Abstract
Background:
Autologous cartilage has been widely accepted as the frame material of ear reconstruction for patients with microtia. Although rare, there are multiple complications related with the surgical reconstruction techniques. The authors performed a systematic review of the English literature of microtia reconstruction to determine significant surgical factors that are predictors of postoperative complications.
Methods:
A PubMed search using the terms “ear reconstruction” and “microtia” was conducted. Articles were screened using predetermined inclusion and exclusion criteria. Data collected included patient characteristics, surgical techniques, the incidence of all kinds of complications, and the specific postoperative morbidity. Patient cohorts were pooled, and the incidence of complications was calculated. Significant predictors such as the use of tissue expander, simultaneously mid-ear reconstruction, with/without skin graft, and different fascia coverage were analyzed by chi-square test.
Result:
Of 320 articles found, 60 met the inclusion criteria. Totally 9415 patients with microtia were analyzed in this review with 1525 cases with complications. The overall complication incidence is 16.2% in average with a range of 0–72.9%. There was no significant difference when comparing the overall complication rate between with/without preexpansion 2-stage and multiple-stage techniques or with/without mid-ear reconstruction simultaneously.
Conclusion:
Although there is little agreement in literature regarding risk factors for complications, the authors were able to demonstrate several significant predictors by systematically analyzing 60 articles. Improved knowledge of the incidence of different complications related with various surgical methods can help surgeons provide improved preoperative counseling and take measures to minimize the risk.
Autologous cartilage has been widely used in ear reconstruction for patients with microtia. According to the latest national survey of American Society of Plastic Surgeons, 91.3% of the plastic surgeons choose autologous cartilage staged reconstruction for patients with microtia.1 Although low complication rates were reported in the literature, multiple kinds of surgical technique–related complications, both at donor and recipient sites, are not uncommon. Little exists in the literature regarding the complication rate of autologous cartilage microtia reconstruction and the related risk factors. In this systemic review, we aim to (1) calculate the kinds and overall rate of complications in autologous ear reconstruction with costal cartilage and (2) identify the complication rate related with certain surgical methods, including fascia type, with/without preexpansion, and surgical stages. Salvage procedures are also listed out for different complications.
MATERIALS AND METHODS
Literature Search
A PubMed database search was conducted in March 2013 using the terms “ear reconstruction” and “microtia” as key words to identify studies in the English language published before 2013. The articles were examined, and references were screened for further relevant articles. The search yielded a total of 320 citations. Inclusion criteria were English-language publication, human subjects, ear reconstruction, extractable outcomes on complications, and full-text availability. Exclusion criteria were systematic reviews and meta-analyses, case reports and case series with fewer than 15 patients, and nonrelated with surgery (the method is also provided in other systemic review about fat necrosis in autologous breast reconstruction by Khansa et al2). Finally, 260 articles were excluded and 60 articles were reviewed and analyzed (Fig. 1).
Fig. 1.
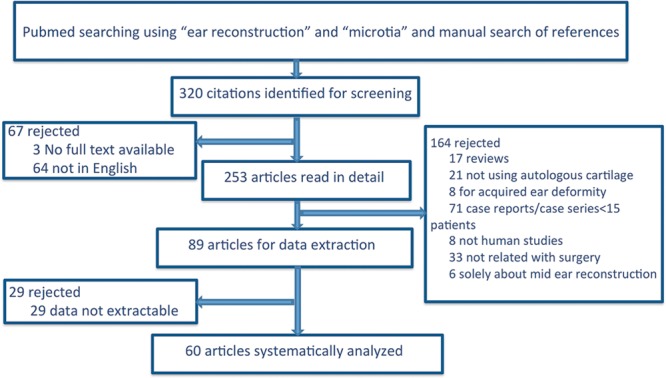
Study attrition diagram.
Data Extraction
Two authors, Yu and Huang, were responsible for evaluation of all the articles. When there is disagreement about inclusion and exclusion, the first author Long will give further evaluation and reached an agreement. The corresponding author Wang assessed the quality and validity of the extracted data finally. For each article, data listed in Table 1 were extracted. The complications according to different surgical methods were listed out and reviewed one by one including with/without expansion, with/without mid-ear reconstruction, stages of operation, and with/without fascia coverage.
Table 1.
