Abstract
Summary:
This is the first reported case of a patient who had a single-stage large-volume breast reconstruction with autologous fat grafting, following rotation flap approach (RoFA) mastectomy. The purpose of this case study was to evaluate the viability of reconstruction of the breast by autologous fat grafting alone, in the context of RoFA mastectomy. The hypothesis was that there would be minimal interval loss of autologous fat on the whole breast reconstruction side. Right RoFA mastectomy was used for resection of an invasive primary breast cancer and resulted in the right breast skin envelope. Eleven months later, the patient underwent grafting of 400 ml of autologous fat into the skin envelope and underlying pectoralis major muscle. Outcome was assessed by using a validated 3D laser scan technique for quantitative breast volume measurement. Other outcome measures included the BREAST-Q questionnaire and 2D clinical photography. At 12-month follow-up, the patient was observed to have maintenance of volume of the reconstructed breast. Her BREAST-Q scores were markedly improved compared with before fat grafting, and there was observable improvement in shape, contour, and symmetry on 2D clinical photography. The 2 new techniques, RoFA mastectomy and large-volume single-stage autologous fat grafting, were used in combination to achieve a satisfactory postmastectomy breast reconstruction. Novel tools for measurement of outcome were the 3D whole-body laser scanner and BREAST-Q questionnaire. This case demonstrates the potential for the use of fat grafting for reconstruction. Outcomes in a larger patient populations are needed to confirm these findings.
The purpose of this case study was to evaluate the viability of reconstruction of the breast by autologous fat grafting alone, in the context of rotation flap approach (RoFA) mastectomy. The hypothesis was that there would be minimal loss of autologous fat volume in the 12 months following surgery.
CASE REPORT
The patient is a 63-year-old woman who presented with screen-detected multicentric cancer of the right breast. She underwent RoFA mastectomy and sentinel lymph node biopsy. Histopathology showed 2 cancers in separate quadrants of the breast, 17 and 11 mm in size, both of low nuclear grade, and neither showing peritumoral vascular invasion. Lymphoscintigraphy for sentinel node biopsy was obtained by peritumoral injection around the larger of the 2 cancers, and the sentinel and 2 adjacent axillary lymph nodes were clear of metastatic disease. Although the tumor was hormone sensitive, the patient opted not to have adjuvant hormonal treatment. With a good prognostic outcome, low risk of cancer recurrence, she was an ideal candidate for autologous fat grafting.
At the time of presentation to the plastic surgeon for consideration of reconstruction, the patient had a large ptotic breast on the left and the skin envelope subsequent to the RoFA mastectomy on the right was capacious and supple (Fig. 1). The patient was keen to have the left breast reduced in size and was interested in reconstructive options for the right side, but not enthusiastic about either flap reconstructions or prosthetic implants due to perceived morbidity of these procedures. The concept of autologous fat grafting was explained to the patient, and she was warned that the outcome was not predictable and specifically that she was likely to experience some fat graft loss. She was willing to accept this outcome. Eleven months after mastectomy, she underwent right breast reconstruction with autologous fat grafting alone. In the same operation, she underwent a Wise pattern inferior pedicle left breast reduction, with the volume resected being guided by a preoperative volumetric assessment by 3D laser scan. These procedures were uncomplicated, and she was discharged from hospital on the first postoperative day. She had reconstruction of the nipple-areolar shape 2 months following mound reconstruction (Fig. 2) and had tattooing of the nipple-areolar reconstruction a further 3 months later (Fig. 3).
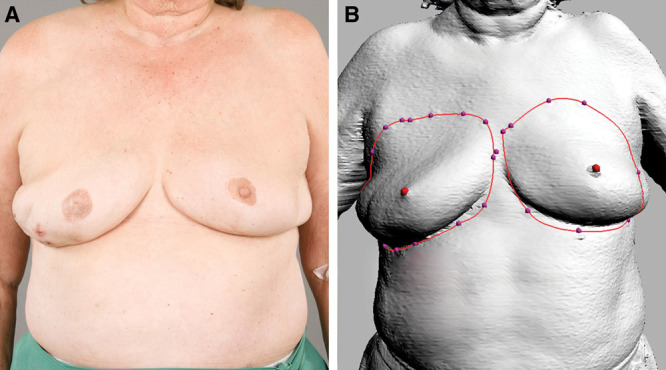
Fig. 1.
