Abstract
Summary:
Obesity increases the risk of upper extremity lymphedema following treatment for breast cancer and can cause lower extremity lymphatic dysfunction in extremely obese individuals. We report the first patient with obesity-induced upper extremity lymphedema. A 62-year-old man with a previous body mass index (BMI) of 105.6, presented with a BMI 60.3 following weight loss. He complained of lymphedema of all 4 extremities, which was confirmed by lymphoscintigraphy. Because the upper limbs are more resistant to lymphedema than the lower extremities, a higher BMI threshold may be necessary to cause upper extremity lymphatic dysfunction.
Lymphedema is a chronic, incurable condition caused by the anomalous development of the lymphatic system (primary lymphedema) or injury to lymphatic vasculature (secondary lymphedema). The disease affects millions of persons worldwide and most commonly involves the extremities. Fluid accumulates in the interstitial space, causing enlargement of the affected area. Complications of lymphedema include psychosocial morbidity, infection, functional disability, skin changes, and malignant transformation.1
Primary lymphedema is idiopathic, rare, and typically presents during infancy, childhood, or adolescence. Secondary lymphedema is the most common cause of the disease and usually results from either a parasitic infection or following nodal radiation and lymphadenectomy. Recently, we have shown that extreme obesity may be a novel cause of lymphedema.2 Patients with a body mass index (BMI) greater than 59 were found to have lower extremity lymphedema, whereas obese individuals with a BMI between 30 and 53 had normal lower extremity lymphatic function.2 Patients in this study were referred for lower extremity lymphedema, and thus, only the lymphatic function of their legs was studied. We now report the first patient with obesity-induced lymphedema involving the upper limbs.
CASE REPORT
A 62-year-old man was referred to our Lymphedema Program with bilateral upper and lower extremity lymphedema (Fig. 1). He was 5 feet 10 inches tall (179 cm) and weighed 420 pounds (191 kg); his BMI was 60.3. He had lost weight by dieting over the previous 10 years since he was at his maximum weight of 736 pounds (BMI, 105.6). He complained of difficulty using his extremities and periodic infections of his lower limbs. His medical history was significant for a herniated disk, asthma, chronic obstructive pulmonary disease, transurethral resection of the prostate, and herniorrhaphy. His medications included lisinopril, percocet, and diazepam. Other than his BMI, he did not have any risk factors for lymphedema (eg, primary lymphedema, penetrating trauma, lymphadenectomy, and radiation). On physical examination, he had pitting edema of all 4 extremities. To determine his extremity lymphatic function, he underwent lymphoscintigraphy, which is 100% specific and 92% sensitive for lymphedema.3–6 His lymphoscintigram showed lymphatic dysfunction of all 4 extremities, with delayed transit to the inguinal and axillary lymph nodes. The patient was managed with static and pneumatic compression and was referred to a bariatric center.
Fig. 1.
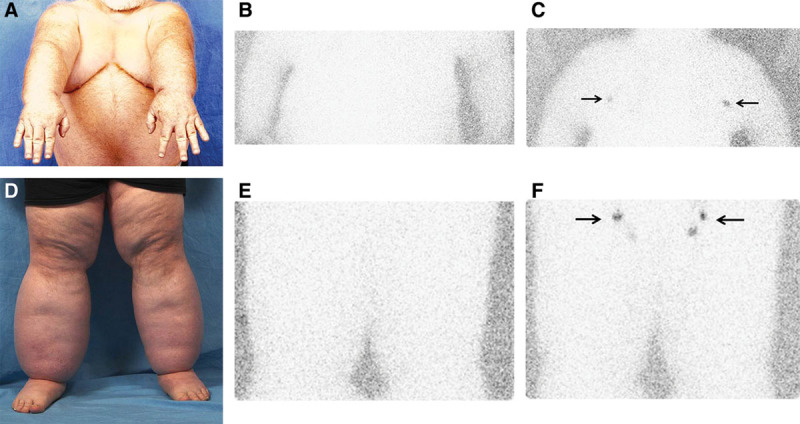
A 62-year-old man with a maximum BMI history of 105.6, presented with a BMI of 60.3 after dieting. He complained of swelling of all 4 limbs (A and D). Extremity lymphoscintigraphy showed absence of tracer in the axillary (B) and inguinal nodes (E) 45 min following radiolabelled colloid injection into the hands and feet (normal transit time to the axillary and inguinal nodes is <45 min).3–6 Minimal, delayed tracer accumulation into the axillary (C) and inguinal nodes (F) occurred 2 h after injection. These findings indicated lymphatic dysfunction of all 4 extremities consistent with lymphedema.3–6 Arrows indicate nodal uptake of radiolabelled tracer.
