Abstract
Background:
The traditional long medial arm incision with its resultant scar is not acceptable. The author presents his long-term experience in performing the posterior scar brachioplasty with fascial suspension. The technique is a modification described by other authors. The aim of the author is to demonstrate the reasons for the choice of the posterior scar technique with fascial suspension.
Methods:
Between 1999 and 2012, the posterior scar technique with fascial suspension was used to treat 205 patients with brachial deformities. Age at operation ranged between 21 and 66 years. All patients were examined, and the author reviewed their medical charts during the follow-up period (29–98 mo). A Likert scale and an evaluation questionnaire were used to assess the aesthetic outcome of the posterior scar brachioplasty technique.
Results:
All patients who underwent the posterior scar technique were free of postoperative contour deformities. Postoperatively, the scar was completely invisible when viewed from patient’s front and patient’s lateral but was partially visible when viewed from patient’s back. And 88.8% of patients tolerated the scar with high satisfaction.
Conclusions:
The current posterior scar maneuver with fascial suspension prevented the tension on the suture line and consequently prevented the widening of the scar and facilitated the modeling procedure by removing the appropriate amount of skin and subcutaneous tissues. It creates a low-lying, posterior, well-hidden scar when viewed from the patient’s front or patient’s lateral. The scar is partially (upper third) visible when viewed from patient’s back. The technique is avoiding injury to the sensory and motor nerves of the arm and decreases the insult to the lymphatic.
A variety of useful methods for arm rejuvenation are now available. Unfortunately, none of these methods has provided full satisfaction. Among these methods are dermolipectomy of the arm with the scar oriented longitudinally and placed in the brachial sulcus,1 W-plasties,2 quadrangular flaps and T closure,3 the deepithelialized rolled-up flap,4 fascial system suspensions,5 and lipoaspiration.6
The focus of the modifications has been mainly to improve the poor aesthetic result of scar sequelae, such as retractility, healing, and widening of the scar.
The loss of support structures to the inferior curve of the arm results in the development of brachial ptosis and subsequently the appearance of the brachial sulcus. In addition, patients who have undergone massive weight loss are likely to develop marked ptosis.
Combination procedures including skin resection and liposuction7 and laser- or radiofrequency-based energy sources are performed to facilitate skin contraction and to improve scar quality.
The demand of the brachioplasty has increased because of the increasing number of individuals who have experienced massive weight loss. Therefore, there is a constant search for new techniques to improve aesthetic outcome. In massive weight loss patients, limited scar brachioplasty does not correct the arm deformity. Thus, the plastic surgeon has to choose between a medially or posteriorly located scar on the upper arm.
In the current report, the author’s aim is to demonstrate, with a 13 years’ experience, the reasons for the choice of the posteriorly located scar.
PATIENTS AND METHODS
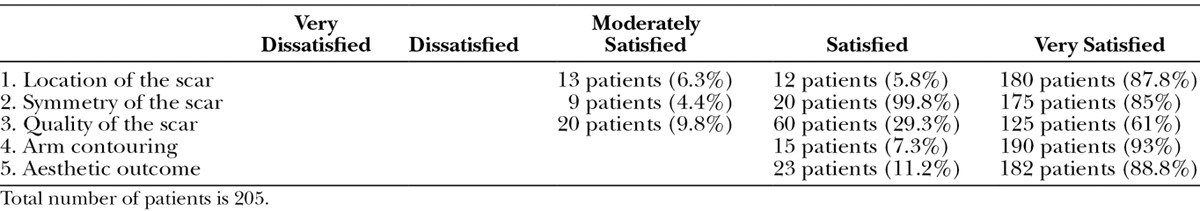
The retrospective study was conducted between February 1999 and March 2012. It included 205 patients. Ages ranged from 21 to 66 years. Informed consent was provided and the postoperative monitoring continued for 29–98 months. A Likert scale and an evaluation questionnaire were used to assess the aesthetic outcome of the posterior scar brachioplasty technique. Patients were rated on a 5-point Likert scale with 1 (very dissatisfied), 2 (dissatisfied), 3 (moderately satisfied), 4 (satisfied), and 5 (very satisfied). A Likert scale is a psychometric scale commonly involved in research that employs questionnaires. It is the most widely used approach to scaling responses in survey research.
Furthermore, we used the pre- and postoperative photographs for evaluation that was judged by the senior author and the patient.
