Supplemental Digital Content is available in the text.
Abstract
Background:
Despite the popularity of these procedures, there are limited published prospective studies evaluating liposuction and abdominoplasty. Lipoabdominoplasty is a subject of recent attention. Several investigators have recommended alternative techniques that preserve the Scarpa fascia in an effort to reduce complications, particularly the risk of seromas.
Methods:
Over a 5-year period, 551 consecutive patients were treated with ultrasonic liposuction alone (n = 384), liposuction/abdominoplasty (n = 150), or abdominoplasty alone (n = 17). In lipoabdominoplasties, the abdomen and flanks were first treated with liposuction. A traditional flap dissection was used for all abdominoplasties. Scalpel dissection was used rather than electrodissection. A supine “jackknife” position was used in surgery to provide maximum hip flexion, allowing a secure deep fascial repair.
Results:
The complication rate after liposuction was 4.2% vs 50% for patients treated with an abdominoplasty. Approximately half of the abdominoplasty complications were minor scar deformities, including widened umbilical scars (17.3%) that were revised. The seroma rate after abdominoplasties was 5.4%; there were no seromas after liposuction alone.
Conclusions:
Lipoabdominoplasty may be performed safely, so that patients may benefit from both modalities. The seroma rate is reduced by avoiding electrodissection, making Scarpa fascia preservation a moot point. A deep fascial repair keeps the abdominoplasty scar within the bikini line. Deep venous thrombosis and other complications may be minimized with precautions that do not include anticoagulation.
Existing studies of liposuction and abdominoplasty are largely retrospective and include either liposuction or abdominoplasty patients. Today, most patients are treated with both procedures simultaneously. However, there are few prospective studies evaluating this large group of patients. Lipoabdominoplasty is a subject of recent attention, particularly with regard to minimizing the rate of seromas and deep venous thrombosis. This clinical study was undertaken to evaluate the safety of combined procedures and compare the results between combined procedures and liposuction and abdominoplasty alone. The same large, prospective database was used for prospective outcomes and measurement studies, and these results are reported separately.1–4 The term “lipoabdominoplasty” is used to describe liposuction of the abdomen and flanks combined with abdominoplasty, with overlapping treatment areas.5 This term is not used to describe simultaneous abdominoplasty and liposuction of other body areas.
PATIENTS AND METHODS
Patients
From January 2002 to November 2006, 551 consecutive patients were treated with liposuction and/or abdominoplasty. The inclusion rate was 100%. Institutional Review Board approval was obtained from the Surgery Center of Leawood.
Surgery
Body fat disproportion was the usual indication for liposuction. Abdominoplasty was recommended for treatment of abdominal skin redundancy and musculofascial laxity, usually (90%) in combination with liposuction. In lipoabdominoplasty cases, the liposuction was performed first, followed by the abdominoplasty. The patient was turned from side to side to complete the superwet infusion and then liposuction was performed using the same sequence of body positioning (Fig. 1). (See video, Supplemental Digital Content 1, which demonstrates the superwet infusion and liposuction body positioning, http://links.lww.com/PRSGO/A4.) The flanks were treated while the patient was positioned on her side, overlapping the lateral ends of the planned abdominoplasty incision, to reduce hip fullness and avoid dog ears. The prone position is not used by the author. The Lysonix 3000 (Mentor, Santa Barbara, Calif.) ultrasonic system and a superwet technique were used in all cases.4
Fig. 1.
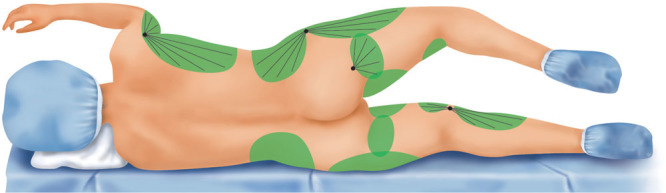
Illustration of liposuction treatment areas with the patient positioned on her left side. The patient starts supine and then is turned from the supine position (not shown) first onto the left side and then onto the right side to allow circumferential infusion of the anesthetic solution. The sequence is repeated for liposuction. Prone positioning is not used. In patients undergoing abdominoplasty, liposuction is performed first, followed by the abdominoplasty. (Illustration reprinted from Swanson E. Prospective clinical study reveals significant reduction in triglyceride level and white cell count after liposuction and abdominoplasty and no change in cholesterol levels. Plast Reconstr Surg. 2011;128:182e–197e.)
Video 1.

See video, Supplemental Digital Content 1, which demonstrates the superwet infusion and liposuction using side-to-side-to-supine body positioning. Prone positioning is not used, http://links.lww.com/PRSGO/A4.
The abdomen was infused approximately 20 minutes before the abdominoplasty with up to 1 L of normal saline containing 0.025% bupivacaine and 1:526,000 epinephrine. The epigastrium and, frequently, the pubic area were treated with judicious liposuction, using radial strokes, ultrasound times of less than 1 minute, and typical suction volumes less than 150 cm3. A single umbilical incision was used to access the upper abdomen.
The abdominoplasty incision was made using a concave incision within the bikini line, with elevation of the flap to the level of the costal margins, maintaining as much vascular supply to the flap as possible.6 Scalpel dissection was used exclusively, preserving an areolar tissue layer and some fat on the abdominal wall (Fig. 2). (See video, Supplemental Digital Content 2, which demonstrates the abdominoplasty dissection and diastasis repair, http://links.lww.com/PRSGO/A5.) Rectus abdominus fascial plication was performed using 2 layers of monofilament polypropylene sutures (0 Prolene, Ethicon, Somerville, N.J.). The operating table was flexed to facilitate closure (Fig. 3). (See video, Supplemental Digital Content 3, which demonstrates the jackknife positioning of the operating table, http://links.lww.com/PRSGO/A6.) The umbilicus was transposed and the wound closed in 3 layers using absorbable, braided polyglactin sutures (2-0 Vicryl) to anchor the Scarpa fascia of the upper flap to the lower Scarpa fascia, with additional passes through the lower muscle fascia medially to anchor the flap and prevent upward migration (See video, Supplemental Digital Content 4, which demonstrates deep fascial anchoring, http://links.lww.com/PRSGO/A7), followed by deep dermal approximation (interrupted 3-0 Vicryl) and skin closure (running intradermal 4-0 Monocryl) under minimal tension. A single drain, exiting the right pubic portion of the abdominoplasty incision, was removed after 3 or 4 days. (See video, Supplemental Digital Content 5, which demonstrates wound closure, the umbilical repair, and 24-h follow-up, http://links.lww.com/PRSGO/A8.)
Fig. 2.