Data Extracted from the Article
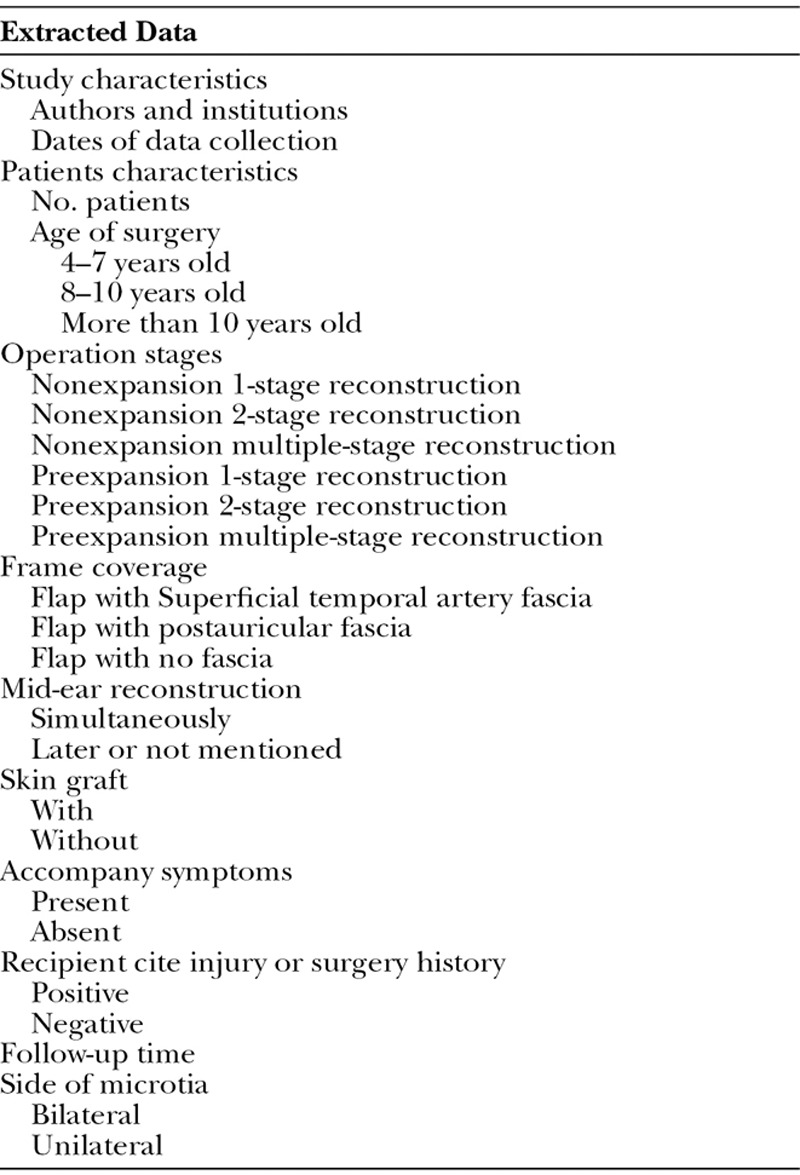
The flap types to cover the cartilage frame included nonexpanded or expanded auricular area skin. Methods to cover the postauricular sulcus include temporoparietal fascia or mastoid fascia. Surgical stages vary from 1 stage without expansion, 2 stages with expansion, 2 stages without expansion, or more stages with/without expansion.
Data Analysis and Statistics
When 2 or more articles from the same authors of the same institution had overlapping data collection dates, they were assumed to be from the same cohort. When computing the overall rate of complications, the article with the largest number of patients was included and redundant articles from the same institution were excluded. However, some of the redundant articles analyzed distinct predictors of complications, and those were included in the analysis of individual risk factor.
All articles that contained extractable data were analyzed. The data were pooled, and the number of reconstructed ear with complications was calculated according to different surgical methods. Significant predictors, such as the use of tissue expander, simultaneously mid-ear reconstruction, with/without skin graft, and different fascia coverage, were analyzed by chi-square test.
RESULTS
Complication Rate
Seventeen articles reported the total complication rate,3–19 and others analyzed the different complications separately. The incidences vary from 0% to 33%. The authors who perform ear reconstruction together with mid-ear reconstruction17 or using tissue expander during the stages reported higher overall complication rates.18,19 Among the 253 full-text available English articles, only 21 of them reported using alloplastic material in ear reconstruction. Totally 9415 patients with microtia were analyzed in this review with 1525 cases with complications. The overall complication incidence is 16.2% in average with a range of 0–72.9%, which is comparable to the average complication rate reported by US surgeons as 13.58% with a range of 1–75% according to the national survey published in 2013.1
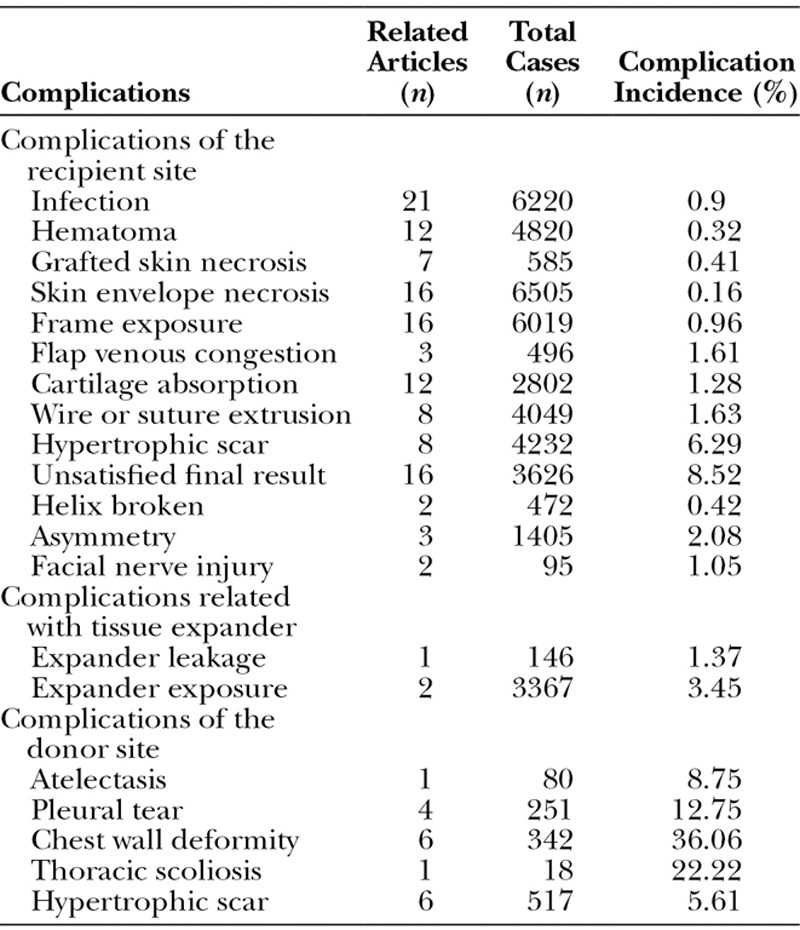
Complications of the recipient site include infection and hematoma. Still there are many plastic surgeons who prefer to use the expanded flaps to perform ear reconstruction; thus, in their series, they reported certain complications related with tissue expander, such as expander leakage or exposure. The donor site also has different kinds of complications, for example, atelectasis and pleural tear. Only 1 article published in 1971 reported a dead case due to the bronchopneumonia after cartilage harvest.20 Table 2 listed out the overall incidence of different complications separately.