The amount of skin excised was marked with the arm at 90° to the body and patient is standing (Figs. 1A, B). The posterior landmark is marked midway between the olecranon and the medial epicondyle and extended to the axilla. The anterior landmark is placed 1 finger breadth below the brachial sulcus and meets the posterior landmark on both ends.
Fig. 1.
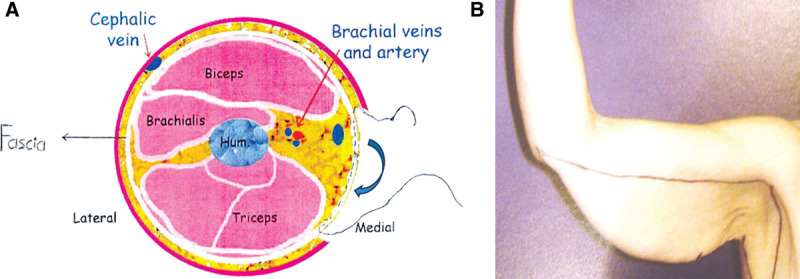
A, A cross section of the midarm to demonstrate how the tackling suture of the upper flap to the deep fascia in the lower part of the defect is performed, to bring the upper skin flap to the desired low lying and posterior position. B, The amount of skin excised was marked with the arm at 90° to the body and patient is standing. The posterior landmark is marked midway between the olecranon and the medial epicondyle and extended to the axilla. The anterior landmark is placed 1 finger breadth below the brachial sulcus and meets the posterior landmark on both ends.
Surgical Technique
The technique was performed as previously described by the author.8 All patients underwent general endotracheal intubation, and all procedures were started with infusion of 0.1% lidocaine in an epinephrine/saline 1:100,000 concentration to create a tumescence of 2:1. The liposuction was started by means of small, multiple stab wounds (0.5-cm long). We used the vacuum pump method (Wells Johnson, Tucson, Ariz.) with 4- and 6-mm (15- to 25-cm) cannulas. Suction was limited deep to the superficial fascia and addressed the entire circumference of the arm. The procedure ended with superficial liposuction to eliminate irregularities and to enhance skin contraction (Fig. 2).
Fig. 2.

Intraoperative view. The posterior technique started with liposuction that is limited deep to the superficial fascia.
An incision was placed in the brachial sulcus (on the long axis of the arm) and extended from the axilla to the middle of the arm and located on the brachial sulcus. The incision was deepened to the honeycomb plane that was created by the liposuction cannula and then dissection proceeded inferiorly to the desired extent. Undermining should be limited to the cutaneous flap that needs to be excised. The skin and subcutaneous tissue of the upper margin of the resultant defect was pulled downward to the inferior landmark of the dissected lower flap and tacked to the deep fascia with 2-0 nylon suspension sutures (Fig. 3). This created a low-lying posterior scar, which decreased tension on the suture line and prevented widening of the scar. The elevated flap was then excised (Fig. 4). Multiple-layered closure was performed with absorbable sutures (Fig. 5). The procedure was ended by liposuction of the lower medial, anterior, and posterior aspects of the arm with a 4-mm cannula to avoid dog-ear and to avoid lengthening of the incision. Patients presented with severe ptosis and had no adipose tissue deposit or relatively little fat; the incision may extend from the axilla to the posterior elbow. We use the compression garments for 3 weeks postoperatively.
Fig. 3.
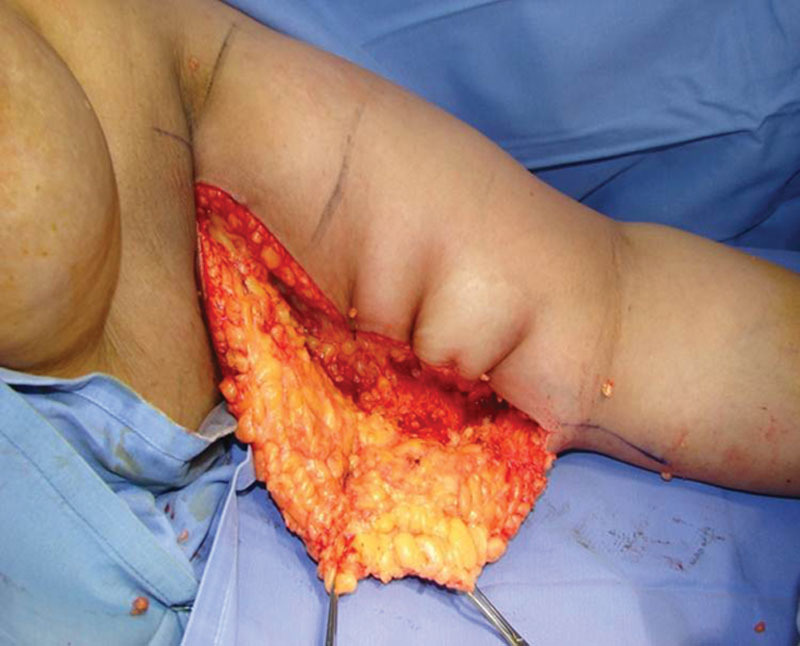
Intraoperative view. The incision deepened to the honeycomb appearance of fat. The skin and subcutaneous tissue flap are pulled posteriorly to the desired location of the scar and secured with permanent sutures.