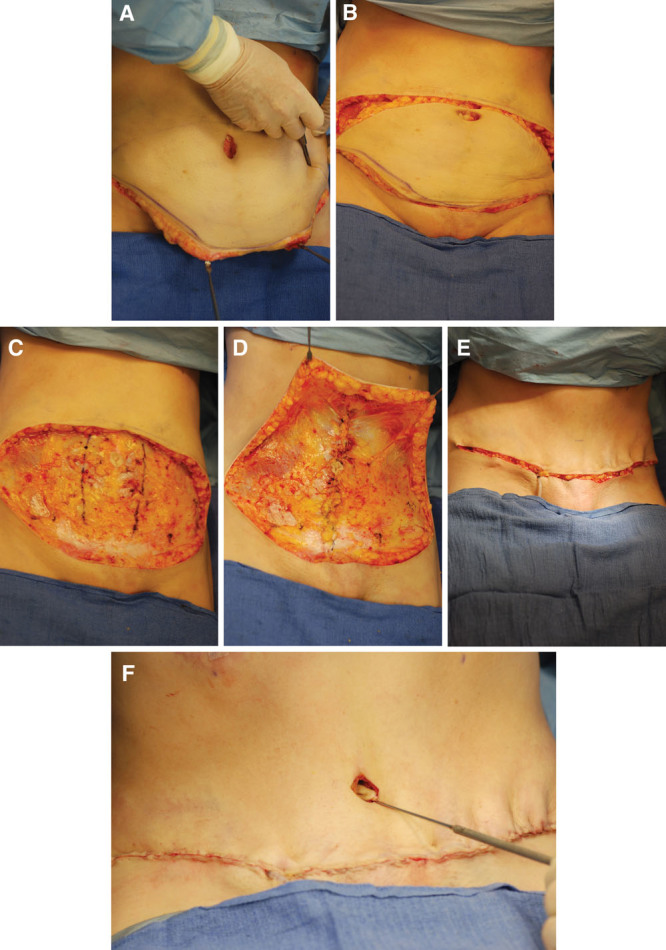
Intraoperative photographs of a 40-year-old woman undergoing abdominoplasty. Liposuction of the abdomen and flanks has already been completed. A, A curved incision is made within the bikini line. B, The superior incision has been made. The resected tissue weighed 500 g. C, The medial borders of the rectus abdominis are marked. D, The superior flap is undermined only as far as necessary to allow wound closure. The diastasis has been repaired. E, Deep fascial closure has been completed, relieving skin tension. A single drain is used, exiting along the incision line. F, The umbilicus is brought out with a slight downward inclination. This patient also underwent bilateral augmentation/mastopexy and buttock fat injection.
Fig. 3.
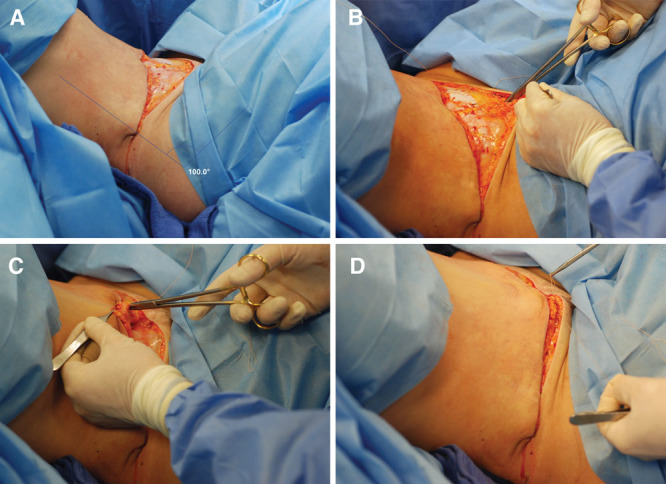
Intraoperative photographs of a 34-year-old woman undergoing abdominoplasty. A, The operating table is flexed 80 degrees. B, A 2-0 Vicryl (Ethicon) suture is anchored to the deep fascia. C, The suture is passed through the Scarpa fascia of the abdominal flap. D, The deep fascial suture provides secure fixation and limits skin tension.
Video 2.

See video, Supplemental Digital Content 2, which demonstrates the abdominoplasty dissection and diastasis repair, http://links.lww.com/PRSGO/A5.
Video 3.

See video, Supplemental Digital Content 3, which demonstrates the jackknife positioning of the operating table, http://links.lww.com/PRSGO/A6.
All surgery was performed by the author in a state-licensed ambulatory surgery center, with anesthesia administered by an anesthesiologist or certified nurse anesthetist using a total intravenous anesthetic.4 Sequential compression devices were used. No patient received enoxaparin.
Statistical Analysis
Statistical analyses were performed using IBM SPSS for Windows version 20.0 (IBM Corp., Armonk, N.Y.). Independent t tests were used to compare means of continuous variables for 2 groups of patients. Pearson’s chi-square test of independence was used to compare categorical variables. Correlations were tested using Pearson correlations. A value of P < 0.01 was considered significant. An a priori power analysis was performed for the independent t test. To achieve 80% power for a two-tailed t test, with an α level of 0.01, sufficient to detect a medium-sized treatment difference (d = 0.50), 192 patients would be needed.
