Abstract
Summary:
This study introduces the options for supercharging and augmenting venous drainage of an anterolateral thigh free flap. Clinical indications and options for additional microvascular anastomoses are reviewed in 5 consecutive patients. The indications were simultaneous mucosal and cutaneous defects, divergent mucosal defects, and extensively wide and long cutaneous defects. Three additional vascular pedicles were anastomosed: the transverse branch of the lateral circumflex (n = 3), a perforator coming directly off the superficial femoral artery (n = 1), and a posterior perforator from the profundus femoral artery (n = 1). The anastomosis of a separate pedicle from the superior, medial, and/or posterior-lateral thigh may be a useful technique when confronted with an extensive defect that may not reliably be reconstructed with a routine anterolateral thigh flap based on a single perforator.
The anterolateral thigh (ALT) free flap has become the most widely used fasciocutaneous free flap for head and neck reconstruction.1 However, there has been no report demonstrating the indications or options for increasing arterial inflow and venous outflow to an ALT flap based on separate vascular pedicles.
The overall size of the ALT flap is dependent on the number and location of perforators. Large series of ALT free flaps report flaps with average dimensions of approximately 8 × 23 cm.2 What remains uncertain is the maximum dimensions of an ALT flap that can be harvested based on a single perforator. Moreover, given that the perforators of the ALT flap sequentially arise from the descending branch of the circumflex artery as it descends down the thigh, it is likely that a long ALT flap can be more reliably harvested than a wide ALT flap. Multiple skin islands can also be created from an ALT flap either with a strip of de-epithelialization between the 2 skin islands or with complete division of the skin paddle if 2 separate perforators exist, each supplying a separate island of skin.
The purpose of this article is to introduce the options and indications for supercharging and venous augmenting an ALT flap when confronted with an extensive head and neck defect that may not reliably be reconstructed with a routine ALT flap based on a single perforator.
METHODS
We present 5 consecutive patients who underwent reconstruction with an ALT flap with an additional vascular pedicle at the University of Colorado between July 2009 and October 2013. Clinical indications and outcomes included site of defect, size of flap, vessels used for anastomosis, flap success rate, and complications.
Surgical Planning for Harvesting an ALT Flap with a Second Vascular Pedicle
The harvest of an ALT flap with a second pedicle begins with the identification with a Doppler of possible perforators (Fig. 1) in the superior, medial, and posterior-lateral thigh. A template of the head and neck defect is then transferred to the thigh where it is centered over the dominant ALT perforator(s) identified by Doppler. If because of the size of the defect, the anticipated free flap overlies the site of perforators in the superior, medial, and/or posterior-lateral thigh (in addition to those perforators supplying a midthigh ALT), then these perforators are dissected back to their pedicle of origin so that a second pedicle can be used for anastomosis.
Fig. 1.
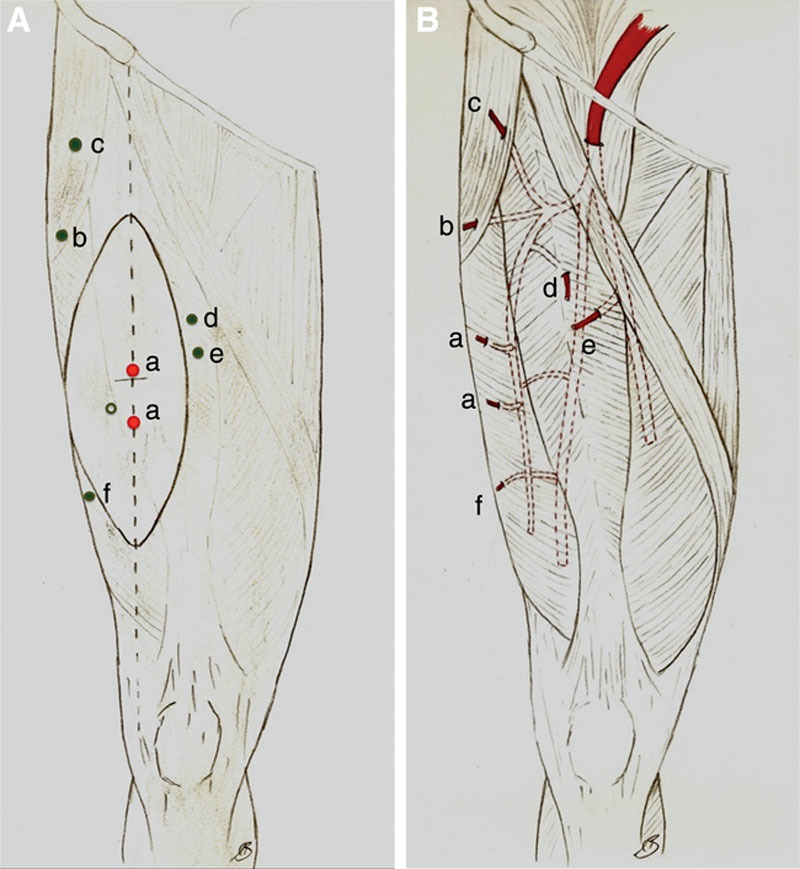
Microvascular options for supercharging an ALT flap. A, Skin paddle for an ALT free flap based on a perforator(s) from the descending branch from the lateral circumflex artery (labeled a). b, Perforator from transverse branch of LCFA. c, Perforator from the ascending branch of LCFA. d, Perforator from rectus femoris branch of the descending branch of LCFA. e, Perforator from superficial femoral artery. f, Perforator from profunda femoris. B, Possible pedicles for a second anastomosis. LCFA indicates lateral circumflex femoral artery.
