Supplemental Digital Content is available in the text.
Abstract
Summary:
Among the many advances in local anesthesia of the hand, some of the most significant changes in the last 5 years have been the following: (1) the acceptance of safety of locally infiltrated epinephrine with lidocaine for hemostasis, which has removed the need for sedation, brachial plexus blocks, and general anesthesia for most common hand surgery operations and minor hand trauma. (2) The elimination of the 2 injection finger block technique in favor of the single injection palmar block. (3) Local anesthesia can now be consistently injected in the hand with minimal pain. (4) Liposomal release of local anesthetic after injection into the surgical site can provide pain control up to 3 days. This article reviews the impact and best evidence related to these changes.
Local anesthesia in the hand has changed a great deal in the last 10 years. The aim of this update is to bring the reader up to speed with the most important changes and to provide a summary of current evidence-based literature regarding recent major changes in the use of local anesthesia in the hand.
THE REMOVAL OF THE NEED FOR THE TOURNIQUET, SEDATION, AND PROXIMAL BLOCKS BY MIXING EPINEPHRINE WITH LOCAL ANESTHESIA IN THE HAND AND FINGER
The long-held belief that epinephrine causes finger necrosis has been disproven.1–4 As a result, the tourniquet has been replaced with finger and hand injection of epinephrine and lidocaine for hemostasis by many practitioners for many procedures.5–7 The dosage and location of local anesthetic infiltration for tourniquet-free common hand surgery operations has been published8 (Table 1). “Wide-awake local anesthesia no tourniquet” (WALANT) technique has been published widely for carpal tunnel surgery,9 flexor tendon repair,10 tendon transfer,11 Dupuytren’s contracture,12 and trapeziectomy.13
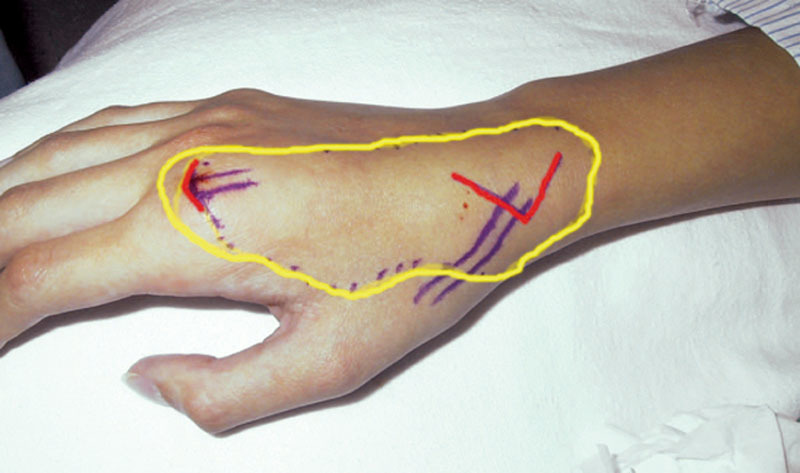
Table 1.
Typical Volumes and Concentrations Used for Tumescent Local Anesthesia in Wide-Awake Hand Surgery
INCREASED PATIENT CONVENIENCE AND DISCOMFORT WITH PURE LOCAL ANESTHESIA FOR CARPAL TUNNEL RELEASE
There is level III evidence that patients who have had wide-awake carpal tunnel release were just as satisfied with their anesthesia as those who have had sedation, but their incidence of adverse reactions such as nausea and vomiting was less while the convenience of their surgical process was increased.14 In addition, their need for preoperative testing and their time in hospital on the day of surgery were greatly reduced.
There is level II evidence that patients who had bilateral carpal tunnel surgery preferred epinephrine to tourniquet hemostasis for their operations performed at the same sitting.15 They found the pain of the tourniquet to be over twice the pain of the local anesthetic injection.
A study of 15 patients who had local anesthesia in one hand for carpal tunnel release and Bier block for the other hand provided level III evidence that local anesthesia was cheaper, was more expeditious, and had less tourniquet time.16
COST/EFFICIENCY/SAFETY OF WIDE-AWAKE CARPAL TUNNEL SURGERY PERFORMED WITH FIELD STERILITY OUTSIDE THE MAIN OPERATING ROOM
Obviating the need for the tourniquet and sedation has permitted moving simple operations such as carpal tunnel and trigger finger release to minor procedure rooms outside of the main operating room. This has resulted in greatly increased efficiency and convenience while greatly reducing costs.17–19
Carpal tunnel surgery performed with field sterility outside of the main operating room is one-fourth the cost of the procedure performed under pure local anesthesia inside the main operating room, even without sedation or the presence of an anesthesia provider.20 The same study also demonstrated that twice as many carpal tunnels could be performed in the same amount of time outside the main operating room as in the main operating room. The main sources of decrease in cost were personnel as only 1 nurse was required instead of 3. The cost of processing patients and unnecessary full sterility were also greatly reduced.
