median age of 61, 93 and 128 days respectively. Comparing each infant’s median feeds in the seven days post-vaccine to their pre-vaccine feeds, there was a median change of +3.5 mL. The incidence rate of HA-RVGE prior to program implementation was 4.86 (95% CI 1.95 to 10) per 10,000 patient-days; the incidence rate in the intervention period (July 2011 to March 2013) has been 0 (95% CI 0 to 2.54) per 10,000 patient-days. The incidence rate ratio was 0 (95% CI 0 to 0.69).
CONCLUSIONS:
There was no case of HA-RVGE after the implementation of our RV vaccination program in our NICU. This study supports the safety and feasibility of a RV vaccination program in NICUs that aims to protect patients with the highest risk of RVGE complications once discharged.
Abstract
BACKGROUND:
Simulation and debriefing are increasingly used for both technical and non-technical skills training. Recent national and international guidelines recommend the use of simulation and video-debriefing for neonatal resuscitation training. The use of simulation and video-debriefing create significant challenges for educators in the delivery of standardized programs such as the neonatal resuscitation program (NRP). The effectiveness of this educational strategy remains unclear.
OBJECTIVES:
To examine the effectiveness of video- debriefing on the performance and beliefs of inter-professional teams following simulated neonatal training sessions.
DESIGN/METHODS:
This REB-approved prospective study examined the role of video-debriefing in improving neonatal resuscitation performance amongst neonatal teams in both technical and non-technical skills. Teams included one of: respiratory therapists (RT), neonatal nurse and senior paediatric residents. Two standardized simulated neonatal resuscitation scenarios were offered using a high-fidelity simulation environment. Neonatal teams were randomly allocated to receive video-debriefing or no debriefing after the initial simulated neonatal resuscitation and invited for a subsequent session four to eight weeks later. Participants were assessed for NRP team performance by reviewers blinded to the intervention. Attitudes and beliefs of participants were collected regarding the use of debriefing for resuscitation and team behavioural skills.
RESULTS:
A total of 25 study teams were recruited comprising 75 participants. Seventeen groups have returned to complete the study. The majority of participants (53%) had attended less than five simulations in the past. Of those who had previously attended, the vast majority had never been exposed to video-debriefing as part of their education. There were no significant differences in NRP performance (time to intubation and NRP score) between groups. In general, adherence to NRP guidelines was poor. Virtually all participants agreed that both the simulation and debriefing components resulted in improved learning in both technical and team behavioural skills. A greater number of participants strongly agreed that the simulation session assisted their acquisition of team behavioural skills (P=0.006).
CONCLUSIONS:
In this study, the use of video-debriefing Inter-professional teams of simulated neonatal resuscitations did not result in significant improvement in subsequent simulated NRP performance. Team members believed the use of both simulation and debriefing resulted in enhanced acquisition of team behavioural skills in particular. The role of inter-professional team training using video-debriefing in this setting requires further study.
Abstract
BACKGROUND:
The main I-PASS Study assesses the effectiveness of a Handoff Bundle (team training, verbal mnemonic, and electronic written handoff tool) at nine residency programs using quantitative data on patient safety outcomes as well as efficiency and provider satisfaction.
OBJECTIVES:
The objective of this ancillary qualitative study was to describe in detail the resident experience of I-PASS implementation, in general and with respect to the individual components, in order to inform future refinements and implementation strategies.
DESIGN/METHODS:
Focus groups with residents (n=54); and semi-structured interviews with faculty (n=28) and other personnel (n=10) were conducted at eight of nine I-PASS sites. A structured codebook was developed to facilitate descriptive coding of transcripts, and data were synthesized and summarized using content analysis. Triangulation was employed by comparing findings across data sources.
RESULTS:
Residents generally accept I-PASS to be a ‘gold standard’ form of handoff and value learning a structured approach. Junior residents and some senior residents feel more secure using a structured format and most recognize that the program enhances handoff quality and patient safety. Efficiency was the most common factor cited when residents expressed concern about I-PASS. They regard it as neither necessary nor feasible to follow I-PASS for every patient and situation. Across all sites, residents report adhering to I-PASS when observed, but adhering selectively in usual practice. Residents were more likely to adhere with complex patients, unfamiliar teams, and evening vs. morning handoff. They also report using elements of the I-PASS mnemonic variably, with “synthesis by receiver” rarely used outside the context of observation. Anything perceived to lengthen handoff was unwelcome. Most residents value the computerized written handoff tool, but at sites with significant tool usability problems, dissatisfaction extended to the whole I-PASS program. The degree to which resident feedback was sought and acted upon moderated this.
Perceptions of the faculty role varied. Residents generally understood that faculty have different handoff needs and practices, so did not perceive faculty as hypocritical if they did not adhere to I-PASS themselves. The experiences of observation and feedback were mixed. Residents reported variation in faculty feedback styles; some residents found it constructive while others found it ‘nitpicky’.
CONCLUSIONS:
Residents felt that the I-PASS program improved safety, but had concerns about efficiency. Optimizing computerized handoff tools, efficiency of verbal handoffs, and feedback to residents will be important in future refinements and implementation efforts.
Abstract
BACKGROUND:
Increased physical activity (PA) in early childhood is associated with improved measures of body composition, motor skill, cognitive development and cardiometabolic health indicators. There are very few studies describing objectively measures of PA in very young children using accelerometry.
OBJECTIVES:
To describe the objectively measured PA levels of infants, toddlers, and preschoolers and assess their compliance with the recently published Canadian physical activity guidelines for this age group.
DESIGN/METHODS:
Children aged four months to five years (n=54) recruited through a primary care practice based research network in Canada wore Actical accelerometers for seven consecutive days. Data were collected in two-second epochs and participants with four or more valid days were included in the analysis. Moderate to vigorous physical activity (MVPA), light physical activity (LPA), and sedentary activity (SA) were calculated using published cut-points for preschoolers. The mean minutes per day (min/d) of MVPA, LPA, and SA were reported by age group (<18 months, and ≥18 months) and sex.
RESULTS:
Children 18 months of age and older (n=31) accumulated a mean (95% CI) of 35 min/day (26 to 45 min/day) of MVPA, 208 min/day (194 to 221 min/day) of LPA, and 390 min/day (370 to 410 min/day) of SA. Children under 18 months (n=23) accumulated a mean (95% CI) of 4 min/day (3 to 6 min/day) of MVPA, 94 min/day (71 to 116 min/day) of LPA and 452 min/day (426 to 477 min/day) of SA. Ninety-two percent of children 18 months to four years of age (n=26) and 17 percent of children under 18 months met the Canadian PA guidelines for children aged 0 to 4 of 180 min of total daily PA. There were no significant differences in boys compared to girls in MVPA: 20 (9 to 31) vs. 24 (14 to 33); P=0.60, LPA: 152 (120 to 183) vs. 165 (139 to 191); P=0.50, or SA: 414 (391 to 437) vs. 418 (391 to 445); P=0.85.
CONCLUSIONS:
Children over 18 months seem to be meeting Canadian PA guidelines. While children under 18 months appeared relatively inactive, further research is necessary to validate accelerometer-based physical activity measurement and cut-points in this age group.
Abstract
BACKGROUND:
Suboptimal lifestyle habits may lead to childhood overweight and obesity. Promotion of healthy active living (HAL) is an important part of clinical practice. To promote healthy lifestyle in youth, we created a resident-led HAL educational program (including a HAL counselling intervention) at the Montreal Children’s Hospital.
OBJECTIVES:
To determine the prevalence of optimal health habits in children followed in our Pediatric Residents Continuity Clinic (RCC);
To examine the effect of our HAL counselling intervention on the health habits of these children.
DESIGN/METHODS:
This prospective cohort included five to 16 year-old children. Our HAL educational program included 1) didactic teaching sessions on childhood obesity screening and management incorporated within the residents teaching curriculum; and 2) creation of HAL counselling tools (brochures, pamphlets, and healthy habits prescription). Pediatric residents implemented the HAL counseling intervention to patients/families using the 5,2,1,0 guidelines (four daily goals: five portions of fruits/vegetables; <2 h screen time; >1 hr physical activity, zero sugar-sweetened beverages); and HAL counselling tools. Recruited patients and families completed a questionnaire reporting their health habits at baseline, six months and one year following the intervention.
RESULTS:
We recruited 81 patients (9.3±3.1 years old; 48% females). 20% of our cohort was overweight or obese. 19% reported optimal healthy habits (i.e., met all four goals). There was an increase in the proportion of children who met three or four goals following our intervention (49% vs 64% at follow-up), P=0.035. Among overweight/obese children, the improvement was from 33% at baseline to 56% at 12 months follow-up; in non-obese children, 51% to 63%. Specifically, changes for each met goal by category from baseline compared to 12 months were: five portions of fruits/vegetables, 32% vs 49%; <2 h screen time, 58% vs 69%; >1 h physical activity, 48% vs 67%; no sugar-sweetened beverages, 44% vs 58% (P value for each goal was non-significant) The mean activity level increased by 18 min/day (75.5±53.2 vs 93.6±65.2 at follow-up), and sleep duration increased by 25 min (10.0±1.4 h vs 10.4±1.2 h), but neither reached statistical significance (P=0.074 and 0.060, respectively).
CONCLUSIONS:
We were able to show for the first time that using a HAL counselling tool in a primary clinical care setting led to a significant increase in the proportion of children meeting 5,2,1,0 guidelines after the intervention, as well as clinically important increases in physical activity level and sleep duration. Future studies are needed to validate our findings.
Abstract
BACKGROUND:
Disasters can have a significant impact on the population. Children are particularly vulnerable due to their anatomical, physiological, developmental and psychological characteristics. Disaster preparedness must include consideration for the needs of pediatric populations. Training for the practical aspects of disaster medicine is a difficult task, simulation being the traditional method for these rare, high impact events.
OBJECTIVES:
To assess the effect of an experiential learning experience, on inter professional pediatric health care providers’ disaster preparedness skills and confidence.
DESIGN/METHODS:
In 2012, the regional health agency launched a project in collaboration with public health, first responders, municipal police and public transit system, the Canadian Armed Forces and our level 1 pediatric trauma center as the first receiver site for pediatric victims. This large-scale unannounced in-situ, real-time, mixed-modality, pediatric disaster simulation included 43 simulated patients (high/medium/low fidelity simulators and standardized patients). The hospital care teams included a variety of inter professional participants. Since this group of learners had never been exposed to such an in- situ experiential learning experience, we assessed its educational value and effects. Ninety-three participants (from most medical and paramedical services) completed a self-assessment survey immediately following the simulation (with a retrospective pre-component to assess perceived change in skills and abilities) to determine perceived acquisition of knowledge and confidence.
RESULTS:
Participants’ ratings of skills, abilities and confidence significantly increased following participation in this simulation for both medical items (n=53; F(1, 642)=44.1; P<0.0001), and non-medical items (n=83; F(1, 228)=29.7; P<0.0001), consistently across participant groups. Some target items were (standard deviations in parentheses): “Differentiate conventional triage from disaster triage” (pre = 3.91/6 (1.7), post = 4.8 (1.3), “Prioritize resources- maximize survival versus individual outcome” (pre = 3.64/6 (1.7), post = 4.40/6 (1.5), “Feel confident in own ability to respond to disaster” (pre = 3.58/6 (1.5) post = 4.94/6 (1.1), “Feel confident in hospital’s ability to respond to disaster” (pre = 4.29/6 (1.3), post = 5.02 (0.9). Participants felt the pediatric disaster simulation day was valuable to their learning (5.68/6).
CONCLUSIONS:
The inter professional members of the pediatric disaster first receiver teams, believed that this simulation experience improved their ability to manage patients and increased their confidence in disaster situations, suggesting that inter professional training is beneficial in preparation for situations that require high level of inter professional communication and coordination, such as disasters.
Abstract
BACKGROUND:
Training in global health topics is increasingly recognized as an important element of pediatric residency. The Canadian Pediatric Society’s (CPS) Global Child and Youth Health Section created a set of four modules to serve as a national curriculum on global health for pediatric residents. The topics of the modules include global child mortality, undernutrition, fever in a returning traveler, and children new to Canada. The modules are available free online for CPS members or by mail order CD (at cost).
OBJECTIVES:
To identify the uptake of the modules in order to understand their utilization and to identify areas for improvement and expansion.
DESIGN/METHODS:
An online survey was distributed to medical educators who underwent module training, requested use of the modules, or ordered them online from the CPS. The survey was used to elicit information regarding the implementation of the modules, feedback on their content and the perceived impact on residents. Descriptive statistics were used to tabulate close-ended responses in aggregate format. All open-ended responses were analyzed using content analysis and key themes were extracted, summarized, and reported. Ethics approval was granted by the McMaster University ethics board.
RESULTS:
Forty-nine pediatricians were invited to participate in the survey. Forty-four percent (22) completed the survey including 17 from Canadian programs and five from the United States, with 67% of Canadian academic centres represented.
The majority of respondents were hospitalist pediatricians (89.5%) working in an academic centre (95%) who had an interest in global health (82%). Forty percent (nine) were involved in the creation of the modules. Only 35% attended the training workshop on the modules and the remainder prepared by reading through the training materials provided. The main forum for the modules was pediatric academic half-day (79%); although, a few individuals used them at conferences and as part of pre-departure training for global health electives. Module content received positive ratings overall: 87% indicated they were well received by the residents, 94% indicated knowledge expansion, and 89% would recommend them to colleagues. The main concern identified was keeping the modules updated. Other notable feedback suggested residents appreciated opportunities within the presentation to apply their knowledge. While there are additional resources available for the modules, only some participants utilized them; including pre-tests (45%), post-tests (32%) observed structural clinical encounters (36%), and resident handouts (59%).
CONCLUSIONS:
These modules received positive responses from pediatric educators with an interest in global health, including among those unable to attend the training session. Future directions include further module dissemination, updating the current modules and creating new ones.
Abstract
BACKGROUND:
The University of Ottawa has two level 3 NICUs, separated by an 8 min walk. In 2010, the on-call schedule changed from having one Attending Neonatologist on-call per weekend, to having two. This allowed for increased Attending supervision in each unit.
OBJECTIVES:
To examine the perceived impact of this schedule change on resident and fellow uncertainty, patient care, and teaching during weekends.
DESIGN/METHODS:
Residents, fellows, clinical assistants, nurses, and Attendings who had worked in the NICU before and after the change were surveyed. Because no survey tool existed, one was created based on domains published in the literature. The survey was piloted for content and readability. Responses were provided on a 5-point Likert scale. Results were analyzed using descriptive statistics and χ2 test for associations.
RESULTS:
Ninety individuals were eligible. The response rate was 62% (n=56). Perceptions of patient care notably improved after the change, with 87% agreeing there was an improved ability to provide safer care, 81% of respondents believing that overall patient safety was improved, and 98% of respondents agreeing that care was timelier during weekend rounds. Eighty-eight percent of respondents perceived a moderate to great improvement in trainee certainty during clinical decision-making. Trainee certainty regarding the management of resuscitations was also improved (71% of respondents agreed). The respondents’ clinical role affected their perceptions, with the greatest impact rated by the nurses, and the least by Attendings.
