Abstract
Background:
The prevalence of pterygium colli (“webbed neck”) is 75% in patients with Turner syndrome. This congenital deformity manifests as a bilateral cervical skin fold stretching from the mastoid to the acromion. Although the visibility of this skin fold varies among patients, it frequently has negative social effects. The surgical management of this malformation remains challenging as it requires the achievement of a harmonious neck profile and natural hairline implantation.
Methods:
We describe a series of 5 girls with Turner syndrome who were managed in our department at the University Hospital Center of Toulouse-Rangueil, France. All patients benefited from a surgical approach based on a new posterior technique, including half-moon resection of the skin fold with an inferior back-cut and suturing of the superficial lamina of the cervical fascia. To ensure solidity, the fascia was fastened to the nuchal ligament.
Results:
Patients’ mean age at surgery was 10 years (range, 6–13 y). The mean duration of follow-up was 13.7 years (range, 2–20 y). No scar enlargement or recurrence was remotely authenticated. The patients were satisfied with the cosmetic results, including an esthetic neck profile and recovery of hairline implantation.
Conclusion:
The “posterior cervical lift,” an innovative surgical technique for the management of pterygium colli, achieved satisfying cosmetic outcomes and stability over time.
Pterygium colli (webbed neck) is a congenital deformity of unknown origin that was first described in 1883 by Kobylinski.1 The prominence of the skin fold is variable, but it usually extends from the acromion to the mastoid. Its anterior surface is always hairless, but its posterior surface often has a low hairline that can extend to the nape of the neck. The exact etiopathogeny of pterygium colli remains unexplained although some authors have attributed the condition to in utero lymphatic malformations.2,3 This condition is associated with many malformative syndromes, most commonly Turner syndrome, which was described in 1938 and is characterized by a 45X0 karyotype abnormality.4,5
Pterygium colli is also associated with Noonan syndrome, first mentioned in 1963 and characterized by a Turner phenotype despite a normal karyotype.6 Klippel–Feil syndrome causes a short neck and, in some cases, a manifestation similar to pterygium colli.7 However, the incidence of this syndrome is very low and the relevant literature is quite poor.
Patients with pterygium colli typically request cosmetic treatment as the condition often has major negative social effects. The surgical management of this malformation is challenging as it requires the achievement of a harmonious neck profile and highly satisfactory recovery of hairline implantation. Choosing among existing surgical approaches is difficult because they provide variable outcomes, depending on the prominence of the pterygium colli. We generally oppose lateral techniques and posterior techniques.1,7 Here, we describe the use of the “posterior cervical lift,” a new posterior surgical technique, in 5 girls with Turner syndrome.
MATERIALS AND METHODS
This study included 5 girls with Turner syndrome and pterygium colli who were managed in the Plastic and Reconstructive Surgery Department of the University Hospital Center of Toulouse-Rangueil, France. All patients benefited from a surgical approach based on a new posterior technique called the “posterior cervical lift,” which includes half-moon resection of the skin fold with, if necessary, an inferior back-cut and suturing of the superficial lamina of the cervical fascia. All patients underwent consultation and clinical examination and photographs were taken (Figs. 1–4).
Fig. 1.