RESULTS
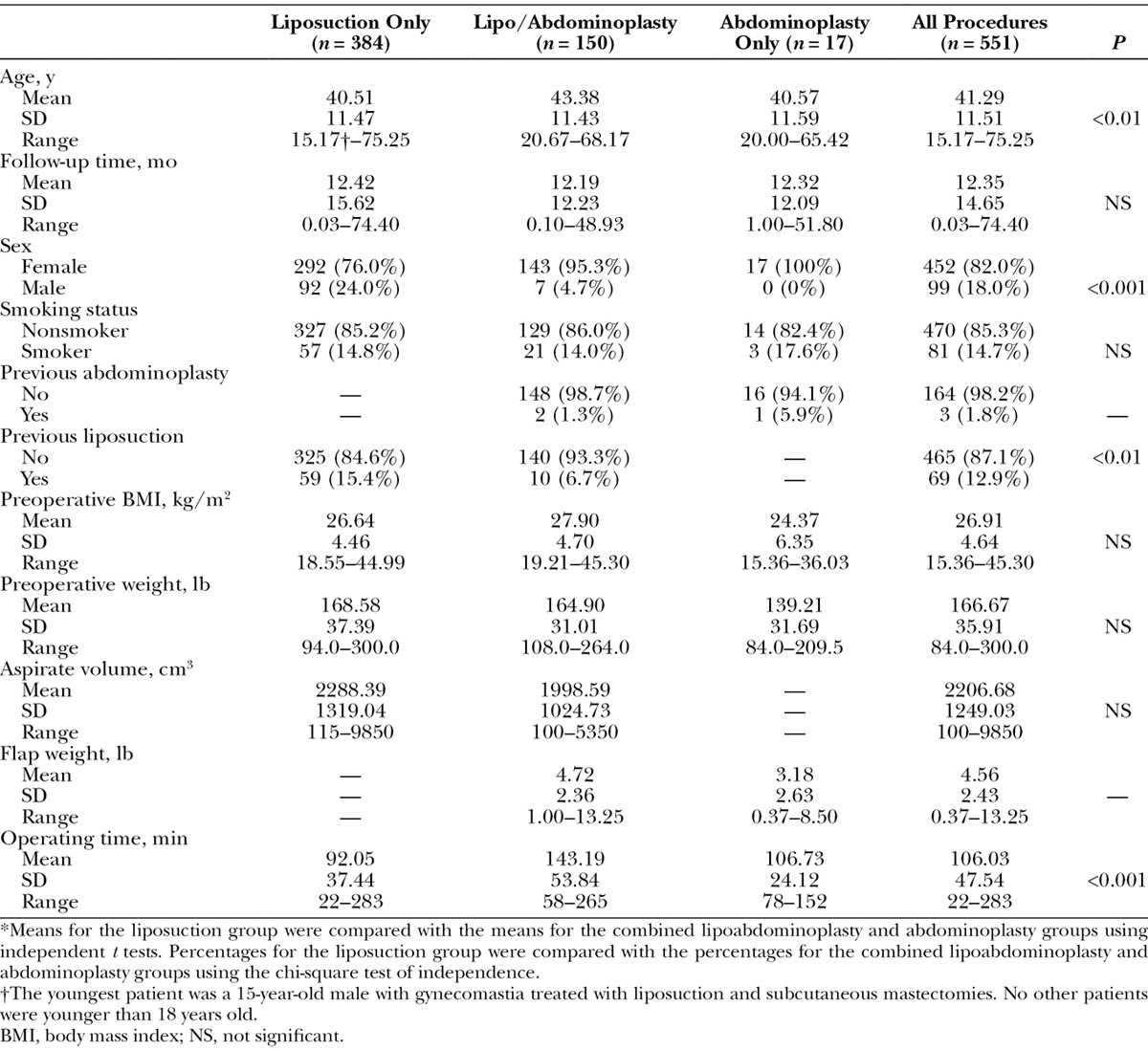
The age and follow-up times for each of the 3 groups were similar (Table 1). Most patients (61.5%) underwent simultaneous cosmetic procedures of the face or breasts.
Table 1.
Patient Data*
Complications
The overall complication rates were 4.2% for liposuction alone and approximately 50% for patients treated with an abdominoplasty (Table 2). There were no deaths. Three patients were admitted to hospital. One patient who developed a deep venous thrombosis after lipoabdominoplasty was hospitalized for anticoagulation. Another patient was hospitalized 3 weeks after surgery to treat a methicillin-resistant staphylococcal infection, likely contracted from her infected partner. This was also the only patient to receive a blood transfusion. A third patient was hospitalized overnight after surgery for suspected negative pressure pulmonary edema, possibly caused by laryngospasm.
Table 2.
Complications
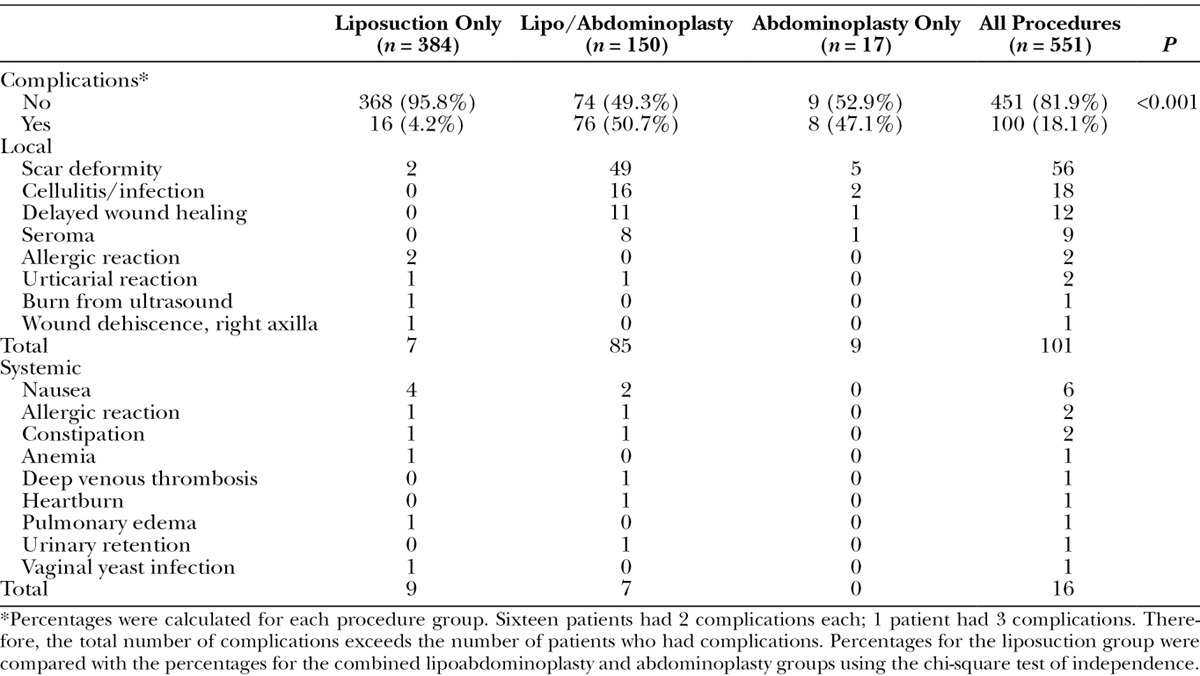
The most common complication after abdominoplasty was an umbilical scar deformity (17.4%), treated with a scar revision under local anesthesia in the office. There were 9 clinical seromas after abdominoplasties (5.4%). All of these were treated successfully by needle aspiration in the office. The mean number of aspirations was 5, with a range of 1–12. The mean time of the last aspiration was 28 days after surgery (range, 15–43 d). The mean aspirate volume was 74 cm3 (range, 3–240 cm3).
No significant correlations were detected between the overall incidence of complications and patient age, smoking history, or body mass index. Men had fewer complications than women overall, but this finding was related to the fact that fewer men underwent an abdominoplasty. There were significantly (P < 0.01) more cases of delayed wound healing in smokers (6.2%) than nonsmokers (1.5%).
DISCUSSION
Study Design
Large sample sizes increase statistical power and improve reliability.7 For over 2 decades, liposuction and abdominoplasty have been performed together.6,8 However, limited prospective data are available comparing this combination with the individual procedures. Because the patients in this study were scheduled regularly for postoperative blood tests, photographs, and surveys as part of their contemporaneous investigations,1–4 patient follow-up was optimized, improving the reliability of the data, and tracking of complications.
Complications
The absence of infection as a complication among the 384 ultrasonic liposuction cases is remarkable but not unusual.9,10 The low overall complication rate after liposuction, 4.2%, is also typical.10–12 Seromas after liposuction were notably absent, likely because ultrasound times were limited (<5 min for the abdomen in primary liposuction; <1 min for the epigastrium in lipoabdominoplasty).