CONCLUSIONS:
Our results are the first to demonstrate that increased Attending supervision in the NICU decreases resident and fellow uncertainty. It may also improve patient care, and this warrants further objective study in the NICU setting. Results indicate support for one Attending per NICU in the case of two distinct physical sites.
Abstract
BACKGROUND:
There is an ever increasing demand for readily available information for patients and their families in the health care system. Access to information should be provided to patients and families by all physicians. There is not currently adequate patient centered information available to all patients nor a validated mechanism for physicians to use to provide their patients with information regarding their diagnosis.
OBJECTIVES:
To validate a method for developing new patient centered informational handouts designed to improve patient understanding of the disease process and management.
DESIGN/METHODS:
A chart review of one physician was done to identify the most common diagnoses in pediatric hematology from December 2011 to May 2012. A literature review view was then conducted to identify diagnoses that already had adequate, patient centered information available. New patient centered informational handouts were generated for each of the most common diagnoses remaining. Existing literature regarding content and structure of informational handouts was identified and incorporated into the new handouts. The handouts were then reviewed and revised by a content expert. The revised handouts were reviewed by 10 patient families using both qualitative and quantitative measurements. These results were used to further revise the handouts.
RESULTS:
The 10 most common pediatric hematology diseases seen in clinic were identified. The patient families identified four major themes when asked to review the handouts. They found the information useful, although they stressed the importance of giving this information to new patients at the time of diagnosis. They stressed the importance of physician counseling, and not using the handouts to replace counseling. Lastly, the patients liked the handouts because they could take the handouts home and use them as a reference. The handouts scored highly in regards to accuracy and being recommended to other patients and their families.
CONCLUSIONS:
Using the described framework, 10 different patient centered informational handouts have been developed and validated. This strategy outlines a way for physicians and other health care workers to create their own patient centered informational handouts to best fit their needs.
Abstract
BACKGROUND:
Medical education is now being delivered in distributed medical education settings in many medical schools in Canada. There are scant financial and manpower resources. Foundational components necessary for faculty development have not been formally established. There was a need to implement a mentorship program to enhance faculty development. The pediatrics department in one such setting undertook a peer group mentoring pilot program to address these needs.
OBJECTIVES:
The objective of this project was to explore the development of mentoring using a peer group model, and evaluate the benefits of such a model on faculty satisfaction, work-life balance, program and process development, personal and faculty development, as well as research gains. Adjunct faculty in the Department of Pediatrics were asked to be part of a pilot mentor-ship project for faculty in a distributed medical education setting.
DESIGN/METHODS:
Research ethics approval was obtained. A collaborative and mixed methods approach was taken. The participants were interviewed at the end of the series of mentorship seminars. Evaluation forms were also collected at the end of each seminar. The group decided on a number of faculty development topics that were relevant to them. The framework for selection of topics was the CanMEDS non-expert roles. The seminars were presented at a regularly scheduled journal club.
RESULTS:
Participants: 6 to 11; Years in pediatric practice: 17 to 26 years; Number of faculty: 15; M:F – 2:1 The participants felt that the sessions were very helpful and increased collegiality. They remarked that they felt valued and that they were part of selecting the topics for peer group mentoring. Evaluation forms revealed moderate to high scores.
CONCLUSIONS:
This peer mentoring model may provide the stepping stone or the scaffolding on which to build a more conventional mentoring relationship. Benchmarks for the number of faculty achieving assistant professor status in the next five years should be made for those departments who adopt a peer mentoring program.
More engagement and willingness to teach medical students and residents; increase research activities; engagement in hospital or medical school leadership; and higher medical student achievement in pediatrics could also be evaluated in the future. There is a lack of funding for this type of research. This pilot project adds to the scant body of work that supports peer or collaborative mentoring as an important pathway to achieving personal, institutional and societal goals.
Abstract
BACKGROUND:
Kawasaki disease (KD) is the leading cause of acquired cardiovascular disease in children in North America and an important cause of childhood morbidity and mortality owing to its predilection for coronary arteries. Proper diagnosis and treatment of KD can decrease this risk. We conducted a retrospective chart review to evaluate adherence to the AHA/AAP guidelines for acute management and follow-up of patients with both typical and incomplete KD.
OBJECTIVES:
Our objectives were to determine the frequency of KD diagnosed at our institution, and the proportion of KD diagnoses which are made and treated according to the AHA guidelines.
DESIGN/METHODS:
This was a retrospective chart review of all patients admitted to our institution with a diagnosis of “Kawasaki Disease” between January 2004 and December 2011. The clinical diagnostic criteria and supporting laboratory criteria were identified for each patient at the time of diagnosis. Each patient was categorized as typical or incomplete KD independently based on the retrospective information and this was compared to the admitting physician’s diagnosis. Dose and duration of IVIG and ASA therapy was reviewed.
RESULTS:
A total of 134 charts were reviewed, with 104 having a discharge diagnosis of KD. Based on retrospective application of criteria, 46 patients (44.2%) had typical KD, 16 (15.4%) had incomplete KD, and 42 (40.4%) who were discharged with a diagnosis of KD did not have the disease based on criteria. At diagnosis, 27 (26%) of patients had abnormal findings on echocardiography. A total of 91 patients (87.5%) were treated with IVIG.
CONCLUSIONS:
Suspected KD patients admitted to our institution are being treated as typical KD at a higher degree than recommended by the AHA/AAP guidelines. Deviation from the algorithm occurred in incomplete KD patients with ≤3 supplemental lab criteria as they often received IVIG despite a negative echocardiogram. This information and ongoing analysis may be used in support of developing a clinical practice guideline for our institution, thus ensuring all patients in our facility are receiving standard of care concerning the diagnosis and treatment of KD.
Abstract
BACKGROUND:
With the emerging evidence that early childhood development and experiences affect not only learning, but also lifelong physical, mental and emotional health, it is important that medical students learn to conduct effective comprehensive well-baby/well-child visits. The Rourke Baby Record (RBR) is a Canadian evidence-based validated system for well-baby/well-child care from one week to five years of age. E-Learning has gained popularity as a new approach to medical education.
OBJECTIVES:
To assess medical student knowledge of well-baby care and the RBR before and after completing an eLearning module of a six month well-baby visit of a healthy infant.
To obtain student feedback regarding the module content, clinical applicability, and web delivery.
DESIGN/METHODS:
Module development began with a medical student summer research award, enabling a student vision for the module format, and involved an instructional design specialist in addition to family physician and paediatric faculty. Participants were medical students from two stages of training: preclinical second year (Y2) and third year clerkship (Y3). The data was analyzed for: 1) knowledge gains using a pre/post test of 10 MCQs; 2) module satisfaction using a questionnaire. Most survey questions used a 5-point Likert scale with results grouped into three categories: agree (strongly agree or agree), neutral, or disagree (disagree or strongly disagree).
RESULTS:
The 121 student participants comprised 96% of the two medical school classes. Both Y2 and Y3 students had a significant increase in their post test scores (P<0.001). For most MCQs, the Y3 students scored slightly higher. Module completion time averaged 90 minutes (range 20 min to 3 h). The extensive involvement of a medical student and an instructional design specialist resulted in a creative, visually appealing module. On average, 90.9% of students answered satisfaction survey questions positively. The majority of students indicated the module should be part of the curriculum, significantly more by Y3 students (78.8% of Y2; 98.0% of Y3 students, P=0.030). More Y3 than Y2 students felt the module enhanced their knowledge (P=0.016) and provided learning applicable to patient care (P=0.022). Suggestions for improvement were largely focused on web delivery and test questions.
CONCLUSIONS:
This eLearning module was an effective tool to teach medical students how to conduct a six month well-baby visit. The module was popular with students; suggestions for improvement were minor. A second module of an 18 month well-child visit is currently under development.
Abstract
BACKGROUND:
Although rare, invasive meningococcal disease (IMD) continues to be a health concern in high-income countries, as it results in severe morbidity and relatively high case fatality, especially in young children. However, studies measuring sequelae of IMD across the spectrum of invasive syndromes have not been systematically reviewed.
OBJECTIVES:
To conduct a systematic review on sequelae attributable to IMD as well as quality of life in survivors in high-income countries.
DESIGN/METHODS:
We searched MEDLINE, EMBASE and HealthStar up to April 2013 and scanned the reference lists of relevant systematic reviews and included studies. Primary studies assessing sequelae and/or quality of life in individuals with IMD and a comparator group were eligible for inclusion. Two reviewers independently screened articles (titles and abstracts, followed by full text), abstracted data and performed quality appraisal. Findings were summarized qualitatively.
RESULTS:
Of 1884 citations screened, 22 articles reporting on 17 studies were included. The most commonly assessed sequelae were hearing impairment (in five studies), cognitive impairment (seven studies), and psychological problems (six studies). Compared with controls, IMD survivors had greater incidence of hearing loss (in children), lower mean IQ test score (children), greater incidence of psychological disorders (eg, ADHD [children], depression [adolescents/adults]), and lower overall quality of life. There were no significant differences in overall cognitive function between exposed and unexposed adults. Odds of death were significantly increased with IMD at hospital discharge and up to 30 years after disease; however, the role of pre-existing co-morbidities remains unclear.
CONCLUSIONS:
A better understanding of the breadth of IMD sequelae in high-income countries is critical to support healthcare planning and decision-making. In particular, this information is useful to assess of the burden of IMD in light of new vaccines.
Abstract
BACKGROUND:
There is evidence to suggest that socioeconomic status impacts neurocognitive functioning via family investment in child human capital. However, the role of parenting remains surprisingly equivocal, largely due to discrepancies in operationalization and measurement. Moreover, many studies examining the social determinants of cognitive development rely on simple metrics of socioeconomic status or risk.
OBJECTIVES:
The current study a) identifies multiple “family risk profiles” across several domains of adversity and b) examines the mediating role of human capital investments and sensitive maternal parenting behavior (coded from videotaped observations).
DESIGN/METHODS:
Family profiles of socioeconomic and contextual risk at two months of age were identified using participants from the Kids, Families and Places Study prospective birth-cohort. Subsequently, the impact of these profiles on child cognitive development via maternal sensitivity and human capital (material) investments was evaluated. Parents were contacted through a universal health screen seven days following childbirth (n=501) and followed until children were >4.5 years of age.
RESULTS:
Latent Class Analysis revealed that families fell into one of four profiles: 1) multilevel risk, 12.0% of sample, 2) maternal abuse history, 15.6%, 3) low-SES and immigrant status, 27.7% or 4) low-risk, 44.7%. Children in the multilevel risk and low-SES immigrant profiles had the poorest outcomes at 4.5 years. Between 35% and 56% of the effect of risk profile on cognitive outcomes was mediated by investments in child development, while 21% to 44% was mediated by maternal sensitivity, both measured at 18 months of age.
CONCLUSIONS:
Findings highlight the importance of material and interpersonal pathways through which socioeconomic and environmental disadvantage impact cognitive development. It will be argued that maternal sensitivity can be conceptualized as an alternative human capital investment, that is, a lived experience that promotes healthy development and successful adaptation across the life course.
Abstract
BACKGROUND:
Few population-based systems exist to monitor child obesity prevalence in Canada. Data from electronic medical records (EMR) have been used in a small number of juridstictions worldwide to estimate obesity prevalence in children.
OBJECTIVES:
To determine the frequency of height and weight documentation in EMRs in children, to describe the prevalence of child overweight and obesity, by age, and sex using data from the Electronic Medical Record Administrative data Linked Database (EMRALD) database in Ontario, and to determine if there are differences in prevalence based on visit type (well-child visit vs. other).
DESIGN/METHODS:
We abstracted height and weight in children zero to 19 years of age in EMRALD who had at least one well-child visit from January 2010 to December 2011. Using the most recent visit with both a documented height and weight, we reported the proportion and 95% CIs of subjects defined as overweight, and obese, by age group and sex, using the WHO growth reference standards. We compared the proportion or overweight and obese children by visit type for all age groups, using χ2 tests.
RESULTS:
There were 28,083 well-child visits in 7705 children over this study period. 84.7% of children who attended well-child visits had both a height and weight documented. The prevalence of overweight and obesity, varied by age group from 12% to 32%, and 2% to 12%, respectively. Obesity rates were significantly higher in one- to four-year-olds compared to children <1 year of age (6.1% vs. 2.3%), and in 10- to 14-year-olds compared to five- to nine-year-olds (12% vs. 9%). Both one- to four-year-old (7.2% vs. 4.9%) and 10- to 14-year-old boys (14.5% vs. 9.6%) had higher obesity rates. The proportion of overweight and obese children was higher using heights and weights reported from other child visit types, compared to well-child visits, for all age groups (P<0.05), except for children less than one year of age (P=0.45).
CONCLUSIONS:
We documented a high rate of overweight and obesity in children. EMR may be a useful tool to conduct population-based surveillance of child overweight and obesity in Canada. The selection of visit type may be an important methodological consideration.
Abstract
BACKGROUND:
Severe neonatal hyperbilirubinemia is very rare and can be associated with significant morbidity, including bilirubin encephalopathy and death. Despite the implementation of routine screening guidelines and access to readily available treatment, severe neonatal hyperbilirubinemia continues to be reported in western industrialized countries.
OBJECTIVES:
Our primary objective is to describe and compare the incidence of severe neonatal hyperbilirubinemia in three western, industrialized nations (Canada, the United Kingdom and Ireland, and Switzerland). Our secondary objective is to identify and describe demographic and clinical variables associated with severe neonatal hyperbilirubinemia.
DESIGN/METHODS:
Using data derived from three national surveillance programs, the Canadian Paediatric Surveillance Program (CPSP) (2002–2004), the British Pediatric Surveillance Unit (BPSU) (2003–2005), and the Swiss Pediatric Surveillance Unit (SPSU) (2007–2008), we compared the incidence of severe neonatal hyperbilirubinemia among the three populations. Descriptive statistics were used to compare demographic and clinically relevant variables as well as treatment practices and indicators of early neurological sequelae. Preliminary comparisons between the CPSP and BPSU data were performed. Chi-square test for differences in proportions was performed on categorical data and CIs were calculated for means with standard deviations. Statistical significance was assumed if CIs did not overlap.
RESULTS:
Preliminary analysis has estimated the incidence of severe neonatal hyperbilirubinemia to be 40 per 100,000 live births in Canada, seven per 100,000 live births in the United Kingdom and Ireland, and 41 per 100,000 live births in Switzerland. The Canadian and British groups reported mean peak serum bilirubin levels to be 471 μmol/L (156 μmol/L to 841 μmol/L) and 580 μmol/L (510 μmol/L to 802 μmol/L) respectively, and the incidence of bilirubin encephalopathy to be five per 100,000 live births and 0.9 per 100,000 live births respectively. Canadian patients were more likely to have vaginal births (78.7% vs. 58.3%); P=0.02. United Kingdom patients were more likely to be delivered by C-section (18.5% vs. 4.3%); P=0.02. There were no statistically significant difference in gender, mean gestational age, mean birth weight, feeding method, and mean age at presentation
CONCLUSIONS:
Despite the implementation of screening guidelines to identify infants with high serum bilirubin levels, severe neonatal hyperbili-rubinemia continues to occur in western, industrialized populations
Abstract
BACKGROUND:
To prevent deficiency several agencies including the CPS recommend 400 IU/d of vitamin D in infancy. For nearly 20 years, Quebec has offered a program of free supplements through its public medication insurance plan (RAMQ). Other jurisdictions have implemented programs to enhance vitamin D supplementation.