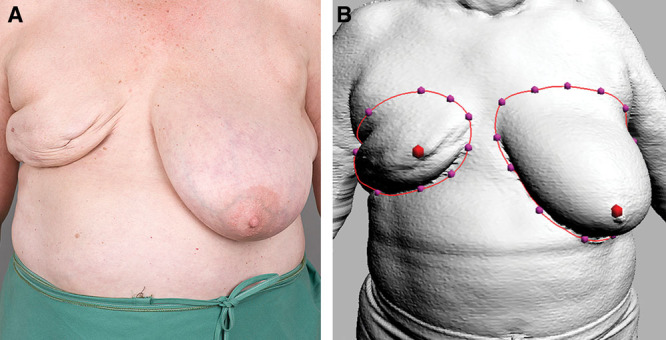
Preoperative clinical photograph of patient (A). 3D laser scan image with measured volumes (B). 3D breast volume measurement: left breast, 1469 ml; right breast, 251 ml.
Fig. 2.
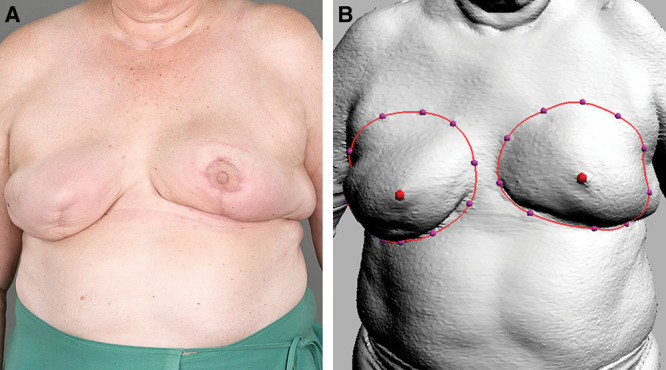
Postoperative (3 mo) clinical photograph of patient (A). 3D laser scan image with measured volumes (B). 3D breast volume measurement: left breast, 583 ml; right breast, 635 ml.
Fig. 3.
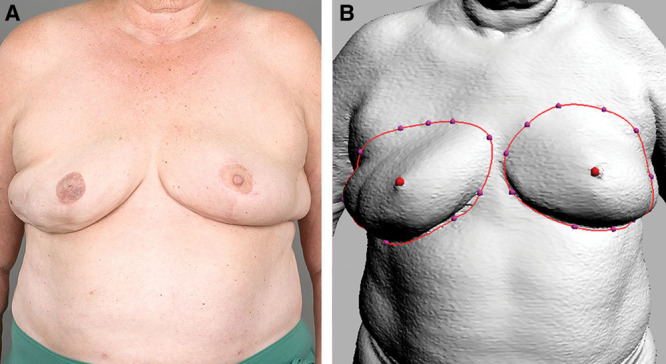
Postoperative (6 mo) clinical photograph of patient (A). 3D laser scan image with measured volumes (B). 3D breast volume measurement: left breast, 634 ml; right breast, 571 ml.
METHODS
The BREAST-Q questionnaire was completed preoperatively and was repeated at 3, 6, and 12 months postoperatively. The raw questionnaire data were converted using the Q-Score program found at the developer’s Web site (https://webcore.mskcc.org/breastq/). This provided summary scores for each BREAST-Q scale, ranging from 0 to 100 in 6 “domains” or areas of interest. The 3 “satisfaction” domains were satisfaction with breasts, satisfaction with outcome, and satisfaction with process of care. The 3 “well-being” domains were physical, psychosocial, and sexual well-being.