Table 2.
Complications of the Recipient Site
Operation Methods
Basically, the operation methods could be divided into 2 groups: with or without tissue expansion. (1) Nonexpansion group: Most surgeons preferred 2-stage or multiple-stage ear reconstruction technique with no expansion since the article published by Brent21 and Nagata.7 Some articles focused on the donor-site complication22 or comparison of different fixation material23 did not provide information of surgical stages. No author reported 1-stage ear reconstruction within the recent 10 years. (2) Tissue expansion group: Chinese surgeons mostly reported their techniques using tissue expander in recent 5 years24–34 with the expander size varing from 50 to 90 ml. Most authors chose skin graft to reconstruct the postauricular sulcus, the concha, or the mid-ear canal. Only 3 articles using tissue expander declared that skin graft was not used at all.24,26,35 Authors of twelve articles reported their experiences of simultaneously external and mid-ear reconstruction.10–12,15,17,27,36–40 Sixteen articles reported the technique of using fascia to cover the framework, including temporoparietal fascia4,5,7,10,36,41–44 or mastoid fascia.3,17,25,30,34,45,46 Table 3 is the list of different surgical methods and the overall complication incidence. Figure 2 shows the difference between nonexpansion and expansion technique.
Table 3.
Operation Stages and Overall Complication Incidence
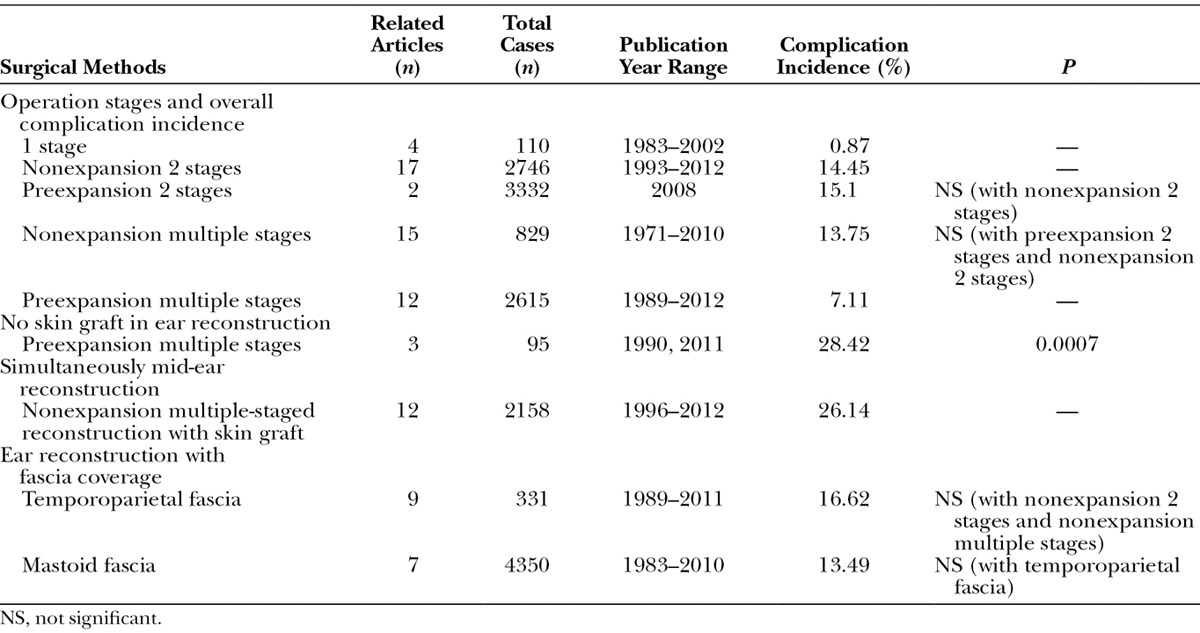
Fig. 2.
