Abstract
Background:
Joint scar contractures are characterized by tight bands of soft tissue that bridge the 2 ends of the joint like a web. Classical treatment methods such as Z-plasties are mainly based on 2-dimensional designs. Our square flap method is an alternative surgical method that restores the span of the web in a stereometric fashion, thereby reconstructing joint function.
Methods:
In total, 20 Japanese patients with joint scar contractures on the axillary (n = 10) or first digital web (n = 10) underwent square flap surgery. The maximum range of motion and commissure length were measured before and after surgery. A theoretical stereometric geometrical model of the square flap was established to compare it to the classical single (60 degree), 4-flap (45 degree), and 5-flap (60 degree) Z-plasties in terms of theoretical web reconstruction efficacy.
Results:
All cases achieved 100% contracture release. The maximum range of motion and web space improved after square flap surgery (P = 0.001). Stereometric geometrical modeling revealed that the standard square flap (α = 45 degree; β = 90 degree) yields a larger flap area, length/width ratio, and postsurgical commissure length than the Z-plasties. It can also be adapted by varying angles α and β, although certain angle thresholds must be met to obtain the stereometric advantages of this method.
Conclusions:
When used to treat joint scar contractures, the square flap method can fully span the web space in a stereometric manner, thus yielding a close-to-original shape and function. Compared with the classical Z-plasties, it also provides sufficient anatomical blood supply while imposing the least physiological tension on the adjacent skin.
Joint scar contractures are generally characterized by tight bands of soft tissue that bridge the 2 ends of the joint like a web. They are common problems for plastic surgeons. The classical treatment approach is to use a Z-plasty, which is a versatile method for breaking up the straight line, increasing length, shifting topographic features, and effacing the web.1 There are a number of popular Z-plasty methods, including the single Z-plasty, the 4-flap Z-plasty, and the 5-flap Z-plasty. When they are used in different angles and lengths, they can help to release joint scar contractures. However, these local flap designs2 are mainly based on 2-dimensional geometrical calculations.3–5 Although 3-dimensional reconstruction designs are much less common than 2-dimensional designs, they have the potential to be superior in terms of restoring the span of a joint because they can provide 3-dimensional features that more closely approximate the architecture of the original web.
The square flap method (Fig. 1) was reported previously by Hyakusoku and Fumiiri6 and is an effective way to elongate the skin. In this article, we used this method to reconstruct scar contracture-bearing axillary and first digital webs and assessed its ability to release the scar contracture and improve joint function. We also used 3-dimensional geometric modeling to assess how well the square flap, single Z-plasty (Fig. 2), 4-flap Z-plasty (Fig. 3), and 5-flap Z-plasty (Fig. 4) methods reconstruct a web so that it forms a stereometric commissure that is sufficiently long and deep and appropriately shaped, thus generating an anatomically, physiologically, and biomechanically correct web. On the basis of these observations, we propose the indications for square flaps.
Fig. 1.
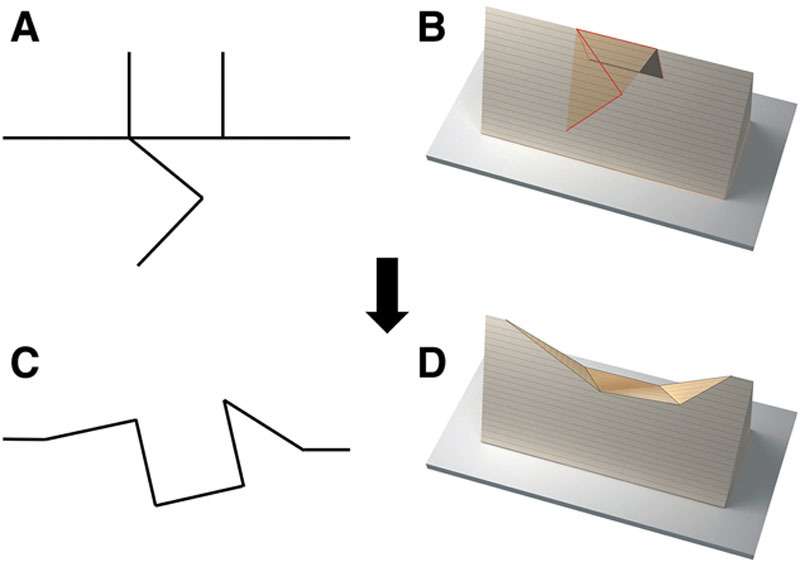
Schematic depictions of the standard square flap method (α = 45 degree and β = 90 degree). The figure shows the linear (A, C) and 3-dimensional (B, D) design before (A, B) and after (C, D) surgery.