RESULTS
A single dominant perforator from the descending branch of the circumflex was captured in each ALT flap and a second perforator based on a second pedicle (Table 1). Three additional vascular pedicles were anastomosed: the transverse branch of the lateral circumflex sending a perforator through the distal fascia latae (Fig. 2), a branch coming directly off the superficial femoral artery (SFA) (n = 1) sending a perforator through the rectus femoris muscle, and a branch originating from the profundus femoral artery sending a perforator to the lateral thigh that traversed the vastus lateralis and biceps femoris (n = 1). The indications were simultaneous mucosal and cutaneous defects (patients 1 and 3), divergent mucosal defects (patient 2), extensively wide and long cutaneous defects (patients 1 and 4), and the intraoperative concern that the main arterial pedicle to the ALT would prove to be inadequate (ie, vessel diameter < 1 mm; patient 5). All flaps were successfully harvested (ie, no flap failures, fistulas, and acute wound breakdowns).
Table 1.
Patients, Defects, and Flap Characteristics
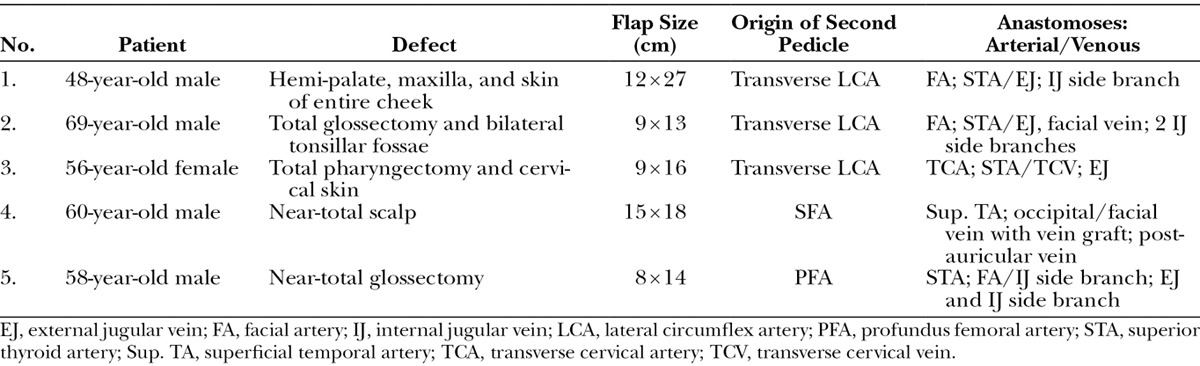
Fig. 2.
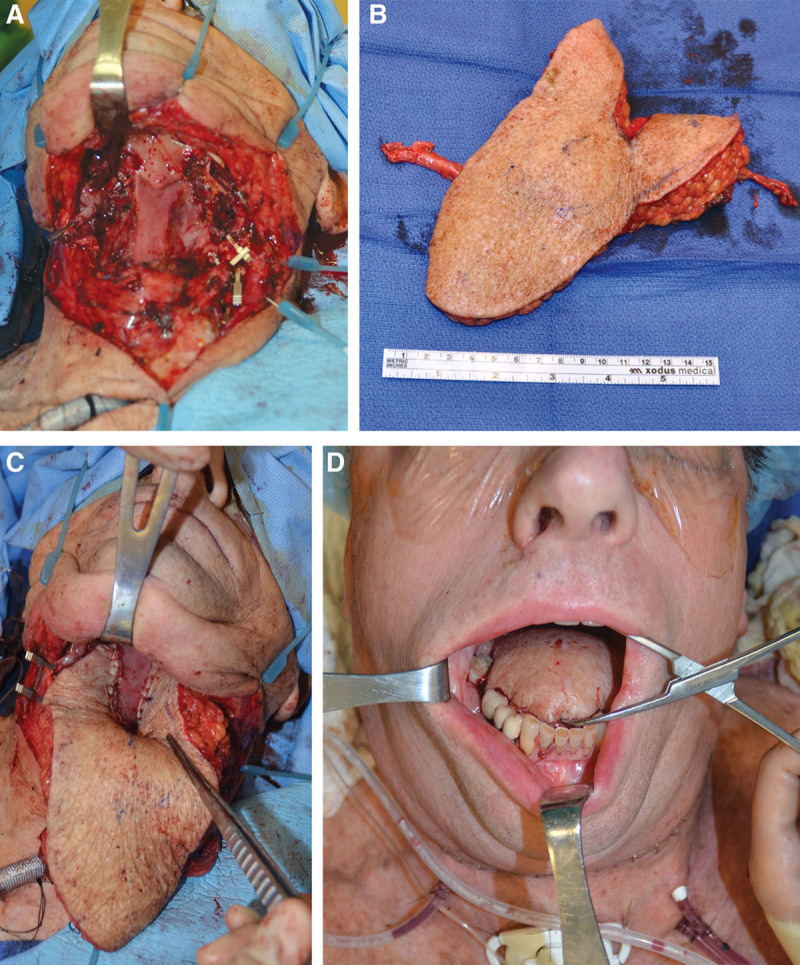
Case 2. A, Total glossectomy and bilateral tonsillar fossae defect with exposure of bilateral carotid arteries. B, ALT free flap with pedicles from the transverse and descending circumflex system. C, Flap inset into the tonsillar fossae. D, Tongue reconstruction.