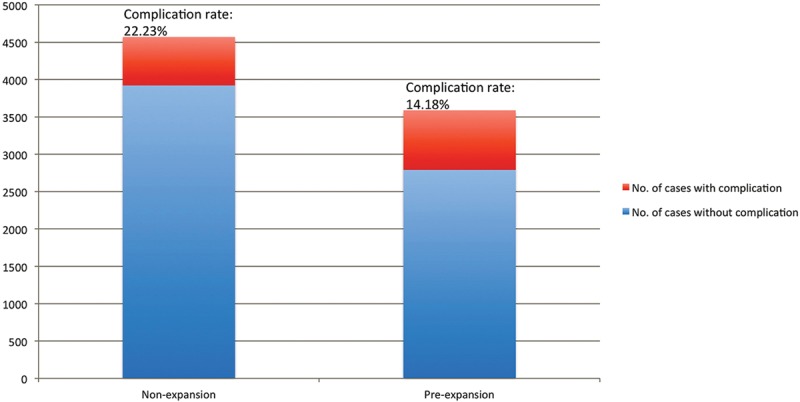
Complication rate of nonexpansion and preexpanded group.
Other Factors
Age of the first operation varies according to different authors. One early article mentioned the start of the serial ear reconstruction before 4 years old.47 Most of the others start to perform the surgery at the age older than 7 years in average,3,4,9,10,12,14,15,18,20,22,24,27,28,31,34–36,39–41,43,45,48–54 which is consistent with the US national survey published in 20131 and the international survey on the fourth International Ear Reconstruction Congress in Edinburgh.55
The average follow-up time varied from 3 months to 9.5 years. Tanzer52 published his article in 1978 with an average follow-up time as 9.5 years, which was the longest one among all the articles. Longer follow-up time is correlated with higher incidence of the late complications, such as wire extrusion and chest wall deformity. Ten articles reported clinical results, with the shortest follow-up time as 3–9 months.5,10–12,24,26,31,42,49,50
Several articles summarized the accompany symptoms of the patients with microtia, including first and second branchial arch syndrome, blind external auditory canal, treacher collins syndrome, lip and palate cleft, and facial dysplasia. Pan et al29 reported the highest incidence of facial dysplasia as 82.24% in 326 microtia cases.
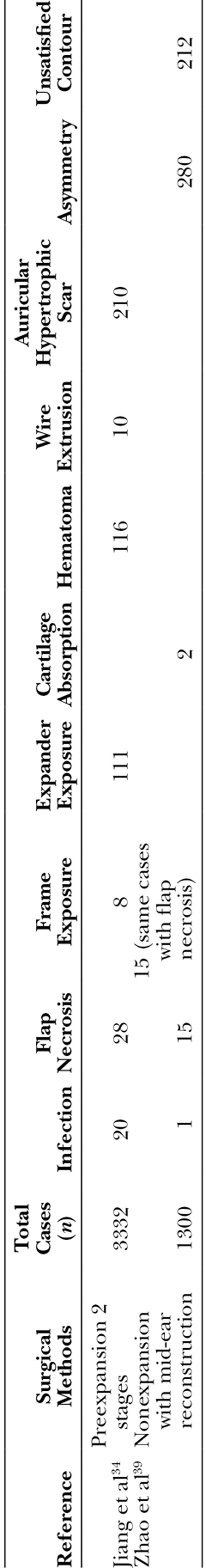
Jiang et al34 reported the largest case series of using tissue expander in 3332 patients with microtia followed by the report by Zhao et al39 about 1300 cases that received mid-ear and external ear reconstruction simultaneously. Brent9 introduced his nonexpanded multiple-staged technique of ear reconstruction for 1200 cases in 1999 and declared there was no complication. The main complications of case series reported by Jiang et al34 and Zhao et al39 are listed in Table 4.
Table 4.
Complications of the 2 Largest Case Series
DISCUSSION
Autologous cartilage staged microtia reconstruction was the most common method according to the literature. Techniques of microtia reconstruction varied among different surgeons. Tissue expander was first reported to be used in ear reconstruction in 198941 and 199035 and then followed by the only attractable data in the report by Park18 in 2000. While from 2007 to 2012, doctors from China and only from China published 11 articles that met the inclusion criteria with large case series. Although there were certain complications related with tissue expander, such as expander leakage and exposure, there was no significant difference when comparing the overall complication rate with nonexpansion 2-stage or multiple-stage techniques. The price of local produced tissue expander in China is about 40–50 dollars, which is cheap and has the advantages of creating adequate skin to cover the frame, and probably, it is the main reason of its wide acceptance by both the Chinese plastic surgeons and patients despite the time-consuming expansion technique. It is noticeable that the 3 articles mentioned using tissue expander with no skin graft in relatively small case series had significant higher complication rate when compared with the other groups (P = 0.0007).