There is also a study of over 1500 patients which provided level IV evidence that carpal tunnel surgery can be performed with field sterility with an acceptably low risk of infection.21 Only 6 of the patients had superficial infections; none had deep infections requiring incision and drainage or intravenous antibiotics. None of those patients got preoperative antibiotics.
There have been great strides in the increase of patient safety with sedation in the last 10 years. However, there is no question that the safest sedation is no sedation. The elimination of the tourniquet has eliminated the need for sedation for most patients.
IMPROVED OUTCOMES WITH HAND OPERATIONS PERFORMED UNDER PURE LOCAL ANESTHESIA WITHOUT TOURNIQUET OR SEDATION
A large series of wide-awake flexor tendon repairs revealed that there were no ruptures in all of the patients who followed the proper postoperative protocol (level IV evidence).22 The authors attributed this to 3 main factors. First, the patients saw and remembered the repair working during the surgery and were educated by the surgeon during the procedure. Second, the patients took the fingers through full flexion and extension to demonstrate that the repair was solid enough not to gap to avoid rupture. Seven percent of the time, the surgeons observed intraoperative gapping from sutures not snugged tightly enough and repaired the gap before the skin was closed to avoid rupture. Third, seeing no gap gave the surgeons and therapists confidence to start true active movement after surgery, as opposed to place and hold.
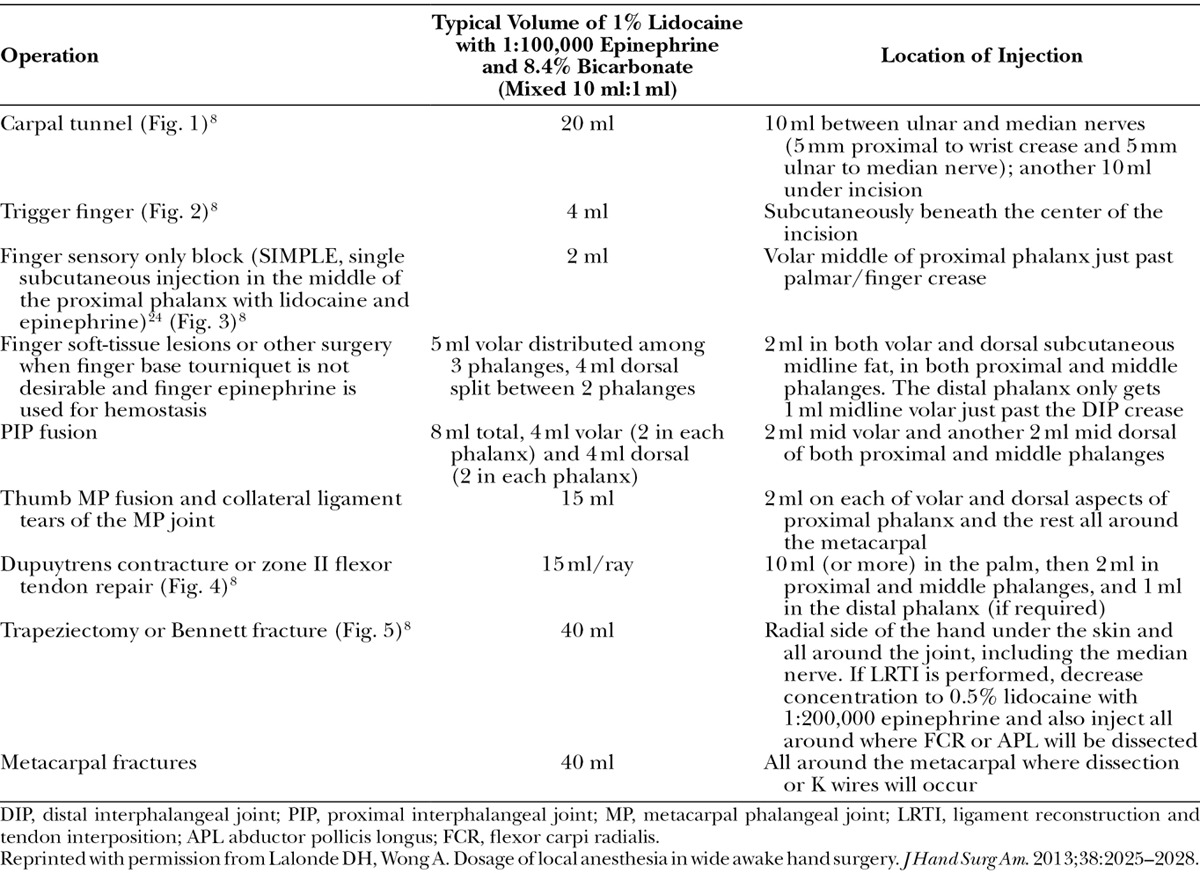
The ability to determine the proper tension with tendon transfers of extensor indicis to extensor pollicis longus has been demonstrated (level IV evidence).11 Patients are able to demonstrate during the surgery that the transfer is too tight or too loose, and the surgeon can adjust the tension before the skin is closed (Fig. 1).