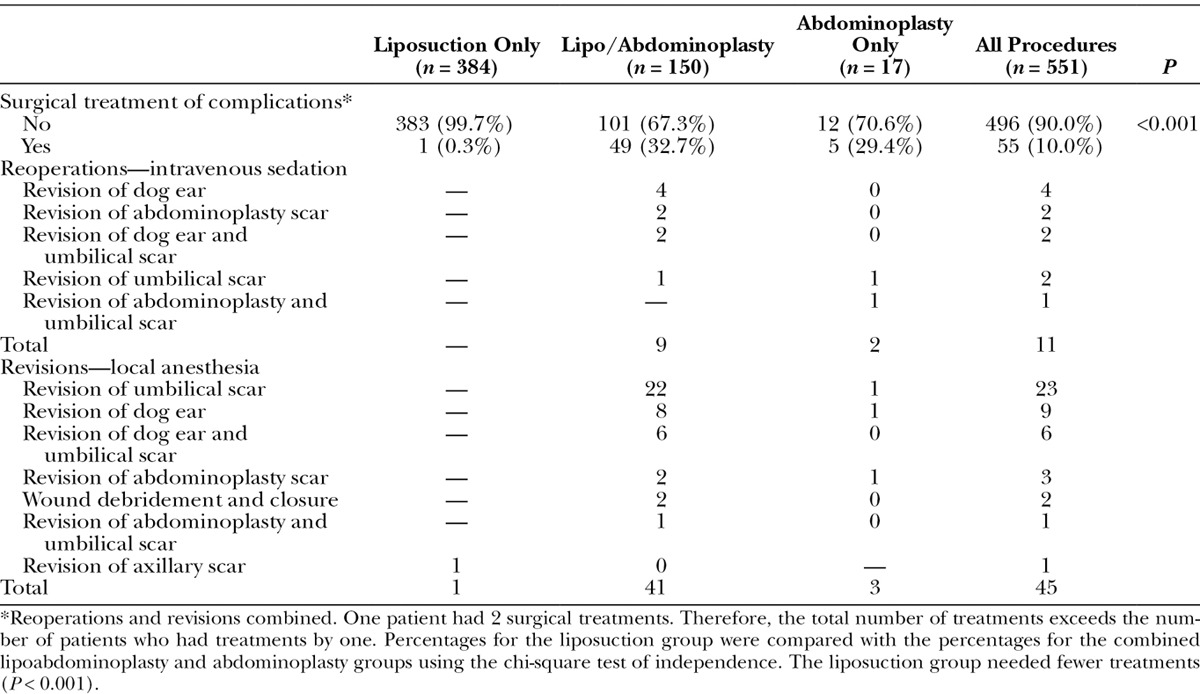
Complication rates after abdominoplasty vary widely, from 0% to 43%, depending largely on the investigator’s definition of a complication.13–27 Although a 50% complication rate is high, a wide net was used in assigning complications. The 10.8% infection rate includes patients with redness, indicating possible cellulitis, that were treated with antibiotics as a precaution. Patients who had minor spreading of the lateral aspect of their umbilical scar or a tiny bump at the end of the abdominoplasty scar were included. If such minor complications treated under local anesthesia in the office (Table 3) are excluded, the complication rate drops to approximately 25%. The author has a low threshold for performing touchups in the office, which are provided at no charge. In many cases, the patients did not mention any concerns regarding their scars; it was their surgeon’s opinion that they could be improved by revision. Patients are informed before surgery that these touchups are common and may be needed to optimize the scar quality. Patients do not typically regard such minor issues as complications. The complication rate as reported by patients after abdominoplasty was 21%.2
Table 3.
Treatment of Complications
Postoperative Nausea
Only 3% of patients reported nausea in the recovery room, compared with 35% in plastic surgery in general.28 No patient vomited in the recovery room. No patient required a postoperative hospital admission for treatment of nausea or dehydration.
Nausea is a major cause of patient dissatisfaction after surgery,18,29 and it is the most frequent cause of delayed discharge16 and unplanned hospital admissions.18 Avoiding an inhalational agent reduces the risk of nausea and vomiting,4 which is particularly important after abdominoplasty to avoid disrupting the muscle diastasis repair. Reducing the use of narcotics and benzodiazepines also reduces nausea and shortens recovery time. The mean length of stay in the recovery room was 50.7 minutes (range, 20–159 min), much shorter than reported stays for patients treated with conscious sedation using midazolam and fentanyl (mean, 235 min; range, 95–520 min).16 An improved balance of greater anesthesia at the tissue level and less anesthesia systemically improves patient comfort, expedites recovery, and reduces troublesome side effects from systemic analgesics.4
Seroma
Nine patients (5.4%) developed a seroma after an abdominoplasty, lower than the rate reported in most other series (range, 3.5–32%).5,13,18–21,25,27,30–36 In all cases, this problem was successfully treated with needle aspirations in the office, without a need for reoperation. In several patients this amounted to a nuisance (1 patient had a single aspiration of 3 cm3), not necessarily rising to the level of a complication as perceived by patients. Only 4 of these patients reported a seroma as a specific complication separate from delayed wound healing in 2 patients and an infection in 3 patients.2 Preservation of a layer of areolar tissue above the abdominal wall has long been recommended to reduce seroma rates.16,31,37,38
Saldanha et al39 describe a technique of performing abdominoplasty that limits tissue undermining and preserves the Scarpa fascia, as originally proposed by Le Louarn.38 These authors report a greatly reduced rate of seromas.39 Costa-Ferreira et al40 recently published a prospective randomized study of abdominoplasty patients, examining seroma risk in patients treated with and without preservation of the Scarpa fascia, reporting a significantly reduced rate of this complication in patients treated with preservation of the Scarpa fascia.
The physical basis for preservation of the Scarpa fascia on the abdominal wall on each side of the lower abdomen (this fascia is resected in the midline) is unclear. Any claim of improved lymphatic function or less opportunity for leak of lymphatic fluid by dissecting above this fascial plane does not have a known basis in anatomy or physiology.41 After traditional removal of the Scarpa fascia and deep fat, there would theoretically be no need for its lymphatic drainage. In fact, leaving behind this partially dissected layer of fat and connective tissue, which may be subjected to the additional trauma of open liposuction,39 might be expected to cause more exudate to leak into the wound. There is no evidence that the nature of the healing surfaces (fat or fascia)40 is relevant to seroma formation. Quilting sutures have also been recommended to reduce seromas,42–45 although there is a substantial extra commitment in operating time.44
Some investigators report an increased risk of seromas in patients treated with simultaneous liposuction27,36; others find no increased risk.21,46 The absence of seromas among patients treated with liposuction alone in this study attests to its safety. Today, most surgeons recognize the importance of treating the flanks with liposuction to eliminate the unattractive “muffin top” deformity. If the epigastrium is not treated with liposuction at the time of abdominoplasty, many patients will complain of persistent excessive fullness of the upper abdomen, which may appear even fuller in contrast to the reduced lower abdomen. Simultaneous liposuction of the flanks and epigastrium optimizes the surgical benefit and reduces the need for subsequent surgery. Limiting epigastric ultrasound (<1 min) and liposuction times (<2 min) minimizes risk.