Mid-ear reconstruction is also related with certain complications, for example, facial nerve injury and postatresiaplasty infection. However, the overall complication incidence of simultaneously mid-ear reconstruction has no significant difference when compared with the other groups (Table 3). It is still controversial whether it is necessary to perform mid-ear reconstruction for unilateral microtia.55 According to the 11 articles that reported the experience of simultaneously external and mid-ear reconstruction, most of the patients gained an improvement in hearing over 20–30 dB pure-tone average.10–12,15,17,27,36–40 According to the result, if performed with fewer operation stages and lower complication rate, simultaneously mid-ear reconstruction could be an option for microtia patients with indications including radiologic evidence of the inner ear and audiometric evidence of cochlear function.
Brent21 and Nagata7 reported their technique of microtia reconstruction separated in different surgical stages. There is no significant difference between the complication rate of 2-stage and multiple-stage microtia reconstruction without tissue expansion (Table 3). However, when using tissue expander, the overall complication incidence is much lower in the multiple-stage group than in the other groups. The main shortcomings of tissue expansion technique are the complications related with expander and the delayed extraction of the expanded flap. According to the data, tissue expansion did not increase the overall complication rate. Thus, the possible reason of the low complication incidence in this group is that the multiple stages help to avoid the delayed extraction but remain the advantage of creating more skin envelope with tissue expansion, which will finally result in better coverage of the frame and satisfied contour of the reconstructed ear.
Different surgeons use different material to fix the framework. Eight articles reported the wire extrusion rate, ranging from 0.3% to 25%.23,28,30,34,42,52,56,57 The follow-up time of these publications vary from 1 to 9.5 years. Not surprisingly, the article reported highest wire extrusion accident (25%) also had the longest follow-up time,52 but it was also the earliest article to report this complication. With the technical development in fixation material and surgical method, the incidence has dropped down dramatically. Sakamoto et al23 compared different material in cartilage frame fixation and found lowest complication rate with absorbable sutures.
Chest wall deformity can range from minor deformities to the development of scoliosis. The incidence ranged from 6.25% to 50%.22,26,33,47,52 Most of the articles did not provide the incidence of chest wall deformity as one of the complications, possibly due to the short follow-up period. Some authors reported their technique of reducing the amount of cartilage harvested or the maintenance of perichondrium to avoid future chest wall deformity.28,58 It is a noticeable problem as there was possibility of thoracic scoliosis after cartilage harvest according to the article by Ohara et al22
Eight articles reported auricular hypertrophic scar after microtia reconstruction. All of these articles are from Asian countries,17,29,30,34,51,56,59,60 which is consistent with the high occurrence of hypertrophic scar and keloid in Asian population. It was also reported by these authors that scar resection and skin graft could help to solve the auricular hypertrophic scar. Instead, authors of the 6 articles reported chest wall hypertrophic scar after cartilage harvest are from the United States,37,52 Colombia,38 Canada,47 and China.28,50 Local injection was the main way to resolve the chest wall hypertrophic scar according to these reports.
Twelve articles reported the technique in treating complications. The salvage procedures included local flap coverage34,49 or temporoparietal fascia transfer and skin graft41,46,54 for frame exposure, cartilage removal,39,48 or expander removal18,27,43 due to infection and wire or suture removal after exposure.34,52,54 Using temporoparietal fascia in the first stage of microtia reconstruction is controversial as it is a useful salvage procedure to cover the exposed cartilage frame. The overall complication incidence of using temporoparietal fascia to cover the postauricular sulcus has no significant difference when compared with the mastoid fascia group, nonexpansion 2-stage, and multiple-stage groups.
The review has some limitations. First, all the case numbers are counted as the number of patients instead of the number of reconstructed ears. As most articles reported the complications number of patients, we extracted the data of total cases in the same way. The included 60 articles totally involved 9415 patients, and there were 30 articles that mentioned the case number of unilateral or bilateral reconstruction; among these series, there were 931 bilateral reconstruction cases. Simply counting the bilateral cases as 1 patient may increase the overall complication incidence. Second, only 3 articles mentioned 86 patients with previous surgery or injury history of the recipient cite,20,44,52 which is also a factor related with high complication incidence but difficult to analyze due to the lack of data in other articles. Third, the variation of mean follow-up time may produce bias in the result as early and late complications happened at different period post operation. Also publishing bias could be one of the factors that influence the statistic results as some of the articles only provided refinements of previous techniques, which may not fully mirror the complication rate.
CONCLUSIONS
There is significant variability in the literature regarding complication rates in autologous cartilage ear reconstruction of patients with microtia. By providing a comprehensive review of different complications with different surgical techniques, this study could help plastic surgeons adequately take measures to minimize the complication rates in their future operations.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by Peking Union Medical College Hospital.