Fig. 1.
Local anesthesia injection for extensor indicis to extensor pollicis longus tendon transfer. The circled area was injected with 30 ml of 1% lidocaine with 1:100,000 epinephrine 30 minutes before the operative procedure. Red lines indicate incisions. Purple lines outline the extensor indicis proprius and extensor pollicis longus tendons. Reprinted with permission from Bezuhly M, Sparkes GL, Higgins A, et al. Immediate thumb extension following extensor indicis proprius-to-extensor pollicis longus tendon transfer using the wide-awake approach. Plast Reconstr Surg. 2007;119:1507–1512.
MINIMIZING THE PAIN OF LOCAL ANESTHETIC INJECTION IN THE FINGER AND HAND
The first texts of local anesthesia written by Braun and Harris20 stated that the finger should be blocked with 2 web space injections because the palmar skin was more sensitive than web space skin.
There is level II evidence that volunteers who had both hands injected preferred the single subcutaneous injection in the middle of the proximal phalanx with lidocaine and epinephrine palmar injection to the 2 injection web space technique23 (Fig. 2). There is also level I evidence from 78 volunteers who had both hands poked with needles in 2013 that needle pokes in the palmar finger skin do not hurt more than needle pokes in the web space skin.24 The 2 dorsal injection block is no longer best evidence practice.
Fig. 2.
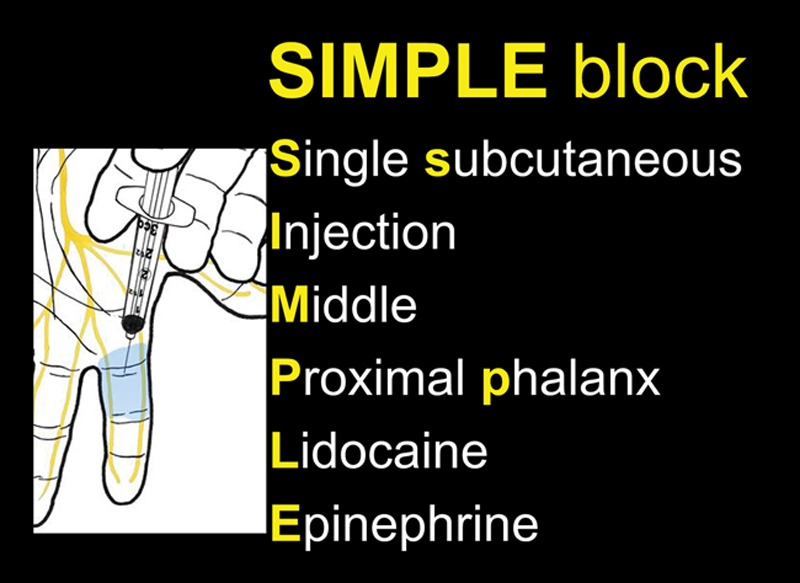
SIMPLE block—Single Subcutaneous Injection in the Middle of the Proximal Phalanx with Lidocaine and Epinephrine (2 ml).
There is level II evidence that a single subcutaneous injection in the middle of the proximal phalanx with lidocaine and epinephrine block given over 60 seconds hurts less than the same block administered over 8 seconds.25 It only takes a minute to give a minimally painful finger block. This adds to many other articles that support slow injection of local anesthetics for decreased pain.