A problem with preservation of the Scarpa fascia and deep fat on the abdominal wall is increased abdominal thickness as the superior abdominoplasty flap is transposed over the lower abdomen, stacking the 2 fascial layers. The quality of the wound closure may be compromised. Costa-Ferreira et al40 report a trend toward more wound healing problems among patients treated with Scarpa fascia preservation. Some proponents of lipoabdominoplasty recommend discarding the lower abdominal Scarpa fascia.47
Avoidance of Electrodissection
The use of Bovie dissection has been implicated as a possible cause of increased tissue necrosis and seromas.16,37 Electrodissection has long been recommended to reduce blood loss8 (before infusion of the abdomen with epinephrine solution was commonly performed) and is used by most plastic surgeons for flap dissection. However, cutting electrocautery produces an internal burn injury, with the usual pathophysiology of such an injury consisting of increased capillary permeability leading to fluid accumulation. Electrodissection causes more tissue destruction and seroma formation than scalpel dissection.48 When the seroma fluid is examined, it is found to resemble an exudate, containing proinflammatory cytokines,48 distinguishing it from purely lymphatic fluid.48,49
The author uses a scalpel exclusively for tissue dissection and a 9 ½ inch (24 cm) Potts-Smith monopolar, insulated, serrated, 2.0 mm handswitch cautery forceps (Kirwan Surgical Products, Marshfield, Mass.) for individual vessels. This technique is facilitated by a wetting solution that is given sufficient time to provide its hemostatic effect (at least 20 min).4 Doubling the concentration of epinephrine (1:526,000) makes vasoconstriction more effective without increasing the risk of skin loss or toxicity.4 The effects of this pretreatment can be profound; even the large superficial inferior epigastric vessels may constrict to the point that they sometimes do not bleed after scalpel transection (but are cauterized regardless). Estimations of blood loss reveal a mean additional blood loss of 290 cm3 from abdominoplasty performed at the time of liposuction.4 Reduced bleeding makes electrodissection unnecessary and avoids a major risk factor for seroma formation. It is also noteworthy that there were no hematomas in this large series of patients, suggesting that rebound bleeding after vasoconstriction is not a clinical problem. Only 4 of the 9 patients who developed a seroma reported it as a complication on their surveys,2 suggesting the problem did not have a major impact on their recovery and result.
The study by Costa-Ferreira et al40 attempts to definitively answer the question regarding any benefit of Scarpa fascia preservation,40 as hypothesized in their earlier study.50 The fact that the present study that does not include Scarpa fascia preservation also features a low seroma rate speaks against the conclusion that Scarpa fascia preservation alone is responsible for the reduced seroma rate. How can the study results be reconciled? Costa-Ferreira et al50 illustrate subfascial tissue resection using Bovie dissection. However, in the group treated with fascial preservation, the superficial tissue is mechanically distracted from the deep layer (“avulsed”), without electrodissection.50 The authors’ conclusions might therefore be explained by this confounding variable. There is no need for conjecture about lymphatic drainage patterns. Simply reducing the tissue burn explains the lower seroma rate and can explain the results of the present study, which otherwise seem contradictory. A reduced risk of seromas with scalpel dissection is not limited to abdominoplasty surgery; fewer seromas are also documented after mammaplasty.51,52
Any benefit from techniques that restrict undermining to a central strip in the upper abdomen may actually be a consequence of reduced tissue injury from electrodissection rather an improved blood supply to the abdominal flap. By overly limiting the degree of tissue undermining, flap mobilization and ultimately scar quality are compromised.
Deep Fascial Anchoring
One might reasonably ask why not preserve the Scarpa fascia out of an abundance of caution. There are 2 reasons: One is the increased abdominal thickness, as discussed above. The other reason is that the deep fascial repair can anchor the superior flap and prevent upward migration of the mons pubis (Figs. 4 and 5). Saldanha et al39 redrape the superior flap using a two-layer superficial fascial and skin closure with no deep fascial repair. These authors rely on their lateral wound closure to reduce central wound tension rather than a deep fascial repair. They remove additional skin at the end of the procedure in an attempt to lower the incision line. This method does not seem to be effective in avoiding a scar that is too high and difficult to conceal in a bikini. The hair-bearing pubic skin is displaced on to the lower abdomen (Fig. 6). This issue a practical concern for women and their clothing.
Fig. 4.
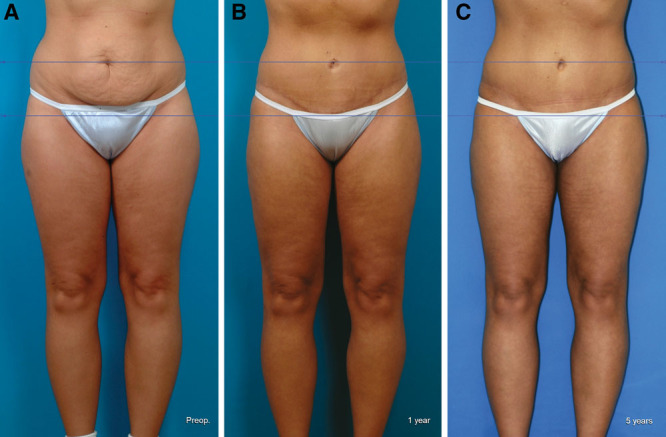
This 28-year-old woman is seen before (A), 1 y (B), and 5 y (C) after an abdominoplasty and liposuction of the lower body. She also underwent augmentation/mastopexies. Photographs are matched for size and orientation. The resected tissue weighed 1000 g. The total liposuction aspirate volume was 2550 cm3. The scar shows no evidence of superior migration. There is no displacement of the mons pubis.
Fig. 5.

This 63-year-old woman is seen before (A) and 3 mo after (B) an abdominoplasty and liposuction of the lower body. Photographs are matched for size and orientation. The resected tissue weighed 2700 g. The total liposuction aspirate volume was 2950 cm3.
Fig. 6.