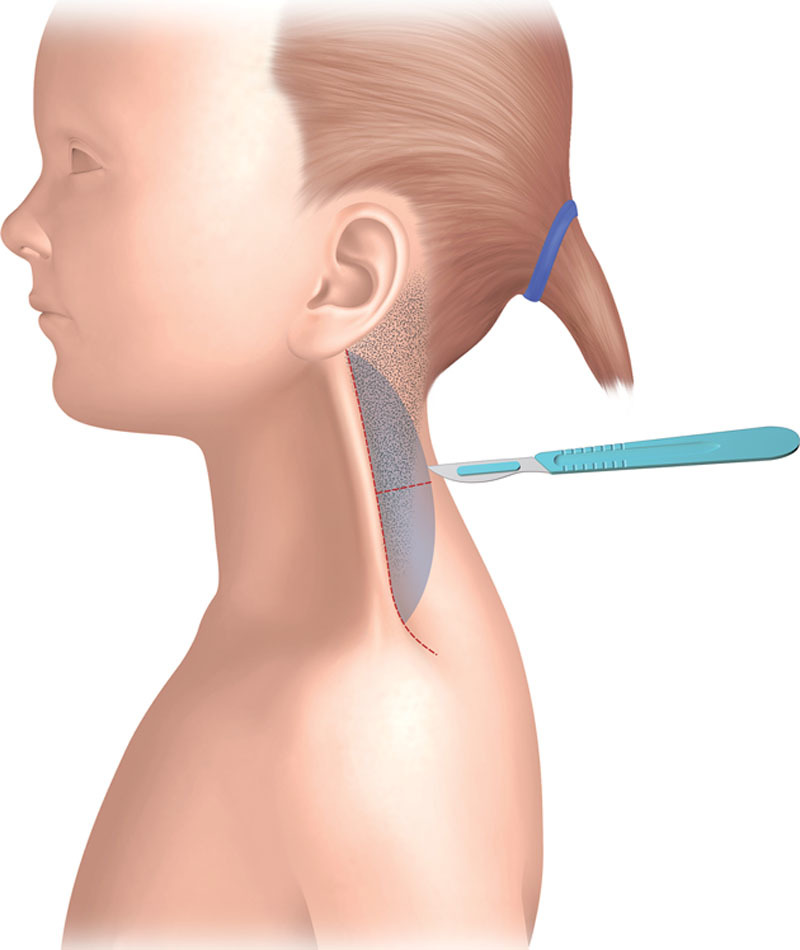
Preoperative pattern: lateral view.
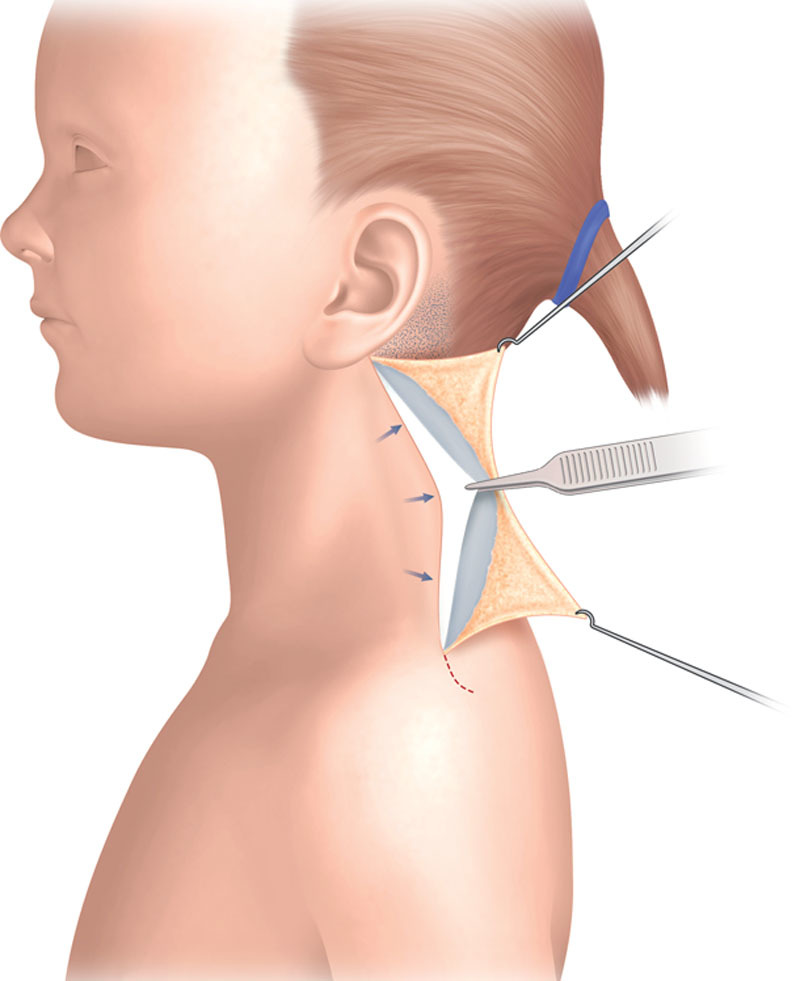
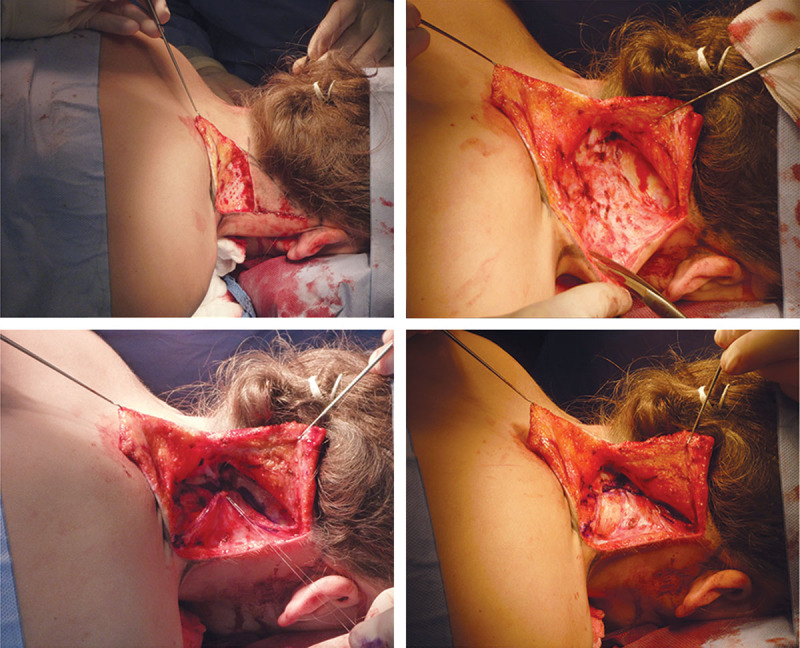
Fig. 4.