Large areas of the hand, wrist, and forearm can be injected with minimal pain to the patient if the technique is carefully performed26 (See Video 1, Supplemental Digital Content 1, which demonstrates a flexor tendon repair injection technique in Part 1, http://links.lww.com/PRSGO/A32. Part 2 demonstrates several other wide-awake hand operations, http://links.lww.com/PRSGO/A34).
Video 1.

See video, Supplemental Digital Content 1, which demonstrates wide awake flexor tendon repair in Part 1, http://links.lww.com/PRSGO/A32, and tenolysis, carpal tunnel, Dupuytren, trigger finger, thumb ligament repair, thumb fusion, hand fractures, spaghetti wrist, and tendon transfer in Part 2, http://links.lww.com/PRSGO/A34. Reprinted with permission from Mustoe TA, Buck DW II, Lalonde DH. The safe management of anesthesia, sedation and pain in plastic surgery. Plast Reconstr Surg. 2010;126:165e–176e.
The 10 principles of minimal pain local anesthetic injection technique are the following27: (1) buffer the lidocaine and epinephrine with 10 ml:1 ml of 8.4% bicarbonate (level I evidence)28–30; (2) warm the local anesthetic31 (level I evidence); (3) distract the patient (look away, music, etc.) or the area of injection (pressure, light pinch near the injection site); (4) use a 27- or 30-gauge needle (level II evidence)32; (5) insert the needle more perpendicular than parallel to the skin (level II evidence)33; (6) stabilize the syringe with the other hand to avoid needle wobble and have the thumb on the plunger before entering the skin; (7) inject 0.5 ml under the dermis rather than in the dermis34 and pause until the patient says the needle pain is gone; (8) inject an additional 2 ml before moving the needle and then inject antegradely while moving the needle very slowly with 1 cm of local always palpable or visible ahead of the needle; (9) reinsert the needle within 1 cm of blanched skin; and (10) learn from each patient you inject by asking them to tell you the number of times they feel pain during the injection process.
Using the above principles of minimal pain injection technique, a series of 25 consecutive medical students and residents (level IV evidence) were able to consistently reproduce minimal pain injection on their first attempt at carpal tunnel injection.35
It takes an average of 5 minutes to consistently have the patient only feel the first poke of a 27-gauge needle when injecting local anesthesia for carpal tunnel surgery9 (See Video 2, Supplemental Digital Content 2, which demonstrates how to inject local anesthesia with minimal pain for carpal tunnel surgery, http://links.lww.com/PRS/A212).
Video 2.

See video, Supplemental Digital Content 2, which demonstrates how to inject local anesthesia with minimal pain for carpal tunnel surgery, http://links.lww.com/PRS/A212. Reprinted with permission from Lalonde DH. “Hole-in-one” local anesthesia for wide-awake carpal tunnel surgery. Plast Reconstr Surg. 2010;126:1642–1644.
There is level I evidence that injecting the carpal tunnel and the carpal tunnel incision generate less patient pain than injecting the carpal tunnel skin alone.36
LOCAL ANESTHESIA FOR ENDOSCOPIC CARPAL TUNNEL RELEASE
There is level II evidence that endoscopic carpal tunnel can be performed just as easily with local injection as with a Bier block but with less tourniquet time.37 A third trial provided level II evidence that local anesthesia reduces postoperative pain in endoscopic carpal tunnel release compared with intravenous regional anesthesia.38 All 3 of the above studies also pointed out that endoscopic carpal tunnel can be easily performed with local anesthetic infiltration into the operative site.
LIDOCAINE VERSUS BUPIVACAINE/ROPIVACAINE
There is level II evidence that the duration of action of lidocaine with epinephrine (10.4 hours) lasts about twice as long in digital blocks as the action of lidocaine without epinephrine (average 4.9 hours).39 Lidocaine is like an on/off switch; when lidocaine wears off, pain, touch, pressure, and temperature all come back at the same time.
On the other hand, bupivacaine does not come out like an on/off switch. There is level I evidence40 that pain relief in digital blocks with bupivacaine lasts only half as long (15 hours) as the return to normal sensation (30 hours). This is likely the reason that patients sometimes call surgeons after a digital bupivacaine block to say that their finger hurts but it is still numb. Some patients also find the prolonged numbness to touch annoying with bupivacaine blocks, particularly after the pain has returned.
There is level III evidence that patients who had carpal tunnel release with ropivacaine had longer pain relief than those who received lidocaine alone.41 However, longer acting anesthesia patients had a poorer first night’s sleep.