REFERENCES
- 1.Daniel DI, Boris P, David AS, et al. Current management of microtia—a national survey. Aesthetic Plast Surg. 2013;37:402–408. doi: 10.1007/s00266-012-0008-x. [DOI] [PubMed] [Google Scholar]
- 2.Khansa I, Momoh AO, Patel PP, et al. Fat necrosis in autologous abdomen-based breast reconstruction: a systematic review. Plast Reconstr Surg. 2013;131:443–452. doi: 10.1097/PRS.0b013e31827c6dc2. [DOI] [PubMed] [Google Scholar]
- 3.Tai Y, Tanaka S, Fukushima J, et al. Refinements in the elevation of reconstructed auricles in microtia. Plast Reconstr Surg. 2006;117:2414–2423. doi: 10.1097/01.prs.0000225449.04098.94. [DOI] [PubMed] [Google Scholar]
- 4.Kobayashi S, Maegawa J. Ear elevation using 2-tiered costal cartilage on the same side as the reconstructed framework. J Craniofac Surg. 2011;22:1796–1799. doi: 10.1097/SCS.0b013e31822e8006. [DOI] [PubMed] [Google Scholar]
- 5.Lim SY, Mun GH, Hyon WS, et al. The elevation of the constructed auricle with a temporoparietal fascial flap wrapping a resorbable plate. J Plast Reconstr Aesthet Surg. 2006;59:505–509. doi: 10.1016/j.bjps.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Jiang H, Pan B, Zhao Y, et al. A 2-stage ear reconstruction for microtia. Arch Facial Plast Surg. 2011;13:162–166. doi: 10.1001/archfacial.2011.30. [DOI] [PubMed] [Google Scholar]
- 7.Nagata S. A new method of total reconstruction of the auricle for microtia. Plast Reconstr Surg. 1993;92:187–201. doi: 10.1097/00006534-199308000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Yotsuyanagi T, Yokoi K, Urushidate S, et al. A supportive technique using a splint to obtain definite contour and desirable protrusion after reconstruction of microtia. Plast Reconstr Surg. 1998;101:1051–1055. doi: 10.1097/00006534-199804040-00025. [DOI] [PubMed] [Google Scholar]
- 9.Brent B. Technical advances in ear reconstruction with autogenous rib cartilage grafts: personal experience with 1200 cases. Plast Reconstr Surg. 1999;104:319–334. doi: 10.1097/00006534-199908000-00001. discussion 335. [DOI] [PubMed] [Google Scholar]
- 10.Siegert R. Combined reconstruction of congenital auricular atresia and severe microtia. Adv Otorhinolaryngol. 2010;68:95–107. doi: 10.1159/000314565. [DOI] [PubMed] [Google Scholar]
- 11.Siegert R. Combined reconstruction of congenital auricular atresia and severe microtia. Laryngoscope. 2003;113:2021–2027. doi: 10.1097/00005537-200311000-00031. discussion 2028. [DOI] [PubMed] [Google Scholar]
- 12.Siegert R, Weerda H. Two-step external ear canal construction in atresia as part of auricular reconstruction. Laryngoscope. 2001;111(4 Pt 1):708–714. doi: 10.1097/00005537-200104000-00026. [DOI] [PubMed] [Google Scholar]
- 13.Ono I. Therapeutic effect of using a long-pulsed alexandrite laser system with a cooling device for epilation in reconstructive surgery of auricular malformations. Ann Plast Surg. 2002;48:115–123. doi: 10.1097/00000637-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Brent B. Auricular repair with autogenous rib cartilage grafts: two decades of experience with 600 cases. Plast Reconstr Surg. 1992;90:355–374; discussion 375. [PubMed] [Google Scholar]
- 15.Aguilar EF. Auricular reconstruction in congenital anomalies of the ear. Facial Plast Surg Clin North Am. 2001;9:159–169. [PubMed] [Google Scholar]
- 16.Osorno G. A 20-year experience with the Brent technique of auricular reconstruction: pearls and pitfalls. Plast Reconstr Surg. 2007;119:1447–1463. doi: 10.1097/01.prs.0000258572.57161.d8. [DOI] [PubMed] [Google Scholar]
- 17.Cho BC, Lee SH. Surgical results of two-stage reconstruction of the auricle in congenital microtia using an autogenous costal cartilage alone or combined with canaloplasty. Plast Reconstr Surg. 2006;117:936–947. doi: 10.1097/01.prs.0000200612.62079.59. [DOI] [PubMed] [Google Scholar]
- 18.Park C. Subfascial expansion and expanded two-flap method for microtia reconstruction. Plast Reconstr Surg. 2000;106:1473–1487. doi: 10.1097/00006534-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Hata Y. Do not forget the fundamental merits of microtia repair using a tissue expander. Plast Reconstr Surg. 2002;109:819–822. doi: 10.1097/00006534-200202000-00071. [DOI] [PubMed] [Google Scholar]