Fig. 2.
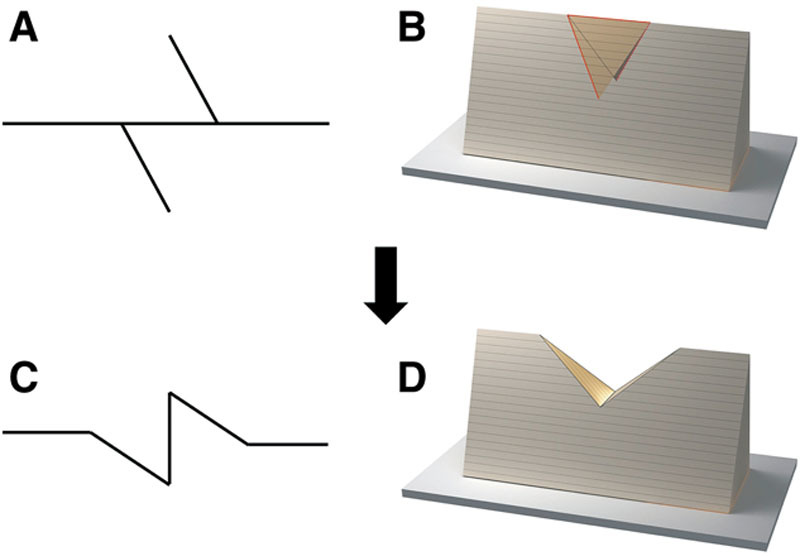
Schematic depictions of the single Z-plasty method (60 degree). The figure shows the linear (A, C) and 3- dimensional (B, D) design before (A, B) and after (C, D) surgery.
Fig. 4.
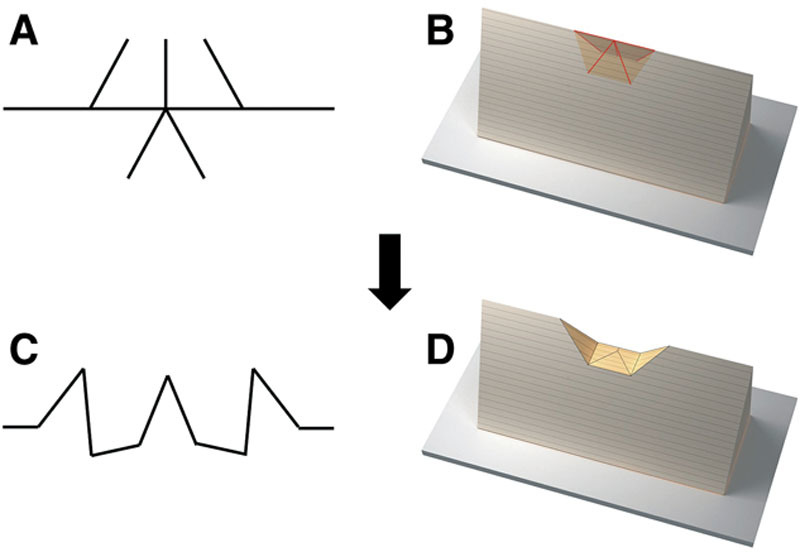
Schematic depictions of the 5-flap Z-plasty (60 degree). The figure shows the linear (A, C) and 3-dimensional (B, D) design before (A, B) and after (C, D) surgery.
Fig. 3.