Lifting of the webbed neck skin. The inferior back-cut is incised if necessary.
Fig. 2.
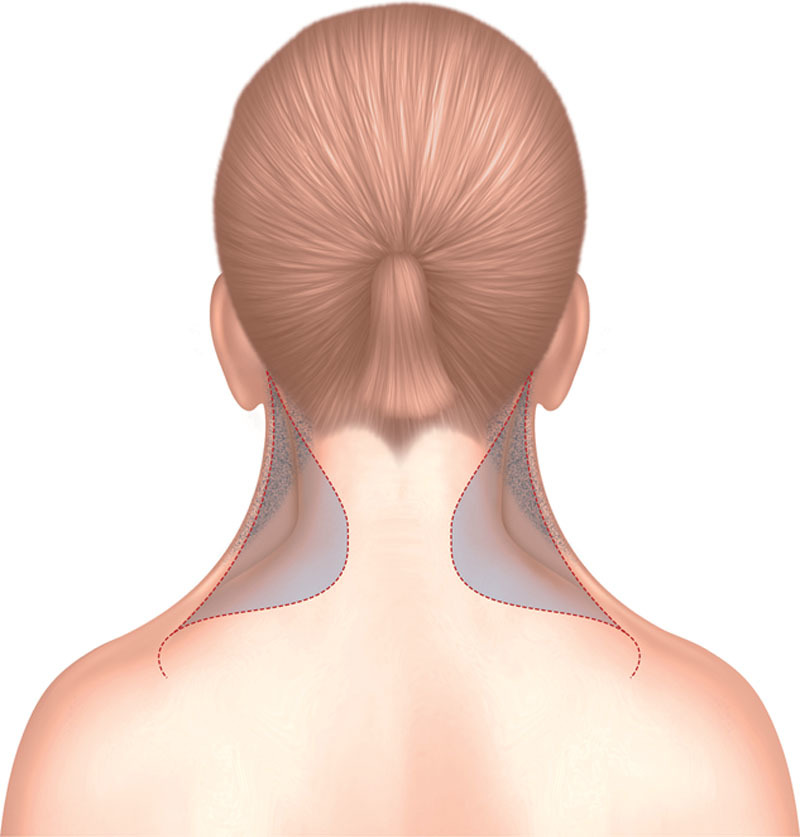
Preoperative pattern: posterior view.