DISCUSSION
In this study, the primary advantages of incorporating a second vascular pedicle were the ability to increase the surface area of the flap and/or reliably to allow independent movement of different cutaneous sections of the flap. Such advantages may not be realized with a routine ALT flap raised on one perforator. Given that the majority of head and neck defects are usually 9 cm or less in width,3 a clinical study has not yet evaluated the maximum width of an ALT flap.
As illustrated in patient 4, a separate medial pedicle can also be harvested, which allowed the width of the ALT flap in this case to be 15 cm. The vascular supply of a medial pedicle comes from perforating arteries that can potentially arise from 2 locations: the rectus femoris branch of the descending branch of the lateral circumflex femoral artery or directly off the SFA.4 Flaps based on perforators arising from the SFA have short pedicles of 3–5 cm. One needs to consider this short length in choosing how to inset the flap and which vessels will be used for the second anastomosis. In our case, the second anastomosis was done to the occipital artery and a postauricular vein.
The superior and posterior-lateral pedicles that were used for an additional anastomosis were based on perforators that respectively arose from the transverse branch of the lateral circumflex femoral artery and from the profundus femoral artery. Each of these pedicles could have supported a proximal ALT and a lateral thigh free flap, respectively.5 If present, perforators from the ascending6 or oblique branch from the lateral circumflex system could also serve as a second pedicle to supercharge an ALT flap.
The main indications for a second pedicle were simultaneous mucosal and cutaneous defects and divergent mucosal defects. Total pharyngeal defects with an anterior cervical skin defect can be reconstructed with tubed ALT with an area of the flap de-epithelialized to allow the flap to be turned over for cervical skin replacement. In our case, the area between the 2 perforators was de-epithelialized, but each skin island was also provided an independent venous outflow and arterial inflow because of the additional anastomoses. In similar manner, coverage of the carotid arteries bilaterally exposed in the tonsillar fossae was successfully performed by partially dividing the ALT flap between the 2 perforators which were each perfused by separate pedicles.
CONCLUSIONS
The anastomosis of a separate pedicle from the superior, medial, and/or posterior-lateral thigh may be a useful technique when confronted with an extensive defect that may not reliably be reconstructed with a routine ALT flap based on a single perforator.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Chana JS, Wei FC. A review of the advantages of the anterolateral thigh flap in head and neck reconstruction. Br J Plast Surg. 2004;57:603–609. doi: 10.1016/j.bjps.2004.05.032. [DOI] [PubMed] [Google Scholar]
- 2.Lakhiani C, Lee MR, Saint-Cyr M. Vascular anatomy of the anterolateral thigh flap: a systematic review. Plast Reconstr Surg. 2012;130:1254–1268. doi: 10.1097/PRS.0b013e31826d1662. [DOI] [PubMed] [Google Scholar]
- 3.Lundgren TK, Wei FC. Oversized design of the anterolateral thigh flap for head and neck reconstruction. J Craniofac Surg. 2013;24:134–135. doi: 10.1097/SCS.0b013e318268d273. [DOI] [PubMed] [Google Scholar]
- 4.Yu P, Jesse S. Perforator patterns of the anteromedial thigh flap. Plast Reconstr Surg. 2011;128:151–157. doi: 10.1097/PRS.0b013e318221dd11. [DOI] [PubMed] [Google Scholar]
- 5.Miller MJ, Reece GP, Marchi M, et al. Lateral thigh free flap in head and neck reconstruction. Plast Reconstr Surg. 1995;96:334–340. doi: 10.1097/00006534-199508000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Hubmer MG, Schwaiger N, Windisch G, et al. The vascular anatomy of the tensor fasciae latae perforator flap. Plast Reconstr Surg. 2009;124:181–189. doi: 10.1097/PRS.0b013e3181ab114c. [DOI] [PubMed] [Google Scholar]