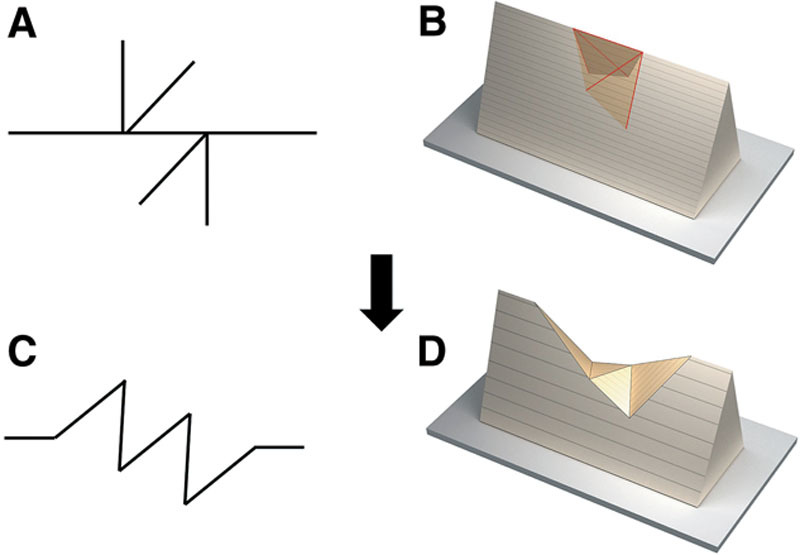
Schematic depictions of the 4-flap Z-plasty (45 degree). The figure shows the linear (A, C) and 3-dimensional (B, D) design before (A, B) and after (C, D) surgery.
PATIENTS AND METHODS
Patients
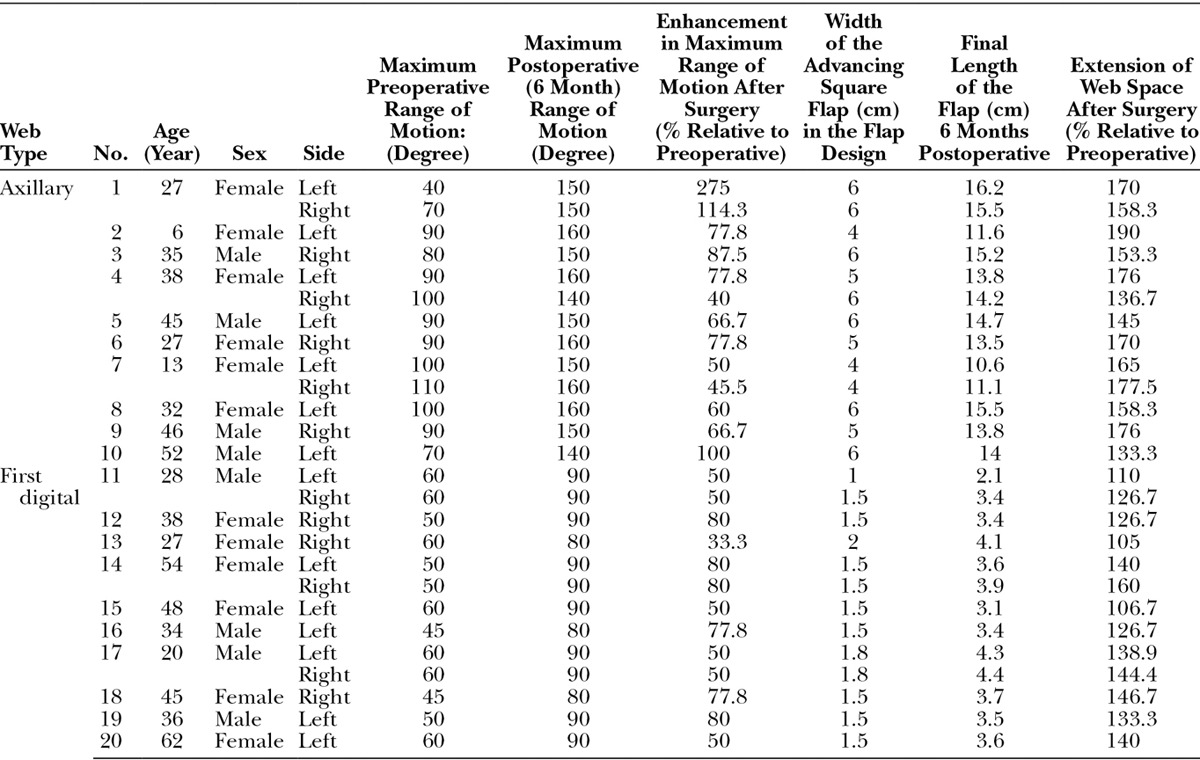
The 20 patients with joint scar contractures after a burn who were treated at Nippon Medical School between 2000 and 2010 were included in the study. Ten had axillary web contractures and 10 had first digital web contractures. The patients’ age, sex, maximum range of motion and web space before and after surgery, width of the square flap, and final commissure length 6 months after the surgery were recorded. The follow-up period after surgery was more than 6 months for each patient.