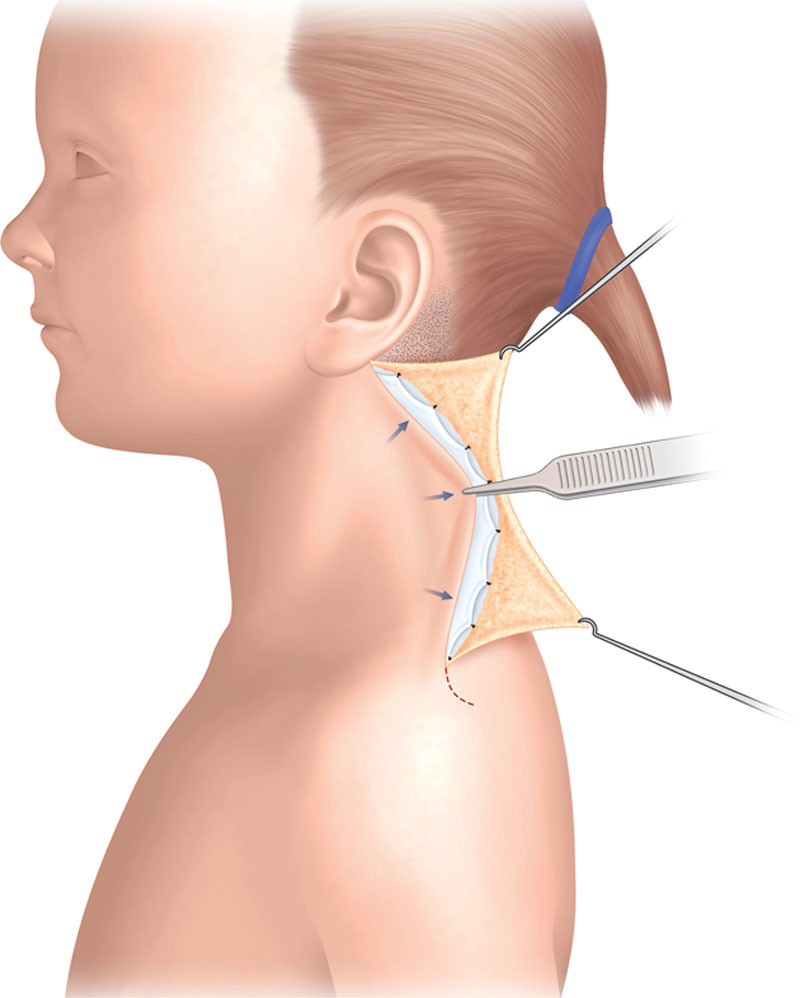
Fig. 3.
Retention of the superficial lamina of the cervical fascia, which is fixed near the nuchal ligament or its interconnection fibers with the trapezius muscle.
The Surgical Technique
Preoperative drawings were made while the patient was in the prone position with the head fixed on a silicon support (Fig. 5). The cervical folds were precisely located by palpation, and a reversed convex half-moon was drawn with the base in direct contact with the posterior implantation of the fold. On the inferior part of the half-moon, a back-cut line was drawn and incised if needed. The purpose of this step was to gain laxity, allowing elevation of the hairline implantation. After the infiltration of lidocaine with 1% epinephrine, surgical exeresis of the cutaneous half-moon was performed. The superior part of this exeresis removed the abnormal hairline implantation and enabled elevation (Fig. 6). The anterior part of the exeresis removed the posterior fibers of the platysma. The superficial lamina of the cervical fascia was then completely exposed. Toothed forceps were used to simulate posterior skin retention of the cervical fascia, allowing complete and sustainable reduction of the cervical fold. The suture locations were marked in blue, and retention was then performed with 2/0 braided absorbable sutures. The sutures were fixed near the nuchal ligament or its interconnection fibers, the closest area of fixity. Finally, skin closure was performed on 2 levels with subcutaneous 3/0 absorbable monofilament sutures (Fig. 7).