DISCUSSION
Obesity, which affects one third of the population in the United States,7 negatively affects lymphatic function. Not only does obesity increase the risk of lymphedema following lymphadenectomy and radiation to the axilla,8–11 but it may cause the disease in extremely obese individuals (BMI, >59).2 Previously, obese patients referred to our center complained of lower extremity enlargement, and thus, only the lymphatic function of their legs was assessed using lymphoscintigraphy. The patient in this report was the first to present with upper extremity edema as well, and he was found to have lymphatic dysfunction of all of his limbs. His maximum BMI of 105 was the highest of the cohort of patients managed in our Lymphedema Program. The patient we have treated with the next highest BMI (88) had bilateral lower extremity lymphedema but did not complain of upper extremity edema. A BMI threshold may exist above 88 at which point upper extremity lymphatic dysfunction might develop, similar to the threshold between 54 and 59 at which point lower extremity lymphedema seems to occur. The upper limbs should be more resistant to developing obesity-induced lymphedema, compared with the lower extremities, because: (1) adipose deposition in obese patients preferentially affects the legs, (2) lymph drainage from the upper limbs is closer to the central venous circulation, and (3) the arms are less affected by having to transport lymph against gravity.
Obesity may reduce lymphatic function by either (1) impairing the function of lymphatic vessels and/or (2) overwhelming normally functioning lymphatics with increased lymph production. An obese limb may compress lymphatics or the adipose tissue might cause inflammation which damages the lymphatic vasculature. Alternatively, as the size of the obese extremity increases, the elevated production of lymph may overwhelm the capacity of the lymphatics to transport the fluid proximally.
Obesity-induced lymphedema may prove to be the only example of lymphedema that is reversible. Following weight loss through diet or a bariatric procedure, lymphatic clearance may improve because of reduced lymph production and/or by restored function of lymphatic vessels. If lymphatic function does not reverse following massive weight loss, then the mechanism for the disease would be less likely elevated lymph production and more likely injury to lymphatic vasculature which cannot be reversed following weight loss. If lymphedema proves to be irreversible following massive weight loss, then patients should undergo a bariatric procedure before reaching a BMI threshold when lymphatic dysfunction occurs. Unlike other comorbidities that improve following weight loss (eg, diabetes, hypertension, and hypercholesterolemia), patients would continue to suffer from lymphedema.
CONCLUSIONS
Extreme obesity previously has been associated with lower extremity lymphedema. We present a patient with a maximum BMI history of 105 who was referred with bilateral arm and leg lymphedema. Lymphoscintigraphy confirmed lymphatic dysfunction of all 4 limbs. Severe obesity may be a novel cause of upper extremity lymphedema.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Schook CC, Mulliken JB, Fishman SJ, et al. Primary lymphedema: clinical features and management in 138 pediatric patients. Plast Reconstr Surg. 2011;127:2419–2431. doi: 10.1097/PRS.0b013e318213a218. [DOI] [PubMed] [Google Scholar]
- 2.Greene AK, Grant FD, Slavin SA. Lower extremity lymphedema and elevated body mass in obese patients. N Engl J Med. 2012;366:2136–2137. doi: 10.1056/NEJMc1201684. [DOI] [PubMed] [Google Scholar]
- 3.Gloviczki P, Calcagno D, Schirger A, et al. Noninvasive evaluation of the swollen extremity: experiences with 190 lymphoscintigraphic examinations. J Vasc Surg. 1989;9:683–699. doi: 10.1067/mva.1989.vs0090683. discussion 690. [DOI] [PubMed] [Google Scholar]
- 4.Moshiri M, Katz DS, Boris M, et al. Using lymphoscintigraphy to evaluate suspected lymphedema of the extremities. AJR Am J Roentgenol. 2002;178:405–412. doi: 10.2214/ajr.178.2.1780405. [DOI] [PubMed] [Google Scholar]
- 5.Szuba A, Shin WS, Strauss HW, et al. The third circulation: radionuclide lymphoscintigraphy in the evaluation of lymphedema. J Nucl Med. 2003;44:43–57. [PubMed] [Google Scholar]
- 6.Scarsbrook AF, Ganeshan A, Bradley KM. Pearls and pitfalls of radionuclide imaging of the lymphatic system. Part 2: evaluation of extremity lymphoedema. Br J Radiol. 2007;80:219–226. doi: 10.1259/bjr/68256780. [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 8.Werner RS, McCormick B, Petrek J, et al. Arm edema in conservatively managed breast cancer: obesity is a major predictive factor. Radiology. 1991;180:177–184. doi: 10.1148/radiology.180.1.2052688. [DOI] [PubMed] [Google Scholar]
- 9.McLaughlin SA, Wright MJ, Morris KT, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: patient perceptions and precautionary behaviors. J Clin Oncol. 2008;26:5220–5226. doi: 10.1200/JCO.2008.16.3766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Helyer LK, Varnic M, Le LW, et al. Obesity is a risk factor for developing postoperative lymphedema in breast cancer patients. Breast J. 2010;16:48–54. doi: 10.1111/j.1524-4741.2009.00855.x. [DOI] [PubMed] [Google Scholar]
- 11.Ridner SH, Dietrich MS, Stewart BR, et al. Body mass index and breast cancer treatment-related lymphedema. Support Care Cancer. 2011;19:853–857. doi: 10.1007/s00520-011-1089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