There is also level I evidence that the addition of epinephrine to bupivacaine digital blocks prolonged the duration of pain relief for only an additional 1.5 hours.36 The main purpose of adding epinephrine to bupivacaine digital blocks is therefore to provide hemostasis, not significant prolongation of anesthesia.
LIPOSOMAL LOCAL ANESTHETICS
Liposomal bupivacaine is a newly approved formulation of bupivacaine intended for single-dose infiltration at the surgical site for postoperative analgesia. Bupivacaine is slowly released from a liposomal vehicle and can provide prolonged pain analgesia longer than bupivacaine alone.42,43
Although there are no articles in PubMed on liposomal anesthetic in hand surgery as of yet, the authors are aware that many surgeons have been using this new medication for this purpose. There are written reports of prolonged pain relief with locally injected liposomal bupivacaine after breast augmentation, bunionectomy, and knee surgery.44,45
In the knee, total arthroplasty liposomal bupivacaine patients required opiate rescue medication at a mean of 9.3 hours versus the nonliposomal bupivacaine group at 6.4 hours.46
The advantages of prolonged pain relief are clear. The possible problems of not keeping the hand elevated, injuring it, or using it inappropriately because of the lack of discomfort remains to be seen.47
COMPLICATIONS OF LOCAL ANESTHESIA
Pure lidocaine and epinephrine local anesthesia with no monitoring have an amazingly good safety record in the dental literature.48,49 We also know that an upper limit of 7 mg/kg of lidocaine with epinephrine hand surgery is very safe because Burk et al46 showed that safe levels of lidocaine after 35 mg/kg were infused in liposuction. However, all local anesthetics can cause fatalities if given in large doses, and bupivacaine50,51 and ropivacaine52,53 are known to be more cardiotoxic than lidocaine, which has actually been used extensively as a rescue agent in cardiac arrest. Intralipid has been used for both bupivacaine54 and lidocaine55 rescue.
There are still no well-documented cases of finger infarction with lidocaine and epinephrine in the finger56, even with 1:1000 accidental finger epinephrine injection.57 There is level I evidence that 1 mg of phentolamine in 1 ml of saline reliably reverses epinephrine vasoconstriction in the finger, should this be required as a rescue agent.58 However, this is almost never required in clinical practice.59,60
CONCLUSION
The last 10 years have seen a great increase in the use of pure local anesthesia for hand surgery. With the new techniques to decrease the pain of local anesthesia injection, and the great cost savings of tourniquet-free pure local anesthesia, this trend is likely to continue.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was waived at the discretion of the Editor-in-Chief.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Lalonde D, Martin A. Epinephrine in local anesthesia in finger and hand surgery: the case for wide-awake anesthesia. J Am Acad Orthop Surg. 2013;21:443–447. doi: 10.5435/JAAOS-21-08-443. [DOI] [PubMed] [Google Scholar]
- 2.Thomson CJ, Lalonde DH, Denkler KA, et al. A critical look at the evidence for and against elective epinephrine use in the finger. Plast Reconstr Surg. 2007;119:260–266. doi: 10.1097/01.prs.0000237039.71227.11. [DOI] [PubMed] [Google Scholar]
- 3.Fitzcharles-Bowe C, Denkler K, Lalonde D. Finger injection with high-dose (1:1,000) epinephrine: does it cause finger necrosis and should it be treated? Hand. 2007;2:5–11. doi: 10.1007/s11552-006-9012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mann T, Hammert WC. Epinephrine and hand surgery. J Hand Surg Am. 2012;37:1254–1256; quiz 1257. doi: 10.1016/j.jhsa.2011.11.022. [DOI] [PubMed] [Google Scholar]