Fig. 5.

Shaving of abnormal hair implantation before infiltration of lidocaine with 1% epinephrine.
Fig. 6.
Surgical technique with retention of the superficial lamina of the cervical fascia. Note that fascia fixation allows fold reduction (intraoperative view).
Fig. 7.

Immediate postoperative results.
Care must be taken to avoid excessive retention, which can lead to cervical constriction that can be severe in children presenting with postoperative edema or hematoma.
RESULTS
Five girls with pterygium colli were managed in our department between 1991 and 2011. The mean age at surgery was 10 years (range, 6–13 y). The mean duration of follow-up was 13.7 years (range, 2–20 y). These patients had no mental retardation. Their malformations were caused by Turner syndrome and represented major cosmetic burdens. We observed no asymmetry of the webbed neck in any patient. Besides, no author has ever reported a potential asymmetry. No surgical complication occurred. Suction drainage was used in 4 patients.
In 1 patient, we simultaneously performed bilateral otoplasty to correct the prominence of the ears.
Locally, we found no fibrous tissue band, which some authors have described as the thickening of the superficial lamina of the cervical fascia or platysma.4,8 Histological analysis of the folds confirmed their normal or nonspecific fibrocollagenic nature (Figs. 8–17).
Fig. 8.

A 13-year-old girl with pterygium colli associated with Turner syndrome.
Fig. 17.

Good results at 1 y postoperatively, but the scar remains inflammatory. The patient was very satisfied with the cosmetic outcome.
Fig. 9.

Results at 16 years old, showing good restitution of the neck profile (anterior view).
Fig. 10.

Scarring is discreet, but hair implantation has not been completely corrected. Nevertheless, the patient was very satisfied (posterior view).
Fig. 11.

A 6-year-old girl with pterygium colli associated with Turner syndrome.
Fig. 12.

Good results at 15 mo postoperatively, with an adequate neck profile and very satisfactory correction of abnormal hair implantation (anterior and posterior views).
Fig. 13.

A 7-year-old girl with pterygium colli associated with Turner syndrome.
Fig. 14.

Abnormal hair implantation has been completely corrected, with a few hairs growing on the scar (posterior view).
Fig. 15.

Good neck profile at 17 years old (anterior view).
Fig. 16.

A 12-year-old girl with severe pterygium colli associated with Turner syndrome.
DISCUSSION
Nosology
Pterygium colli is mainly observed in association with 3 major malformative syndromes: the Turner, Klippel–Feil, and Noonan syndromes.
Turner syndrome is a 45X0 karyotype abnormality; the classic triad of manifestations was first described in 1938 as pterygium colli, cubitus valgus, and infantilism syndrome.
Klippel–Feil syndrome, described in 1912, consists of a cervical vertebral deformity resulting in a short neck, combined with a cleft lip.
Noonan syndrome mimics Turner syndrome but occurs in boys with normal karyotypes.
Pterygium colli can also be associated with Freeman–Sheldon syndrome (craniocarpotarsal dysplasia), fetal alcohol syndrome, and trisomies 18 and 21.7
The etiopathogenesis of this condition remains unknown, but it could result from in utero cervical lymphatic developmental defects2 or in utero cystic hygroma of the posterior surface of the neck, which would create 2 excess lateral skin folds during resorption.9 In 1984, Clark3 reported that pterygium colli was associated with heart malformation in patients with Turner syndrome. He argued that increased lymphatic pressure and jugular lymphatic sac obstruction resulting in pterygium colli would distend the thoracic duct, compressing the ascending aorta. Blood flow would thus be altered, favoring aortic coarctation and repercussion in the left heart.
Heredity must be taken into account, as Leandris and Ricbourg7 described 3 cases of pterygium colli in the same family (a mother and 2 sons), although they did not specify the associated syndrome. Graham and Smith10 also described the entity of “dominantly inherited pterygium colli.”