OBJECTIVES:
Our study sought to evaluate the uptake of vitamin D via this prescription program in both term and preterm infants and determine the incidence of nutritional rickets over this time.
DESIGN/METHODS:
This was a retrospective cohort study of infant; the data are derived from the province of Quebec, Canada. All healthy infants born between 1998 and 2008 and covered by RAMQ drug plan were included. Data were extracted from the Quebec Pregnancy Cohort built by the linkage of three databases: RAMQ medical and prescription databases (diagnoses, medications, SES), MedEcho (hospitalizations), and ISQ (birthweight, SES). Predictors of program participation were identified through logistic regression (GEE).
RESULTS:
A total of 123,018 term infants were eligible for RAMQ and the mean annual prevalence of supplemental vitamin D exposure was 17.9±5.6%. The median age for obtaining the first bottle was 36 days (range 1 to 370). The majority (51.0%) obtained only one bottle of fifty doses (median 1, range 1 to 20). 8812 preterm infants were similarly eligible; vitamin D exposure was 34% in early (23 to 33 weeks) and 17% in late preterm infants. The median age was 49 days and the median number of bottles was two (range one to 15). For all infants, mothers of higher SES, those who lived as a couple, older mothers, or a prescription by a pediatrician significantly increased the odds of obtaining vitamin (P<0.05). Additionally, there was a statistically significant decline in program participation over time (OR 0.89 per year, 95% CI 0.88 to 0.90). The overall incidence of nutritional rickets was 23.9 cases per 100,000 live births with an annual increase of 1.12 cases per year (Poisson regression, 95% CI 1.01 to 1.24).
CONCLUSIONS:
Without specific educational measures, a free prescription program for vitamin D failed to encourage participation or long-term adherence. Moreover, participation decreased with time and coincided with an increase in the incidence of rickets. Higher SES and care by a pediatrician increased odds for participation. New strategies targeting these variables and providing educational support for healthcare workers and the general community may need to be developed to increase vitamin D supplementation rates.
Abstract
BACKGROUND:
Infant mortality rate is a key perinatal health indicator, widely used as an index of population health status. International comparisons of infant mortality rates need to be interpreted with caution. Differences in birth registration criteria are a recognised problem, especially for preterm infants at the borderline of viability. Variations in the reporting of stillbirths/live births are another concern. Varied definitions are used to calculate perinatal mortality rates and this is further complicated by whether induced abortions and terminations of pregnancy are included or excluded.
OBJECTIVES:
We examined perinatal and infant mortality rates in selected high income countries for evidence of differences in registration practices, classification of stillbirths and live births and selective registration of extremely preterm infants who survive.
DESIGN/METHODS:
We carried out a retrospective population-based cohort study using national data from Canada, the United States, Denmark, Finland, Iceland, Norway, and Sweden for the period 1995 to 2005. The main outcome measures included live birth distribution by gestational age and birth weight; gestational age- and birth weight-specific fetal, neonatal, and post-neonatal mortality; and cause-specific (congenital anomalies, immaturity-related and other conditions) infant mortality.
RESULTS:
Our results show country-specific live birth distributions by birth weight and gestational age, birth weight- and gestational age-specific mortality and cause-specific mortality over a 11 year period, from 1995 to 2005. We observed differences between countries when crude neonatal mortality rates were compared to neonatal mortality excluding near-viable births. Similar results were obtained for stillbirths but not for postneonatal mortality which were essentially unaffected by the exclusion of near-viable births.
CONCLUSIONS:
These findings provide a comprehensive perspective of infant mortality rates in these countries by using specific birth weight and gestational age cut-off values, to preclude artefacts that often arise from such international comparisons. It also highlights the need for standardizing birth registration and infant death registration procedures globally, in order for international comparisons of fetal and infant mortality rates to be more meaningful.
Abstract
BACKGROUND:
Adolescents with inflammatory bowel disease (IBD) are vulnerable to increased morbidity during transition from pediatric to adult health care. Current approaches to transition are based on expert opinion and limited research on the anticipated needs of adolescents and their families.
OBJECTIVES:
The aim of this study was to identify the needs of young adults with IBD at transition by examining the views of young adults who transitioned in the past and to see if those needs differed from IBD patients diagnosed as young adults.
DESIGN/METHODS:
A qualitative interpretive description approach was utilized. Participants aged 18 to 30 years recruited from the McMaster University Medical Centre IBD clinic between July 2012 and May 2013. Semi-structured interviews were conducted using an interview guide with questions probing participants to discuss their needs. Interviews were audiotaped, transcribed verbatim and coded using a constant comparative method. QSR NVivo10 was used to manage the data. Sample size was established when no new additional themes were encountered.
RESULTS:
Twenty-one young adults were interviewed: 15 subjects diagnosed <18 years of age and six subjects diagnosed as young adults. Among those diagnosed <18, transition needs were identified in the key areas of psychosocial, informational, self management, and daily living needs. Psychosocial needs were most commonly reported with subjects citing needs for support networks, removing social barriers, and coping with anger, depression, sadness, and anxiety. Subjects detailed how IBD led to intentional self-isolation from social settings. A paucity of information was reported on the impact of smoking, drugs, and alcohol use. Overcoming financial barriers and participation in decision-making were noted as the primary signs of achieving independence. Subjects diagnosed as adults more often sought peer support groups and experienced more difficulties with healthcare access, financial concerns, and social isolation. Participants with less severe disease sought more client-centered care and those with more severe disease were more likely to describe social isolation.
CONCLUSIONS:
We report the first study in the transition literature of already transitioned individuals’ needs during the transition process. Individuals with IBD who have undergone transition focus most on psychosocial and financial needs rather than self management of their chronic illness. This finding is likely generalizable to most adolescents and young adults with chronic life-long diseases. Psychosocial and financial readiness are not presently assessed in existing transition and self-management tools, and may need to incorporate these areas to more effectively measure the success of transition interventions.
Abstract
BACKGROUND:
Newborn pulse oximetry screening increases detection of critical congenital heart disease otherwise missed by antenatal ultrasound and physical examination. The AAP endorsed a protocol checking oxygen saturations in the right hand and one foot at ≥24 h of age, with abnormal results (<95%) subject to repeat screening.
OBJECTIVES:
We describe our experience in implementing a simplified protocol at a Canadian tertiary children’s hospital and a referring regional hospital.
DESIGN/METHODS:
We collected information from the screening program organizers.
RESULTS:
Cardiology chose a simplified screening protocol, checking oxygen saturations in one foot between 24 h and 36 h of age. This was supported by a meta-analysis indicating no significant differences in sensitivity or false positive rates compared to checking both foot and right hand (Thangaratinam, Lancet 2012). A single abnormal saturation (<95%) requires physician assessment. If the low saturation is confirmed and no other cause identified, an echocardiogram would be arranged within 24 h (utilizing telemedicine at the regional hospital).
Physicians and nurses welcomed more ways to improve detection of CHD. Screening was started in February 2013 in the post partum unit at the tertiary hospital (approximately 4500 neonatal admissions annually) and in July 2013 at the regional hospital (approximately 900 annually). As of December 2013, there have been no positive screens. All cardiac surgery in the region comes to the tertiary hospital; we are aware of no false negative results.
Education was delivered at a staff meeting followed by individual teaching as required, and a written protocol was distributed. As nurses were familiar with pulse oximetry, education focused on teaching the protocol.
Reusable oximetry probes and probe wraps were used. Three dedicated oximeter machines were adequate for the tertiary unit and one was used at the regional site. Testing was usually done at bath time. We estimate it takes 10 minutes to do the screen, clean the probe and document.
A selective chart review showed excellent compliance, but inconsistency in where results were being documented. Newborns discharged from the birthing unit and home births were not being screened.
CONCLUSIONS:
Our experience shows that a pulse oximetry screening program can be readily implemented. There are areas for improvement in documentation, and we identified groups to target for screening. We believe the simplified protocol and shifting the management of abnormal screens to the physician allowed for easier implementation.
Abstract
BACKGROUND:
Mothers of infants admitted to hospital with jaundice are at risk of stopping breastfeeding.
OBJECTIVES:
We examined the impact of a breastfeeding support intervention on breastfeeding duration in infants admitted to hospital with jaundice.
DESIGN/METHODS:
This was a randomized controlled trial with a qualitative component. We aimed to recruit 124 participants (62 per group). Mothers of breastfeeding infants <1 month of age admitted to the Children’s Hospital of Eastern Ontario (CHEO) with a diagnosis of jaundice between October 2010 to 2013 were randomly assigned to the intervention or control group. Mothers in the intervention group met with an International Board-certified Lactation Consultant in hospital, and one to three times after discharge. Both groups received hospital standard of care for jaundice treatment. The main outcome measure was exclusive breastfeeding at three months of age. Secondary outcomes included partial and exclusive breastfeeding at various time points, number of re-hospitalizations, number of physician encounters, and number of mothers seeking breastfeeding help, all in the first six months of life. Semi-structured interviews elicited feedback on participant experiences.
RESULTS:
A total of 99 participants were recruited (49 in the control and 50 in the intervention group). 86 were included in the analysis of the primary outcome. There was no difference in exclusive breastfeeding at three months between groups (RR 0.77 [95% CI 0.51 to 1.14]; P=0.20) or in any of the secondary outcomes. Thirty-one participants (13 in the control group, 18 in the intervention) were included in the qualitative analysis. Intervention group participants reported an increase in comfort and confidence levels with breastfeeding, an enhanced emotional wellbeing, and a feeling of empowerment to pursue breastfeeding. Control group participants reported limited breastfeeding support in hospital, which was largely restricted to verbal information. Recommendations from both groups included the presence of an on-site lactation consultant at CHEO.
CONCLUSIONS:
Although the quantitative analysis failed to demonstrate significant differences between groups, feedback on the study intervention obtained in the qualitative analysis was positive. Qualitative analysis suggests an increase in mothers’ confidence, which has been linked to breastfeeding duration. Further larger studies are needed to elucidate the impact of an inhospital lactation support program on successful breastfeeding.
Footnotes
Trial registry: www.Clinicaltrials.gov; Identifier: NCT 00966719 Funded by the Physicians’ Services Incorporated Foundation
Funded by the Physicians’ Services Incorporated Foundation
Abstract
BACKGROUND:
Bronchiolitis, a lower respiratory tract infection is a common cause of illness and hospitalization in infants and young children.
Although several studies suggest that routine bacteriological testing in children with typical bronchiolitis have limited value, there is a dispute when it comes to the assessment of young febrile infants. Precisely, it is not known whether viral respiratory infections might lead to urinary tract infections
OBJECTIVES:
to determine the risk of acquiring urinary tract infection in infants and children with acute bronchiolitis
DESIGN/METHODS:
A retrospective and descriptive study was conducted at Hamad Medical Corporation. Patients aged zero to 18 months hospitalized with acute bronchiolitis from October 2010 to March 2013 were included in the study. The following data were collected: age at diagnosis, sex, direct fluorescent antibody (DFA) and urine culture results.
RESULTS:
There were 836 infants in the study, mean age 3.6±3.5 months and boys constituted 60% of the total number; DFA was conducted on 770 infant and children; 352 (45.7%) were RSV-positive, 142 (18.5%) infants were RSV-negative and 276 (35.8%) infants were positive for other non-RSV (Human metapneumo virus, Adenovirus, Rhinovirus, Influenza Virus, Parainflenza virus, and Boca virus). Urine cultures were obtained for 586 (70.1%) of enrolled infants. The overall prevalence of UTI was 8.7% (95% CI 6.62 to 11.2). The prevalence of UTI in the RSV-positive was 4.9% (11 of 224; 95% CI 2.7% to 8.7%) compared with 8% (eight of 100; 95% CI 3.9% to 15.2%) in the RSV-negative, and others non-RSV 13.4% (30 of 224; 95% CI 9.5% to 18.5%)
CONCLUSIONS:
Infants and children with acute bronchiolitis due to viruses other than RSV at risk for acquiring urinary tract infections, and obtaining urine culture might be warranted. However, further and larger studies are required
Abstract
BACKGROUND:
L’intimidation scolaire est endémique. Plusieurs consultations pédiatriques découlent de maux physiques chez les élèves; certains étant secondaires à l’intimidation scolaire. Plusieurs facteurs protecteurs envers les douleurs physiques sont rapportés.
OBJECTIVES:
Cette étude vise à dresser un portrait global du phénomène d’intimidation scolaire et des maux physiques exprimés par les élèves. Elle explore l’apport de la communication parent-enfant, l’implication du vécu scolaire parental et les antécédents de maux physiques parentaux dans la reconnaissance de l’intimidation scolaire causant ces maux physiques.
DESIGN/METHODS:
Collecte de données via trois questionnaires : en deux temps et à un mois d’intervalle (192 élèves de la Commission Scolaire de la Région de Sherbrooke et leurs parents respectifs). Ces questionnaires évaluent l’identification de l’intimidation scolaire et la présence de maux physiques chez les étudiants (auto-rapportés par les jeunes et suspectés par les parents), qu’ils pensent reliés à cette intimidation. Les facteurs protecteurs face à l’intimidation scolaire et l’apport du vécu scolaire des parents sont également investigués. Critères d’inclusion : formulaire de consentement signé par un parent, langue française comprise de tous, élève fréquentant soit 4e, 5e ou 6e année du primaire.
RESULTS:
L’intimidation scolaire auto-rapportée par les élèves du primaire persiste sous quatre formes : physique (44%), verbale (68%), sociale (49%), cyber-intimidation (21%). La distribution des maux physiques demeure semblable selon les sexes; la céphalée et la douleur abdominale prédominent.Concernant la communication parent-enfant face à l’intimidation scolaire, 84 % (n=169) des enfants et 88 % (n=177) des parents se disent satisfaits. Seulement 32 % des enfants et 38 % des parents reconnaissent le lien entre l’intimidation scolaire et leurs maux physiques. De ces parents, 25 % consulteront un médecin. Cette décision semble fortement influencée par leur exposition antérieure à de l’intimidation scolaire et/ou à la présence de maux physiques lors de leur jeunesse.
CONCLUSIONS:
Le phénomène d’intimidation scolaire persiste au sein des écoles primaires de Sherbrooke. Plusieurs présentent des maux physiques y
étant reliés, entraînant des consultations médicales. Les parents exposés anté-rieurement à de la douleur et/ou à de l’intimidation scolaire reconnaissent davantage la présence de maux physiques chez leur enfant. Ceci démontre qu’un phénomène douloureux éprouvé pendant l’enfance laisse longtemps des traces, d’où l’importance d’agir précocement. Ainsi, en améliorant la communication parent-enfant relative à l’intimidation scolaire, ces maux devraient être plus rapidement reconnus et adéquatement investigués.