- 5.Lalonde D. Minimally invasive anesthesia in wide awake hand surgery. Hand Clin. 2014;30:1–6. doi: 10.1016/j.hcl.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 6.Leinberry CF, Rivlin M, Maltenfort M, et al. Treatment of carpal tunnel syndrome by members of the American Society for Surgery of the Hand: a 25-year perspective. J Hand Surg Am. 2012;37:1997–2003.e3. doi: 10.1016/j.jhsa.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 7.Shin EK, Bachoura A, Jacoby SM,, et al. Treatment of carpal tunnel syndrome by members of the American Association for Hand Surgery. Hand. 2012;7:351. doi: 10.1007/s11552-012-9455-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg Am. 2013;38:2025–2028. doi: 10.1016/j.jhsa.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 9.Lalonde DH. “Hole-in-one” local anesthesia for wide-awake carpal tunnel surgery. Plast Reconstr Surg. 2010;126:1642–1644. doi: 10.1097/PRS.0b013e3181f1c0ef. [DOI] [PubMed] [Google Scholar]
- 10.Lalonde DH, Kozin S. Tendon disorders of the hand. Plast Reconstr Surg. 2011;128:1e–14e. doi: 10.1097/PRS.0b013e3182174593. [DOI] [PubMed] [Google Scholar]
- 11.Bezuhly M, Sparkes GL, Higgins A, et al. Immediate thumb extension following extensor indicis proprius-to-extensor pollicis longus tendon transfer using the wide-awake approach. Plast Reconstr Surg. 2007;119:1507–1512. doi: 10.1097/01.prs.0000256071.00235.d0. [DOI] [PubMed] [Google Scholar]
- 12.Denkler K. Dupuytren’s fasciectomies in 60 consecutive digits using lidocaine with epinephrine and no tourniquet. Plast Reconstr Surg. 2005;115:802–810. doi: 10.1097/01.prs.0000152420.64842.b6. [DOI] [PubMed] [Google Scholar]
- 13.Farhangkhoee H, Lalonde J, Lalonde DH. Wide-awake trapeziectomy: video detailing local anesthetic injection and surgery. Hand (N Y) 2011;6:466–467. doi: 10.1007/s11552-011-9367-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davison PG, Cobb T, Lalonde DH. The patient’s perspective on carpal tunnel surgery related to the type of anesthesia: a prospective cohort study. Hand (N Y) 2013;8:47–53. doi: 10.1007/s11552-012-9474-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Braithwaite BD, Robinson GJ, Burge PD. Haemostasis during carpal tunnel release under local anaesthesia: a controlled comparison of a tourniquet and adrenaline infiltration. J Hand Surg Br. 1993;18:184–186. doi: 10.1016/0266-7681(93)90103-m. [DOI] [PubMed] [Google Scholar]
- 16.Tomaino MM, Ulizio D, Vogt MT. Carpal tunnel release under intravenous regional or local infiltration anaesthesia. J Hand Surg Br. 2001;26:67–68. doi: 10.1054/jhsb.2000.0426. [DOI] [PubMed] [Google Scholar]
- 17.Bismil M, Bismil Q, Harding D, et al. Transition to total one-stop wide-awake hand surgery service-audit: a retrospective review. JRSM Short Rep. 2012;3:23. doi: 10.1258/shorts.2012.012019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand. 2007;2:173. doi: 10.1007/s11552-007-9043-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chatterjee A, McCarthy JE, Montagne SA, et al. A cost, profit, and efficiency analysis of performing carpal tunnel surgery in the operating room versus the clinic setting in the United States. Ann Plast Surg. 2011;66:245–248. doi: 10.1097/SAP.0b013e3181db7784. [DOI] [PubMed] [Google Scholar]
- 20.Braun H, Harris ML. Chapter 16: operation on the extremities. In: Braun H,, Harris ML, editors. Local Anesthesia: Its Scientific Basis and Practical Use. Philadelphia, PA and New York, NY:: Lea & Febiger;; 1914. p. 367. [Google Scholar]
- 21.Leblanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y) 2011;6:60–63. doi: 10.1007/s11552-010-9301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Higgins A, Lalonde DH, Bell M, et al. Avoiding flexor tendon repair rupture with intraoperative total active movement examination. Plast Reconstr Surg. 2010;126:941–945. doi: 10.1097/PRS.0b013e3181e60489. [DOI] [PubMed] [Google Scholar]
- 23.Williams JG, Lalonde DH. Randomized comparison of the single-injection volar subcutaneous block and the two-injection dorsal block for digital anesthesia. Plast Reconstr Surg. 2006;118:1195–1200. doi: 10.1097/01.prs.0000237016.00941.96. [DOI] [PubMed] [Google Scholar]