This study complied with the Declaration of Helsinki and was approved by the ethics committee of Nippon Medical School. Written/oral informed consent was obtained from all participants.
Surgical Technique
Figure 1 shows the design of the standard square flap, which is composed of a square advancement flap with 2 triangular transposition flaps. The angles of the triangular flaps are 45 and 90 degrees (designated as the α and β angles, respectively). After subcutaneous injection of local anesthesia with adrenaline diluted in normal saline (1:200,000), the whole thickness of the skin was incised with a No. 15 blade along the line marks. This was followed by incision of the subcutaneous tissue. Before skin closure, it was necessary to perform electrocautery and subcutaneous dissection as standard procedures. The incision was then closed by applying subcutaneous/superficial fascial sutures with 3-0 PDS II (Ethicon, Tokyo), dermal sutures with 4-0 PDS II (Ethicon), and finally, superficial sutures with 6-0 Ethilon (Ethicon). All patients were treated with taping fixation for the first 3 months after surgery; this treatment was initiated immediately after the sutures were removed.
Statistical Analyses
Statistical analyses were performed by using SPSS 16.0 for Windows v16.0.1 (SPSS, Tokyo, Japan). The nonparametric Wilcoxon signed ranks test was used to compare the range of motion before and after the operation and to assess whether the surgery increased the web space. Statistical significance was set at a double-sided P value of <0.05.
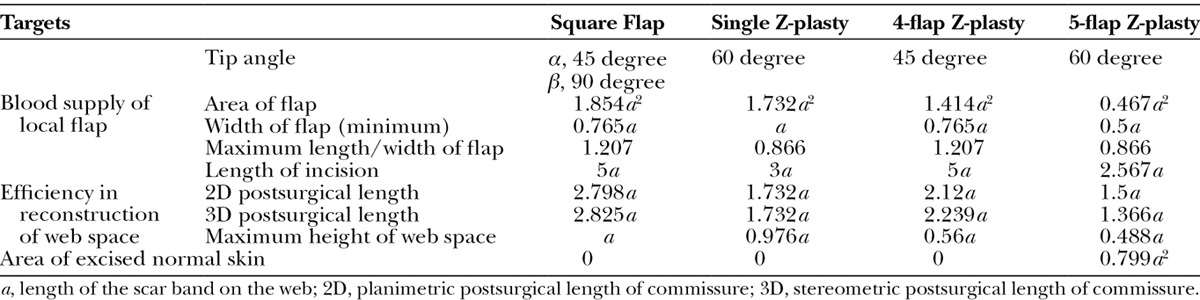
Stereometric Geometrical Modeling of the Square Flap
A theoretical stereometric geometrical model of the square flap was established on the basis of principles of trigonometry. It was used to compare the standard square flap method to the single (60 degree), 4-flap (45 degree), and 5-flap (60 degree) Z-plasty methods in terms of the length and height of the commissure after surgery, the flap area, the minimum width of the base of the flap, the maximum length/width ratio of the flap, the length of the incision, and the area of excised normal skin. The effect of changing the α angle of the square flap while maintaining the β angle at 90 degree on the difference between the stereometric and planimetric postsurgical commissure lengths was also assessed.
RESULTS
Outcomes of Patients Who Underwent Square Flap Surgery
The patients in the axillary and first digital web groups were on average 32.1 and 39.2 years old, and 60% of both groups were women (Table 1). All cases achieved contracture release. Complications such as infection, hematoma, or skin necrosis were not observed. The maximum range of motion of the affected joint increased significantly after square flap surgery by 87.61% in the axilla web group (P = 0.001) and by 62.22% in the first digital web group (P = 0.001). The surgery also significantly extended the web space in the 2 groups by 162.27% (P = 0.001) and 131.15% (P = 0.001), respectively (Table 1).
Table 1.