- 20.Spina V, Kamakura L, Psillakis JM. Total reconstruction of the ear in congenital microtia. Plast Reconstr Surg. 1971;48:349–357. doi: 10.1097/00006534-197110000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Brent B. The correction of microtia with autogenous cartilage grafts: II. Atypical and complex deformities. Plast Reconstr Surg. 1980;66:13–21. doi: 10.1097/00006534-198007000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Ohara K, Nakamura K, Ohta E. Chest wall deformities and thoracic scoliosis after costal cartilage graft harvesting. Plast Reconstr Surg. 1997;99:1030–1036. doi: 10.1097/00006534-199704000-00017. [DOI] [PubMed] [Google Scholar]
- 23.Sakamoto A, Kiyokawa K, Rikimaru H, et al. An investigation of the fixation materials for cartilage frames in microtia. J Plast Reconstr Aesthet Surg. 2012;65:584–589. doi: 10.1016/j.bjps.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 24.Chen Z, Zhang W, Huang J, et al. Exceedingly expanded retroauricular flaps for microtia reconstruction. J Plast Reconstr Aesthet Surg. 2011;64:1448–1453. doi: 10.1016/j.bjps.2011.06.025. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Q, Quan Y, Su Y, et al. Expanded retroauricular skin and fascial flap in congenital microtia reconstruction. Ann Plast Surg. 2010;64:428–434. doi: 10.1097/SAP.0b013e3181b0bb7e. [DOI] [PubMed] [Google Scholar]
- 26.Liu J, Sun J, Li X. Total auricular reconstruction without skin grafting. J Plast Reconstr Aesthet Surg. 2011;64:1312–1317. doi: 10.1016/j.bjps.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Zou YH, Zhuang HX, Wang SJ, et al. Satisfactory surgical option for congenital microtia with defects of external auditory meatus (EAM) and middle ear. Acta Otolaryngol. 2007;127:705–710. doi: 10.1080/00016480601053065. [DOI] [PubMed] [Google Scholar]
- 28.Zhou X, Zhang Q, Liu T, et al. Modification in the technique of ear framework fabrication for congenital microtia. J Craniofac Surg. 2012;23:1296–1300. doi: 10.1097/SCS.0b013e3182564a49. [DOI] [PubMed] [Google Scholar]
- 29.Pan B, Jiang H, Guo D, et al. Microtia: ear reconstruction using tissue expander and autogenous costal cartilage. J Plast Reconstr Aesthet Surg. 2008;61(Suppl 1):S98–103. doi: 10.1016/j.bjps.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 30.Wang Y, Zhuang X, Jiang H, et al. The anatomy and application of the postauricular fascia flap in auricular reconstruction for congenital microtia. J Plast Reconstr Aesthet Surg. 2008;61(Suppl 1):S70–S76. doi: 10.1016/j.bjps.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 31.Liu X, Zhang Q, Quan Y, et al. Bilateral microtia reconstruction. J Plast Reconstr Aesthet Surg. 2010;63:1275–1278. doi: 10.1016/j.bjps.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 32.Jing C, Hong-Xing Z. Partial necrosis of expanding postauricular flaps during auricle reconstruction: risk factors and effective management. Plast Reconstr Surg. 2007;119:1759–1766. doi: 10.1097/01.prs.0000259092.58025.89. [DOI] [PubMed] [Google Scholar]
- 33.Dashan Y, Haiyue J, Qinghua Y, et al. Technical innovations in ear reconstruction using a skin expander with autogenous cartilage grafts. J Plast Reconstr Aesthet Surg. 2008;61(Suppl 1):S59–S69. doi: 10.1016/j.bjps.2008.06.051. [DOI] [PubMed] [Google Scholar]
- 34.Jiang H, Pan B, Lin L, et al. Ten-year experience in microtia reconstruction using tissue expander and autogenous cartilage. Int J Pediatr Otorhinolaryngol. 2008;72:1251–1259. doi: 10.1016/j.ijporl.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 35.Tanino R, Miyasaka M. Reconstruction of microtia using tissue expander. Clin Plast Surg. 1990;17:339–353. [PubMed] [Google Scholar]
- 36.Park C. Balanced auricular reconstruction in dystopic microtia with the presence of the external auditory canal. Plast Reconstr Surg. 2002;109:1489–1500. doi: 10.1097/00006534-200204150-00001. discussion 1501. [DOI] [PubMed] [Google Scholar]
- 37.Aguilar EF., 3rd Auricular reconstruction of congenital microtia (grade III). Laryngoscope. 1996;106(12 Pt 2 Suppl 82):1–26. doi: 10.1097/00005537-199612001-00001. [DOI] [PubMed] [Google Scholar]
- 38.Osorno G. Autogenous rib cartilage reconstruction of congenital ear defects: report of 110 cases with Brent’s technique. Plast Reconstr Surg. 1999;104:1951–1962. doi: 10.1097/00006534-199912000-00001. discussion 1963. [DOI] [PubMed] [Google Scholar]
- 39.Zhao S, Wang D, Han D, et al. Integrated protocol of auricle reconstruction combined with hearing reconstruction. Acta Otolaryngol. 2012;132:829–833. doi: 10.3109/00016489.2012.662716. [DOI] [PubMed] [Google Scholar]
- 40.Yellon RF. Combined atresiaplasty and tragal reconstruction for microtia and congenital aural atresia: thesis for the American Laryngological, Rhinological, and Otological Society. Laryngoscope. 2009;119:245–254. doi: 10.1002/lary.20023. [DOI] [PubMed] [Google Scholar]