Fig. 4.

This maneuver (fascial suspension) facilitates the excision of the proper amount of tissue.
Fig. 5.

Intraoperative view. Note the incision is placed posteriorly.
RESULTS
The widening of the scar caused by the tension supported by the sutures no longer existed because of the use of the current technique. The scar was invisible from patient’s front and patient’s lateral, but only its upper third was visible from patient’s back.
Postoperative skin laxity and ptosis in the axillary regions were encountered in 6 patients who sustained the more extreme deformities and needed secondary revisions. Five patients experienced hypertrophied scar and were treated with topical therapy (silicone gel sheets). Three patients developed postoperative distal edema. Compressive dressing that was applied to the entire upper limb and arm elevation resolved this edema. One patient experienced dysesthesia due to skin tightness and resolved spontaneously. Women were able to wear bathing suits and short-sleeved clothing (Figs. 6–9).
Fig. 6.
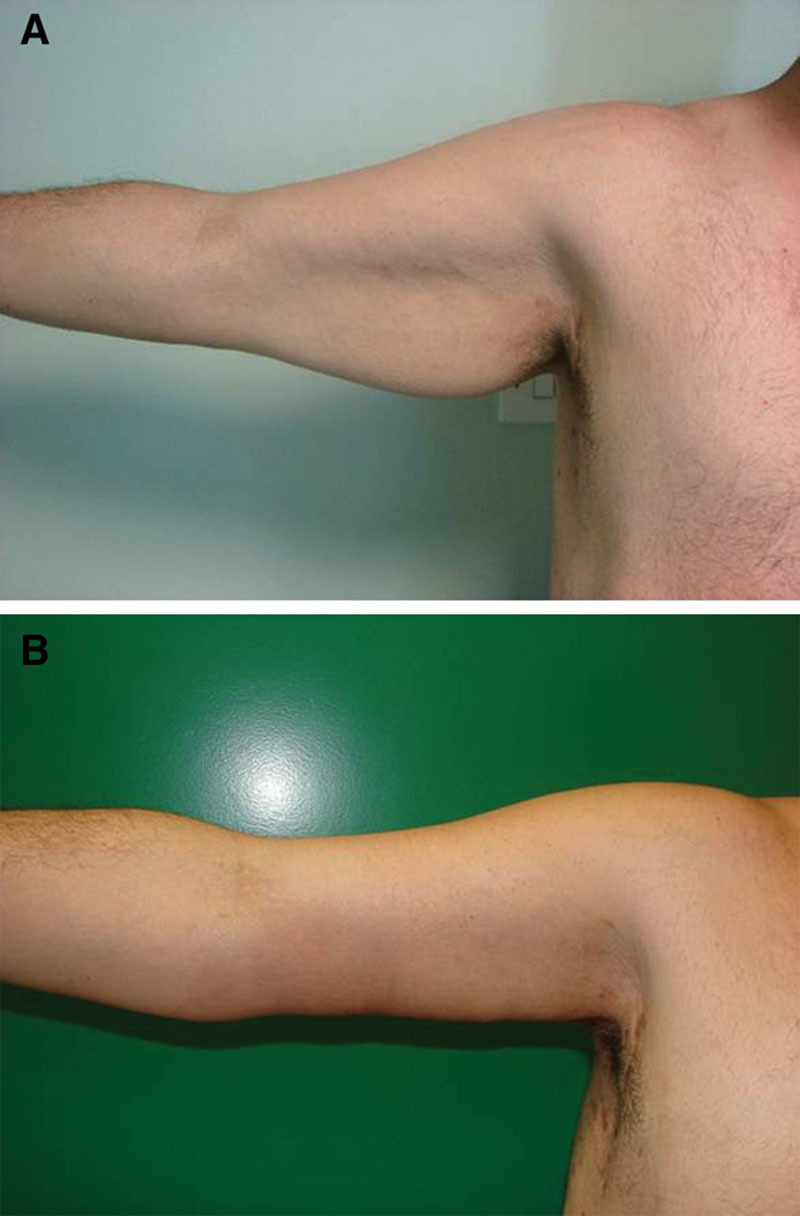
A and B, Preoperative and postoperative views of a 37-year-old male patient at 30 months follow-up.