Abstract
BACKGROUND:
The Royal College of Physician and Surgeon of Canada mandates that all pediatric trainees gain expertise in specific procedural skills prior to completing their training. The current landscape of medical education, however, may not provide residents with enough opportunity to observe and perform such skills. The reason for this change is multifactorial; with factors such as reduction in learners’ working hours or a movement towards more non-invasive treatments. The cumulative effect could be that residents fail to achieve the competency required in essential procedures by the end of their training.
OBJECTIVES:
To determine the frequency and level of comfort of pediatric residents in performing procedural cited as essential to the practice of general pediatrics by the Royal College of Physicians and Surgeons of Canada.
To examine if there is any perceived difference in the importance of competency in each procedural skill between residents and practicing general pediatricians.
DESIGN/METHODS:
This prospective survey was undertaken at a single academic institution. Residents and general pediatricians were surveyed on how often they performed procedures listed by the Royal College of Physicians of Canada training objectives. Participants were also asked to rate their confidence level in performing each skill, along with their perception of which skills were necessary for pediatrics practice.
RESULTS:
Thirty seven participants completed the survey (22 residents, 15 staff). 14 residents were in their first two years of training. All staff physicians had community practices, >90% also had academic appointments. 100% of residents and practitioners identified neonatal and pediatric resuscitation skills as essential to practice though used this skill set <5 times in the last year. Competence in all other non-resuscitation procedures were rated as either useful or important, but not essential to general pediatrics. The emphasis placed on a skill was not predictably related to the frequency they were performed. Residents uniformly described less confidence in performing all procedures than attending physicians.
CONCLUSIONS:
This study shows that despite limited training and exposure to a skill, residents are able to distinguish which procedural skills are important to the practice of general pediatrics.
Abstract
BACKGROUND:
The Canadian Pediatric Society (CPS) and the American Academy of Pediatrics (AAP) publish clinical practice guidelines (CPGs).
OBJECTIVES:
The objective of this study was to describe how Canadian pediatric residents, pediatric emergency physicians (EPs) and general pediatricians (GPs) are currently using CPGs, to identify barriers to CPG use and to suggest ways to make CPGs more user-friendly.
DESIGN/METHODS:
An observational cross-sectional on-line survey (mailed to those without email) was sent to GPs and EPs affiliated with two Canadian pediatric hospitals, and to all general pediatric residents in Canada. The study focused on patterns of reviewing CPGs, preferred methods of access, barriers to use, and suggestions to improve CPGs. Responses were compared between residents, EPs and three groups of GPs: 1) work on clinical teaching unit (CTU) for >6 weeks/year (GPA), 2) work on CTU for one to six weeks/year (GPB), 3) rarely or never work on CTU(GPC).
RESULTS:
Response rate was 21% (178 of 847). Almost all respondents reported using CPGs published by the CPS (98%) and/or AAP (94%) in their practice. Frequency of use was different between groups (P<0.001); most residents (62%), emergency physicians (54%) and GPA (55%) reported referring to CPGs at least once/month as compared to GPB (14%) and GPC (21%). The percentage of physicians who routinely read or skim CPS/AAP guidelines as they are published was: residents (24%/6%), EP (49%/19%), GPA (36%/0%), GPB (57%/21%) and GPC (58%/46%) with AAP guidelines often being used for specific cases. Barriers that respondents “often” encountered were: “Forget that guidelines exist” (22%), “Don’t have time” (18%), “Find guidelines to be too long” (16%) and “No guideline on my question, even though I think that there should be one” (14%). Most (57%) of respondents said disagreement with guidelines was “often” or “sometimes” a barrier. Most are now referring to guidelines electronically and would be likely to utilize Smartphone applications (median of the five groups 89%), online summaries (82%), email reminders (75%) and CME credits (74%) for reading CPS CPGs.
CONCLUSIONS:
Almost all respondents are using CPGs for clinical advice, but GPB and GPC do so less frequently than the other groups. Addressing awareness and accessibility of CPGs, as well as expanding topics covered may improve frequency of use. Few respondents were accessing guidelines via paper-based publications, suggesting resources would be better directed towards creating smartphone applications, online summaries and email reminder systems.
Abstract
BACKGROUND:
Feeding rehabilitation of feeding-tube dependent and feeding-disordered infants and children can be a protracted challenge. Standard outpatient approaches rely on behavioural and sensory interventions based on largely anecdotal data.
Effective stimulus-based intervention has until now required prolonged admission to the few specialized centers that offer this approach.
OBJECTIVES:
To assess effectiveness of a community hospital or clinic stimulus-based intervention for feeding-tube dependent and feeding-disordered children.
DESIGN/METHODS:
Uncontrolled non-randomized prospective clinical study. Children were either managed as inpatients (17) or outpatients (3) with immediate discontinuation of all tube feeds and implementation of a standard “picky eater” behavioural management program. Supplemental fluids were provided by tube during sleep if the child was noted to have significant ketosis, weight loss and lethargy.
RESULTS:
A total of 20 children (17 in-patient and three out-patient) were enrolled. Successful progression to full or partial oral feeding was seen within one week of admission in 17 of 19 (89%) of inpatient managed children and three of three (100%) of children managed as outpatients. Three children subsequently required re-initiation of tube feeding due to parental or medical concern with adequacy of intake (74% long-term successful feeding outcome). Two children with severe behavioral or developmental challenges were resistant to this intervention.
CONCLUSIONS:
Selected tube-dependent and feeding disordered children can be successfully managed in a community-based setting without multidisciplinary support using a naturalized non-coercive hunger and thirst-stimulated approach. Parent satisfaction was extremely high.
Table 1).
In-patient details. FA Feeding aversion; GT G-tube; NG Nasogastric tube; P Partial success (fluid only); S Complete success (full range of foods); F Failure; *Some oral intake at admission
| History | Age (m) | Tube | Outcome |
|---|---|---|---|
| FA | 21 | N/A | S |
| 22qll,.Tetralogy of Fallot | 20 | GT | S |
| Trisomy 21 | 36 | GT | S |
| VSD, Laryngomalacia | 6 | NG* | S |
| Post-viral encephalophy | 23 | NG* | S |
| Hypoplastic LV (Norwood, Fontan) | 18 | NG | P* |
| VSD, myocarditis | 15 | GT* | S* |
| SGA,.GDD | 23 | NG | P* |
| FA | 35 | N/A | S |
| SGA, CP, GDD | 30 | NG | P |
| Robin Sequence, tracheotomy | 60 + 72 | GT | F |
| Congenital diaphragmatic hernia, pulmonary hypertention | 9 | NG | S |
| FA, hypotonia | 30 | GT | S |
| Hypoplastic LV, cardiac transplant | 24 | NG* | S |
| Recurrent pyelo, Vesico-ureteric reflux | 24 | NG* | S |
| Ex-prem, GDD, CP | 74 | GT | F |
| Ex-prem, IVH, CP, seizure disorder | 55 | GT* | S |
Abstract
BACKGROUND:
Receiving a new developmental diagnosis is challenging for families. The considerable variability in how long it takes families to access services and the proportion of services families receive reflects challenges families face in navigating and accessing the right developmental services.
OBJECTIVES:
To determine how developmental pediatricians can better support families with a new developmental diagnosis to access the right developmental services.
To develop a new tool designed to better support these families through iterative dialogue with both physicians and families.
DESIGN/METHODS:
We conducted a written survey with developmental pediatricians to elicit concerns on whether families are accessing the right developmental services and to determine the features of an ideal standardized instrument. We used this feedback to develop a new tool, the Developmental Passport, designed to better support parents while accessing services. This tool is inspired by existing passport-type tools already used in healthcare (eg, immunization record), but tailored for the needs of families with a new developmental diagnosis. We conducted a focus group with developmental pediatricians and standardized telephone interviews with caregivers of children with ASD to evaluate the design and utility of the Developmental Passport. We performed a thematic analysis with a semantic approach.
RESULTS:
Among the 14 developmental pediatricians, half felt that families are usually able to access fewer than 50% of developmental services recommended. The physicians recognized important barriers exist to service access, but indicated families can best identify these. Important barriers identified by 11 caregivers included 1) feeling overwhelmed, both by the diagnosis and their child’s symptom severity; 2) difficulty in navigating the developmental service system, which is archaic, time-consuming, and not transparent; 3) financial barriers; 4) lack of communication with publicly-funded developmental service agencies. To provide family-centered care, physicians suggested parents should take ownership of the Developmental Passport. Families supported the Developmental Passport as a simple, effective tool. They made concrete suggestions on the tool’s design including best organization of agency presentation and greater focus on accessing financial support. The final tool is a product of an iterative dialogue among the tool’s developers, developmental pediatricians, and caregivers.
CONCLUSIONS:
Families are struggling to access the right services. Both developmental pediatricians and families supported the Developmental Passport in its current form and believe it will be an effective tool to both identify and address these gaps. Further evaluation of the Developmental Passport is required to determine its utility prospectively.
Abstract
BACKGROUND:
The School-based health center (SBHC) is an emerging model for developmental healthcare delivery in Canada. Despite access to universal healthcare, barriers such as language, cultural differences and transportation affect access for children in underserved populations in Canada. The Model Schools Pediatric Health Initiative is the first SBHC program in Ontario, Canada established to alleviate barriers inner city children face to accessing developmental care. As part of the program, pediatricians attend interdisciplinary monthly school based (school support team, SST) meetings to help identify which students require developmental assessments and then offer them through the participating SHBC.
OBJECTIVES:
To provide an update on the Model Schools Pediatric Health Initiative SHBC program with respect to feasibility and efficacy.
DESIGN/METHODS:
A retrospective chart review of all clinic users from November 2010 to January 2012 was conducted and a prospective longitudinal cross-sectional analysis was implemented from February 2012 to June 2013. Among those referred for developmental concerns, time from identification at the SST meeting to first developmental assessment at the SBHC was calculated. The feasibility metrics included the number of children who enrolled at the SBHC. The efficacy metrics included the proportion of enrolled children who attended the SBHC, the proportion of new diagnoses established, as well as wait times.
RESULTS:
In total, 1042 children enrolled at the SBHC and 443 (43%of those that enrolled) attended the SBHC. There were a total of 282 new diagnoses established at the SBHC and among these 181 (64%) were in the developmental diagnostic category. From March 2012 to April 2013, 41 students were referred for developmental assessments from the School Support Team (SST). Thirty-three assessments were completed at the time of analysis and the mean wait time from presentation at the SST to developmental assessment was 102 days.
CONCLUSIONS:
The SBHC has proven to be feasible and efficacious. This model relies on an integrated approach whereby pediatricians and school board professionals meet monthly to discuss and triage at risk students needing developmental assessments. This process allows for better understanding of school related problems and provides assessments within the school setting thereby eliminating some barriers to healthcare access. Relative to the standard of care this process is fast and efficient and creates an optimal setting to increase access to specialized developmental services for inner city children facing barriers to accessing health-care in Canada.
Abstract
BACKGROUND:
In Canada, Neonatal Intensive Care Units (NICU) and Neonatal Follow-Up (NFU) programs are regionalized health services. Families who experience preterm birth (infants <29 weeks gestation) therefore travel greater distances to access specialized health services. The effect of distance from NICU, inter-NICU transfers and infant factors on attendance at NFU programs has not been studied at a national level.
OBJECTIVES:
To determine distances from home to NICU, home to NFU and factors affecting attendance rates at NFU programs in Canada.
DESIGN/METHODS:
Canadian-born infants born <29 weeks gestation between January 1 and December 31, 2010 were followed from NICU admission through to 18 months corrected age (CA). Data were tracked through the integrated Canadian Neonatal Network (CNN) and Canadian Neonatal Follow-Up Network (CNFUN) databases. Mean travel distance was calculated using postal code data. Significance was assessed based on attendance status using Pearson Chi-Square for categorical variables and ANOVA for continuous variables.
RESULTS:
Of 1661 NICU admissions, 462 were excluded due to mortality, transfer out of country and NICU without a NFU program. Of the remaining 1199 infants, 950 (79.2%) attended NFU. Infant factors associated with NFU attendance were lower gestational age (P=0.02), lower mean birth weight (P<0.01) and higher severity of illness (SNAP II score, bronchopulmonary dysplasia [O2 at 36 weeks CA], P<0.01, retinopathy of prematurity [Grade 3 or higher], P=0.01 and intraventricular hemorrhage [Grade 3 or 4], P=0.03). The median distance in kilometres to NICU was 23.4 [IQR 8.6 to 90.3] ranging from 6.4 to 195.8 between NICUs and to NFU was 22.9 [IQR 8.8 to 75] range 4.3 to 265.1. Travel distance, number of inter-NICU transports and infant surgical necrotizing enterocolitis status were not associated with attendance.
CONCLUSIONS:
Families of preterm infants, on average, travel considerable distances to access health services. Despite this, attendance at NFU programs was associated with infant factors rather than travel distance. The outcome of this study provides new insight into Canadian attendance rates and infants who are less likely to attend NFU.
Abstract
BACKGROUND:
Pediatric injury is highly prevalent and has significant impact both physically and emotionally. The vast majority of pediatric injuries are treated in emergency departments (EDs), where treatment of physical injuries is the main focus. In addition to physical trauma, children often experience significant psychological trauma, which often goes unrecognized. The development of posttraumatic stress disorder (PTSD) is common, sometimes even after seemingly mild trauma. The consequences of failing to recognize childhood PTSD are stark and extend into adulthood. Currently, screening guidelines to identify children at risk for developing for these stress disorders do not exist in the pediatric emergency setting.
OBJECTIVES:
The goal of this systematic review is to summarize evidence on psychometric properties, diagnostic accuracy, and clinical utility of screening tools that identify or predict PTSD in children and adolescents with acute injury.
DESIGN/METHODS:
Computerized databases including MEDLINE, EMBASE, CINAHL, ISI Web of Science and Psychological Abstracts/PsycINFO were searched and included MeSH headings (posttraumatic stress or acute stress), (pediatric or children) and diagnosis. After duplicate removal, titles and abstracts were screened by two independent reviewers for eligibility and taken for full text review. Quality of included studies was assessed using the QUADAS tool for diagnostic accuracy.
RESULTS:
A total of 10,415 articles were screened by title/abstract by two independent reviewer reviewers and 228 potentially relevant articles were retrieved in full text. Interrater reliability (kappa) score of 0.833 was calculated for article screening. Screening tool characteristics; including type of instrument, number of items and administration time as well as quantitative diagnostic data (specificity, sensitivity, positive and negative likelihood/odds ratios, as appropriate) were compiled for 89 screening tools. Of these tools, we identified one immediate use risk assessment tool and 88 symptom assessment tools including three clinician-administered screening tools, 56 self-report screening tools, seven parent-report screening tools and 22 (semi-) structured diagnostic interviews.
CONCLUSIONS:
Numerous PTSD screening tools exist and span a wide variety of clinical pediatric settings. Although most tools are overly complex and lengthy to be suitable for ED use, a small number of simple/abbreviated tools exist and further research is warranted to determine their efficacy in the ED setting of pediatric injury.
Abstract
BACKGROUND:
A clinical score was reported in 2010 by Bin et al to identify head-injured infants that are at higher risk of skull fracture.