Demographic, Presurgical, and Postsurgical Characteristics of the Patients Who Underwent Axillary Web and First Digital Web Reconstructions with the Square Flap Method
Stereometric Geometrical Modeling of the Square Flap
For theoretical purposes, the length of the scar band on the web is defined as a. Thus, for the 4 types of local flaps, the flap area will be 1.854a2 (square flap) > 1.732a2 (single Z-plasty) > 1.414a2 (4-flap Z-plasty) > 0.467a2 (5-flap Z-plasty). The maximum length/width ratio of the flap will be 1.207 (square flap) = 1.207 (4-flap Z-plasty) > 0.866 (single Z-plasty) = 0.866 (5-flap Z-plasty). The total length of the incision will be 5a (square flap) = 5a (4-flap Z-plasty) > 3a (single Z-plasty) > 2.567a (5-flap Z-plasty). A lthough the mathematically calculated 2-dimensional (planimetric) postsurgical length of the commissure will be 2.798a (square flap) > 2.12a (4-flap Z-plasty) > 1.732a (single Z-plasty) > 1.5a (5-flap Z-plasty), the stereometric postsurgical commissure length will be 2.825a (square flap) > 2.239a (4-flap Z-plasty) > 1.732a (single Z-plasty) > 1.366a (5-flap Z-plasty). Moreover, if the peak angle is defined as 25 degree to simulate the peak angle of the web space in the hand after surgery,7 the maximum height of the web space after surgery will be a (square flap) > 0.976a (single Z-plasty) > 0.56a (4 flap Z-plasty) > 0.488a (5 flap Z-plasty), respectively. The area of excised normal skin will be 0.799a2 (5-flap Z-plasty) > 0 (all other local flaps) (Table 2 and Figs. 1–4).
Table 2.
Comparison of the 4 Local Flaps in Terms of Their Web Reconstruction Efficacy
We also assessed whether changing angle α in the square flap while maintaining angle β at 90 degree will change the difference between the stereometric and planimetric postsurgical lengths of the commissure (Table 3 and Fig. 5). The stereometric advantage of the square flap method will only appear when angle α exceeds 37.5 degree. A similar threshold was also observed for angle β when angle α was maintained (data not shown). Similarly, the analyses also revealed that the stereometric elongation effect of the square flap method will be realized when (1) angle α exceeds 44.9, 52.4, and 60 degrees in flaps where angle β is 80, 70, and 60 degrees, respectively, or (2) angle α is smaller than 67.9, 76.2, and 85.1 degrees in flaps where angle β is 50, 40, and 30 degrees, respectively.
Table 3.
Effect of Changing Angle α While Maintaining Angle β at 90 Degree on the Stereometric and Planimetric Elongation of the Commissure
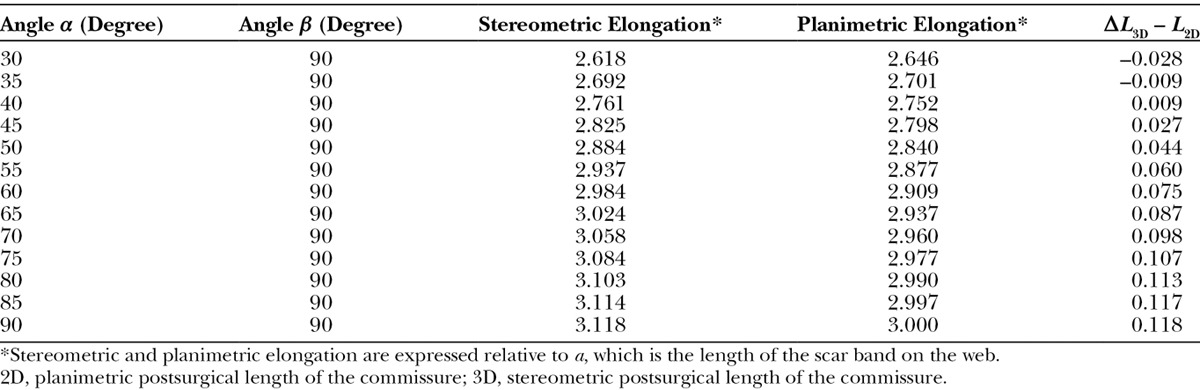
Fig. 5.