Three-dimensional (3D) laser scans were performed using a Cyberware whole-body laser scanner and the Cyslice software (Headus, Australia) to measure the volume of the breasts. This was done using the protocol previously described in the validation study by Yip et al.1 Image capture was performed using Cyscan (Cyberware), image analysis was performed using Cyslice (Headus) (metamorphosis), and statistical analysis was performed using Stata version 11.0 (StataCorp, College Station, TX). The patient was scanned preoperatively and at 3, 6, and 12 months postoperatively.
Operatively, the patient’s first procedure was the RoFA mastectomy as previously described by Dean et al.2 This technique involves a vertical incision from the areola, dropped medial to the breast axis, down toward the inframammary fold. The incision extends along the inframammary fold laterally to the anterior axillary line. The rotation flap that is created allows access for mastectomy, recruits skin to the apex of the breast, and prevents scarring in the medial half of the chest. Her second procedure was reconstruction of the whole breast with fat grafting and simultaneous left breast reduction using a Wise pattern inferior pedicle technique. One thousand milliliters of aspirate was harvested from the abdomen using the Lipivage System. Four hundred milliliters of filtered fat was then injected in layers using a vertical and horizontal fanning technique, creating tunnels in several directions within the mastectomy skin envelope. Injection of fat included the pectoral fascia and the pectoralis major muscle. The amount of tissue removed in the left breast reduction was 980 g.
RESULTS
Preoperative BREAST-Q scores indicated that the patient had good physical well-being but was unsatisfied with her breast area and had low sexual well-being (Table 1). In particular, she was very dissatisfied with wearing fitted clothes and how she looked naked in the mirror. The preoperative difference in breast size is shown in Figure 1.
Table 1.
Quality of Life Scales with BREAST-Q Scores Preoperatively and 3, 6, and 12 Months Postoperatively
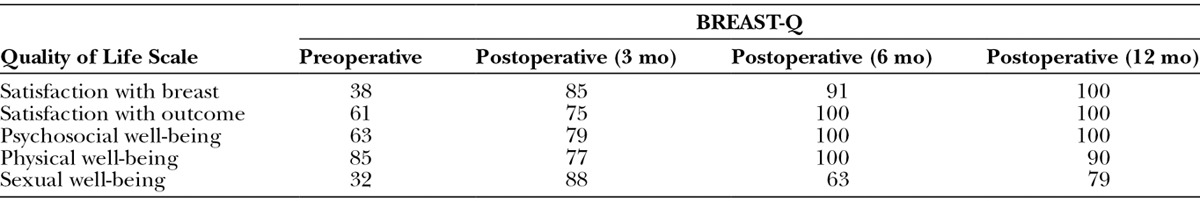
Postoperatively, the wounds healed without complication, and by 3 months, the mastectomy scar had become softer. The reconstructed breast was soft and nontender. The patient reported that she had lost 6 kg in the 6 months after surgery, and this was confirmed using scales and comparing her weight preoperatively. During the period between 6 and 12 months, she had lost a further 3.5 kg. At 3, 6, and 12 months postoperatively, she was very satisfied with the outcome of surgery (Table 1), and symmetry was objectively found to be better than preoperatively (Figs. 1–4). The volumes of the 3D laser scans taken preoperatively and at 3, 6, and 12 months postoperatively are shown beside her 2D clinical photography in Figures 1–4.
Fig. 4.
Postoperative (12 mo) clinical photograph of patient (A). 3D laser scan image with measured volumes (B). 3D breast volume measurement: left breast, 521 ml; right breast, 541 ml.