OBJECTIVES:
To determine the criterion validity of the clinical score to identify skull fracture among children younger than two years old with head trauma and no need for head tomography.
DESIGN/METHODS:
A prospective cohort study was conducted in two pediatric emergency departments. Participants were all children younger than 24 months who sustained a head trauma and for whom head tomography was not highly recommended according to the PECARN head CT scan rule. The exposure of interest was the clinical score (from 0 to 8) composed of the age of the patient, the size and location of the hematoma. The previous study suggested that a score higher than two would be predictive of skull fracture. The primary outcome was the presence of a skull fracture according to radiological report. All participants were initially evaluated by a physician using a standardized datasheet before radiological evaluation. Skull radiography ordering was left at the primary physician’s discretion. The primary analysis was the association between the clinical score and presence of a skull fracture. It was estimated that a sample of 50 cases of fracture would provide a width of ±0.05 if the sensitivity of the score was higher than 0.90.
RESULTS:
A total of 765 patients were recruited during the study period. Among them, 271 had a radiological evaluation and 50 had a skull fracture. Most children had low clinical score but 209 had a score >2. A clinical score >2 points resulted in a sensitivity of 0.86 (95% CI 0.74 to 0.93) and a specificity 0.77 (95% CI 0.74 to 0.80).
CONCLUSIONS:
The clinical decision score demonstrated a moderated sensitivity to identify children at risk of skull fracture. Further studies are required to derive a useful clinical decision rule for young children with head trauma.
Abstract
BACKGROUND:
A massive haemorrhage can be a rare but serious complication of paediatric trauma and obstetrical cases. In order to optimize the management of massive haemorrhages, a protocol was implemented at our centre. However, recent audits showed that necessary improvements were to be made to many aspects of its application.
OBJECTIVES:
To evaluate the application of a massive hemorrhage protocol and the ability to work in interdisciplinary teams using simulation and targeted training. We also aimed to evaluate confidence levels of different team members to apply the protocol and to hold their role in an interdisciplinary team during a crisis situation.
DESIGN/METHODS:
Prospective observational study held at the simulation lab of a tertiary mother-child health care facility. Participants were nurses, respiratory technicians, orderlies, anesthetists, obstetricians, pediatric emergency physicians, pediatric intensivists and hematologists. Pediatric emergency/intensive care and obstetrical/anesthesia teams were submitted to high fidelity simulated pediatric trauma and post-partum massive hemorrhage scenarios respectively (Simbaby (Laerdal) and Noelle (Gaumard)). Each participant was asked to hold their usual role in an interdisciplinary team. Targeted training consisted of a debriefing session and a presentation reviewing the massive hemorrhage protocol as well as teamwork skills. All sessions were videotaped. Documents were given during the first session for future references and to prepare for the post session two weeks later. Confidence questionnaires were filled out during both sessions. Four blinded independent trained raters reviewed the videos and assessment was done using a checklist derived from the protocol and the Mayo High Performance Teamwork Scale. Means and standard deviations of scores for performances were calculated for each scenario and compared using an ANOVA test. Descriptive statistics for the confidence questionnaires were compared using a Mann Whitney test.
RESULTS:
A total of 62 healthcare professionals involved in eight interdisciplinary teams (four obstetrics/anaesthesia and four paediatric emergency/intensive care) as well as eight blood bank technologists and eight haematologists participated in the study. Following training, scores for the application of the protocol improved by 24% (95% CI 10 to 39). Scores for the ability to work in teams improved by 17% (95% CI 6 to 28). Confidence levels in the ability to apply the protocol and work in teams improved by 13% (95% CI 11 to 16).
CONCLUSIONS:
Targeted training involving HF simulated scenarios and protocol review improved participant ability to apply the massive haemorrhage protocol and to work in interdisciplinary teams. Confidence levels improved among participants from all disciplines.
Abstract
BACKGROUND:
Although long to administer, the State Trait Anxiety Inventory (STAI) is the gold standard to measure anxiety in children.
OBJECTIVES:
To evaluate the agreement between the STAI and other anxiety scales (a visual analog scale [VAS], a likert scale, and a new Faces Anxiety Scale [FAS]), to determine whether these shorter scales could replace the STAI.
DESIGN/METHODS:
This was a prospective cohort study on a convenience sample of French-speaking children, aged nine to 17 years, presenting to a pediatric emergency department (ED). We excluded patients with drug intoxication, altered level of consciousness, decreased visual acuity, clinically unstable status, requiring admission to the intensive care unit, or with developmental delay. Patients were divided into two groups: pre-teens (PT) (aged nine to 12 years) completed the pediatric STAI; and teens (T) (aged 13 to 17 years) completed the adult STAI. Participants also completed a VAS (0 to 100 mm), a Likert scale (1 to 5), and the FAS (1 to 5). All scales were administered in random orders, twice during the ED visit, to assess anxiety states and traits. Intra-class correlation (ICC) (two way-mixed model, average measures) was used to evaluate agreement between the STAI and other scales. A sample size of 100 patients per group was estimated as sufficient.
RESULTS:
Between January 2012 and September 2013, 215 and 268 patients in the PT and T groups, respectively, were approached to obtain 100 participants in each group. The median (IQR) STAI state anxiety scores were 33 (28.25 to 36.75) and 37.5 (32 to 44), in the PT and T groups, respectively. The median (IQR) STAI trait anxiety scores were 33.5 (28 to 38.75) and 36 (31 to 44), in the PT and T groups, respectively. ICCs are presented in the table.
CONCLUSIONS:
There appears to be poor agreement between the STAI and other scales designed to measure anxiety in children nine to 17 years of age presenting to the ED. These scales cannot be used to measure anxiety until they are as well validated as the STAI.
Table 1).
| ICC (95% CI) | |||
|---|---|---|---|
| VAS | Likert | FAS | |
| Pre-teens Anxiety State | 0.43 (0.16, 0.62) | 0.30 (−0.04, 0.53) | 0.34 (0.02, 0.56) |
| Pre-teens Anxiety Trait | 0.38 (0.07, 0.58) | 0.17 (−0.24, 0.44) | 0,16 (−0.24, 4.44) |
| Teens Anxiety State | 0.59 (0.39, 0.72) | 0.20 (−0.19, 0.46) | 0.24 (−0.13, 0.49) |
| Teens Anxiety Trait | 0.64 (0.46, 0.76) | 0.17 (−24, 0.44) | 0.19 (−0.21, 0.45) |
Abstract
BACKGROUND:
Fever as a chief complaint is one of the common presenting problems for the pediatric patient in the emergency department. Although previous studies have demonstrated reliability in mothers’ tactile fever assessment, there are no studies that have investigated the reliability of such measurement in fathers.
OBJECTIVES:
The objective of this study was to assess the reliability of fathers compared to mothers at detecting fever by palpation in their children.
DESIGN/METHODS:
With Hospital Ethics Board approval, the inclusion criteria consisted of children zero to four years of age with both parents, and in stable condition, presenting to the emergency department with a complaint which included fever. After consent, parents were separated and blinded to one another. In addition to being asked for their demographic information and their usual methods of fever determination, each parent was also asked if their child currently had a fever, and if so, asked for an estimate of the temperature. Emergency department nurses then obtained a rectal temperature with consent.
RESULTS:
A total of 435 parents submitted complete forms. Sensitivity and specificity of mothers in identifying ‘any fever’ in their child by palpation were 84.5% and 44.9% respectively, and for fathers, 89.1% and 35.4%. For fevers greater than 39°C in triage, mothers’ sensitivity and specificity in assigning a fever greater than 39°C by palpation were 48.4% and 76.5% respectively, and for fathers, 47.4% and 65.4%. In this latter category, fathers’ specificity of assessment of fever greater than 39°C was significantly lower (P<0.05). As well, in both ‘any fever’ and fever greater than 39°C categories, unemployed participants were significantly inferior in their assessment compared to those working 20 to 60 h/week; odds ratio of 0.50 and 0.53 respectively.
CONCLUSIONS:
Fathers’ specificity assessment of ‘high’ fevers was poorer compared to mothers’ assessment. Furthermore, in groups of unemployed persons, regardless of degree of fever, this group performed inferiorly. Treating the description of tactile fevers as any diagnostic test, sensitivities greater than 80% by fathers and mothers indicates palpation to be a fairly good screening test. Therefore, dismissing a parent’s report of fever by palpation is misguided.
Abstract
BACKGROUND:
Pediatric mental health emergencies constitute a significant and growing proportion of overall visits to pediatric emergency departments (PEDs), as demonstrated by American studies. However, there is little published data on the utilization of PEDs by patients with mental health issues in Canada.
OBJECTIVES:
To describe the trends in utilization of PED resources by mental health patients over the last 10 years at the British Columbia Children’s Hospital (BCCH). We primarily reported the number and acuity of mental health related visits, their length of stay (LOS), admission rate and return visits, relative to all PED visits.
DESIGN/METHODS:
We conducted a retrospective cohort study of PED visits at BCCH from 2003 to 2012. All visits with chief complaints or discharge diagnosis including terms related to mental health disorders were selected for evaluation. Descriptive statistics were used to summarize our findings.
RESULTS:
We observed a 38% increase in the number of pediatric mental health presentations compared to a 9% increase in the number of total visits to the PED over the study period. Repeat visits represented a significant proportion of all mental health related visits to the ED. Yearly, 31% to 36% of all mental health related visits were repeated visits, a third of those occurring within 30 days from the index visit. Moreover, while the proportion of visits for mental health concerns triaged to a high acuity level has steadily decreased, the proportion of visits triaged to the mid-acuity level has steadily increased. Mean LOS in the ED for mental health patients increased from 295 min in 2003 to 318 min in 2012. These LOS are significantly longer then for overall visits to the ED (171 min in 2003; 234 min in 2012). We also observed that the number of PED visits for a psychiatric concern resulting in an admission has increased by 50% between 2003 and 2012.
CONCLUSIONS:
Mental health related visits represent a significant and growing burden for the ED at a tertiary care PED. The largest proportion of psychiatric related visits are now triaged to mid-level acuity, possibly reflecting a shortage of community mental health services. These results highlight the need to reassess health resource allocation to ensure optimal care for children affected by mental health illnesses and to consider alternative ways to optimize risk assessment as well as improving the linkage to mental health services upon disposition from the PED.
Abstract
BACKGROUND:
Pain control in pediatric emergency department (PEDs) is often suboptimal, but quality improvement (QI) initiatives to change healthcare providers’ practices are often fraught with difficulties.
OBJECTIVES:
To develop a multidisciplinary team approach to the management of pain in a PED, in order to improve procedural pain control.
DESIGN/METHODS:
In spring 2013, an interdisciplinary group of ED staff (nurses, physicians, administrative) from a tertiary care pediatric university hospital was created to explore pharmacological and non-pharmacological opportunities to improve pain relief in ED patients. Frequent, brief meetings – in collaboration with hospital pharmacists, pain management researchers, and the hospital’s pain team - allowed for the identification of barriers to pain management, areas needing improvement and easy, low-cost solutions that would be acceptable with minimal staff resistance. To assist these practice changes, one nursing team was identified as test group, facilitating feedback about chosen methods and enhancing both the pain team’s and the staff’s capacity to adapt to barriers to implementation. During the trial period, structured written feedback (quantitative and qualitative) was provided for every intervention to guide choices. Training regarding new approaches was then provided to all PED physicians and nurses. Venipuncture was chosen as the first QI initiative.
RESULTS:
The table presents achieved practice changes to reduce procedural pain during venipuncture (six months after pain team’s creation). The topical anesthetic was chosen based on literature review but also on written comments from nursing staff regarding pain control efficacy, loss of vascular anatomy and ease of use.
CONCLUSIONS:
Using an interdisciplinary approach to pain management methods allowed for the development of creative, realistic, low-cost and achievable goals in a short time span. Also, implementing the project progressively allowed for constant, immediate feedback and adjustments. Such working models could be used to create various clinical guidelines and to facilitate actual practice changes.
Table 1).
Changes of practice to reduce procedural pain during venipuncture in a PED
| Implemented changes |
|---|
|
Abstract
BACKGROUND:
Despite a plethora of review and guideline literature in anaphylaxis, there is a paucity of randomized controlled trials examining the efficacy of pharmacological treatment. Consequently, there is wide variability in prescribing patterns and adherence to published guidelines.
OBJECTIVES:
The objective of this study was determine if the use of epinephrine, corticosteroids or antihistamines affect rates of biphasic reactions in patients presenting to the emergency department (ED) with anaphylaxis.
DESIGN/METHODS:
We searched Medline (1946 to September 2013) and EMBASE (1974 to September 2013) using a peer-reviewed search string to identify original, English-language studies describing pharmacological intervention for patients of all ages presenting to the ED with anaphylaxis. Exclusion criteria included single case reports, review articles, or treatment not reported. The primary outcome was the association of pharmacological treatment with biphasic reaction. Secondary outcome was the adherence to recommended guidelines for the use of pharmacotherapy in anaphylaxis.
RESULTS:
Of 1424 citiations, 1153 remained after removal of duplicates. After dual review, 35 observational studies remained. Twenty-seven studies were inlcuded in qualitative analysis, and seven studies were included in meta-analysis (pooled n=1471).
Qualitative analysis revealed that current anaphylaxis guidelines are not being followed, regardless of population age or location. Corticosteroids and antihistamines are consistently prescribed more often than epinephrine. Meta-analysis revealed no significant association between of any of the medications studied and biphasic reactions.
CONCLUSIONS:
Minimal evidence supports the use of adjunctive therapy to prevent biphasic reaction for anaphylaxis. There is poor application of existing guidelines for the use of epinephrine in anaphylaxis, highlighting a role for further knowledge translation. Prospective, controlled clinical trials are needed to determine the role for adjunctive medications (corticosteroids, antihistamines) in anaphylaxis.
Abstract
BACKGROUND:
Since concussions commonly occur during play/sport, parents may have a key role in advocating for sport removal and assessment by a physician. However, information on parental knowledge of recognizing and understanding concussion is currently very limited.
OBJECTIVES:
We determined how frequently parents knew that a concussion represented brain injury without associated bleeding. We also examined parental awareness of symptoms after head injury that may be related to a concussion, appropriate actions if concussion is suspected, and return-to-play guidelines
DESIGN/METHODS:
Parents of children five to 18 years of age presenting to a pediatric emergency department within two weeks of a head injury were asked to participate in a 24-item questionnaire. Survey questions were derived and validated using expert opinion, available literature, and pre and pilot testing of questions on the target audience.
RESULTS:
Of 674 eligible parents, 507 (75.2%) were enrolled. Of these, 342 (67.5%) were female, 411 (81.1%) were 31 to 50 years of age, 435 (85.8%) had post-secondary education, and 77 (15.2%) reported a history of concussion. Importantly, 288 (57.4% [95% CI 53.1% to 61.7%]) parents correctly identified concussion as non-hemorrhagic brain injury, and 414 (82.5%; [95% CI 79.2% to 85.8%]) were aware of short and long-term symptoms after head injury that may be related to concussion. There were no parental demographics that were significantly predictive of concussion knowledge. Of the respondents, 40.0% believed their child’s current head injury may be a concussion, while physician diagnosed concussions for this population’s was 29.3% (P=0.45). The inter-rater agreement between physicians and parents in labeling the child’s head injury as a concussion was poor, kappa = 0.011. If a parent thought their child had a concussion, 460 (91.5%) would appropriately stop the child’s play and see a physician. Although 502 (99.0%) understood that a concussion would lead to restricted activities for the child, only 147 (29.0%) were familiar with return-to-play guidelines.
