Abstract
Summary:
The reconstruction of defects around the knee often poses a challenge due to the limited availability of local soft tissues. Indeed, this same problem is encountered when attempting to revise a below-knee amputation stump. Moreover, due to a paucity of recipient vessels in those who have undergone previous amputation secondary to trauma, free-flap reconstruction is often challenging and not always successful. We report a case of a reverse anterolateral thigh (ALT) flap used to revise a long below-knee amputation stump. Previous reports in the literature attest to the versatility of the reverse ALT to cover defects around the knee and proximal tibia, but to our knowledge, this is the first report of a reverse ALT reaching to the mid-tibial level.
Several local options exist for the reconstruction of defects around the knee joint1–4; however, the success and versatility of these flaps are limited by their relatively short pedicle lengths and small size of the skin flaps. For these reasons, the reverse anterolateral thigh (ALT) has become a popular choice in the reconstruction of knee and occasionally proximal tibial defects due to its long pedicle length, large skin flap size,5 and the ability to harvest vascularized tensor fascia lata with the flap to reconstruct the extensor mechanism of the knee (Table 1).6 When tackling defects that extend to the level of the middle third of the tibia, however, local fasciocutaneous, muscle, or free flaps tend to be used. Indeed, this area is perceived to be beyond the arc of rotation of a reverse ALT. However, we present a case recently encountered at our institution where a reverse ALT pedicled to the mid-tibial level was successfully performed to revise a below-knee amputation (BKA) stump.
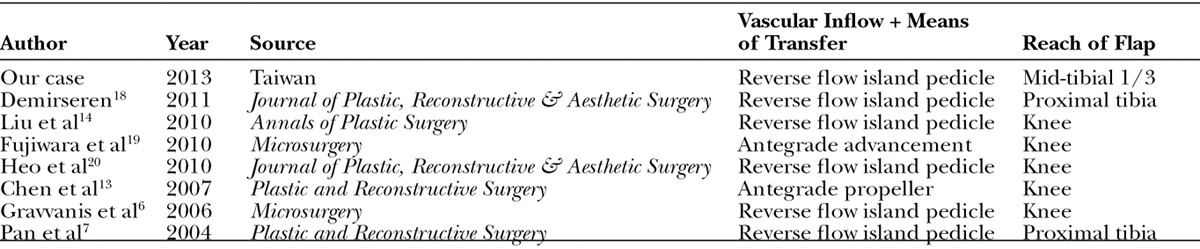
Table 1.
Summary of Local ALT Flaps to Distal Defects Reported in the Literature
CASE PRESENTATION
A 30-year-old patient presented with an intractable, unstable scar over the distal aspect of his long BKA stump that was hindering his ability to wear a prosthesis (Fig. 1). He declined tibial shortening and preferred to undergo a reconstructive procedure. Plans were therefore made to debride the area of unstable scar (Fig. 2) and reconstruct with a trapezius perforator flap (TPF). This option was selected as the patient wanted to avoid further scarring to either leg, and as we were planning to perform the microvascular anastomosis to the popliteal vessels in the lateral decubitus position, the TPF represented a flap that could be conveniently harvested while maintaining this patient position. Unfortunately, however, the TPF failed due to venous congestion secondary to postoperative pedicle compression. Indeed, given the paucity of recipient vessels and our desire to avoid another microanastomosis to the popliteal system, we selected a reverse ALT for secondary reconstruction. A proximal perforator was identified using hand-held Doppler, and a 15 × 8 cm skin paddle was designed around this. Choosing a proximal perforator is of paramount importance as it results in maximal pedicle length when raising the ALT as a reverse flow flap. The flap was then raised on one musculocutaneous perforator and dissection continued distally along the descending branch of the lateral circumflex femoral artery (LCFA). A vascular clamp was then applied to the proximal LCFA to confirm good dermal bleeding of the skin flap based on retrograde flow through the distal communicating branches of the LCFA and the lateral superior geniculate artery (LSGA) and profunda femoris. Once this was confirmed, we could confidently ligate the LCFA proximally and continue with the distal dissection. As we needed a very long pedicle, we had to dissect to within the vicinity of the communicating branches between the descending branch of the LCFA and the LSGA/profunda femoris. At this point, located between 3 and 10 cm above the lateral patella,7 we included a cuff of vastus lateralis (Fig. 3) to preserve all collateral communications between these 2 systems and prevent any vascular compromise to the flap. We then rotated the flap 180 degrees and were able to inset under no tension into the defect over the distal tibial stump. The donor site closed primarily and no postoperative complications were encountered. The resurfaced tibial stump and donor site both subsequently healed well (Fig. 4), and the patient is now fully mobile using a below-knee prosthesis.
Fig. 1.

Preoperative appearance of BKA stump.
Fig. 2.

BKA stump post debridement.
Fig. 3.