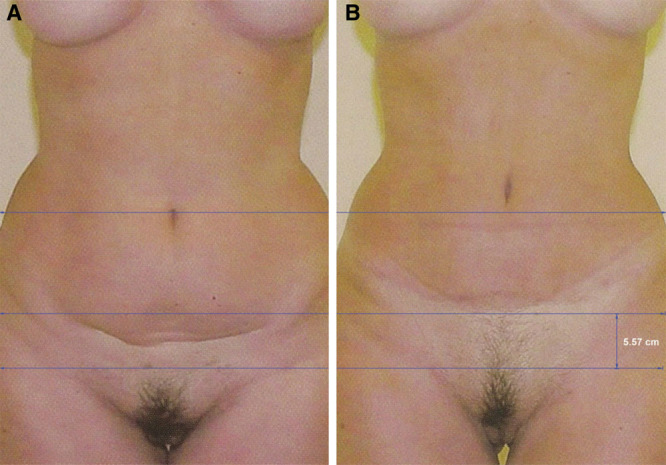
Example of published result of lipoabdominoplasty with limited undermining and preservation of the Scarpa fascia. The preoperative view (A) is matched for size and orientation to the postoperative view (B), allowing comparisons. The orientation of the mons pubis has been changed, which can be a benefit to such a woman with ptosis. However, the superior border of the mons pubis has been moved upward, extending the pubic hair on to the lower abdomen. The scar may be difficult to conceal in a bikini. Postoperatively, the umbilicus is positioned slightly higher, with an upward orientation. For calibration, a 34 cm width at the iliac crest level was used. (Saldanha OR, Federico R, Daher PF, et al. Lipoabdominoplasty. Plast Reconstr Surg. 2009;124:934–942.)
Video 4.

See video, Supplemental Digital Content 4, which demonstrates deep fascial anchoring, http://links.lww.com/PRSGO/A7.
Video 5.

See video, Supplemental Digital Content 5, which demonstrates wound closure, the umbilical repair, and 24-h follow-up, http://links.lww.com/PRSGO/A8.
The vertical level of the scar is more important than its horizontal length. It is essential to keep the scar low so that it may be concealed. Liposuction of the mons pubis avoids a contour mismatch with the reduced lower abdomen. A layered repair ideally causes temporary eversion of the tissues48 and avoids a depressed scar. With these measures, patient scar dissatisfaction may be limited to 4.3%.2
Preservation of the Scarpa fascia on the abdominal flap is needed to allow deep fascial closure, and may also better preserve the vascularity of the abdominal flap, explaining the low rate of delayed wound healing encountered in the present study. Flexed positioning of the operating table is important. It has long been appreciated that intraoperative patient positioning with the hips flexed (the “beach chair” position) is helpful.53 The author uses a more flexed position, a supine jackknife position. Simultaneous Trendelenburg positioning of the operating table and back elevation provide hip flexion up to 90 degrees (Fig. 3). This position may seem peculiar in the operating room, with the lower extremities elevated 45 degrees and one might reasonably wonder how long it will take for the patient to resume a fully erect position after surgery. The mean time for fully erect standing is 3 weeks.2 In the author’s experience, all women will trade an extra week of walking in a slightly stooped position for a scar that may be tucked within their panty line. Another advantage of such maximum intraoperative flexion is that an unattractive vertical midline scar (inverted-T) may be avoided in almost all cases.
Deep Venous Thrombosis
Chemoprophylaxis is being increasingly recommended to prevent thromboembolism.54 However, there are safer ways to reduce the risk of this complication, and ones that are aimed at the root of the problem—venous stasis.4,55
Limitations of the Study
Conclusions are applicable to liposuction and abdominoplasty performed using a superwet technique and ultrasonic assistance under a total intravenous anesthetic with scalpel dissection. Other surgical and anesthesia techniques are likely to have different outcomes.
Strengths of the Study
Because of its prospective nature, large sample sizes, consecutive patients, and the consistency of 1 surgeon and technique, this study benefits from a high degree of reliability and little opportunity for confounding factors that might affect the conclusions.
CONCLUSIONS
Liposuction and abdominoplasty, individually and in combination, may be performed safely with appropriate measures to reduce complications by minimizing tissue trauma. Scalpel dissection is preferred. Scarpa fascia preservation is unnecessary. A deep fascial repair can assist in keeping the abdominoplasty scar within the bikini line. Flexed patient positioning in surgery is essential. Deep venous thrombosis and other complications may be minimized using safe precautions without anticoagulation. Scar revisions, particularly of the umbilicus, remain common. (For the full video, see video 6, which demonstrates a patient undergoing liposuction of the abdomen, flanks, and inner thighs, followed by an abdominoplasty and medial thigh lifts. It includes preoperative marking, the preparation of the patient, details of the total intravenous anesthetic and infusion solutions, body positioning including the jackknife position, and details of the wound closure including deep fascial anchoring sutures. A short segment on the medial thigh lifts is provided and the patient is also seen in follow-up 24 h after surgery. The full video is available in the “Related Videos” section of the full-text article at http://www.PRSGO.com.)
Video 6.

See video, Liposuction, abdominoplasty, and medial thigh lifts. This video demonstrates a patient undergoing liposuction of the abdomen, flanks, and inner thighs, followed by an abdominoplasty and medial thigh lifts. It includes preoperative marking, the preparation of the patient, details of the total intravenous anesthetic and infusion solutions, body positioning including the jackknife position, and details of the wound closure including deep fascial anchoring sutures. A short segment on the medial thigh lifts is provided and the patient is also seen in follow-up 24 h after surgery. The full video is available in the “Related Videos” section of the full-text article on http://www.PRSGO.com.
ACKNOWLEDGMENTS
The author thanks Jane Zagorski, PhD, for statistical analyses; Lindsey Kroenke, BSN, for data collection; and Gwendolyn Godfrey for the illustration.