CONCLUSIONS:
Many parents were aware that a concussion is a type of non-hemorrhagic brain injury. Further, most knew the symptoms after head injury that may be associated with a concussion, and the appropriate actions to take once this injury is suspected. However, an early physician visit is recommended to provide families with an assessment for correct diagnosis and educate families on appropriate anticipatory guidance and follow up for this injury.
Abstract
BACKGROUND:
Elbow injuries are common in children and adolescents accounting for 3% of total emergency room visits. The elbow extension test alone has not been shown to reliably exclude the presence of fractures in pediatrics, thereby most children are referred for a diagnostic elbow x-ray.
OBJECTIVES:
Determine whether the combination of point tenderness and the elbow extension test improves the diagnostic accuracy for pediatric elbow injuries requiring immobilization.
DESIGN/METHODS:
Prospective observational study of patients less than 18 years of age with acute elbow injuries presenting to a tertiary care pediatric emergency department. Patients were managed according to the discretion of the treating physician with imaging and immobilization. The index test was defined as positive if elbow tenderness was present at one of five locations or had incomplete extension of the injured elbow. The assessment was performed by attending physicians or senior residents (≥PGY-3) and inter-observer reliability was assessed on ∼10%. The radiologist’s report of the radiographs or, for those without radiographs, a diagnosis of a missed fracture after a structured follow-up phone call one week post-injury was used as the reference standard for the diagnosis of a fracture and/or elbow effusion.
RESULTS:
A total of 2331 patients were screened with elbow injuries; 1380 excluded (66% pulled elbow, 22% referred in, 7% obvious deformity, 2% uncooperative with exam, 2% polytrauma and 1% other). Amongst the 951 eligible patients, a research assistant recruited a convenience sample of 43%. The mean age was 8.8±4.1 years and 52% male. Of the 334 recruited patients, 97.9% had radiographs and 186 (57%) were diagnosed with an elbow injury requiring immobilization (75.3% had a fracture, 24.7% an isolated effusion). A positive index test was present in 302 (90.4%) and had a sensitivity and specificity of 95.6% (95% CI 91.0% to 98.1%) and 16.9% (95% CI 11.1% to 24.7%), respectively. In comparison, elbow extension alone had a sensitivity and specificity of 82.1% (95% CI 75.1% to 87.5%) and 62.3% (95% CI 53.3% to 70.5%), respectively. Inter-observer reliability assessed on ∼10% was excellent (kappa of 1 for index test and 0.86±0.09 for elbow extension test). Diagnostic accuracy for elbow fractures as the reference standard (ie, not isolated effusions) revealed a sensitivity of 99.2% (95% CI 97.7% to 100.7%) and specificity 16.3% (95% CI 10.5% to 22.0%). Subgroup analysis revealed similar trends for children younger than three years of age.
CONCLUSIONS:
The addition of point tenderness to the elbow extension test improves the sensitivity for the detection of elbow injuries requiring imaging and immobilization, but at a significant decrement of specificity. Future studies are needed to determine how to improve the detection of injuries requiring immobilization from those who can forego any further diagnostic tests.
Abstract
BACKGROUND:
Pain is a component of up to 80% of all emergency department (ED) visits. Oligoanalgesia, the under-treatment of pain, is a recognized problem in the ED and can have numerous detrimental effects for the pediatric patient.
OBJECTIVES:
Surveying emergency medicine residents, our primary objectives were to describe a) the extent and type of training received in pediatric acute pain management, b) their management approach to common painful pediatric presentations, c) their level of comfort in assessing and treating acute pain, d) their perceived facilitators and barriers to optimally managing pain, and e) their attitudes towards managing such pain in the ED.
DESIGN/METHODS:
A descriptive, cross-sectional survey was administered to all Royal College Emergency Medicine (EM) and Pediatric Emergency Medicine (PEM) residents, the Canadian College of Family Physician’s EM residents, Clinical Fellows and PEM Fellows at three Canadian universities. A novel survey tool was created and distributed from May to June 2013. Surveys were completed online, using a modified Dillman approach.
RESULTS:
Our response rate was 46% (56 of 122). Forty-five percent (25 of 55) of residents had not received any training for pediatric pain assessment. All years of residents were uncomfortable with the assessment of pain in 0- to 2-year-olds (P=0.07). For patients aged two to 12 years, level of comfort with pain assessment increased with years of training (P=0.02). When assessing pain in children with disabilities, 83% (45 of 54) of residents were ‘extremely’ or ‘somewhat’ uncomfortable; 65% (47 of 55) of residents had not received any training on how to assess pain for such patients. Sixty-nine percent (38 of 55) of residents had received training on how to treat pediatric pain. All residents were more comfortable using pain medication for a nine-year-old, as compared to a one-year-old (oral oxycodone P=0.00003, oral morphine P=0.00002, IV morphine P=0.004). Ninety-eight percent (54 of 55) of residents felt that it was ‘extremely’ or ‘somewhat’ important to receive education about pediatric pain management. Their preferred methods to learn children’s pain management were through role modeling (61%) and lectures (57%). Top challenges to optimal pediatric pain management were non-verbal patients, patients with disabilities, and young infants.
CONCLUSIONS:
Pediatric pain management education is important to EM residents. Residents recall receiving sub-optimal training on this important topic. They are especially uneasy in the management of younger children and those with disabilities. This study’s findings can be used to inform post-graduate curriculum planning, in order to optimize pediatric pain assessment and treatment education.
Abstract
BACKGROUND:
Soft tissue neck radiographs (STNRs) are viewed as a helpful tool to investigate causes of acute upper airway obstructions (AUAO) among children. Some findings on STNR guide clinicians in identifying life-threatening causes of AUAO such as epiglottitis, retropharyngeal abscess or foreign body aspiration.
OBJECTIVES:
Do the clinicians are skilled enough to recognize those radiologic signs?
DESIGN/METHODS:
A retrospective, observational study was conduct to examine STNR use in the pediatric population. The medical files from children aged 0 to 17 who had a STNR between January 1, 2010 and December 31, 2011 in Canadian university pediatric hospital were reviewed. STNRs were identified using the hospital electronic radiologic studies database. From all STNRs, only those performed in an AUAO context were analyzed. We collected data about clinicians’ (emergency physicians, pediatricians, ENT specialists) and radiologists’ interpretations. Identification by clinicians of significant findings on STNRs related to life-threatening causes of AUAO (swollen epiglottis or aryepiglottic, swelling of the retropharyngeal space, decrease tracheal diameter/tracheal deviation, and presence of a foreign body) were compared to radiologists’ reports (gold-standard) to establish their global and individual sensibility and specificity. Kappa coefficients were determined to describe inter-rater agreement on SNRT findings, with scores >0.75 depicting excellent agreement, 0.40 to 0.75 fair to good, and <0.40 poor. The frequency at which SNRTs were described as technically inadequate by radiologists was also analyzed.
RESULTS:
Among 457 STNRs intended to evaluate AUAO among children, 11% (n=52) showed significant findings of life-threatening causes of AUAO according to clinicians, compared to 17% (n=77) according to radiologists (global sensibility=35%, specificity=93%; kappa=0.327). Respectively, sensibility and specificity vastly differed according to signs evaluated: 26% and 97%, kappa=0.27 for swollen epiglottis/aryepiglottic edema (n=23 according to radiologists); 37% and 96%, kappa=0.37 for swelling of the retropharyngeal space (n=38); 0% and 99% kappa=−0.01 for decrease tracheal diameter/tracheal deviation (n=16); 100% and 99%, kappa=0.86 for the presence of a foreign body (n=3). Moreover, 15% of SNRTs were described as technically inadequate by radiologists.
CONCLUSIONS:
Overall, the identification of life-threatening causes of AUAO on STNRs in the pediatric population appears quite challenging for clinicians. Furthermore, SNRTs are technically difficult to perform among children. Some radiological findings seemed easier to identify. Owing to those difficulties, physicians’ training in interpreting SNRTs and the importance of STNRs in evaluating AUAO among children need to be reassessed.
Abstract
BACKGROUND:
Among industrialized countries, age at menarche (AAM) declined until cohorts born mid-20th century, likely due to improvements in socioeconomic conditions and population health. In China, extensive economic reform during recent decades may have impacted AAM.
OBJECTIVES:
To examine secular trends in AAM in southeast China.
DESIGN/METHODS:
AAM data were retrospectively collected from 1,167,119 Han Chinese women born between 1955 and 1985 who registered in the Perinatal Health Care Surveillance System during 1993 and 2005. Trends in AAM by birth year were estimated using multivariable linear regression for all women and separately within 10-year birth cohorts.
RESULTS:
Mean AAM declined from 15.7 to 14.7 years for women born 1955–60 and 1981–85, respectively. The overall rate of decline was −0.33 (95% CI −0.33 to −0.32) years per decade after adjustment for urban/rural residence region, education and age at registration. AAM declined faster among urban women born 1955–65, but faster among rural women born 1976–85, and greatest among women with the lowest level of education born 1966–75 and 1976–85. Among every residence and education subgroup, the rate of decline was slower within the 1976–85 than 1966–75 cohort.
CONCLUSIONS:
Conclusions: Mean AAM declined for women born in 1955–85 in southeast China. Further study is warranted to evaluate the impact of socio-economic development on AAM, as well as health outcomes associated with earlier AAM in China.
Table 1).
Changes in age at menarche in the overall birth cohort and in each 10-year birth cohort by region and education for women born in southeast China between 1955 and 1985. a Adjusted for residence, education and age at registration; b Adjusted for education and age at registration; c Adjusted for residence and age at registration; Significant P<0.05 interactions detected between residence and birthyear for women born 1955–65, 1976–85, and overall 1955–85. Significant P<0.05 interactions detected between education and birthyear for women born 1966–75,1976–85, and overall 1955–85.
| 1955–65 | 1966–75 | 1976–85 | |
|---|---|---|---|
| Coef.(95%CI) | Coef.(95%CI) | Coef.(95%CI) | |
| All a | −0.038(−0.046,−0.030) | −0.043(−0.045,−0.042) | −0.032(−0.034,−0,031) |
| Residence b | |||
| Rural | −0.038(−0.046,−0.029) | −0 044(−0.046,−0.043) | −0.033(−0.035,−0.032) |
| Urban | −0.044(−0.068,−0.019) | −0.040(−0.044,−0.036) | −0.028(−0.033,−0.023) |
| Education c | |||
| High school or above | −0.061(−0.084,−0.037) | −0.036(−0.040,−0.033) | −0.027(−0.030,−0.023) |
| Middle school | −0.040(−0.052,−0.028) | −0.043(−0.045,−0.041) | −0.035(−0.037,−0.032) |
| Primary school or less | −0.030(−0.042,−0.019) | −0.050(−0.054,−0.047) | −0.047(−0.054,−0.040) |
Abstract
BACKGROUND:
Every year between 4000 and 5000 adolescents are placed in Quebec Youth Protection Centers (YPCs). Many of these adolescents use psychotropic substances that impact their mental and physical well-being.
OBJECTIVES:
To document the prevalence of tobacco, alcohol and drug use among youth residing in YPCs and to identify factors associated with problematic substance use (PSU) among these adolescents.
DESIGN/METHODS:
Between July 2008 and May 2009, adolescents aged 14 to 17 and living in six YPCs across Quebec were recruited on a volunteer basis to participate in a second generation surveillance study on risk behaviours and prevalence of sexually transmitted infections. Data on socio-demographics, substance use and sexual risk behaviours, and certain associated health conditions were obtained by questionnaire during structured, face-to-face interviews. Analyses were carried out on the profiles of participants identified with PSU (measured using the standardized “DEP-ADO” screening tool). Multivariate logistic regression was used to identify correlates of PSU.
RESULTS:
Of the 578 participants interviewed, 499 youth who had been living in YPCs for less than two years were kept in the analyses to improve reliability of data collected for the year prior to admission (59% boys; median age: boys, 16; girls, 15). During that year, the prevalence of regular substance use (3× weekly and +) was: tobacco, 75%; alcohol, 24%; cannabis, 63%; amphetamines, 17%; and cocaine, 4%. Almost one-third of girls (31%) and one-fifth of boys (21%) reported a first episode of regular use of alcohol before 14 years of age, while 50% of girls and 41% of boys reported a first episode of regular drug use before that age. PSU, measured by “DEP-ADO” and indicating a need for specialized professional intervention, was documented for 58% of girls and 63% of boys. Only 18% of these youth had received therapy for their problematic consumption. In multivariate analysis, factors associated with adolescent PSU were daily use of cigarettes (AOR 6.40 [95% CI 3.90 to 10.48]); precocious use of alcohol (3.99 [95% CI 2.41 to 6.62]); family history of problematic substance use (2.37 [95% CI 1.32 to 4.25]); having at least six sexual partners (lifetime) (3.26 [95% CI 2.00 to 5.31]); and a history of self-mutilation (lifetime) (1.88 [95% CI 2.11 to 3.16]).
CONCLUSIONS:
Substance use is prevalent among adolescents entering YPCs and certain factors are associated with problematic use. Youth with these risk factors merit early and on-going substance use screening by health professionals. Timely detection and referral of adolescents with PSU for therapy may help prevent associated health consequences and decrease their risks of developing life-long dependencies.
Abstract
BACKGROUND:
Studies in adults have shown a correlation between the number of adverse childhood experiences (ACE) and an increasing risk of mental health issues, substance abuse, suicide and premature death. However, there are few data on the impact of ACEs on the health status of teenagers. Moreover, youth living in custodial facilities represent an especially at-risk group.
OBJECTIVES:
To evaluate if there is a correlation between the number ACEs and the health status of teenagers in custodial facilities.
DESIGN/METHODS:
This is a secondary analysis from a cross sectional health evaluation study of youth in custodial facilities that took place in 13 facilities in Quebec in 2011 to 2013. A total of 315 teenagers 14 to 17 years of age were evaluated by a nurse/doctor shortly after admission using a comprehensive standardized data collection form/check list. We identified seven ACEs: single parent family, violent death of a family member, family history of incarceration/mental health issues/substance abuse and personal history of physical or sexual abuse before 13 years old. CHI square analysis were performed between the number of ACEs and a number of relevant variables.
RESULTS:
94% of girls and 91% of boys had at least one ACE and 39% of girls and 25% of boys had ≥4 ACEs. More youths who had an increased number of ACEs evaluate their health status as being worse (P<0.03), had a history of mental health issues (P<0.00), ADHD (P<0.04), learning disabilities (P<0.2), had at-risk sexual behaviors (girls, P<0.04; boys, P<0.003), had psychosomatic symptoms (P<0.002), respiratory problems (girls, P<0.04; boys, P<0.01) and dental problems (P<0.05). More boys with higher number of ACEs had oral and vaginal sex before 13 years of age (P<0.01), were more prone to engage in violent behavior, ie, frequent threats of harming (P<0.014), frequent threats of taxing (P<0.02); while more girls had personal history of having sex for money (P<0.04), STI (P<0.05), suicidal attempts (P<0.03) and expressed more need for mental health consultation (P<0.01).