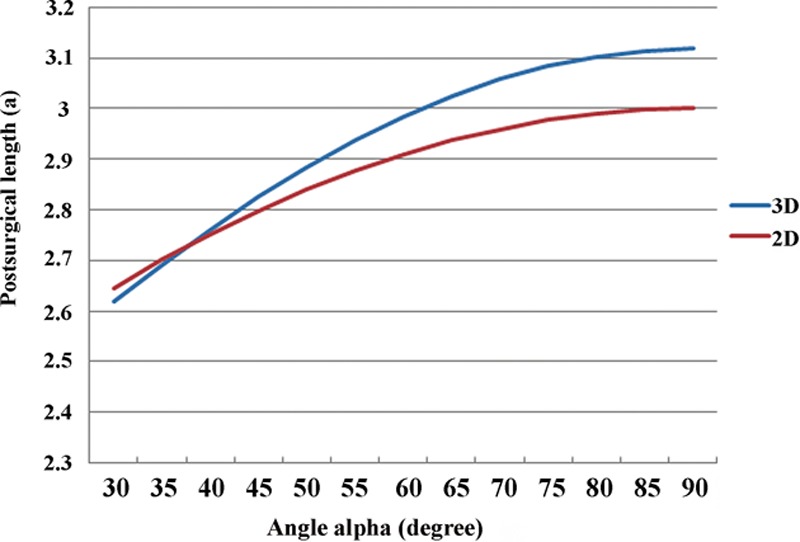
Effect of changing angle α of the square flap while maintaining angle β at 90 degree on the 3-dimensional (stereometric) and 2-dimensional (planimetric) postsurgical length of the commissure. Postsurgical length is expressed relative to a, which is defined as the length of the scar band on the web.
Illustrative Cases
Case 1 (Axillary Web).
A 53-year-old female had a flame burn on her right axilla. Six months later, the patient had developed thick hypertrophic scars on the right anterior line of the axilla (Fig. 6). The range of motion of the elevation of the right shoulder was 60 degree. A square flap was designed on the anterior line. To ensure that the hairy regions were not divided, the sides of the square advancement flap were set at 3 cm (Fig. 6). The scar on the anterior line was excised and the 3 flaps were elevated (Fig. 6). In addition, a hypertrophic scar on the posterior line was reconstructed by a transposition flap that was designed next to the scar. The range of motion of elevation of the right shoulder improved to 150 degree immediately after surgery (Fig. 6). This outcome was still effective 1 year after surgery. The postoperative course was uneventful. Twelve months after surgery, recurrences of the hypertrophic scars and scar contractures were not observed.
Fig. 6.
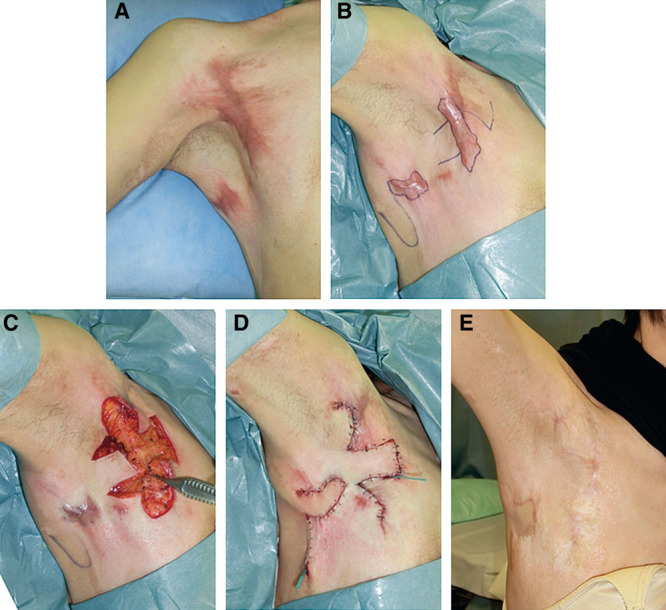
Images of a clinical case where the square flap method was used for the 3-dimensional reconstruction of scar contractures on the axillary web. A, Original contracture. B, Incision design. C, After flap elevation. D, Immediately after surgery. E, At the 12-month follow-up visit.
Case 2 (First Digital Web).
A 30-year-old male had a flame burn on his right hand. One year later, the patient had developed scar contractures on the first web space (Fig. 7). The range of motion of abduction of the right thumb was 60 degree. A square flap was designed on the anterior line. The sides of the square advancement flap were set at 2 cm (Fig. 7). The incision was made and the 3 flaps were elevated. The range of motion of abduction of the right thumb improved to 90 degree immediately after surgery (Fig. 7). The postoperative course was uneventful. One year after surgery, recurrences of the hypertrophic scars and scar contractures were not observed (Fig. 7).