Supplemental Digital Content
Footnotes
Disclosure: The author has no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the author.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Swanson E. Prospective clinical study reveals significant reduction in triglyceride level and white cell count after liposuction and abdominoplasty and no change in cholesterol levels. Plast Reconstr Surg. 2011;128:182e–197e. doi: 10.1097/PRS.0b013e31822213c6. discussion 198e–200e. [DOI] [PubMed] [Google Scholar]
- 2.Swanson E. Prospective outcome study of 360 patients treated with liposuction, lipoabdominoplasty, and abdominoplasty. Plast Reconstr Surg. 2012;129:965–978. doi: 10.1097/PRS.0b013e318244237f. discussion 979–980. [DOI] [PubMed] [Google Scholar]
- 3.Swanson E. Photographic measurements in 301 cases of liposuction and abdominoplasty reveal fat reduction without redistribution. Plast Reconstr Surg. 2012;130:311e–322e. doi: 10.1097/PRS.0b013e3182589ef7. discussion 323e–324e. [DOI] [PubMed] [Google Scholar]
- 4.Swanson E. Prospective study of lidocaine, bupivacaine and epinephrine levels and blood loss in patients undergoing liposuction and abdominoplasty. Plast Reconstr Surg. 2012;130:702–722. doi: 10.1097/PRS.0b013e31825dc408. discussion 723–725. [DOI] [PubMed] [Google Scholar]
- 5.Heller JB, Teng E, Knoll BI, et al. Outcome analysis of combined lipoabdominoplasty versus conventional abdominoplasty. Plast Reconstr Surg. 2008;121:1821–1829. doi: 10.1097/PRS.0b013e31816b1350. [DOI] [PubMed] [Google Scholar]
- 6.Matarasso A. Abdominolipoplasty. Clin Plast Surg. 1989;16:289–303. [PubMed] [Google Scholar]
- 7.Chung KC, Kalliainen LK, Spilson SV, et al. The prevalence of negative studies with inadequate statistical power: an analysis of the plastic surgery literature. Plast Reconstr Surg. 2002;109:1–6; discussion 7–8. doi: 10.1097/00006534-200201000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Grazer FM. Abdominoplasty. In: McCarthy J, editor. Plastic Surgery. Philadelphia: Saunders; 1990. pp. 3929–3963. [Google Scholar]
- 9.Zocchi ML. Ultrasonic assisted lipoplasty. Technical refinements and clinical evaluations. Clin Plast Surg. 1996;23:575–598. [PubMed] [Google Scholar]
- 10.Roustaei N, Masoumi Lari SJ, Chalian M, et al. Safety of ultrasound-assisted liposuction: a survey of 660 operations. Aesthetic Plast Surg. 2009;33:213–218. doi: 10.1007/s00266-008-9293-9. [DOI] [PubMed] [Google Scholar]
- 11.Katz BE, Bruck MC, Felsenfeld L, et al. Power liposuction: a report on complications. Dermatol Surg. 2003;29:925–927. doi: 10.1046/j.1524-4725.2003.29253.x. discussion 927. [DOI] [PubMed] [Google Scholar]
- 12.Hanke W, Cox SE, Kuznets N, et al. Tumescent liposuction report performance measurement initiative: national survey results. Dermatol Surg. 2004;30:967–977. doi: 10.1111/j.1524-4725.2004.30300.x. discussion 978. [DOI] [PubMed] [Google Scholar]
- 13.Hensel JM, Lehman JA, Jr, Tantri MP, et al. An outcomes analysis and satisfaction survey of 199 consecutive abdominoplasties. Ann Plast Surg. 2001;46:357–363. doi: 10.1097/00000637-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Cooper JM, Paige KT, Beshlian KM, et al. Abdominal panniculectomies: high patient satisfaction despite significant complication rates. Ann Plast Surg. 2008;61:188–196. doi: 10.1097/SAP.0b013e318158a7b2. [DOI] [PubMed] [Google Scholar]
- 15.Momeni A, Heier M, Torio-Padron N, et al. Correlation between complication rate and patient satisfaction in abdominoplasty. Ann Plast Surg. 2009;62:5–6. doi: 10.1097/SAP.0b013e318174f973. [DOI] [PubMed] [Google Scholar]
- 16.Byun MY, Fine NA, Lee JY, et al. The clinical outcome of abdominoplasty performed under conscious sedation: increased use of fentanyl correlated with longer stay in outpatient unit. Plast Reconstr Surg. 1999;103:1260–1266. doi: 10.1097/00006534-199904040-00026. [DOI] [PubMed] [Google Scholar]
- 17.Floros C, Davis PK. Complications and long-term results following abdominoplasty: a retrospective study. Br J Plast Surg. 1991;44:190–194. doi: 10.1016/0007-1226(91)90125-4. [DOI] [PubMed] [Google Scholar]
- 18.Kryger ZB, Fine NA, Mustoe TA. The outcome of abdominoplasty performed under conscious sedation: six-year experience in 153 consecutive cases. Plast Reconstr Surg. 2004;113:1807–1817. doi: 10.1097/01.prs.0000117303.63028.7d. discussion 1818–1819. [DOI] [PubMed] [Google Scholar]
- 19.Spiegelman JI, Levine RH. Abdominoplasty: a comparison of outpatient and inpatient procedures shows that it is a safe and effective procedure for outpatients in an office-based surgery clinic. Plast Reconstr Surg. 2006;118:517–522. doi: 10.1097/01.prs.0000227630.88566.74. discussion 523. [DOI] [PubMed] [Google Scholar]
- 20.Stewart KJ, Stewart DA, Coghlan B, et al. Complications of 278 consecutive abdominoplasties. J Plast Reconstr Aesthet Surg. 2006;59:1152–1155. doi: 10.1016/j.bjps.2005.12.060. [DOI] [PubMed] [Google Scholar]
- 21.Kim J, Stevenson TR. Abdominoplasty, liposuction of the flanks, and obesity: analyzing risk factors for seroma formation. Plast Reconstr Surg. 2006;117:773–779. doi: 10.1097/01.prs.0000200056.57357.3f. discussion 780. [DOI] [PubMed] [Google Scholar]
- 22.Matarasso A, Swift RW, Rankin M. Abdominoplasty and abdominal contour surgery: a national plastic surgery survey. Plast Reconstr Surg. 2006;117:1797–1808. doi: 10.1097/01.prs.0000209918.55752.f3. [DOI] [PubMed] [Google Scholar]
- 23.Neaman KC, Hansen JE. Analysis of complications from abdominoplasty: a review of 206 cases at a university hospital. Ann Plast Surg. 2007;58:292–298. doi: 10.1097/01.sap.0000239806.43438.54. [DOI] [PubMed] [Google Scholar]
- 24.Bragg TW, Jose RM, Srivastava S. Patient satisfaction following abdominoplasty: an NHS experience. J Plast Reconstr Aesthet Surg. 2007;60:75–78. doi: 10.1016/j.bjps.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 25.Weiler J, Taggart P, Khoobehi K. A case for the safety and efficacy of lipoabdominoplasty: a single surgeon retrospective review of 173 consecutive cases. Aesthet Surg J. 2010;30:702–713. doi: 10.1177/1090820X10381879. [DOI] [PubMed] [Google Scholar]
- 26.Trussler AP, Kurkjian TJ, Hatef DA, et al. Refinements in abdominoplasty: a critical outcomes analysis over a 20-year period. Plast Reconstr Surg. 2010;126:1063–1074. doi: 10.1097/PRS.0b013e3181e60537. [DOI] [PubMed] [Google Scholar]