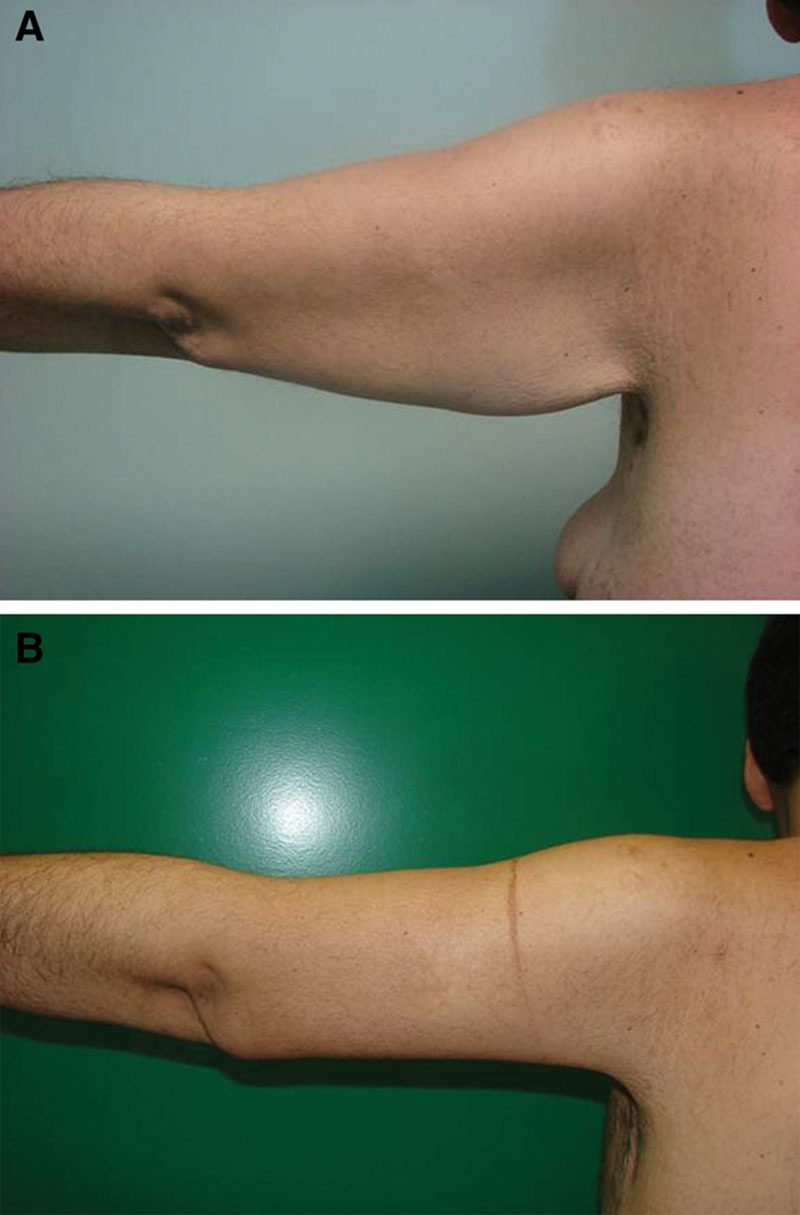
Fig. 9.

A and B, Preoperative and postoperative views of a 34-year-old female patient at 38 months after surgery.
Fig. 7.
A and B, Preoperative and postoperative views of a 37-year-old male patient at 30 months follow-up.
Fig. 8.

A and B, Preoperative and postoperative views of a 34-year-old female patient at 38 months after surgery.