Fig. 7.

Images of a clinical case where the square flap method was used for 3-dimensional reconstruction of scar contractures on the first digital web. A, Original contracture status and incision design. B, Flap transfer and the outcomes immediately after surgery. C, At the 1-year follow-up visit.
DISCUSSION
Of the various local flap methods that are currently available, the square flap method meets all the requirements for reconstructing webs that bear joint scar contractures, thereby transforming the web into a deep and broad commissure that closely mimics the original architecture of the web space.8 In essence, the square flap is a 3-flap Z-plasty that is composed of a square advancement flap combined with 2 triangular transposition flaps. After surgery, the centrally located square flap becomes a suitably large and pliable floor of the web space. Its dimensions thus dictate the width of the commissure. After surgery, the 2 lateral triangular flaps become the lateral walls of the web space. Thus, their dimensions determine the depth of the commissure. These features ensure that the web will have a normal appearance and function after square flap surgery because the commissure will have a U-shape that is sufficiently deep and will slope naturally with a flat palm surface. The dorsal surface will also have a palmar inclination.9 All of this is achieved with minimal donor site morbidity and normal skin excision. In fact, our geometric modeling analyses revealed that the square flap method is more efficient than the single, 4-flap, and 5-flap Z-plasty methods in terms of the maximum stereometric commissure lengthening: it lengthens the original scar band by 2.825-fold, compared with the ≤2.239-fold lengthening ability of the Z-plasties. In particular, if the peak angle is set at 25 degree to simulate the peak angle of the web spaces in the hand,7 the square flap method can yield the largest maximum height of the commissure of the 4 local flaps.
The square flap method also has anatomical and physiological advantages over the 3 transposition Z-plasties. First, it yields the largest nourishable flap area (1.854a2) and involves the longest incision/contact length (5a). Moreover, the minimum width of the square flap is equal to the minimum width of the 4-flap Z-plasty (0.765a), despite the fact that the 2 methods have identical maximum length/width ratios (1.207). Second, the square flap method seems to be associated with the lowest physiological tension, which means that the deformity of the adjacent skin and the dependence on the laxity of the adjacent skin is minimized. In other words, the advantage identified by stereometric analysis could translate into lower physiological tension and secondary benefits for patients.
Although the square flap method seems to be excellent for the 3-dimensional reconstruction of joint scar contractures, these flaps should only be used after considering the relative merits and disadvantages of the available methods in relation to the severity of the joint scar contractures (which is determined by 4 key scar features, namely size, depth, location, and shape). The square flap is a local flap and thus is at a lower level on the reconstruction ladder than counterparts such as skin grafts and the pedicled flap.10 Therefore, the square flap is suitable for medium-sized and medium-deep tissue defects and deformities. In particular, it is indicated for single linear or band contractures in the web spaces at various locations. Specifically, it is suitable for (1) type IIa and IIb axillary web scar contractures where single band contractures involve the anterior or posterior axillary line,11 (2) type I digital joint contractures where there is a single digital joint contracture on the palmar or dorsal side, (3) chin/anterior neck web scar contractures with linear or band contractures within the unit, and (4) type I cubital and wrist joint contractures where there are linear or band contractures on the flexor/palmar or dorsal surface.12 Larger and deeper tissue defects should be treated by other methods, such as skin grafts, propeller flaps,13 pedicled flaps, or free flaps.
It is also possible to modify the square flap to optimize the length, depth, and architectural shape of the resulting commissure, thus yielding the best possible appearance and function. This can be achieved by altering the proper tip angles of the 2 small lateral triangular flaps of the square flap. This versatility makes the square flap method suitable for a wide variety of tissue deformities and defects.14 In particular, our stereometric geometrical calculations show that when the tip angle β is set at 80, 70, or 60 degrees, the tip angle α should exceed 44.9, 52.4, and 60 degrees, respectively. Moreover, when angle β is set at 50, 40, or 30 degrees, the tip angle α should be smaller than 67.9, 76.2, and 85.1 degrees, respectively.
The limitations of this study lie mainly in the small number of patients. More cases with longer follow-up periods will be required to confirm the effectiveness and efficiency of the square flap method for the 3-dimensional reconstruction of scar contracture-bearing axilla and digital webs.