- 41.Boudard P, Benassayag C, Dhillon RS, et al. Aesthetic surgery for microtia. Arch Otorhinolaryngol. 1989;246:349–352. doi: 10.1007/BF00463592. [DOI] [PubMed] [Google Scholar]
- 42.Sabbagh W. Early experience in microtia reconstruction: the first 100 cases. J Plast Reconstr Aesthet Surg. 2011;64:452–458. doi: 10.1016/j.bjps.2010.07.027. [DOI] [PubMed] [Google Scholar]
- 43.Nakai H. Reconstruction of microtia. Pursuing a natural appearance. Clin Plast Surg. 1990;17:287–304. [PubMed] [Google Scholar]
- 44.Park C, Lew DH, Yoo WM. An analysis of 123 temporoparietal fascial flaps: anatomic and clinical considerations in total auricular reconstruction. Plast Reconstr Surg. 1999;104:1295–1306. doi: 10.1097/00006534-199910000-00009. [DOI] [PubMed] [Google Scholar]
- 45.Park C. Modification of two-flap method and framework construction for reconstruction of atypical congenital auricular deformities. Plast Reconstr Surg. 1997;99:1846–1857. doi: 10.1097/00006534-199706000-00007. [DOI] [PubMed] [Google Scholar]
- 46.Song Y, Song Y. An improved one-stage total ear reconstruction procedure. Plast Reconstr Surg. 1983;71:615–623. doi: 10.1097/00006534-198305000-00005. [DOI] [PubMed] [Google Scholar]
- 47.Thomson HG, Kim TY, Ein SH. Residual problems in chest donor sites after microtia reconstruction: a long-term study. Plast Reconstr Surg. 1995;95:961–968. doi: 10.1097/00006534-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Leach JL, Jr, Jordan JA, Brown KR, et al. Techniques for improving ear definition in microtia reconstruction. Int J Pediatr Otorhinolaryngol. 1999;48:39–46. doi: 10.1016/s0165-5876(99)00008-7. [DOI] [PubMed] [Google Scholar]
- 49.Chin WS, Zhang R, Zhang Q, et al. Techniques for improving tragus definition in auricular reconstruction with autogenous costal cartilage. J Plast Reconstr Aesthet Surg. 2011;64:541–544. doi: 10.1016/j.bjps.2010.04.044. [DOI] [PubMed] [Google Scholar]
- 50.Zhang Q, Zhang R, Xu F, et al. Firm elevation of the reconstructed auricle with a retroauricular fascial flap wrapping an EH (a mixture of epoxide acrylate malelic and hydroxyapatite) composite wedge. J Plast Reconstr Aesthet Surg. 2010;63:1452–1458. doi: 10.1016/j.bjps.2009.07.042. [DOI] [PubMed] [Google Scholar]
- 51.Zhang Q, Zhang R, Xu F, et al. Auricular reconstruction for microtia: personal 6-year experience based on 350 microtia ear reconstructions in China. Plast Reconstr Surg. 2009;123:849–858. doi: 10.1097/PRS.0b013e318199f057. [DOI] [PubMed] [Google Scholar]
- 52.Tanzer RC. Microtia—a long-term follow-up of 44 reconstructed auricles. Plast Reconstr Surg. 1978;61:161–166. doi: 10.1097/00006534-197802000-00001. [DOI] [PubMed] [Google Scholar]
- 53.Chauhan DS, Guruprasad Y. Auricular reconstruction of congenital microtia using autogenous costal cartilage: report of 27 cases. J Maxillofac Oral Surg. 2012;11:47–52. doi: 10.1007/s12663-011-0290-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jiang H, Pan B, Lin L, et al. Fabrication of three-dimensional cartilaginous framework in auricular reconstruction. J Plast Reconstr Aesthet Surg. 2008;61(Suppl 1):S77–S85. doi: 10.1016/j.bjps.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 55.Breugem CC, Stewart KJ, Kon M. International trends in the treatment of microtia. J Craniofac Surg. 2011;22:1367–1369. doi: 10.1097/SCS.0b013e31821c9464. [DOI] [PubMed] [Google Scholar]
- 56.Chen J, Yang Q, Wang X, et al. Fabrication of a three-dimensional autogenous costal cartilage framework in auricular reconstruction: experience with 250 cases of Asian lobule-type microtia. J Otolaryngol Head Neck Surg. 2008;37:901–908. [PubMed] [Google Scholar]
- 57.Firmin F. Ear reconstruction in cases of typical microtia. Personal experience based on 352 microtic ear corrections. Scand J Plast Reconstr Surg Hand Surg. 1998;32:35–47. doi: 10.1080/02844319850158930. [DOI] [PubMed] [Google Scholar]
- 58.Quatela VC, Goldman ND. Microtia repair. Facial Plast Surg. 1995;11:257–273. doi: 10.1055/s-2008-1064542. [DOI] [PubMed] [Google Scholar]
- 59.Jiang H, Pan B, Lin L, et al. Lifting the reconstructed ear using remnant ear cartilage in lobule-type microtia. J Plast Reconstr Aesthet Surg. 2009;62:273–277. doi: 10.1016/j.bjps.2008.03.058. [DOI] [PubMed] [Google Scholar]
- 60.Cho BC, Kim JY, Byun JS. Two-stage reconstruction of the auricle in congenital microtia using autogenous costal cartilage. J Plast Reconstr Aesthet Surg. 2007;60:998–1006. doi: 10.1016/j.bjps.2005.12.052. [DOI] [PubMed] [Google Scholar]