The posterior scar is comparatively the least visible: not only anterior and posterior in abduction but also posterior in adduction. The aesthetic outcomes were highly satisfactory in 88.8% of patients, as judged by both the author and the patients based on the Likert scale and the evaluation questionnaire provided during the follow-up period. The evaluation of the preoperative photographs compared with the postoperative photographs illustrated the degree of lifting (judged by an independent surgeon). Table 1 demonstrates the analysis of the Likert scale data.
Table 1.
Analysis of the Data of the Likert Scale
DISCUSSION
Brachial lipodystrophy and ptosis are increasingly evident with age and especially after massive weight loss following bariatric surgery. Despite the reports of various surgical techniques to treat brachial ptosis, the problems of scars have remained. The combination of liposuction and arm dermolipectomy decreased the length of the scar where it ends midway between the axilla and the posterior elbow. The author placed the incision in the brachial sulcus and extended it midway between the axilla and the posterior elbow to address the excess skin in both longitudinal and transverse directions. The skin and subcutaneous tissue of the upper margin of the resultant defect were pulled to the inferior landmark of the dissected flap and tacked to the deep fascia with suspension, nonabsorbable sutures to create a low-lying posterior scar. This maneuver prevented tension on the suture line.
Brachioplasty was first introduced in 1954 by Correa-Iturraspe and Fernandez.9 Since then, the procedure has undergone a series of modifications to improve the appearance of the scar and the resulting contour of the arm. Teimourian and Malekzadeh10 described 4 categories of upper arm problems and offered guidelines to provide simple procedures and recommended a purse-string closure of the modest brachioplasty incision to decrease the scar size. Glanz and Gonzalez-Ulloa11 demonstrated the progression with age of the inferior curve of the upper arm and the loss of support structures that resulted in the obvious ptosis or “bat wing” appearance. Strauch et al12 presented a technique of sinusoidal excision in the posterior medial arm that provided good extremity contour with posterior scars while simultaneously addressing axillary contour deformities with a generous Z-plasty. This scar may extend from the olecranon process to the chest wall. Abramson13 treated 8 patients after massive weight loss with short scar brachioplasty or minibrachioplasty. This technique reduced the skin envelope and minimized the visible scar. The S-shaped brachioplasty14 and the Kris Knife brachioplasty are reported recently.15
Aly et al16 has created a double-ellipse marking technique to avoid overresecting and leave adequate skin for closure. After resecting, they prevent the interference of soft-tissue swelling during wound closure by immediately closing each segment with temporary staples. The technique is ideal for patients with massive weight loss.
The remaining problems of the previous techniques reported in the literature continue to include widening of the scar, hypertrophied scars, visible scars, postoperative residual contour deformities, residual skin ptosis, and patient dissatisfaction with the length and location of the scar. To avoid these unsolved problems, and to explore the strengths of the posterior scar brachioplasty with fascial suspension, we proposed the following operative guidelines:
In patients who have body mass index less than 30 and did not experienced massive weight loss, a combination of liposuction and arm dermolipectomy will decrease the length of the scar where it ends midway between the axilla and the olecranon process.
In elderly and slim patients, liposuction is usually not performed. In patients with mild and moderate fat deposit, liposuction is performed. In patients who experienced massive weight loss, a conservative liposuction is performed. Liposuction serves to remove a small amount of fat and creates a honeycomb tissue plane that is used for dissection to preserve lymphatics.
To avoid the presence of the scar along the medial border of the arm, the skin and subcutaneous tissue of the upper margin of the resultant defect were pulled to the inferior landmark of the dissected flap and tacked to the deep fascia with suspension, nonabsorbable sutures to create a low-lying posterior, well-hidden scar when viewed from the patient’s front or patient’s lateral.
The incision is placed in the brachial sulcus. The lower flap is undermined, whereas the upper flap is pulled downward. The superficial fascial system of the upper flap is suspended to the muscle fascia as low as possible with nonabsorbable sutures; hence, the tension on the suture line is prevented and consequently prevented the widening of the scar and facilitated the modeling procedure by removing the appropriate amount of skin and subcutaneous tissues.
Placement of the incision straight and along the long axis of the arm decreased the insult to the lymphatic and venous drainage and prevented postoperative distal edema.
The procedure is ended with liposuction of the lower arm for eliminating the resultant dog-ear and preventing the extension of the incision to the olecranon process.