CONCLUSIONS:
The results of the study confirm that increased adverse experiences in childhood are associated with increased health problems during adolescence for youth in custodial facilities. This shows the importance of not only asking about ACEs, but to consider their cumulative impact. For teenagers with more than three ACEs, services should be intensified in order to avoid their negative impact.
Abstract
BACKGROUND:
Little attention has been paid to minimizing pain during childhood vaccination which is the most frequent adverse event following immunization. This lack of pain management exposes children to unnecessary suffering and the potential for long-term consequences, such as needle fears and healthcare avoidance behaviours. Vaccination pain negatively affects parents, nurses and physicians as well; all are uncomfortable seeing children being vaccinated and may be non-compliant with immunization schedules in an attempt to reduce the burden of pain. To address this important care gap between what we know about pain and pain management during vaccine injections and what we do, an inter-disciplinary team, Help ELiminate Pain in KIDS Team (HELPinKIDS) was convened in 2008.
OBJECTIVES:
Identify relevant stakeholders involved in childhood vaccination.
Increase awareness of the need to manage pain.
Produce knowledge syntheses of evidence-based pain management interventions.
Develop a national clinical practice guideline.
Develop educational tools (videos and pamphlets) for clinicians and parents.
Integrate information about pain in national immunization education and processes of care.
Measure impact on health care delivery.
DESIGN/METHODS:
A mixed methods approach was used:
Focus group interviews
Individual interviews
Quantitative surveys
Systematic reviews
Guideline creation
Observational studies
Randomized trials
RESULTS:
HELPinKIDS has provided evidence-based knowledge synthesis and practice tools (a clinical practice guideline (CPG) and educational videos and pamphlets) to assist in the development of national and regional immunization policies and education. Outcomes that reflect the implementation of best practices for vaccine pain management include: 1. 60% increase in utilization of new analgesic strategies by public health nurse immunizers (49.8% at baseline vs. 77.6% post-CPG implementation: n=2239). 2. 60% increase in utilization of new analgesic strategies by parents after reading pamphlet (10% control vs. 16% intervention: n=436). 3. 100% increase in utilization of any of the most effective analgesic strategies (breastfeeding, topical anesthetics, or sugar water) by parents after education in prenatal class (17% control vs. 34% intervention: n=174). 4. 5% increase in H1N1 vaccination by hospital employees after provision of analgesia (n=392).
CONCLUSIONS:
HELPinKIDS has had a measurable impact on what we know about pain and the implementation of pain management during vaccine injections and will expand a wide-reaching and comprehensive knowledge translation strategy to continue to address these issues.
Abstract
BACKGROUND:
Regular physical activity (PA) promotes optimum health and development. Youth with chronic pain are less physically active than healthy peers. Recommendation by a health care provider is a key factor influencing the decision to initiate a regular program. The Canadian Paediatric Society provides general fitness guidelines and some disease-specific recommendations. Little is known about PA prescribing behaviors of paediatricians working with children and youth with chronic pain.
OBJECTIVES:
Describe PA prescribing behaviors of paediatricians for children and youth with chronic pain. Examine patient/provider characteristics that influence PA prescribing.
DESIGN/METHODS:
Ethics approval was obtained. The survey was developed on FluidSurveys. A survey link was distributed to 360 paediatricians on the Canadian Paediatric Society Community Paediatrics listserv. Ten vignettes varied on eight factors (age, sex, income level, pain intensity, pain frequency, pain duration, location and current physical activity participation). No vignette patient achieved recommended PA levels and all were safe to increase PA. Analysis included descriptive analysis and Generalized Estimating Equations with confidence as the dependent.
RESULTS:
Eighteen paediatricians participated, providing 122 completed vignette responses; 67% of participants were female, 50% of participants indicated they were regularly active, 78% worked in a unidisciplinary setting. The mean duration of practice was 17 years. Paediatricians recommended the following activity for vignette patients with chronic pain: restrict or reduce PA (2.5%), continue current level (13.1%), general activity increase recommendations (26.2%), specific advice to increase (27%), refer to other provider for advice on increasing level (31.1%). Paediatricians (n=121) had the following level of confidence in their recommendations: 2.5% were not at all confident, 38.8% were not so confident, 47.1% were confident and 11.6% were highly confident. Paediatricians (n=119) had the following level of confidence that their recommendations would be followed: 9.8% were not at all confident, 41% were not so confident, 34.4% were confident and 12.3% were highly confident. Factors significantly associated with confidence in PA prescribing included regular physician PA practices (P=0.035), multi-disciplinary setting (P=0.014) and fewer years of practice (P=0.024).
CONCLUSIONS:
Most participants’ recommended increased PA. Higher physician activity level, multidisciplinary practice and fewer years in practice were associated with increased confidence in recommendations. Development of supports such as educational material or clinical decision tools for PA prescribing for children and youth with chronic pain may benefit community paediatricians and their patients.
Abstract
BACKGROUND:
Acute kidney injury (AKI) is a frequent complication following cardiopulmonary bypass in pediatric patients. The pediatric Risk Injury Failure Loss End-stage renal disease (pRIFLE) definition based either on a serum creatinine increment (SCr) or on low urine output (UO) threshold, is now used to stratify patients with AKI. However, it is not clear if these two criteria identify the same patients.
OBJECTIVES:
Therefore, we wish to verify the concordance of the pRI-FLE UO and SCr criteria, the latter used as gold standard, to identify patients with AKI.
DESIGN/METHODS:
This retrospective single-center study included patients zero to 18 years of age who underwent cardiac surgery with cardio-pulmonary bypass between May 2009 and 2011. Exclusion criteria were death during surgery, preoperative chronic kidney failure and anterior heart transplant. Data abstracted from medical records were independently verified by two observers. Patients were divided into non-AKI and AKI subgroups (AKI-Risk, AKI-Injury, AKI-Failure) using the pRIFLE SCr and UO criteria. The McNemar test was applied to show concordance between groups while Cohen Kappa coefficient was used to measure the inter-rater agreement between definitions. ROC curves were used to identify the most predictive diuresis cut-off values to predict pRIFLE SCr AKI.
RESULTS:
Among the 141 patients, 50 (36%) met the AKI group according to pRIFLE SCr Risk definition. In the AKI-Risk category, the sensitivity of the UO definition to predict SCr AKI was 36% and the specificity was 93% (McNemar P<0.0001, Kappa = 0.33). The AKI-Injury UO definition had sensitivity of 27% and 98% specificity (McNemar P=0.03, Kappa = 0.32). Finally, the AKI-Failure UO definition had sensitivity of 6% and 100% specificity (McNemar P<0.001, Kappa = 0.09). ROC curves revealed that the most predictive diuresis cut-off values to predict pRIFLE SCr AKI-Risk, AKI-Injury and AKI-Failure are 0.3 mL/kg/h for 2 h (sensitivity 50%, specificity 80%, AUC 0.70), 0.6 mL/kg/h for 12 h (sensitivity 47%, specificity 86%, AUC 0.75) and 0.6 mL/kg/h for 11 h (sensitivity 56%, specificity 84%, AUC 0.71), respectively.
CONCLUSIONS:
As shown in this study population, AKI is highly prevalent and the concordance and inter-rater agreement between UO and SCr criteria is poor. Moreover, the accepted diuresis cut-off of the pRIFLE definition may not be adequate. Hence, UO and SCr are not interchangeable criteria in patient selection for clinical studies. More studies are needed to confirm the best diuresis cut-off values.
Abstract
BACKGROUND:
Extra Corporeal Life Support (ECLS) has evolved to a standard of care in many pediatric centers, with thousands of patients supported to date. There is a lack of studies examining long-term outcomes including health related quality of life (HRQL).
OBJECTIVES:
We aim to assess the HRQL of children who received cardiac ECLS, and to compare them with a healthy sample, children with chronic conditions and children who had cardiac surgery and did not receive ECLS.
DESIGN/METHODS:
Prospective cohort study including children <5 years of age with diagnosis of cardiac disease who received ECLS at the Stollery Children’s Hospital between 1999 and 2009. HRQL was assessed using the PedsQLTM 4.0 Generic Core Scales. Analysis was performed with t-test for independent samples and multiple linear regression. Study approved by institutional health research ethics board.
RESULTS:
Ninety-eight patients received ECLS between 2000 and 2009, 50 (51%) survived and 47 children were assessed at a median age of four years. Children who received veno-arterial ECLS have significantly lower PedsQLTM 4.0 than healthy children (64.9 vs. 82.2; P<0.0001), children with chronic conditions (64.9 vs. 73.1; P=0.007), and children who underwent cardiac surgery and who did not receive ECLS (64.9 vs. 81.1; P<0.0001). Multiple linear regression analysis found an independent association between higher inotrope score in the first 24 h of ECLS, longer hospital length of stay and lower PedsQLTM 4.0 scores.
CONCLUSIONS:
Pediatric cardiac ECLS survivors showed lower HRQL than healthy children, children with chronic conditions and those with congenital heart disease who did not receive ECLS.
Abstract
BACKGROUND:
Acute kidney injury (AKI) is an important complication following cardiopulmonary bypass in pediatric cardiac surgery patients. However, its prevalence is highly variable in studies depending on the choice of AKI definition.
OBJECTIVES:
Therefore, we aim to describe the epidemiology and outcome associated with AKI according to the accepted pediatric Risk Injury Failure Loss End-stage renal disease criteria (pRIFLE) in our postoperative population of pediatric cardiac surgery patients.
DESIGN/METHODS:
Patients from zero to 18 years of age admitted to our PICU after cardiac surgery with cardiopulmonary bypass between May 2009 and May 2011 were included in this retrospective cohort study. Data were abstracted from the medical records and independently validated by two observers. Exclusion criteria were death during surgery, preoperative chronic kidney failure and prior heart transplant. Patients were classified according to the pRIFLE categories of risk, injury and failure before comparing their outcomes. Descriptive analyses were based on one-way analysis of variance F-test with correction for unequality of variances when appropriate.
RESULTS:
Of the 141 patients who met the inclusion criteria, 59 met the pRIFLE definition for AKI, representing a prevalence rate of 42%. Compared to the non-AKI group, AKI patients were younger (median 0.5 [IQR 0.01 to 1.41] vs 1.8 [IQR 0.72 to 8.07] years; P<0.0001), had higher Pediatric Risk of Mortality (PRISM) scores (median 10 [IQR 8 to 13] vs 8 [IQR 6 to 10]; P<0.05), higher maximal serum creatinine levels (mean 56 μmol/L [95% CI 48 μmol/L to 63 μmol/L] vs 37 μmol/L [95% CI 33 μmol/L to 40 μmol/L]; P<0.0001), longer intensive care unit length of stay (mean 129 h [95% CI 95 h to 163 h] vs 58 h [95% CI 40 h to 75 h]; P<0.05), longer mechanical ventilation duration (mean 57 h [95% CI 26 h to 89 h] vs 21 h [95% CI 5 h to 37 h]; P<0.05) and longer duration of cardiopulmonary bypass (mean 142 min [95% CI 125 min to 159 min] vs 95 min [95% CI 85 min to 106 min]; P>0.05). One patient in each group died.
CONCLUSIONS:
AKI is highly prevalent following cardiopulmonary bypass in pediatric cardiac surgery. Increasing severity of AKI is associated with longer duration of cardiopulmonary bypass, longer intensive care unit length of stay and duration of mechanical ventilation. Specific modifiable risk factors and therapeutic approaches for AKI still need to be identified in order to prevent and treat AKI in this specific population.
Abstract
BACKGROUND:
Medically complex children are becoming a larger proportion of the inpatient population at pediatric tertiary care centers. With increasingly lengthy stays, the families of these children feel significant effects. Notably, siblings of medically complex and chronically unwell children are often not the primary focus of most families. There is a body of qualitative research that shows regardless of the underlying etiology of pathology, many siblings feel overlooked and demonstrate compromised psychosocial wellbeing. ‘Sibling Superhero Day’ at the Alberta Children’s Hospital was established to recognize and celebrate the siblings of chronically ill children.
OBJECTIVES:
Review literature surroundings the needs of siblings of medically complex children
Review reported outcomes of siblings in a variety of medical environments
Describe the execution of Sibling Superhero Day at the Alberta Children’s Hospital as a resident advocacy project
Review findings of a needs assessment survey completed by parents at the event
DESIGN/METHODS:
A survey was provided to all families who attended the event. Sample size was limited by the families attending Sibling Superhero Day.
RESULTS:
21 families completed the survey
– Siblings participating in the event ranged from three mos to 22 years
– Families attending the event had between 0 and four siblings - some families did have more than one child they considered “sick”
– 19 of 21 (90%) of respondents reported moderate to significant impact on the well sibling
– 18 of 21 (86%) felt that their family would benefit from additional programs for siblings while another child is admitted to hospital
– 8 of 21 (86%) felt that their family would benefit from additional programs for siblings in the community
– None of the respondents are accessing community therapy programs for siblings
– All respondents found Sibling Superhero Day “helpful”
CONCLUSIONS:
Sibling Superhero Day was a great success and many families appreciated the hospital community acknowledging the well siblings in these families. None of the families that participated in the event were accessing any outside resources to provide support to siblings and these families rely on in-hospital programming, though the majority felt their family would benefit from such programs.
Abstract
BACKGROUND:
The use of the Internet to search for medical and health related information is increasing and associated with concerns around quality and safety. We investigated the current use and perceptions of reliable websites for children’s health information by parents.
OBJECTIVES:
The objectives of our study were to determine:
Patterns of Internet use by parents for their child’s health information
Types of devices used to access information around child’s health
Perceived reliability of websites and cross-corroboration of information
Future uses of Internet for child’s health information
DESIGN/METHODS:
Following institutional ethics approval we conducted a survey of 146 parents/guardians of children presenting for day surgery with a 95% CI and 8% margin of error. A 20-item survey instrument developed and tested by the investigators was administered. Consent for participation in the study was implied by completion of the survey. Descriptive statistics were used to summarize the data.
RESULTS:
The majority (143 of 146 [98%]) of parents/guardians used the Internet to search for information around their child’s health. Eighty percent of respondents reported using public search engines as their first resource while less than 20% used university/hospital based websites (Figure 1). Common conditions such as colds/flu, skin conditions and fever were the most frequently searched and unique conditions directly affecting the child were second (Figure 2). Despite low usage levels of university/hospital based websites for child’s health information, the majority of parents/guardians (74%) regarded these as providing safe, accurate and reliable information. In contrast, only 24% of respondents regarded public search engines as providing safe and reliable information. Interestingly 50% of parents/guardians cross-checked information found on the internet with the family physician.