- 24.Wheelock ME, Leblanc M, Chung B, et al. Is it true that injecting palmar finger skin hurts more than dorsal skin? New level 1 evidence. Hand (N Y) 2011;6:47–49. doi: 10.1007/s11552-010-9288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hamelin ND, St-Amand H, Lalonde DH, et al. Decreasing the pain of finger block injection: level II evidence. Hand (N Y) 2013;8:67–70. doi: 10.1007/s11552-012-9478-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mustoe TA, Buck DW, II, Lalonde DH. The safe management of anesthesia, sedation and pain in plastic surgery. Plast Reconstr Surg. 2010;126:165e–176e. doi: 10.1097/PRS.0b013e3181ebe5e9. [DOI] [PubMed] [Google Scholar]
- 27.Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg. 2013;132:675–684. doi: 10.1097/PRS.0b013e31829ad1e2. [DOI] [PubMed] [Google Scholar]
- 28.Lee HJ, Cho YJ, Gong HS, et al. The effect of buffered lidocaine in local anesthesia: a prospective, randomized, double-blind study. J Hand Surg Am. 2013;38:971–975. doi: 10.1016/j.jhsa.2013.02.016. [DOI] [PubMed] [Google Scholar]
- 29.Vossinakis IC, Stavroulaki P, Paleochorlidis I, et al. Reducing the pain associated with local anaesthetic infiltration for open carpal tunnel decompression. J Hand Surg Br. 2004;29:399–401. doi: 10.1016/j.jhsb.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 30.Frank SG, Lalonde DH. How acidic is the lidocaine we are injecting, and how much bicarbonate should we add? Can J Plast Surg. 2012;20:71–73. doi: 10.1177/229255031202000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hogan ME, vanderVaart S, Perampaladas K, et al. Systematic review and meta-analysis of the effect of warming local anesthetics on injection pain. Ann Emerg Med. 2011;58:86–98.e1. doi: 10.1016/j.annemergmed.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Watts AC, Gaston P, Hooper G. Randomized trial of buffered versus plain lidocaine for local anaesthesia in open carpal tunnel decompression. J Hand Surg Br. 2004;29:30–31. doi: 10.1016/j.jhsb.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 33.Martires KJ, Malbasa CL, Bordeaux JS. A randomized controlled crossover trial: lidocaine injected at a 90-degree angle causes less pain than lidocaine injected at a 45-degree angle. J Am Acad Dermatol. 2011;65:1231–1233. doi: 10.1016/j.jaad.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 34.Arndt KA, Burton C, Noe JM. Minimizing the pain of local anesthesia. Plast Reconstr Surg. 1983;72:676–679. doi: 10.1097/00006534-198311000-00017. [DOI] [PubMed] [Google Scholar]
- 35.Farhangkhoee H, Lalonde J, Lalonde DH. Teaching medical students and residents how to inject local anesthesia almost painlessly. Can J Plast Surg. 2012;20:169–172. doi: 10.1177/229255031202000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patil S, Ramakrishnan M, Stothard J. Local anaesthesia for carpal tunnel decompression: a comparison of two techniques. J Hand Surg Br. 2006;31:683–686. doi: 10.1016/j.jhsb.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 37.Nabhan A, Steudel WI, Dedeman L, et al. Subcutaneous local anesthesia versus intravenous regional anesthesia for endoscopic carpal tunnel release: a randomized controlled trial. J Neurosurg. 2011;114:240–244. doi: 10.3171/2008.2.17395. [DOI] [PubMed] [Google Scholar]
- 38.Sørensen AM, Dalsgaard J, Hansen TB. Local anaesthesia versus intravenous regional anaesthesia in endoscopic carpal tunnel release: a randomized controlled trial. J Hand Surg Eur Vol. 2013;38:481–484. doi: 10.1177/1753193412453664. [DOI] [PubMed] [Google Scholar]
- 39.Thomson CJ, Lalonde DH. Randomized double-blind comparison of duration of anesthesia among three commonly used agents in digital nerve block. Plast Reconstr Surg. 2006;118:429–432. doi: 10.1097/01.prs.0000227632.43606.12. [DOI] [PubMed] [Google Scholar]
- 40.Calder K, Chung B, O’Brien C, et al. Bupivacaine digital blocks: how long is the pain relief and temperature elevation? Plast Reconstr Surg. 2013;131:1098–1104. doi: 10.1097/PRS.0b013e3182865dbb. [DOI] [PubMed] [Google Scholar]
- 41.Chan ZH, Balakrishnan V, McDonald A. Short versus long-acting local anaesthetic in open carpal tunnel release: which provides better preemptive analgesia in the first 24 hours? Hand Surg. 2013;18:45–47. doi: 10.1142/S0218810413500081. [DOI] [PubMed] [Google Scholar]