DISCUSSION
Autologous fat grafting for breast reconstruction is gaining popularity. The most encouraging article by Delay et al3 reported on the technique, results, and indications of fat injection on 880 procedures, spanning 10 years. Rigotti et al4 followed-up 137 radical mastectomy patients who underwent fat grafting over a 7.6-year period. He did not find an increased risk of cancer compared with the nontreated group. These results helped to dispel earlier concerns about the oncological risk of fat grafting. Earlier reports on fat grafting suggested that nodule formation and calcifications would interfere with breast cancer screening.5 In turn, concerns were raised regarding interpretation of mammographic findings leading to a higher false-positive cancer diagnosis. Studies since have found no evidence of fat grafting causing interference with breast cancer screening.6–8 Calcifications from fat grafting have a benign eggshell appearance.5
Now with increasing reports of success,3,4,6–12 and reports of patient satisfaction, surgeons are trying to establish techniques to provide the best results with fat grafting. Loss of volume can adversely affect patient satisfaction and may require further reconstructive procedures. Previous studies that report graft loss vary greatly in technique, amount lost, and methods in which loss was measured.4,6–10
The majority of cases reported in the literature discuss fat grafting for partial mastectomy defects or for aesthetic augmentation purposes. There is little reported on whole breast reconstruction. Panettiere et al13 documented success in whole breast reconstruction, but the grafting of fat was carried out in several sessions. Interestingly, in his patient, the mastectomy scar softened after fat grafting, as did the scar in the patient described in this case. Rigotti et al14 theorized that adipose-derived stem cells can restore ischemic tissue vascularization and organ function by recruitment of endothelial progenitor cells.
Using the 3D laser scanner, we were able to accurately measure and compare the maintenance of volume at intervals. The use of 3D laser scanners for assessment of patients undergoing breast reconstruction has been validated in previous studies.15,16 Yip et al1 validated the 3D laser scanner that has been assisting our unit in the preoperative preparation phase, the postoperative evaluation of results, and longer term assessment of outcome. This case demonstrated a volume loss of approximately 25% in a 12-month period. A better outcome when compared with estimated volume losses of 30–40% by Delay et al3 and 43.5% at 9 months by Beck et al.17
Compared with other techniques, the RoFA mastectomy resulted in a large skin envelope, which facilitated reconstruction and aided ptosis, giving a very natural-looking breast.
The majority of articles reporting patients’ perceptions on outcome do not have quantitative measurement of patient satisfaction.3,4,6–10 Patient satisfaction was simply registered as good, moderately good, or very good.3 The BREAST-Q was developed in 2009 to elicit and quantify patient perception of outcomes post augmentation, reduction, and reconstruction.18 The use of the BREAST-Q pre and post autologous fat grafting demonstrates interval improvement.
Our hypothesis that there would be minimal loss of breast volume in the reconstructed side was supported in this case. There was slight interval change with a volume difference of 64 ml between 3 and 6 months, then only 30 ml between 6 and 12 months. Interestingly, the 3D scanner detected increase in volume on the left reduction side despite the patient’s weight loss of 6 kg. Superimposing the 3D images, it can be observed that there was a slight difference in the breast border mapping from the body surface markers on the left.
CONCLUSION
This case has demonstrated promising results using 2 new techniques, the RoFA mastectomy and whole breast reconstruction with autologous fat grafting, and confirms the potential for fat grafting as an option for whole breast reconstruction.
ACKNOWLEDGMENTS
The authors wish to acknowledge David Summerhayes and Lynton Emerson, Medical Illustration and Media Unit, Flinders Medical Centre, and Philip Griffin, Head of Plastic Surgery, Flinders Medical Centre.
Footnotes
Presented at the Royal Australian College of Surgeons Annual Scientific Meeting August 2013. Accepted for Poster Presentation at the Breast Coordinated Care Conference, 2014, Washington, D.C.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by Flinders University, Adelaide, Australia.