CONCLUSIONS:
An unprecedented majority of parents/guardians are using the internet for their child’s health information. Of concern is that parents/guardians are currently not using reliable and safe sources of information. Health care providers should begin to focus on improving access to safe, accurate and reliable information for parents and guardians through various modalities including education, design for multiplatform and incorporation of ‘safe seals’ and better search engine optimization.
Figure 1).
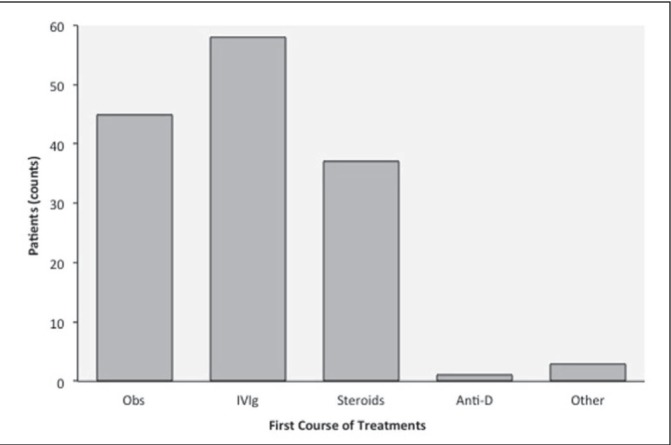
Figure 2).
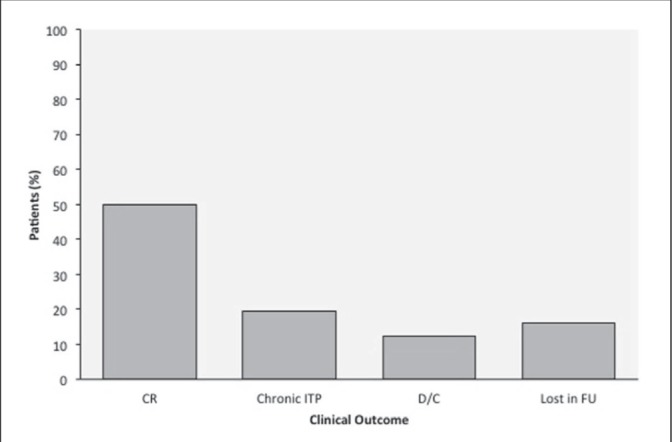
Abstract
BACKGROUND:
Medical educators are challenged to integrate new strategies to prepare future pediatricians with the necessary skills to address health disparities (Ford-Jones et al, 2008). In response, the Social Pediatrics Research Summer Studentship (SPReSS) program was developed and implemented for medical students at the University of Toronto.
OBJECTIVES:
Transformative learning principles were applied to the program and curriculum design to facilitate critical reflection and learning, and as an innovative approach to program development and evaluation.
DESIGN/METHODS:
The curriculum consisted of research and clinical placements, as well as a formal seminar series. Students were asked to write a reflection describing a situation that challenged their thinking or caused them to re-evaluate previously held attitudes or perceptions. The reflections were assessed with a rubric, and the program was evaluated through thematic analysis of the reflections and an exit survey of faculty and students.
RESULTS:
The analysis revealed that students were preoccupied by their empathic responses to marginalized patients. They described feeling empowered to act as advocates and that these feelings were reinforced through assigned readings or role modeling of faculty. Students found the program both challenging and rewarding, particularly the integration of a clinical and research experience. Faculty found students to be engaged and reflective, making connections between assigned readings and practical experiences.
CONCLUSIONS:
The theory of transformative learning can be applied to medical education programs and curricula to help students identify with advocacy and develop the necessary critical reflective and advocacy skills to address health disparities. A key strategy to fostering transformative learning is the incorporation of an authentic assessment tool such as the rubric to encourage and evaluate student reflections.
Abstract
BACKGROUND:
Studies suggest that rates of anaphylaxis, the most severe form of an allergic reaction, are increasing in Pediatric Emergency Departments (PED). Significant gaps still exist regarding the prevalence, triggers and temporal trends of anaphylaxis in Canada.
OBJECTIVES:
The Cross-Canada Anaphylaxis Registry (C-CARE) was created with the primary goal of determining the societal burden of anaphylaxis in Canada; our aim was to use C-CARE to examine temporal trends in anaphylaxis rates
DESIGN/METHODS:
Over a two-year period (April 2011 to April 2013), children presenting to the PED with anaphylaxis were recruited. The treating physician documented characteristics and triggers of anaphylactic reactions using a standardized data entry form. Charts of all PED patients were reviewed to identify anaphylactic cases that were missed in prospective recruitment.
RESULTS:
Among 81,677 PED visits in Year 1, 168 anaphylaxis cases were identified (0.21%) versus 218 anaphylaxis cases among 78,650 PED visits in Year 2 (0.27%), yielding a difference of 0.06% (95% CI 0.02% to 0.12%) between the two years. The median age of anaphylaxis was 4.8 years (IQR 2.3 to 10.1 years) in Year 1 and 5.9 years (IQR 2.1 to 11.1 years) in Year 2. There was a slightly higher male predominance in cases of anaphylaxis in both Year 1 (51.8%; 95% CI 44%, 59.5%) and Year 2 (61%; 95% CI 54.2%, 67.4%). The major triggers in both years were food allergens (87.5% and 80.6% respectively) with peanut being the most predominant (29.5% and 20.6%) followed by tree nuts (15.5% and 14.8%). Severe anaphylaxis (hypoxia, cyanosis, circulatory collapse, incontinence or neurological symptoms) was found in 7.1% (95% CI 3.9%, 12.4%) of patients from Year 1 versus 3.7% (95% CI 1.7%, 7.4%) in Year 2.
CONCLUSIONS:
There was a greater rate of anaphylaxis in the second year of the C-CARE study. In both years, food allergens were found to be the most common trigger with peanuts being the most common food. These results are comparable to the increasing rates of anaphylaxis seen in other westernized countries. Future studies in the leading PED as well as in other centers are required to establish temporal trends in anaphylaxis rates, triggers and reaction characteristics.
Abstract
BACKGROUND:
Intranasal (IN) delivery is a fast and effective administration route for several medications. We recently implemented IN use of fentanyl and midazolam in the emergency department (ED) for pain control and anxiolysis during short term procedures in pediatric patients with no intravenous (IV) access.
OBJECTIVES:
This review identifies indications for IN medication use, dosing, adverse effects, and patient/family/staff satisfaction.
DESIGN/METHODS:
Patients who received IN fentanyl or midazolam in the ED between April 1st–June 1st, 2011 were identified utilizing computerized physician order entry (CPOE) and electronic medical record (EMR) data. Patient age, indication for medication, dose received, adverse effects, and discharge status were evaluated. ED staff satisfaction and patient and family satisfaction with IN medication delivery versus alternative methods were evaluated through anonymous surveys.
RESULTS:
A total of 102 patients were identified during the two-month study period. The most common indications for IN fentanyl and/or mid-azolam were to provide pain control and/or anxiolysis during abscess incision and drainage, laceration repair, IV and Foley catheter insertion. All patients receiving IN midazolam were pretreated with buffered lidocaine 1% 0.5 to 1 ml IN to prevent nasal burning associated with the concentrated (5 mg/ml) midazolam product. Midazolam demonstrated to be safe and effective at 0.2 to 0.5 mg/kg/dose (maximum dose 15 mg) and fentanyl at 2 to 5 mcg/kg/dose (maximum dose 200 mcg). The most common doses utilized were midazolam 0.3 mg/kg and fentanyl 3 mcg/kg. The majority of patients received a combination of fentanyl and midazolam, versus fentanyl or midazolam alone. Adverse effects included rash in one patient, which resolved with oral diphenhydramine, and paradoxical agitation to midazolam in one patient, which resolved with no intervention. No patients required hospital admission due to adverse effects. The majority of patients were discharged home with no complications and positive experiences, according to ED staff, patient, and family satisfaction surveys.
CONCLUSIONS:
IN fentanyl and midazolam are advantageous alternatives to oral or intramuscular (IM) pain or anxiolysis medications, particularly in the ED. With a fast onset, short duration of action, and demonstrated safety and effectiveness for pain control and/or anxiolysis, many short procedures or exams can be performed effectively and quickly without waiting for the delayed onset of action of oral or IM medications.
Abstract
BACKGROUND:
Well appearing febrile infants with viral illnesses cannot be easily distinguished from those with occult life-threatening infections by history and physical exam alone. This study sought to assess current approaches to febrile infants under six weeks of age, and determine how management is influenced by respiratory virus testing.
METHODS:
A scenario-based survey describing two hypothetical cases of febrile infants without an infectious focus aged three and five weeks was sent to tertiary care pediatric ED and hospitalist physicians at a single center. Participants were asked multiple-choice questions regarding management decisions with and without results of respiratory virus testing. Chi-square testing was used to compare proportions.
RESULTS:
Response rate was 93% (n=32 ED, 22 hospitalists). Investigations most commonly performed for both three- and five-week old infants were urine culture, urine analysis, CBC and blood culture. Lumbar puncture was performed less frequently in five-week old infants (69% vs. 98%, P<0.001), and by hospitalists compared to ED physicians (50% vs. 81%, P<0.05). Respiratory virus testing by nasopharyngeal swab (NPA) did not differ between age groups (67% in both), however hospitalists performed NPA testing more frequently than ED physicians (82% vs. 56%, P<0.05). Infant age impacted admission decisions (three- vs. five weeks; 100% vs. 72%, P<0.001), but detection of a respiratory virus did not. Overall, positive NPA decreased empiric antibiotic treatment (P<0.05). Among hospitalists, 82% would discharge five-week old infants in ≤24 h with a positive NPA and otherwise negative workup; whereas admission duration among three-week old infants was highly variable.
CONCLUSIONS:
The management of febrile infants under six weeks differs between ED and hospitalist physicians, and by infant age. Respiratory virus testing could potentially reduce empirical antimicrobial treatment and permit earlier discharge. Establishment of clinical guidelines for this patient population is warranted.
Abstract
BACKGROUND:
Integrated community case management (iCCM) involves assessment and treatment of common childhood illnesses by community health workers (CHWs). Evaluation of a new Ugandan iCCM program is needed.
OBJECTIVE:
To assess whether iCCM by lay volunteer CHWs will affect the proportions of children treated for fever, presumed pneumonia and diarrhea in rural Uganda.
DESIGN/METHOD:
A pre and post intervention study used quasi-experimental design and included comparison with a non-intervention community. CHWs in intervention areas received basic CHW training then two CHWs from each village were selected, trained and equipped to assess and treat children under five years old with fever, fast breathing and cough (presumed pneumonia), and diarrhea. Evaluation involved CHW registry analysis, retrospective review of CHW patient encounter records, and analysis of household mother surveys from intervention and control communities before and after iCCM intervention.
RESULTS:
A total of 196 CHWs (72% female, average age 36 years) received iCCM training and reported 6276 sick child assessments from April–October 2012 (average 4.6 monthly encounters/CHW), classified as 46% presumed pneumonia, 45% fever, and 9% diarrhea. 93% of treatment records were consistent with iCCM algorithm recommendations (96%, 90% and 92% for fever, pneumonia and diarrhea, respectively). Post intervention absolute proportions of children receiving (from any source by maternal report) treatment were significantly increased: antimalarial for fever (+24% intervention versus +4% control) and oral rehydration salts/zinc for diarrhea (+14% intervention versus +1% in control). A higher percentage of children had received antibiotics for pneumonia symptoms in intervention (64%) versus control communities (28%).
CONCLUSION:
In our rural Ugandan setting with limited health services, ICCM significantly increased the proportion of young children treated for malaria, pneumonia and diarrhea. ICCM involving lay CHWs is feasible here though more studies are needed to understand if and how iCCM scale up should occur, particularly to remote communities with limited human resources for health.
Abstract
BACKGROUND:
Childhood dental cavities remain a public health challenge. Although cavities are believed to be associated with low socioeconomic status, ethnic and racial minorities, single parenting, and low parental education, the relationship of breastfeeding and cavities is likely multifactorial. There is insufficient evidence to support or refute a link between breastfeeding duration and childhood dental cavities. While breastfeeding is an important and well known preventative health practice, evidence-based information on total duration of breastfeeding is lacking. The World Health Organization recommends breastfeeding up to two years or beyond. However, the age beyond two years after which breastfeeding remains beneficial is unclear. Understanding the effect of breastfeeding duration on cavities will assist parents and clinicians in choosing the optimizing total breastfeeding duration.
OBJECTIVES:
The primary objective was to determine if the total duration of breastfeeding is associated with childhood dental cavities. The secondary objective was to determine if demographic, dietary, behavioural, and life-style factors modify the relationship between total duration of breastfeeding and cavities. We hypothesized that longer total duration of breastfeeding is associated with a higher incidence of childhood dental cavities.
METHODS:
Cross-sectional study of healthy children, aged one to five years who attended well-child visits at primary care physician’s offices from September 2011 to August 2013 was conducted through the TARGet Kids! practice-based research network. Univariate and Poisson regression analyses were used to measure the association between total breastfeeding duration and childhood dental cavities.
RESULTS:
Survey and anthropometric data were collected from 2043 healthy children (median age 61.1 months) who met inclusion criteria. Longer total duration of breastfeeding was significantly associated with ECC (Incidence risk ratio [IRR] 1.023 per month [95% CI 1.018 to 1.029]; P<0.001). This association remained statistically significant after adjusting for potential confounders (IRR 1.018 per month [95% CI 1.011 to 1.025]; P<0.001). Significant covariates included older child (P<0.001), higher number of siblings (P=0.008), single parenting (P=0.003), lower birth weight (P=0.019), younger maternal age (P=0.021), bedtime bottle use (P=0.004), and lower family income (P<0.001).
CONCLUSION:
Longer total duration of breastfeeding was associated with a small but clinically relevant 2% increased risk of dental cavities per month of breastfeeding beyond one year of age.
Abstract
BACKGROUND:
Early Childhood Caries (ECC) is considered to be the most common pediatric disease. By the age of five, Québec children are reported to have up to 40% more caries than do children in Ontario or the United States. Combined efforts, including early dental visits, caries risk assessment, appropriate therapeutic interventions and preventive counseling of parents are all essential in reducing the risk of ECC. Despite the importance of early dental visits, multiple factors act as barriers to early first oral examinations. The baby dental clinic (BDC) is a novel project that was launched to overcome those barriers and address the oral health needs of inner city infants making early dental visits available in community health centre setting.
OBJECTIVES:
To assess the feasibility and efficacy of the BDC by reporting the results of the programme for its first two years
DESIGN/METHOD:
A retrospective chart review of all BDC users was conducted from September 2011 to December 2013. The feasibility metric included the number of infants referred to the clinic. The efficacy metrics included the number and type of carious lesions detected.
RESULTS:
A total of 244 infants were seen at the BDC. Most of them were referred by immunization clinics (33%), community healthcare providers (19%) and daycares (15%). A total of 58 infants had carious lesions on their first visit. The average DFMS1–4 rate was of 2.25 at the first visit. The most affected surfaces and teeth were the buccal surfaces of the upper incisors.
CONCLUSION:
The BDC was feasible and efficacious while being focused on preventive dental care. More research is needed to measure the long-term impact of early dental visits in this patient population.