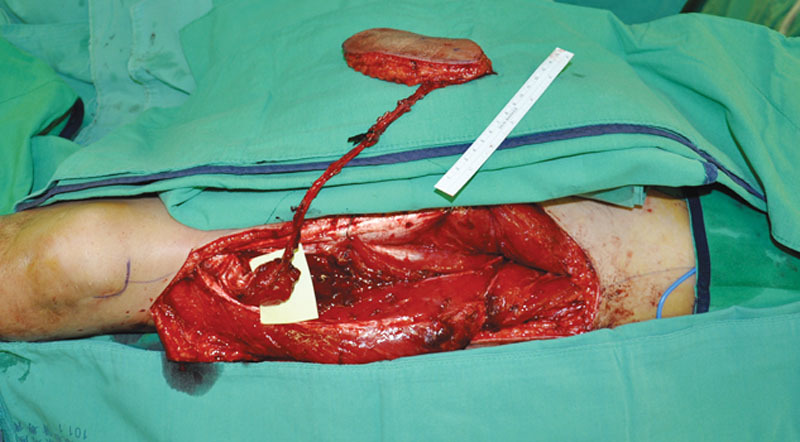
Reverse ALT raised on proximal perforator with cuff of vastus lateralis protecting the pedicle distally.
Fig. 4.

Postoperative appearance at 2 mo.
DISCUSSION
The reverse ALT is a well-recognized reconstructive option when tackling defects around the knee and upper third of the tibia.6–9 The vascular basis for the reverse ALT is the anastomosis between the descending branch of the LCFA and the LSGA or profunda femoris, which is located approximately 3–10 cm above the lateral superior patella border.7 The skin flap itself is nourished by musculocutaneous or septocutaneous perforators of the LCFA system, and the arc of rotation of the flap is a circle, the radius of which is equal to the distance between the perforating vessel at its point of entry into the flap, and the pivot point, located at the distal most extent of the descending branch of LCFA dissection. Local flap options around the knee and proximal tibia have short pedicles and are of limited size; moreover, the recipient vessels for possible free-flap reconstruction are deep and can therefore be technically demanding to access and anastomose to. In this setting, the reverse ALT has grown in popularity.6–14
When tackling the problem of revising a BKA stump, it is important to maintain tibial length to reduce the work required by the hamstrings and quadriceps to flex and extend the prosthesis while ambulating. Some authors recommend the use of a free latissimus dorsi (LD) to provide muscular coverage of amputation stumps,15,16 whereas others suggest a variety of free flaps depending on the situation.17 In the case of harvesting a free LD, the resultant weakness in ipsilateral arm adduction may be a consideration in a young active patient. Indeed, the relative extra upper body work required by patients during the rehabilitation process after losing a limb may well make the LD a less attractive reconstructive option in this setting. Moreover, with any free-tissue transfer to a BKA stump, the ease with which the recipient vessels can be accessed and their inherent quality remains a challenge and can be a source of complications.
The reverse ALT was first described by Zhang10 in 1990 and has since become a popular choice in the reconstruction of large defects around the knee, proximal tibia, and even proximal calf.6–9,11–14 With its extremely long pedicle, wide arc of rotation, and large skin flap size, it certainly is a versatile reconstructive option. Moreover, the need to access deep recipient vessels is avoided and donor site morbidity is minimal.10 Drawbacks include the long pedicle dissection, especially if the flap is raised on perforators of the transverse branch of the LCFA, and risk of venous congestion or arterial compromise due to pedicle compression or kinking upon transfer. Indeed, venous congestion secondary to a long retrograde venous outflow is a fear among reconstructive surgeons with this flap. This was not encountered with our case; however, if encountered, this can be overcome by supercharging a vein from the flap to a superficial vein around the knee.