Posterior scar brachioplasty with fascial suspension, as described by our technique, is the treatment of choice for the extreme arm deformity, especially after massive weight loss.
The only limitation of the posterior scar technique includes the visibility of the most proximal part of the scar when viewed from patient’s back. However, wound closure in the posterior brachioplasty often requires the help of an assistant.
CONCLUSIONS
The posterior scar is comparatively the least visible: not only anterior and posterior in abduction but also posterior in adduction. The aesthetic outcomes were highly satisfactory in 88.8% of patients, as judged by both the author and the patients based on the Likert scale and the evaluation questionnaire provided during the follow-up period. A part of the posterior scar is partially visible when viewed from the patient’s back, and better contouring of the arm can be achieved.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by Hamad Medical Corporation.
REFERENCES
- 1.Baroudi R. Dermolipectomy of the upper arm. Clin Plast Surg. 1975;2:485–489. [Google Scholar]
- 2.Borges AF. W-plastic dermolipectomy to correct “bat-wing” deformity. Ann Plast Surg. 1982;9:498–501. [PubMed] [Google Scholar]
- 3.Juri J, Juri C, Elías JC. Arm dermolipectomy with a quadrangular flap and “T” closure. Plast Reconstr Surg. 1979;64:521–525. doi: 10.1097/00006534-197910000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Goddio AS. A new technique for brachioplasty. Plast Reconstr Surg. 1989;84:85–91. doi: 10.1097/00006534-198907000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Lockwood T. Brachioplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96:912–920. doi: 10.1097/00006534-199509001-00022. [DOI] [PubMed] [Google Scholar]
- 6.Lillis PJ. Liposuction of the arms. Dermatol Clin. 1999;17:783–797. doi: 10.1016/s0733-8635(05)70127-3. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen AT, Rohrich RJ. Liposuction-assisted posterior brachioplasty: technical refinements in upper arm contouring. Plast Reconstr Surg. 2010;126:1365–1369. doi: 10.1097/PRS.0b013e3181ebe23c. [DOI] [PubMed] [Google Scholar]
- 8.Elkhatib HA. Classification of brachial ptosis: strategy for treatment. Plast Reconstr Surg. 2007;119:1337–1342. doi: 10.1097/01.prs.0000254796.40226.92. [DOI] [PubMed] [Google Scholar]
- 9.Correa-Iturraspe M, Fernandez JC. Dermolipectomia braquial. Prensa Med Argent. 1954;41:2432–2435. [PubMed] [Google Scholar]
- 10.Teimourian B, Malekzadeh S. Rejuvenation of the upper arm. Plast Reconstr Surg. 1998;102:545–551. doi: 10.1097/00006534-199808000-00041. discussion 552–553. [DOI] [PubMed] [Google Scholar]
- 11.Glanz S, Gonzalez-Ulloa M. Aesthetic surgery of the arm. Part I. Aesthetic Plast Surg. 1981;5:1–17. doi: 10.1007/BF01981677. [DOI] [PubMed] [Google Scholar]
- 12.Strauch B, Greenspun D, Levine J, et al. A technique of brachioplasty. Plast Reconstr Surg. 2004;113:1044–1048. doi: 10.1097/01.prs.0000105648.54174.11. discussion 1049. [DOI] [PubMed] [Google Scholar]
- 13.Abramson DL. Minibrachioplasty: minimizing scars while maximizing results. Plast Reconstr Surg. 2004;114:1631–1634; discussion 1635–1637. doi: 10.1097/01.prs.0000139296.80079.1a. [DOI] [PubMed] [Google Scholar]
- 14.Aboul Wafa AM. S-shaped brachioplasty: an effective technique to correct excess skin and fat of the upper arm. Plast Reconstr Surg. 2013;131:661e–663e. doi: 10.1097/PRS.0b013e318282793e. [DOI] [PubMed] [Google Scholar]
- 15.Bracaglia R, D’Ettorre M, Gentileschi S, et al. “Kris knife” brachioplasty after bariatric surgery and massive weight loss. Aesthetic Plast Surg. 2013;37:640–642. doi: 10.1007/s00266-013-0101-9. [DOI] [PubMed] [Google Scholar]
- 16.Aly A, Pace D, Cram A. Brachioplasty in the patient with massive weight loss. Aesthet Surg J. 2006;26:76–84. doi: 10.1016/j.asj.2005.11.004. [DOI] [PubMed] [Google Scholar]