REFERENCES
- 1.Yip JM, Mouratova N, Jeffery RM, et al. Accurate assessment of breast volume: a study comparing the volumetric gold standard (direct water displacement measurement of mastectomy specimen) with a 3D laser scanning technique. Ann Plast Surg. 2012;68:135–141. doi: 10.1097/SAP.0b013e31820ebdd0. [DOI] [PubMed] [Google Scholar]
- 2.Dean NR, Yip JM, Birrell S. Rotation flap approach mastectomy. ANZ J Surg. 2013;83:139–145. doi: 10.1111/ans.12008. [DOI] [PubMed] [Google Scholar]
- 3.Delay E, Garson S, Tousson G, et al. Fat injection to the breast: technique, results, and indications based on 880 procedures over 10 years. Aesthetic Surg J. 2009;29:360–376. doi: 10.1016/j.asj.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 4.Rigotti G, Marchi A, Stringhini P, et al. Determining the oncological risk of autologous lipoaspirate grafting for post-mastectomy breast reconstruction. Aesthetic Plast Surg. 2010;34:475–480. doi: 10.1007/s00266-010-9481-2. [DOI] [PubMed] [Google Scholar]
- 5.Rosing JH, Wong G, Wong MS, et al. Autologous fat grafting for primary breast augmentation: a systematic review. Aesthetic Plast Surg. 2011;35:882–890. doi: 10.1007/s00266-011-9691-2. [DOI] [PubMed] [Google Scholar]
- 6.Parrish JN, Metzinger SE. Autogenous fat grafting and breast augmentation: a review of the literature. Aesthetic Surg J. 2010;30:549–556. doi: 10.1177/1090820X10380859. [DOI] [PubMed] [Google Scholar]
- 7.Claro F, Jr, Figueiredo JC, Zampar AG, et al. Applicability and safety of autologous fat for reconstruction of the breast. Br J Surg. 2012;99:768–780. doi: 10.1002/bjs.8722. [DOI] [PubMed] [Google Scholar]
- 8.Carvajal J, Patiño JH. Mammographic findings after breast augmentation with autologous fat injection. Aesthetic Surg J. 2008;28:153–162. doi: 10.1016/j.asj.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Peer LA. Loss of weight and volume in human fat grafts: with postulation of a “cell survival theory”. Plast Reconstr Surg. 2007;119:775–785. [Google Scholar]
- 10.Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg. 2007;119:775–785. doi: 10.1097/01.prs.0000252001.59162.c9. [DOI] [PubMed] [Google Scholar]
- 11.Delaporte T, Delay E, Toussoun G, et al. [Breast volume reconstruction by lipomodeling technique: about 15 consecutive cases]. Ann Chir Plast Esthet. 2009;54:303–316. doi: 10.1016/j.anplas.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 12.Khouri RK, Eisenmann-Klein M, Cardoso E, et al. Brava and autologous fat grafting is a safe and effective breast augmentation alternative: results of a 6-year, 81-patient, prospective multicenter study. Plast Reconstr Surg. 2012;129:1173–1187. doi: 10.1097/PRS.0b013e31824a2db6. [DOI] [PubMed] [Google Scholar]
- 13.Panettiere P, Accorsi D, Marchetti L, et al. Large-breast reconstruction using fat graft only after prosthetic reconstruction failure. Aesthetic Plast Surg. 2011;35:703–708. doi: 10.1007/s00266-011-9670-7. [DOI] [PubMed] [Google Scholar]
- 14.Rigotti G, Marchi A, Galie M, et al. Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg. 2005;119:1409–1422. doi: 10.1097/01.prs.0000256047.47909.71. [DOI] [PubMed] [Google Scholar]
- 15.Losken A, Pinell XA, Sikoro K, et al. Autologous fat grafting in secondary breast reconstruction. Ann Plast Surg. 2011;66:518–522. doi: 10.1097/SAP.0b013e3181fe9334. [DOI] [PubMed] [Google Scholar]
- 16.Kovacs L, Eder M, Papadopulos NA, et al. Validating 3-dimensional imaging of the breast. Ann Plast Surg. 2005;55:695–696. doi: 10.1097/01.sap.0000186964.82170.4f. [DOI] [PubMed] [Google Scholar]
- 17.Beck M, Amar O, Bodin F, et al. Evaluation of breast lipofilling after sequelae of conservative treatment for cancer—a prospective study of ten cases. Eur J Plast Surg. 2011;35:1–8. [Google Scholar]
- 18.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–353. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]