CONCLUSIONS
We feel that in situations where local options are not available, and the recipient vessels are unreliable or challenging to access, the reverse ALT represents a robust and relatively straightforward reconstructive strategy when dealing with defects around the knee, proximal tibia, and even those approaching the middle tibial third. It is a useful option when faced with the challenge of revising a BKA stump, avoids the need to access deep recipient vessels, and results in minimal donor site morbidity.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.McCraw JB, Fishman JH, Sharzer LA. The versatile gastrocnemius myocutaneous flap. Plast Reconstr Surg. 1978;62:15–23. doi: 10.1097/00006534-197807000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Petty CT, Hogue RJ., Jr Closure of an exposed knee joint by use of a sartorius muscle flap: case report. Plast Reconstr Surg. 1978;62:458–461. doi: 10.1097/00006534-197809000-00032. [DOI] [PubMed] [Google Scholar]
- 3.Arnold PG, Prunes-Carrillo F. Vastus medialis muscle flap for functional closure of the exposed knee joint. Plast Reconstr Surg. 1981;68:69–72. doi: 10.1097/00006534-198107000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Hallock JG. Local knee random fasciocutaneous flaps. Ann Plast. 1989;23:289–296. doi: 10.1097/00000637-198910000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Mosahebi A, Disa JJ, Pusic AL. The use of the extended anterolateral thigh flap for reconstruction of massive oncologic defects. Plast Reconstr Surg. 2008;112:492–496. doi: 10.1097/PRS.0b013e31817dc4c0. [DOI] [PubMed] [Google Scholar]
- 6.Gravvanis AI, Tsoutsos DA, Karakitsos D, et al. Application of the pedicled anterolateral thigh flap to defects from the pelvis to the knee. Microsurgery. 2006;26:432–438. doi: 10.1002/micr.20267. [DOI] [PubMed] [Google Scholar]
- 7.Pan SC, Yu JC, Shieh SJ, et al. Distally based anterolateral thigh flap: an anatomic and clinical study. Plast Reconstr Surg. 2004;114:1768–1775. doi: 10.1097/01.prs.0000142416.91524.4c. [DOI] [PubMed] [Google Scholar]
- 8.Yildirim S, Avci G, Akan M, et al. Anterolateral thigh flap in the treatment of postburn flexion contractures of the knee. Plast Reconstr Surg. 2003;111:1630–1637. doi: 10.1097/01.PRS.0000055017.39339.C2. [DOI] [PubMed] [Google Scholar]
- 9.Gravvanis AI, Iconomou TG, Panayotou PN, et al. Medial gastrocnemius muscle flap versus distally based anterolateral thigh flap: conservative or modern approach to the exposed knee joint? Plast Reconstr Surg. 2005;116:932–934. doi: 10.1097/01.prs.0000180888.41899.a8. [DOI] [PubMed] [Google Scholar]
- 10.Zhang G. [Reversed anterolateral thigh island flap and myocutaneous flap transplantation]. Zhonghua Yi Xue Za Zhi. 1990;70:676–678. [PubMed] [Google Scholar]
- 11.Lin RY, Chien WH. Experiences in harvesting type II distally based anterolateral thigh flaps. Plast Reconstr Surg. 2006;118:282–284. doi: 10.1097/01.prs.0000222243.18349.52. [DOI] [PubMed] [Google Scholar]
- 12.Wang XC, Lu Q, Li XF, et al. Reversed anterolateral thigh adipofascial flap for knee and proximal calf defects. Burns. 2008;34:868–872. doi: 10.1016/j.burns.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Chen CY, Hsieh CH, Kuo YR, et al. An anterolateral thigh perforator flap from the ipsilateral thigh for soft-tissue reconstruction around the knee. Plast Reconstr Surg. 2007;120:470–473. doi: 10.1097/01.prs.0000267432.03348.97. [DOI] [PubMed] [Google Scholar]
- 14.Liu TY, Jeng SF, Yang JC, et al. Reconstruction of the skin defect of the knee using a reverse anterolateral thigh island flap: cases report. Ann Plast. 2010;64:198–201. doi: 10.1097/SAP.0b013e31819bd6f7. [DOI] [PubMed] [Google Scholar]
- 15.Kim YH, Youn S, Sung IH, et al. Latissimus dorsi flap coverage of soft tissue defect following below-knee amputation: emphasis on flap design and recipient vessels. Eur J. 2013;23:603–610. doi: 10.1007/s00590-012-1023-y. [DOI] [PubMed] [Google Scholar]
- 16.Tukiainen EJ, Saray A, Kuokkanen HO, et al. Salvage of major amputation stumps of the lower extremity with latissimus dorsi free flaps. Scand J Plast Reconstr Surg Hand Surg. 2002;36:85–90. doi: 10.1080/028443102753575220. [DOI] [PubMed] [Google Scholar]
- 17.Kasabian AK, Colen SR, Shaw WW, et al. The role of microvascular free flaps in salvaging below-knee amputation stumps: a review of 22 cases. J Trauma. 1991;31:495–500. doi: 10.1097/00005373-199104000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Demirseren ME. Efenddioglu K. Demiralp CO. Clinical experience with a reverse-flow anterolateral thigh perforator flap for the reconstruction of soft-tissue defects of the knee and proximal lower leg. J Plast Reconstr Aesthet Surg. 2011;64:1613–1620. doi: 10.1016/j.bjps.2011.06.047. [DOI] [PubMed] [Google Scholar]
- 19.Fujiwara T. Chen CC. Ghetu N. Antegrade anterolateral thigh perforator flap advancement for soft-tissue reconstruction of the knee: case report. Microsurgery. 2010;30:549–552. doi: 10.1002/micr.20804. [DOI] [PubMed] [Google Scholar]
- 20.Heo C. Eun S. Bae R. Distally based anterolateral-thigh (ALT) flap with the aid of multidetector computed tomo graphy. J Plast Reconstr Aesthet Surg. 2010;63:e465–e468. doi: 10.1016/j.bjps.2009.08.009. [DOI] [PubMed] [Google Scholar]