Patients with Turner syndrome rarely have mental retardation and generally seek consultation due to the negative cosmetic and social effects of pterygium colli. The literature on the surgical correction of pterygium colli is poor; most authors have described the use of a given technique in 1 or 2 cases, with little follow-up data. The achievement of a harmonious cervical profile and normal hairline implantation are the 2 main objectives of management, but analysis of the results presented in the literature is complex, in part, because the prominence of the malformation can vary.10
Surgical Techniques
For plastic surgeons, the ideal technique provides the best cosmetic results with the fewest complications and recurrences and, especially in the cases described here, the least scarring.
We oppose lateral techniques for pterygium colli management7,8,11 and favor posterior techniques,7,9,10,12–17 following Thomson et al.1 Techniques involving balloon skin expansion have also been described and seem to have yielded good results in isolated cases,7,18,19 but we do not use them. Expansion could aid posterior techniques by providing vertical laxity, which is especially lacking in pterygium colli. Expansion has been found to provide superior skin lifting while minimizing the risk of recurrence. However, it requires several sessions, which pediatric patients may find difficult to tolerate.
Lateral techniques are mainly Z-plasties or modified Z-plasties, which provide good fold reduction but less efficient hairline implantation, with a risk of unattractive anterior hair transposition. These techniques also cause significant scarring, which is readily visible on the lateral surfaces of the neck.
Posterior techniques also provide good fold reduction, but the sutures are often tightened, which could favor recurrence or scar enlargement and hypertrophic scarring.20 Nevertheless, they enable the complete resection of abnormal hairline implantation and the scars can be hidden in the hair.
We prefer posterior techniques because they can provide a harmonious cervical profile. The “posterior cervical lift” is thus named because it involves posterior retention of the superficial lamina of the cervical fascia, such as in cervicofacial rhytidectomy with superficial musculoaponeurotic system suspension. Solid, reliable fixation of the paranuchal connective fibers of the trapezius is possible. All published descriptions of pterygium colli management have focused on how to lift or resect the skin. We suggest a different approach using the superficial lamina of the cervical fascia, with deep suturing that reduces the tightness of the skin sutures.
Another important implication of the surgical management of this condition is the danger to the spinal nerve posed by complete and deep resection of the fold, with removal of fibers from the sternocleidomastoid muscle. Our technique consistently remains above the superficial lamina of the cervical fascia, and so poses no danger to the spinal nerve.
To facilitate the surgical procedure, we systematically operated on young patients (mean age, 10 y) who had laxer and more plastic skin. This surgery should be performed in preschool-aged patients to limit questions from other children; however, patients usually request cosmetic correction in early adolescence if their parents had not requested it earlier.
Recurrence is possible, but we found only 1 case described by Posso et al.9 A 6-year-old girl initially benefited from surgery using a “butterfly” technique, but the result was unsatisfying at 2 years postoperatively, requiring revision surgery with a Z-plasty.
CONCLUSION
The management of pterygium colli remains a surgical challenge. Through this clinical series, we have described the “posterior cervical lift,” an innovative surgical technique for the management of pterygium colli. It provided satisfactory cosmetic results and stability over time. Patients assessed the outcomes as excellent. We favor posterior techniques, which we believe provide the best compromise between fold reduction and risk of recurrence.