- 42.Saraghi M, Hersh EV. Three newly approved analgesics: an update. Anesth Prog. 2013;60:178–187. doi: 10.2344/0003-3006-60.4.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Owen RT. Bupivacaine liposome injectable suspension: a new approach to postsurgical pain. Drugs Today (Barc) 2013;49:475–482. doi: 10.1358/dot.2013.49.8.2006992. [DOI] [PubMed] [Google Scholar]
- 44.Lambrechts M, O’Brien MJ, Savoie FH, et al. Liposomal extended-release bupivacaine for postsurgical analgesia. Patient Prefer Adherence. 2013;7:885–890. doi: 10.2147/PPA.S32175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baxter R, Bramlett K, Onel E, et al. Impact of local administration of liposome bupivacaine for postsurgical analgesia on wound healing: a review of data from ten prospective, controlled clinical studies. Clin Ther. 2013;35:312–320.e5. doi: 10.1016/j.clinthera.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 46.Burk RW, 3rd, Guzman-Stein G, Vasconez LO. Lidocaine and epinephrine levels in tumescent technique liposuction. Plast Reconstr Surg. 1996;97:1379–1384. doi: 10.1097/00006534-199606000-00009. [DOI] [PubMed] [Google Scholar]
- 47.Brand P, Yancey P. The Gift of Pain. Grand Rapids, MI: Zondervan; 1997. [Google Scholar]
- 48.Jeske AH. Xylocaine: 50 years of clinical service to dentistry. Tex Dent J. 1998;115:9–13. [PubMed] [Google Scholar]
- 49.Gaffen AS, Haas DA. Survey of local anesthetic use by Ontario dentists. J Can Dent Assoc. 2009;75:649. [PubMed] [Google Scholar]
- 50.Dudley MH, Fleming SW, Garg U, et al. Fatality involving complications of bupivacaine toxicity and hypersensitivity reaction. J Forensic Sci. 2011;56:1376–1379. doi: 10.1111/j.1556-4029.2011.01829.x. [DOI] [PubMed] [Google Scholar]
- 51.Cordell CL, Schubkegel T, Light TR, et al. Lipid infusion rescue for bupivacaine-induced cardiac arrest after axillary block. J Hand Surg Am. 2010;35:144–146. doi: 10.1016/j.jhsa.2009.10.018. [DOI] [PubMed] [Google Scholar]
- 52.Gnaho A, Eyrieux S, Gentili M. Cardiac arrest during an ultrasound-guided sciatic nerve block combined with nerve stimulation. Reg Anesth Pain Med. 2009;34:278. doi: 10.1097/AAP.0b013e31819a1333. [DOI] [PubMed] [Google Scholar]
- 53.Hübler M, Gäbler R, Ehm B, et al. Successful resuscitation following ropivacaine-induced systemic toxicity in a neonate. Anaesthesia. 2010;65:1137–1140. doi: 10.1111/j.1365-2044.2010.06449.x. [DOI] [PubMed] [Google Scholar]
- 54.Harvey M, Cave G, Chanwai G, et al. Successful resuscitation from bupivacaine-induced cardiovascular collapse with intravenous lipid emulsion following femoral nerve block in an emergency department. Emerg Med Australas. 2011;23:209–214. doi: 10.1111/j.1742-6723.2011.01401.x. [DOI] [PubMed] [Google Scholar]
- 55.Dix SK, Rosner GF, Nayar M, et al. Intractable cardiac arrest due to lidocaine toxicity successfully resuscitated with lipid emulsion. Crit Care Med. 2011;39:872–874. doi: 10.1097/CCM.0b013e318208eddf. [DOI] [PubMed] [Google Scholar]
- 56.Denkler KA. Comprehensive review of epinephrine in the finger: to do or not to do. Plast Reconstr Surg. 2001;108:112. doi: 10.1097/00006534-200107000-00017. [DOI] [PubMed] [Google Scholar]
- 57.Muck AE, Bebarta VS, Borys DJ, et al. Six years of epinephrine digital injections: absence of significant local or systemic effects. Ann Emerg Med. 2010;56:270–274. doi: 10.1016/j.annemergmed.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 58.Nodwell T, Lalonde D. How long does it take phentolamine to reverse adrenaline-induced vasoconstriction in the finger and hand? A prospective, randomized, blinded study: the Dalhousie project experimental phase. Can J Plast Surg. 2003;11:187–190. doi: 10.1177/229255030301100408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lalonde D, Bell M, Benoit P, et al. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie Project clinical phase. J Hand Surg Am. 2005;30:1061–1067. doi: 10.1016/j.jhsa.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 60.Lalonde DH. Reconstruction of the hand with wide awake surgery. Clin Plast Surg. 2011;38:761–769. doi: 10.1016/j.cps.2011.07.005. [DOI] [PubMed] [Google Scholar]