CONCLUSIONS
In summary, the square flap method is a 3-flap Z-plasty that combines flap transposition and advancement and provides an effective solution to the reconstruction of joint scar contractures. Our comparisons of the square flap with the single, 4-flap, and 5-flap Z-plasty methods confirm that the square method can fully span the web space in a stereometric manner, thus yielding the best shape and function. It is also associated with sufficient anatomical blood supply, yields the least physiological tension on the adjacent skin, and does not require excision of normal skin. When used at the appropriate angles, it can be a powerful tool for the 3-dimensional reconstruction of single linear or band joint contractures in the web spaces at various locations of the body.
Footnotes
The authors contributed equally to this work.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Furnas DW. The four fundamental functions of the X-plasty. Arch Surg. 1968;96:458–463. doi: 10.1001/archsurg.1968.01330210136027. [DOI] [PubMed] [Google Scholar]
- 2.Furnas DW, Fischer GW. The Z-plasty: biomechanics and mathematics. Br J Plast Surg. 1971;24:144–160. doi: 10.1016/s0007-1226(71)80034-6. [DOI] [PubMed] [Google Scholar]
- 3.Vegter F, Hage JJ. A theoretical consideration of extensions of the Z-plasty principle. Eur J Plast Surg. 1997;20:71–76. [Google Scholar]
- 4.Hove CR, Williams EF, 3rd, Rodgers BJ. Z-plasty: a concise review. Facial Plast Surg. 2001;17:289–294. doi: 10.1055/s-2001-18828. [DOI] [PubMed] [Google Scholar]
- 5.Hudson DA. Some thoughts on choosing a Z-plasty: the Z made simple. Plast Reconstr Surg. 2000;106:665–671. doi: 10.1097/00006534-200009030-00024. [DOI] [PubMed] [Google Scholar]
- 6.Hyakusoku H, Fumiiri M. The square flap method. Br J Plast Surg. 1987;40:40–46. doi: 10.1016/0007-1226(87)90009-9. [DOI] [PubMed] [Google Scholar]
- 7.Fraulin FO, Thomson HG. First webspace deepening: comparing the four-flap and five-flap Z-plasty. Which gives the most gain? Plast Reconstr Surg. 1999;104:120–128. [PubMed] [Google Scholar]
- 8.Lewis RC, Nordyke MD, Duncan KH. Web space reconstruction with a M-V flap. J Hand Surg Am. 1988;13:40–43. doi: 10.1016/0363-5023(88)90197-9. [DOI] [PubMed] [Google Scholar]
- 9.Ostrowski DM, Feagin CA, Gould JS. A three-flap web-plasty for release of short congenital syndactyly and dorsal adduction contracture. J Hand Surg Am. 1991;16:634–641. doi: 10.1016/0363-5023(91)90186-f. [DOI] [PubMed] [Google Scholar]
- 10.Erba P, Ogawa R, Vyas R, et al. The reconstructive matrix: a new paradigm in reconstructive plastic surgery. Plast Reconstr Surg. 2010;126:492–498. doi: 10.1097/PRS.0b013e3181de232b. [DOI] [PubMed] [Google Scholar]
- 11.Ogawa R, Hyakusoku H, Murakami M, et al. Reconstruction of axillary scar contractures–retrospective study of 124 cases over 25 years. Br J Plast Surg. 2003;56:100–105. doi: 10.1016/s0007-1226(03)00035-3. [DOI] [PubMed] [Google Scholar]
- 12.Ogawa R, Pribaz JJ. Diagnosis, assessment, and classification of scar contractures. In: Hyakusoku H, Orgill DP, Teot L, editors. Atlas of Burn Reconstructive Surgery. Berlin-Heidelberg:: Springer; 2010. [Google Scholar]
- 13.Hyakusoku H, Yamamoto T, Fumiiri M. The propeller flap method. Br J Plast Surg. 1991;44:53–54. doi: 10.1016/0007-1226(91)90179-n. [DOI] [PubMed] [Google Scholar]
- 14.Chin T, Hyakusoku H, Kubo K, et al. Modified square flap method. J Plast Reconstr Aesthet Surg. 2008;61:1515. doi: 10.1016/j.bjps.2008.05.037. [DOI] [PubMed] [Google Scholar]