Footnotes
Presented at French Plastic Surgery Meeting, November 2011, Paris, France.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Thomson SJ, Tanner NS, Mercer DM. Web neck deformity; anatomical considerations and options in surgical management. Br J Plast Surg. 1990;43:94–100. doi: 10.1016/0007-1226(90)90051-z. [DOI] [PubMed] [Google Scholar]
- 2.Mulliken JB. Vascular malformations of the head and neck. In: Young AE, editor. Vascular Birthmarks. Philadelphia: WB Saunders; 1988. p. 309. [Google Scholar]
- 3.Clark EB. Neck web and congenital heart defects: a pathogenic association in 45 X-O Turner syndrome? Teratology. 1984;29:355–361. doi: 10.1002/tera.1420290305. [DOI] [PubMed] [Google Scholar]
- 4.Monney C, Pescia G, Addor MC. [Turner syndrome]. Schweiz Med Wochenschr. 2000;130:1339–1343. [PubMed] [Google Scholar]
- 5.Jones HW, Turner HH, Ferguson-Smith MA. Turner’s syndrome and phenotype. Lancet. 1966;1:1155. doi: 10.1016/s0140-6736(66)91169-x. [DOI] [PubMed] [Google Scholar]
- 6.Qian JG, Wang XJ. Noonan syndrome and correction of the webbed neck. J Plast Reconstr Aesthet Surg. 2007;60:316–319. doi: 10.1016/j.bjps.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Leandris M, Ricbourg B. [Surgical treatment of pterygium colli. A case report and review of the literature]. Ann Chir Plast Esthet. 1997;42:615–622. [PubMed] [Google Scholar]
- 8.Menick FJ, Furnas DW, Achauer BM. Lateral cervical advancement flaps for the correction of webbed-neck deformity. Plast Reconstr Surg. 1984;73:223–229. doi: 10.1097/00006534-198402000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Posso CM, Wolff GA, Suarez LD. [Pterigium colli: secondary surgical correction of one severe case]. Ann Chir Plast Esthet. 2012;57:299–303. doi: 10.1016/j.anplas.2010.10.017. [DOI] [PubMed] [Google Scholar]
- 10.Graham JM, Jr, Smith DW. Dominantly inherited pterygium colli. J Pediatr. 1981;98:664–666. [PubMed] [Google Scholar]
- 11.Rossillon D, De Mey A, Lejour M. Pterygium colli: surgical treatment. Br J Plast Surg. 1989;42:178–183. doi: 10.1016/0007-1226(89)90200-2. [DOI] [PubMed] [Google Scholar]
- 12.Lindsay WK. Lateral cervical advancement flaps for the correction of webbed-neck deformity. Discussion. Plast Reconstr Surg. 1984;73:229. doi: 10.1097/00006534-198402000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Gargan TJ. Web neck deformity in Turner syndrome. Plast Reconstr Surg. 1997;99:871–874. doi: 10.1097/00006534-199703000-00042. [DOI] [PubMed] [Google Scholar]
- 14.Hikade KR, Bitar GJ, Edgerton MT, et al. Modified Z-plasty repair of webbed neck deformity seen in Turner and Klippel-Feil syndrome. Cleft Palate Craniofac J. 2002;39:261–266. doi: 10.1597/1545-1569_2002_039_0261_mzprow_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 15.Shearin JC, Jr, DeFranzo AJ. Butterfly correction of webbed-neck deformity in Turner’s syndrome. Plast Reconstr Surg. 1980;66:129–133. doi: 10.1097/00006534-198007000-00025. [DOI] [PubMed] [Google Scholar]
- 16.Agris J, Dingman RO, Varon J. Correction of webbed neck defects. Ann Plast Surg. 1983;11:299–307. doi: 10.1097/00000637-198310000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Reichenberger MA, Goertz O, Lehnhardt M, et al. Surgical correction of pterygium colli. J Pediatr Surg. 2013;48:464–469. doi: 10.1016/j.jpedsurg.2012.11.054. [DOI] [PubMed] [Google Scholar]
- 18.Miller LB, Kanter M, Wolfort F. Treatment of webbed neck in Turner’s syndrome with tissue expansion. Ann Plast Surg. 1990;24:447–450. doi: 10.1097/00000637-199005000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Niranjan NS. Webbing of the neck: correction by tissue expansion. Plast Reconstr Surg. 1989;84:985–988. doi: 10.1097/00006534-198912000-00021. [DOI] [PubMed] [Google Scholar]
- 20.Hoffmann J, Cornelius CP, Schwenzer K, et al. Possibilities for correcting the neck profile in pterygium colli. Mund Kiefer Gesichtschir. 1997;1(Suppl 1):S141–S143. [PubMed] [Google Scholar]