- 27.Najera RM, Asheld W, Sayeed SM, et al. Comparison of seroma formation following abdominoplasty with or without liposuction. Plast Reconstr Surg. 2011;127:417–422. doi: 10.1097/PRS.0b013e3181f95763. [DOI] [PubMed] [Google Scholar]
- 28.Steely RL, Collins DR, Jr, Cohen BE, et al. Postoperative nausea and vomiting in the plastic surgery patient. Aesthetic Plast Surg. 2004;28:29–32. doi: 10.1007/s00266-004-3015-8. [DOI] [PubMed] [Google Scholar]
- 29.Mustoe TA, Buck DW, Lalonde DH. The safe management of anesthesia, sedation, and pain in plastic surgery. Plast Reconstr Surg. 2010;126:165e–176e. doi: 10.1097/PRS.0b013e3181ebe5e9. [DOI] [PubMed] [Google Scholar]
- 30.Stevens WG, Repta R, Pacella SJ, et al. Safe and consistent outcomes of successfully combining breast surgery and abdominoplasty: an update. Aesthet Surg J. 2009;29:129–134. doi: 10.1016/j.asj.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 31.Fang RC, Lin SJ, Mustoe TA. Abdominoplasty flap elevation in a more superficial plane: decreasing the need for drains. Plast Reconstr Surg. 2010;125:677–682. doi: 10.1097/PRS.0b013e3181c82f78. [DOI] [PubMed] [Google Scholar]
- 32.Beer GM, Wallner H. Prevention of seroma after abdominoplasty. Aesthet Surg J. 2010;30:414–417. doi: 10.1177/1090820X10374116. [DOI] [PubMed] [Google Scholar]
- 33.Cárdenas Restrepo JC, García Gutiérrez MM. Abdominoplasty with anchor plication and complete lipoplasty. Aesthet Surg J. 2004;24:418–422. doi: 10.1016/j.asj.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 34.Stokes RB, Williams S. Does concomitant breast surgery add morbidity to abdominoplasty? Aesthet Surg J. 2007;27:612–615. doi: 10.1016/j.asj.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Antonetti JW, Antonetti AR. Reducing seroma in outpatient abdominoplasty: analysis of 516 consecutive cases. Aesthet Surg J. 2010;30:418–425. doi: 10.1177/1090820X10372048. [DOI] [PubMed] [Google Scholar]
- 36.Neaman KC, Armstrong SD, Baca ME, et al. Outcomes of traditional cosmetic abdominoplasty in a community setting: a retrospective analysis of 1008 patients. Plast Reconstr Surg. 2013;131:403e–410e. doi: 10.1097/PRS.0b013e31827c6fc3. [DOI] [PubMed] [Google Scholar]
- 37.Buck DW, II, Mustoe TA. An evidence-based approach to abdominoplasty. Plast Reconstr Surg. 2010;126:2189–2195. doi: 10.1097/PRS.0b013e3181f83115. [DOI] [PubMed] [Google Scholar]
- 38.Le Louarn C. Partial subfascial abdominoplasty. Aesthetic Plast Surg. 1996;20:123–127. doi: 10.1007/BF02275530. [DOI] [PubMed] [Google Scholar]
- 39.Saldanha OR, Federico R, Daher PF, et al. Lipoabdominoplasty. Plast Reconstr Surg. 2009;124:934–942. doi: 10.1097/PRS.0b013e3181b037e3. discussion 943-945. [DOI] [PubMed] [Google Scholar]
- 40.Costa-Ferreira A, Rebelo M, Silva A, et al. Scarpa fascia preservation during abdominoplasty: randomized clinical study of efficacy and safety. Plast Reconstr Surg. 2013;131:644–651. doi: 10.1097/PRS.0b013e31827c704b. [DOI] [PubMed] [Google Scholar]
- 41.Aly A. Discussion. Scarpa fascia preservation during abdominoplasty: a prospective study. Plast Reconstr Surg. 2010;125:1240–1241. doi: 10.1097/PRS.0b013e3181d0aa3c. [DOI] [PubMed] [Google Scholar]
- 42.Pollock H, Pollock T. Progressive tension sutures: a technique to reduce local complications in abdominoplasty. Plast Reconstr Surg. 2000;105:2583–2586. doi: 10.1097/00006534-200006000-00047. discussion 2587. [DOI] [PubMed] [Google Scholar]
- 43.Nahas FX, Ferreira LM, Ghelfond C. Does quilting suture prevent seroma in abdominoplasty? Plast Reconstr Surg. 2007;119:1060–1064; discussion 1065. doi: 10.1097/01.prs.0000242493.11655.68. [DOI] [PubMed] [Google Scholar]
- 44.Andrades P, Prado A, Danilla S, et al. Progressive tension sutures in the prevention of postabdominoplasty seroma: a prospective, randomized, double-blind clinical trial. Plast Reconstr Surg. 2007;120:935–946. doi: 10.1097/01.prs.0000253445.76991.de. discussion 947. [DOI] [PubMed] [Google Scholar]
- 45.Di Martino M, Nahas FX, Barbosa MV, et al. Seroma in lipoabdominoplasty and abdominoplasty: a comparative study using ultrasound. Plast Reconstr Surg. 2010;126:1742–1751. doi: 10.1097/PRS.0b013e3181efa6c5. [DOI] [PubMed] [Google Scholar]
- 46.Samra S, Sawh-Martinez R, Barry O, et al. Complication rates of lipoabdominoplasty versus traditional abdominoplasty in high-risk patients. Plast Reconstr Surg. 2010;125:683–690. doi: 10.1097/PRS.0b013e3181c82fb0. [DOI] [PubMed] [Google Scholar]
- 47.Matos WN., Jr . Presented at Meeting of the American Society for Aesthetic Plastic Surgery. Vancouver, BC: 2012. May 6, Lipoabdominoplasty and body contouring. [Google Scholar]
- 48.Özdoğan M, Yilimaz KB, Ozaslan C, et al. Scalpel versus electrocautery dissection: the effect on wound complications and pro-inflammatory cytokine levels in wound fluids. Turk J Med Sci. 2008;38:111–116. [Google Scholar]
- 49.Prado A, Andrades P. Composition of postabdominoplasty seroma. Aesthetic Plast Surg. 2007;31:514–518. doi: 10.1007/s00266-007-0078-3. [DOI] [PubMed] [Google Scholar]
- 50.Costa-Ferreira A, Rebelo M, Vásconez LO, et al. Scarpa fascia preservation during abdominoplasty: a prospective study. Plast Reconstr Surg. 2010;125:1232–1239. doi: 10.1097/PRS.0b013e3181d0ac59. [DOI] [PubMed] [Google Scholar]
- 51.Lejour M. Vertical mammaplasty: early complications after 250 personal consecutive cases. Plast Reconstr Surg. 1999;104:764–770. doi: 10.1097/00006534-199909030-00023. [DOI] [PubMed] [Google Scholar]
- 52.Swanson E. Prospective clinical study of 784 consecutive cases of breast augmentation and vertical mammaplasty, performed individually and in combination. Plast Reconstr Surg. 2013;132:30e–45e. doi: 10.1097/PRS.0b013e3182910b2e. [DOI] [PubMed] [Google Scholar]
- 53.Richter DF, Stoff A. Abdominoplasty procedures. In: Neligan PC, Warren RJ, editors. Plastic Surgery. 3rd ed. Vol. 2. London: Elsevier Saunders; 2013. pp. 530–558. [Google Scholar]
- 54.Pannucci CJ, Dreszer G, Wachtman CF, et al. Postoperative enoxaparin prevents symptomatic venous thromboembolism in high-risk plastic surgery patients. Plast Reconstr Surg. 2011;128:1093–1103. doi: 10.1097/PRS.0b013e31822b6817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Swanson E. Reducing venous thromboembolism risk without chemoprophylaxis. Plast Reconstr Surg. 2013;131:450e–451e. doi: 10.1097/PRS.0b013e31827c7224. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


